pgd authorised on
advertisement
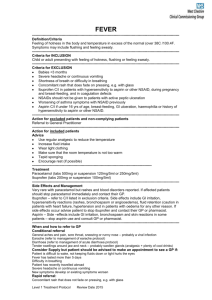
Patient Group Direction for the supply or administration of aspirin 300mg tablets to hospital in-patients, or attendees of out of hours, minor injury units and the emergency department presenting with suspected myocardial infarction This document authorises the supply or administration of aspirin 300mg tablets by registered nurses to patients with suspected myocardial infarction who meet the criteria for inclusion under the terms of the document The registered nurses seeking to supply or administer aspirin 300mg tablets must ensure that all patients have been screened and meet the criteria before supply takes place The purpose of this Patient Group Direction is to decrease the length of wait prior to aspirin administration in the event of a suspected myocardial infarction in the absence of medical staff This PGD was initially approved 1/5/2006 This direction was authorised on: October 2011 The direction will be reviewed by: October 2013 Clinician Responsible for Training and Review: Gillian Donaldson Reviewed by: Helen Oxenham, Paul Neary, Gillian Donaldson NHS Borders Aspirin PGD 1 Patient Group Direction for administration of aspirin 300mg tablets without a prescription for a named individual by registered nurses employed by NHS Borders in hospital in-patients, or attendees of Out of Hours, Minor Injury Units and the emergency department 1. This Patient Group Direction relates to the following specific preparation: Name of medicine, Aspirin 300mg tablets strength, formulation Legal status GSL (General Sales List) or P (Pharmacy Only) depending on pack size Storage Store in a dry place below 25°C Dose 300mg immediately Route/method 300mg should be chewed or dissolved in water for rapid effect. This should be given even if the patient has had aspirin previously that day. Frequency This should be given once only. Total dose Quantity 300mg (one tablet) (Maximum/Minimum) Advice to Patients Explain treatment and course of action Relevant Warnings May cause nausea and vomiting. Potential adverse drug reactions: Aspirin can irritate the GI mucosa and cause bleeding/ulceration. Hypersensitivity reactions include rashes, angioedema and bronchospasm. Please refer to current BNF or SPC for full details Use the Yellow Card System to report adverse drug reactions directly to the Committee of Safety of Medicines. Guidance on its use is available at the back of a BNF. Follow up Arrangements Patients with STEMI if not in BGH call 999 for paramedic ambulance and follow STEMI protocol regarding transfer to RIE or BGH NHS Borders Aspirin PGD 2 2. Clinical condition Clinical Condition Patient presenting with suspected myocardial to be treated infarction, in adults awaiting urgent transfer to the BGH or NRIE Criteria for inclusion Patients over the age of 16 presenting with acute chest pain that is consistent with myocardial infarction in site and duration. (Regardless of previous aspirin intake that day.) Signs of Myocardial infarction may include autonomic upset such as sweating and nausea, cardiogenic shock may be present i.e. hypotension and tachycardia without evidence of blood loss or infection Criteria for exclusion Patients who: Are under 16 years old Are allergic to aspirin or other NSAID Are pregnant Have active peptic ulceration Have aspirin-sensitive asthma Have haemophilia or other clotting disorders Are taking oral anti-coagulants eg warfarin Have already received a dose of 300mg aspirin before admission as an emergency. Action if excluded Urgent transfer to the BGH by ambulance or discussion with medical staff if in the BGH. As the benefit of a single dose of aspirin may outweigh the risks in many situations for any patient excluded the nurse should contact a doctor and record their advice if the drug is to be administered while awaiting an ambulance Action if declines The nurse must discuss the patient with a doctor and refer patient if willing. Document fully all discussions. Interactions with other medicaments and other forms of interaction NHS Borders Aspirin PGD Aspirin and corticosteroids may enhance the effects of aspirin on the gastrointestinal tract. Aspirin may enhance the effects of warfarin and oral hypoglycaemics of the sulphonylurea type. The toxicity of methotrexate may be enhanced by concomitant use of aspirin. Aspirin diminishes the action of uricosurics. 3 3. Records- use designated recording form for MIU/OOH/ED. For ward staff please record on kardex in the ‘once only’ section of the prescription kardex and nursing notes. Ensure that all administrations are recorded. a) The following records should be kept (either paper or computer based) The GP practice, clinic, hospital, and ward or department The patient name and CHI number The medicine name, dose, route, time of dose Drug batch number and expiry The signature and printed name of the approved healthcare professional that supplied or administered the medicine The patient group direction title and/or number Whether patient met the inclusion criteria and whether the exclusion criteria were assessed b) Preparation, audit trail, data collection and reconciliation c) Stock balances should be reconcilable with receipts, administration, records and disposals on a patient by patient basis. Quantity supplied / received and current stock balance d) Storage:- Store in a dry place below 25°C 4. Professional Responsibility All Health Professionals will ensure he/she has the relevant training and is competent in all aspects of medication, including contraindications and the recognition and treatment of adverse effects. He/she will attend training updates as appropriate. For those involved in immunisation, regular anaphylaxis updates are mandatory. Nurses will have due regard for the NMC Code of Professional Conduct, standards for conduct, performance and ethics (2008) and NMC Standards for Medicines Management (2008) 5. References British National Formulary (BNF) current edition http://bnf.org/bnf/index.htm Borders Joint Formulary (BJF) http://intranet/new_intranet/microsites/index.asp?siteid=65&uid=1 SPC Aspirin Caplets 300mg www.medicines.org NHS Borders Aspirin PGD 4 Patient Group Direction for administration of aspirin 300mg tablets by registered nurses employed by NHS Borders This Patient Group Direction is approved for use by the under-signed : Job Title Name Senior Doctor/Dentist for relevant clinical area Ross Cameron NHS Borders Director of Pharmacy Alison Wilson NHS Borders Senior Health Professional for Clinical Area Sheena Wright Signed Date PGD AUTHORISED ON ……/……/…….. Signed by ADTC CHAIRPERSON: ……………………………………………….. Name: …John Hammond………..……………………………………………… The Health Professionals named below, being employees of NHS Borders are authorised to provide and/or administer this medication under this Patient Group Direction and agree to supply and/or administer this medication in accordance with this Patient Group Direction Name of Health Professional NHS Borders Aspirin PGD Job Title Signed Date 5