Neurological Complications of SYSTEMIC DISEASE
advertisement

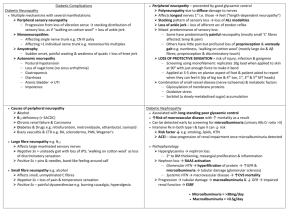
CHAPTER XIII NEUROLOGICAL COMPLICATIONS OF SYSTEMIC DISEASE NEUROLOGICAL COMPLICATIONS OF DIABETES MELLITUS (DM) Diabetes Mellitus is a worldwide life long disease characterized by persistent hyperglycemia secondary to lack of insulin, cellular resistance to the effects of insulin or a combination of both. It has a wide range of complications such as renal failure, blindness, neuropathy, peripheral vascular disease with gangrenous complications, coronary artery disease & stroke. Classification of Diabetes Mellitus Insulin-dependant DM (IDDM, type I): Usually young, thin patient, absolute insulin deficiency; ketosis prone. Non-Insulin-dependant DM (NIDDM, type II): Usually older obese patients; relative insulin lack & tissue resistance to insulin effects, not ketosis prone; often have positive family history. DM associated with other conditions (secondary diabetes): Hyperglycemia associated with other hormonal, metabolic or genetic disorders (e.g., acromegaly). Impaired glucose tolerance (IGT): Hyperglycemia that is not of significant degree to meet the criteria for DM. Gestational diabetes mellitus (GDM): Hyperglycemia associated with pregnancy & meeting the criteria for diagnosis of DM, resolves after parturition. Both insulin-dependent DM (IDDM) & non-insulin-dependent DM (NIDDM) have similar complications. The incidence of complications increases with duration of disease & severity of hyperglycemia. The association of diabetic neuropathy, retinopathy & nephropathy is frequent & suggests a common underlying mechanism for these complications. Neurological Complications of DM include: I. Peripheral N.S. Complications: Diabetic Neuropathy. II. Central N.S. Complications: 1. Metabolic Derangement: Diabetic ketoacidosis. Non-ketotic hyperosmolar coma. Hypoglycemia. 1. Cerebrovascular Diseases: HTN & Arteriosclerosis. Stroke in Diabetics. 2. Other CNS abnormalities in DM. 355 PERIPHERAL NS COMPLICATIONS OF DM Diabetic Neuropathy Pathogenesis of Diabetic Neuropathy: The pathogenesis of diabetic neuropathy is still uncertain. Neuropathy is commoner in poorly controlled DM of long duration.However, it may occur in controlled DM of short duration. Three factors (metabolic, vascular & genetic) participate in the causation of diabetic neuropathy: 1. Metabolic factors: - (Sorbitol accumulation, myoinositol depletion & decrease Na,K-ATPase activity). - Persistent hyperglycemia (aldose reductase) → accumulation of Sorbitol within the nerve → hypertonicity. 2. Vascular & Hypoxic factors: - (Microvascular ischemia of nerve + endothelial hypoxia). - Occlusion of vasa nervosum → mononeuropathy - Ischemia →generalized polyneuropathy. 3. Genetic factors may explain the development of complications in some diabetics irrespective of the control or duration of DM. Classification of Diabetic Neuropathy I. Peripheral Nervous System (Somatic Neuropathy) Polyneuropathy: Acute sensory Chronic sensorimotor Mononeuropathy: Mononeuritis simplex Mononeuritis multiplex Truncal mononeuropathy. Proximal motor neuropathy (Amyotrophy). II. Autonomic Nervous System: Autonomic neuropathy (Visceral neuropathy). III. Central Nervous System: Cranial mononeuropathy. Another Classification of Diabetic Neuropathy Symmetrical distal neuropathy: Small fiber predominant (painful or anesthetic). Large fiber predominant (ataxic or pseudotabetic) Autonomic neuropathy. Asymmetrical neuropathy: Cranial neuropathies (especially 3rd nerve palsy). Plexopathies (including amyotrophy). Mono- & polyradiculopathies. Increased susceptibility to pressure palsy. 356 Evaluation of Diabetic Neuropathy Symptoms 1. Symptom Sensory symptoms o Negative symptoms o 2. Numbness, deadness, “cotton wool feeling”, “walking on stilts”, “feels like I am wearing gloves”, loss of balance (especially with eyes closed), loss of dexterity, inability to find or identify objects in pocket or purse, painless injuries, ulcers. Burning, prickling, pain, super-sensitivity to light touch, stabbing, electric shock, tearing, tight, band-like. Depends on severity & distribution Positive symptoms o Focal symptoms Motor symptoms o Distal weakness o 3. Common Description Impaired fine coordination of hands, inability to turn keys or open jars, toe scuffing, tripping, foot slapping. Difficulty with stairs, inability to rise from chair or floor, falls due to knee “giving”, difficulty working with or raising arms above the shoulder. Depends on severity & distribution. Proximal weakness o Focal weakness Autonomic System o Sudomotor o Cardiovascular o Pupillary System o Sexual o Bladder o Bowels Loss of sweating, excessive sweating in definite areas, gustatory sweating, dry skin. Postural light-headedness, fainting, micturition syncope, cough syncope & exertional syncope. Usually asymptomatic, poor dark adaptation, intolerance of bright light. Impotence, loss of ejaculation, retrograde ejaculation, loss of ability to reach sexual climax. Urgency, incontinence, dribbling, hesitancy. Vomiting (especially of retained food), diarrhea, nocturnal diarrhea, constipation. Evaluation of Sensations in DM Sensory loss: extent, distribution, modality involved. Use defined points on the 4 limbs (e.g., the dorsum of digit just proximal to the nails). Assessment of threshold for vibration, light touch, joint position, pin sensation. Quantitation of sensory deficit using automated or computer-assisted techniques. 357 Evaluation of Motor deficit in DM Comparison of the Mayo & Medical Research Council (MRC) Muscle Strength Grading Systems Description of muscle strength •Normal power •Mild weakness (25% loss) •Active but weak movement against gravity & resistance •Active movement against gravity but not resistance •Moderate weakness (50% loss) •Active movement with gravity eliminated •Severe weakness (75% loss) •Flicker of contraction •No contraction Mayo grade 0 -1 MRC grade 5 - - 4 -2 -3 -4 3 2 1 0 Evaluation of Autonomic Functions in DM Orthostatic hypotension: Measuring BP in supine, sitting & standing positions - A fall in systolic Bp > 20% on standing > l min. - A fall in systolic BP > 25-30mmHg on standing - A fall in diastolic BP > 10mmHg on standing (All are considered abnormal) A “reflex tachycardia” should accompany the fall of BP. If the “pulse rate” does not , sympathetic denervation should be suspected. A “fixed tachycardia” which does not slow in response to the “Valsalva maneuver” may indicate loss of parasympathetic vagal innervation to the heart. Dry skin may indicate loss of sudomotor function. The “thermoregulatory sweat test” measures distribution of sweating in response to heating the body core temperature by 1oC. “Sudomotor axon reflex testing” is also helpful. Electrophysiological Testing in DM N.C. Studies & EMG may aid in: 1. Confirmation of the clinically diagnosed diabetic neuropathy. 2. Identification of a pattern of changes characteristic of diabetes. 3. Monitoring of progression or remission of diabetic neuropathy. 4. Detection of asymptomatic cases or atypical cases e.g. purely autonomic, those presenting with pain alone. Electrophysiological studies cannot specifically diagnose diabetic neuropathy. Patterns that are suggestive of diabetic neuropathy: - Mild or asymptomatic cases →distal slowing of conduction. - Clinically overt neuropathy →a mixture of changes suggesting both “demylination” & “axonal degeneration”. - Progressive worsening of the neuropathy → “axonal degeneration” predominance. Electrophysiological changes are usually more widespread than clinical signs. 358 Reversibility of EMG & NCV changes can be accomplished by controlling the diabetes, dietary supplementation with myoinositol or the use of aldose reductase inhibitors that prevent sorbitol in nerve. Clinical Patterns of Diabetic Neuropathy Approximately 2/3 of diabetics have some form of neuropathy: - 66% of patients with type I (IDDM) - 59% of patients with type II (NIDDM) Approximately: - 1/2 of pts have “symmetrical polyneuropathy” - 1/4 of pts have “carpal tunnel syndrome” - The remainder have autonomic or other neuropathies. Symptoms of symmetrical polyneuropathy occur in: - 15% of IDDM patients - 13% of NIDDM patients Severe disabling neuropathy occurs in: - 6% of IDDM pts - 1% of NIDDM pts Carpal tunnel syndrome is clinically diagnosed in: - 7.7% of diabetics. Distal Symmetrical Neuropathy in DM It is the most common form of diabetic neuropathy. Symptoms: Negative symptoms: - Loss of feeling. - Charcot joints → progressive painless ankle & foot deformity - Loss of balance (at night & with eyes closed) - Burning & stinging sensations. Positive symptoms: - Tight, band-like feeling around the extremities. - An electrical tingling sensation. Signs: - Distal symmetrical sensory loss - Weakness of toe dorsiflexion & intrinsic hand muscles. - Distal hyporeflexia or areflexia NCV & EMG: - Distal slowing of both sensory & motor conduction - Distal changes indicating chronic partial denervation with reinnervation. 359 Clinical Features Suggesting a Non-diabetic Etiology For Neuropathy in Diabetic Pts Clinical features o Family history of neuropathy, painful feet. o Abrupt onset o Pes cavus & hammer toes o Monoclonal gammopathies in serum o o CSF protein >100mg/dl ESR, +ve RF, +ve ANA (Antinuclear antibodies) Consider Hereditary motor & sensory neuropathy (HMSN) Inflammatory Neuropathy HMSN Primary systemic amyloidosis. Myeloma Lymphoma Inflammarory Neuropathy Inflammatory Neuropathy Necrotizing angiopathy Autonomic Neuropathy in DM It occurs in most pts. with diabetes & peripheral neuropathy. It may be asymmetric. Pupil abnormalities: - Miosis & lost response to light or accommodation. - May mimic Argyll-Robertson pupil of tabes dorsalis Sudomotor function: - Loss of sweating; - Loss of thermoregulation; + - Compensatory hyperhidrosis or gustatory sweating. Cardiovascular abnormalities: - Orthostatic hypotension & loss of compensatory tachycardia. Gastrointestinal function: - Gastroparesis: nausea & vomiting. - Diarrhea: explosive, nocturnal, painless & watery. - Resistant constipation alternating with diarrhea. Diabetic bladder disease: - Loss of afferent information from nerves in detrusor muscle, progressive bladder enlargement. - UT infection may precipitate renal failure. Impairment of sexual function: - Erectile impotence or ejaculatory failure. Insensitivity to hypoglycemia: - Hypoglycemia → epinephrine release & sympathetic activity. - Epinephrine release is mediated by the splanchnic nerves. - This response may be lost in pts. with autonomic neuropathy Subacute Symmetrical Neuropathies in DM Acute Painful Neuropathy with Wt. Loss: - Wt. loss → Cachexia. - Severe pain, burning or stinging or electric shock-like. - Depression. - Impotence. - Complete resolution of symptoms within 6-24 months. 360 Hypoglycemic Neuropathy: - Neuropathic symptoms begin or worsen following insulin therapy. - Insulinoma or insulin shock therapy has a similar effect. - Severe, prolonged hypoglycemia may cause neuronal or axonal damage. Focal & Multifocal Neuropathy in DM Two types of focal neuropathy occur in diabetics: 1) Spontaneously occurring neuropathies: At the level of root, plexus or individual nerve 2) Those occurring in nerves crossing common pressure points: The underlying pathology in these cases is vascular. Diabetic Radiculopathy & Polyradiculopathy Occur in long-standing DM. Uncommon below 40 years. Mononeuropathies may occur at any spinal level. Characteristically: thoracic & upper lumbar roots are involved. Acute or subacute pain, with minimal sensory loss. Burning & supersensitivity of the skin. Symptoms & signs may be entirely at one root level. Electrophysiologic changes are more diffuse e.g. fibrillation potentials in the paraspinal muscles. Imaging: excludes a mass lesion. Prognosis: is excellent, pain resolves gradually in few months. Recurrent diabetic radiculopathy may occur. Polyradiculopathy may occur in some diabetics. DD: CIDP, AIDS, Lymphoma, Sarcoidosis. (Differentiated by: NCV, CSF protein, cells & cytology). Diabetic Plexopathy (D.Amyotrophy; D.Myelopathy; D.Femoral Neuropathy;Proximal Motor Neuropathy; Radiculoplexopathy) Symptoms & Signs: Rapid onset. Pain in the anterior thigh. Buckling of the knee due to quadriceps weakness. Weakness & severe atrophy of quadriceps muscle. Sensory loss is minimal (Patchy hypoesthesia or hyperpathia over the thigh) Knee reflex is or absent. + Evidence of distal peripheral neuropathy. Cranial Neuropathy in Diabetics Isolated 3rd & 6th nerve palsies are frequent. Oculomotor Palsy: Rapid onset with pain in the forehead. Typical 3rd nerve palsy with ptosis, but sparing of the pupillary reflex. 361 The underlying pathology is a vascular lesion. DD: Compressive lesions → early loss of pupillary reflex. Compression Neuropathies in Diabetics Common Types: Carpal Tunnel Syndrome (CTS) (Median neuropathy at the wrist) Ulnar neuropathy at the elbow. Peroneal neuropathy at the fibular head. Their incidence is higher among diabetics. Surgical decompression is reserved for patients with a significant deficit. Treatment of Diabetic Neuropathy I. Therapies to correct the underlying pathogenetic mechanism. II. Symptomatic treatment. I. Therapies to correct the underlying pathogenetic mechanism: Control of blood glucose level: Normalization of blood glucose levels prevents microvascular complications including neuropathy. Aldose reductase inhibition : Drugs that inhibit aldose reductase can reduce accumulation of alcohol sugars in the nerves. Supplementary dietary intake of myoinositol may be useful. II. Symptomatic Treatment 1. Physical Approaches: - Foot care. - Proper footwear. - Treat local infection aggressively. - Cessation of wt. bearing to allow healing of plantar ulcers. - Alternating hot & cold soaks for painful foot. - Avoidance of repeated trauma in compression neuropathy. - Avoidance of crossing of legs & leaning on elbows. - Nocturnal splinting for pts. with CTS. - Avoidance of intra-operative pressure or traction trauma to nerves. - Physiotherapy for pts. with focal neuropathies. 2. Pharmacological Approaches: - Carbamazepine, (Tegretol): for the lancinating or lightning pains. Dose: 100 mg. tid., to 200 mg. tid. Action: It membrane stability. - Gabapentin (Neurontin), 400-800 mg tid for neuropathic pain - Antidepressants e.g. Amitriptyline (Tryptizol) or Doxepin( Sinequan): for burning steady pain. - Mexilitine (Mexitil) improves peripheral nerve blood flow. - Simple analgesics. 362 CNS COMPLICATIONS OF DM Metabolic Derangement: Diabetic Ketoacidosis. Non-ketotic Hyperosmolar Coma. Hypoglycemic Coma. II. Cerebrovascular Disease: Hypertension. Atherosclerosis. Stroke in Diabetics. III. Other CNS Abnormalities in Diabetes: Spinal cord lesions: - Posterior column degeneration. - Corticospinal tract degeneration. - Diabetic myelopathy. Primary diabetic encephalopathy. Autonomic neuropathy → Orthostatic hypotension & Syncope. Diabetic nephropathy may → Uremic encephalopathy. Secondary diabetes may occur in Friedreich's ataxia & dystrophic myotonia. Risk of DM in Huntington's disease (HD). I. Diabetic Ketoacidosis It results from hypoinsulinism. It is characterized by: Hyperglycemia (>400 mg/dl) Dehydration (due to osmotic diuresis with thirst, polyuria, anorexia, fatigue). Metabolic acidosis (Bl. PH < 7.2) with ketone bodies in blood & urine. Hepatic fatty acid catabolism → Ketosis. Coma in 10% of cases due to: - Serum hyperosmolality. - Acidosis. - Alteration of CBF. - DIC. - Hypoxia. - Toxicity by fatty acids & lysolethicins. - A defect in brain carbohydrate metabolism. Complications of Therapy for Diabetic Ketoacidosis They may contribute to CNS dysfunction They include: Electrolyte disorders: - Hypokalemia (with insulin & fluid replacement) - Hypophosphatemia. - Hyponatremia (with rapid correction of hyperosmolality). Thromboembolic disorders - Precipitated by: Bl. viscosity due to dehydration Platelet adhesiveness Fibrinolytic activity - Myocardial, cerebral. or mesenteric infarction may cause death 363 Infection Hypoxemia due to pulmonary edema Cerebral edema is fatal due to ICP with herniation Non-Ketotic Hyperosmolar Coma Hyperglycemia with hyperosmolality without ketosis → progressive mental obtundation or coma. Common in elderly diabetics. Hyperglycemia ( > 800 mg/dl), osmotic diuresis & dehydration. Hyperosmolality (serum osmolality > 350 mOsm/kg). Some degree of renal dysfunction potentiates hyperglycemia. No significant ketoacidosis. It may be accompanied by serious diseases e.g. gram -ve pneumonia, MI, stroke, GI hemorrhage, gram -ve sepsis, pulmonary embolism, uremia, pancreatitis. Precipitating factors include: steroid therapy, thiazide diuretics, renal dialysis, severe burns, heat stroke. Seizures, focal neurological deficits & stroke-like syndromes are common. Flapping tremors, hemichoreoathetosis, hallucinations & hemianopia. Cerebral edema is rare. Lactic acidosis is frequent (? vascular disease & CHF → tissue ischemia → lactic acidosis). Treatment: Lactic acidosis is treated by IV sodium bicarbonate & treatment of its cause. Non-ketotic hyperosmolar coma is treated by little insulin + fluid replacement. Hypoglycemic Coma It is commonly produced by excessive dose of insulin. Post-prandial hypoglycemia may occur in early diabetics & in those with renal insufficiency. Sympathetic phase of hypoglycemia → dizziness, weakness, tremors & palpitations due to endocrine release. Neuroglycopenic symptoms → behavioral abnormalities. Recurrent nocturnal hypoglycemia → dementia. Hypoglycemia → 4 forms of acute metabolic encephalopathy: 1. Delirium, quiet or manic. 2. Multifocal brainstem dysfunction → neurogenic hyperventilation & decerebrate spasms. 3. Stroke-like events + focal deficits + coma. 4. Seizures, single or multiple. Hypothermia is common. Recurrent or persistent choreoathetosis may occur. Blood glucose < 30-40 mg/dl → confusion & behavioral changes. Further of blood glucose → stupor & seizures. Blood glucose < 10 mg/dl → profound coma. Hypoglycemia is corrected by oral or IV glucose. 364 Cerebrovascular Disease in Diabetics Ischemic stroke is 5-6 times more common in diabetics than in non-diabetics. Cerebral atherosclerosis, HTN & IHD contribute to stroke in diabetics. Hemorrhagic stroke is less frequent in diabetics. Hypertension affects 50% of diabetics & is a major risk factor for stroke. Hypertension is 1.5-3 times more common in diabetics Atherosclerosis is associated with HTN. Atherosclerosis is more common in diabetics. Stroke in Diabetics The incidence of ischemic stroke is higher in diabetics. DM, HTN, hyperlipidemia & obesity are major risk factors. The relative risk for ischemic stroke in diabetics is higher in women & may reach 13 fold in younger age groups. Diabetic stroke pts. have a 20% 5-years survival, compared to 40% in matched age nondiabetic stroke pts. DM appear to the morbidity & mortality following stroke Hyperglycemia promotes artherogenesis. Alterations in platelet adhesiveness, coagulation factors & fibrinolytic activity, contribute to atherogenesis in diabetics & thrombosis. Good control of hyperglycemia & HTN reduce the risk of stroke. 365 NEUROLOGICAL COMPLICATIONS OF RENAL FAILURE UREMIC ENCEPHALOPATHY Symptomatology differs in: 1. Early cases 2. Moderate cases 3. Severe cases The symptoms are ameliorated by dialysis, & relieved after successful renal transplantation. Symptomatology of Uremic Encephalopathy I. Early cases Anorexia Nausea Insomnia Restlessness Decreased attention span Inability to manage ideas Decreased sexual interest II. Moderate cases: Vomiting Sluggishness Easy fatigue Drowsiness Sleep deprivation Labile emotions Paranoia Decreased cognitive function Inability to abstract Decreased sexual performance III. Severe Cases: Itching Disorientation Confusion Bizarre behavior Slurring of speech Hypothermia Myoclonus Asterixis Convulsions Stupor, coma Clinical Assessment & Investigations of Uremic Encephalopathy It occurs in renal failure, acute or chronic. Initial symptoms: Apathy, fatigue, inattentiveness & irritability 366 Later symptoms: Confusion, disorientation, disturbed perception, hallucinations, dysarthria & asterixis. Toxic psychosis, with hallucinations, delusions, insomnia, or catatonia. Symptoms fluctuate from day to day or even from hour to hour. In anuric patients, symptoms develop abruptly → stupor & coma. Gradual uremia → visual hallucination & inattentiveness. Altered excretion of drugs in uremic pts. → their accumulation → toxic effects. In acute RF, clouding of sensorium is associated with motor phenomena (the uremic twitch-convulsive syndrome): Twitching & jerking. Convulsions. Asterixis. The involuntary movements continue during both wakefulness & sleep. As the uremia worsens → Uremic coma. Metabolic acidosis. Kussmaul breathing → Cheyne-Stokes breathing → death. HTN is frequently associated with uremia & may cause “Hypertensive Encephalopathy” EEG → diffuse slowness. CSF is normal. BUN & serum creatinine levels. CT-scans & MRI → cerebral shrinkage in chronic RF. No cerebral edema. Restoration of renal function → recovery of the neurologic syndrome. Treatment of Uremic Encephaloparthy Dialysis or renal transplantation is mandatory in irreversible progressive RF Anticonvulsants in low doses to control convulsions. Hyponatremia makes seizure control difficult & must be corrected. We must be cautious in prescribing certain drugs for uremic pts., e.g.: Aminoglycosides (vestibular damage). Furosemide (cochlear damage). Nitrofurantoin, INH, & Hydralazine (peripheral neuropathy). THE DIALYSIS “DISEQUILIBRIUM SYNDROME” It refers to a group of symptoms that may occur during & following hemodialysis or peritoneal dialysis. Symptoms include: Headache, bilateral & throbbing, or migraine-like, occur in 70% of pts. Nausea, vomiting, anorexia, blurring of vision. Muscular cramps, twitching Nervous irritability, restlessness, tremor. Agitation. Drowsiness, dizziness, disorientation. Convulsions. It has been attributed to cerebral edema due to: Inappropriate secretion of ADH → water intoxication → shift of water into the brain. 367 The reverse urea effect. Increased brain osmolality in rapid hemodialysis. Increased intracellular pH of cerebral cortex from production of organic acids. It is ameliorated by: Decreasing the rate & increasing the frequency of hemodialysis. DD: Subdural hematoma occurring in 3 - 4% of pts. undergoing dialysis. DIALYSIS ENCEPHALOPATHY (DIALYSIS DEMENTIA) A subacute progressive syndrome complicating chronic hemodialysis. It is a form of aluminum intoxication (from the dialysate & aluminum gels). Symptoms include: A hesitant, stuttering dysarthria, slurred speech. Dysphasia. Apraxia of speech. Facial & then generalized myoclonus. Focal & generalized seizures. Personality & behavioral changes. Intellectual decline. EEG: paroxysmal or periodic sharp wave or spike & wave activity, intermixed with abundant theta & delta activity. CSF is normal, except for occasional protein. Diazepam (Valium) may → dramatic reversal of the clinical symptoms & EEG changes in pts. with dialysis encephalopathy. Three forms of Dialysis Dementia are known: 1. Epidemic Form: is related to: Aluminum in dialysis water, Other trace elements in water (Mn, Mg, Fe, Cobalt, Tin) + abnormalities of the B.B.B. Normal pressure hydrocephalus (NPH). Slow virus infection of the CNS. Regional alterations in CBF. 2. Endemic Form: is related to chronic hemodialysis for > 2 yrs. 3. Childhood Form: may be due to nonspecific effect of uremia on immature brain. Treatment: Diazepam (valium) or Clonazepam (Rivotril) controls seizures. Desferoxamine improves other symptoms. Removing Aluminium from dialysate water prevents the epidemic form. UREMIC NEUROPATHY Three types: 1. Uremic Polyneuropathies 2. Uremic Mononeuropathies 3. Uremic Autonomic Neuropathies 1. Uremic Polyneuropathies: Peripheral neuropathy is the most frequent neurologic complication of chronic RF. It affects 2/3 of all pts. about to begin dialysis. 70% of those on regular dialysis have uremic polyneuropathy. Symptoms & Signs: Painless, progressive, symmetrical sensori-motor paralysis of the legs, then the 368 2. arms. Muscle weakness & atrophy, areflexia & sensory loss. Uremic polymyositis with hypophosphatemia. Muscle cramps, Restless-leg syndrome (crawling, prickling, & pruritus sensations in LLs) Burning-foot syndrome (swelling sensations & tenderness of feet) Glove & stocking hypoesthesia, Posterior column dysfunction, Both gloves & stocking, & posterior column dysfunction. Abnormal NCV may even precede clinical neuropathy. Uremic Polyneuropathies may be: A nonspecific effect of uremia on nerve function. Potential uremic neurotoxins including: Urea Creatinine Parathyroid hormone Myoinositol Transketolase Guanidine derivatives Middle molecules Secondary demyelination of spinal cord → posterior column dysfunction. Treatment of Uremic Polyneuropathies: Long-term hemodialysis → stabilization of the symptoms. Rapid hemodialysis may worsen the polyneuropathy. Peritoneal dialysis is more successful in improving polyneuropathy. Successful renal transplantation → complete recovery over 6-12 months, through eliminating the causative toxins e.g. methylguanidine & myoinositol. Carbamazepine (Tegretol), 400-600mg/d PO in 3 doses. Gabapentin (Neurontin), 400-800mg tid Clonazepam (Rivotril), 0.5mg PO tid, by 0.5/2-3 days up to 20mg/d. Uremic Mnononeuropathies: Carpal tunnel syndrome (CTS) Vestibulocochlear dysfunction → deafness. L.M.N.facial palsy. Uremic Mononeuropathies are attributed to: Hearing Loss ( Vestibulocochlear dysfunction ): - Bleeding in the inner ear space as a consequence of heparinization. - Cellular injury in hair cells of the cochlea as a result of edema - Desferrioxamine neurotoxicity → Auditory toxicity. Carpal Tunnel Syndrome: - A-V fistula. - Prolonged time of dialysis. - The uremia itself. - Deposition of B2 - microglobulin in the carpal tunnel synovia & tendons. L.M.N.Facial Palsy: - Diffuse disorder of neural conduction as a consequence uremia. Deterioration of vision - Pseudotumor cerebri associated with uremia. - Desferrioxamine neurotoxicity → visual toxicity. 369 3. Uremic Autonomic Neuropathies: Orthostatic hypotension, Impotence. Bowel disturbance. Autonomic Dysfunction in Uremia is attributed to: Altered plasma levels of catecholamines. Depressed baroreceptor activity. Toxic sympathetic neuropathy. Afferent autonomic lesion . Uremic Myopathy is attributed to: Vitamin D deficiency. Secondary to hyperparathyrodism. Vascular calcification. CEREBROVASCULAR STROKE IN RF Ischemic Stroke: 1. Accelerated atherosclerosis. Endothelial damage. Isolated elevation of plasma triglycerides. Reduction in HDL. Accelerated diabetes mellitus 2. Arrhythmogenic events related to hemodialysis uremic cardiomyopathy: Abnormal catecholamine levels in plasma. Premature aortic & mitral annular calcification. 3. Reduction of Protein C, Protein S. & Antithrombin III in the chronic condition. Hemorrhagic Stroke: 1. Heparin anticoagulation in hemodialysis. 2. Coagulopathic effect of uremia. 3. The extremely prolonged half life of Prostacyclines in plasma → bleeding tendency in uremics . HEMODIALYSIS HEADACHE Migraine may by hemodialysis. The dialysis disequilibrium syndrome → headache during & for up to 8 hrs after dialysis. Persistent headache points to subdural hematoma. Mechanism: 1. Increase Interleukin- I activity → release of Prostopeptidin E2 → alteration of Neuropeptide release. 2. Increase activity of Renin - Angiotensin - Aldosterone system → vasodilatation → vascular headache. SEIZURES IN RF Causes: 1. Uremic encephalopathy 2. Cerebral edema, water intoxication & hyponatremia 3. Hypocalcemia 4. Hypomagnesemia 5. Hypertensive encephalopathy 370 6. Dialysis disequilibrium syndrome 7. Very large doses of penicillin 8. Blood transfusion 9. Erythropoietin treatment Treatment of Seizures: Correction of the underlying metabolic problem. Dialysis for uremic encephalopathy-induced seizures. AEDs: Phenytoin (Epanutin) in usual dosages. Phenobarbital (Sominal, Sominalette) in lower dosages. Diazepam (Valium), up to 10 mg IV, or Lorazepam (Ativan), 2-4 mg IV. Valproic acid (Depakine) in usual dosages. Carbamazepine (Tegretol) in usual dosages. Ethosuximide (Zarontin) in usual dosages. Seizures during hemodialysis, due to the disequilibrium syndrome are controlled by: 1. The rate & duration of dialysis & its frequency. 2. Phenytoin (Epanutin), 100 mg tid for hemodialysis pts. Muscle Cramps Occur during or immediately following dialysis → pain. Treated by: Quinidine sulfate, 320 mg PO at the beginning of each dialysis. COMPLICATIONS OF RENAL TRANSPLANTATION Primary lymphoma of the brain may develop in immunosuppressed pts. Immunosuppressants e.g. Cyclosporin → wide-spread cerebral edema, more occipitally. Systemic fungal infections (Cryptococcus, Listeria, Aspergillus, Candida, Nocardia & Histoplasma). Other CNS infections (Toxoplasmosis & Cytomegalic inclusion disease). Bleeding diathesis may → Subdural or Cerebral hemorrhage. 371 NEUROLOGICAL COMPLICATIONS OF HEPATIC DISEASE HEPATIC ENCEPHALOPATHY Portal-Systemic Encephalopathy Hepatic Stupor & Coma It affects pts. with chronic hepatic disease e.g. cirrhosis, as well as those with acute hepatitis. Predisposing factors: Excess dietary protein. GI hemorrhage. Hypoxia. Hypokalemia. Metabolic alkalosis. Electrolyte depletion. Excessive diuresis. Sedative-hypnotic drugs. Constipation. Clinical Features of Hepatic Encephalopathy Mental confusion with psychomotor activity. Progressive drowsiness, stupor & coma. Wing-flapping tremor (asterixis). Fluctuating rigidity of the trunk & limbs. Grimacing. Suck & grasp reflexes. Hyperreflexia & Babiniski sign. Focal or generalized seizures. Concentrations of blood ammonia (NH3) > 200 µg/dL. EEG changes: Paroxysms of bilaterally synchronous slow or triphasic waves in the delta range, more frontally. Pathogenesis of Hepatic Encephalopathy The most accepted hypothesis relates hepatic coma to an abnormality of Nitrogen metabolism, wherein Ammonia (NH3), which is formed in the bowel by the action of urase-containing organisms on dietary protein, is carried to the liver in the portal circulation but fails to be converted to urea, either because of hepatocellular disease, or portal-systemic shunting of blood, or both → excess amounts of ammonia reach the systemic circulation, where they interfere with cerebral metabolism. Treatment of Hepatic Encephalopathy General Principles: Restriction of dietary protein. Oral Neomycin or Kanamycin to reduce bowel flora. Enemas. Lactulose orally → acidification of colonic contents. Liver transplantation for intractable liver failure. Other therapies: Bromocriptine (Parlodel) -a dopamine agonist-enhance dopaminergic transmission. Keto-analogues of essential amino acids -a nitrogen-free source of essential amino acids. 372 Elimination of predisposing factors: Avoid sedatives, tranquilizers, & analgesics Correct fluid & electrolyte balance Correct hypokalemia & alkalosis. Avoid potassium-wasting diuretics Maintain intravascular volume to prevent prerenal azotemia Treat hyponatremia promptly but cautiously (to avoid central pontine myelinolysis) A careful search for occult infection; e .g. peritonitis, & treatment of any infection Acute inflammation (e .g pancreatitis), trauma, & surgery Supportive measures: Foley’s catheter, skin care, fluid balance. Tracheal intubation in deeply comatose. Dietary protein restriction: Protein – free diet until improvement of neurologic function; Feeding; oral, NGT, or parenteral. Enough calories (at least 500 kcal/day) to inhibit proteolysis (1500 ml of 10% D/W → 600 kcal). A mixture of 10 %or 20% D/W & lipids via NGT to give 1500 – 2000 kcal/day . Cathartics on admittance Mg citrate, 200 ml, or Sorbitol, 50 gm in 200 ml water via NGT or PO GI bleeding may precipitate hepatic coma: Vigorous treatment of GI bleeding Aspirate bl.in stomach through a NGT Enemata followed by cathartics Repeated doses of Sorbitol, 50 gm in 200ml water to one loose motion q4 hrs. Adequate vit. supplementation, ê daily doses of folate, 1mg, vit.k, 10mg, & multivitamins. As the pt improves, a diet of 20 gm protein/day is provided, & daily protein intake by 10 gm every 2 – 3 days (up to 50 gm/day) Decrease gut ammonia absorption: Neomycin, 1gm qid PO, or by retention enema. It may → Hearing loss, renal impairment, colitis, candidiasis of bowel, & malabsorption. Lactulose, 30-50ml (0.65gm/ml) tid PO, by NGT, or by retention enema → acidify the stool & ammonia absorption. Flumazenil (Anexate), an inverse agonist of the benzodiazepine receptor, 1-3 mg by IV infusion, may reverse some of the neurologic effects. L–Dopa have no long-term benefit in pts ê hepatic encephalopathy. Monitoring Therapy: Hepatic Encephalopathy Stages: Stage 1 (Precoma): Mild confusion & mental slowness. No asterixis or EEG slowing Stage 2 (Impending coma): Disorientation, drowsiness, asterixis ± mild EEG slowing Stage 3 (Pt is asleep most of the time, confused + asterixis + EEG slowing Stage 4 (Coma): Pt responds only to pain + hypotonia + marked EEG slowing In mild stages of encephalopathy, a handwriting chart & tests of constructional ability (e.g. drawing a clock or constructing a star ê match sticks) Blood ammonia levels correlates ê clinical status. Arterial levels correlate better than venous levels. EEG slowing correlates ê the pt’s clinical status in deeper stages of hepatic 373 encephalopathy. Abnormalities in VERs have a similar correlation CSF glutamine concentrations correlates with the presence & degree of hepatic encephalopathy. Chronic Management: Low– protein diet (usually 50 gm/day) + Vit. supplementation. Pt should have at least one bowel motion each day. Neomycin, 500 mg PO bid – qid for a few wks or even months. Lactulose (Duphalac), 10 – 30 ml tid, is equally effective & safer. Surgical exclusion of the colon from the bowel → high mortality & morbidity. ACQUIRED CHRONIC HEPATOCEREBRAL DEGENERATION (ACHD) Clinically: → dementia, dysarthria, cerebellar ataxia, tremor, spastic paraparesis, & choreoathetosis. Often superimposed on recurrent bouts of hepatic encephalopthy. Treatment: No specific treatment It is preventable through appropriate management of liver disease & prevention of bouts of hepatic encephalopathy Choreoathetosis respond to neuroleptics. Behavioral abnormalities respond to protein restriction. Bromocriptine (Parlodel) - a dopamine receptor agonist improves mental status. It is givenPO, 2.5 mg/day in 3 or 4 divided doses, by 2.5 mg every 3 days up to 15 mg/day, improves mental status. ACUTE LIVER FAILURE Clinically → CNS dysfunction, coma & death, if not treated Treatment: Bl. ammonia by protein restriction + neomycin or lactulose Mannitol 20% for ICP IV dextrose to correct hypoglycemia HEPATOLENTICULAR DEGENERATION (Wilson’s disease) An autosomal recessive disorder of copper metabolism Clinically: → liver cirrhosis & cerebral dysfunction → movement disorders, tremor, & personality changes Treatment: discussed in Chapter II “Movement Disorders”. Fulminant Hepatic Failure Acute Hepatitis → Confusion, delirium & coma Cerebral edema is a prominent finding in all cases Cerebral edema is detected by CT scan Monitoring the ICP, osmotic diuresis & hyperventilation can prevent death from cerebral edemas 374 HEART & BRAIN (NEUROCARDIOLOGY) Cardiac sympathetic nerves arise from cells in the dorsal root ganglia (DRG) at T1 - T5 levels & enter the sp. cord via T 1 - T5 roots. Fibers ascending from the thoracic sp. cord toward the thalamus also project to NTS & other cardiovascular nuclei. Axonal projections from NTS terminate on preganglionic parasympathetic neurons in the dorsal motor nuclei of vagus & nuclei ambiguous, on preganglionic sympathetic neurons in the intermediolateral columns, & on cells in the ventrolateral medulla & raphe nuclei that regulate the cardiovascular system (CVS) by modulating activity of the sympathetic cells. The cerebral cortex projects to NTS both directly & via limbic system, hypothalamus, or parabrachial nuclei. Neural Control of The Heart Neuroanatomy of Cardiovascular Regulation Cardiac Afferents Both the vagus (parasympathetic) & the sympathetic nerves carry afferent nerve fibers from the heart. Mechanoreceptor & chemoreceptor endings of these nerves are located in the atria, ventricles, coronary vessels & pericardium. Vagal fs → cells in the nucleus tractus solitaria (NTS) in the medulla oblongata. Other afferents regulating heart rate are part of arterial baroreceptor & chemoreceptor reflexes. Those from aortic arch are carried in the vagus or aortic depressor nerves. Those from carotid sinus (baroreceptors) & carotid body (chemoreceptors) are carried in the carotid sinus & 9th nerves. Cardiac Efferents Preganglionic parasympathetic fs. originate in the nuclei ambiguus & pass via ipsilateral cardiac vagal ns. to the heart, to terminate on neurons of the intracardiac ganglia. Efferent preganglionic sympathetic fs. arise in the upper 4-5 thoracic segments of the sp. cord. Pregang. vagal & postgang. sympathetic fs. combine at the base of the heart to form the cardiac plexus. Parasympathetic fs. → Sinoatrial (SA) & AV node, where fs from the Rt. & Lt. vagus overlap. Rt. sympathetic ns. predominantly innervate the SA node. Lt. sympathetic ns. innervate the AV node. Autonomic Influences on Cardiac Function: Parasympatetic ns. discharge of SA nodal pacemaker. Sympathetic ns. exert the opposite effect. Parasymp. & sympath. contractility of atrial & ventricular myocardium. Parasymp. & sympath. AV nodal conduction. Cardiac vagal responses are mediated by Acetylcholine (Ach). Cardiac sympathetic responses are mediated by Norepinephrine (NE). 375 Sympath. & parasympath. outflow to the SA node is primarily influenced by arterial baroreceptors. Cardiac influences of the vagus & sympath. ns. are interdependent. Ach can inhibit the release of norepinephrine from sympath. fs. Norepinephrine can inhibit acetylcholine release from vagal fs. Thus, autonomic NS has powerful effects on cardiac conduction & contractility. The NS may contribute to control of coronary blood flow. A central pathway from lateral hypothalamus to neurons in the periaqueductal gray matter & thence to the rostral ventrolateral medulla that modulates cardiac sympathetic activity → modulation of coronary bl. flow. 376 Figure 2. Innervation of the Heart 377 1. 2. Autonomic neuropathies → cardiac denervation → fixed tachycardia. Primary neurologic disorders may cause ECG signs of ischemia & arrhythmias. Cardiac disease may coexist with ischemic strokes. The incidence of ECG changes is: 60-70% in pts. with IHD. 40-60% in pts. with SAH. 15-40 in pts with ischemic strokes. Stress alone can induce arrhythmias or sudden death. Intense release of catecholamines may be responsible for this. ECG Changes in CNS Disease Changes in ECG Morphology: LVH (evidence of chronic HTN). Pathologic Q waves (evidence of a prior MI). ST-T wave abnormalities (seen in subendocardial MI). QT prolongation. U waves. Mechanisms for Neurally-induced ECG Abnormalities MI associated with CAD. Diffuse MI in absence of CAD, 2ry to exposure to local catecholamines. Changes in ventricular repolarization 2ry to activation of the sympathetic NS, or direct stimulation of the thalamus & insula. Disturbances of Cardiac Rate & Rhythm: Sinus tachycardia / bradycardia. AF / A. Flutter (in 1/3 of pts with acute neurologic disorders). Atrial tachycardia. Premature atrial / ventricular complexes (PVCs). Intermittent AV node block. Nonsustained / sustained ventricular tachycardia. Neurally Induced Cardiac Damage Neurogenic Pulmonary Edema (NPE) Mechanism of NPE: Lt. atrial HTN. Systemic HTN. Pulmonary venoconstriction. Sympathetic overactivity. Sympath. n. stimulation → pulm. capillary permeability to protein. Sympath. n. stimulation may → lymphatic constriction. Pathogenesis of NS-Induced Pulmonary Edema: Two major causes: (1) Elevated intravascular pr. (2) Pulmonary capillary leak. Pulm. edema may follow epileptic seizures or éICP. The neuroeffector site for NS-induced pulm. edema is located in the caudal medulla, where nuclei regulating systemic arterial pr. & aff. & eff. pathways to & from the lungs are located. 378 Neurogenic Heart Disease Two categories of ECG changes are noted in neurologic disease: 1. Arrhythmias. 2. Repolarization changes. Mechanism of the Production of Neurogenic Heart Disease: Catecholamines levels. Stress + Steroids, via the hypothalamic sympathetic NS. NS stimulation e.g. stim. of hypothalamus. Reperfusion → myofibrillar degeneration, due to entry of Ca. Sudden Death: A Neurocardiologic Phenomenon A tight relation between brain activation of unbalanced autonomic function & arrhythmias, exists & ends in SCD. Insular & infralimbic cortex exert direct & indirect effects on hypothalamus & other brain stem nuclei in modulating cardiac sympathetic - parasympathetic interactions. Sympathetic hyperactivity → life-threatening cardiac arrhythmias Vagal activation exerts protective & antifibrillatory effects Epileptic activation of cortical brain sites can turn this system on, & incidence of unexpected death in epileptics. The role of environmental stress in arrhythmogenesis & SCD is of great importance in the outcome of Heart disease. Cardiac Arrhythmias & Syncope Bradyarrhythmias That Can Cause Syncope: Sinus node dysfunction → inappropriate sinus bradycardia or episodic sinus pauses. AV conduction disturbances → symptomatic bradyarrhythmias. Tachyarrhythmias That Can Cause Syncope: Supraventricular tachycardias. Ventricular tachyarrhythmias. Cardioneurogenic Syncope (Vasovagal Syncope = Vasodepressor Syncope = Reflex Syncope) It results from stimulation of the medullar vasodepressor region of the brain stem → parasympathetic tone (via vagus n.) & vasodilatation → Cardiac filling & bradycardia à syncope It is characterized by being: - Situational & recurrent, occurs in younger pts. - Preceded by prodromal symptoms (lightheadedness, ringing in ears, visual disturbances, diaphoresis, or nausea). - It occurs in upright position. - It is aborted by assuming the supine position. Cardiac Valvular Disease & Stroke Valvular heart disease may → Systemic embolization → Stroke. Antithrombotic therapy can but not eliminate this risk. The incidence of embolism in pts with rheumatic valvular diseases is decreasing. Mechanical & bioprosthetic valves may → thromboembolism. 379 Percutaneous balloon valvuloplasty for mitral stenosis & aortic stenosis may → embolic events. Surgical repair of the mitral valve the risk of embolic events. Aortic valve disease rarely causes systemic embolization. Emboli associated with aortic insufficiency occur in patients with endocarditis, AF, or coexistent mitral valve disease. Mitral valve disease frequently causes thromboembolism. The presence of AF the risk of thromboembolism by 3-7 times. Recurrent emboli occur in 30-65% of cases. The mortality rate may reach 42% in such patients. Anticoagulants are indicated in patients with rheumatic mitral valve disease particularly if associated with AF. Persistance of AF after surgery or balloon valvuloplasty requires continuous anticoagulation. Mitral valve prolapse affects 5-7% of adult population. It may cause cerebral ischemia by embolism of valvular thrombi. Long - term aspirin therapy is prophylactic against TIAs. Long - term warfarin is indicated in patients with mitral valve prolapse (MVP) & AF. Mitral annular calcification is more in females & the elderly & is associated with double mitral, calcific aortic stenosis, H.B., arrhythmias, endocarditis, & embolic stroke. Prophylactic anticoagulation should be reserved to patients with AF. Balloon valvuloplasty for mitral stenosis & aortic stenosis may → Systemic embolization → TIAs & strokes ? by calcific emboli. Prosthetic valves (mechanical or tissue prosthesis) may → Thromboembolism more with mitral valve replacement than with aortic. Life - long anticoagulation is needed in all patients. Mitral valve repair for mitral insufficiency the morbidity & mortality rates, & the risk of thromboembolism. Coronary Artery Disease, MI & Brain Embolism The incidence of in - hospital stroke after acute MI is 1%. Ischemic strokes are most common after large anterior wall MIs. Lt. ventricular thrombi are common after anterior wall MIs. High - dose anticoagulation prevents their formation. Aspirin is an alternative if anticoagulants are contraindicated. Mobile, pedunculated LV thrombi à high risk of embolization. Thrombi in LV aneurysms, probably do not require anticoagulation. Aspirin the risk of stroke after MI & should be given to all MI patients. t-PA treatment of MI → high risk of stroke than streptokinase due to excessive risk of cerebral hemorrhages. Neurologic Complications of Infective Endocarditis The overall incidence is 30%, mostly in patients with Lt-sided valvular disease. The incidence of CNS complications is higher with more virulent organisms. CT/MRI scanning are useful for diagnosis of CNS complications. Cerebral angiography is used in patients with suspected I.C. mycotic aneurysms. Appropriate antimicrobial therapy is mandatory 380 Aneurysm surgery may be needed for I.C. mycotic aneurysms. Anticoagulants should be continued in patients with prosthetic valve endocarditis, with no evidence of I.C. hemorrhage. They should be avoided in patients with native valve endocarditis because of the high risk of hemorrhagic CNS complications. Mortality rate is higher in patients with neurologic complications of infective endocarditis. Early diagnostic & therapeutic interventions will improve the outcome. Neurologic Complications of Congenital Heart Disease I. Spontaneous Neurologic Complications: 1. Rt - to - Lt Shunt Lesion: (e.g. Tetralogy of Fallot & Transposition of the great arteries). CVAs occur in 17-19% of patients, due to hypoxia & polycythemia. Arterial or venous thrombosis. A prolonged hypercyanotic spell → brain hypoxia → seizures. Clotting abnormalities → prolongation of prothrombin & thromboplastin time → hemorrhagic diathesis. CT/MRI are useful in diagnosis. 2. Silent Atrial Septal Defect (ASD): May → paradoxic thromboembolism → stroke or retinal ischemia. Transesophageal echocardiography is helpful in diagnosis. 3. Ventricular Septal Defect (VSD): May → paradoxic embolization. 4. Coarctation of the Aorta: It may à intracranial arterial aneurysms. Rarely ruptured aneurysm + HTN → SAH. Development of collateral vessels within the sp. canal → compression of the sp. cord → paraplegia, or may rupture → SAH. 5. Infective Endocarditis: May → infective emboli → stroke, more with left - sided valve affection. Two - dimensional echocardiography is helpful in diagnosis. 6. Brain Abscess: It is common with cyanotic C.H.D. with Rt.- to - Lt. shunt. Septic embolization from infective endocarditis & hematogenous dissemination from a nearby infection. 7. Pre-existing or Congenital Neurologic Problems: e.g. CNS abnormalities, chromosomal abnormalities. 8. Arrhythmia May → Dizziness, Lightheadedness, Syncope, Seizures. II. Neurologic Complications Related to Procedures: 1. Cardiac Catheterization: May → thromboembolism, air embolism, CNS hypoxia → seizures 2. Cardiac Surgery: May → thromboembolism, air embolism, hypoxia, metabolic derangement e.g. azotemia, hypoglycemia, hyponatremia, or hypocalcemia. Neurologic problems in early years include: seizures, impaired consciousness, hypotonia, hemiparesis, personality changes, & choreoathetosis. 381 Postoperative Neurologic Complications 1. Horner’s syndrome. 2. Vocal cord palsy. 3. Phrenic nerve palsy. 4. Spinal cord injury. 5. Subclavian steal syndrome. 6. Superior vena caval syndrome. Cerebrovascular Complications Associated With The Use of Artificial Circulatory Support Services Neurological complications are associated with the use of total artificial hearts & with ventricular support systems. They include thromboembolism → device - related strokes. Cardiac Arrhythmias & Stroke They → hypoperfusion & cerebral hypoxia AF → Thromboembolic strokes. AF pts should receive Warfarin or Aspirin 325 mg/d. CNS Complications In Coronary Artery Bypass Graft Surgery (CABG) CABG → CNS complications in 3.8% (altered mental state, stroke & seizures). Ophthalmoplegia, primitive reflexes, psychosis, depression, & brachial plexopathy may also occur. Minor cognitive impairment may follow CABG procedures. CABG encephalopathy is characterized by: a delay in emerging from anesthesia, agitation or restlessness, poor visual fixation, small reactive pupils, Babinski sign Post-CABG stroke occurs in 0.9-5.9% of cases, due to: - Macroemboli from the heart & atheromatous emboli from aorta. - Stroke prone pts those with CHF, elderly, carotid stenosis/bruit, TIAs. Hypotension: - Peri-operative hypotension is due to LVF, arrhythmias, or blood loss. - Operative hypotension is rare (in 2% of cases). BP of 50 mmHg is enough. - CABG encephalopathy reflects bilateral frontal lobe damage, & is due to hypoperfusion. Microemboli: - During CABG surgery, microemboli → microvascular occlusion → neurocognitive decline. - Cerebral & retinal microemboli are detected by TCD & retinal fluoroscein angiography. - Using “membrane oxygenators” is safer than “bubble oxygenators”. 382 NEUROCUTANEOUS DISORDERS Also known as Neuroectodermatoses or Phakomatoses (Phakos is the Greek word for lentil, mole; birthmark) The diseases customarily considered neurocutaneous syndromes are notable for their dysplastic nature & tendency to form tumors in various organs particularly the skin & nervous system Common types of phakomatoses include: 1. Neurofibromatosis (Von Recklinghausen disease) 2. Tuberous Sclerosis 3. Sturge-Weber syndrome (Encephalofacial angiomatosis) 4. Von Hippel-Lindau disease 5. Ataxia-telangiectasia 6. Incontininta Pigmenta The six diseases are considered the major phakomatoses & except for Sturge-Weber syndrome, all are inherited, although sporadic cases could occur. Each of these conditions is a distinct clinical entity, although there are scattered reports of “Double phakomatoses” or clinical overlap. The clinical spectrum ranges from frequent abortive forms “Formes frustes” to severe lethal conditions. Additional Neurocutaneous Syndromes Autosomal- Dominant Hemorrhagic telangiectasia (Osler-Rendu-Weber syndrome): Telangiectasiae of the skin & mucus membranes, particularly involving the face, ears, fingers, conjunctiva & nasopharynx, often associated with epistaxis. The lung, liver, GIT, bladder & brain are sometimes affected. Pulmonary arteriovenous fistulae & polycythemia can occur. Autosomal- Recessive Chediak-Hagashi syndrome: Partial albinism, photophobia, nystagmus & hepatosplenomegaly. Mental retardation, seizures & severe neuropathy are associated findings. Giant peroxidase-positive granules are found in polymorphonuclear leukocytes; functional abnormalities are noted in the platelets & leukocytes, & recurrent pyogenic infections can occur. Divry-Van Boegart syndrome: Cutis marmorata, leptomeningeal angiomatosis & leukodystrophy manifested as M.R & dementia, seizures, visual loss & spasticity. Meckel-Gruber syndrome (dysencephalic splachnocystica): Craniofacial anomalies include microcephaly, encephalocele, meningocele, ocular anomalies, & facial clefts. Associated cystic changes are found in the kidney, liver, &/or pancreas; skeletal anomalies may occur. Xeroderma pigmentosum: Cutaneous atrophy, telangiectasiae, & ulceration + extreme photosensitivity. Mental retardation, seizures, dysarthria & ataxia are present. Endocrine abnormalities. X-linked Albright syndrome (Polyostotic fibrous dysplasia): Short stature, brachydactyly, subcutaneous ossification, & large areas of cutaneous hyperpigmentation. Mental deficiency & seizure; precocious puberty is found in female. 383 Dyskeratosis congenita (Zinsser-Cole-Engman syndrome): Gray skin hyperpigmentation is particularly noted in the face, neck, & chest. Dystrophic nails with ridging Oral leukoplakia & hyperhidrosis. Excessive lacrimation. Fabry`s disease Punctate reddish-black skin eruption is commonly found about the hips,genitalia, & occasionally the face. Progressive cerebrovascular disease & renal disease & recurrent cerebral infarction. Sensory neuropathy with burning or shooting pains. Abnormal ceramide dihexosides & trihexosides. No Inheritance Recognized Cobb syndrome (Cutaneomeningeal angiomatosis) Cutaneous angiomas are associated with spinal angiomas at the corresponding spinal segment. NEUROFIBROMATOSIS (NF) (Von Recklinghausen Disease) Although Von Recklinghausen is credited with the initial clinical & pathological account of this disease in 1882, he cited Tilesius (1793) for the first description of a patient with multiple fibrous skin tumors. Wishart (1822) & Smith (1849) also provided clinical accounts of the disease before the report of Von Recklinghausen . Neurofibromatosis (NF) is a multisystem neurocutaneous disorder involving both neuroectodermal & mesenchymal derivatives, transmitted as autosomal-dominant trait. NF is notable for its great variability of clinical expression. The expression of this disease is highly variable, even within an affected family, ranging from mild inconvenience with normal lifespan, to serious & progressive manifestations leading to death as early as the perinatal period. The disease is autosomal dominant without predilection for sex, race, or color, & penetrance is complete Eight distinctive types of NF are recognized. At least 85% are represented by Type I (von Recklinghausen or Classic peripheral neurofibromatosis, with a prevalence of 1:4000 live births) & an additional 10% by Type II (Acoustic or Central neurofibromatosis, with a prevalence of 1:50000 live births). NF Subtypes: NF I: Classic or von Recklinghausen NF, Peripheral NF is an autosomal dominant form, characterized by multiple café-au-lait spots (six or more 1.5 cm diameter lesions in an adult), axillary freckling, numerous fibromas, & Lisch nodules or iris hamartomas. NF II: Acoustic or Central NF is an autosomal dominant form, characterized by an almost 100% incidence of bilateral acoustic neuromas. Cafe-au-lait spots tend to be few, very large, & pale. Few neurofibromas are present. Lisch nodules are absent. NF III: Mixed NF is an autosomal dominant form combining features of the above two forms: few large, pale cafe-au-lait lesions & more numerous cutaneous neurofibromas with higher frequency of CNS tumors, such as optic gliomas, neurilemomas, & meningiomas than found in NF I. NF IV: Variant NF is an autosomal dominant form in which cutaneous, acoustic & other CNS lesions may be present but that does not fit well into other groupings. 384 NF V: Segmental NF consists of unilateral localized distribution of either cafe-au-lait spots or neurofibromas, or both. There have been 15 reported cases. A post zygotic mutation restricted to somatic cells has been assumed to be responsible for most cases. However, in two cases of segmental disease, genetic transmission of the generalized disease has been reported. NF VI: This autosomal dominant form is characterized by cafe-au-lait spots but no cutaneous neurofibromas. NF VII: Late-onset NF is a form in which no signs of the disease appear before age 20, when neurofibromas may start developing. No cafe-au-lait spots have yet been reported. One reported case had a maternal uncle with neurofibromatosis. No offspring have yet been reported to develop neurofibromatosis. NF VIII: Unspecified NF includes those cases that do not fit into the above groupings. Genetics Transmission of NF is by an autosomal dominant mode of inheritance. In about 50%, the condition is due to a new mutation. Furthermore, advanced paternal age is associated with increased risk of new mutations. Patients born of affected mothers tend to have more severe expression of their disease than those born of affected fathers. The NF-1 gene has been localized to chromosome 17 at band q11.2. The NF-2 gene has been localized to chromosome 22 at band q12. Clinical symptoms & signs in NF Café au lait spots (Fig:1) Present in 95% of patients with neurofibromatosis (& 10-20% of normal individuals), are usually present at birth, but may appear up to the first year of age, often increasing in size & number over the first decade of life. They vary from few millimeters to few centimeters in size & are found commonly on the trunk than on limbs & not found on the scalp, palms or soles. Six or more macules are seen in 78% of NF-I patients. Pigmentation & size increase with aging. The cafe-au-lait spots of patients with neurofibromatosis are distinguished by the presence of more DOPA-positive melanocytes than surrounding normal skin, whereas similar macules in normal individuals, & in patients with other diseases associated with cafe-au-lait spots (such as McCune-Albright syndrome), contain fewer DOPA-positive melanocytes per square centimeter in their cafe-au-lait macules than in surrounding skin. Crowe's sign (Fig: 2) Axillary or inguinal freckling, appearing as 1-4 mm cafe-au-lait spots in the axilla or inguinal region, occurs in 20-50% of patients with NF. Blue-red macules & pseudoatrophic macules Generally occurring around the time of puberty, these lesions are slightly elevated to dome shaped, & may contain small blood vessels with the appearance of telangiectasia. Neurofibromas The appearance of neurofibromas is often associated with puberty. They may be few or many, & increase in size & number as the patient ages, or during pregnancy in affected female patients. Areolar neurofibromas are particularly common in post-pubertal females with NF. (Fig 3) Neurofibromas can develop at any time & at any location from the dorsal root ganglion to the terminal nerve twigs. They vary from a few millimeters to several centimeters & are more commonly found in trunk than limbs. The subcutaneous tumors, take two forms: 385 1. 2. Firm nodules attached to a nerve, An overgrowth of subcutaneous tissue, sometimes reaching enormous size. The latter, is called plexiform neuromas (also pachydermatocele, elephantiasis neuromatosis, la tumeur royale). (Fig: 4) When the hyperpigmentation overlies a plexiform neurofibroma & extends to the midline, one should suspect an intraspinal tumor at that level Lisch nodules (Fig: 5) Lisch nodules are the most common clinical feature of NF I, seen in 5% of children under 3 years of age, 55% of children 5-6 years of age, 94% of children older than 6 years, & 97 to 100% of postpubertal patients with peripheral neurofibromatosis II. Although they are not seen in normal individuals, the absence of Lisch nodules does not exclude the diagnosis. Seizures & intellectual compromise Neurologic disease is present in over 50% of affected individuals, including seizure, intellectual compromise, & tumors . Seizures occur in 8 – 13 % of patients, often associated with intracranial tumors . Intellectual impairment (including retardation, hyperactivity, learning disabilities, & speech impediments) occurs in 10 – 20 % of affected individuals, often with onset prior to school age ranging from mild to severe, but not progressive .While only 2-5% of affected patients will have mild mental retardation, 30 – 40 % will have speech pathologies . Optic involvement (Fig: 6) Eyelid ptosis in early childhood is a harbinger of eyelid neurofibroma or plexiform neuroma . Optic nerve gliomas, neurofibromas, schwannomas, & optic nerve sheath meningiomas may involve the globe & surrounding soft tissues . Optic gliomas tend to appear in the first decade, show sarcomatous degeneration, & have a perineural pattern of growth (unlike the intraneural pattern seen in similar lesions of non-NF patients). Glaucoma is a rare complication. Intracranial & spinal tumors The intracranial tumors associated with neurofibromatosis include optic gliomas, other astrocytomas, neurilemmomas, acoustic neuromas, neurofibromas, & meningiomas Spinal tumors are usually meningiomas or neurofibromas Malignancies (Fig: 7) Malignant degeneration of neurofibromas in NF may occur in 3 – 15 % of affected individuals .These secondary tumors are most often sarcomatous, although other forms have been reported . Other neoplastic entities, such as leukemia, malignant schwannoma, Wilms' tumor, & pheochromocytoma, have also been reported in increased association with neurofibromatosis . Osseous defects & congenital dislocations (Fig: 8) 50 % of individuals affected with neurofibromatosis may have osseous defects, including focal kyphoscoliosis, in more than 10% of NF patients, pseudoarthrosis, & dysplasia or thinning of the long bone cortex .These lesions all relate to neurofibromas near or within the affected bone . 386 Oral Pathology Pathologic oral lesions may occur in up to 72% of affected individuals . ommon associations include: neurofibromas of oral soft tissues (27%), enlarged fungiform papillae (32%), mandibular bony lesions (18%), widened inferior alveolar canal (27%), & enlarged mandibular foramina (27%). Endocrine disorders Early (most common) or late sexual maturation Menstrual abnormalities, Gynecomastia Acromegaly Hyper -or hypo-thyroidism Hyperparathyroidism Medullary thyroid carcinoma, Infertility Addison's disease Hypoglycemia Gastrointestinal involvement Complications related to mucosal bleeding overlying intestinal neurofibromas are reported in 10% of affected patients, & include dyspepsia, hematemesis, melena, obstruction & intestinal perforation . Hypertension Secondary hypertension is a frequent finding in adults with NF . The cause may either be renovascular, or pheochromocytoma, or both . In affected patients under 18 years of age, renovascular hypertension is a seven times more likely cause of hypertension than pheochromocytoma . The prevalence of pheochromocytoma in NF patients is 1:223, while the prevalence of NF in patients with pheochromocytoma is between 1:5 & 1:20 . Medical & endovascular treatments have, to date, had poor long-term outcomes. Surgical reconstruction remains the therapy of choice . Vascular anomalies (Fig: 9) Almost all children with NF develop vascular lesions, most commonly involving the abdominal aorta, & the renal, internal carotid & vertebral arteries, although any artery may be affected . NF is the most common genetically determined renovascular disorder in children . The renal artery stenosis, resulting from fibromuscular dysplasia of the media, often begins at the origin of the artery from the aorta, & may extend into the intrarenal branches. Features Listed For NF1 (Chromosome 17;q;11) Macrocephaly Macrodactyly Lipomata Absent or hypoplastic patella Adrenal tumors (excluding neuroblastoma) 387 Neurofibromas Asymmetric arms/forelimbs Optic atrophy Asymmetric legs/hind limbs Optic disc & nerve, general abnormalities Osteosclerosis or osteopetrosis Bifid/fused ribs Patchy depigmentation of skin Brain tumors/cysts Patchy pigment of skin/cafe au lait spots Pedunculated skin lesions/skin tags Fibrous dysplasia of bones Pigmentary abnormalities of iris Glaucoma Pseudoarthrosis Hemi-hypertrophy Ptosis of eyelids Hypertrophy of leg/hind limb Renal artery stenosis Hypertrophy of arm/forelimb Renal tumours (including Wilms') Iris, general abnormalities Axillary freckles Early puberty in male Features Listed For NF 2 (Chromosome(s) 22;q;12) Aplasia or dysplasia of retina Brain tumors/cysts Cataract Deafness, sensorineural Intra-cranial calcification Neurofibromas Patchy pigment of skin/cafe au lait spots Pedunculated skin lesions/skin tags Spinal tumors Diagnostic Criteria for NF1 Criteria for the diagnosis of NF 1 are met in an individual if two or more of the following are found: 1. Six or more cafe-au-lait macules over 5 mm in greatest diameter in prepubertal & over 1.5 cm in postpubertal individuals . 2. Two or more neurofibromas of any type, or one plexiform neurofibroma 3. Multiple freckles (Crowe's sign) in the axillary or inguinal regions . 4. A distinctive osseous lesion such as sphenoid dysplasia or thinning of long bone cortex, with or without pseudoarthrosis 5. Optic glioma. 6. Two or more iris hamartomas (Lisch nodules) on slit lamp or biomicroscopy examination. 7. A first-degree relative (parent, sibling, or offspring) with NF-I by the above criteria. 388 Diagnostic Criteria for NF2 1. CT or MRI evidence of bilateral internal auditory canal masses consistent with acoustic neuromas, 2. or A first-degree relative with NF-II & either: a. Unilateral eighth nerve mass or b. Two of the following: neurofibroma, meningioma, glioma, schwannoma, juvenile posterior subcapsular lenticular opacity. Complications of NF Disfigurement. Kyphosis &/or scoliosis. Malignancy Mental retardation, speech retardation, hyperacivity & seizures Large heads. Optic gliomas Hypertension Congenital defects of bone: Congenital absence of the orbital wall. Bowing of the leg bones below the knee (tibia or fibula). Differential diagnosis of neurofibromatosis: Characteristic cutaneous lesions: Watson's syndrome – autosomal disorder characterized by cafe-au-lait macules, pulmonary stenosis & intellectual compromise . Albright syndrome -polyostotic fibrous dysplasia with endocrine dysfunction & precocious puberty & somatic development . Multiple mucosal neuroma syndrome Leopard syndrome Characteristic tumors: Isolated optic glioma Multiple lipomatosis Solitary neurofibroma Isolated hemihypertrophy Management of NF: The multi-organ occurrence of neurofibromas & their complications often requires care from a variety of medical & surgical specialists. The physician should coordinate such care. Treatment is aimed at facing the complications as they occur. Some of the problems, such as renal artery stenosis, if detected early, can be managed successfully. Enlarging tumors can sometimes be managed by observation & surgery. If malignancies (including leukemia) develop, treatment is the same as for children without NF. 389 In the medical supervision of a child with NF, a number of areas require ongoing assessment & periodic review throughout life, including the following: Evaluate the child for new neurofibromas & progression of lesions. Examine the skin carefully for signs of plexiform neurofibromas that may impinge on or infiltrate underlying structures. Check the child's blood pressure. Because renal disease (particularly renal artery stenosis), aortic stenosis, pheochromocytomas (more common in adults) & adrenal tumors may occur, regular & careful blood pressure measurements are important. A variety of vascular hypertrophic lesions may be found. Evaluate neurodevelopmental progress. Evaluate the child for skeletal changes. Look for scoliosis, vertebral angulation, & limb abnormalities. Sometimes localized hypertrophy of a leg, arm, or other part of the body results from plexiform neurofibromata. If any complications occur or if neurocutaneous lesions appear to be rapidly advancing, refer to the appropriate specialist. Recommend available resources for patients with NF (e.g, NF clinics, support groups, & individual NF-1 families). TUBEROUS SCLEROSIS (TS) Bourneville & Brissaud (1880) First pathologic description of TS First to call the disease tuberous sclerosis First to relate cerebral sclerosis to the renal tumors Vogt (1908) Emphasized association of adenoma sebaceum & cerebral sclerosis Emphasized cardiac & renal tumors are constituents of TS Triad of: mental retardation (MR), seizures & adenoma sebaceum Tuberous Sclerosis A neurocutaneous syndrome characterized by cutaneous & manifestations (mental retardation & seizures), & tumors. Clinical triad is adenoma sebaceum, seizures, & mental retardation. Incidence: 1/30,000 Age of onset: 1st decade neurologic Genetics Familial - autosomal dominant with variable penetrance Rates of spontaneous mutation have varied but have been approximated as greater than 50% Genetic linkage studies of the gene for TS: - gene 1 chromosome 9q33-34 (TSC1) - gene 2 chromosome 11q23 (TSC 2) - gene 3 chromosome 12q23.3 (TSC 3) - gene 4 chromosome 16p13 (TSC 4) If 2 or more siblings have Tuberous Sclerosis (TS) then one parent always has at least one skin manifestation of TS If both parents are normal, the TS in a child is probably a new mutation Sporadic rate varies from 58-77% 390 Clinical features Clinical presentation is extremely variable depending on the age of the patient, which organs are involved, & the severity of involvement Clinical variability even within the same family Cutaneous Manifestations 1. Adenoma Sebaceum (80%) rarely present at birth usually presents between 4-6 years of age: - present in 12 % at 1 year - present in 33 % at 2 years - present in 40 % at 3 years are angiofibromas: - usually pink or red papules appearing in patches or in a butterfly-shaped distribution on or about the nose, cheeks, & chin - with time may enlarge, coalesce, & assume a fleshy appearance 2. Ash-leaf Spots (90%) hypopigmented oval or leaf-shaped spots vary in size from mm to cm vary in number from several to 75 or more found on the trunk & limbs in a linear orientation apparent at birth & seen prior to 2 years in 50% of patients visualized using a Wood's light (melanin absorbs wavelengths at 360 nm) represent depigmented macules in which the melanocytes are normal but the melanosomes are reduced in number & contain less melanin 3. Shagreen Patches (35%) isolated "leathery" raised & thickened plaques have an orange-peel consistency may be grayish-green or light brown in colour found over the lumbosacral or gluteal region develop in late infancy or early childhood but may also be present at birth may be preceded by patches of grey or white hair (these hairy patches may be the first manifestation of TS) 4. Others cafe-au-lait spots (7-16%) fibromas angiomas Neurologic Manifestations 1. Seizures (90%) most common symptom of TS initially present as infantile spasms: - 25-50% of patients with infantile spasms later develop signs of TS - can appear as early as 1 week of age later develop other types of generalized seizures: - tonic, clonic, myoclonic, akinetic, Lennox-Gastaut syndrome 2. Mental Retardation (60-70%) highly variable but when present is irreversible 391 may be initially normal but then deteriorate intellectually during the latter part of the 1st decade (secondary to seizure or increased intracranial pressure) The earlier the onset of seizures the greater the likelihood of mental retardation (if seizures begin <1 year of age a 92% chance of MR) all who have mental retardation (MR) have had seizures 33% of TS have normal intelligence 3. Others hydrocephalus: if tubers obstruct the foramina of Monro or the Sylvian aqueduct developmental delay may develop autistic features Tumors 1. Retinal (50-80%) a. Mulberry Tumor - a nodular astrocytoma of the retina on or about the optic nerve head - refractile, yellowish, multinodular cystic lesions b. Hamartomas - round or oval grey-yellow glial flat patches found centrally or peripherally - complications do not include papilledema or impaired vision 2. Renal (50-80%) 3. Heart (50%) 4. Cutaneous (20%) 5. Intracranial (15%) 6. Oral Investigations Imaging Studies (CT/ MRI) 1. Intracranial Calcifications (60%) - most reliable finding in TS is calcified subependymal tubers - also occur in the region of the foramina of Monro & periventricular regions - multiple scattered calcium deposits may vary in size up to several cm - occur as early as 5 months & become more prominent with time (typically around 3-4 years of age) - tubers which project into the lateral & 3rd ventricles may appear as "candle drippings" 2. Others - only 5% of patients with the clinical features of TS have normal CT's - may also identify cerebral atrophy, subependymal tumors, ventriculomegaly, & areas of diffuse demyelination EEG 1. Infantile Spasms - hypsarrhythmias, can persist up to 8 years of age 2. Generalized Seizures - generalized slow wave-&-spike activity or independent multifocal spike discharges 392 STURGE – WEBER SYNDROME (SWS) Most cases are sporadic, but affected siblings suggest autosomal recessive inheritance in some families. Most cases are sporadic, but affected siblings suggest autosomal recessive inheritance in some families. Schirmer (1860) initially described a patient with a facial vascular nevus who had associated buphthalmus but, he did not mention the CNS lesion. Sturge (1879) initially describe this syndrome by providing the clinical findings of 6 year-old girl with a facial nevus who also had angiomas of the lips, gingiva, palate, floor of the mouth, uvula, & pharynx. The child had buphthalmos & was hemiparetic, & Sturge suggested that she had a similar vascular nevus of the underlying brain. Weber (1929) Associated intracranial calcification was later described. Sturge-Weber syndrome A neurocutaneous syndrome characterized by facial nevus (port-wine stain, nevus flammeus), ipsilateral vascular anomalies & intracranial calcifications, & contralateral hemiparesis, hemianopia, & seizures Incidence: 1/50,000 Age of onset: - nevus (birth), - seizures (< l year) Genetics Most cases are sporadic, but affected siblings suggest autosomal recessive inheritance in some families. Other cases suggest an autosomal dominant pattern, with incomplete penetrance with marked variability of the clinical manifestations. The gene locus has not yet been mapped. Although a port-wine stain on the face is a relatively common malformation, occurring in about 3/1000, only 5% of affected infants have Sturge-Weber syndrome. Clinical features I. Cutaneous Manifestations Facial Nevus (Port Wine Stain) Capillary nevus that is flat & blanches on pressure, usually conforms to the sensory distribution of the 1st & sometimes the 2nd &/or the 3rd divisions of the trigeminal nerve. Some authors suggested that the distribution of facial angioma is determined by embryologic development of a facial cleft. The facial angioma can extend to other facial areas including the lips, gingiva, palate, tongue, pharynx, & larynx. Moreover, the neck, trunk & extremities can also be involved either ipsilaterally or contralaterally to the facial angioma II. Neurological Manifestations 1. Seizures - Contralateral partial or secondarily generalized seizures usually begin in the first year of life. Increase in frequency & severity do not correlate with the extent of cutaneous involvement - Recurring Todd's paralysis which requires longer periods to recover with eventual permanent paresis occurred in one third 2. Hemiparesis 393 - Gradually develops contralateral to the facial nevus associated with hemiatrophy of limbs, cortical sensory deficits & hemianopia spasticity with pyramidal signs 3. Mental Retardation - Progressive - ? role of seizures vs the disease process itself 4. Hemianopia III. Ocular Manifestations 1. Fundal Choroidal Angiomas - affected area has a dark color - dilated retinal veins, ectopia lentis, optic atrophy - homonymous hemianopia (33%) 2. Others - iris heterochromia - congenital (buphthalmos) or acquired glaucoma (25-50%) Investigations 1. 2. 3. 4. Skull X-Ray Intracranial calcifications in 90% (railroad track pattern) CT/MRI Leptomeningeal angiomatoses, atrophy of the cortex & calcification Cerebral angiography PET VON HIPPEL-LINDAU DISEASE (VHL) A neurocutaneous syndrome characterized by hemangioblastomas (cerebellar & retinal), visceral cysts, & tumors. Incidence: 1/36,000 Age of onset; any but usually in the 2nd decade Risk factors: familial - autosomal dominant chrom.#: 3p25-p26 gene: plasma membrane calcium-transporting ATPase isoform 2 (PMCA-2) gene penetrance is almost complete by age 65 with delayed & variable expression even within the same kindred Diagnostic criteria: 1. more than 1 hemangioblastoma in the CNS 2. one hemangioblastoma in the CNS + visceral cyst or renal carcinoma 3. any manifestation with a family history Clinical features: I. Neurological Manifestations 1. CNS Hemangioblastomas - 2% of all brain tumors - 7-10% of all posterior fossa tumors 2. Cerebellar Hemangioblastomas (83%) - mean age of onset is 32 yrs; before age 15 is rare 394 - may present with posterior fossa signs/symptoms associated with polycythemia in 10-50% of patients all children presenting with cerebellar hemangioblastomas have VHL disease 3. Spinal Cord - 2nd most frequent site of CNS hemangioblastomas - present with abnormalities of proprioception, gait, & bladder dysfunction II. Ophthalmologic Manifestations Retinal Hemangioblastomas (46%) may appear as early as the 1st decade but usually in 2nd (before the presentation of cerebellar hemangioblastomas) may be multiple & bilateral no sex predilection Vision unaffected (if tumor in periphery) Visual impairment may occur with: - macular involvement - intraocular hemorrhage - retinal detachment secondary to exudation III. Others 1. Visceral Cysts tend to progress & become apparent during adult life pancreatic (72%) renal (59%) hepatic (17%) epididymis (7%) 2. Other Tumors Pheochromocytomas (17%) Renal cell carcinoma (51%) Neurofibromatoses Multiple endocrine neoplasia syndrome Investigations CT/MRI Cerebellar hemangioblastomas appear as cystic lesions with a vascular mural nodule For visceral cysts & tumors Arteriography To visualize blood supply to hemangioblastomas ATAXIA TELANGIECTASIA (AT) It is characterized by progressive cerebellar ataxia, oculocutaneous telangiectasia, choreoathetosis, proclivity to pulmonary infections & immunoincompetence, associated with underdevelopment or absence of the thymus gland & lymphoreticular neoplasm. Incidence 1/40,000 Gene 11q22-23 autosomal recessive inheritance 395 Fig (1) Café au lait spot Fig 2: Crowe's sign 396 Fig 3:Areolar neurofibromas Fig 4:Plexiform neuromas 397 Fig 5: Lisch nodules Fig 6: MRI of Optic nerve Glioma 398 Fig 7: Sarcomatous degeneration of pelveic neurofibroma Fig 8: Osseous defects 399 Fig9: Vascular anomalies. There is middle aortic coarctation & stenosis of superior right renal artery, left renal artery & superior mesenteric artery 400