CarePlan Aperts Syndrome
advertisement
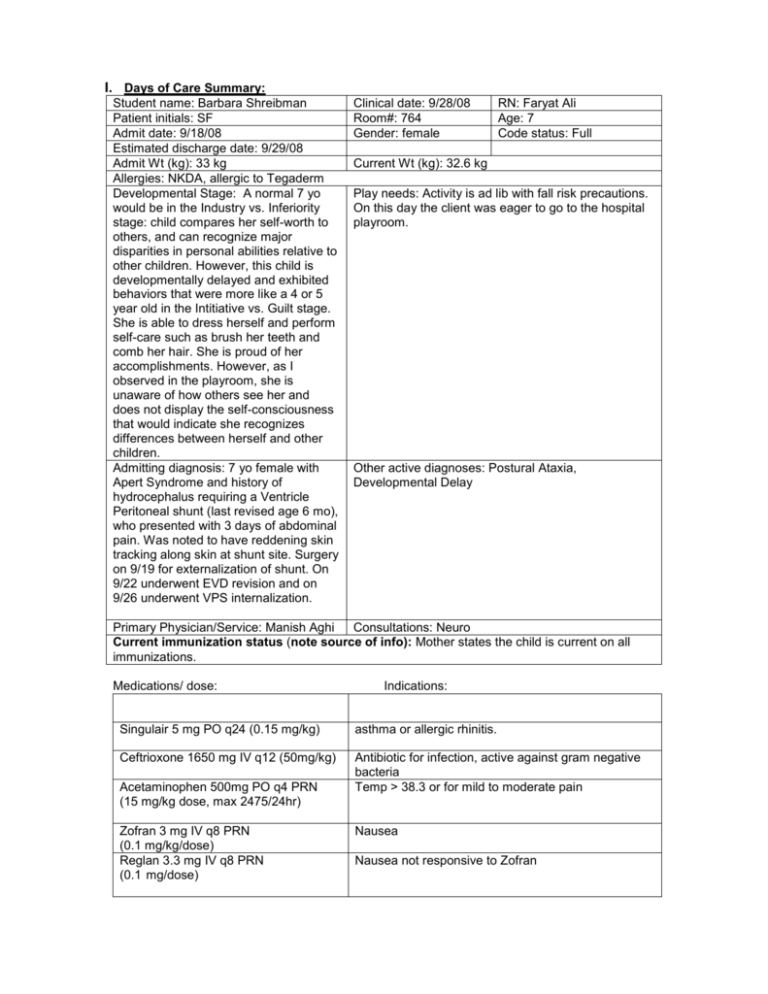
I. Days of Care Summary: Student name: Barbara Shreibman Patient initials: SF Admit date: 9/18/08 Estimated discharge date: 9/29/08 Admit Wt (kg): 33 kg Allergies: NKDA, allergic to Tegaderm Developmental Stage: A normal 7 yo would be in the Industry vs. Inferiority stage: child compares her self-worth to others, and can recognize major disparities in personal abilities relative to other children. However, this child is developmentally delayed and exhibited behaviors that were more like a 4 or 5 year old in the Intitiative vs. Guilt stage. She is able to dress herself and perform self-care such as brush her teeth and comb her hair. She is proud of her accomplishments. However, as I observed in the playroom, she is unaware of how others see her and does not display the self-consciousness that would indicate she recognizes differences between herself and other children. Admitting diagnosis: 7 yo female with Apert Syndrome and history of hydrocephalus requiring a Ventricle Peritoneal shunt (last revised age 6 mo), who presented with 3 days of abdominal pain. Was noted to have reddening skin tracking along skin at shunt site. Surgery on 9/19 for externalization of shunt. On 9/22 underwent EVD revision and on 9/26 underwent VPS internalization. Clinical date: 9/28/08 Room#: 764 Gender: female RN: Faryat Ali Age: 7 Code status: Full Current Wt (kg): 32.6 kg Play needs: Activity is ad lib with fall risk precautions. On this day the client was eager to go to the hospital playroom. Other active diagnoses: Postural Ataxia, Developmental Delay Primary Physician/Service: Manish Aghi Consultations: Neuro Current immunization status (note source of info): Mother states the child is current on all immunizations. Medications/ dose: Indications: Singulair 5 mg PO q24 (0.15 mg/kg) asthma or allergic rhinitis. Ceftrioxone 1650 mg IV q12 (50mg/kg) Antibiotic for infection, active against gram negative bacteria Temp > 38.3 or for mild to moderate pain Acetaminophen 500mg PO q4 PRN (15 mg/kg dose, max 2475/24hr) Zofran 3 mg IV q8 PRN (0.1 mg/kg/dose) Reglan 3.3 mg IV q8 PRN (0.1 mg/dose) Nausea Nausea not responsive to Zofran Miralax 17 g PO q24 PRN constipation (0.5 g/kg) Morphine 1-2 mg IV q3 PRN Severe pain (0.03-0.06 mg/kg) Brief pathophysiology summary of the primary and admitting diagnoses: The client’s primary diagnosis is Apert Syndrome and Ventricle Peritoneal shunt revision for infection. *Apert Syndrome is a condition involving distortions of the head and face and webbing of the hands and feet. It is a genetic disease in which the seams of the cranial bones close earlier than normal (craniosynostosis). It is caused by mutations in a gene called fibroblast growth factor receptor 2. My client showed characteristic abnormalities of the syndrome: her skull is short from back to front, wide on the sides, and overly tall. Her eyes are slightly side-spaced, bulging, and the eyelids tilt downward abnormally at the sides. My client’s mid-face has a sunken-in appearance, her upper jaw slopes backward, and the lower teeth project in front of the upper teeth, all characteristics of the syndrome. Individuals may have full-length webbing or fusion between the 2nd, 3rd, and 4th fingers, as well as the toes. As the child grows, the bones in the hands and feet become progressively fused, which reduces flexibility and function. Even though my client showed the physical manifestations of this disease, she seems to have found ways to compensate for her limitations. Other signs of Apert Syndrome are cognitive delay or slowing of intellectual development, vision loss from imbalanced eye muscles, and hearing loss from recurrent ear infections. My client did not show signs of hearing or vision loss. She did show signs of developmental delay, which was evident in the way she related to children in the playroom and also by her verbal communication. This may improve as she grows older. Treatment for Apert Syndrome consists of surgery to correct abnormal bone growth of the skull, mid-face, and jaw area. **This client also has a history of hydrocephalus, a sequelae of Apert Syndrome, requiring a ventricle peritoneal shunt, which was last revised at age six months. Hydrocephalus results from (1) obstruction of cerebrospinal fluid (CSF) flow, (2) interference with absorption of CSF, and (3) overproduction of CSF. When the movement or flow of CSF is restricted, intracranial pressure (ICP) rises, the ventricular system dilates proximal to the obstruction of the flow, resulting in hydrocephalus. Complications of hydrocephalus include increased ICP, infection, shunt malfunction, delays in cognitive, psychosocial, and physical development, and decreased IQ. Clinical manifestations in older children include vital sign changes (decreased HR, decreased RR, increased BP, increased T), frontal headache, nausea and vomiting, anorexia and/or abdominal pain, ataxia, lower extremity spasticity, visual changes, change in mental status, behavioral changes, deterioration in cognitive ability, and seizures. When this client was admitted on 9/18 she presented with reddening along the skin shunt and abdominal pain that had persisted for three days, perhaps signs of increased ICP and infection. On 9/19 the shunt was removed, and her CSF was tested for the presence of bacteria. On 9/26 she underwent externalization of the shunt with a R occipital ventricular drain draining to the abdomen. She was treated with Vancomycin for infection. The client has a secondary active diagnosis of postural ataxia. The word ataxia means without coordination. People with ataxia have problems with coordination because parts of the nervous system that control movement and balance are affected. Postural ataxia affects my client’s ability to balance when walking. She walks with feet placed further apart to compensate for poor balance. *Mosby’s Pediatric Nursing Reference, 2004 **http://www.nlm.nih.gov/medlineplus/ency/article/001581.htm Diagnostic procedures/ tests recently done or ordered and indications/ findings: The client was evaluated for an abdominal pseudocyst or free air. On 9/19 CSF was evaluated for the presence of gram negative bacteria. There were two subsequent draws from CSF for the evaluation of presence of gram negative bacteria. The client was put on Vancomycin. The Vanco trough on 9/21 was 8. Following a dose change the trough was 12. Physicians were unable to obtain CSF in the OR on 9/26 during internalization of the VP shunt, Lab data relevant to care (be specific) and interpretation: *Abnormal lab values (CBC with Platelet Count, collected 9/27/08) RBC Count: 3.82 Low (range: 4-5). Interpretation: A decreased value could indicate anemia, but this client is borderline low at 3.82. This client may have had a slightly diluted blood concentration owing to being on IV fluids (which were discontinued on 9/28) when she was also drinking normal amounts on her own. Hemoglobin: 10.9 Low (range: 11.4-15.5). Interpretation: A decreased value could indicate anemia. However, antibiotics could cause decreased levels of hemoglobin, and this client was on both vancomycin for infection followed by Ceftrioxone (Cefoperazone). Hematocrit: 32.2 Low (range: 35-45). Interpretation: A decreased value could indicate anemia. However, a decreased hematocrit level could also be caused by antibiotics. *Mosby’s Manual of Diagnostic and Laboratory Tests, Third Edition, 2006 Current immunization status (per chart or parent report): Mother states her daughter is current on all immunizations. ***First focused AM assessment (optimally done by 8AM): Vital Signs Day 1 * Pain scale used: Faces Pain Rating Scale 0800 T: 36.7 P: 87 R: 22 1200 T: 36.8 P: 99 R: 22 1600 T: P: R: Vital Signs Day 2: 0800 T: P: R: 1200 T: P: R: 1600 T: P: R: Frequency ordered: q4 hr BP: 113/67 BP: 113/72 BP: Frequency ordered: BP: BP: BP: Intake & Output Previous 24 hr total intake: Dietary orders/ restrictions: no food restrictions Day 1 Oral IV Previous 24 hr total output: 0800 1200 1600 Totals 75% breakfast 75% lunch 135 ml D51/2 IV stopped, but access maintained NG UOP/Stool 200 ml urine 500 ml urine 200 ml urine Pain: 0 Pain: 0 Pain: Pain: Pain: Pain: Suction /drains Shift Totals 900 ml *A neuro assessment was also ordered q4 hrs. I assessed pupillary response at 0800 and 1200. Both assessments showed pupil size 3 and a brisk response to light (++). Body system assessments: Skin: Surgical scar on R occiput at VP shunt site. No reddening or signs of infection. Webbing between fingers has been removed on both hands. Skin between toes is dry. Skin in general is pink, warm, and dry, with good capillary refill. Head & neck: Head shows cranial changes consistent with Apert Syndrome. The client’s vision and hearing were not impaired and she was able to compensate for the side-spaced position of her eyes by bringing objects into view. Neuro: Eyes: PERL. Pupillary response 3 ++. A&O x 3. Appropriate speech and pleasant demeanor. Client reported no discomfort or pain. Musculoskeletal: Gross motor: Some weakness in legs when asked to push against hands. Postural ataxia with unsteady gait with hx of falls. Toes on both feet are fused. The L great toe has been surgically separated. Fine motor: client able to manipulate objects and perform ADLs such as tooth brushing and feeding self. However, she has reduced manual dexterity. There was stiffness in the wrist and ankle joints. No muscle atrophy or asymmetry noted. Cardiovascular: Apical pulse strong and regular. Pedal pulses strong bilaterally. Respiratory: Lungs clear. Client was taking Singulair PO for asthma but no signs of respiratory difficulty. GI: I did not see a bowel movement but heard in report that the last BM was normal. Abdomen soft without distention; bowel sounds 4 quads. GU: Voided normal amounts. Client’s IV fluids were dc’d at 12 pm as she was eating and drinking sufficiently. Urine was clear, yellow, and odorless. IV lines assessment: IV site on L hand clean and dry, without reddening or reported pain. Isolation issues aside from universal precautions (Contact/ airborne): none Special precautions (neutropenia/ thrombocytopenia): High risk for altered LOC r/t shunt revision and changes in ICP *Psycho-Social needs/ family issues: Risk for caregiver role strain r/t competing role commitments. Mom and Dad visited daily and did not have much time for each other. They also have three other children at home to care for. I was able to spend enough time with the client to allow the parents to go for a walk and have lunch together. Mom also stated she was a Medical Assistant and hoped to go to nursing school, but thought it would be difficult to do that as well as balance being a wife, mother, and caregiver. Resources utilized or potentially utilized outside the hospital: The following web links provide resources for support for families affected by Apert Syndrome: http://www.aboutfaceusa.org, and http://www.ccakids.org In addition, families can contact the Apert Support and information Network, Don and Cathie Sears, PO Box 2571, Columbia, SC 29202 or check their web site, http://www.apert.org/ II. HEALTH PATTERNS ASSESSMENT (O: objective S: subjective) Self-Perception-Self-concept: Nutrition Metabolic: O: Client on IVF D51/2 NS 35mL/h. This was dc’d at 12 noon on 9/28/08. Client was eating 75% of regular diet meals and drinking adequate amounts. Lab values for electrolytes on 9/27/08 were wnl, lab values for CBC showed borderline low values for RBCs, hematocrit, and hemoglobin, probably owing to course of antibiotics. At time of discharge client had lost 0.4 kg of weight. ND: Effective feeding pattern. Sleep Rest: Client has normal and regular sleeping patterns. ND: Effective sleep rest patterns Coping Stress: Medical Diagnosis: O: Client is a 7 yo female with Apert Syndrome and history of hydrocephalus requiring a Ventricle Peritoneal shunt and treatment for infection. Secondary active dx: postural ataxia and developmental delay. Activity Exercise: S: Client stated she was ready and eager to go to the playroom. O: She had been using a bedside commode with supervision as she had fallen previously. When her IV was disconnected I supervised her walking to the bathroom, which she accomplished without difficulty. I then went with her to the playroom, where she was able to walk and even climb stairs (again, with careful supervision on my part in case she lost her balance). ND: Risk for Injury RT postural ataxia, fused toes, and stiff ankle joints secondary to Apert Syndrome AEB unsteady gait. when walking and previous falls. Role Relationship: O: This client is developmentally delayed and presently does not appear to have a negative selfconcept or self-perception. S: Mother states she is currently enrolled in a “regular” school and is teased by a boy there, but when I asked the client if anyone bothers her, she stated “no.” Mother also stated her daughter underwent separation of the great toe on L foot so she could wear flip flops and be “like the other kids.” ND: Risk for ineffective selfperception-self-concept RT social issues at school AEB mother states child is teased by classmate. Value-Belief: Did not determine family’s value-belief patterns. O: Mother and Father were at bedside and visited daily. S: Both parents stated they did not have much time to spend with each other, as both were working and caring for three other children at home. Mom and Dad both seemed to understand Apert Syndrome and Mom in particular was tuned in to her daughter’s needs. ND: Risk for Caregiver Role Strain RT multiple competing roles ND AEB mother stating she is having difficulty balancing responsibilities of wife, mother, and work. ND S: Mom and Dad were in good spirits but stated were ready for their daughter to come home so they could all get back to their regular ND routine. The client was feeling better and had a lot of energy and was eager to ND go back to school. ND: Effective coping-stress pattern. ND Elimination: ND O: Client has no elimination problems. Bowel sounds present 4 quadrants. ND: Effective elimination patterns. Cognitive Perceptual: Health Maintenance-Perception: O: Client has a hx of hydrocephalus and a VP shunt draining to her abdomen. On 9/28 the client was A&O x 3 and pupillary reaction was 3++. No signs of hearing or vision loss were observed, and client was able to compensate for structural differences related to Apert’s syndrome. Client is developmentally delayed, which affects her ability to communicate and interact with other people. O: Client has Apert Syndrome. Client has a VP shunt draining CSF to her abdomen. Client is developmentally delayed and has postural ataxia. Client was treated for infection and underwent shunt revision. Incision site is clean, dry, intact, and free of infection. No changes in LOC on 9/28. Parents ND understand Apert Syndrome and S&S of ICP. Both are involved in child’s care at home. ND: Developmental delay RT hx of hydrocephalus secondary to Apert syndrome AEB interactions with other children in the playroom. ND: Effective Health Maintenance-Perception. ND III. Nursing diagnoses/ problems identified and prioritized (2-3 per clinical day) and rational for identifying each of these problems on today's list: *Nursing Diagnosis 1: Risk for Injury RT postural ataxia, fused toes, and stiff ankle joints secondary to Apert Syndrome AEB unsteady gait when walking and previous falls. Assessment/ functional pattern: Client has postural ataxia, which affects coordination and balance. She also has fused toes on both feet, which creates difficulty planting her feet while walking. She compensates by placing her feet farther apart for balance but her gait is unsteady. Client is able to ambulate well but has fallen while hospitalized and needed to be supervised at all times. Nursing goals/ expected outcome: Client will not fall and injure self. Nursing interventions: 'The nursing student will..........' 1. Keep siderails up on bed 2. Have bedside commode available so client doesn’t have to walk to the bathroom 3. Monitor ambulation at all times 4. Keep floor free of clutter Rationale/ Patho Siderails up on the bed will prevent client from falling out Minimize need for walking any distance that might increase risk for falling Close supervision provides the opportunity to prevent a fall, while still supporting independence Clutter is an added risk for falling 5. Make sure the client is wearing hospital socks with rubber Hospital socks provide greater tread traction while walking Evaluation (can be current and/or prospective): On 9/28 the client was eager to go to the playroom. I supervised her ambulating to the bathroom instead of using the bedside commode to assess her readiness to walk in the playroom. She was able to ambulate to the toilet without losing her balance, so I accompanied her to the playroom. She successfully walked and even climbed a short stairway without losing her balance or falling. *Nursing Diagnosis 2: Risk for Caregiver Role Strain RT multiple competing roles AEB mother stating she is having difficulty balancing responsibilities of wife, mother, and work. Assessment/ functional pattern: Mother stated she is a Medical Assisstant and hopes to go to nursing school someday. She is currently taking care of four children at home, including the client. She stated it has been difficult to find time to go out with her husband and get everything done around the house, especially since she is also working part time. Nursing goals/ expected outcome: Caregiver reports that formal and informal support systems are adequate and helpful. Nursing interventions: 'The nursing student will..........' 1. Encourage caregiver to identify available family and friends who can assist with caregiving. Rationale/ Patho Successful caregiving should not be the sole responsibility of one person. In some situations there may be no readily available resources; however, often family members hesitate to notify other family members or significant others because of unresolved conflicts in the past. 2. Encourage caregiver to set aside time for self. This could be as simple as a relaxing bath, a time to read a book, or going out with friends 3. Acknowledge to caregiver the role he or she is carrying Caregivers have identified how out and its value. important it is to feel appreciated for their efforts 4. Provide time for caregiver to discuss problems, concerns, As a caregiver, the nurse is in an and feelings. Ask caregiver how he or she is managing. excellent position to provide emotional support. 5. Encourage caregiver in support group participation. Groups that come together for mutual support can be quite beneficial in providing education and anticipatory guidance. Groups can meet in the home, social setting, by telephone, or even through computer access. Evaluation (can be current and/or prospective): Mom appears to have some information regarding Apert Syndrome and has the support of her husband, but has not participated in support groups or used her family much as a resource. Hopefully she will see her family and others as an option for relief of caregiving, will find balance in her responsibilities as mother and wife, and will feel she is able to one day go to nursing school. *Wong’s Nursing Care of Infants and Children, Eighth Edition, 2007 * *Mosby’s Pediatric Nursing Reference, 2004 IV. Medication Administration Worksheet Show all calculations for at least 4 medications per 2 clinical days (at least 2 IV meds!): dose range and maximum dose for weight, dose to be given, concentration of mixture and volume to draw up, final dilution and rate to infuse) 1. Medication: Ceftrioxon (Cefoperazone) 50mg/kg dose Pt’s current weight (kg): 32.6 kg* What is the safe dosage range** per day & dose: 50-200 mg/kg/day What is the maximum dose for this patient? Dose ordered: 1650 mg IV *(calculated for 33 kg, weight on admission. Calculated using current weight of 32.6 kg, dose should be 1630 mg) Frequency: q12 50 x 33kg =1650 mg/day 200 x 33kg= 6600 mg/day safe dose range = 1650mg-6600mg/day 6520 mg/day Is the ordered dose safe? Yes: 2x1650=3300 mg/day How is it reconstituted? Intermittent: Dilute each 1 g with 5 mL sterile water. Shake vigorously to dissolve, then dilute in 50–100 mL of D5W or NS. Continuous: Further dilute in 500–1000 mL of the selected IV solution. How is it administered? (i.e. solutions, volumes and rate) Intermittent: Give 50-100 mL over 15–30 min. Continuous: Give 500–1000 mL over 6–24 h. Client’s IV of D51/2 NS was set at a continuous rate of 35 mL/h on 9/28/08. 1650mg/12h=137.5 mg/h. 137.5 mg/35 mL/h= 3.9 mg/h. Client received 3.9 mg/mL/h of ceftrioxone 2. Medication: Zofran (0.1 mg/kg/dose) Dose ordered: 3 mg IV Pt’s current weight (kg): 32.6 kg Frequency: q8h PRN What is the safe dosage range** per day & dose: Child: IV 1 mo–12 y, <40 kg, 0.1 mg/kg I did not find a specific reference for max dose per day. What is the maximum dose for this patient? 32.6 kg x 0.1mg = 3.26 mg/dose Is the ordered dose safe? yes How is it diluted? IV Infusion: Dilute a single does in 50 mL of D5W or NS. May be further diluted in selected IV solution. How is it reconstituted? How is it administered? (i.e. solutions, volumes and rate) IV Infusion: Give over 15 min. When three separate doses are administered, infuse each over 15 min. 50 mL/15 min = 3.3 mL/min 3 mg/15 min = 0.2 mg/min 3. Medication: Singulair Dose ordered: 5 mg PO (0.15 mg/kg) Pt’s current weight (kg): 32.6 kg Frequency: q24 What is the safe dosage range** per day & dose: Child: PO 6–14 y, 5 mg chewable tablet q.d. in evening What is the maximum dose for this patient? 5mg How is it reconstituted? Is the ordered dose safe? yes How is it diluted? How is it administered? (i.e. solutions, volumes and rate) 4. Medication: Acetaminophen (15 mg/kg dose, max) Dose ordered: 500mg PO Or 2000mg/day Pt’s current weight (kg): 32.6 kg Frequency: q4 PRN What is the safe dosage range** per day & dose: 10x32.6=326mg/dose 15x32.6=489mg/dose What is the maximum dose for this patient? How is it reconstituted? For children under 12 years of age, the recommended dose of acetaminophen is 10 to 15 mg/kg every 4 to 6 hours, not to exceed five doses (50-75 mg/kg) in 24 hours 4 x 326 = 1304 mg/day 50 x 32.6 = 1630 mg 4 x 489 = 1956 mg/day 75 x 32.6 = 2445 mg 15 mg x 32.6 kg = 489 mg x 4 = 1956 mg/day Is the ordered dose safe? How is it diluted? How is it administered? (i.e. solutions, volumes and rate) *Nurse’s Drug Guide, 2008. Wilson, Shannon, Shields and Strang. yes








