Emergency Evacuation Plan

Logo
Facility Name
Emergency Evacuation
Plan
Version Number:
Date Issued:
Authorized by:
Page 1 of 34
Table of Contents
Introduction
Background
Decision to Evacuate
Purpose
Scope
Review of Procedures
Residential Aged Care Network
Glossary of terms
Staff Roles and Responsibilities
Evacuation Coordinator
2 nd In Charge
Other Staff
Co-ordinator of Receiving Facility
Sending facility emergency evacuation procedures
Resources
Emergency equipment System Checklist
Evacuation kit
Education & staff Training
First Aid Kit
Resident Identification Protocol
Emergency Documentation
Resident Emergency Admission to Acute Care Setting
Resident Short Term Emergency Accommodation Listing
Emergency Reception of Evacuation Documentation
Resident Care Plan
Body Chart
Evacuation Progress Notes
General Guidelines for Receiving Facility
Appendix 1 Hazard Management Agencies Contact List
Appendix 2 Function Support Agencies Contact List
Appendix 2 Key Staff Contact Numbers
Appendix 3 Aged Care Network Contact List
Appendix 4 Evacuation Co-ordinator / DON Checklist
Appendix 5 WA Emergency Management Arrangements
Appendix 6 Emergency Management Plan Structure
Appendix 7 Transport Plan
Appendix 8 Communication Management Plan
Appendix 9 Emergency Electrical Supply for Facility
Appendix 10 Residential Aged Care Facility Resources
16
17
18
19
20
11
11
11
12
13-15
16
3
3
3
3
3
4
4
5
6-10
26
27
28
29
30
32
33
21
22
22
23
24
Page 2 of 34
Introduction
Background
These procedures have been developed in consultation with the Senior
Management Team and specific committee members for Emergency
Management Planning.
Evacuation is something that should not be undertaken lightly and there are situations where it will be preferable to shelter in place rather then evacuate. Evacuation of aged care residents requires special consideration due to their medical condition and physical restrictions. Facilities that are best able to receive these evacuees are other aged care institutions within the local area.
This plan outlines a procedure for the planned transition of our residents requiring evacuation from our facility to another receiving aged care facility.
Decision to Evacuate
For the purpose of this plan the decision to evacuate offsite for any local emergency, will be made by the Hazard Management Agency
(HMA).
Further information on Emergency Management can be found on the
FESA website at www.fesa.wa.gov.au
Purpose
These procedures are designed to ensure the safe and effective transition of our residents between aged care facilities and acute hospitals in the event of an emergency situation. The procedures also ensure all required information is available for ongoing care and requires the evacuating facility to be prepared to respond to the emergency situation. The procedures will assist the receiving facility to be prepared to cope with the sudden increase in residents.
Scope
In preparing these procedures it is assumed that the residents will:
Only be cared for in the short term (up to a maximum of 24
Page 3 of 34
hours)
Arrive unescorted
Have limited documentation or history available to the receiving facility
Will have no personal property except items worn at the time of the emergency
Managers / Owners of the facilities included in the plan will have entered into an agreement, (MOU) that addresses the financial and liability issues placed on the receiving facility and the capacity to assist for a period of up to 24 hours.
Review of Procedures
These procedures will be tested and reviewed internally on an annual basis and with other members of the Residential Aged Care Network two yearly or following an evacuation event, whichever occurs earlier.
Aged Care Network
The Residential Aged Care organizations that are party to the
Memorandum of Understanding and have adopted these procedures are:
Organisation Aged Care Facilities
Other Services
Local Emergency Management Committee
Hazard Management Agencies (see Appendix )
Disaster and Emergency Support Services
Fire & Emergency Services WA
St John’s Ambulance Services
West Australian Police Services
Department of Health
Page 4 of 34
LEMC
LG
MOU
PPRR
SECG
SEMC
SES
SREMP
WESTPLAN
Glossary of Terms
AWARE All West Australians Reducing Emergencies
ACEERP
CBR
Aged Care Emergency Evacuation & Reception
Procedures
Chemical, Biological and Radiological
DEMC
DEMTT
DON
EM
EMA
ERM
HAZMAT
HMA
ICS
District Emergency Management committee
District Emergency Management Training Team
Director of Nursing
Emergency Management
Emergency Management Australia
Emergency Risk Management
Hazardous Materials
Hazard Management Agency
Australian Inter-Service Incident Management
System’s Incident Control System
Local Emergency Management Committee
Local Government
Memorandum of Understanding
Prevention, Preparedness, Response and Recovery
State Emergency Coordination Group
State Emergency Management Committee
FESA State Emergency Service
State Recovery Emergency Management Plan
Western Australian Emergency Management Plan
Page 5 of 34
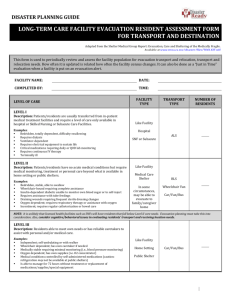
PROCEDURES AND GUIDELINES FOR EVACUATING RESIDENTS TO ANOTHER
AGED CARE FACILITY SHORT TERM – UP TO a maximum 24 HOURS
Staff Roles and Responsibilities
Evacuation Co-coordinator / Chief Warden
(Sending Facility)
To alert emergency services to the emergency, request their assistance & provide them with information re the emergency and the planned response (See attached list of Hazard
Management Authority).
To alert the Director of Nursing/Manager of the facility of the emergency & actions being taken
To oversee the internal evacuation process until emergency services personnel arrive
Liaise with Emergency Services when they arrive on site.
Follow instructions from the emergency service of choice e.g.
F.E.S.A.
Contact facilities that are party to the MOU to see if beds available and warn them of an impending arrival of temporary resident(s). See attached list for participating Aged Care
Facilities
Allocate residents to appropriate alternative facility.
Provide resident information pertinent to evacuation safety and transfer of residents. E.g: o Number of Residents involved o Resident Health status and mobility o Interim accommodation available
Refer to Evacuation Coordinator Checklist
2 nd in Charge
Allocate staff roles to assist with o Evacuating residents o Care of residents o Control of resident movements
Ensure all residents have an identification card attached
To ensure that all residents have at least one form of identification on their person that cannot be easily removed by
Page 6 of 34
Page 7 of 34 the resident. It is suggested that Photo ID is worn on the residents chest area, unless demented then worn on back of body, also wrist tags could be used.
Treat any minor injuries / first aid and medical needs. Some first aid equipment available in emergency case.
Arrange for identified residents (red card) to be transferred directly to an acute hospital, arrange ambulance transport in consultation with emergency services.
Transport is available through a number of sources – see transport section plus list of facilities party to the MOU for available transport.
Supervise the preparation of all medications, medication charts, continent products and transfer letters and/or care plans for ready transfer.
Ensure that suitable numbers of staff members are sent with residents’ to receiving facilities for initial handover, confirmation of resident identification and immediate health needs.
Ensure all staff sent to receiving facilities has suitable identification on them (keep spare identification cards in
Emergency box). Staff to leave receiving facility once the facility is satisfied with information provided
Where possible the following should be sent with the resident: o Transfer letter or care plan kept in a fire proof box in a o designated area
Medication charts / medications. If unavailable from care centre, contact pharmacy to obtain a copy of medication profiles and medications.
O
Medications o Continence products
To Contact representatives/families & to ensure that they are aware of the situation & where their loved one has been sent for care updated list of N.O.K contact details also kept in fire proof box.
Contact the receiving facility and ensure all residents are suitably housed.
Remove own staff from receiving facility once receiving facility is satisfied with information provided
Other Nursing & Care Staff (Sending Facility)
Ensure that internal evacuation processes are followed
Ensure that all residents are suitably attired ready for transfer to another facility
Ensure that the DON is aware of any immediate medical needs of each resident
Ensure all residents have an identification card attached.
To separate remaining residents into suitable groups ready for transfer to receiving facilities.
Continue with the evacuation process until told otherwise by
Evacuation Coordinator/Emergency Services Personnel
Go with residents to receiving facility as requested by the DON
& provide information & assistance to receiving facility until identification is confirmed for all residents & told to leave by the DON
Ensure no one enters a previously evacuated area unless authorized by Emergency services personnel.
All staff to follow duties and requests designated to them by the Evacuation Co-coordinator.
To alert the contracted pharmacy of the emergency & request medications & resident profiles to be forwarded to the receiving facilities as soon as possible
To contact all GP’s & alert them to the situation & where their patient’s are temporarily accommodated. This can be done during the next day if the emergency occurs late at night.
Page 8 of 34
Sending Facility Emergency Evacuation Procedures (Up to a maximum of 24 hours)
Evacuation Co-ordinator Role & Responsibilities
Emergency
Services
Contact the Fire
Communications
Centre (000) & alert to the emergency.
Staff & Clients
Allocate staff roles to
evacuate residents
Care for residents
Control residents movements
Receiving Facility
Contact all receiving facilities & alert tol arrivals needed.
Organisational
Management &
Support Services
Contact Site
Manager & alert them to emergency.
Family and
Representatives
Answer queries as per protocol.
Liaise with
Emergency Services when they arrive on site.
Provide resident information pertinent to evacuation safety & transfer of residents.
Ensue all residents have Identification
Cards attached.
Allocate residents to appropriate alternative facilities.
Locate & prepare all medications, med charts & transfer letters or care plans for transfer.
Arrange staff to assist at temporary holding facilities for set periods.
Ensure ‘staff’, ‘acute staff’ & ‘short term’ lists are completed.
Provide additional information to receiving facilities as requested.
Alert all receiving facilities once ‘all clear’ has been given.
Arrange transport & staff assistance to return once ‘all clear’ has been given.
Arrange payment to the receiving facility for assistance as per agreement.
Contact:
Pharmacy
GP’s
Recontact within 24 hours re health status
& movement of residents.
Page 9 of 34
CO-ORDINATOR OF RECEIVING FACILITY
1.
Notify Manager and Chief Executive Officer of the facility, security if after hours.
2.
Notified Hospitality Manager.
3.
Identify and prepare an area to receive evacuees.
4.
Allocate extra staff to the area as required.
5.
Assemble equipment ready for evacuees
Beds / chairs
Continence Products
Equipment for assessment
Oxygen
Medical supplies for skin tears
Linen skip identified for these evacuees
Additional Blankets / Linen
Manager of Facility
1. Resource additional staff
2.
Attend as soon as possible to assist with co-ordination
3.
Communicate with outside resources and families
4.
Media communication as per organization policy, e.g. CEO.
Food Service Staff
1.
Prepare additional thickened fluids
2.
Prepare soup or warm drinks
3.
Supply Cups
Housekeeping Staff
1.
A variety of clean clothing available for both female and males use in various sizes.
2. Clean clothing stored in the laundry.
Page 10 of 34
Resources
Emergency Equipment System Checklist
Evacuation Co-ordinator (sending facility)
Backpack contents:
Current resident handover sheets
Current staff roster
Blank staff identification badges
Maps of the facility
Copies of the resident identification cards
The box with all current resident ID cards
Copies of Evacuation Procedures
Resealable plastic bags for medications, medication charts & care plans/transfer letters (1 per resident)
Evacuation Resource Box
A mobile evacuation resource box is to be assembled and kept in a location that is both readily accessible and secure. It should contain enough resources for the number of evacuees that the facility is able to accommodate.
As a minimum it should contain the following:
Identification devices
Paperwork — Original template to be photocopied when required.
Clothing including pyjamas and socks
Plastic bags for notes and valuables
Sticky labels for plastic bags
Clipboard and pens
Education and Staff Training
Training to receive evacuees is be included in all evacuation training sessions Emergency Procedure manuals are to be updated to reflect these requirements.
Page 11 of 34
Emergency Evacuation Plan
First Aid Kit
The following items are to be available in the emergency management case.
Number
6
10
6
6
3
3
3
1
3
1
1
6
5
1
1
10
1 box
Items
Dressing packs
Normal saline for dressings
Mololite dressings
Adaptic dressings
Packets steri strips
100mm crepe bandages
150mm crepe bandages
Surgical scissors
Large combine dressings
Triangle bandage
Wide micropore tape
Primapore dressings
Water for injection
Oxygen mask
Nebuliser mask
Alcohol swipes
Disposable gloves
Ensure box is re-stocked after use.
Page 12 of 34
Resident Identification Protocol
Objective:
Scope:
To ensure that all residents who have been evacuated from the care facility have correct photographic and essential medical / personal identification on their person prior to being transported to a temporary holding facility.
This process is required to include all residents of the evacuating facility.
Responsibility: Reception staff is responsible for maintaining and updating the photographic and essential personal / medical identification cards. This is to be attended
Identification
Update
Process: monthly and at the time of resident admission or discharge.
Check identification cards against a resident list for
Alert Colour
Codes: each unit monthly.
The person who is checking the cards is to sign & date back of resident’s list. Leave list in container with identification cards. At this time all discharged or deceased resident cards are to be removed and destroyed. Update current residents photograph annually or as required.
Where a resident has a health condition requiring extra care identified by the Clinical Nurse Manager the following colour alert is applied by highlighting the back of card:
RED – Residents who may require transfer to acute care o Unstable Insulin dependant diabetic (IDD) o Palliative care
YELLOW – Residents who may wander away/aggressive behaviour
BLUE – Residents who have a swallowing deficit
GREEN – Residents with diagnosis of diabetes
(NIDDM)
PINK – Highlight Resident’s name and location on front side of card if able to go home
.
Page 13 of 34
Technology
Requirements:
Additional
Requirements:
Identification
Cards:
Digital camera
Coloured photo printer
Adobe Photoshop or equivalent software
8Ogsm card or greater
I x plastic box to hold the identification cards & labelled as such
Lanyards for ID cards for every resident within the facility
The identification cards must contain the following information; care centre & phone number, resident name, date of birth, regular GP, GP phone number, next of kin, next of kin phone number, alerts, principle diagnosis and interpreter required.
An example is displayed below
Facility Name
Ph: 9333 44 55
Name : Mrs Joan Smith
DOB : 25/04/1920
GP : Dr Who Phone: 9123 4567
NOK : Allen Smith
NOK Phone: 9345 6789
Alerts :
Principle Diagnosis
Mrs Joan
Smith
Facility
Picture
:
Storage
Location:
Identification cards are to be kept in the labelled plastic box at all times. This box is to be kept within the emergency backpack.
Backup
System:
It is vital that at least one set of either coloured or black & white copies of all identification cards are kept within the Emergency resource box. This will enable identification of residents should they wander away during the emergency evacuation.
Page 14 of 34
Identification
Updates:
Current
Residents:
New
Residents:
Identification
Cards Use:
Staff
Identification:
All identification cards are to have the following information listed on the back.
“CORRECT AT (DATE) & (SIGNATURE)”.
It is recommended that the correct date and signature be checked monthly.
This process is to be completed at least once per year at the emergency policy & procedure reviews, and as individual resident health needs change.
Identification cards are required to be updated as part of the regular admission process of new residents to the home. At this time, all discharged or deceased resident cards are to removed & destroyed & the copies within the Emergency Backpack are to be changed.
Identification cards are only to be used when the HMA has indicated that residents are to be evacuated to another care facility.
Identification cards are to be attached to the residents using the lanyards purchased. Where a resident is known to have high level dementia and will remove the identification card, it is to be attached to the resident’s back on their left scapula.
Where staff are not wearing their own individual identification badge, a name label needs to be made up by using the sticky labels available in the emergency file.
Logo
Name:__________________________
Position:________________________
__
Page 15 of 34
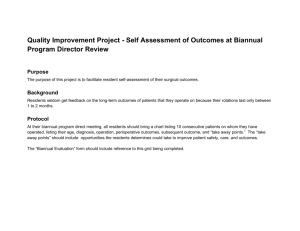
Documentation
Facility Name
RESIDENT EMERGENCY ADMISSION TO ACUTE CARE LISTING
Resident Name Transport
Arranged
√ = Yes
Sent To Representatives or Family Notified
√ = Yes
Facility Name
RESIDENT SHORT TERM EMERGENCY ACCOMMODATION LISTING
Resident Name Transport
Arranged
√ = Yes
Sent To Representatives or Family
Notified √ = Yes
Page 16 of 34
Emergency Reception of Evacuees Documentation
Admission
NAME Date Of Birth
Regular Doctor
Principle Diagnosis
Arrival Date I I
Escort No / Yes details
Written Information No / Yes details
Next of Kin Relationship
Previous Facility
Pharmacy contact details
Assessment
Completed Date /
Name & Designation
Summary
Diet & Fluids
Behaviours
I
Phone
Arrival Time
Contact
Time
Signature
Mobility
Continence
Medical Alerts
Discharge
Date I
Discharged to
I Time
Mode of transport
Copy of Interim notes with resident Yes I No details
Page 17 of 34
Please Note: the Interim care plan should go on the back of this document.
Nursing Assessment
Cardio-Vascular
Pulse Rate Character
Blood Pressure ….. / …… lying / sifting / standing
Build Slight / Average I Muscular / Overweight / Obese
B.S.L
Respiratory
Please explain any abnormality observed (Clubbing of fingers, Cyanosis,
Dissymetry of chest wall) or signs of respiratory distress
Urinary
Continent
Pads
Bladder Yes / No
Day
Catheter
Urinalysis
Yes / No
Communication
Language
Able to verbalise needs
Details
Digestive
Bowel
Night
Yes / No
Orientated to time and place Yes I No
Yes I No
Device in-situ No / Yes
Special Diet critical No / Yes peg / N.G / other
Skin
Using the attached chart fully document any observed abnormality of the skin, including skin tears, bruises, lacerations, scars and rashes.
Page 18 of 34
BODY CHART
Page 19 of 34
Evacuee Progress
Notes
Surname
Forenames
ID Number
Page 20 of 34
General Guidelines for attending to residents for
Receiving Facilities
If there is any doubt about what care needs a resident requires then these guidelines are to be used until an assessment has been conducted.
Diet For smooth diet and thickened fluids until full assessment can be completed.
Mobility
Continence
Skin Care
Documentation
Activities of
Daily Living
Valuables
For assistance with assessment can be completed.
Products to be used until continence assessment can be completed
To be re-positioned 2- hourly until skin integrity assessment can be completed
All staff interactions with evacuees are to be documented, this includes interactions such as offering fluids, re-positioning and urinary output, which are not usually recorded in an Aged Care setting. It is anticipated that an entry will be recorded every hour for every evacuee.
Full assistance is required until otherwise demonstrated
two
staff member until full
In progress notes list and describe all articles that arrive with the new resident including but not limited to Jewellery / Watches / Spectacles / Hearing Aids /
Books / Photographs.
Page 21 of 34
Fire
Appendix 1
HAZARD MANAGEMENT AGENCIES
(HMA List by Hazard)
HAZARD /
EMERGENCY
Storm / tempest
Human Epidemic
Flood
Fuel Shortage
Emergencies
Hazardous Materials
Emergencies (including chemical, biological and radioactive)
Road Transport
Emergencies
Land search & Rescue
Tropical Cyclone
HAZARD MANAGEMENT
AGENCY
Fire & Emergency Service
Authority (FESA)
Fire & Emergency Services
Authority
Health Department WA
Fire & Emergency Services
Authority
DOCEP - Department of
Energy Safety Directorate
Fire & Emergency Services
Authority
WA Police Force
CONTACT PHONE
NUMBER
000
000
1800 022 222
000
9422 5200
000
000 / 131 444
000 / 131 444
000
Earthquake
Space Re-Entry Debris
Landslide
Building Collapse
WA Police Force
Fire & Emergency Services
Authority
Fire & Emergency Services
Authority
WA Police Force
Fire & Emergency Services
Authority
Fire & Emergency Services
Authority
000
000 / 131 444
000
000
Page 22 of 34
Appendix 2
‘FUNCTION’ SUPPORT AGENCIES
The following table lists the agencies responsible for managing the provision of support functions in emergencies are:
Support Function Responsible Agency Contact Phone
Number
Health & Medical
Services
Health Department of WA
1800 022 222
Lifelines – Electrical &
Gas
Public Information
DOCEP - Department of
Energy Safety Directorate
WA Police Service
9422 5200
Recovery
Resources
Premier & Cabinet (Dept)
Respective HMA
Manager – High Care
Manager – Low Care
Building & Facilities Officer
Human Resource Manager
Risk Manager
131 444
9222 9888
000
Telecommunications Fire & Emergency Services
Authority
Welfare Services Department of Community
Development
9222 2555 / 1800
622 258
KEY STAFF – TELEPHONE NUMBERS
These staff are to be contacted immediately incase of emergency.
Name Position Contact Phone
Number
CEO
Page 23 of 34
Aged Care Network Contact List
–
Organisation
Appendix 3
(last updated dd/mm/yy)
Facilities Number Contact
Primary
Contact
Alternate
Contact
Primary
Contact
Alternate
Contact
Primary
Contact
Alternate
Contact
Page 24 of 34
Appendix 4
EVACUATION CO-ORDINATOR CHECKLIST
Alert emergency services of emergency
Alert Director Of Nursing/Manager of the emergency
Oversee situation until emergency services personnel arrive
Contact receiving facilities & alert them to impending arrivals
Complete “Emergency evacuation transfer details” form for each receiving facility
Staff sent to receiving facilities:
Facility Name Contact Number Staff Name and Position
Alert contracted pharmacy
Alert GP’s
Check with receiving facilities for resident suitability
Remove own staff once information is settled
Send residents requiring acute care to closest facilities
& complete “Resident emergency admission to acute
Page 25 of 34
care listing”
Treat minor injuries/immediate medical or first aid needs
Separate residents into suitable groups for transfer & alert representatives & families of transfer
Complete “Resident short term emergency accommodation listing”
Collect Care plans & medications & medication charts if possible for transport with residents or complete transfer letter if possible
Ensure that all residents have at least one form of identification on their person prior to transport (see resident ID protocol below)
Page 26 of 34
Appendix 5
Western Australian Emergency Management Arrangements
FESA Policy Statement No 7.
(this needs to be a hyperlink to http://www.fesa.wa.gov.au/internet/default.aspx?MenuID=296
Click on above box to open document
Page 27 of 34
Page 28 of 34
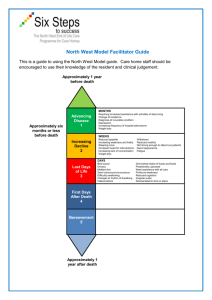
Appendix 6
Example
City of Stirling Emergency Management Plan Structure
This page is to put into context where the Residential Aged Care
Emergency Plan sits in the overall Emergency Management Process.
Level I
The Western Australian Government has a
• State Emergency Plan
• State Recovery Plan and
• A State Welfare Plan
Level 2
The City of Stirling Local Emergency Management Committee has developed the:
• City of Stirling Local Emergency Management Plan Components of the
City of Stirling Local Emergency Plan are the:
• City of Stirling Recovery Plan
• City of Stirling Welfare Sub Plan
This Plan, the Residential Aged Care Emergency Management Plan will form part of the City of Stirling Welfare Plan
Page 29 of 34
Appendix 7
Transport Plan
The following resources are accessible in an emergency situation:
Aged Care Facilities:
Alfa Facility – wheel chair bus e.g. 3 wheelchairs & 6 persons able to sit or 9 residents.
Emergency Contact: Manager of High Care – Phone Number
Beta Facility – wheel chair bus e.g. 2 wheelchairs & 10 persons able to sit or 12 residents.
Emergency Contact: Manager of Low Care – Phone Number
Local Councils:
St John’s Ambulance:
Whilst St John’s Ambulance has around 48 vehicles on the road at any one time there are additional 30 – 40 vehicles that would be suitable for use in emergencies.
These vehicles would need to be called into emergency situation by the
Hazard Management Agency (HMA) who is in control of the incident. It is possible for non St John’s Ambulance personnel to drive ambulances provided there is on St John’s staff member on board.
Easy Access – Perth (Multi Purpose Taxi):
They would send a message to all vehicle owners seeking there assistance.
There is approximately 140 vehicles available
.
Emergency Contact: 9422 2240 – 24 hours x 7 days per week.
Page 30 of 34
Appendix 8
Communication Management
Telephones:
During an emergency if the normal telephone system is not working, back up telephones are available in the following locations.
House 1 Blue Phone Ph:
Ph: House 3 Blue Phone
All senior management staff have mobile phones and they are to ensure they are fully charged.
A spare phone charger is available in Reception for emergency use.
Outline – the communication plan
Page 31 of 34
Appendix 9
Emergency Electrical Supply Plan
X Care Centre:
If a power failure occurs the generator will automatically be activated.
Contact Building and Facilities Officer / after hours Security Personal and inform them that the generator has started.
Emergency power will only service some lights and power outlets such as:
Lift – No 1 west end, kitchen side of reception.
Lighting – alternate lighting in passage ways / bathrooms / treatment rooms / nurses stations.
Power – nurse call system. Power points as marked.
Y Care Centre:
1. In the event of a power failure the Building & Facilities / Security
Officer will be notified by the Senior Nurse on duty:
Monday to Friday 0730 – 1600
Building & Facilities / Security Officer Ph
After hours and weekends
Contact Security Officer Ph
2. A battery back up system will give sufficient light until the generator is started (1/2 hour maximum).
3. All maintenance and security staff are trained in starting the generator – emergency power supply.
The generator is located in the undercroft are – rear of Y Care Centre.
The key for the generator is located on the inside of the pillar adjacent to the cage surrounding the generator.
Start engine as per instructions (copy of instructions are attached to cage of generator).
Check generator for fuel each hour if normal power supply is out for an extended period.
Page 32 of 34
When normal power is restored, follow instructions to shut down the generator.
Report level of fuel reserved in tank and container to Building &
Facilities Officer.
4. Lighting, telephone at reception and circulating hot water pumps
and igniters for gas hot water system will operate automatically from the Emergency Power Supply.
5. When normal power is resumed, Building & Facilities Officer or
Security personnel are to be notified to disconnect and close down emergency generator safely.
6. With our ‘Preventative Maintenance Program’ the generator will be tested monthly.
Page 33 of 34
Facility
Appendix 10
Residential Aged Care Facility Resources
Number
Of Beds
Number
Of
Additional
Residents
Number
Of Staff
Available
Transport
Other
Resources
Page 34 of 34