Polyuria
advertisement

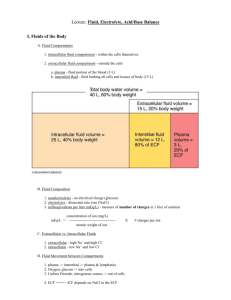
POLYURIA 1 Dr M du Plessis Dept of Chemical Pathology February 2002 1. DEFINITION OF POLYURIA: Polyuria is defined as a urinary volume >3 l/day or >4 m/lmin. 2. ANTIDIURETIC HORMONE (ADH): Arginine vasopressin. Synthesized and secreted: supraoptic and paraventricular nuclei hypothalamus Stored in posterior pituitary lobe. 2.1 REGULATION OF SECRETION OF ADH: 1. Tonicity (Osmolality): Osmoreceptors (anterior HT) (changes of 1-2%) Direct relationship: osmol ADH osmol ADH Osmotic threshold for ADH release > 280 mosmol/kg 2. Circulating blood volume: Baroreceptors (responds to changes in IVV > 10%) Inverse log-linear relationship: IVV ADH IVV ADH Baroreceptors can override osmoreceptors in severe hypovolemia (maintenance of IVV at expense of osmol ( IVV precedence over osmol). 2 3. Other non-osmotic stimuli for ADH release: Pain, stress, sleep, exercise Chemical stimuli: catecholamines, angiotensin II, opiates, PG’s, anesthetics, nicotine, barbiturates. 4. Other non-osmotic inhibitors of ADH release: ANP (negative feedback during IVV, osmol) Alcohol, phenytion, glucocorticoids. 5. Thirst centre: Regulated by the same factors as ADH. Higher osmotic threshold of 290 mosmol/kg. Responses involving ADH, thirst and the kidney are coordinated to maintain plasma osmol within a narrow range (284-295 mosmol/kg). 3 2.2 PHYSIOLOGICAL ACTIONS: 1. Regulation of water reabsorption by kidney and concentration of urine: Normal urine concentration dependent on: o ADH action ( AQP 2 channels in collecting tubules) o Countercurrent mechanism responsible for maintenance of concentration gradient. 2. Vasopressin: vasoconstriction and BP 3. Augments action of CRH in stimulating ACTH-release 4 3. DIFFERENTIAL DIAGNOSIS OF POLYURIA: 3.1 Water diuresis: 3.1.1 Water diuresis with intact ADH: Overhydration with isotonic fluid (postoperatively/ resuscitation) physiologically appropriate free water diuresis. 3.1.2 Water diuresis without intact ADH: Decreased ADH secretion/action = Diabetes insipidus 3.1.3 Psychogenic /primary polydipsia: Chronic, excessive intake of water suppressing ADH secretion and leading to washout of medullary solutes. 3.2 Osmotic diuresis: Increased amounts of osmotically active material causing diuresis: 3.2.1.Hyperglycemia (DM) 3.2.2 Myoglobinuria 3.2.3 Administration of mannitol or IV contrast 3.2.4 Renal tubular injury (CRF, postobstructive nephropathy, post-ATN) ( urea) 5 4. DEFINITION OF DIABETES INSIPIDUS: Absence of an ADH effect causes: Failure to produce a maximally concentrated urine Polyuria and polydipsia Hypernatremia and hyperosmolality will develop when fluid intake does not match losses ( mental alertness - ability to sense thirst or obtain access to fluids). 5. ETIOLOGY OF DIABETES INSIPIDUS: 5.1 Hypothalamic diabetes insipidus (HDI): (neurogenic, central, cranial DI) Decreased ADH secretion. Destruction of 80% of ADH-secreting neurons required for HDI. Causes: i. Acquired: Hypothalamic disease: neoplastic diseases, trauma, surgery, ischemia, infections, granulomatous diseases. ii. Hereditary: autosomal dominant trait. iii. Idiopathic: 30% Importance in anaesthetic setting: i. Emergencies in patients with established DI ii. DI following neurosurgical procedures iii. DI in the posttrauma setting 5.2 Nephrogenic diabetes insipidus (NDI) : Defective ADH action in the kidney (due to a defect in the ADH receptor or AQP2 water channel). Causes: i. Hereditary: X-chromosome linked trait ii. Acquired: Metabolic disorders: Hypokalemia, hypercalcemia, amyloidosis Drugs: Lithium, demeclocycline, barbiturates Renal diseases: Polycystic diseases, CRF. iii. Idiopathic. 6 6. LABORATORY EVALUATION OF POLYURIA: 6.1 Determination of Serum and urine osmol and UKE. U-Osmol: o Osmotic diuresis: U-osmol similar to serum ( 50 mosm/kg) o Water diuresis (+/- intact ADH): U-osmol < 200 mosm/kg S-Na and S-Osmol: o Water diuresis with intact ADH: S-Na and S-Osmol normal/ o Water diuresis with defective ADH: S-Na and S-Osmol normal/ 6.2 Exclude osmotic diuresis: P-Glucose S-Urea S/U-Myoglobin 6.3 Water deprivation test: 6.3.1 Indications: o If DI is suspected in a patient with normal S-Na and Osmol (to exclude water diuresis due to fluid overload/PP) o Hypernatremia ( 145 mmol/l) and hyperosmolality ( 295 mosm/kg) in the presence of polyuria confirms the diagnosis of DI, and obviates the need for performing a water deprivation test. 6.3.2 Criteria for interpretation: o Normal ADH with fluid overload/PP: N S-Na and S-Osmol (< 295 mosm/kg) Concentrated U-Osmol (> 400 mosm/kg) (often > 850 mosm/kg) Ratio of U/S-Osmol > 1.5 o DI: S-Na (>145 mmol/l) and S-Osmol (> 295 mosm/kg) U-Osmol 400 mosm/kg (often < 200) Ratio U/S Osmol < 1.5 (often < 1) Response to DDAVP: HDI: Increase in U-Osmol 10% (often > 50%) NDI: Increase in U-Osmol < 10% 7 7. TREATMENT OF DI: 7.1 Fluids: Hypernatremia and hyperosmolality develop if inability to maintain oral fluid intake. Preferred fluid for IV use: dextrose in water (hypotonic) Inappropriate fluid: Normal saline added renal solute load osmotic diuresis and dehydration. 7.2 DDAVP: (1-desamino 8-D-arginine vasopressin) Analogue with duration of action (6-24 h) pressor and uterotonic effects antidiuretic properties. Administration: parenteral (IV/IM/SC): 1-2 ug intranasally: 10-20 x parenteral dose (metered dose spray of 10ug). 7.3 ARGININE VASOPRESSIN: Significant pressor and uterotonic activity, in addition to antidiuretic effects. Administration: Continuous infusion: short duration of action allows safe management of rapid fluctuations in osmol. Dosage: 1-2 mU/kg/hour CARE MUST BE TAKEN NOT TO CONTINUE EXCESS HYPOTONIC FLUID WHILE PRODUCING ANTIDIURESIS WITH DDAVP HYPONATREMIA: Measure hourly urine output and osmolality. Allow some return of hypotonic polyuria before readministering DDAVP. Be aware of syndrome of triphasic diabetes insipidus. 8 8. TRIPHASIC DIABETES INSIPIDUS: (Following neurosurgical procedures or head trauma) 8.1 FIRST PHASE: Diabetes insipidus: Hours to days after injury Impaired ADH release due to axonal shock (not neuron death) 8.2 SECOND PHASE: Inappropriate antidiuresis: 2-14 days post-injury Uncontrolled vasopressin release due to leakage out of damaged neurons HYPONATREMIA if high fluid intake continues 8.3 THIRD PHASE: Diabetes insipidus: After 14 days ADH deficiency recurs as neuronal granules are depleted Temporary or prolonged Depending on proximity of lesion to neuronal cell body. 9 CONCLUSION: The abrupt onset of hypertonic polyuria and hypernatremia, in the post-neurosurgery or posttrauma setting, may reflect new onset DI. Established DI becomes an emergency and leads to severe hyperosmolality and dehydration when there is impairment in mental status (eg due to anaesthesia) that precludes compliance with a previous medical regimen and impairs the ability to sense and act on thirst. Postoperative patients, especially after neurosurgery or head trauma, are at particular risk of complicated DI. Correct and prompt diagnosis and appropriate treatment are of equal importance in prevention of complications. 10 LABORATORY EVALUATION OF POLYURIA: POLYURIA U-Osmol U-Osmol ~ S-Osmol ( 50) (ratio ~ 1) U-Osmol < 200 S-Na S-Osmol Water diuresis due to fluid overload Normal after fluid deprivation S-Na (> 145) S-Osmol (>295) U/S-Osmol < 1.0 N S-Na S-Osmol Fluid deprivation N S-Osmol + Na U-Osmol > 400 U/S-Osmol > 1.5 Normal Fluid Overload S-Osmol + Na U-Osmol 400 U/S-Osmol < 1.0 Dx of DI P-Glucose DM S-Urea Renal disease Mioglobin Mioglobinuria DDAVP Response: HDI No response: NDI