A Minute for the Medical Staff
advertisement

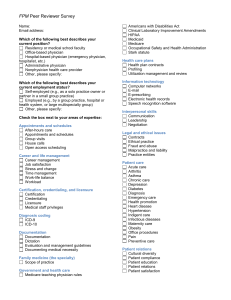
A Minute for the Medical Staff A supplement to medical records briefing August 1999 Emergency! ER codes misused and abused Simple rules for staying out of trouble “I would say that a high percentage of non-ER doctors coding in the emergency room are coding incorrectly’” says Diane Jepsky, RN, MHA, a president and CEO of Jepsky Health Care Consultants in Issaquah, WAS and a former emergency room nurse. The misuse of ER evaluation and management (E/M) codes also occurs outside the emergency room, Jepsky notes—a particularly troubling situation. According to coding rules, Jepsky points out, ER codes “should only be used in true hospital-based emergency facilities that are open 24 hours a day and deliver unscheduled episodic care to patients who present for immediate medical attention.” How ER coding mistakes happen According to Jepsky, problems in ER coding arise when private physicians see their patients in the emergency room instead of their offices. Any physician can use ER codes—as long as the service he or she is providing is part of a true emergency. “You can’t use ER codes when seeing a patient in the ER as a matter of convenience,” Jepsky says. For example, “Billy’s mom calls and says that Billy has a sore throat. The physician decides to meet Billy and his mom in the ER to check out the problem as it is more convenient for the patient and the physician. In this case, the physician should use outpatient codes (99211-99215), assuming the patient is established,” Jepsky explains. Another scenario that leads to inappropriate use of ER codes occurs when the ER physician calls in a specialist for a consultation. For example, the ER physician asks for a surgical consult for a patient with abdominal pain. If this patient is ruled out as a surgical candidate and the ER physician discharges the patient to home, the surgeon should use the outpatient consultation codes (9924199245), Jepsky says. But if the patient with abdominal pain becomes a surgical patient and is admitted to the hospital, a transfer of care has taken place. In that case, Jepsky says, the surgeon should code the appropriate admission code (99221-99223). The consultative work done in the ER is rolled into the admission and the consult codes should not be used in addition to the admit codes. Jepsky points out that there are times when the ER physician and the private medical doctor will both use the ER codes. For example, the ER physician may see the patient first and then call in the private physician and transfer care over to her or him. If the private physician elects not to admit the patient, and discharges the patient to home, then the physician may also use an ER code. “Just remember that even though the providers are different, two ER codes hitting an adjudication system with the same date of service may cause the bill to suspend, deny, or pay on the first bill submitted, which may not be the appropriate bill, “ Jepsky says. Problems outside the ER “One of the bigger problems I see is doctors using ER codes when they see patients emergently in their office,” Jepsky says. In such cases, physicians should use outpatient codes plus the add-on code 99058, which indicates that the patient was seen emergently. Walk-in/urgent care centers are also susceptible to these coding errors. While care provided in these centers may be urgent, walk-in centers do not meet the definition of emergency departments. Outpatient codes (99201-99215) should be used. Understanding correct ER coding That said, here are some basic rules and tips for correct sue of ER codes in reporting E/M services: Know the codes. The following codes are used to report E/M services provided in the emergency department: 99281-99285. The place of service (POS) code for the emergency department is 23. If codes 99281-99285 are used with a POS code other and 23—indicating that the services were provided in a setting other than an emergency room—then the codes are incorrect. Check your charge tickets. Outpatient facilities such as physician offices and outpatient facilities should remove ER codes (99281-99285) from their charge tickets. If the physician sees a patient in the ER and the situation meets the requirements for using the ER codes, the physician can write the code in on the charge ticket. Educate the physicians. Makle sure hospital physicians know the rules. Inform them that unless they’re seeing a patient in the ER truly for an emergency, they should use outpatient or consultation codes. Audit the coders. Many hospitals use outside coding companies in the emergency departments. Jepsky notes that coding companies today often undercode because they don’t grasp the total clinical picture of the ER patient and they fear compliance issues. “A lot of them fear the higher code levels and dampen out the profile in the ER,” Jepsky says. “They code too conservatively and lose revenue for the ER.” She recommends auditing ER coding at least once a year. Put well-trained coders in charge. ER coding is complicated because there are more procedures done in the ER than in other departments, Jepsky notes. Coders assigned to the ER should have a more sophisticated understanding of coding and medical terminology. “It’s important to have someone who is oriented to what’s going on in the ER and has a good rapport with the ER physicians,” Jepsky says. E/M documentation tips Lynne Northcutt-Greager, CPC, of the MGMA Health Care Consulting Group in Englewood, CO, says that a common problem with physician documentation is confusing the review of systems (ROS) with the physical exam or the history of present illness. “They physicians that I find who are most successful with documentation are breaking up the different sections—chief complaint, history of present illness, (ROS), and past family and social history—in their progress notes,” she says. “It seems to help them channel their thinking.” And if your practice’s physicians depend on forms or checklists to assist with gathering information, Northcutt-Greager warns that you need to clearly note the date of service on the forms. “Checksheets need to have the patient’s name on it, and should have the date on it,” she says. And the major elements to accomplish this task include writing about the disease processes that are getting better but are not yet good enough for discharge and writing about the ones that have developed since hospitalization and need further work. Utilization reviewers have tools such as “intensity of service” and “severity of illness” criteria that can help. A Minute for the Medical Staff is an exclusive service for subscribers to Medical Records Briefing. Reproduction of A Minute for the Medical Staff within the subscriber’s institution is encouraged. Reproduction of any form outside the subscriber’s institution is forbidden without prior written permission.