Respiratory adaptations in response to exercise , high altitude and
advertisement
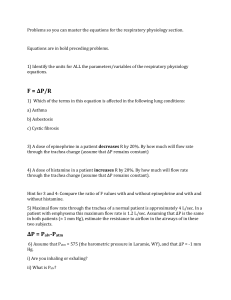
Respiratory adaptations in response to exercise , high altitude and deep sea diving Learning objectives At the end of lecture , the student should be able to: 1. Understand the respiratory responses in relation to exercise 2. Changes occurring in the muscles during exercise 3. The response of Oxygen hemoglobin dissociation curve during exercise 4. Oxygen debt and its importance 5. How does the respiratory system adapt to high altitude pressures 6. Changes occurring in the body at high altitudes 7. Acclimitization and its importance 8. Under water diving and changes in the body 9. Decompression sickness and its consequences Lecture outline Response of respiratory system to Exercise The respiratory and cardiovascular systems make adjustments in response to both intensity and duration of exercise The response of respiratory system to exercise is remarkable As the body’s demand for O2 increases more O2 is supplied by increasing the ventilation rate. Excellent matching occurs b/w O2 consumption, CO2 production and the ventilation rate Respiratory adaptations ► Increased lung ventilation ► Increased oxygen uptake ► Increased anaerobic or lactate threshold INCREASED LUNG VENTILATION Aerobic training results in a more efficient and improved lung ventilation. At REST and during SUB MAX. work ventilation may be decreased due to improved oxygen extraction (pulmonary diffusion), however during MAX. work ventilation is increased because of increased tidal volume and respiratory frequency. INCREASED MAXIMUM OXYGEN UPTAKE (VO2 MAX) VO2 max is improved as a result of aerobic training – it can be improved between 5 to 30 %. Improvements are a result of: - Increases in cardiac output - red blood cell numbers - a-VO2 difference - Muscle capillarisation - Greater oxygen extraction by muscles INCREASED ANAEROBIC OR LACTATE THRESHOLD Lactate Threshold As stages continue to increase, a point is reached at which blood lactate concentration suddenly increases Lower work rates, lactate metabolized as fast as it is produced Lactate threshold changes as a result of endurance training As a result of improved O2 delivery & utilization , a higher lactate threshold (the point where O2 supply cannot keep up with O2 demand) is developed. Changes in the Muscle tissue The following tissue changes occur: ► Increased O2 utilization ► increased size and number of mitochondria ► Increased myoglobin stores ► Increased muscular fuel stores ► Increased oxidation of glucose and fats ► Decreased utilization of the anaerobic glycolysis (LA) system ► Muscle fiber type adaptations Exercise and rate of diffusion Pulmonary diffusion humans : 4-5 fold increase in pulmonary blood flow; expanding capillary blood volume 3 times Tissue diffusion O2 and CO2 diffuse down the pressure gradient PO2 returning from muscle tissue following heavy exercise, only 16mm Hg increased driving pressure of O2 from arterial blood into muscle tissues with high aerobic needs are more vascularized greater surface area for exchange Arterial PO2 & PCO2 during exercise ► Remarkably, mean values for arterial PO2 & PCO2 do not change during exercise. ► An increased ventilation rate and increased efficiency of gas exchange ensure that there is neither a decrease in arterial PO2 nor an increase in arterial PCO2. ► The total amount of O2 entering the blood increases from 250ml/min at rest to about 4000ml/min. ► The PO2 of blood entering the lungs is reduced which increases the pressure difference b/w blood and alveolar PO2 leading to increased O2 diffusion into the blood from alveoli. Changes during Exercise ► Blood flow/min is increased from 5L/min to about 25-30L/min. ► The total amount of O2 entering the lungs increases from 250ml/min at rest to about 4000ml/min. ► Similarly CO2 removal increases from 200ml/min to about 8000ml/min. Oxygen diffusion at rest and exercise Oxygen Diffusion at rest Air--> alveoli-->arteriolar blood--> cells (159) (100) (100) (40) Oxygen Diffusion during exercise Air--> alveoli-->arteriolar blood--> cells (159) (100) (100) (20) CO2 diffusion at rest and exercise CO2 Diffusion during rest Air<-- alveoli <--venous blood <-- cells (.3) (40) (46) (46) CO2 Diffusion during exercise Air<-- alveoli <--venous blood <-- cells (.3) (40) (55) (55) O2 – Hb dissociation curve During exercise the O2 – Hb dissociation curve shifts to the right. This right shift is due to multiple reasons including : ► Increased tissue PCO2 ►Decreased tissue pH ►Increased temperature ►Increased 2,3- BPG Oxygen debt The oxygen dept is the amount of air that is consumed after the exercise is over until a constant, basal condition is reached. The trained athletes can increase the O2 consumption to a greater extent than untrained person. So O2 dept in athletes is less. Adaptation to high altitude ►The respiratory responses to high altitude are the adaptive adjustments a person must make to the decreased PO2 in inspired and alveolar air. ►At high altitude the decrease in PO2 is due to: ►At sea level, the barometric pressure is 760mmHg. ►At 18,000 feet above sea level, the barometric pressure is one half that value or 380 mmHg ►To calculate the PO2 of humidified inspired air at 18000 feet above sea level, correct the barometric pressure of dry air by the water vapor pressure of 47 mmHg, then multiply by the fractional concentration of O2, which is 21%. Thus ,at 18,000 feet, PO2 =70mmHg (360 – 47mmHg) x 0.21 = 70 mmHg The pressure at the peak of Mount Everest yields a PO2 of inspired air of only 47 mmHg. Pressures at high Altitude Altitude sea level 10,000ft 20,000ft Pb 760 523 349 PO2 159 110 73 Alveolar PO2 104 67 40 ►Despite severe reductions in the PO2 of both inspired and alveolar air, it is possible to live at high altitude ,if the following adaptive responses occur: ►Hyperventilation : the most significant response to high altitude is hyperventilation (increase in ventilation rate). ►For example if the alveolar PO2 is 70mmHg, then the arterial blood which is almost perfectly equilibrated, also will have a PO2 of 70 mmHg , which will not stimulate peripheral chemoreceptor. ►However, if alveolar PO2 is 60mmHg then arterial blood will have a PO2 of 60 mmHg, in which the hypoxemia is severe enough to stimulate peripheral chemoreceptors in the carotid and aortic bodies. ►In turn, the chemoreceptors instruct the medullary inspiratory center to increase the breathing rate. ►A consequence of hyperventilation is that extra CO2 is expired by the lungs and arterial PCO2 decreases, producing respiratory alkalosis ►However, the decrease in PCO2 and resulting increase in pH will inhibit central and peripheral chemoreceptors and offset the increase in ventilation rate ►These offsetting effects of CO2 and pH occur initially, but within several days HCO3- excretion increases. ►HCO3- leaves the CSF, and the pH of CSF decreases toward normal ►Thus, within a few days, the offsetting effects are reduced and hyperventilation resumes. ►The respiratory alkalosis that occurs as a result of ascent to high altitude can be treated with carbonic anhydrates inhibitors (acetazolamide). ►These drugs increase HCO3- excretion, creating a mild compensatory metabolic acidosis. Other changes in response to Adaptation to high altitude Polycythemia: ascent to high altitude produce an increase in red cell conc. and as a consequence increase in in Hb conc. The increase in Hb conc. In turn increase the O2 carrying capacity, which increases the total O2 content of blood in spite of arterial PO2 being decreased. O2- hemoglobin dissociation curve ►The most interesting feature of body adaptation to high altitude is an increase synthesis of 2,3- DPG by red blood cells. ►This increase 2,3- DPG causes shift of O2-Hb curve to the right. ►This right shift is advantageous to the tissues, b/c it is associated with increased P50, decreased affinity, and increased unloading of O2 to the tissues. ►This right shift is disadvantageous in the lungs b/c it becomes more difficult to load the pulmonary capillary blood with O2. Pulmonary vasoconstriction: At high altitude ,alveolar gas has a low PO2, which has a direct vasoconstriction effect on pulmonary vasculature (hypoxic vasoconstriction). Changes in cell in response to adaptation to high altitude Compensatory changes also occur in the tissues: The mitochondria (site of oxidative reactions) increase in number and myoglobin increases which facilitates the movement of O2 in the tissues. The tissue content of cytochrome oxidase also increases. Acclimatization ►If a person remains on high altitude for a week, month or year then he becomes more acclimatized and the effects of hypoxia are faded, this is called acclimatization ►Acclimatization to altitude is due to the operation of a variety of compensatory mechanism. ►The respiratory alkalosis produced by the hyperventilation shift the O2- Hb dissociation curve to the left, but a concomitant increase in red cell ,2,3DPG tends to decrease the O2 affinity of Hb. The net effect is a small increase in P50. ► ►The decrease in O2 affinity makes more O2 available to the tissue ►However ,the value of the increase in P50 is limited b/c when the arterial PO2 is markedly reduced, the decrease O2 affinity also interferes with O2 uptake by Hb in the lungs. ►The initial ventilatory response to increase altitude is relatively small, b/c alkalosis tends to counteract the stimulating effect of hypoxia ►However ventilation slowly increases over next 4 days b/c the active transport of H+ into CSF, causes a fall in CSF pH that increases the response to hypoxia. HYPERBARIC CONDITIONS - EXERCISING UNDERWATER ►Submersion in Water Exposure to hyperbaric conditions -volume decreases when pressure increases. ►More molecules of gas are forced into solution, with rapid ascent, they come out of solution and can form bubbles - emboli develop, block major vessels, extensive tissue damage. ►Resting HEART RATE DECREASES by 5 - 8 beats per minute (facilitation blood return to the heart) diving in cold water - greater bradycardia, higher incidence of arrhythmias ►During diving under water, the pressure increases by one atmosphere (760mmHg) for every 10 meters or 33 feet descent. ►The density of gas increases in depth leads to increase work of breathing. ►During diving due to high atmospheric pressure the air filled cavities are compressed as they failed to communicate with external air ►As the person ascends these air filled cavities over expand. ►The increased pressure (hyperbarism) do not affect the solid tissue or liquids of the body but only the gas filled cavities are affected. ►During diving at high pressure the nitrogen (which is poorly soluble in blood) enters into the body ►Nitrogen is relatively soluble in fats. ►During descent nitrogen diffuses slowly into the tissues. ►During ascend it slowly removed from the tissues b/c decompression occur due to decrease in pressure from deeper to upper levels in water. ►Decompression sickness can be avoided if the divers are trained to ascends slowly, which prevents increase in size of oxygen bubbles. ►The divers ascend in stages (at intervals) and spend some time at different depth to avoid nitrogen toxicity. Weightlessness in space Physiological consequences of prolonged periods in space are following: ►Decreased blood volume ►Decreased red cell mass ►Decreased muscle strength & work capacity ►Decreased maximum cardiac output ►Loss of calcium and phosphate from bones and loss of bone mass Physiological problems with Weightlessness: ►Motion sickness during the first few days of travel. ►Translocation of fluids in the body b/c of failure of gravity to cause hydrostatic pressure. ►Diminished physical activity b/c no strength of muscle contraction is required to oppose the force of gravity.