Therapeutics/EBM Module Student Curriculum Pharmacotherapy

Therapeutics/EBM Module Student Curriculum
Pharmacotherapy
Appropriate and successful treatment requires choice of the correct medication, the appropriate dose, and both a dosage form and regimen that will maximize compliance. The pharmacokinetics (absorption, metabolism, distribution, and elimination) of medications changes under the influence of growth and physiologic maturation. Child behavior and psychomotor development influence the form of medication dispensed and the expectation for compliance.
Competencies
1.
Know medications that are contraindicated or must be used with extreme caution in specific pediatric populations, e.g. tetracycline, oral retinoic acid, aspirin.
2.
Know the components of and demonstrate the ability to write a prescription for a pediatric medication. Know how to calculate a drug dose in milliliters/milligrams for infants and prepubertal children based on body weight.
3.
Describe the appropriate use of the following common medications in the outpatient setting, including when it is NOT appropriate to treat with a medication:
Analgesics/antipyretics
Antibiotics
Cough and cold preparations
Ophthalmic preparations
Bronchodilators
Corticosteroids
Otic preparations
Vitamin and mineral preparations
4.
Demonstrate the ability to choose the appropriate medication(s) for management of the following conditions which may be seen in the pediatric inpatient or outpatient setting:
Acne
Allergic Rhinitis
Impetigo
Meningitis
Asthma
Bronchiolitis
Conjunctivitis
Eczema
Fever
Otitis media
Sepsis
Status epilepticus
Streptococcal pharyngitis
Urinary tract infection
5.
Know the importance of patient education in ensuring adherence with treatment regimens and be able to negotiate a treatment plan with the patient and family to maximize adherence and assess the family’s understanding of the plan.
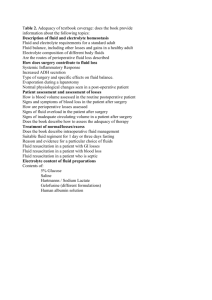
Fluid and Electrolyte Management
All human beings need an uninterrupted supply of water, electrolytes, and energy. Excessive or diminished fluid intake or losses may lead to severe physiologic derangements, with significant morbidity and even mortality.
Competencies
1.
Know the daily water and electrolyte requirements for children of all ages. Describe conditions in which fluid administration may need to be restricted (e.g. SIADH) or increased (e.g. fever).
Understand the definition of maintenance, deficit, ongoing losses and how these are important in fluid management.
2.
Know and be able to obtain the key historical and physical examination information necessary to determine the hydration status of children of all ages.
3.
Describe the physical findings in hypovolemic shock and the approach to restoration of circulating fluid volume. Be able to calculate and write orders for fluid therapy for a child with these findings. Be able to calculate fluid deficits and incorporate these calculations into fluid management.
4.
Know how to calculate and write maintenance fluid orders for children of all ages and weights.
5.
Describe the causes and consequences of fluid imbalances and electrolyte disturbances, such as hypernatremia, hyponatremia, hyperkalemia, hypokalemia, acidosis. Know how abnormalities in electrolytes affect rehydration strategies, and know the effect of pH on serum potassium levels.
6.
Know how to explain to parents the use of oral rehydration therapy for mild to moderate dehydration.
Poisonings
Poisonings and ingestions are major preventable causes of childhood morbidity and mortality. Poisoning control centers across the U.S. receive millions of calls a year regarding accidental and non-accidental ingestions and exposures to toxic materials.
Competencies
1.
Describe the developmental vulnerability for poisoning and accidental ingestions in infants, toddlers, children, and adolescents. Know the importance of and how to use the Poison Control
Center in management.
2.
Discuss the ages at which prevalence of unintentional and intentional poisonings is highest and the passive and active interventions that decrease the incidence of childhood ingestions (e.g. locks, safety caps).
3.
Know the clinical manifestations, risk of toxicity, and management of the following important ingestions:
Acetaminophen
Aspirin
Lead
Narcotics
Alcohol
Alkali
Caustics
Hydrocarbons
Organophosphates
Tricyclic antidepressants
Iron
PCP
4.
Be able to elicit a complete history to evaluate an unintentional or intentional ingestion or exposure to a toxic substance, including the substance, route of exposure, quantity, and timing.
Demonstrate sensitivity to the emotions/guilt of the patient, parent, or caregiver.
Pediatric Emergencies
All health care providers must be able to identify the infant, child, or adolescent with a medical emergency.
A systemic and thorough approach to the seriously ill child may significantly reduce morbidity and mortality.
Competencies
1.
List the symptoms of and describe the initial emergency management of shock, respiratory distress, lethargy, apnea, and status epilepticus in pediatric patients.
2.
Demonstrate the “ABC” assessment as a means for identifying who requires immediate medical attention and intervention.
3.
Describe the age-appropriate differential diagnosis for each of the emergent clinical problems noted in the table below.
4.
Describe the key clinical findings and management for each diagnoses listed in the table below.
Emergent Clinical Problem
Airway
Obstruction/Respiratory
Distress
Diagnoses to Consider
Croup Bronchiolitis Asthma
Pneumonia Foreign body aspiration Anaphylaxis
Altered mental status
Epiglottitis Peritonsillar/retropharyngeal abscess
Head injury Increased ICP Toxic ingestion
Infection DKA Hypoglycemia
Hepatic failure Nonaccidental trauma Hypoxemia
Uremia
Apnea
Ataxia
Gastrointestinal bleeding
Injuries
Proptosis
Seizures
Shock
Suicidal ideation
Acute life threatening event (ALTE) Seizure
RSV infection Pertussis GERD
Sepsis Nonaccidental trauma
Toxic ingestion Postinfectious ataxia Meningitis
Tumor
Anorectal fissure Meckel’s diverticulum Intussusception
Allergic colitis Inflammatory bowel disease Gastritis/PUD
Animal bites Minor head injury Sprains/fractures
Nursemaid’s elbow Near drowning
Nonaccidental trauma
Tumor Perioribital/orbital cellulites
Meningitis Encephalitis Febrile seizure
Toxic ingestion Electrolyte disturbances Hypoxemia
Status epilepticus Nonaccidental trauma
Sepsis Severe dehydration DKA
Anaphylaxis Cardiogenic / CHF Burns
Neurogenic shock Adrenal insufficiency
Depression