BIOGRAPHICAL SKETCH - Jacobs Institute of Women`s Health
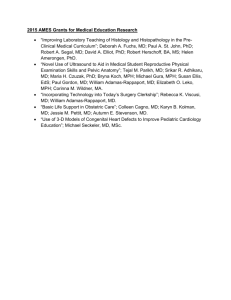
advertisement

Skip to main content o o o o o o o Home About About Milken Institute School of Public Health Leadership Message from the Dean Faculty Directory Administrative Offices Pressroom Events Jobs CEPH Self-Study GWSPH Source Admissions Graduate Admissions Undergraduate Admissions Admissions Visits Virtual Visits Deadlines Apply Academics Undergraduate Programs Graduate Programs Certificate Programs Online Programs Academic Advising Courses Practicum Graduation Academic Forms Academic Integrity Requirements Archive of Retired Programs Departments Environmental and Occupational Health Epidemiology and Biostatistics Exercise and Nutrition Sciences Global Health Health Policy and Management Prevention and Community Health Undergraduate Public Health Research Research Overview Organized Research Units SPH Office of Research Excellence Research Computing Resources Research Accelerator! Blog GW Office of the Vice President of Research Services For Students For Faculty For Alumni o o o Facilities Overview 950 New Hampshire Avenue 2175 K Street Directions and Parking Give Make a Gift Giving Opportunities Ways to Give Donors Making a Difference Frequently Asked Questions SPH Development Staff Search Search Search You are here Home HomeAboutAffiliated FacultyWomen’s Health IssuesNewsResearch ProjectsSchiffer FellowsContact Jacobs Institute of Women's Health Founded in 1990, the Jacobs Institute of Women’s Health works to improve women’s health through research, dialogue, teaching, and information dissemination. Our mission is to: Identify and study aspects of healthcare and public health, including legal and policy issues, that affect women’s health at different life stages; Foster awareness of and facilitate dialogue around issues that affect women’s health; and Promote interdisciplinary research, coordination, and information dissemination on women’s health issues. The Jacobs Institute focuses primarily on the health of U.S. women, while also collaborating with colleagues who work internationally. The Jacobs Institute promotes environments where an interdisciplinary audience – including healthcare professionals, researchers, policymakers, and advocates – comes together to discuss ways to advance women’s health. Affiliated Faculty Faculty from across the George Washington University are affiliated with the Jacobs Institute of Women's Health: Milken Institute School of Public Health Jeffrey (Bart) Bingenheimer, PhD, MPH Assistant Professor, Department of Prevention and Community Health Amanda D. Castel, MD, MPH Associate Professor, Department of Epidemiology & Biostatistics Program Co-Director, Master of Science in Public Health, Microbiology and Emerging Infectious Diseases Topic areas include: HIV among Women in Washington, DC (or nationally); Prevention of Mother to Child Transmission of HIV Mary A. Foulkes, PhD Research Professor, Biostatistics Center; Department of Epidemiology and Biostatistics; Department of Health Policy Mimi Ghosh, PhD Assistant Professor, Department of Epidemiology & Biostatstics Topic areas include: Biological mechanisms of sexual transmission of HIV in women; HIV immune responses in postmenopausal women; HIV immune responses in women experiencing sexual violence Jeanne A. Jordan, PhD Professor, Department of Epidemiology and Biostatistics Leighton Ku, PhD, MPH Interim Chair and Professor, Department of Health Policy and Management; Director, Center for Health Policy Research Topic areas include: Budget issues in health policy, immigrant health care, DC's health insurance exchange: DC Health Link Anne Rossier Markus, PhD, JD Associate Professor, Department of Health Policy and Management Leah Masselink, PhD Assistant Professor, Department of Health Policy and Management Melissa McCarthy, ScD, MS Associate Professor, Department of Health Policy and Management Karen McDonnell, PhD Associate Professor, Department of Prevention and Community Health; Director, DrPH Program in Health Behavior Topic areas include: HIV, DV, Substance Use, Poverty: Looking at women's health through a syndemic lens; Gender Based Violence (Latina, programs, community); Chronic Pelvic Pain: It's not all in my head Katherine (Holly) Mead, PhD Assistant Professor, Department of Health Policy and Management Melissa Perry, ScD, MHS Professor and Chair, Department of Environmental and Occupational Health Marsha Regenstein, PhD Professor, Department of Health Policy; Director, DrPH Program Naomi Seiler, JD Associate Research Professor, Department of Health Policy and Management Topic areas include: Affordable Care Act and public health; HIV policy; and public health law Peter Shin, PhD, MPH Associate Professor, Department of Health Policy and Management James Tielsch, PhD Professor and Chair, Department of Global Health Amita Vyas, PhD, MHS Assistant Professor, Department of Prevention and Community Health; Director, Maternal and Child Health Program Susan F. Wood, PhD Associate Professor, Department of Health Policy and Management and Department of Environmental and Occupational Health; Executive Director, Jacobs Institute of Women’s Health Topic areas include: Women's Health and Health Care Reform; Emergency Contraception: FDA Policy and Action; Family Planning Services at Community Health Centers Ami R. Zota, ScD, MS Assistant Professor, Department of Environmental and Occupational Health Medical Faculty Associates / School of Medicine & Health Sciences/ School of Nursing Jillian Catalanotti, MD, MPH Assistant Professor of Medicine and of Health Policy; Director, Internal Medicine Residency Program, School of Medicine & Health Sciences Jehan El-Bayoumi, MD Associate Professor of Medicine; Founding Director, Rodham Institute Medical Faculty Associates / School of Medicine & Health Sciences Topic areas include: Domestic Violence; Health Equity in DC; Medical Education Sara Imershein, MD, MPH Associate Clinical Professor, Department of Obstetrics & Gynecology, School of Medicine & Health Sciences Professorial Lecturer, Department of Prevention & Community Health, Milken Institute School of Public Health Topic areas include: Abortion in America: Patients, Politics and Procedures; Contraception: The Methods and the Madness; and From Population Control to Civil Rights: the History of the Reproductive Rights Movement Jennifer Keller, MD, MPH Associate Professor; Director, Residency Program, School of Medicine & Health Sciences Beverly K. Lunsford, PhD, RN, CNS-BC Director, Center for Aging, Health and Humanities; Director, Washington Area Geriatric Education Center Consortium (WAGECC); Assistant Professor, School of Nursing Whitney Pinger, CNM Director, Midwifery Services; Associate Clinical Professor, School of Medicine & Health Sciences Topic areas include: Cesarean Prevention; Midwifery Pearls: Evidence for Clinical Practice; Midwifery in general Global Women's Institute Manuel Contreras-Urbina, PhD Director of Research, Global Women's Institute Topic areas include: Methodological and Ethical Considerations in Research on GenderBased Violence; What Works to Prevent Gender-Based Violence?; International Agenda on Women's Rights Mary Ellsberg, PhD Director, Global Women’s Institute Columbian College of Arts & Sciences Affiliated faculty from the George Washington University's Columbian College of Arts & Sciences include: Rachelle S. Heller, PhD Director, Elizabeth J. Somers Women’s Leadership Program; Associate Provost for Academic Affairs, Mount Vernon Campus; Professor, Computer Science, School of Engineering & Applied Sciences Carly Jordan, PhD Program Coordinator, Women's Leadership Program, Science, Health & Medicine Cohort; Assistant Professor, Department of Biological Sciences Barbara Miller, PhD Professor of Anthropology and International Affairs; Director, Institute for Global and International Studies; Director, Culture in Global Affairs Research and Policy Program; Director, Global Gender Program Daniel Moshenberg, PhD Associate Professor, Department of English and Women's Studies Law School Naomi Cahn, JD Harold H. Greene Chair Topic areas include: Marriage Markets: Gender and Income Inequality; The Honor Commandment and Elder Care; Gender, Sexual Violence, and Post-Conflict Reconstruction Phyllis Goldfarb, JD, LLM Jacob Burns Foundation Professor of Clinical Law and Associate Dean for Clinical Affairs Joan S. Meier, JD Professor of Clinical Law Women’s Health Issues Women's Health Issues is a peer-reviewed, bimonthly, multidisciplinary journal of the Jacobs Institute. It publishes original research, systematic review articles, and commentaries on women's health care and policy. The journal seeks to inform health services researchers, social scientists, healthcare and public health professionals, and policymakers and to engage readers in the perspectives of multiple disciplines relevant to the study of women's health. WHI gives priority to scholarly articles that improve understanding of how social, healthcare, and policy factors relate to women’s health. It has a particular focus on women's issues in the context of the U.S. healthcare delivery system and policymaking processes, although it invites submissions addressing women's healthcare issues in a global context if relevant to North American readers. Chloe E. Bird, PhD is the journal’s Editor-in-Chief. The journal accepts unsolicited manuscripts, which are subject to peer review under the discretion of the editors. Current and past issues, author guidelines, and submission instructions are available at http://www.whijournal.com. Call for Papers: Policy Matters articles Special Collections and Supplements Gibbs Leadership Prize Call for Papers: Policy Matters articles The Editors and Editorial Board of Women's Health Issues invite article submissions for a new category of peer-reviewed manuscripts for the “Policy Matters” category. We invite authors to submit scholarly, thoughtful, and timely policy analyses related to various issues affecting women's health. These could include, for example: Policy implications of proposed legislation, regulations, judicial decisions at the federal, state, and local levels as they may affect women's health; Policy implications of current and future developments in programs integral to women's health (e.g., Medicaid, Medicare, community health, Healthy Start, WIC, family planning, public health, and private sector insurance coverage); Scholarly policy analyses of health and social issues affecting women's health from a historical perspective, e.g., the effects of delinking Medicaid from welfare and subsequent reproductive health choices, or the effects of state and national health reform efforts on women's health; and, Scholarly policy analyses that contribute to our understanding of how effective policy actions can improve the scope and quality of women's health care services and the organization, financing, and delivery of these services. “Policy Matters” submissions may contain recommendations for “next steps,” however a key peer review criterion will be the extent to which such recommendations are supported by the rigor and comprehensiveness of the supporting policy analysis. “Policy Matters” manuscripts should not exceed 3,000 words – charts and graphs are encouraged when appropriate. The journal continues to give priority to scholarly health services research articles that report the results of original research and that improve understanding of how social, health care, and policy factors relate to women’s health. We seek in particular research articles and commentaries that: Contribute to a better understanding of gender-based health services research and policy; and Document applied integration and implementation strategies that translate new clinical, health services, and health policy research findings into women's health care practice and policy. Special Collections and Supplements The journal's editors select some of our highest-quality articles for inclusion in the Editor's Choice Collection. These articles are free to read (no subscription required) on the Free Editor's Choice Collection page. Our Special Collections highlight previously published articles on specific topics. Recent collections address Women Veterans' Health and Women's Heart Health. In addition, we have published several special supplements on specific topics, including: Bringing Gender Home: Implementing Gender-Responsive HIV/AIDS Programming for U.S. Women and Girls Health and Health Care of Women Veterans and Women in the Military: Research Informing Evidence-based Practice and Policy Abortion, Reproductive Rights and Health: Highlights from the Charlotte Ellertson Social Science Postdoctoral Fellowship 2003-2010 Transforming Maternity Care: 2020 Vision for a High Quality, High Value Maternity Care System, Blueprint for Action and Proceedings from the Childbirth Connection 90th Anniversary Symposium Policy and Financing Issues for Preconception and Interconception Health Gibbs Leadership Prize The Charles E. Gibbs Leadership Prize is awarded annually to recognize excellence in research on women’s health care or policy. Priority is given to manuscripts that report the results of original research and that improve understanding of an important women’s health issue. Members of the staff and Editorial Board of Women’s Health Issues are not eligible. The prize includes a $1,000 award. All winning articles are available to read for free on the journal website. Women’s Health Issues Awards 2014 Gibbs Leadership Prize to Study on Sexual Behaviors and Bullying in High School Students The Editorial Board of Women’s Health Issues is pleased to announce that the Charles E. Gibbs Leadership Prize for the best paper published in Women's Health Issues in 2014 (Volume 24) has been awarded to Hailee K. Dunn, MPH, a PhD student in clinical psychology at the University of Rhode Island. Dunn's manuscript, “Association between Sexual Behaviors, Bullying Victimization and Suicidal Ideation in a National Sample of High School Students: Implications of a Sexual Double Standard,” was co-authored by Annie Gjelsvik, PhD; Deborah N. Pearlman, PhD; and Melissa A. Clark, PhD. The manuscript was published in Women's Health Issues Volume 24, Issue 5 (September/October 2014), pages 567-574. In the study, Dunn and her colleagues analyzed data on 13,065 high school students from the nationally representative 2011 Youth Risk Behavior Survey. They found that students who reported having engaged in sexual intercourse were more likely to report having been bullied (at school or electronically) over the past 12 months than students who did not report intercourse experience. They also found that girls who engaged in sexual intercourse were more likely to be bullied than were boys who engaged in sexual intercourse. Students of both genders who reported both engaging in intercourse and being bullied had more than five times the adjusted odds of depression and three times the adjusted odds of suicidal ideation when compared to students who reported neither of these experiences. The authors explain that their finding of a stronger association between sexual intercourse and bullying victimization in girls than in boys provides “some evidence that girls are held to different sexual standards than boys." They recommend that "schoolbased bullying interventions should address peer norms regarding sexual behaviors, attitudes toward the sexual double standard and more broadly, attitudes and norms regarding traditional gender roles held in U.S. culture." The Charles E. Gibbs Leadership Prize is awarded annually to recognize excellence in research on women’s health care or policy. Priority is given to manuscripts that report the results of original research and that improve understanding of an important women’s health issue. Members of the staff and Editorial Board of Women’s Health Issues are not eligible. The prize includes a $1,000 award. “The Editorial Board congratulates Hailee Dunn and her colleagues for producing a study that is methodologically strong and has clear policy implications,” said Chloe Bird, Editor-in-Chief of Women’s Health Issues. “It is an important contribution to the ongoing discussions about how best to prevent and address bullying in school.” Bird presented the prize to Dunn at the Gender & Health Interest Group session at the AcademyHealth Annual Research Meeting on June 13th, 2015. The Women’s Health Issues Editorial Board also designated two excellent manuscripts in 2014 to receive “Honorable Mention" recognition: “Selected Preconception Health Indicators and Birth Weight Disparities in a National Study” by Kelly L. Strutz, PhD, MPH; Liana J. Richardson, PhD, MPH; and Jon M. Hussey, PhD, MPH. Published in Volume 24, Issue 1 (January/February), pages e89– e97. “Maternal Morbidities and Postpartum Depression: An Analysis Using the 2007 and 2008 Pregnancy Risk Assessment Monitoring System” by Swathy Sundaram, PhD, MPH; Jeffrey S. Harman, PhD; and Robert L. Cook, MD, MPH. Published in Volume 24, Issue 4 (July/August), pages e381–e388. The Charles E. Gibbs Leadership Prize was established to honor the founding President of the Board of Governors of the Jacobs Institute of Women Health. Charles E. Gibbs, MD (1923–2000) was a Fellow of the American Congress of Obstetricians and Gynecologists (ACOG) and past chair of ACOG’s Committee on Health Care for Underserved Women, the Task Force on the Voluntary Review of Quality of Care, the Health Care Commission, and the Task Force on Maternal Health Policy. Dr. Gibbs served on the Jacobs Institute of Women Health Board of Governors from 1990–1999 and was instrumental in shaping the Institute’s mission and structure. Previous winners of the Gibbs Prize include: Cynthia A. LeardMann, MPH (2013) Nathan L. Hale, PhD (2012) Jacqueline L. Angel, PhD (2011) Diana Greene Foster, PhD (2010) Paula Lantz, PhD (2009) Sherry Glied, PhD (2008) Richard C. Lindrooth, PhD (2007) Joan S. Tucker, PhD (2006) JiWon R. Lee, MS, RD, MPH (2005) Dawn M. Upchurch, PhD (2004) Sherry L. Grace, PhD (2003) Sarah Hudson Scholle, DrPH (2002) Sandra K. Pope, PhD (2001) Ilene Hyman, PhD (2000) Usha Sambamaoorthi, PhD (1999) Claire Murphy, MD (1997) Barbara A. Bartman, MD, MPH (1996) News Recent news: December 22, 2015: Women's Health Issues Launches 25th Anniversary Special Collection December 15, 2015: New Study in Women’s Health Issues: Gender Differences in Treatment of Acute Coronary Syndrome Patients December 15, 2015: Gibbs Leadership Prize: Best Manuscript of 2015 in Women's Health Issues December 2, 2015: New White Paper on Medication Abortion Provides Overview on Research and Policy November 19, 2015: Susan F. Wood and Diana Zuckerman Author Washington Post Oped on 21st Century Cures Act November 12, 2015: New Featured Study in Women’s Health Issues: Long-acting Reversible Contraception in the Postpartum Period October 20, 2015: Women’s Health Issues Commentary: Proposed Planned Parenthood Funding Cuts Would Harm Women in Medically Underserved Communities October 13, 2015: Workplace Accommodations for Breastfeeding Mothers Fall Short, According to New Study in Women’s Health Issues September 29, 2015: New Study in Women’s Health Issues: Health of Postmenopausal Women Veterans September 9, 2015: New Study in Women's Health Issues: Alzheimer’s Puts Heavier Economic Burden on Women August 26, 2015: New Study in Women’s Health Issues: Screening Mammography in a Public Hospital Serving Predominantly African-American Women August 19, 2015: New Commentary in Women's Health Issues: Advancing Women’s Heart Health July 27, 2015: New Study in Women's Health Issues: Alcohol Use and Unintended Sexual Consequences June 16, 2015: Women's Health Issues Awards 2014 Gibbs Leadership Prize to Study on Sexual Behaviors and Bullying in High School Students May 6, 2015: New Study in Women's Health Issues: Trauma-Informed Primary Care April 15, 2015: New Study in Women's Health Issues: Sex Differences in Home-Based Care January 28, 2015: Women's Health Issues Launches Special Collection on Women's Heart Health December 22, 2015 Women's Health Issues Launches 25th Anniversary Special Collection WASHINGTON, DC (December 22, 2015) — The peer-reviewed journal Women's Health Issues (WHI) today released a new Special Collection of articles on women’s health in celebration of its 25th anniversary. The 25th Anniversary Collection includes a sample of some of the best work the journal has published since its launch in 1990, all of which are free to read for the next 30 days. “This collection showcases the breadth and high quality of the work Women’s Health Issues has published over the past 25 years,” said Chloe E. Bird, editor-in-chief of Women’s Health Issues and senior sociologist at RAND. “The selected articles address a wide range of factors that affect women’s health outcomes, from experiences of violence to healthcare services. What they have in common is findings that healthcare providers, policymakers, and others can use to help women lead healthier lives.” Women’s Health Issues is the official journal of the Jacobs Institute of Women’s Health, which is based at the Milken Institute School of Public Health at the George Washington University. It is dedicated to improving the health and health care of all women throughout the lifespan and in diverse communities, and seeks to inform health services researchers, healthcare and public-health professionals, social scientists, policymakers, and others concerned with women's health. Studies in the 25th Anniversary Collection address health conditions from HIV to heart disease; disparities in care and health outcomes; specific populations, from veterans to women with disabilities; reproductive health; healthcare costs and financing; and more. The collection does not include articles that have won the journal’s annual Charles E. Gibbs Leadership Prize, which already receive special recognition and are continually accessible for free. Anniversary collection articles will be free to read until January 22, 2016. “As this collection makes clear, Women’s Health Issues has benefited enormously from the talent and expertise of our authors, peer reviewers, and editorial board members,” said Bird. “We are deeply grateful to everyone who has contributed so much to this journal over the past 25 years.” December 15, 2015 New Study in Women’s Health Issues: Gender Differences in Treatment of Acute Coronary Syndrome Patients WASHINGTON, DC (December 15, 2015) – Women admitted to hospitals in the Australian state of Victoria with acute coronary syndrome (ACS) were less likely to receive coronary interventions, found a study published today in the journal Women’s Health Issues, the official journal of the Jacobs Institute of Women’s Health, which is based at Milken Institute School of Public Health at the George Washington University. Linda Worrall-Carter, of Her Heart Ltd and Australian Catholic University, and her colleagues analyzed data on all 28,295 patients admitted to Victoria hospitals with a first-time primary diagnosis of ACS between June 2007 and July 2009. They report that women, who accounted for 36 percent of the patients, were less likely than men to receive three common kinds of invasive coronary interventions: angiograms, percutaneous coronary intervention (PCI), and coronary artery bypass graft (CABG). Worrall-Carter and her colleagues examined several factors that can affect treatments and outcomes in ACS patients, including the number of other health conditions recorded for each patient and the type of ACS. They categorized patients as having either STEMI (ST-segment elevation myocardial infarction) or NSTEACS (non–STsegment elevation ACS, which includes non-STEMI and unstable angina). Compared to men, they found women were more likely to be age 75 or older, have multiple other health conditions, and be diagnosed with NSTEACS. Even after adjusting for factors such as age, other health conditions, and type of ACS, Worrall-Carter and colleagues found that women were around one-half as likely to be treated with an invasive coronary intervention – and the in-hospital death rate was higher in patients who did not receive these interventions. While their unadjusted analysis found a higher rate of in-hospital death for women, the difference disappeared after adjustment. The frequent decision to not refer women ACS patients for angiography means that clinicians may miss opportunities to provide early revascularization treatment, the authors warn. They conclude, “Clinicians should be wary of inherent gender bias in decisions to refer patients for angiography.” The article, “Gender Differences in Presentation, Coronary Intervention, and Outcomes of 28,985 Acute Coronary Syndrome Patients in Victoria, Australia,” appears in the January/February 2016 issue of Women’s Health Issues. December 15, 2015 Gibbs Leadership Prize: Best Manuscript of 2015 in Women's Health Issues The Editorial Board of Women’s Health Issues is pleased to announce that the Charles E. Gibbs Leadership Prize for the best paper published in Women's Health Issues in 2015 (Volume 25) has been awarded to Miao Jiang, PhD, a research fellow at the Harvey L. Neiman Health Policy Institute and adjunct faculty member with the Department of Health Administration and Policy, George Mason University. Jiang's manuscript, “Screening Mammography Rates in the Medicare Population before and after the 2009 U.S. Preventive Services Task Force Guideline Change: An Interrupted Time Series Analysis,” was co-authored by Danny R. Hughes, PhD and Richard Duszak Jr., MD. The manuscript was published in Women's Health Issues Volume 25, Issue 3 (May/June 2015), pages 239–245. The study explores how new guidelines on screening mammography released by the US Preventive Services Task Force (USPSTF) in 2009 may have affected screening mammography among women ages 65 and older. Jiang and her colleagues used Medicare fee-for-service claims data from 2005 through 2012 for a 5% random sample of beneficiaries. They found that rates of screening mammography had been increasing for all Medicare beneficiaries ages 65 to 90 prior to the 2009 guideline change. After the guidelines’ release, they found an immediate and significant decrease in screening of 1.76 per 1,000 women. By comparison, they found that use of two other preventive services, Pap tests and routine eye examinations, did not show any similar shift during the time period under study – suggesting that the drop in screening mammography is likely associated with the USPSTF guideline change. Screening mammography rates decreased immediately after the guideline change for all age groups studied, Jiang and her colleagues found; three years later, the rate stabilized for those aged 65 to 74, and continued to decline for those aged 75 and older. The authors comment, "Behavioral changes should be anticipated when professional organizations issue competing guidelines; their important public policy implications may impact distinct demographic groups differently, and their results may not be fully quantifiable for many years after their implementation." “The Editorial Board congratulates Miao Jiang and her colleagues for conducting a methodologically strong study that makes an important contribution to the ongoing debate over mammography screening guidelines,” said Chloe Bird, Editor-in-Chief of Women’s Health Issues. The Editorial Board also designated two manuscripts in 2015 to receive “Honorable Mention" recognition: “Understanding Disparities in Lipid Management Among Patients with Type 2 Diabetes: Gender Differences in Medication Nonadherence after Treatment Intensification” by John Billimek, PhD; Shaista Malik, MD, PhD; Dara H. Sorkin, PhD; Priel Schmalbach, PhD; Quyen Ngo-Metzger, MD, MPH; Sheldon Greenfield, MD; and Sherrie H. Kaplan, PhD, MPH. Published in Volume 25, Issue 1 (January/February), pages 6–12. “Why Are U.S. Girls Getting Meningococcal But Not Human Papilloma Virus Vaccines? Comparison of Factors Associated with Human Papilloma Virus and Meningococcal Vaccination Among Adolescent Girls 2008 to 2012” by Rebecca B. Perkins, MD, MS; Mengyun Lin, MPH; Rebecca A. Silliman, MD, PhD; Jack A. Clark, PhD; and Amresh Hanchate, PhD. Published in Volume 25, Issue 2 (March/April), pages 97-104. The Charles E. Gibbs Leadership Prize is awarded annually to recognize excellence in research on women’s health care or policy. Priority is given to manuscripts that report the results of original research and that improve understanding of an important women’s health issue. Members of the staff and Editorial Board of Women’s Health Issues are not eligible. The prize includes a $1,000 award. Previous winners of the Gibbs Prize include: Hailee K. Dunn, MPH (2014) Cynthia LeardMann, MPH (2013) Nathan L. Hale, PhD (2012) Jacqueline L. Angel, PhD (2011) Diana Greene Foster, PhD (2010) Paula Lantz, PhD (2009) Sherry Glied, PhD (2008) Richard C. Lindrooth, PhD (2007) Joan S. Tucker, PhD (2006) JiWon R. Lee, MS, RD, MPH (2005) Dawn M. Upchurch, PhD (2004) Sherry L. Grace, PhD (2003) Sarah Hudson Scholle, DrPH (2002) Sandra K. Pope, PhD (2001) Ilene Hyman, PhD (2000) Usha Sambamaoorthi, PhD (1999) Claire Murphy, MD (1997) Barbara A. Bartman, MD, MPH (1996) The Charles E. Gibbs Leadership Prize was established to honor the founding President of the Board of Governors of the Jacobs Institute of Women Health. Charles E. Gibbs, MD (1923–2000) was a Fellow of the American Congress of Obstetricians and Gynecologists (ACOG) and past chair of ACOG’s Committee on Health Care for Underserved Women, the Task Force on the Voluntary Review of Quality of Care, the Health Care Commission, and the Task Force on Maternal Health Policy. Dr. Gibbs served on the Jacobs Institute of Women Health Board of Governors from 1990–1999 and was instrumental in shaping the Institute’s mission and structure. December 2, 2015 New White Paper on Medication Abortion Provides Overview on Research and Policy A new white paper from the Bridging the Divide project at the Jacobs Institute of Women's Health provides a comprehensive and up-to-date overview and explanation of the evolving body of research on medication abortion. It also highlights laws that create barriers to providing medication abortion in accordance with the current evidence. In the 15 years since the Food and Drug Administration (FDA) approved the drug Mifeprex for medication abortions, knowledge about safe, effective, and accessible medication abortion practices has advanced substantially -- but in some states, restrictive laws prevent healthcare providers from adopting evidence-based practices. Mifeprex (known generically as mifepristone) is used in combination with misoprostol for medication abortions. Although medication abortions are highly safe and effective, with fewer than one percent of patients experiencing serious complications, the FDA label specifies drug dosages and a minimum of three clinical visits, and limits its use to women with pregnancies of 49 days or fewer. This is despite a robust body of evidence showing that lower doses and fewer visits result in better outcomes for patients and that the regimen is effective up to 70 days. The label also requires both prescribers and patients to sign formal medication-specific agreements. Research, reviewed and explained in this white paper, demonstrates that a lower dose of mifepristone is more effective and has fewer side effects; that women can safely take misoprostol at home rather than returning to the provider's office to receive it; and that medication abortions are safe and effective for pregnancies of up to 70 days. These and other variations, often referred to as "evidence-based regimens," are common, except where states mandate that providers adhere to the FDA label. Research is accumulating to support additional protocol variations that can improve women’s access and experiences. Currently, three states -- North Dakota, Ohio, and Texas -- require providers to follow the FDA label for medication abortion. These requirements exist, despite the common occurrence of off-label prescribing across all types of medicine, as drug labels often do not keep pace with research. Thirty-eight states require that medication abortions be provided by a licensed physician, despite substantial evidence that mid-level providers such as nurse practitioners can do so with comparable safety and efficacy, and 18 states require the clinician to be in the physical presence of the patient, even though research on medication abortions by telemedicine finds this process to be safe and effective. "Providers want to offer the highest quality of care based on the best available evidence, and patients should expect that, regardless of the state where they reside," said Susan F. Wood, PhD, Associate Professor and Director of the Jacobs Institute of Women's Health at the George Washington University’s Milken Institute School of Public Health. "We created this white paper to help advocates, policymakers, and the public understand what the research has found about ensuring women have access to safe, high-quality medication abortion care. This knowledge can help them address legislative proposals and policies on medication abortion." Bridging the Divide is a project of the Jacobs Institute of Women’s Health and brings together researchers, policy-makers, and policy advocates with an active interest in women’s and reproductive health issues in order to improve the impact of each community in advancing their common goals. Read the white paper: Medication Abortion: Overview of Research & Policy in the United States November 19, 2015 Susan F. Wood and Diana Zuckerman Author Washington Post Op-ed on 21st Century Cures Act Susan F. Wood, PhD, Executive Director of the Jacobs Institute, has co-authored with Diana Zuckerman of the National Center for Health Research the Washington Post oped "The 21st Century Cures Act could be a harmful step backward." November 12, 2015 New Featured Study in Women’s Health Issues: Long-acting Reversible Contraception in the Postpartum Period Two-thirds of North Carolina women who wanted to begin using an intrauterine device or contraceptive implant after giving birth had not received it at six weeks postpartum, often because they were told that they needed to schedule a separate office visit for insertion. These are among the findings from the Editor’s Choice study in the latest issue of the journal Women’s Health Issues, “Barriers to Receiving Long-acting Reversible Contraception in the Postpartum Period.” Women’s Health Issues is the official journal of the Jacobs Institute of Women’s Health, which is based at the Milken Institute School of Public Health at the George Washington University. In the study Matthew Zerden, of the University of North Carolina-Chapel Hill and WakeMed Health and Hospitals, and his colleagues analyzed responses from 324 women who completed a survey about contraception approximately six weeks after giving birth in an urban, not-for-profit hospital in Raleigh, North Carolina. The participants were part of a larger study on postpartum use of long-acting reversible contraception (LARC) methods, and all 324 expressed an interest in using an intrauterine device (IUD) or contraceptive implant, which have failure rates below one percent. The authors found that two-thirds (65%) of this study’s participants reported that they had not received LARC methods when they were contacted for the follow-up survey, which occurred after each woman’s scheduled six-week postpartum visit. The most common reasons were being told they would need to return for another visit to have the device inserted, missing the postpartum visit, or being unable to afford the IUD or implant. Zerden and his colleagues suggest that postpartum LARC use may increase if women can receive LARC before postpartum hospitalization discharge or if clinics are able to provide same-day insertion at the postpartum visit. An increase in LARC use, they note, can reduce unintended pregnancies and short interpregnancy intervals, which are associated with increased health risks for mothers and children. This study is one of several articles on postpartum contraception in the November/December 2015 edition of Women’s Health Issues: “Barriers to receiving long-acting reversible contraception in the postpartum period,” by Matthew L. Zerden, Jennifer H. Tang, Gretchen S. Stuart, Deborah R. Norton, Sarah B. Verbiest, and Seth Brody “Postpartum Contraception Use by Urban/Rural Status: An Analysis of the Michigan Pregnancy Risk Assessment Monitoring System (PRAMS) Data” by Katherine A. Starr, Summer L. Martins, Sydeaka Watson, and Melissa L. Gilliam “Geographic variation in characteristics of postpartum women using female sterilization” by Kari White, Joseph E. Potter, and Nikki Zite “Trends and Disparities in Postpartum Sterilization following C-Section, 2000-2008” by Ginny Garcia, Dawn M. Richardson, Kelly L. Gonzales, and Adolfo G. Cuevas October 20, 2015 Women’s Health Issues Commentary: Proposed Planned Parenthood Funding Cuts Would Harm Women in Medically Underserved Communities Eliminating federal funding for Planned Parenthood, as some members of Congress urge, would only make it harder for low-income women in medically underserved communities to obtain healthcare, warns a new commentary in the journal Women’s Health Issues. The piece notes that while the Affordable Care Act has allowed many women to gain insurance that covers contraception and other preventive care without cost-sharing, accessing healthcare services is still difficult for those in areas with few healthcare providers. The authors explain that if Planned Parenthood clinics were to close, many communities’ remaining providers would be unable to serve all of the clinics’ former patients – and some communities would be left without any safety-net provider at all. Women’s Health Issues is the official journal of the Jacobs Institute of Women’s Health, which is based at the Milken Institute School of Public Health (Milken Institute SPH) at the George Washington University. The commentary, "Turning Back the Clock on Women’s Health in Medically Underserved Communities," was co-authored by Sara Rosenbaum, JD, the Harold and Jane Hirsh Professor of Health Law and Policy at Milken Institute SPH, and Susan F. Wood, PhD, the Executive Director of the Jacobs Institute of Women’s Health at Milken Institute SPH. “Underserved communities need more healthcare providers, not fewer,” Rosenbaum said. “I have been working with community health centers for almost four decades, and I know how much they have achieved. But they don’t have the capacity to replace the high-quality reproductive healthcare that millions of women get from Planned Parenthood clinics today.” In the commentary, Rosenbaum and Wood highlight two federally funded providers that promote access to care for those with low incomes: Community health centers and Title X–funded family planning centers. Community health centers provide comprehensive primary care in medically underserved areas, while Title X centers offer family planning and other preventive reproductive health services. Both charge fees on a sliding scale to accommodate low-income patients. While both of these safety-net providers are present in some areas, many poorer communities have only one or the other. Funding cuts that result in Planned Parenthood clinics’ closures would leave many low-income women without a source of reproductive healthcare, the authors say. “Title X plays an essential role in US women’s health, and Planned Parenthood plays an essential role in Title X,” said Wood, who also noted that a US House of Representatives proposal would eliminate the Title X program completely. “Cutting federal funding for Planned Parenthood – or, even worse, for the entire Title X program – would be catastrophic for millions of women.” October 13, 2015 Workplace Accommodations for Breastfeeding Mothers Fall Short, According to New Study in Women’s Health Issues Fewer than half of breastfeeding mothers who returned to work after giving birth reported having access to time and space to express breastmilk at work, a new study found. This is despite a requirement in the 2010 Affordable Care Act that employers provide break time and private space for breastfeeding mothers. The study, "Access to Workplace Accommodations to Support Breastfeeding after Passage of the Affordable Care Act," has been published online ahead of print and will appear in the January/February issue of the journal Women's Health Issues. Lead author Katy Kozhimannil, of the School of Public Health at the University of Minnesota, and colleagues analyzed data from the Listening to Mothers III survey, a national survey of 2,400 women aged 18 to 45 who gave birth in U.S. hospitals in 2011 and 2012. They found that only 59 percent of breastfeeding women who returned to work postpartum had access to adequate break time, and only 45 percent had access to private space other than a bathroom to express breastmilk. Low-income women and single mothers were less likely to have access to either break time or private space to express breastmilk. The authors found that those mothers who did have access to workplace accommodations were more than twice as likely as those without these accommodations to exclusively breastfeed their baby for 6 months, as recommended by the American Academy of Pediatrics. The Affordable Care Act requirement to provide accommodations for breastfeeding mothers applies to all employers, although those with fewer than 50 employees can be exempted if providing such a space is a hardship. The study authors noted that efforts to fully implement and enforce the provisions of the Affordable Care Act would likely benefit low-income families and single mothers, the groups least likely to have access to workplace support for breastfeeding. September 29, 2015 New Study in Women’s Health Issues: Health of Postmenopausal Women Veterans WASHINGTON, DC (September 29, 2015)—A new study using data from the Women's Health Initiative found that risk of all-cause mortality was higher among postmenopausal women veterans than among postmenopausal non-veterans despite similar risk for postmenopausal cardiovascular disease, cancer, diabetes, or hip fractures. The study, "Prospective Analysis of Health and Mortality Risk in Veteran and Non-Veteran Participants in the Women’s Health Initiative," has been published online ahead of print and will appear in the November/December issue of the journal Women's Health Issues. The lead author of the study is Julie Weitlauf, Ph.D., Director of the Women’s Mental Health and Aging Core of the VISN 21 Mental Illness, Research, Education and Clinical Center of the Veterans Administration Palo Alto Health Care System and Clinical Associate Professor (Affiliated) of Psychiatry and Behavioral Sciences at Stanford University. She and her colleagues analyzed data from the Women's Health Initiative on postmenopausal women—141,009 non-veterans and 3,706 veterans—who were between ages 50 and 79 when they enrolled. Participants were recruited from 1993 to 1998 at 40 sites around the U.S., and this study uses follow-up data collected through 2011 with annual questionnaires and medical examinations. This is one of the first large-scale investigations of postmenopausal health among women veterans. Moreover, as nearly half of the veteran women participants in the Women’s Health Initiative are of ages consistent with eligibility for military service prior to the Vietnam war, this study represents one of the only to date to address postmenopausal health and mortality risk among the oldest generation of women veterans living in the U.S. today—those who served in World War II and the Korean War. Though examination of the mechanistic factors underlying heightened mortality risk among women veteran participants in WHI were beyond the scope of this work, the authors recommend that future research further explore risk factors such as smoking and specific forms of cancer affecting postmenopausal women veterans. "It is our hope that this work will encourage further research efforts that will further deepen our understanding of this unique population of women," they conclude. The full text of this article is available for free on the Women's Health Issues website. For more studies on women veterans, see the journal's 2014 Special Collection on Women Veterans' Health and the 2011 special supplement Health and Health Care of Women Veterans and Women in the Military. September 9, 2015 New Study in Women's Health Issues: Alzheimer’s Puts Heavier Economic Burden on Women Women are not only at greater risk of developing Alzheimer’s disease (AD) when compared to men; per capita, they also bear six times the cost of AD care that men do, reports a study published today in the journal Women’s Health Issues. Authors Zhou Yang of Emory University’s Rollins School of Public Health and Allan Levey of the Emory University School of Medicine used a lifetime perspective to calculate AD costs to women and men based on three factors: the probability of developing AD, the disease’s duration, and the required formal or informal care for the patients. Women’s greater cost burden, they report, is largely due to the informal care they deliver to family members with Alzheimer’s disease and the lack of Medicaid relief for caregiving. “As Baby Boomers age, Alzheimer’s disease and other forms of dementia will place a greater strain on our healthcare system and on families,” said Chloe E. Bird, PhD, editor-in-chief of Women’s Health Issues. “This study demonstrates the importance of policies to address the needs not only of patients but of caregivers, the majority of whom are women.” Women’s Health Issues is the official journal of the Jacobs Institute of Women’s Health, which is based at Milken Institute School of Public Health at the George Washington University. The article, "Gender Differences: A Lifetime Analysis of the Economic Burden of Alzheimer’s Disease," appears in the September/October edition of Women’s Health Issues. Yang and Levey used 2000-2010 data from the Medicare Current Beneficiary Survey, a nationally representative sample of Medicare beneficiaries that merges survey responses with Medicare and Medicaid claims data. They calculated costs for clinical care paid by Medicare; long-term-care (LTC) costs paid by Medicaid; out-of-pocket costs for care at home or in assisted living facilities; and the costs of informal, uncompensated care. When considering aggregate costs for the Baby Boom generation, care for women with AD costs more than care for men with AD across the lifetime, the authors found, with a women-to-men cost ratio of 1.5 for Medicare costs, 2.2 for Medicaid costs, and 5.8 for out-of-pocket payments for assisted living and home health care. By far the greatest difference is in the informal care, though: Yang and Levey, who initiated this study in consultation with the advocacy group WomenAgainstAlzheimer’s, report that women provide informal, uncompensated AD care worth 20 times the care from men. Some female caregivers are still in the workforce and must juggle unpaid care with job and other family responsibilities. Others are older and often struggling with health or economic problems of their own, yet still provide many hours of unpaid care to a spouse or other family members, the authors say. Alzheimer’s can last up to ten years, and caregiving can be physically and psychologically demanding as well as exact a financial toll that is often shouldered by women. Yang and Levey go on to note that advances to cure, prevent, or postpone the onset of AD would ease the disproportionate burden on women. They also urge policy reforms, including reforms to Medicare and Medicaid payments to meet the needs of AD patients and their families. “Public policy interventions that aim at curing or slowing the progress of AD, as well as those meeting the special home health care or long-term care need of the AD patients, will greatly benefit the welfare and economic status of women,” Yang says. To interview Zhou Yang contact Robin Reese at 404-727-9371 or robin.j.reese@emory.edu. August 26, 2015 New Study in Women’s Health Issues: Screening Mammography in a Public Hospital Serving Predominantly African-American Women Findings from a new study of women diagnosed with breast cancer at Grady Memorial Hospital in Atlanta suggest that low-income African-American women treated at urban public hospitals may benefit from the use of American Cancer Society (ACS) screening mammography guidelines rather than the most recent US Preventive Services Task Force (USPSTF) recommendations. This is among the conclusions from the Editor’s Choice study in the latest issue of the journal Women’s Health Issues, “Screening Mammography in a Public Hospital Serving Predominantly African-American Women: A Stage–Survival–Cost Model.” In the study Clara Farley, of Emory University School of Medicine, and her colleagues reviewed the charts of 274 women diagnosed with stage I, II, or III breast cancer at Grady Memorial Hospital from 2008 and 2010, and estimated cohort survival and costs under both observed and hypothetical scenarios. The study sample was 83% AfricanAmerican and 96% publicly insured or uninsured. For this group, the authors' simulation found that if the women had annual screening mammography beginning at age 40 (as the ACS guidelines recommend), more of the cancers would be caught sooner and more women would survive five years after diagnosis than if the women had screening mammograms every two years beginning at age 50 (as the USPSTF guidelines recommend). The USPSTF guidelines do state, "The decision to start regular, biennial screening mammography before the age of 50 years should be an individual one and take patient context into account." Women with an elevated risk of breast cancer may wish to discuss with their healthcare providers beginning screening mammography sooner or having it more frequently than the USPSTF guidelines advise. Farley and her colleagues note that research has found "wide ethnic and socioeconomic variations in breast cancer patterns," with African-American women being more likely than Caucasian women to be diagnosed with breast cancer at younger ages. They write that their study findings "support the continued use of ACS screening schedules in lowincome African-American women treated in urban public hospitals." The full text of this Editor’s Choice article is available for free on the Women’s Health Issues website. Editor’s Choice articles from past issues are listed on the Free Editor’s Choice Collection Page. August 19, 2015 New Commentary in Women's Health Issues: Advancing Women’s Heart Health Research and care for women’s heart health has improved substantially over the past three decades, but cardiovascular disease is still the top cause of death for US women. In a commentary published today in the journal Women’s Health Issues, Sharonne N. Hayes, MD and colleagues from the Scientific Advisory Council of WomenHeart: The National Coalition for Women With Heart Disease explore the recent advances and key unanswered research questions for women’s cardiovascular health. Women’s Health Issues is the official journal of the Jacobs Institute of Women’s Health, which is based at the Milken Institute School of Public Health (Milken Institute SPH) at the George Washington University. The commentary, "Taking a Giant Step Toward Women’s Heart Health: Finding Policy Solutions to Unanswered Research Questions," has been published online ahead of print and will appear in the September/October edition of Women’s Health Issues. Susan F. Wood, PhD, executive director of the Jacobs Institute and associate professor in the Department of Health Policy and Management at Milken Institute SPH, is a co-author of the paper. The authors recommend that policy change and research investment focus on answering three key questions, which address disparities in the occurrence and outcomes of cardiovascular disease in men and women; strategies to modify women’s risk of heart disease; and the biological variables that influence the development and outcomes of heart disease in women. These questions, they explain, will be central to the upcoming October 2015 National Policy & Science Summit on Cardiovascular Health, which WomenHeart is convening to bring together women with heart disease and leaders in women’s cardiovascular health. The goal, Hayes and her colleagues write, “is to develop a patient-centered holistic approach to sex- and gender-specific heart health that is supported by research and policies addressing women’s needs.” July 27, 2015 New Study in Women's Health Issues: Alcohol Use and Unintended Sexual Consequences Research has demonstrated the link between alcohol and unintended sexual consequences, but a better understanding of alcohol’s role in such events can improve efforts to reduce emotional and physical harms among women who experience these consequences. In a study published today in the journal Women’s Health Issues, Dinah Lewis and colleagues from the Johns Hopkins University School of Medicine report results from their study involving in-depth interviews with 20 women who attended a sexually transmitted infection (STI) clinic in Baltimore and reported recent binge drinking or engaging in intercourse while under the influence of alcohol. Study participants reported binge drinking in clubs increased their vulnerability to male targeting, often resulting in unintended sexual consequences. Women’s Health Issues is the official journal of the Jacobs Institute of Women’s Health, which is based at Milken Institute School of Public Health at the George Washington University. The article, "Alcohol Use and Unintended Sexual Consequences among Women Attending an Urban Sexually Transmitted Infections Clinic," has been published online ahead of print and will appear in the September/October edition of Women’s Health Issues. The authors’ analysis of the interviews identified five major unintended sexual events occurring while under the influence of alcohol: sex with new partners, often strangers; engaging in types of sexual activity that they would not engage in while sober; “blackedout sex,” or alcohol-related amnesia about sexual activities; unprotected sex; and rape. Interventions to reduce harm should involve both women and men, the authors suggest. They highlight particularly promising interventions that address the discrepancy between what women expect to occur when they drink and what may actually happen. June 16, 2015 Women's Health Issues Awards 2014 Gibbs Leadership Prize to Study on Sexual Behaviors and Bullying in High School Students The Editorial Board of Women’s Health Issues is pleased to announce that the Charles E. Gibbs Leadership Prize for the best paper published in Women's Health Issues in 2014 (Volume 24) has been awarded to Hailee K. Dunn, MPH, a PhD student in clinical psychology at the University of Rhode Island. Dunn's manuscript, “Association between Sexual Behaviors, Bullying Victimization and Suicidal Ideation in a National Sample of High School Students: Implications of a Sexual Double Standard,” was co-authored by Annie Gjelsvik, PhD; Deborah N. Pearlman, PhD; and Melissa A. Clark, PhD. The manuscript was published in Women's Health Issues Volume 24, Issue 5 (September/October 2014), pages 567-574. In the study, Dunn and her colleagues analyzed data on 13,065 high school students from the nationally representative 2011 Youth Risk Behavior Survey. They found that students who reported having engaged in sexual intercourse were more likely to report having been bullied (at school or electronically) over the past 12 months than students who did not report intercourse experience. They also found that girls who engaged in sexual intercourse were more likely to be bullied than were boys who engaged in sexual intercourse. Students of both genders who reported both engaging in intercourse and being bullied had more than five times the adjusted odds of depression and three times the adjusted odds of suicidal ideation when compared to students who reported neither of these experiences. The authors explain that their finding of a stronger association between sexual intercourse and bullying victimization in girls than in boys provides “some evidence that girls are held to different sexual standards than boys." They recommend that "schoolbased bullying interventions should address peer norms regarding sexual behaviors, attitudes toward the sexual double standard and more broadly, attitudes and norms regarding traditional gender roles held in U.S. culture." The Charles E. Gibbs Leadership Prize is awarded annually to recognize excellence in research on women’s health care or policy. Priority is given to manuscripts that report the results of original research and that improve understanding of an important women’s health issue. Members of the staff and Editorial Board of Women’s Health Issues are not eligible. The prize includes a $1,000 award. “The Editorial Board congratulates Hailee Dunn and her colleagues for producing a study that is methodologically strong and has clear policy implications,” said Chloe Bird, Editor-in-Chief of Women’s Health Issues. “It is an important contribution to the ongoing discussions about how best to prevent and address bullying in school.” Bird presented the prize to Dunn at the Gender & Health Interest Group session at the AcademyHealth Annual Research Meeting on June 13th. The Women’s Health Issues Editorial Board also designated two excellent manuscripts in 2014 to receive “Honorable Mention" recognition: “Selected Preconception Health Indicators and Birth Weight Disparities in a National Study” by Kelly L. Strutz, PhD, MPH; Liana J. Richardson, PhD, MPH; and Jon M. Hussey, PhD, MPH. Published in Volume 24, Issue 1 (January/February), pages e89– e97. “Maternal Morbidities and Postpartum Depression: An Analysis Using the 2007 and 2008 Pregnancy Risk Assessment Monitoring System” by Swathy Sundaram, PhD, MPH; Jeffrey S. Harman, PhD; and Robert L. Cook, MD, MPH. Published in Volume 24, Issue 4 (July/August), pages e381–e388. Previous winners of the Gibbs Prize include: Cynthia LeardMann, MPH (2013) Nathan L. Hale, PhD (2012) Jacqueline L. Angel, PhD (2011) Diana Greene Foster, PhD (2010) Paula Lantz, PhD (2009) Sherry Glied, PhD (2008) Richard C. Lindrooth, PhD (2007) Joan S. Tucker, PhD (2006) JiWon R. Lee, MS, RD, MPH (2005) Dawn M. Upchurch, PhD (2004) Sherry L. Grace, PhD (2003) Sarah Hudson Scholle, DrPH (2002) Sandra K. Pope, PhD (2001) Ilene Hyman, PhD (2000) Usha Sambamaoorthi, PhD (1999) Claire Murphy, MD (1997) Barbara A. Bartman, MD, MPH (1996) The Charles E. Gibbs Leadership Prize was established to honor the founding President of the Board of Governors of the Jacobs Institute of Women Health. Charles E. Gibbs, MD (1923–2000) was a Fellow of the American Congress of Obstetricians and Gynecologists (ACOG) and past chair of ACOG’s Committee on Health Care for Underserved Women, the Task Force on the Voluntary Review of Quality of Care, the Health Care Commission, and the Task Force on Maternal Health Policy. Dr. Gibbs served on the Jacobs Institute of Women Health Board of Governors from 1990–1999 and was instrumental in shaping the Institute’s mission and structure. May 6, 2015 New Commentary in Women's Health Issues: Trauma-Informed Primary Care Media Contact: Kathy Fackelmann, kfackelmann@gwu.edu, 202-994-8354 WASHINGTON, DC (May 6, 2015) — Patients with a history of trauma can benefit from working with healthcare providers who understand trauma’s role in health and can offer resources to assist with healing. A commentary published today in the journal Women's Health Issues proposes an approach to providing such trauma-informed primary care (TIPC). Edward L. Machtinger, MD, director of the Women’s HIV Program (WHP) at the University of California, San Francisco, and his co-authors identify four core components of a TIPC approach: environment, screening, response, and a robust organizational foundation. Women’s Health Issues is the official journal of the Jacobs Institute of Women’s Health, which is based at Milken Institute School of Public Health at the George Washington University. The commentary, "From Treatment to Healing: The Promise of TraumaInformed Primary Care," appears in the May/June edition of Women’s Health Issues. To develop the proposed framework, Machtinger and his colleagues drew on the work of the National Strategy Group to Develop a Model of Trauma-informed Primary Care, which WHP and the Positive Women’s Network—USA convened in 2013. Trauma is an especially important factor in women’s health. The landmark Adverse Childhood Experiences (ACE) study found that women were more likely than men to report a high number of adverse childhood experiences (including physical or sexual abuse, neglect, and household dysfunction). As adults, many women experience physical violence and/or rape from an intimate partner. For primary-care practices seeking to become trauma-informed, Machtinger and his colleagues recommend getting training on trauma and health for all staff members and creating a physical space that provides opportunities for privacy, confidentiality, and community. They suggest that practices routinely screen patients for trauma and, when patients disclose trauma, be prepared to respond supportively and offer specific steps such as safety assessments and referrals for community resources. A strong organizational foundation that includes respect for patient choices, support for staff, and local partnerships is essential, the authors explain. Practices adopting this kind of trauma-informed approach can partner effectively with trauma survivors for better health outcomes and quality of life, the authors say. About Women’s Health Issues: Women's Health Issues is the official publication of the Jacobs Institute of Women's Health, and the only journal devoted exclusively to women's health care and policy issues. The journal has a particular focus on women's issues in the context of the U.S. health care delivery system and policymaking processes, although it invites submissions addressing women's health care issues in global context if relevant to North American readers. It is a journal for health professionals, social scientists, policymakers, and others concerned with the complex and diverse facets of health care delivery and policy for women. For more information about the journal, please visit http://www.whijournal.com. About Milken Institute School of Public Health at the George Washington University: Established in July 1997 as the School of Public Health and Health Services, Milken Institute School of Public Health is the only school of public health in the nation’s capital. Today, more than 1,700 students from almost every U.S. state and 39 countries pursue undergraduate, graduate and doctoral-level degrees in public health. The school also offers an online Master of Public Health, MPH@GW, and an online Executive Master of Health Administration, MHA@GW, which allow students to pursue their degree from anywhere in the world. April 15, 2015 New Study in Women's Health Issues: Sex Differences in Home-Based Care Media Contact: Kathy Fackelmann, kfackelmann@gwu.edu, 202-994-8354 WASHINGTON, DC (April 15, 2015)—Are there differences in the quality of care provided to men and women receiving publicly funded home care services in Ontario, Canada? An article published today in the journal Women's Health Issues investigates this question, as well as differences between patient outcomes in the Canadian province's 14 health planning regions. In the study, Amanda T. Lo, of St. Michael's Hospital in Toronto, and her colleagues found while there were sizable differences in outcomes before adjustment, no important differences in outcomes between men and women remained after risk adjustment. This indicates that sex-specific strategies will be needed to improve the quality and outcomes of home care services. Women’s Health Issues is the official journal of the Jacobs Institute of Women’s Health, which is based at Milken Institute School of Public Health at the George Washington University. The article, "Sex Differences in Home Care Performance: A PopulationBased Study," was published online April 15, 2015 and will appear in the May/June edition of Women’s Health Issues. The study analyzed data from the Home Care Reporting System database collected on nearly 120,000 residents of Ontario 65 and older who received publicly funded home care service for 60 days or more between April 2009 and March 2010. It used four quality indicators to determine whether men and women were receiving the same quality of service: decline or failure to improve in the activities of daily living such as bathing, dressing and eating, cognitive functioning, symptoms of depression and pain control. The authors found there were important differences between men and women receiving home care in the health outcomes that matter to patients, such as pain and ability to care for themselves. But those differences disappeared when the quality indicators were risk-adjusted for clinical conditions such as mobility or dementia, or for caregiver stress. After risk adjustment there were geographic differences in quality of home care across Ontario’s 14 Local Health Integration Network health-planning regions. The authors note that the differences indicate the potential to improve home care services for both men and women. The full text of the article, "Sex Differences in Home Care Performance: A PopulationBased Study," is available on the Women’s Health Issues website. January 28, 2015 Women's Health Issues Launches Special Collection on Women’s Heart Health Media Contact: Kathy Fackelmann, kfackelmann@gwu.edu, 202-994-8354 WASHINGTON, DC (January 28, 2015)—Today the peer-reviewed journal Women's Health Issues (WHI) released a new Special Collection on Women’s Heart Health, with a focus on improving healthcare services to women at risk for cardiovascular disease. The special collection also highlights recent studies addressing social determinants of health and physical activity in women of different backgrounds. "Many people still don't realize that heart disease is the number one killer of women," said Chloe Bird, editor-in-chief of Women’s Health Issues and a senior sociologist at RAND. “Women should be getting treated for high blood pressure, high cholesterol, and other conditions that pose risks to their long-term cardiovascular health – but research is finding that education and healthcare still need to improve so women get the necessary preventive care.” Women’s Health Issues is the official journal of the Jacobs Institute of Women’s Health, which is based at Milken Institute School of Public Health at the George Washington University. This Special Collection includes 20 articles published between mid-2011 and early 2015. Several of the studies in the collection demonstrate the need to improve healthcare services to assure that both women and men receive appropriate care to control risk factors for cardiovascular disease. Two of the studies in the special collection analyzed data on veterans' health and found higher LDL cholesterol levels among women veterans than their male counterparts. A third found a greater proportion of women veterans with elevated LDL cholesterol levels, and concluded that individual patientlevel factors could only explain one-third of the difference. Researchers are working to identify reasons why women’s cholesterol might be more poorly controlled than men’s. A study involving veterans found that providers were less likely to order or adjust cholesterol medications for women veterans than for male veterans, while women were more likely than men to be unwilling to take such medications. And a study in the general population involving patients from seven outpatient clinics found that women and men received comparable care for diabetes and lipid management. However, more of the women reported that due to side effects or costs, they were not taking the lipid-lowering medications they were prescribed. Such findings fit with a previous report that concluded that gaps persist in our understanding of how cardiovascular disease affects women. That report noted that many questions still remain about gender differences in this arena, including how best to treat women with heart disease. The report authors, including Jacobs Institute of Women’s Health Executive Director Susan Wood as well as colleagues at the Mary Horrigan Connors Center for Women's Health & Gender Biology and the Kaiser Family Foundation, called for researchers to push forward with investigations of women and heart disease. Studies in this collection help address that need, Wood says. At the same time, additional education on what we do know about treating women with heart disease may be necessary to assure that healthcare providers are fully equipped to help female patients reduce their risk--and two studies in the collection address this. One study involved focus groups with obstetrician/gynecologist (OBGYN) residents and practicing physicians, and concluded, “Additional training, development of referral networks, and access to local and practice specific data are needed to support an increased role for the OBGYN in the prevention of cardiovascular disease in women.” A second report, one that evaluated the “Heart Truth” education campaign for healthcare providers, found that doctors and other health professionals who attended Heart Truth educational lectures improved their knowledge on cardiovascular disease prevention in women. “There is a growing understanding of the need to address heart disease in women,” said Bird. “As the studies in this collection show, though, we still need more research and education to assure that healthcare providers can provide the best care to both men and women, and for women to be able to work together with their healthcare teams to keep their hearts healthy.” The Women’s Health Issues Special Collection on Women’s Heart Health is available online, and all articles can be accessed for free during February 2015. A previous special collection addressed Women Veterans' Health. About Women’s Health Issues: Women's Health Issues is the official publication of the Jacobs Institute of Women's Health, and the only journal devoted exclusively to women's health care and policy issues. The journal has a particular focus on women's issues in the context of the U.S. health care delivery system and policymaking processes, although it invites submissions addressing women's health care issues in global context if relevant to North American readers. It is a journal for health professionals, social scientists, policymakers, and others concerned with the complex and diverse facets of health care delivery and policy for women. For more information about the journal, please visit http://www.whijournal.com. About Milken Institute School of Public Health at the George Washington University: Established in July 1997 as the School of Public Health and Health Services, Milken Institute School of Public Health is the only school of public health in the nation’s capital. Today, nearly 1,534 students from almost every U.S. state and more than 45 countries pursue undergraduate, graduate and doctoral-level degrees in public health. The school also offers an online Master of Public Health, MPH@GW, and an online Executive Master of Health Administration, MHA@GW, which allow students to pursue their degree from anywhere in the world. Research Projects The Jacobs Institute works with GW and external colleagues on the following projects: Confidential and Covered: Analysis of the challenges and opportunities facing Title X providers of family-planning services to low-income women, as they determine how best to maintain confidentiality while billing insurers for covered services (in partnership with the National Family Planning & Reproductive Health Association, funded by the DHHS Office of Population Affairs) Bridging the Divide: A project that brings together researchers, policy-makers, and policy advocates with an active interest in women’s health issues in order to improve improve the impact of each community in advancing their common goals (funded by an anonymous donor) ADVHOCAT: Accomplishments of the Domestic Violence Hotline, On-line Connections, and Text: Evaluation of the efficacy of support and resources provided by the National Domestic Violence Hotline and the National Dating Abuse Helpline (funded by the DHHS Administration for Children and Families) Evaluation of Make the Call, Don’t Miss a Beat Campaign: Evaluation of the DHHS Office on Women’s Health (OWH) “Make The Call, Don’t Miss A Beat” campaign, which aimed to increase women’s 9-1-1 calls in response to heart attack symptoms (funded by OWH) Recent past projects include the following: Teen Pregnancy Prevention/ Empowering Latino Youth: Study of the effectiveness of the “Be Yourself/ Sé Tu Mismo” intervention for reducing the teen pregnancy rate among Latino youth in Washington, DC and Montgomery County, Maryland (funded by the DHHS Office of Adolescent Health) Community Health Centers and Family Planning: Surveys of federally qualified health centers and their patients explore family-planning services that health centers provide and the challenges they face in doing so (funded by an anonymous donor) Achieving Healthy Weight Among Lesbian and Bisexual Women: Study of the effectiveness of “MOVE: Making Our Vitality Evident,” an intervention to help lesbian and bisexual women achieve and maintain healthy body weights (partnership between GW, the Mautner Project of Whitman-Walker Health, and Vanderbilt University, funded by OWH) Women's Health and Health Insurance Exchanges: Creation of resources to assist in the implementation of state health insurance exchanges developed under the Affordable Care Act, with a focus on preventive care for women, health disparities in women, and family planning and reproductive health (in partnership with the Mary Horrigan Connors Center for Women's Health and Gender Biology and the Henry J. Kaiser Family Foundation) Continuing Medical Education for Women’s Cardiovascular Health: Development of "Heart Truth" continuing medical education training modules for clinicians, based on 2011 American Heart Association Guidelines on Women a Cardiovascular Disease (funded by OWH) Legislative Training Program for NIH Research Scholars: Workshops on the federal legislative process and Congressional committees, laws, and proposals with major effects on women’s health for scholars in the NIH Building Interdisciplinary Research Careers in Women’s Health program (supported by the NIH Office of Research on Women’s Health) Schiffer Fellows Clara Schiffer Project on Women’s Health The Jacobs Institute of Women's Health is pleased to announce the establishment of the Clara Schiffer Project on Women’s Health, honoring the legacy of social-justice advocate and GW supporter Clara Schiffer. The Clara Schiffer Project will provide financial support for graduate students to participate in either student- and faculty-directed research designed to improve women’s health and facilitate communication around women’s health issues. Eligible students must be currently enrolled in either the MPH, MSPH, or MHA program or a relevant doctoral program (see requirements by student type below) and must not be full-time GW employees. Funding & Application Timeline Eligible students may apply for up to $5,000 in funding for a one-time award. The first award will provide support for research activities starting in the Spring 2016 semester. Applications for the Spring 2016 fellowship will be due November 16, 2015. Fellowship award announcements will be made in December 2015. Clara Schiffer Doctoral Fellows The Clara Schiffer Fellowship is available for doctoral students conducting dissertation research on a topic related to women’s health across the lifespan. The application for funding must be made just prior to proposal defense, for one year following proposal approval. Funding may be used for limited salary support (no more than 50% of total award) or supplies, travel, database acquisition, specific training requirements, and/or other dissertation-related costs. The doctoral dissertation and any papers generated from the research must acknowledge support from the Schiffer Fellowship and will be submitted to JIWH for posting on the website. Doctoral students may apply for up to $5,000 in funding for the entire project period. All funds must be spent within a single calendar year, and a written progress report (no more than 5 pages) must be provided at the end of the funding period; the full dissertation may serve in lieu of the progress report if it is completed and defended within the one-year funding period. During the funding period, doctoral fellows will also participate in regular roundtable discussions (approximately four times per year) with JIWH-affiliated faculty. These lunchtime roundtables will create an opportunity for mentoring and learning about ongoing research, while creating a community of fellows and faculty with ongoing connections. Additionally, fellows will participate in events dedicated to women’s health issues during the spring Public Health Week events (April 4-10, 2016). Doctoral Fellow Application Requirements Doctoral-level applicants must provide: An abstract from the proposed dissertation A brief essay describing the proposed research topic, student responsibilities, and brief explanation of how funds will be used; this essay should not exceed 500 words A current CV A copy of an official or unofficial transcript from GW A brief letter of support from the dissertation committee chair, which must include a statement about the feasibility of the proposed research project and a statement of support for the student and his/her work; letters should not exceed 500 words; no more than one letter will be accepted The student’s GWID Please combine all documents into a single PDF for submission. Letters from committee chairs should not be sent separately. Clara Schiffer Masters Fellows The Clara Schiffer Fellowship is available for masters level students (including joint degree students) working with faculty members as hourly research assistants on projects related to women’s health across the lifespan. Funding is available only for hourly work, up to 15 hours per week for up to 6 months. Students must contact faculty members in advance to establish their role on a research project directed by that faculty member. Students may create sub-projects within existing projects or may perform work already planned. At the completion of the fellowship, fellows must provide some type of written report detailing their work over course of the fellowship; this report may take the form of a manuscript, abstract, poster, or other format previously agreed upon with the fellow’s faculty preceptor. Research reports from fellows and faculty will be posted online to the Milken Institute School of Public Health/JIWH site and may also be submitted to the journal Women’s Health Issues. Upon request, students may delay project work for up to six months, but all project work must be completed within the calendar year (by the end of December). Projects with a focus on engaging community organizations or individuals in the community will be given priority in the application process. Projects/findings will be presented at GWSPH research day as poster presentations and made available on the JIWH website. During the funding period, fellows will also participate in regular roundtable discussions (approximately two times per semester) with JIWH-affiliated faculty. These lunchtime roundtables will create an opportunity for mentoring and learning about ongoing research, while creating a community of fellows and faculty with ongoing connections. Additionally, fellows will participate in events dedicated to women’s health issues during the spring Public Health Week events (April 4-10, 2016). Masters Fellow Application Requirements Masters-level applicants must provide: An essay describing the proposed research topic, the student’s role/responsibilities, the project timeline, and the type of written product that will be provided at the end of the project period; this essay should not exceed 500 words A current resume A copy of an official or unofficial transcript from GW A brief letter of support from the faculty member who will serve as preceptor/advisor for the research project, which must include a description of the proposed or existing project, and a description of the student’s responsibilities on the project; letters should not exceed 500 words, and no more than one letter will be accepted The student’s GWID and date of anticipated graduation Please combine all documents into a single PDF for submission. Letters from faculty members should not be sent separately. APPLICATION DEADLINE: November 16 Please submit completed application package to: Susan F. Wood, PhD Associate Professor, Department of Health Policy and Management Director, Jacobs Institute of Women's Health The George Washington University Milken Institute School of Public Health 950 New Hampshire Ave, NW Floor 2 Washington, DC 20052 202-994-4171 sfwood@gwu.edu Please submit applications as a single, combined PDF with all required documentation, including your GWID. About Founded in 1990, the Jacobs Institute of Women’s Health works to improve women’s health through research, dialogue, teaching, and information dissemination. Our mission is to: Identify and study aspects of healthcare and public health, including legal and policy issues, that affect women’s health at different life stages; Foster awareness of and facilitate dialogue around issues that affect women’s health; and Promote interdisciplinary research, coordination, and information dissemination on women’s health issues. The Jacobs Institute focuses primarily on the health of U.S. women, while also collaborating with colleagues who work internationally. The Jacobs Institute promotes environments where an interdisciplinary audience – including healthcare professionals, researchers, policymakers, and advocates – comes together to discuss ways to advance women’s health. Susan F. Wood, PhD is the Executive Director of the Jacobs Institute. Liz Borkowski, MPH is the Managing Director. Contact Jacobs Institute of Women's Health Milken Institute School of Public Health The George Washington University 950 New Hampshire Ave., NW, 6th Floor Washington, DC 20052 Liz Borkowski, MPH Managing Director 202-994-0034 WHIeditor@gwu.edu Milken Institute School of Public Health Twitter Facebook LinkedIn YOUTUBE 950 New Hampshire Ave, NW 7th Floor Washington, DC 20052 Phone (202) 994-9412 Fax (202) 994-3773 Admissions gwsphadmit@gwu.edu Phone (202) 994-2160 Fax (202) 994-1850 Student Services Phone (202) 994-0822 Media Relations gwsphmedia@gwu.edu Phone (202) 994-5179 Security Info Report a Website Issue/Suggestion The George Washington University 2121 Eye Street, NW Washington, DC 20052 Phone: (202) 994-1000 Campus Advisories Non-Discrimination Policy Contact GW A-Z Index Privacy Policy Terms of Use Copyright