Beware the tropical flood
advertisement
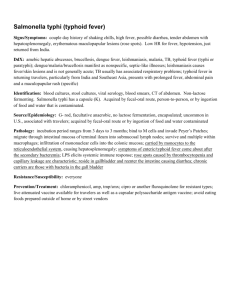
“Beware the Tropical Floods” By Dr Penny Warring Introduction This year is showing itself as a year of extremes. While the worst bush fires in a century rage in Victoria torrential rains and floods deluge Western Fiji. Flooding leads to contaminated water supplies vastly increasing the risk of diarrhoeal illnesses such as typhoid fever and leptospirosis. As a direct result of flooding an outbreak of leptospirosis in Nadi, Fiji has infected nine people, killing two of them. The most recent large outbreak of this disease was in 2000, when 23 Fijians died. Leptospirosis is carried by both domestic and wild animals and the causative organism, a spirochaete, is excreted in urine. Humans can become infected through wading or swimming in contaminated, untreated open water or through contact with urine contaminated soil. Infection may be asymptomatic, or cause only mild symptoms, such as fever, chills, myalgia, nausea, diarrhoea, cough or conjunctival injection. Conversely lepstospirosis can progress to become life threatening with the development of Weil's syndrome. This may involve jaundice, renal failure, neurologic disorders, hemorrhage, and progress to respiratory failure and circulatory collapse. (Coast-to-Coast winner and multisport athlete Steve Gurney suffered from this complication). Once the diagnosis is established treatment can be commenced with antibiotics. The problem is obviously identifying those people who have this, or another potentially serious disease as opposed to another flu-like illness. So what do you do for your patients with a spot of tummy trouble or flu-like symptoms after a recent South Pacific holiday? And what if one such patient presented to you now? Consider a 44 year old man with fever, myalgia and abdominal pain two weeks after a holiday in a 4 star Fijian resort? Maybe having thought about the contaminated water supply in Fiji you consider typhoid at the top of your diagnostic list. You then look in your DML laboratory handbook to see how best to test for typhoid. You find the following:- Salmonella antibodies (Widal Test) specimen: serum A test of limited value in the diagnosis of typhoid fever, blood culture being the preferred diagnostic method. Interpretation O antigens H antigen Vi antigen titre >1:160 and rising sharply over 7-14 days suggests current infection. >1:160 suggests immunity high titre sometimes indicates the carrier state. Titres can be non-specifically elevated in diseases not caused by Salmonella and vaccination can give positive titres. As this test seems unlikely to be helpful, and your patient is complaining of increasing abdominal pain, you decide to pick up the phone and talk to the infectious diseases registrar. Perhaps he should be admitted and blood cultures performed in the hospital setting? You are well prepared to answer the registrar’s questions and brief her appropriately, “I have a 44 year old otherwise well male who returned two weeks ago from a 5 day resort holiday in the Fiji islands. He has a three day history of fever, feels lethargic and fluey, and has abdominal pain. I am concerned about typhoid fever due to the sanitation and flooding issues in Fiji at the moment. I don’t suspect leptospirosis because he only swam in the resort pool” The infectious diseases registrar cleverly asks, “Any diarrhoea?” “No,” you reply, “but it can take three weeks before diarrhoea starts” “Did he wash his hands before eating and boil all water or drink and brush with bottled water only?” she might ask. You quickly ask this of your patient, and pass on that he did take excellent precautions; and he never left the resort. “Then a diagnosis of typhoid fever is unlikely, isn’t it Doctor”, she replies. At this point your patient groans and slumps in his chair. You quickly explain that you have to go, and will get back to the registrar shortly. You get off the phone, only to find he is extremely drowsy with a blood pressure of 80/50mmHg, a tachycardia of 126 beats/minute and cold clammy skin. Your receptionist calls for an ambulance and in the meantime you lie him down with his legs elevated on a pillow. At this point, for the first time you notice a subtle petechial rash on his shins. The ambulance arrives and you provide the officers with a brief history. They put on an oxygen mask delivering 6L/min and hook up a bag of saline to the large bore intravenous line you have put in and deliver him straight to the hospital ED. What is your working diagnosis? You might draw up a list. Typhoid fever with shock Other infectious gastroenteritis with shock Meningococcal meningitis Influenza Other severe viral illness Measles Rubella Malaria Acute vasculitis of some sort You call the patient at his house several times over the next week, but get no reply. You eventually call the hospital and find that he is admitted to the infectious diseases ward. Finally you speak with the registrar only to find out that your patient does not have typhoid fever but dengue hemorrhagic fever. He has only just been stepped down from intensive care. Dengue fever (also called break-bone fever) is a viral illness caused by any one of four closely related viral serotypes (DEN1, DEN2, DEN3, DEN 4) from the flavivirus family. Infection with one dengue virus serotype provides lifelong immunity to that serotype. Dengue is spread by the bites of infected Aedes mosquitoes (most often Aedes aegypti). The incubation period is 3 to14 days. Photo courtesy of www.scienceblogs.de Dengue is a very important emerging disease in Southeast Asia, the American tropics and the South Pacific. There has been a 30-fold increase in incidence over the past 50 years worldwide, and more than 100 countries world wide have reported dengue fever. Several factors have contributed to the rapid rise in the incidence of dengue fever. As well as increasing tourism and migration, climate change and increasingly wet conditions have created a favourable environment for mosquitoes to thrive and there have been economic shifts resulting in inadequate mosquito eradication plans. Notably influencing the spread of the disease is the fact that dengue is usually contracted in towns and cities, unlike malaria which is prevalent in rural areas. Experts anticipate that dengue will continue to spread so we can expect that more cases of this illness will be seen in New Zealand’s Accident and Medical Clinics in the coming years. Symptoms Abrupt onset of high fever Severe frontal headache Nausea and vomiting Retro-orbital pain Arthralgia Myalgia Maculopapular rash. Dengue is typically a mild and well tolerated illness that produces minimal or no symptoms, particularly in older children and adults. The above acute symptoms generally last a week, but weakness, loss of appetite and fatigue can carry on for several weeks after the initial acute illness has subsided. Dengue Hemorrhagic fever (DHF) The severe form of dengue, dengue hemorrhagic fever (DHF) is paradoxically more common in those who have had dengue fever before, and is fatal in 10% of people if allowed to progress to shock. The typical presentation is increasing lethargy or restlessness, three to five days following the onset and generally when the fever starts to subside. There may be signs of circulatory collapse and the development of a petechial rash. Bleeding gums, haematuria, epistaxis, haematemesis, and melaena are less common manifestations of the thrombocytopenia that develops. Imminent signs of shock are hypotension, tachycardia, intractable abdominal pain, vomiting, hypothermia, mental confusion or irritability. It is the loss of volume from the intravascular compartment due to leaky capillaries that causes the hypovolaemic shock, and not a consequence of the haemorrhage. Treatment Frequent oral hydration is the mainstay of treatment for outpatients and must be clearly stressed to the patient. If the patient is unable to maintain a good oral intake, and does not have a reliable support person who can assist with oral rehydration, then consider admitting for observation, monitoring and intravenous fluids. Schedule daily reviews for outpatients with dengue to monitor the following parameters: temperature, blood pressure, pulse (looking for signs of circulatory collapse), levels of hydration, mental state, signs of hemorrhage and platelet count. If there are any signs of early circulatory collapse, declining mental function, hemorrhage, admit for intravenous rehydration and possible inotropic support. The best medication to control pain and reduce fever is regular acetaminophen. The use of aspirin or antiinflammatories is contra-indicated due to the risk of aggravating the bleeding tendency and the risk of Reye’s Syndrome in children. Laboratory Diagnosis Diagnosis is made by measuring IgM and IgG antibodies preferably in paired sera. As there are 4 subtypes of Dengue, the presence of both antibodies may indicate an earlier infection. It is the ratio of IgM to IgG, or rising titres in paired sera that determines whether infection is current. Vaccination No vaccine is currently available to prevent dengue fever or dengue haemorrhagic fever. Advice to give your patients travelling to the Islands this year :- For patients considering an island holiday in Fiji for example it is best to advise them to avoid contact with standing water (like flood waters, rivers or farming paddies). If avoidance is impossible, advise them to wear thigh-high waterproof boots. Doxycycline at 100mg per day is a suitable to use for chemoprophylaxis. Boil all water or use bottled water for drinking and teeth brushing. Consider vaccination against Salmonelli Typhi. Wear long sleeve tops, long sleeve pants when outdoors, at dusk and dawn when mosquitoes are most likely to bite. Stay in accommodation with mosquito screens/ bed netting. Use a good insect repellent containing DEET, picaridin (KBR 3023), Oil of Lemon Eucalyptus/PMD, or IR3535. Note: repellents with less than 10% of an active ingredient may offer only limited protection, often no longer than 1-2 hours. Wear repellent under sun screen. Ode to South Pacific Paradise Lost (with apologies to surviving relatives of John Milton) For all the Typhoid, Dengue, and Leptospirosis To leave this Paradise, but shalt possess A paradise within me, happier far.