Cardiac Glycosides
advertisement

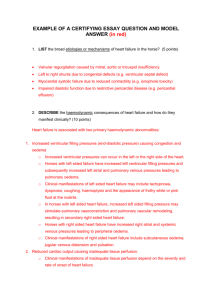
DRUGS USED IN THE TREATMENT OF HEART FAILURE Hanna Winiarska MD, PhD I. Positive inotropic drugs: 1.Cardiac Glycosides – a. no effect on mortality b. reduce hospitalization c. increase quality of life Mechanism of action: inhibition of Na+/K+-ATPase in cardiac myocytes – increased Ca intracellular level Pharmacological effects: Cardiac effects: 1. positive inotropic effect – increased contractility 2. electrical effects: a. decrease in action potential duration as a result of increased K+ conductance b. reduced resting membrane potential (less negative) due to inhibition of the Na pump and reduced intracellular K+ concentration c. overloading of the intracellular Ca++ stores and oscillation in the free intracellular Ca++ ion concentration - delayed afterdepolarizations, (ectopic beat, bigeminy) - positive batmotropic effect d. cardioselective parasympathomimetic effects (atrial and atrioventricular nodal tissue) in low doses – negative chronotropic and dromotropic effect e. toxic doses - stimulation of sympathetic activity Effects on other organs: a. decrease in vascular tone b. GI tract – anorexia, nausea, vomiting, diarrhea (direct effects and stimulation of chemoreceptor trigger zone in cns) c. CNS – vagal and chemoreceptor zone stimulation; disorientation, hallucinations (especially in the elderly), visual disturbances (aberrations of color perception), agitation and conmvulsions d. Gynecomastia (peripheral estrogenic action or hypothalamic stimulation) Toxicity of cardiac glycosides: Psychiatric - delirium, fatigue, malaise, confusion, dizziness, abnormal dreams Visual- blurred or yellow vision, halos Gastrointestinal -anorexia, nausea, vomiting, abdominal pain Respiratory - enhanced ventilatory response to hypoxia Cardiac arrhythmias - atrial and ventricular ectopic arrhythmias Conduction disturbances - sinoatrial and atrioventricular node conductions disturbances 1 Interaction with potassium, calcium and magnesium ions K+- hypokalemia increases the toxicity of cardiac glycosides Ca2+ - hypercalcemia facilitates the toxic actions of cardiac glycosides Mg2+ - hypomagnesemia, a risk factor for arrhythmias Clinical uses of digitalis: 1. heart failure (STAGE B-D; NYHA class I-IV) in patients with atrial fibrillation 2. symptomatic heart failure (Stage C-D; NYHA class II-IV) in patients with sinus rhythm 3. atrial fibrillation in patients without HF (second-line therapy) Contraindication: 1. ventricular arrhythmias 2. arrhythmias associated with pr-excitation syndrome 3. hypertrophic cardiomyopathy 4. recent myocardial infarction with sinus rhythm 5. sinus bradycardia, second- or third-degree AV conduction delay Preparations: digoxin Other positive inotropic drugs used in heart failure: Clinical indications: Acute or decompensated heart failure - patients with peripheral hypoperfusion (hypotension, decreased renal function) with or without congestion or pulmonary edema refractory to diuretics and vasodilators at optimal doses Beneficial hemodynamic effect may be counteracted by the risk of arrhythmias and myocardial ischemia 1. drugs that inhibit phosphodiesterases (PDE-I) a. selective- bipyridines (ENOXIMONE, MILRINONE) mechanism of action: selective inhibition of isoform III of PDE; pharmacodynamic effects: increased myocardial contractility; some vasodilating effect toxicity - nausea, vomiting, thrombocytopenia, liver enzyme changes. indication: short-term parenteral treatment of acute HF; alternative for patients on beta-blocker therapy 2. beta-adrenoreceptor stimulants (dobutamine, dopamine) Dopamine - inotropic, chronotropic and vasoactive properties – dose dependent 0.5-2(3)ug/kg/min – dopaminergic receptors renal blood flow 2(3) – 5 ug/kg/min – stimulation of beta-1 receptors inotropic effect, chronotropic effect CO 5-10 ug/kg/min – stimulation of beta-1 and alpha-1 receptors vasoactive effect unpredictable > (10)15-20 ug/kg/min – activation of alpha-1 receptors SVR Onset of action – within minutes Hemodynamic response – variable among patients Dobutamine - agent with predominant direct beta-1 agonist effects and weak beta-2 and alpha-1 effects compared to dopamine – equal or greater inotropic action - in PCWP and SVR with increasing doses - less chronotropic at lower infusion rates - preferred in patients with CO, normal or moderately PCWP and moderate or severe hypotension Levosimendan - calcium sensitizer, binds to troponin-C in cardiomyocytes; - mild PDE inhibitory action; - significant vasodilating action via ATPsensitive action; Indication: patients with decompensated chronic HF; alternative for patients on betablocker therapy II.Diuretics Loop diuretics (furosemide, bumetanide, torasemide) Thiazides (hydrochlorothiazide) Potassium sparing diuretics (aldosterone antagonists – spironolactone, eplerenone; triamterene) Clinical use of diuretics in patients with HF: 1. indications: patients with fluid retention (edema, dyspnoe) 2. contraindications: orthostatic hypotonia, side effects related to particular drug 3. the choice of therapy: a. mild heart failure – thiazides b. moderate heart failure – loop diuretic (typically furosemide 40 mg 1-2/day) c. severe heart failure – loop diuretic (furosemide 120-250mg in one dose or bumetanide 3-5mg/day; or combination of loop diuretics and thiazidemetolazone) 2 potassium sparing diuretics – additive therapy in patients with hypokalemia e. aldosterone antagonists (spironolactone, eplerenone) – additive therapy (to improve survival rate) in patients with HF 4. adequate monitoring of daily weights, blood pressure, and blood electrolyte levels 5. side effects: hypokalemia/hyperkalemia, hyponatremia, hyperuricemia, hypomagnesemia, acid-base equilibrium disturbances III. Vasodilators 1. ACE inhibitors (ACE-Is) Mechanism of action : inhibition of the conversion of the angiotensin I to angiotensin II; increase in bradykinin levels; increase of rennin release and angiotensin I formation. Effects of ACE inhibition in heart failure 1. reduced afterload and systolic wall stress increased cardiac output, reduced heart rate, increased exercise tolerance 2. decreased blood pressure 3. increased renal blood flow – increased natriuresis 4. reduced venous return to heart (venodilation) - diminished preload and diastolic wall stress 5. improvement in ventricular geometry (changes in preload and afterload, prevention of the growth effects of angiotensin II, decrease aldosteron induced cardiac fibrosis) Clinical use of ACE-I in patients with heart failure: chronic heart failure (STAGE A-D; NYHA class IIV) with left ventricle dysfunction (LVEF<40-45%) – first-line therapy! Contraindications: 1. pregnancy 2. hypotension 3. angineurotic edema - during previous therapy with ACE-Is 4. bilateral renal stenosis or stenosis of the artery to a single remaining kidney, others severe kidney’s diseases 5. hyperkalemia K>5.5mmol/l Adverse effects of ACE-I 1. related to decreased AT II plasma level: a. hypotension b. hyperkalemia c. worsening of renal function (patients with low renal perfusion pressure) d. fetopathic potential 2. related to increased bradykinin plasma level a. dry cough (5-10% patients) d. b. angineurotic edema 0,1-0,2% of patients 2. Angiotensin II receptor antagonists (ARBs) Mechanism of action: ARBs bind to AT1 receptor and inhibit biological effects of angiotensin II Differences between ACE-I and ARBs ARBs reduce activation of AT1 more 1. effectively than do ACE-I; ACE-I do not inhibit the alternative angiotensin II generating pathway 2. ARBs indirectly activate AT2 receptors increasing angiotensin II level 3. ARBs do not increase ACE substrates (bradykinin) Indications: 1. alternative therapy for patients who cannot tolerate ACE-Is (caught, angioedema) 2. in combination with ACE-Is in symptomatic patients despite the use of standard therapy who cannot tolerate aldosteron antagonists 3. Combination nitrates/hydralazine Nitrates (isosorbide dinitrate) relatively selective for veins – decreases ventricular filling pressure (low doses) in higher doses decreases the systemic and pulmonary arterial resistance adverse effects: - hypotension - tachycardia - dizziness, headache - fluid retention Hydralazine direct action in vascular smooth muscle reduces right and left ventricular afterload has direct moderate positive inotropic activity has minimal effect on venous capacitance (should be combined with agents with venodilating activity – organic nitrate) reduces renal vascular resistance and increases renal blood flow – may be useful in heart-failure patients with renal dysfunction who cannot tolerate an ACE-I adverse effects: - hypotension - headache, dizziness - lupus erythematosuslike syndrome Clinical indications: - an alternative to an ACE-I/ARB when are not tolerated - as add-on therapy to an ACE-I/ARB 3 4.Nesiritide recombinant human brain natriuretic peptide (BNP) pharmacological action: venous, arterial, coronary vasodilator indications: management of acute heart failure; patients with AHF with fluid overload, with PCWP >18-20 mmHg despite of high doses of diuretics and NTG iv; should be avoided in patients with SBP<90-100mmHg 5.Ca2+channel antagonists The use of amlodipine or felodipine may be considered in patients requiring: additional control of blood pressure or afterload reduction or if other vasodilators are contraindicated or poorly tolerated verapamil and diltiazem may be useful in the treatment of diastolic heart failure (by slowing heart rate may facilitate diastolic relaxation and lower diastolic filling pressures); are contraindicated in patients with systolic heart failure IV. beta-adrenergic receptor antagonists : First-line drugs in HF Effects of beta-blockers in patients with HF: 1. improve in left ventricular structure and function 2. decrease in chamber size 3. increase in ejection fraction 4. decrease in malignant ventricular arrhythmias 5. reduce of oxidative stress in the mycoradium Clinical use of beta-adrenergic receptor antagonists in HF (metoprolol, carvedilol, bisoprolol, nebivolol): 1.indications: beta-blockers should be prescribed to: all patients with stable HF due to left ventricular systolic dysfunction patients with normal LVEF or with diastolic dysfunction to reduce HR and increase diastolic period IN GENERAL, BETA-BLOCKERS ARE USED TOGETHER WITH AN ACE INHIBITORS Procedure for starting a beta-blocker: *patient should be on a background therapy with ACE-I *patient should be stable *therapy should be started with a very low doses and titrate up to maintenance dose *the dose may be doubled every 1-2 weeks if the preceding dose was well tolerated *patient should be monitor for the symptoms of worsening of HF and side effects of beta-blockers ( initiation of therapy can cause fluid retention) Contraindication: hypotension, decompensated HF, asthma, symptomatic atrioventricular blocks and bradycardia V. IVABRADINE Mechanism of action: inhibition of the If channel in the sinus node Its only known pharmacological effect is TO SLOW THE HEART RATE in patients in sinus rhythm (it does not slow the ventricular rate in AF) Should be considered 1. to reduce the risk of HF hospitalization in patients in sinus rhythm with an EF ≤35%, a heart rate ≥70 b.p.m., and persisting symptoms (NYHA class II–IV) despite treatment with an evidence-based dose of beta-blocker (or maximum tolerated dose below that), ACE inhibitor (or ARB), and an aldosteron antagonist (or ARB) 2. to reduce the risk of HF hospitalization in patients in sinus rhythm with an EF ≤35% and a heart rate ≥70 b.p.m. who are unable to tolerate a beta-blocker.Patients should also receive an ACE inhibitor (or ARB) and an MRA (or ARB) VI. Anticoagulation and antiplatelet drugs in HF Anticoagulation therapy with warfarin is recommended for patients: with atrial fibrillation or a history of previous embolic event, if there is evidence of a left venticular thrombus, if the left ventricular dysfunction is severe and the ventricles are markedly dilated Aspirin therapy: patients with coronary artery disease related HF VII. Antiarrhytmic drugs in HF ALL antyarrhythmic drugs have negative inotropic and proarrhythmic properties. It is not recommended to use antyarrhythmic drugs in patients with HF. Possible exception is amiodarone (agent with additional beta-adrenergic suppressing properties). Patients with HF and ventricular arrhythmias should be managed with implanted cardiac defibrillator (ICD). 4