Surgery notes
advertisement

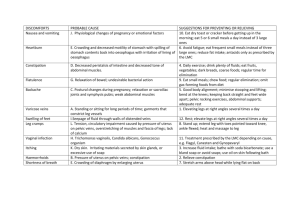
Upper GI surgery Cancer of the Oesophagus Epidemiology The epidemiology of oesophageal cancer shows that the UK is not a high risk cancer for the development of this type of cancer there are areas in Iran, Japan and South Africa that are high risk but in the UK the risk is 45/100,000. The cancer is normally developed between the ages of 50-70 and is more prevalent in men than women. In the UK the most common form of oesophageal cancer is an adenocarcinoma followed by a squamous cell carcinoma. Risk Factors There are a number of risk factors for the development of oesophageal cancer including alcohol, smoking, and nutrition deficiency in vitamins A, B and many more. There has also been found to be an increase risk for those who are exposed to fugal contamination, consume a lot of nitrates and are involved in Betel nut chewing. There are also some conditions which can increase the risk that someone will develop oesophageal cancer these are, long standing oesophagitis, Achalasia which is when the oesophagus doesn’t correctly relax following swallowing, Plummer-Vinson syndrome is when there is a web of mucosal tissue across the oesophagus. The main oesophageal problem which leads to cancer is having a Barretts oesophagus which is when there is metaplastic changes in the oesophagus as a result of long term acid exposure there is a 1% chance each year that someone with barrets oesophagus will develop an adenocarcinoma. Carcinoma of the stomach Factors influencing carcinoma of the stomach There are a number of very important factors which impact upon the development of gastric cancers. Enviromental factors such as a diet including large amounts of nitrates, smoked and salted food and pickled vegetables is highly influential along with smoking. There are also a number of host factors which can increase the risk of developing cancer such as hypochlorhydria, H.pylori infection, a previous partial gastrectomy, gastric adenomas and Barretts oesophagus. There is a genetic impact in the development of gastric cancers which isn’t fully understood but if you are blood group A, have a family history of gastric cancers or a hereditary nonpolyposis colon cancer syndrome you are at increased risk. Pathology Two types of tumour make up most of the cases of gastric cancer they are a gastric lymphoma and a gastric adenocarcinoma. Early gastic cancer has a good five year survival rate of 90% however the more of the organ which is effected the worse the prognosis. Clinical features There are a number of types of onset when it comes to gastric cancer. First you have the people who present with new dyspepsia after the age of 40 which should set alarm bells off. Then you have the insidious onset of the 3 A’s anaemia, anorexia and asthenia. Finally you have the obstructive group who can present with a vast number of symptoms including jaundice, ascites, trousseau’s sign, a palpable virchows node (troisiers sign) and sister Josephs umbilical nodule. Investigations General blood tests should be done including LFT’s, CEA as well as the other standard blood tests. There should also be an OGD, US and CT carried out. Treatment Surgery is the only curative treatment for gastric cancers the options are a total gastrectomy, or a partial gastrectomy Post operative complications There are many post operative complications following gastrectomy including small gastric pouch syndrome, chronic gastroparesis, alkaline reflux, early dumping syndrome, duodenal stump leak and postvagotomy diarrhoea. Benign Disorders of the Oesophagus and Stomach Gastro-oesophageal reflux This is a condition characterised by a number of symptoms including heartburn, regurgitation/vomiting, epigastric pain and dysphasia it can also present with hoarseness, a cough or chest pain though this is less common. You would investigate it by doing a Ba swallow and a GI endoscopy looking for underlying causes such as reflux oesophagitis, hiatus hernia, barretts oesophagus and a peptic stricture. Treatment of GORD The treatment of gastro-oesophageal reflux can be lifestyle modifications, medical, endoscopic or surgical. The life-style modifications that care carried out can be weight reduction, avoidance of acidic foods and foods which promote reflux such as high fat or caffeinated foods and raising the head to sleep. The medical interventions would be the use of antacids, H2 receptor agonist and PPI’s. Endoscopic treatment involves reinforcing the sphincter using a Endocinch, injecting bio-polymer to reinforce the LOC or the stretta procedure which damages the LOC causing a reduction in transient relaxations. The first option is to do a surgical procedure, you could do a Laproscopic Nissen fundoplication this is when the fundus of the stomach is wraped around the base of the oesophagus to reinforce the sphincter. There are two physiological studies which have to be done before there can be a surgical procedure to fix GORD. Manometry ensures that there is no achalasia and that there is peristalsis and ambulatory 24 hour PH ensures that there is a baseline for post operative comparison. Oesophageal Dysphasia There are a huge number of possible causes for oesophageal dysphasia including a pharyngeal pouch high up and a benign stricture lower down. With a pharyngeal pouch the symptoms will surround regurgitation of food. The investigations that you will do are a contrast swallow. You would then close the pouch using one of a number of procedures such as criptopharyngeal Myotomy or pouch resection. Another cause of dysphasia is Achalasia which is impaired peristalsis. This would be investigated using a swallow and an upper GI endoscopy, and would be treated using dilatation using a balloon. Oesophageal Rupture This normally occurs following a substantial meal or bout of drinking, it will be followed by retrosternal chest pain, or dyspnoea. In this situation a contrast swallow is essential as the patient may have a very varied differential diagnosis list and this is a definitive test. They must then be taken to surgery and have the tear repaired. Peptic ulcer disease With peptic ulcer disease there may be epigastric pain which is alleviated by food and worse at night. If the ulcer has ruptured there maybe a sudden onset of epigastric pain and signs of peritonism. A rupture is a surgical emergency. Gallstone Problems Causes of Jaundice The causes of jaundice in a patient can be divided into three main groups. Prehepatic, hepatic and post hepatic. Pre-hepatic causes are normally related to the blood cells being haemolysed for example hereditary spherocytosis. Hepatic causes are related to a failure of the liver and post hepatic causes are things like sepsis. Obstructive jaundice The patient with obstructive jaundice with present with right upper quadrant pain if it is caused by gallstones and weight loss if caused by malignancy. They are also likely to have pale stools and dark urine. It is also important that you think about Courvoisier’s Law when looking at obstructive jaundice, if you can feel an enlarged gall bladder the cause is unlikely to be gall stones. The investigations that you would do in the patient presenting with obstructive jaundice are bilirubin, liver enzymes as you would expect ATL and AFT to be raised, INR and also a live ultrasound. Biliary colic Gallstones have an incidence of 5-10% within the population and there are three types pigmented, cholesterol and mixed. A typical pain history of a patient with biliary colic may well look like Site = Right upper quadrant Radiation = Back/shoulder tip Onset = Rapid Character = Sharp/colicky Duration = Minutes – hours Severity = +++ Exacerbating/relieving factors = ↑ by fatty food Periodicity = Intermittent Associated symptoms = Nausea, vomiting There are a number of complications that can arise from gallstones you can have a mucocele, empyema or cancer in the gall bladder. You can have acute pancreatitis or gallstone ileus. The treatment of gallstones is mostly conservative manage with painkillers and wait for the stone to pass. However in acute pancreatitis or when the patient is presenting with obstructive jaundice and ERCP needs to be carried out. Acute pancreatitis To remember the possible causes for pancreatitis remember get smashed. Gallstones Ethanol Trauma Steroids Mumps Autoimmune Scorpion bites Hypothermia/hypolipidaemia Elevated calcium Drugs. There are a number of possible implications of a bout of acute pancreatitis it can locally cause pancreatic infarction/necrosis, a pseudocyst, or an abscess. Systemically it can cause hypovolaemia, acute renal failure, acute respiratory distress syndrome and paralytic ileus. If you were going to take a pain history from someone with acute pancreatitis you may well find. Site = Epigastric Radiation = Back Onset = Gradual Character = Constant/dull Duration = Hours – days Severity = +++ Exacerbating/relieving factors = ↑ by movement Periodicity / Associated symptoms = Vomiting +++ Colorectal Surgery Constipation Constipation is defined as either excessive straining at stool or the passage of two of fewer stools in a week. It is important to ask the patient about their normal bowel habit as what is normal for some may be abnormal for others.. Causes of constipation 1) Inadequate dietary fibre 2) Neoplasm of the colon, rectum or anus 3) Benign lesion of the anus 4) Endocrine disease 5) Drugs 6) Hirschsprungs disease (neonates) 7) Slow transit constipation 8) Psychological 9) Neurological/behaviour 10) Spinal e.g. MS Constipation should be investigated with sigmoidoscopy and barium enema to rule out a malignancy. There should also be blood tests for endocrine and metabolic abnormalities such as hypothyroidism and hypocalcaemia. Slow transit constipation this is when a patient (usually female does not respond to an increase in dietary fibre or to laxatives. This is the result of a slow transit time and may need to have a surgical total colectomy and anastamosis of ileum to rectum The treatment of constipation can take the form of lifestyle based interventions for example making sure that the patient is taking in adequate fibre and being well hydrated. Their drug regime could be modified to look at causes that may come from there. If these methods fail laxatives could be tried to address the issue. Rectal Bleeding This is when the patient complains of rectal bleeding not when a random stool test happens to find blood. Possible causes of rectal bleeding include 1) Haemorrhoids 2) Diverticular disease 3) Large bowel polyps/carcinoma 4) Angiodysplasia- small bleeding bowel capillaries 5) IBS 6) Ulcer The investigations that must be done for rectal bleeding are sigmoidoscopy and if nothing is found then colonoscopy should be done as soon as possible if this is also negative then do a technetium scintiscan to look for lesions. The management depends on what the diagnosis is. Abdominal pain When a patient presents with abdominal pain it is important that you take a full history including Socrates. Causes of abdominal pain 1) Acute appendicitis 2) Bilary colic 3) Colon carcinoma 4) Diverticular disease 5) Gastic carcinoma 6) Pancreatitis 7) Dissection aortic aneurysm You would have to do a number of tests as there are a number of possible differentials for acute abdominal pain. These includes blood tests like and FBC, serum amylase, U’s and E’s, glucose, LFT’s, calcium, and a clotting studies. Imaging studies are also important an abdominal x-ray and ultrasound for pancreatitis. Irritable bowel syndrome Pathogenesis: It isn’t really known what causes IBS there have been abnormalities discovered in the lower GI tract, patients have been found to have previously had a low fibre diet. There are abnormal intraluminal pressures. Genetics and psychological factors are also thought to play a role. Clinical features Patients with IBS will classically present with left iliac fossa pain relieved by defecation. This pain is not related to meals. There will also be an abnormal bowel habit of alternating constipation and loose stools. Investigations IBS is a diagnosis of exclusion so it is important to rule our diagnosis which might be more sinister in origin you would do a FBC, CRP, LFT’s, TFT’S, faecal occult blood test, serological markers for celiac disease. If thought necessary then CT scan, sigmoidoscopy and other method of looking for tumours. Management The management of IBS is usually provided by systematic relieve of symptoms. Patients should increase their dietary fibre. Drug therapy in the form of antispasmotics, antidepressants, bulk forming agents and hypnotherapy Acute appendicitis Pathology The pathology of appendicitis is thought to be obstruction of the appendix. This causes the blood supply to be reduced and gangrene can be a problem. Clinical features The history will often describe central abdominal pain which is quite generalised and accompanied by anorexia, nausea and vomiting. The pain will then become localised to the RIF. Investigations You would want to do the normal blood tests as well as a pregnancy test in women of child baring age. You may do an ultrasound and a CT scan. Management Once the diagnosis has been made the likely progression of the disease means that it is important that the appendix is removed. This can be done through either a small transverse incision in the RIF or laproscopically. You may also decide to watch a wait keeping the patient nil by mouth and on pain killers. Haemorrhoids Pathology Haemorrhoids are engorgement of the haemorrhoidal venous plexus with redundancy of their covering. Clinical features Haemorrhoids can present in a number of ways including bleeding, discharge, discomfort, prolapse, pain and a change in bowel habit. Management Patients can be helped quite a lot by reassuring them and alleciating the dear of a more sinister diagnosis. The regulation of bowel habit can help and constipation appears to exacerbate haemorrhoids. You can use suppositories containing corticosteroids, local anaesthetic and antibiotics. There are a number of surgical procedures too. Diverticular disease Pathology Diverticula have a narrow neck and faeces may accumulate within them causing inflammation and increasing the risk of inflammation. Clinical features There are very few symptoms however there maybe left lower abdominal pain, and long standing irregularity or bowel habit. Investigations Barium enemas are the usual methods of confirming the diagnosis. The diverticular openings may also be seen on colonoscopy. ManagementThere is no evidence to suggest that if you increase the amount of dietary fiber then diveticular disease is less likely to develop however mild symptoms seem to benefit. Resection of the affected area might be considered in sever disease. Complications The main possible complications of Diverticular disease are inflammation leading to a risk of perforation and fistulation. Ulcerative colitis Pathology The major feature of is inflammation of the mucosa with increased vascularity and haemorrhage. It is rare for the whole of the large bowel to be involved. Clinical features Bloody diarrhoea associated with social embarrassment and physical discomfort. This is a relapsing and remitting condition Complications Toxic megacolon is quite a serious condition which can evolved as a result of ulcerative colitis which means that perforation is a big risk. It is treated with blood transfusions, water and electrolyte replacement. Massive haemorrhage is a rare complication. There can also be systemic complications such as urinary calculus. Investigations Sigmoidoscopy and biopsy of the rectal mucosa. If an infective cause is suspected then stool samples may be carried out. A barium enema and colonoscopy may be necessary. Management Management can be medical or surgical. Minimal disease can be managed by a combination of prednesilone and oral sulfasalazine. Surgical treatment can be the fitting of an illiostomy which divert faeces away from the effected area, an ileorectal anastomosis after a colectomy can be done finally a continent ileostomy could be done. Crohns disease Pathology It is not known exactly what causes this condition although it is thought that it might be inflammation caused by unusual strains of bacteria. The pathological features of this disease is that there is transmural inflammation with oedema and fissures. Skip lesions can occur throughout the whole bowel. Oedema and fibrosis can cause obstruction. Fistulae may form. Clinical features Acutely it may present as RIF pain and tenderness. However chronically there are symptoms of general ill health such as weight loss, colicky abdominal pain and diarrhoea. Investigations Imaging may be done most commonly a barium meal which may show mucosal irregularities, strictures and skip lesions. A biopsy will also be done. Management There is no specific treatment of crohns disease and management is often symptomatic with steroids. Surgical management is also sometimes required when there is an intestinal obstruction, abscess or fistula. Surgery normally takes the form of resection. Vascular Surgery Carotid Artery disease Carotid dissection Background This is a rare thing to happen, the mean age that it happens is 45 and the main causes are spontaneous, traumatic and iatrogenic. Risk factors Predisposing factors are the oral contraceptive pill, marfans, hypertension and fibromuscular dysplasia. Clinical features The patient can prevent with a large number of symptoms including headache, TIA/CVA, syncope and cranial nerve lesions. Investigation You would investigate this patient with duplex, ct and mri Management They would have to be on anticoagulation for 3-6 months, Carotid aneurysm Risk factors Previous infection with TB or syphilis Causes Atherosclerosis, trauma, marfans, fibromuscular dysplasia and previous caroid endarterectomy Clinical features Lump, pain, dysphasia and TIA Investigation Duplex, angiography, CT and MRI Management Aspirin, ligation, resection and repair Carotid body tumours Pathology Chemodectoma, Glomus tumour and paraglangionoma which can be neural crest tissue or neuropeptide hormones. Clinical features Lump (pulsatile), headache, tinnitus and vocal cord paralysis Investigations Duplex ultrasound, CT, MRI, angiography Management Surgical incision Carotid occlusive disease Pathology Athroma at carotid bifurcation, Emboli from carotid plaque Risk factors Age, smoking, hyperlipidaemia, hypertention and diabetes Clinical features Amaurosis fugax, TIA, CVA Management Control risk factors that are modifiable, prevent emboli with antiplatelet therapy e.g. asprin, clopidogrel, LMWH and warfarin. Endarterectomy, Post-operative complications Cerebral hyperperfusion, risk of nerve damage to transverse cutaneous nerve or greater auricular nerve. Varicose Veins, Venous thromboembolism and Venous Ulceration Varicose Veins Definition A varicose vein is a vein that is tortuous and dilated Aetiology Caused by a defect in the venous valve or a defect in the vein wall. Clinical presentation Aching, cosmetic, ankle swelling, eczema, bleeding, ulceration. All the way down the inside of the leg suggests LSV, bellow the knee in the calf area suggests SSV. Investigation Hand held Doppler, duplex ultrasound, radiological Management Need to establish if superficial or deep? If superficial can be corrected by surgery or injection, new techniques include use of ablation and lasers. If deep pressure stockings are main form of treatment. Venous thromboembolism Background For venous thromboembolism to form there has to be one of blood stasis, altered coagulability and injury to the vessel wall. Risk factors These are age/sex/pregnancy, injury/surgery, malignant disease, previous DVT, VV, obesity, OCP and long distance travel. Clinical presentation Pain, swelling, calf tenderness, blue discoloration and rarely gangrenous changes. Investigation Screening ultrasound, D-dimer, plebography Management Mobilise, anticoagulants LMWH then warfarin consider surgery but rarely done. Pulmonary embolism Clinical presentation Will present with collapse, SOB, pleuritic chest pain and haemoptysis Investigation CXR, ECG, ABG, CT. angiography, test for DVT see above. VQ mismatch scan, pulmonary Management Anticoagulant, thrombolysis, inferior vena cava filter and rarely surgery Peripheral vascular disease Leg ulcers Leg ulcers can either be arterial or venous Venous= VV/DVT, sloping sides, painful, medial, normal pulses normal ABPI Arterial= Smoking, a lot of pain, lateral, punched out, necrotic, low ABPI, absent pulses. Treatment Venous Compression bandages Acute ischemia Causes Embolism due to cardiac/atrial fibrillation, no previous claudication history Clinical presentation = 5 P’s Pain Pulseless Pale Parathetic Perishing cold Treatment Heparin, ECG, Duplex angiography (if streptokinase, embolectomy, possibly faciotomy time), Thrombolyse, Chronic arterial disease Clinical presentation Pain in calf on walking, relived by rest, pain in toes feet at rest, ulcers, gangrene Investigation Hb, FBC, U’s and E’s, lipids, ABPI, Duplex, MRA, angiography, CT Treatment Lifestyle modification, Asprin, statin, consider surgery (angioplasty) in sever cases,