Immunosuppression for neurological disease

Immunosuppression for neurological disease
M.Engelen
J.
de Gans
A.J. v.d. Kooi
I.N. van Schaik
A.
Seeber
M.
Vermeulen
M.
de Visser
Last updated: may 2009
Introduction
The information in this protocol is based on the most recent peer reviewed literature. The authors tried to provide several standardised treatment protocols for the different diseases.
The treatment protocols are described in the appendices. For a prednison dose of 40 mg or higher a twice daily dosing regimen can be considered.
General precautions:
Before starting immunosuppresive medication active infection has to be excluded if there is an index of clinical suspicion:
urine culture
sputum culture
serologic test for specific viruses
chest X-ray
if exposure to tropical environment and/or high eosinophil count: feces test for amoebe and Strongyloides
During immnosuppressive treatment
if fever (> 38 degrees C): blood cultures (3 times)
urine culture
specific culture (sputum, skin defects or ulcers)
viral pathogens (serologic test, urine, throat swabs)
chest X-ray (also if low index of suspicion based on physical examination)
Specific diseases
Acute disseminated encephalomyelitis
Arteriitis temporalis (giant cell arteritis)
Behcet disease
Chronic inflammatory demyelinating polyneuropathy
Churg-Strauss disease
Dermatomyositis
Gullain-Barre syndrome (acute inflammatory demyelinating polyneuropathy)
Isolated cerebral vasculitis
Horton’s neuralgia (cluster headache)
Leukoclastic vasculitis (hypersensitivity vasculitis; cutaneous vasculitis)
Multifocal motor neuropathy
Multiple sclerosis
Myasthenia gravis and Lambert-Eaton myasthenic syndrome
Polymyalgia rhaumatica
Polymyositis and dermatomyositis
Giant cell arteriitis
Neurosarcoidosis
Systemic vasculitis (PAN; microscopic polyangiitis; vasculitis not otherwise classified)
Systemic lupus erythematosus with neurologic and/or neuropsychiatric symptoms
Takayashu’s arteriitis
Appendices with treatment protocols:
Treatment protocol 1 (prednison)
Treatment protocol 2 (methylprednisolon)
Treatment protocol 3 (prednison/cyclofosfamide)
Appendices with information on medication: azathioprine ciclosporine cyclofosfamide
NSAID
IV immunoglobulin corticosteroids (pulse) corticosteroids (maintenance therapy) methotrexate thalidomide
Acute disseminated encephalomyelitis
I.
methylprednisolone i.v. (3 - 5 days 1 gram/day), then prednisolone maintenance therapy (treatment protocol 2).
II.
IV immunoglobulin
III.
plasmapheresis
IV.
mitoxantrone / cyclofosfamide p.o.
No randomized controlled trials are available to guide therapy. Treatment of ADEM is in part extrapolated from MS treatment. There is class I evidence for the use of plasmapheresis in case of life threathening demyelination (not necessarily ADEM), there are case series. Advice is to be considered expert opinion only.
Literature
Acute Disseminated encephalomyelitis. Marchioni E, Tavazzi E, Minoli L, et al. Curr Infect Dis Rep
2008; 10 (4): 307-14.
Post Infectious encephalitis in adults: diagnosis and management. J Infection 2009 in press Acute
Disseminated encephalomyelitis. An Update. Menge T, Hemmer B, Nessler S, et al. Arch Neurol
2005: 62: 1673-80.Acute Disseminated encephalomyelitis.Tenembaum S, Chitnis T, Ness J et al.
Neurology 2007'68: S23-S36.
Arteriitis temporalis (giant cell arteriitis)
I A. Start with prednisolon 40 mg/day orally (treatment protocol 1). When symptoms disappear and ESR is < 30 mm/h, reduce dosis as in treatment protocol 1. If symptoms return double prednisolon dose (return to starting dose if necessary). Class Ib.
B. Start with Ascal 100 mg once daily after temporal artery biopsy, and PPI (Class
III).
Consider a twice daily dosing regimen (possibly more effective, but more toxic). When symtpoms dissapear dose once daily over a period of 4 weeks. Then reduce dose as in treatment protocol 1, using the ESR as a parameter for disease activity.
II In high-risk patient (e.g. diabetes mellitus, osteoporosis, etc) or second recurrence of symptoms during dose reduction, request a rheumatology consultation. Add methotrexate to treatment regimen (0.15 - 0.25 mg/kg/week).
NB If there are ocular symptoms consult a ophthalmologist. If recent severe loss of visual acuity consider methylprednisolone 1g/day during 3 days and then prednisolone 1 mg/kg during 4 weeks. If symptoms are controlled and ESR < 30 mm/h, reduce dose as described in treatment protocol 1.
Literature
G Nesher, Y Berkun, M Mates et al. Low-dose aspirin and prevention of cranial ischemic complications in giant cell arteritis. Arthritis Rheum 2004; 50: 1332-37
N Pipitone and C Salvarani. Improving therapeutic options for patients with giant cell arteritis.
Curr Opin Rheumatol 2008; 20:17-22.C Salvarani, F Cantini, GG Hunder. Polymyalgia rheumatica and giant-cell arteritis. Lancet 2008: 372: 234-45.
Behcet disease
I. Treatment for (meningo)encephalitis:
- methylprednisolone i.v. 1 g/day for 3 - 7 days, then maintenance therapy with
- prednisolone orally 1 mg/kg (treatment protocol 1). if not effective or recurrence of symptoms add methotrexate (7.5-12.5 mg/week) or azathioprine (2.5 mg/kg/day), consult a rheumatologist.
- if not effective consider TNF-alpha antagonist (after rheumatology consultation)
II. Therapy for cerebral venous sinus thrombosis (CVST)
Refer to appropriate protocol. If also vasculitis see below.
III. Therapy for vasculitis / aneurysms (also consult with rheumatologist)
- prednisolon (treatment protocol 2) and cyclofosfamide 2 mg/kg per day orally for 3 months. Then substitute with azathioprine 2 mg/kg per day; continue for at least 1 year after reaching clinical remission.
- dose.
- if no remission after 3 months consider methotrexate 10 mg/week orally, up to 30 mg/week. Add folic acid 5 mg per week 24 hours after methotrexate thalidomide can be considered (teratogenic!)
NB if aneurysms of pulmonary vessels are present anticoagulation is not advisable.
NB2 ciclosporin (used for BD uveitis) is neurotoxic
NB3 diagnostic criteria are summarized in Lancet Neurology 2009;8:192-204.
Treatment is based on Class III and IV evidence.
Literature
A Al-Araji and DP Kidd. Neuro-Behcet’s disease: epidemiology, clinical characteristics, and management. Lancet Neurol 2009: 8: 192-204
G Hatemi et al. EULAR recommendations for the management of Behcet disease. Ann Rheum Dis
2008; 67: 1656-62G Tomasson, PA Monach and PA Merkel. Thromboembolic disease in vasculitis.
Curr Opin Rheumatol 2009; 21: 41-46
A Saenz et al: Pharmacotherapy for Behcet’s syndrome (Review). The Cochrane Library 2009, issue 2
Chronic inflammatory demyelinating polyneuropathy
I. Dexamethasone 40 mg/day 4 days per week in week 1,4,7,11,15 and 19 (Class IV).
II. Prednisolone as in treatment protocol 1. If recurrence during dose reduction, double dose (maximum 60 mg/day) (Class II).
III. IV immunoglobulin 2 g/kg in 2 or 5 days, if rapid response is necessary or complications of long-term steroid treatment are expected. Af induction, maintenance therapy will be necessary, usually 0.4 g/kg in one day every 2 to 4 weeks (titrate based on clinical respone in individual patients) (Class I).
IV. Prednisolon as maintenace therapy after III: use treatment protocol 1, but start in week 6.
V. Consider plasmapheresis if other treatments fail.
VI. Azathioprine (as detailed in appendix). Consider combination with prednisolone
(Class IV). The supposed “steroid sparing” effect is not conclusively proven!
Literatuur
Hughes RAC, Bouche P, Cornblath DR, Evers E, Hadden RDM, Illa I, Koski CL, Léger JM, Nobile-
Orazio E, Pollard JD, Sommer C, Van den Berg PYK, Van Doorn PA, van Schaik IN. European
Federation of Neurological Societies/Peripheral Nerve Society Guideline on management of chronic inflammatory demyelinating polyradiculoneuropathy. Report of a joint task force of the
European Federation of Neurological Societies and the Peripheral Nerve Society. Eur J Neurol.
2006;13:326-32.
Churg-Strauss disease
I. Methylprednisolone (treatment protocol 2).
II. If neurological symptoms or incomplete response to I, add cyclofosfamide 2 mg/ kg / day for 3 months. Then start azathioprine 2 mg/kg/day until 1 year after reaching remission.
Literature
Pagnou C, Guilpain P, Guillevain L. Churg-Strauss Syndrome. Curr Opin Rheumatol 2007; 19: 25
– 32.
Polymyositis and dermatomyositis
I. A. Dexamethason pulse therapy 40 mg/day during 4 subsequent days with an interval of 28 days.
OR
B. Prednisone (1-1.5 mg/kg/day orally) during 4 - 6 weeks, then taper in 1 year
(Class 4).
II. If relapse repeat treatment or combine first treatment with immunosuppressive drug
(azathioprine, methotrexate) (Class 4). Side-effect are an important determinant in considering whether maintenance therapy with prednisolone can be prescribed.
III. If treatment with prednisolone fails another treatment needs to be initiated or added.
From other immunosuppressive drugs there is little evidence for a beneficial effect, while considerable side-effects are likely. There is some experience with methotrexate (up to 25 mg/week orally) and azathioprine (up to 3 mg/kg/day). IVIG can have a beneficial but short-lasting effect in some patients with dermatomyositis.
Dosages:
Prednisolone: use treatment protocol 1, but start with 1 - 1.5 mg/kg/day from week 1 - 6 in
1 - 3 doses orally, then follow protocol.
Azathioprine: 2 mg/kg/day, up to 3 mg/kg day in 3 doses orally. Start at 1 mg/kg/day
(Class IV).
Methotrexate: up to 30 mg/week. Start with 7.5 mg/week; increase dose every 6 weeks with 2.5 mg if necessary. Supplement folic acid 24 hours after dose of methotrexate (5 mg). Class IV.
Cyclofosfamide: 2 mg/kg/day orally with prednisolone orally or intravenously at a dose of
0.5 - 1 g per m2 in 150 ml NaCl 0.9% in 60 minutes, 6 times with an interval of 4 weeks.
IVIG: 0.4 mg/kg/day for 5 consecutive days. Maintain diuresis. Class III.
NB: in dermatomyositis the affected skin needs to be protected against sunlight. Treatment with hydroxychloroquine is the initial treatment for amyopathic DM. The treatment of severe amyopathic DM is similar to DM.
PM: if no response to treatment with prednisolone reconsider the diagnosis
Literature
Richtlijn Dermatomyositis, polymyositis en sporadische ‘inclusion body’-myositis. Nederlandse
Vereniging voor Neurologie en ISNO. Van Zuiden Communications B.V. Alphen aan den Rijn,
2005.
Dalakas MC, Illa I, Dambrosia JM, Soueidan SA, Stein DP, Otero C, et al. A controlled trial of high-dose intravenous immune globulin infusion as treatment for dermatomyositis. N Engl J Med
1993;329:1993-2000.
De Visser M, Van de Vlekkert Hoogendijk JE,, De Haan RH, Algra A, Van der Tweel I, Van der Pol
WL, Uijtendaal EV. Oral dexamethasone pulse therapy versus daily prednisolone in subacute inflammatory myopathies: A randomised clinical trial. Neuromusc Disord 2008;18:833
(Proceedings to WMS congres, Newcastle 2008).
Drake LA, Dinehart SM, Farmer ER, Goltz RW, Graham GF, Hordinsky MK, et al. Guidelines of care for dermatomyositis. J Am Acad Dermatol 1996;34:824-9.
Kasteler JS, Callen JP. Low-dose methotrexate administered weekly is an effective corticosteroidsparing agent for the treatment of the cutaneous manifestations of dermatomyositis. J Am Acad
Dermatol 1997;36:67-71.
Miller FW, Leitman SF, Cronin ME, Hicks JE, Leff RL, Wesley R, et al. Controlled trial of plasma exchange and leukapheresis in polymyositis and dermatomyositis. N Engl J Med 1992;326:1380-4.
Vencovsky J, Jarosova K, Machacek S, Studynkova J, Kafkova J, Bartunkova J, et al. Ciclosporine
A versus methotrexate in the treatment of polymyositis and dermatomyositis. Scand J Rheumatol
2000;29:95-102.
Villalba L, Hicks JE, Adams EM, Sherman JB, Gourley MF, Leff RL, et al. Treatment of refractory myositis: a randomised crossover study of two new cytotoxic regimens. Arthritis Rheum
1998;41:392-9.
Guillain-Barre syndrome
IVIG 0.4 mg/kg/dag during 5 days can be considered (Class I). Plasmapheresis can be considered as an alternative; similar efficacy but less practical (Class I).
Literature
Richard ACH, Swan AV, van Koningsveld R, van Doorn PA. Corticosteroids for Guillain- Barré syndrome. Cochrane Database of Systematic Reviews, Issue 2, 2009
Raphaël JC, Chevret S, Hughes RAC, Annane D. Plasma exchange for Guillain-Barré syndrome.
Cochrane Database of Systematic Revieuws, Issue 2, 2009
Geisoleerde cerebrale vasculitis
Methylprednisolone iv (treatment protocol 2), then maintenance therapy with treatment protocol 1 (start in month 10), add cyclofosfamide. After 3 - 6 months replace cyclofosfamide with azathioprine, MTX, or mycophenolate mofetil.
Expert opinion only.
Literature
Central nervous system vasculitis. Hajj-Ali R and Calabrese LH. Curr opin Rheumatol 21: 10-18.
Primary angiitis of the central nervous system. Molloy ES, Hajj-Ali RA. Curr Treat options neurol
2007; 9 (3): 169-75.
Horton’s neuralgia (cluster headache)
Prednisolone 60 mg/day, during 15 days.
Literature
Rozen TD. Trigeminal autonomic cephalalgias. Neurol Clin 2009; 27(2): 537-56.
Multifocal Motor Neuropathy
I. IVIG 2 g/kg in 2 or 5 days (induction; Class I), then maintenance dose titrated to individual respose (Class IV).
Alternative: subcutaneous IVIG (convert 1:1 from iv dose, sometimes a higher dose is necessary).
II. If no response, try cyclofosfamide, cyclosporine, azathioprine or rituximab (Class
IV). Cyclofosfamide is less preferable due to toxicity.
Literature van Schaik IN, Bouche P, Illa I, Leger JM, Van den Bergh P, Cornblath DR, Evers EM, Hadden
RD, Hughes RA, Koski CL, Nobile-Orazio E, Pollard J, Sommer C, van Doorn PA. European
Federation of Neurological Societies/Peripheral Nerve Society guideline on management of multifocal motor neuropathy. Report of a joint task force of the European Federation of
Neurological Societies and the Peripheral Nerve Society. Eur J Neurol. 2006;13:802-8.Elovaara I,
Apostolski P, van Doorn P, Gilhus NE, Hietaharju A, Honkaniemi J, van Schaik IN, Scolding N,
Soelberg Sørensen N, Udd B. The EFNS task force on the use of intravenous immunoglobulin in
treatment of neurological diseases. EFNS guidelines for the use of intravenous immunoglobulin in treatment of neurological diseases. Eur J Neurol 2008;15:893-908.
Multiple Sclerosis
See appropriate protocol.
Myathenia gravis and Lambert-Eaton myasthenic syndrome
See appropriate protocol.
Polymyalgia rheumatica
I. Prednisolone 20 mg/day orally. When symptoms are controlled and ESR is normalizing, reduce dose as in treatment protocol 1. If recurrence, double dose (or return to initial dose if necessary).
II. If no clinical response increase dose to 30 mg/day orally, reduce dose as described in I.
PM: reconsider diagnosis if no response to treatment.
Literature
C Salvarani, F Cantini, GG Hunder. Polymyalgia rheumatica and giant-cell arteritis. Lancet 2008:
372: 234-45.
Sarcoidose
I. Prednisolone 1 mg/kg/day orally (up to 80 mg/day) during 6 - 8 weeks; reduce as in treatment protocol 1. Consider initiating treatment with methylprednisone 1000 mg per day intravenously for 3 days.
II. If clinical deterioration during dose reduction of prednisolone , double the dose and quickly decrease dose (in < 2 months) to the lowest effective dose of prednisolone and consider addition of MTX or azathioprine.
III. If clinical deterioration after treatment : re-introduce prednisolone depending on previous response and tolerance with for instance 0.5 mg/kg/day. Maintenance dose of 5 to 15 mg/day during 1 year. Aim for the lowest possible maintenance dose of prednisolone.
Systemic vasculitis (PAN; vasculitis not otherwise classified)
Prednisolone as outlined in treatment protocol 1 with cyclofosfamide 2 mg/kg/day orally during 3 month as induction therapie. Maintenance treatment is azathioprine 2 mg/kg/day during at least 1 year after reaching remission.
NB: if PAN associated with hepatitis B or C, consult rheumatologist.
Literature
Burns TM, Schaublin GA, Dyck PJB. Vasculitic neuropathies. Neurol Clin 2007; 25: 89 – 113.
Systemic lupus eryhtematosus with neurologic and/or neuropsychiatric symptoms
I. Methylprednisolone 1g/day during 3 days, continue with prednisolone 1 mg/kg day from day 4 for 3 months.
AND cyclofosfamide 0.75 g/m2/month intravenously during 1 year, then 0.75 g/m2 every
3 months for 1 year.
(Class I)
II. methylprednisolone (treatment protocol 2).
Literature
Barile-Fabris L, Aziza-Andraca R, Olguin-Ortega L, et al. Controlled clinical trial of IV cyclophosphamide versus IV methylprednisolone in severe neurological manifestations in SLE. Ann
Rheum Dis 2005; 64: 620-625.
Trevisani VFM, Castro AA, Fereira Neves Neto JJFNN, et al. Cyclophosphamide versus methylprednisolone for treating neuropsychiatric involvement in SLE. Cochrane Database of
Systematic Reviews 2006(2), art no CD002265.
Takayashu’s arteriitis
I. Prednisolone 1 mg/kg/day orally (with a maximum of 100 mg/day), consider dosing twice a day. If clinical response switch to once daily dosing regimen and after 2 to 3 months start an alternating regimen: 1 mg/kg/day and 0 mg/kg/day the next day.
Then reduce dose as detailed in treatment protocol 1. If recurrence of symptoms return to starting dose and taper of more time.
II. If disease recurrence from the beginning or after slowly tapering the prednisolone dose add MTX (10 mg/week orally, up to 30 mg/week), or cyclofosfamide orally ( 2 mg/kg/day, during a maximum of 3 months). There are case studies in which patients with no clinical response to the outlined treatment received TNF-alpha blockers (infliximab) with some success.
Appendices
Treatment protocol 1: prednisolone
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
5
5
4
10
7,5
7,5
20
15
15
10
4
3
3
2
2
Start with 1 mg/kg/dag orally (rounded off to nearest 10-fold)
Max: 100 mg/day
MAAND DOSIS (MG/DAG)
1
2
3
100
90
80
4
5
6
7
8
9
10
70
60
50
40
30
25
20
26
27
1
1
28 0
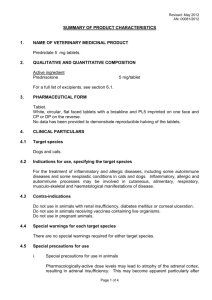
Treatment protocol 2: methylprednisolone pulse
Methylprednisolon i.v. 1 gram:
Week
1
3
7
Day
1,2,3
15,16,17
43,44,45
Start prednisolone orally concurrently at day 1:
Week week 1 - 23 week 24 - 28 week 29 - 52
Dose
20 mg once daily
15 mg once daily week 53 - >
10 mg once daily taper slowly
Treatment protocol 3: prednsilone/cyclofosfamide iv
Week 1-4 prednisolone 1 mg/kg/day cyclofosfamide 750 mg/m2 iv (once)
Week 5-8 prednisolone 0.75 mg/kg/day cyclofosfamide 750 mg/m2 iv (once)
Week 9-12 prednisolone 0.50 mg/kg/day cyclofosfamide 750 mg/m2 iv (once)
Week 13-20 reduce prednisolone with 5 mg every 4 weeks cyclofosfamide 750 mg/m2 iv (once)
Week 21-104 reduce prednisolone with 5 mg every 4 weeks to 10 mg once daily cyclofosfamide 750 mg/m2 once every 3 months iv
Week 105 - 208 prednisolone 10 mg per day
Week 108 - 208 azathioprine 2 mg/kg/day
To summarize: cyclofosfamide iv on month 1, 2, 3, 4, 5, 6, 9, 12, 15, 18, 21.
Azathioprinen (Imuran)
Important contra-indications:
increased transaminases indicative of liver disease
anaemia, leukopenia, thrombopenia (other than the result of auto-immune disease)
relative contra-indication: (planned) pregnancy
Important interactions
allopurinol: reduce azathioprine to 0.25 of regular dose
trimethoprim: the combination can induce bone marrow suppression
Important side effects
gastro-intestinal, increased liver transaminases, leuko- and thrombopenia
rarely: anemia, pancytopenia, pancreatitis, hepatic veno-occlusive disease, allergic reaction, interstitial pneumonitis
Instructions for patients (tablet 25 or 50 mg)
provide folder with information
starting dose 50 mg once daily, if no side-effects increase to 50 mg twice daily, then increase to 2 mg/kg/day (in some cases up to 2.5 mg/kg/day).
Laboratory follow-up
Hb, leukocytes and differentiation, thrombocytes, transaminases after 1 week, and every 2 weeks for the first 8 weeks. Then reduce frequency.
If laboratory follow-up is abnormal, adjust dose:
0.5 dose if leukocytes < 3 x 10^9/L, granulocytes < 1 x 10^9/L, thrombocytes < 100 x
10^9/L
stop if leukocytes < 2 x 10^9/L, granulocytes < 0.5 x 10^9/L, thrombocytes < 50 x 10^9/L, transaminases > 3 times the upper limit of normal.
Ciclosporine
Important contra-indications
hypertension
impaired renal function
malignancy
(planned) pregnancy
Important interactions
NSAID, grapefruit, ketoconazol, erythromycin, doxycyclin, oral anticonception, propafon, verapamil and diltiazem increase plasma levels (by inhibition of CYP450).
Saint John’s wort, carbamazepin, phenytoin, metamizole, rifampicin, nafcillin, iv sulfadimidine and trimethoprim reduce plasma levels (induction of CYP450).
combination with colchicin and lovastatin increase risk of muscle toxicity.
Important side effects
nephrotoxicity (30%), reversible if timely dose adjustment.
gout
hirsutism (25%), hypertension (15%), gingival hyperplasia (8%)
increase of transaminases, gastro-intestinal complaints, pruritus, fatigue
less common: tremor, paresthesia, headache, hyperkalemia, pancreatitis
Start treatment (capsules 25 and 100 mg)
lab check-up: lipid spectrum, creatinin (2 x)
provide folder
starting dose: 2.5 mg/kg/day orally in a twice daily regimen. If inadequate response after
6 weeks increase every 4 weeks with 25% up to 5 mg/kg/day.
If after 3 months inadequate response stop or add MTX
If remission taper dose after 3 months by reducing with 0.5 mg/kg/day every 2 months
Follow-up
for the initial 3 months every 2 weeks: blood pressure, creatinin, potassium, then reduce frequency.
if > 30% increase in creatinin, reduce dose bij 50%.
if no normalisation of creatinin stop
after 1 month of treatment lipid spectrum and transaminases
if suspected side-effects, inadequate response or possible non-compliance, do plasma levels 12 hours after last dose.
NSAIDs
General principles:
if possible, use only acetaminophen for pain. If inadeqate, add NSAID in lowest possible dose
preferably no NSAID if renal impairment
preferably not in case of pregnancy
proton pump inhibitor to prevent gastric ulcer can be considered, if no prophylaxis aim for lowest effective dose
NSAIDs in case of impaired renal function
preferably no NSAID
if slightly decreased renal function and no other options, start sulindac (Clinoril) 200 mg twice daily. Follow-up renal function!
Ulcer prophylaxis
Reasons to start prophylaxis
age > 65 years
previous ulcer
Consider prophylaxis
age 60 - 65 years
use of acetylsalicic acid or coumarines
sever rheumatoid arhtritis
cardiac failure, diabetes mellitus or other severe co-morbid conditions
high dose of NSAID
steroids
SSRI
Treatment protocol for IVIG
Precautions
Vaccinations with live virus needs to be postponed until at least 3 month after the last treatment. Beware of fluid overload in cardia failure.
Before initiating treatment
IgA level (once), renal function.
Interactions
Immuneresponse to several vaccinations (measles, mumps, rubella) can be reduced.
Important side-effects
Headache, back pain, nausea, eczema, erythema multiforme, general malaise and fever,
(temporary) increase in plasma creatinin, acute renal failure in cryoglobinaemia, anaphylaxis, Coombs-positive hemolytic anemia, leukpenia, increased blood viscosity with thrombo-embolic complications, aseptic meningitis.
Contra-indications
IgA deficiency (relative), severe side effects after previous administration of blood products.
Prednisolone (pulse)
Precautions
None
Follow-up
Glucose, electrolytes and blood pressure during administration.
Interactions
Increase in dose insulin or oral diabetics often necessary during treatmen, avoid combination with platelet aggregation inhibitors during treatment (especially if also hypoprothrombinemia).
Important side effects
Rapid administration of high-dose intravenous prednisolone (>0.5 g in less than 10 min) has been reported to cause cardiac arrhythmia, circulatory collapse and cardiac arrest.
Contra-indications
Decribed elsewhere (prednisolon maintenance).
Prednisolone (maintenance)
Precautions
Beware of Addisonian crisis in stress situations during tapering or after discontinuation.
Consult endocrinologist if necessary. Discontinuation after long term treatment can cause withdrawal syndrome (fever, myalgia, arthralgia and malaise). The medication should always be tapered (see treatment protocols). Consider ranitidin to prevent gastric ulcers.
Reduce dose if also hypothyroidism and cirrhosis. Beware: corticosteroids mask infection and weaken the immune system.
Follow-up
Measure glucose, elektrolytes and blood pressure frequently after starting treatment, then less frequently if normal. Beware decrease in potassium if co-administration with diuretics.
Interactions
Effect is reduced when combined with phenytoine, barbiturates, efedine, rifampicine. Avoid combination with salicic acid. Dose adjustment of anti-diabetic medication will be necessary. Vaccination might be ineffective.
Important side effects:
Fluid balance and elektrolytes : sodium and fluid retention, hypertension, hear failure, hypokalemia, alkalosis, increase calcumexcretion.
Musculoskeletal : muscle wasting and weakness, myopathy, osteroporosis, fractures, aseptic necrosis of the head of femur and humerus, tendon ruptures
Digestive tract : ulcer, perforation, pancreatitis, esophagitis, nausea, increased appetite
Skin : impaired healing, skin atrophy, ecchymosis, petechiae, erythema, sweating, burning sensation, dermatitis, urticaria, angi-edema.
Neurological : seizures, increased intracranial pressure, vertigo, headache.
Endocrine : menstrual disturbance, Cushing, growth retardation, adrenal suppression, impaired glucose tolerance, diabetes mellitus.
Eye : cataract, glaucoma, exophthalmus, eye infections by viruses or fungus.
Metabolism : catabolic state
Psychiatric : depression, psychosis.
Hypersensitivity reactions : thrombo-embolic complications, weight gain, malaise, dependency (psychological and physiological).
Contra-indications infections, active TBC. Relative: latent TBC, hypertension, osteoporosis, renal failure, diabetes mellitus, ulcer, aspecific ulcerative colitis, perforation of gastro-intestinal tract, abces, diverticulitis, recent anastomosis of the bowel, previous medical history with psychiatric disease, pregnancy.
MTX
Start methotrexate
check contra-indications: relative: pulmonary problems (because of the risk of interstitial pneumonitis). absolute: creatinin clearance < 40 ml/min, hepatitis, cirrhosis, anemia, leukopenia, thrombopenia, (planned) pregnancy
interactions: trimethoprim, ketoprofen should not be co-administered. Beware of combination with MTX, NSAID, diuretics.
Chest X-ray (if not already present)
Provide information folder and discuss the need for contraception; do not co-administer trimethoprim; alcohol max 1 - 2 units per day; no vaccination with “live attenuated virus”
Dosing tablets 2.5 and 10 mg. Start at 7.5 to 15 mg, if necessary increase every 2 - 4 weeks, up to 25 mg/week.
If creatinin clearance < 40 - 70 ml/min decrease dose bij 50%
Add folic acid 5 mg once every week at least 24 hours after last MTX dose
Consider MTX subcutaneous if gastro-intestinal side-effects or incomplete response
Follow-up
The first 6 weeks laboratory check-up every 2 weeks, dan less frequently and eventually once every 4 months. Request the following tests: Hb, leukocytes, thrombocytes, creatinin, ASAT, ALAT, AF. For ASAT and ALAT up to 3 times the upper limit of normal is acceptable.
In case of surgical procedure do not discontinue MTX
no live attenuated vaccines, other vaccines acceptable.
Common side-effects
gastro-intestinal disturbances, stomatitis, nodulosis, CNS effects, cytopenia
rarely: pneumonitis, cirrhosis, nephritis, MTX-osteopathy
Thalidomide
Important contra-indications
(planned) pregnancy, lactation
peripheral neuropathy
use with caution if liver failure, cardiovascular disease, constipation, epilepsy
NB: beware of co-medication that interferes with oral contraceptives.
Important side-effects
sensory axonal polyneuropathy (15-40%; dose-dependent) , can be irreversible, causes painful paresthesias in feet and hands with hypesthesia in glove- and stocking distribution, proximal muscle weakness, and hyporeflexia.
sleepiness (38%), headache (13%), fever (20%), rash (21%), diarrhea (15%), nausea
(13%), lymfadenopathy (9%), oral candida (8%), bradycardia, orthostasis.
leukopenia (20%), anemia (9%), increased transminases (8%).
Important interactions
Possibly increased probability of serious infections when combines with Anakinra.
Follow-up
leukocytes and differentiation, Hb, thrombocytes, ASAT, pregnancy test (when pregnancy suspected).
History and physical examination for signs of peripheral neuropathy every month. EMG
(SNAP n. suralis, n. medianus, and n. ulnaris according to protocol) every 6 months.
Prescribing (capsules 50 mg)
discuss possible alternatives with colleagues
discuss side-effects and possible teratogenic effects with patient. Discuss adequate anticonception. Avoid during lactation.
before starting medication EMG according to protocol (twice; interval of 2 weeks).
if m. Behcet 100 - 400 mg after evening meal.
stop treatment if:
paraesthesia
SNAP > 40% reduced from baseline at follow-up
neutrophil count < 0.75 x 10^9/L
NB: continue anticonception at least 4 weeks after discontinuing medication.
Cyclofosfamide (oral and intravenously)
Prescribing
Contra-indications: active infection, bone marrow depression, serious bladder disorders, urethral obstruction
Interactions: more bone marrow toxicity if combined with allopurinol or thiazide diuretics.
Precautions:
aim for diuresis of > 3 L/24 h because of toxic effect of metabolites on bladder. If oral administration, take tablets in the morning and void bladder before sleep in the evening.
if Wegener granulomatosis, start PCP prophylaxis.
after initiating treatment lab check-up every 2 weeks: Hb, leukocytes and differentiation, thrombocytes, transaminases, creatinin, G-GT, AF. Bone marrow depression can occur 1
- 2 weeks after start of treatment.
if macroscopic hematuria beware of hemorrhagic cystitis, discontinue treatment. Consult urologist.
for effects on fertility: see below.
Gonadal toxicity and cryopreservation
Men
If expected cumulative dose of cyclofosfamide > 100 mg/kg:
referral to fertility lab for cryopreservation of spermatocytes
Women
Consider if expected dose of cyclofosfamide > 200 mg/kg:
adequate conctraception during treatment and until 3 months after treatment
consider cryopreservation of oocytes
Information for intravenous administration of cyclofosfamide
initial dose 750 mg/m2 body surface area (maximum dose 1500 mg in men and 1350 mg in women). Reduce to 500 mg/m2 body surface area if renal creatinin clearance is less than 40 ml/min or age over 70 years.
reduce subsequent infusion with 250 mg/m2 body surface area if leukocytes < 3 x
10^9/L or neutrophils < 1 x 10^9/L.
aim at a cumulative dose of cyclofosfamide of less than 20 g because of risk of malignancy
Information for oral administration of cyclofosfamide (tablet 50 mg)
2 mg/kg/day (max 200 mg/day in men, 150 mg/day in women). Reduce to 1.5 mg/kg/day if renal creatinin clearance is less than 50 ml/min, reduce to 1 mg/kg/day if renal creatinin clearance is < 15 ml/min. Use caution in patient older than 70 years.
stop treatment if leukocytes < 3 x 10^9 / L, neutrophils < 1 x 10^9/L, thrombocytes < 100 x 10^9 / L, or rapid decrease in any of these parameters. After normalisation (usually after 10 - 14 days) restart treatment but reduce dose with 25 mg/day.
Side-effects
common: nausea, vomiting, anorexia, diarrhea, constipation, stomatitis, reversible alopecia, pigmentation of skin and mucosa.
bone marrow depression (1 - 2 weeks after start of treatment).
hemorrhagic cystitis, secondary malignancies
if high cumulative dose risk of irreversible aspermia / oligospermia or irreversible amenorrhoea
Vaccinations
No live attenuated vaccines until 3 months after discontinuation of treatment.