Spinal Hemangiopericytoma: a Rare Ocurrence. Antônio Santos de
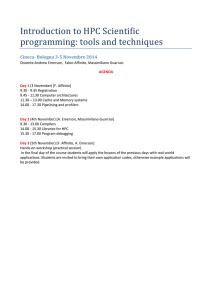
advertisement

Spinal Hemangiopericytoma: a Rare Ocurrence. Antônio Santos de Araújo Júnior, MD1; Arnaldo Salvestrini Jr, MD1; Pedro Alberto Arlant, MD, PhD1; Orlando Parisi, MD2; Mirella Martins Fazzito, MD3; Conrado Furtado de Albuquerque Cavalcanti, MD4; Hae Won Lee, MD4; Ricardo Antenor de Souza e Souza, MD5; Luiz Heraldo Arouche da Câmara Lopes, MD, PhD5. 1. Neurosurgeon from Sírio Libanês Hospital, São Paulo, Brazil 2. Head and Neck Surgeon from Sírio Libanês Hospital, São Paulo, Brazil 3. Neurologist from Sírio Libanês Hospital, São Paulo, Brazil 4. Radiologist from Sírio Libanês Hospital, São Paulo, Brazil 5. Neuropathologist from Sírio Libanês Hospital, São Paulo, Brazil Antônio Santos de Araújo Júnior Correspondence Address: Rua Peixoto Gomide, 515, cj 96, Cerqueira César, São Paulo, São Paulo, Brazil. CEP 01409-001. Phone/Fax: 05511-32890411 Cel: 05511-84567404 Email: dr.antonioaraujojr@gmail.com; Website: araujoefazzito.com.br Abstract Introduction: Most hemangiopericytomas (HPC) are located in the musculoskeletal system and the skin, while the location in the central nervous system (CNS) is rare. Objective and Methods: We describe a patient suffering from a spinal extradural huge HPC, with marked spinal cord compression, extending from C6 to T3 level, who was elected to surgery. Results: Patient was submitted to surgery, via a posterior approach, indentifying a huge red-brown firm mass, highly vascular, that was softly dissected from surrounding tissues. Total gross removal was accomplished, with “in-block” resection, preserving neurological function, as shown by somatosensitive evoked potential. Histopathological examination and immunohistochemistry essay were performed confirming the diagnosis of Hemangiopericytoma. Conclusion: Spinal HPCs respond to approximately 8% of all HPC, tend to occur isolated and attached to spinal dura-mater, and usually present a good surgical cleavage between the tumor and the dura. Key-words: CNS tumor, spinal tumor, hemangiopericytoma. Introduction Most hemangiopericytomas (HPC) are located in the musculoskeletal system and the skin, while the location in the central nervous system (CNS) is rare. The latter represents 2 to 4% in large series of meningeal tumors, thus accounting for less than 1% of all CNS tumors. In the CNS, tumors with a hemangiopericytomatous histopathological pattern can be either hemangiopericytomas, or solitary fibrous tumors 1. Another differential diagnosis of CNS tumors with hemangiopericytoma-like pathological characteristics, originating especially in the lumbar spine, is the synovial sarcoma 2. Solitary fibrous tumour (SFT) is a rare soft tissue tumour of uncertain histogenesis and unpredictable biological behavior, which was first described in the pleura and subsequently in many extra-pleural locations 3. Solitary fibrous tumours (SFT) of the central nervous system are rare neoplasms that usually present as dura-based masses and clinically resemble meningiomas. Histologically, they can be similar to haemangiopericytoma or fibrous meningioma 4. A synovial sarcoma is a mesenchymal spindle cell tumor that displays variable epithelial differentiation including glandular formation. It is unrelated to a synovium. More than 80% of these lesions arise in the deep soft tissue of the extremities. The tumor frequently arises adjacent to joints or tendon sheaths, especially in the lumbar spine 2. CNS hemangiopericytomas (HPC), by definition, are highly cellular and vascularized mesenchymal tumour exhibiting a characteristic monotonous lowpower appearance and a well-developed, variably thick-walled, branching “staghorn” vasculature; almost always attached to the dura and having a high tendency to locally recur and to metastasize outside the CNS 5. Thirty years-ago HPC were still classified as variant of ‘angioblastic meningiomas’, but it has now been long accepted that hemangiopericytoma and meningioma are different entities 5. In large series, the ratios of meningeal hemangiopericytoma to meningioma were about 1:40 6. Epidemiological differences between hemangiopericytomas and meningiomas include: HPC tend to occur at a younger age than meningiomas; HPC are slightly more often in men than in women. Meningiomas tend to occur eventually in every location of the neuroaxis, instead of HPC that occur slightly more often in the occipital region, around the confluence of sinuses, and attached to venous sinuses 5. By its time, HPC are almost invariably solitary, with approximately 8% located attached to spinal dura 6. On radiographic films, HPC appear as a well-demarcated, lytic lesion of adjacent bone, without hyperostosis, a typical feature of meningiomas. Unlike meningiomas, HPC typically lack calcification 5. On macroscopic examination, meningeal HPC is a solid, welldemarcated tumor, with a tendency to bleed during removal, sometimes profusely 5. The tumor is usually globoid, slightly lobulated, with firm consistency, grayish to red-brown colored. On histopathology, HPC appears as monomorphous tumors composed of closed packed, randomly oriented tumor cells, with little intervening fibrosis and marked extracellular matrix. A rich network of reticulin fibers, typically investing individual cells, is one of the most characteristic features of this tumor 5. HPCs are very highly vascular tumors, with numerous slit-like vascular channels lined by flattened endothelial cells and branching vascular spaces, the “staghorn sinusoids” 5. Necroses are uncommon. Calcification, including psammoma bodies, is not seen. They may destroy adjacent bone, without hyperostotic reaction, but rarely invade adjacent brain parenchyma or the spinal cord 5. On immunohistochemistry essay, HPC cells are diffusely immunoreactive for vimentin (85% of cases), factor XIIIa (80-100%) in individual scattered cells, Leu-7 (70%) and CD34 (33-100%) in a patchy pattern. Diffuse CD34 pattern diagnoses solitary fibrous tumor. Meanwhile, strong and diffuse immunoreactivity for epithelial membrane antigen, claudin-1, desmin, smooth muscle actin, endothelial antigens (CD31) and progesterone receptor diagnose meningioma. Immunohistochemistry differentiation of HPC from solitary fibrous tumor and meningioma is usually feasible and possible. Spinal hemangiopericytomas Spinal HPCs respond to approximately 8% of all HPC, tend to occur isolated and attached to spinal dura-mater, and usually present a good surgical cleavage between the tumor and the dura. Spinal HPCs are very rare and mostly involve the extradural bony structures. Primary intradural HPC has only been reported in 10 cases, all of which occurred in the extramedullary region 7. We describe a patient suffering from a spinal extradural huge HPC, with marked spinal cord compression, extending from C6 to T3 level, who was elected to surgery. Case report We describe a 66-year-old male patient harboring a chronic onset of right leg distal paresis, and instable gait. On neurological examination, he presented with right leg monoparesis (strength grade 4 distal, 5 proximal), intact pain and light touch sensitivity, loss of unconscious proprioception, with deep tendon patellar hyperreflexia, and abnormal Romberg´s test with sensory ataxia. The patient was promptly submitted to cervicothoracic MRI, showing a huge paravertebral mass, ranging from C6 to T3 level, with homogeneous Gadolinium enhancement, and marked spinal cord compression at T1 level (Figure 1-2). A B C Figure 1. Sagital cervicothoracic T2-weighted (A and B) and post-contrast T2weighted (C) MRI. (A) Paravertebral cervico thoracic mass, with lobulated appearance; (B) At T1 level, tumoral spinal cord compression without dural invasion, intratumoral heterogeneous signal; (C) Post-Gadolinium, homogeneous tumoral enhancement. A B C Figure 2. Axial cervicothoracic T2-weighted MRI (A and B) and post-contrast T1weighted MRI (C). (A) Paravertebral mass with lytic lesion from right T1 lamina and spinous process, dislocating the spinal cord to anterior left position; (B) At T1 level, marked spinal cord compression by heterogeneous signal lesion; (C) PostGadolinium, homogeneous tumoral enhancement. In the same day, patient was prepared to surgery, and to general anesthesia, with intraoperative somatosensitive evoked potential and intermittent pneumatic leg compression. Patient was turned to prone position. Patient was then submitted to surgery, via a posterior approach, indentifying a huge red-brown firm mass, highly vascular, with profuse bleeding even through small cuts. Therefore, surgical strategy was, every moment, in a patient fashion, to contour the lesion, without cutting it. At last, T1 laminectomy was performed in order to dissect the tumor from the dura-mater, with clear cleavage plane. Total gross removal was accomplished, with “in-block” resection (Figure 3), preserving adjacent tissues and the neurological function, as shown by somatosensitive evoked potential. Histopathological examination and immunohistochemistry essay were performed confirming the diagnosis of HPC (Figure 4-5). Postoperatively, patient was symptom-free, with accomplishing normal daily activities within 2 weeks. Figure 3. Total gross ‘in block’ resection, measuring almost 10 cm. normal gait, A B Figure 4. Hematoxylin and eosin (HE) stain histopathology. (A) 40x magnification, monomorphous tumor composed of closed packed, randomly oriented tumor cells; (B) 100x magnification, highly cellular tumor with staghorn-type vessels, little intervening fibrosis and marked extracellular matrix, and with lipomatous deposition. A B C Figure 5. (A) HE stain, 400x, closed packed monomorphous cells with lipomatous deposition; (B) Immunohistochemistry essay, 400x, patchy pattern immunoreactivity for CD34; (C) Immunoreactivity for CD31, 400x, patchy pattern. Prognosis HPCs tend to grow faster than anaplastic meningiomas, instead the same median Ki-67 labelling index of 5% (1.2-39%)8. Therefore they recur more frequently and in short time intervals, with median time of recurrence of 40 to 70 months. The local recurrence occurs in approximately 85 to 91% of cases after 15 years 6,9. Radiotherapy appears to postpone recurrence, in one series, 9 of 17 irradiated HPCs recurred with a median of 58 months, but 13 of 15 nonirradiated tumors recurred with a median of only 29 months 6. Eventually meningeal HPCs can metastasize to the bones, lungs and liver. Overall, in a series of 28 patients harboring intracranial HPCs, the probability of tumor-related death was 61% at 15 years 9, and the survival after the diagnosis of metastases was only 2 years 9. Nonetheless, all clinical series about HPCs report recurrences rates, predictive and prognostic factors of intracranial tumors. Up to now there is no information over this issue exclusively about spinal HPCs. Conclusion Spinal HPCs respond to approximately 8% of all HPC. They tend to occur isolated and attached to spinal dura-mater, and usually present a good surgical cleavage between the tumor and the dura, and between the tumor and the surrounding tissues, allowing almost always total resection. References 1. Mekni A, Kourda J, Chelly I, et al. Hemangiopericytoma in the central nervous system. A study of eight cases. Neurochirurgie 2008; 54(1):1520. 2. Sakellaridis N, Mahera H, Pomonis S. Hemangiopericytoma-like synovial sarcoma of the lumbar spine. Case report. J Neurosurg Spine 2006; 4(2):179-82. 3. Aftab S, Casey A, Tirabosco R, et al. Fat-forming solitary fibrous tumour (lipomatous haemangiopericytoma) of the spine: case report and literature review. Skeletal Radiol. 2010; 39(10):1039-42. 4. Mekni A, Kourda J, Hammouda KB, et al. Solitary fibrous tumour of the central nervous system: pathological study of eight cases and review of the literature. Pathology 2009; 41(7):649-54. 5. Giannini C, Rushing EJ, Hainfellner JA. Haemangiopericytoma. In:Louis DN, Ohgaki H, Wiestler OD, Cavenee WK, ed. WHO Classification of tumours of the central nervous system. 3rd ed. Lyon, FR. IARC; 2007: 178-180. 6. Guthrie BL, Ebersold MJ, Scheithauer BW, et al. Meningeal hamangiopericytoma: histopathological features, treatment, and long term follow-up of 44 cases. Neurosurgery 1989; 25:514-522. 7. Chou CW, Hsu SP, Lin SC, et al. Primary intradural hemangiopericytoma with intramedullary invasion. J Chin Med Assoc. 2009 Oct; 72(10):536-41. 8. Probst-Cousin S, Bergmann M, Schroder R, et al. Ki-67 and biological behavior in meningeal haemangiopericytomas. Histopathology 2006; 29:57-61. 9. Vuorinen V, Sallinen P, Haapasalo H, et al. Outcome of 31 intracranial hemangiopericytomas: poor predictive value of cell proliferation indices. Acta Neurochir. 1996; 138:1399-1408.