phar3812 – lecture outline – allergic rhinitis
advertisement

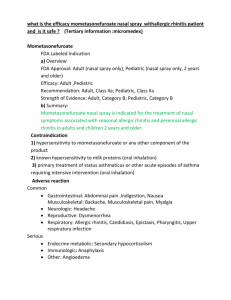
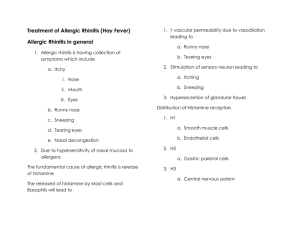
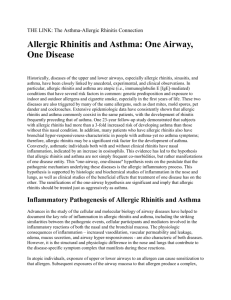
PHAR3812 – LECTURE OUTLINE – ALLERGIC RHINITIS DR LORRAINE SMITH lorraine.smith@sydney.edu.au So far: Histamines and antihistamines Respiratory herbs Case study – Mrs Kearns Clinical interventions Asthma therapy and devices Case 1: Mrs Kearns – Allergy and Asthma: Learning Outcomes Have an understanding of the link between Asthma and Allergic Rhinitis Identify the different structure of antihistamines Understand the structural features likely to cause adverse effects with antihistamines Demonstrate an ability to develop appropriate allergic rhinitis and asthma management plans. Mrs Kearns: Mrs Kearns, a healthy 78 year old female is visiting Sydney to attend her grandson’s wedding. Active for her age, she is very relieved that she was able to make the trip as a bout of tonsillitis almost forced her to cancel. She is 5 days in to a 14-day course of erythromycin therapy. Yesterday she had an upset stomach and diarrhoea, (taking Lomotil for this). The Lomotil has left her feeling a little tired and she also as a dry mouth and slightly blurred vision. Last night she woke in the night coughing and this morning she has woken up with red itchy, watery eyes and is sneezing frequently. She tells you that when she lived in Sydney before she retired, she used to suffer from hayfever and her doctor had treated her with Teldane. The antihistamines you have available are Claratyne (loratadine), Phenergan (promethazine), Telfast (fexofenadine) and Polaramine (dexchlorpheniramine). She also presents her asthma card and asks for a Ventolin inhaler. Your pre-work and tutorial activities: Possible causes of her cough Link between asthma and allergic rhinitis Structures of antihistamines, side effects, pros and cons of each Metabolism of erythromycin and interaction with Lomotil Devise an allergy and asthma action plan Counsel on correct use of antihistamines Counsel her on her management of AR (both if she stays in Sydney and goes home) Today – the CLINICAL PICTURE Causes Symptoms Triggers Classification Treatment options Learning outcomes: State the known causes of allergic rhinitis Name the common symptoms and triggers of allergic rhinitis Describe the classification system of allergic rhinitis Describe and give examples of strategies for helping patients control symptoms and triggers Resources: Case 1: Mrs Kearns NAC Guide for Health Professionals: Allergic rhinitis and the patient with asthma Lecture notes Tutorial workshop notes References at the end of these lecture notes What is allergic rhinitis? An inflammatory disorder of the nasal mucosa, mediated by specific IgE antibodies in response to allergen exposure (Bousquet, J., van Cauwenberge, Khaltaev & the WHO Panel, 2001). What is an allergy? Some common allergens: Dust mites Pollen / Grasses Animal dander Mould Epidemiology: Australia has a high incidence of AR Prevalence increasing Co-morbidities – related conditions: Asthma Eczema, Ottis media (middle-ear infection), Sinusitis, Conjunctivitis, Nasal polyps Classification of allergic rhinitis: OLD: Traditional classification Seasonal Perennial Based on when one is exposed to triggers Seasonal Spring/Autumn Perennial All year round NEW: Allergic Rhinitis and Its Impact on Asthma (ARIA) Classification Based around the symptoms Duration Severity (impact on quality of life) Allergic Rhinitis DURATION Intermittent Persistent < 4 days/week or < 4 weeks > 4 days/week and > 4 weeks SEVERITY Mild All of the following: Moderate-severe One or more items: •Normal sleep •No impairment of daily •Abnormal sleep •Impairment of daily activities, sport, leisure activities, sport, leisure •No impairment of work and •Impaired work and school school •No troublesome symptoms •Troublesome symptoms Mild All of the following: Moderate-severe One or more items: •Normal sleep •No impairment of daily •Abnormal sleep •Impairment of daily activities, sport, leisure activities, sport, leisure school school •No impairment of work and •Impaired work and •No troublesome symptoms •Troublesome symptoms Allergic Rhinitis symptoms: 1 2 3 4 5 6 7 8 What the AR person looks like: Swollen nose Nasal quality to the voice from continuous mouth breathing Is is a cold or an allergy? COLD ALLERGY Usually lasts up to a week Sometimes mild fever Usually no fever Nasal discharge is thick and cloudy, perhaps coloured Nasal discharge is thin, clear & watery Infrequent sneezing Nasal congestion Nasal or sinus congestion Unlikely watery eyes Sore throat Itchy, rather than sore throat Unlikely itchy eyes, nose, or throat Itchy eyes, nose, throat Sydney sufferers – symptom proportions: Nasal = Eye = Throat = Physical = Do symptoms vary according to season? Yes? No”? A little? Triggers of allergens – proportions Sydney sufferers: Classical = Weather = Chemical = Other = Do triggers vary according to season? Yes? No”? A little? - eg: Quality of life can be ++++ affected by allergic rhinitis: Typical effects include - What are the treatment options: Allergen control Medication Immunotherapy But there is a problem ….. Commonly used treatments: Antihistamine = INC = Saline or nasal sprays = Oral decongestant = Other = Pharmacy practice – care of the patient….. what can you DO? Just dispense a medication and give dose information? NO!! Ask the patient: What are their specific What are their specific Collaboratively, work out some strategies to control symptoms and triggers Strategies must be Strategies to help your patients control their hayfever: Strategy Explanation Example Useful? Adherence – Non-specific strategy for . non specific reinforcing the taking of medication. Adherence – Strategies including dose [xxxxx] nasal spray – 1 Specific amounts and daily puff in each nostril instructions. More twice a day. guidance given for Take one tablet of patient adherence. [xxxx] a day until a few days after feeling better. Avoidance Non-specific strategy with reference to the trigger. Practical Action Specific strategies with additional instructions on how, when or why to achieve the goal. Other Strategies unable to be classified above and more applicable to general health. Close the windows when the neighbor is mowing. Shower and wash hair every night to remove pollens. Wash hands after patting the cat. Wear sunglasses to prevent pollen getting into eyes. Personally relevant strategies for controlling AR make the difference for patient control: • For symptoms: • For triggers: There is a greater scope in optimizing strategies for managing AR triggers through practical advice than for symptoms. Encouraging adherence to meds will not help to control triggers. Why is this important? Remember, only 35% of patients are adherent to allergic rhinitis medications Effective control of allergic rhinitis requires patient self-management strategies Pharmacists are the key point of contact for management of allergic rhinitis Summary: Allergic rhinitis affects approx. 20% of Australian population Most patients do not seek professional help with the management of the condition Most patients are not adherent to meds Pharmacists intervention is best when: individual patient symptoms and triggers are identified practical strategies for controlling triggers are devised dose info and tips on remembering to meds for controlling symptoms are devised This is done COLLABORATIVELY WITH THE PATIENT Acknowledgements: Dr Celina Seeto, Schering Plough Tony Nguyen, Registered Pharmacist Lin Brown, Project Manager, Pharmacy Allergic Rhinitis Project References: Bousquet, J., van Cauwenberge, P., Khaltaev, N., & the WHO Panel. (2001). Allergic rhinitis and its impact on asthma. ARIA, in collaboration with the World Health Organisation. Journal of Allergy and Clinical Immunology, 108, S1-S315.