Bacterial infections
The skin’s normal bacterial flora prevents colonization by pathogenic organisms. A break in epidermal
integrity by trauma, leg ulcers, fungal infections (e.g. athlete’s foot) or abnormal scaling of the skin (e.g. in
eczema) can allow entry of bacteria. If reinfection occurs this may be due to asymptomatic nasal carriage of
bacteria or the presence of other infected close contacts.
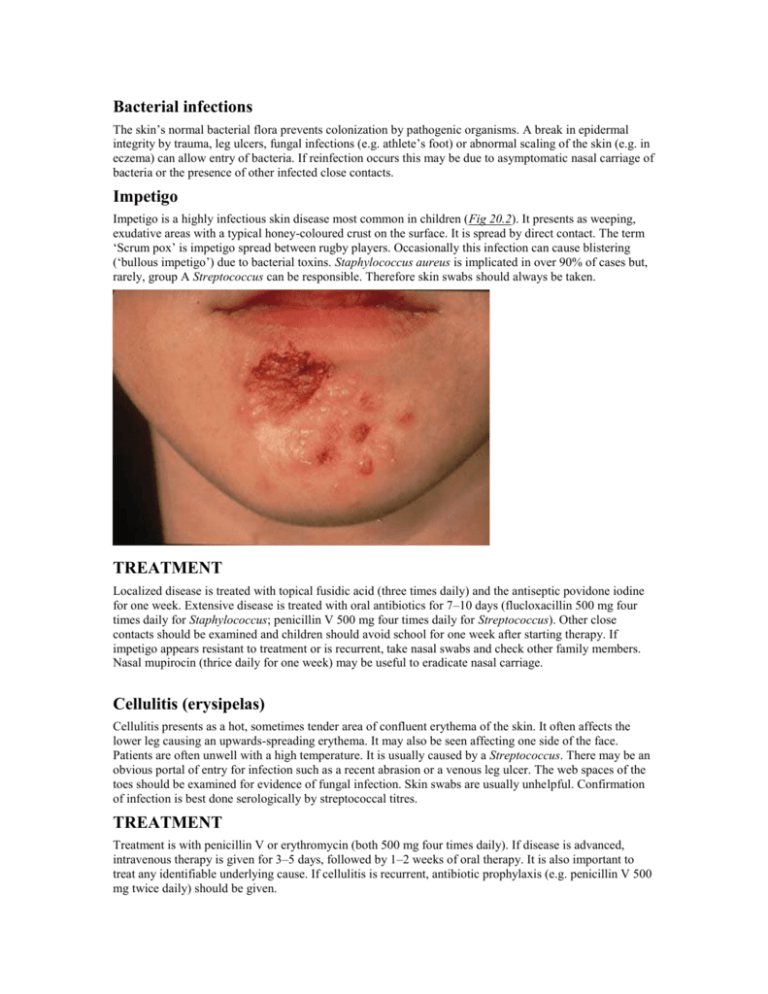
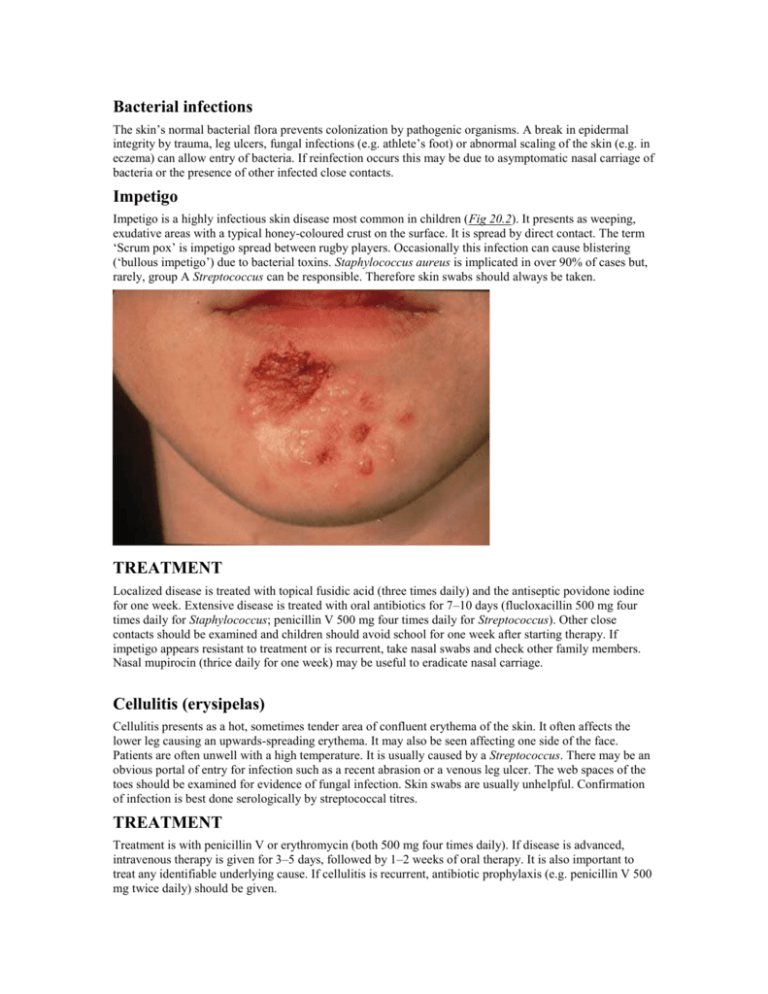
Impetigo
Impetigo is a highly infectious skin disease most common in children (Fig 20.2). It presents as weeping,
exudative areas with a typical honey-coloured crust on the surface. It is spread by direct contact. The term
‘Scrum pox’ is impetigo spread between rugby players. Occasionally this infection can cause blistering
(‘bullous impetigo’) due to bacterial toxins. Staphylococcus aureus is implicated in over 90% of cases but,
rarely, group A Streptococcus can be responsible. Therefore skin swabs should always be taken.
TREATMENT
Localized disease is treated with topical fusidic acid (three times daily) and the antiseptic povidone iodine
for one week. Extensive disease is treated with oral antibiotics for 7–10 days (flucloxacillin 500 mg four
times daily for Staphylococcus; penicillin V 500 mg four times daily for Streptococcus). Other close
contacts should be examined and children should avoid school for one week after starting therapy. If
impetigo appears resistant to treatment or is recurrent, take nasal swabs and check other family members.
Nasal mupirocin (thrice daily for one week) may be useful to eradicate nasal carriage.
Cellulitis (erysipelas)
Cellulitis presents as a hot, sometimes tender area of confluent erythema of the skin. It often affects the
lower leg causing an upwards-spreading erythema. It may also be seen affecting one side of the face.
Patients are often unwell with a high temperature. It is usually caused by a Streptococcus. There may be an
obvious portal of entry for infection such as a recent abrasion or a venous leg ulcer. The web spaces of the
toes should be examined for evidence of fungal infection. Skin swabs are usually unhelpful. Confirmation
of infection is best done serologically by streptococcal titres.
TREATMENT
Treatment is with penicillin V or erythromycin (both 500 mg four times daily). If disease is advanced,
intravenous therapy is given for 3–5 days, followed by 1–2 weeks of oral therapy. It is also important to
treat any identifiable underlying cause. If cellulitis is recurrent, antibiotic prophylaxis (e.g. penicillin V 500
mg twice daily) should be given.
Ecthyma
Ecthyma is also an infection due to Streptococcus or Staphylococcusaureus or occasionally both. It presents
as chronic, well-demarcated, ulcerative lesions sometimes with an exudative crust. It is more common in
developing countries, being associated with poor nutrition and hygeine. It is rare in the UK but is seen more
commonly in intravenous drug abusers and people with HIV infection.
TREATMENT
Treatment is with 10–14 days of penicillin V and flucloxacillin (both 500 mg four times daily).
Erythrasma
Erythrasma is caused by Corynebacterium minutissimum. It usually presents as an orange-brown flexural
rash, and is often seen in the axillae or toe web spaces (Fig 20.3). It is frequently misdiagnosed as a fungal
infection. The rash shows a dramatic coral pink fluorescence under Wood’s (ultraviolet) light.
TREATMENT
It responds well to oral erythromycin 500 mg four times daily for 10 days.
Folliculitis
Folliculitis is an inflammation of the hair follicle. It presents as itchy or tender papules and pustules.
Staphylococcus aureus is frequently implicated. It is more common in humid climates and when occlusive
clothes are worn. A variant occurs in the beard area (called ‘sycosis barbae’) which is more common in
Afro-Caribbeans. This is probably caused by the ability of shaved hair to grow back into the skin,
especially if the hair is naturally curly.
Extensive, itchy folliculitis of the upper trunk and limbs should alert one to the possibility of underlying
HIV infection.
TREATMENT
Treatment is with topical antiseptics, topical antibiotics (e.g. fucidin) or oral antibiotics (e.g. flucloxacillin
500 mg or erythromycin 500 mg both four times daily for 2–4 weeks).
Boils (furuncles)
Boils are a rather deep-seated infection of the skin often caused by Staphylococcus. They can cause painful
red swellings. Boils are more common in teenagers and are often recurrent. Recurrent boils may also occur
rarely in diabetes mellitus or in immunosuppression. Large boils are sometimes called ‘carbuncles’.
TREATMENT
Treatment is with oral antibiotics (e.g. erythromycin 500 mg four times daily for 10–14 days) and
occasionally by incision and drainage. Antiseptics such as povidone iodine, chlorhexidine (as soap) and a
bath oil (e.g. Oilatum plus™) can be useful in prophylaxis.
Hidradenitis suppurativa
This is a rare condition characterized by a painful, discharging, chronic inflammation of the skin at sites
rich in apocrine glands (axillae, groins, natal cleft). The cause is unknown, but it is more common in
females and within some families it appears to be inherited in an autosomal dominant fashion. Clinically it
presents after puberty with papules, nodules and abcesses which often progress to cysts and sinus
formation. With time, scarring may arise. The condition follows a chronic relapsing/remitting course.
TREATMENT
Treatment is very difficult, but antibiotics, oral retinoids and Dianette™ (2 mg cyproterone acetate + 35 µg
ethinyloestradiol in females only) have been tried. They should be used as for acne vulgaris (p. 1169).
Severe recalcitrant cases have been treated occasionally with surgery and skin grafting.
Pitted keratolysis
This is a superficial infection of the horny layer of the skin caused by a corynebacterium. It frequently
involves the soles of the forefoot and appears as numerous small punched-out circular lesions of a rather
macerated skin (e.g. as seen after prolonged immersion). There may be an associated hyperhidrosis of the
feet and a prominent odour.
TREATMENT
Topical antibiotics (e.g. fucidic acid or clindamycin, applied thrice daily for 2–4 weeks) and topical antisweating lotions are effective therapies.
Erysipeloid
This is a very rare infection due to Erysipelothrix insidiosa. It is seen in people who handle raw meat
(especially pork) and fish. The organism gains entry through breaks in the skin. It presents as a spreading,
well-demarcated purplish-red lesion usually on the fingers, hands or forearms. There are no systemic
symptoms.
TREATMENT
Treatment is with penicillin V or oxytetracycline (both 500 mg four times daily for 7–10 days).