Tumors of Kidney & Urinary Tract
advertisement

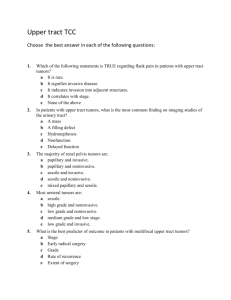
Course: IDPT 5005 University of Colorado Denver, School of Medicine Francisco G. La Rosa, M.D. (Francisco.LaRosa@ucdenver.edu) Associate Professor TUMORS OF KIDNEY & URINARY TRACT I. LEARNING OBJECTIVES 1. List the most common benign and malignant tumors of the kidney and describe their most important characteristics in regards to: a. Incidence b. Clinical features c. Imaging features d. Urinary findings e. Gross pathology f. Microscopic pathology g. Staging and Prognosis 2. Understand the basic genetic differences between spontaneous and familial renal tumors. 3. Describe the most important benign and malignant tumors of the urinary tract, calyx, pelvis, ureter, urinary bladder, and urethra. II. TUMORS OF THE KIDNEY Both benign and malignant tumors occur in the kidney. With the exception of oncocytoma, the benign tumors rarely cause clinical problems. Malignant tumors, on the other hand, are of great importance clinically and deserve considerable emphasis. By far the most common of these malignant tumors is renal cell carcinoma (RCC), followed by Wilms tumor, which is found in children and will be discussed in a separate lecture, and finally urothelial tumors of the calyces and pelves. Although some tumors that occur more commonly in adults may also occasionally be encountered in children and vice versa, a broad separation of renal tumors according to patient age is an arbitrary but widely accepted practice whose usefulness has been validated by many years of experience. Most of the pathological categories of neoplasms have been documented as primary tumors of the kidney, particularly in adults, but most tumors are carcinomas that conform to a rather narrow range of histologic lesions differentiating in whole or in part toward renal tubular epithelial structures. A. BENIGN TUMORS: 1. Renal Papillary Adenoma: Well circumscribed nodules within the cortex, 7 – 22 % at autopsy, small (5 mm diameter). Surgically removed since they are considered “early cancers.” 2. Renal Fibroma or Hamartoma (Renomedullary Interstitial Cell Tumor): Fibrous, less than 1 cm, within pyramids, no malignant tendency. 3. Angiomyolipoma: Vessels, smooth muscle and fat. 25 -50% in patients with tuberous sclerosis. 4. Oncocytoma: Eosinophilic epithelial cells, numerous mitochondria, 5 – 15% of all renal neoplasms. Some cases are familial. 5. Metanephric adenoma. Very rare, only one case in a child known to produce metastases. Tumors of Kidney and Urinary Tract Page 1 B. MALIGNANT TUMORS: In the broadest sense, most renal tumors could be classified as adenocarcinoma, but current usage prefers the term renal cell carcinoma (RCC) to distinguish them. In the USA, renal cancer is the 7th leading malignant condition among men and the 12th among women, accounting for 2.6 % of all cancers. About 2% of cases of renal cancer are associated with inherited syndromes. In the USA, more than 36,000 new cases of renal cancer are predicted to occur every year, many of which are being discovered earlier because of the widespread availability of radiographic testing. Nevertheless, more than 12,000 deaths from the disease are predicted to occur every year. RCC arise from the renal epithelium and account for about 85 % of renal cancers. A quarter of the patients present with advanced disease, including locally invasive or metastatic RCC. Moreover, a third of the patients who undergo resection of localized disease will have a recurrence. Median survival for patients with metastatic disease is about 13 months. Thus, there is a great need for more effective surgical and medical therapies. The biological behavior of RCC is generally malignant, but the few benign tumors in the group cannot be distinguished by size alone. The classification of RCC has recently undergone revision, based on correlative cytogenetic, genetic, and histologic studies of both familial and sporadic tumors. 1. Clear Cell Carcinoma Incidence: Most common type, accounting for 70% to 80% of renal cell cancers (third most common urologic malignancy, found in 3% of the adult population). Male to female ratio 3:1. Clinical: o Hematuria. o Renal mass may be incidental finding on imaging study. o Arises in the renal cortex, has a propensity to invade the renal vein and can extend into the inferior vena cava up to the heart. o Regional lymph nodes may be enlarged. Hematogenous spread to lungs may occur, too. Metastatic disease often as multiple nodules in the lungs. Imaging: o Ball-like mass of renal cortex; tumor enhances less than normal parenchyma. o Engorged, tumor-filled renal vein with extension to inferior vena cava. o Look for metastatic disease. Pathology: o Gross: Most often as single tumor (multifocal and bilateral in Von Hippel-Lindau disease), somewhat spherical, yellowish gray mass, variegated appearance, focal hemorrhage, 20% are cystic. o Histology: In clear cell RCC three cell types are generally recognized -clear, granular, and spindle. Most tumors are composed of clear cells, granular cells, or a mixture of these two cell types. Nuclear grade of tumor cells is assigned according to Fuhrman's criteria, and varies from 1 to 4. Nuclear grade in RCC is an important independent predictor of survival; that is tumors of grades 1-2 carry a better prognosis than tumors of grades 3-4. Spindle cell types or sarcomas tend to grow and spread more quickly than the other kinds of RCCs. They can be associated with any of subtype mentioned and this subtype portends poorer prognosis. Genetics: o Current studies implicate the VHL gene in the development of both familial and sporadic clear cell tumors. a. Familial, associated with VHL (Von Hippel-Lindau) disease (4% of cases) b. Most cases (95%) are sporadic. Tumors of Kidney and Urinary Tract Page 2 o 98% of tumors: loss of sequences on short arm chromosome 3 by deletion (3p-) or by unbalanced chromosomal translocation (3;6, 3;8, 3;11) resulting in loss of chromosome 3 spanning 3p12 to 3p26. This region harbors the VHL gene (3p25.3). o A second nondeleted allele of the VHL gene shows somatic mutations or hypermethylation-induced inactivation in about 80% of clear cell cancers, indicating that the VHL gene acts as a tumor-suppressor gene in both sporadic and familial cancers. o VHL gene: encodes a protein that is part of a ubiquitin ligase complex involved in targeting other proteins for degradation. Important among the targets of the VHL protein is hypoxia-inducible factor-1 (HIF-1). When VHL is mutated, HIF-1 levels remain high, and this constitutively active protein increases the transcription and production of hypoxia-inducible, pro-angiogenic proteins such as VEGF and TGF-β1. In addition, insulin-like growth factor-1, another VHL target, is upregulated. Thus, both cell growth and angiogenesis are stimulated. Prognosis: The average 5-year survival rate of patients with renal cell carcinoma is about 45% and up to 70% in the absence of distant metastases. With renal vein invasion or extension into the perinephric fat, the figure is reduced to approximately 15% to 20%. Nephrectomy has been the treatment of choice, but partial nephrectomy to preserve renal function is being done with increasing frequency and similar outcome. 2. Papillary carcinoma (Chromophilic) Incidence: Represent 10% to 15% of renal cancers. Pathology: o Gross: Unlike clear cell RCCs, papillary carcinomas are frequently multifocal. o Histology: Papillary growth pattern. Genetics: Occurs in both familial and sporadic forms. Not associated with 3p deletions. o Most common cytogenetic abnormalities are trisomies 7, 16, and 17 and loss of Y in male patients in the sporadic form, and trisomy 7 in the familial form. o The gene for the familial form has been mapped to a locus on chromosome 7 (MET locus, a protooncogene that serves as the tyrosine kinase receptor for hepatocyte growth factor). This gene has also been shown to be mutated in a proportion of the sporadic cases of papillary carcinoma. Prognosis: Better than clear cell RCC. 3. Chromophobe Renal Carcinoma Incidence: Represents 5% of renal cell cancers Pathology: Cells with prominent cell membranes and pale eosinophilic cytoplasm, usually with a halo around the nucleus. Histologic distinction from oncocytoma can be difficult. Genetis: multiple chromosome losses and extreme hypodiploidy. They are, like the benign oncocytoma, thought to grow from intercalated cells of collecting ducts. Prognosis: Excellent compared with that of the clear cell and papillary cancers; similar to oncocytomas. 4. Collecting Duct (Bellini duct) Carcinoma Incidence: Represents approximately 1% or less of renal epithelial neoplasms. They arise from collecting duct cells in the medulla. Pathology: Nests of malignant cells enmeshed within a prominent fibrotic stroma, typically in a medullary location. Genetics: A number of chromosomal losses and deletions have been described for this tumor, but a distinct pattern has not been identified. Prognosis: Associated with aggressive behavior and poor prognosis. For the majority of patients surgical treatment will not result in a cure. Previously recommended chemotherapy Tumors of Kidney and Urinary Tract Page 3 and/or immunotherapy appear to have a limited role in treatment of this disease, and early detection may be the best method for prolonging patient survival. 5. Familial RCC: Incidence: o Although they account for only 4% of renal cancers, familial variants have been enormously instructive in studying renal carcinogenesis. Von Hippel-Lindau (VHL) syndrome: 1/2 to 2/3 of VHL patients: o hemangioblastomas of the cerebellum and retina o develop renal cysts and bilateral, often multiple, renal cell carcinomas (nearly all, if they live long enough) o Current studies implicate the VHL gene in the development of both familial and sporadic clear cell tumors. Hereditary (familial) clear cell carcinoma, confined to the kidney, without the other manifestations of VHL but with abnormalities involving the same or a related gene. Hereditary papillary carcinoma. This autosomal-dominant form is manifested by multiple bilateral tumors with papillary histology. These tumors exhibit a series of cytogenetic abnormalities and, as will be described, mutations in the MET protooncogene. C. STAGING MALIGNANT RENAL TUMORS The most important factor in predicting prognosis is the stage. The stage describes the cancer's size and how deeply it has spread beyond the kidney. The Staging System of the American Joint Committee on Cancer (AJCC) is sometimes known as TNM system. The letter T followed by a number from 1 to 3 describes the tumor's size and spread to nearby tissues. Higher T numbers indicate a larger tumor and/or more extensive spread to tissues near the kidney. The letter N followed by a number from 0 to 2 indicates whether the cancer has spread to lymph nodes near the kidney and, if so, how many are affected. The letter M followed by a 0 or 1 indicates whether or not the cancer has spread to distant organs (for example, the lungs or bones) or to lymph nodes that are not near to the kidneys. 1. Stage I: The tumor is 7 cm (about 2 3/4 inches) or smaller, and limited to the kidney. There is no spread to lymph nodes or distant organs. 2. Stage II: The tumor is larger than 7.0 cm but still limited to the kidney. There is no spread to lymph nodes or distant organs. 3. Stage III: There are several combinations of T and N categories that are included in this stage. These include tumors of any size, with or without spread to fatty tissue around the kidney, with or without spread into the large veins leading from the kidney to the heart, with spread to one nearby lymph node, but without spread to distant lymph node or other organs. Stage III also includes tumors with spread to fatty tissue around the kidney and/or spread into the large veins leading from the kidney to the heart, that have not spread to any lymph nodes or other organs. 4. Stage IV: There are several combinations of T, N, and M categories that included in this stage. This stage includes any cancers that have spread directly through the fatty tissue and the fascia ligament-like tissue that surrounds the kidney. Stage IV also includes any cancer that has spread to more than one lymph node near the kidney, to any lymph node not near the kidney, or to any other organs such as the lungs, bone, or brain. Tumors of Kidney and Urinary Tract Page 4 T, N, M categories and stage groupings T - Primary tumor: TX: Primary tumor cannot be assessed T0: No evidence of primary tumor T1: Tumor 7 cm or less, limited to kidney T2: Tumor greater than 7 cm, limited to kidney T3: Tumor extends into major veins/adrenal/perinephric tissue; not beyond Gerota's fascia T3a: Tumor invades adrenal/perinephric fat T3b: Tumor extends into renal vein(s) or vena cava below diaphragm T3c: Tumor extends into vena cava above diaphragm T4: Tumor invades beyond Gerota's fascia N - Regional lymph nodes: NX: Regional nodes cannot be assessed N0: No regional lymph node metastasis N1: Metastasis in a single regional lymph node N2: Metastasis in more than one regional lymph node M - Distant metastasis: MX: Distant metastasis cannot be assessed M0: No distant metastasis M1: Distant metastasis III. TUMORS OF THE URINARY TRACT About 95% of urinary tract tumors are of epithelial origin, the remainder being mesenchymal tumors. Most epithelial tumors are composed of urothelial (transitional) type cells and are thus interchangeably called urothelial or transitional tumors, but squamous and glandular carcinomas also occur. A small number of benign neoplasias of the urinary tract are represented by small tumors generally of mesenchymal origin. The two most common are fibroepithelial polyps and leiomyomas. The fibroepithelial polyp is a tumor-like lesion that grossly presents as a small mass projecting into the lumen. The lesion occurs more commonly in the ureters (left more often than right) but may also appear in the bladder, renal pelves, and urethra. The polyp presents as a loose, vascularized connective tissue mass lying beneath the mucosa. A. TRANSITIONAL CELL NEOPLASMS Incidence: 80% patients between 50 -80 years. Male to female ratio 3:1. More frequent in urban areas. Fifty to 80% of all bladder cancers are in smokers. Industrial exposure to acrylamides (2-snaphthylamine). Schistosoma haematobium infections in Egypt and Sudan. Exposure to radiation. Clinical: o Comprise more than 90% of tumors that arise from the urinary tract, other cell types include squamous cell and adenocarcinomas. o Clinical presentation includes hematuria and irritative bladder symptoms such as dysuria, urinary frequency and urgency. Tumors of Kidney and Urinary Tract Page 5 o o o o The hematuria may be episodic, gross or microscopic. May be an incidental finding on urinalysis. TCC may arise from the renal calyces, pelvis, ureters, bladder, urethra and urothelium lined ducts in the prostate. The tumor can extend to the pelvic sidewalls and metastases can go to the lungs, bones and liver. The tumor can cause ureteral obstruction leading hydronephrosis, unilateral or bilateral depending on its location. Imaging: o Multiple modalities, CT, MRI, cystography, IVP can demonstrate the tumor o Tumors appear as filling defects in the urinary tract. o Appearance depends on the size of the tumor and whether it is polypoid or sessile Pathology: The gross patterns of urothelial cell tumors vary from purely papillary to nodular or flat. The tumors may also be noninvasive or invasive. The level of invasion has prognosis significance and can involve the lamina propria, muscularis propria, peri-cystic fat tissue and other organs. Papillary lesions appear as red, elevated excrescences varying in size from less than 1 cm in diameter to large masses more than 5 cm in diameter. Multicentric origins may produce separate tumors. The histologic changes encompass a spectrum from benign papilloma to highly aggressive anaplastic cancers. Overall, the majority of papillary tumors are low grade. Most arise from the lateral or posterior walls at the bladder base. Genetics: There is no familial tendency. Prognosis: Depending on grade and stage. Grading of Urothelial (Transitional Cell) Tumors (WHO/ISUP Grades): - Urothelial papilloma (benign) - Urothelial neoplasm of low malignant potential (Grade 0) - Papillary urothelial carcinoma, low grade (Grade 1) - Papillary urothelial carcinoma, high grade (Grades 2 and 3) Staging of Bladder Carcinoma, AJCC/UICC (Depth of Invasion): Noninvasive, papillary (Ta) Carcinoma in situ (noninvasive, flat) (Tis) Lamina propria invasion (T1) Muscularis propria invasion (T2) Microscopic extra-vesicle invasion (T3a) Grossly apparent extra-vesicle invasion (T3b) Invades adjacent structures (T4) Therapy: BCG, Electrocautery, Surgery REFERENCES - Chapters 20 & 21. Kumar, Robbins and Cotran: Pathologic Basis of Disease, 7th ed. WB Saunders Co. Online: http://www.mdconsult.com/das/book/body/94286448-2/0/1249/0.html Urological Pathology by William M. Murphy, Saunders, 2nd Edition, 1997, pp. 442-502 Herbert T. Cohen HT, McGovern FJ. Renal-Cell Carcinoma. N Engl J Med 2005;353:2477-90. http://medinfo.ufl.edu/~bms5191/renal/renal.html http://library.med.utah.edu/WebPath/RENAHTML/RENALIDX.html http://www.uchsc.edu/pathology/smallgroups/renal/ Tumors of Kidney and Urinary Tract Page 6 Disclaimers: 1. The primary goal of this chapter is to study the learning objectives outlined at the beginning of this handout. The material to study is provided in the lectures, the handouts and the recommended textbooks. All these sources provide the content over which you will be tested. The lectures are intended to provide broad information of the material found in the textbooks and handouts, and to give the students the opportunity to ask questions on subjects not clear in the texts. The handouts do not seek to follow up the sequence of the lectures, and most importantly, they are not a surrogate of the books. 2. The text presented in this handout has been edited by Dr. La Rosa from material found in your books, from published articles and other educational works. This handout is solely for educational purpose and not intended for commercial or pecuniary benefit (see USA Copyright Law, Section 110, “Limitations on exclusive rights: Exemption of certain performances and displays”). Reproduction and use of this handout can be done only for educational use. [Download] the USA Copyright Law version, October 2009. Tumors of Kidney and Urinary Tract Page 7