Group B Strep Support
advertisement
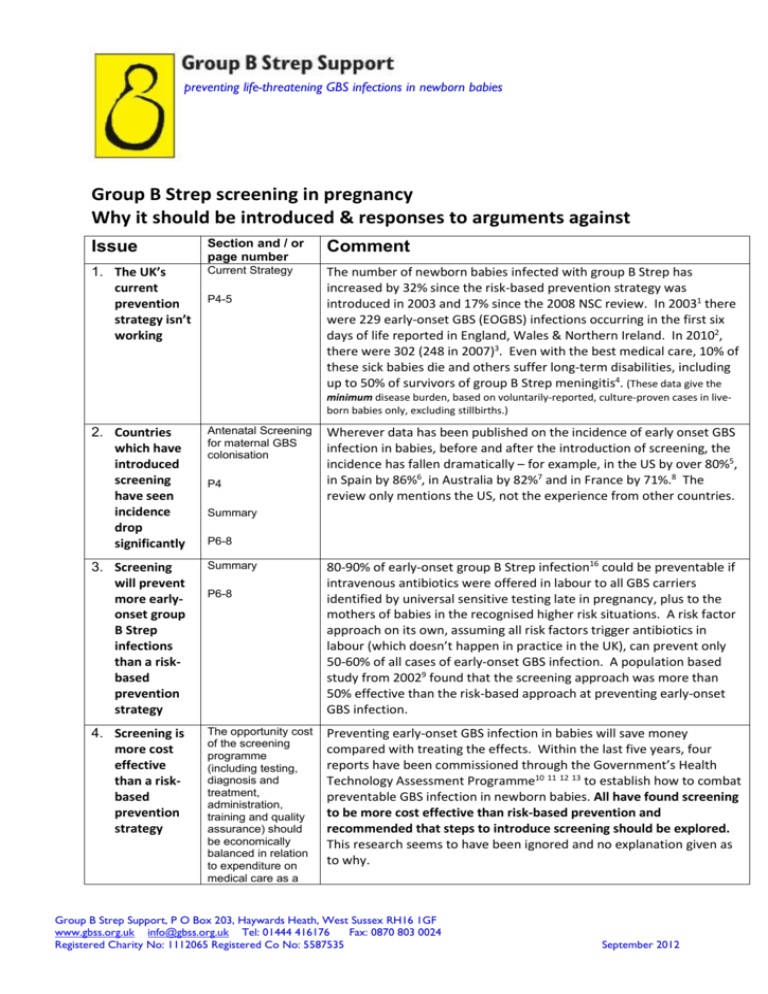
preventing life-threatening GBS infections in newborn babies Group B Strep screening in pregnancy Why it should be introduced & responses to arguments against Issue Section and / or page number Comment 1. The UK’s current prevention strategy isn’t working Current Strategy The number of newborn babies infected with group B Strep has increased by 32% since the risk-based prevention strategy was introduced in 2003 and 17% since the 2008 NSC review. In 20031 there were 229 early-onset GBS (EOGBS) infections occurring in the first six days of life reported in England, Wales & Northern Ireland. In 20102, there were 302 (248 in 2007)3. Even with the best medical care, 10% of these sick babies die and others suffer long-term disabilities, including up to 50% of survivors of group B Strep meningitis4. (These data give the P4-5 minimum disease burden, based on voluntarily-reported, culture-proven cases in liveborn babies only, excluding stillbirths.) 2. Countries which have introduced screening have seen incidence drop significantly Antenatal Screening for maternal GBS colonisation 3. Screening will prevent more earlyonset group B Strep infections than a riskbased prevention strategy Summary 4. Screening is more cost effective than a riskbased prevention strategy The opportunity cost of the screening programme (including testing, diagnosis and treatment, administration, training and quality assurance) should be economically balanced in relation to expenditure on medical care as a P4 Wherever data has been published on the incidence of early onset GBS infection in babies, before and after the introduction of screening, the incidence has fallen dramatically – for example, in the US by over 80%5, in Spain by 86%6, in Australia by 82%7 and in France by 71%.8 The review only mentions the US, not the experience from other countries. Summary P6-8 P6-8 80-90% of early-onset group B Strep infection16 could be preventable if intravenous antibiotics were offered in labour to all GBS carriers identified by universal sensitive testing late in pregnancy, plus to the mothers of babies in the recognised higher risk situations. A risk factor approach on its own, assuming all risk factors trigger antibiotics in labour (which doesn’t happen in practice in the UK), can prevent only 50-60% of all cases of early-onset GBS infection. A population based study from 20029 found that the screening approach was more than 50% effective than the risk-based approach at preventing early-onset GBS infection. Preventing early-onset GBS infection in babies will save money compared with treating the effects. Within the last five years, four reports have been commissioned through the Government’s Health Technology Assessment Programme10 11 12 13 to establish how to combat preventable GBS infection in newborn babies. All have found screening to be more cost effective than risk-based prevention and recommended that steps to introduce screening should be explored. This research seems to have been ignored and no explanation given as to why. Group B Strep Support, P O Box 203, Haywards Heath, West Sussex RH16 1GF www.gbss.org.uk info@gbss.org.uk Tel: 01444 416176 Fax: 0870 803 0024 Registered Charity No: 1112065 Registered Co No: 5587535 September 2012 whole (ie value for money). Assessment against this criteria should have regard to evidence from cost benefit and/or cost effectiveness analyses and have regard to the effective use of available resource P65-67 5. Screening identifies women most likely to be carrying GBS at delivery and allows antibiotics to be targeted to women whose babies are most at risk of earlyonset GBS infection. 6. Summary: Criterion 2 Partly Met P20-21 Government focus on preventative medicine 7. Women want to be told about group B Strep and offered GBS screening during pregnancy Using screening to identify women carrying GBS will allow antibiotics to be targeted to women who are actually most likely to be carrying GBS at delivery and whose babies are at greatest risk. Risk factors are ineffective at identifying which women are likely to be carrying GBS at delivery. Error! Bookmark not defined. Currently many women given antibiotics during labour based on risk factors do not require them, while others, whose babies would benefit, are ignored. With screening, fewer women who are not carrying group B Strep at delivery will be given unnecessary antibiotics. Error! Bookmark not defined. With the recent Government focus on preventative medicine, now is the ideal time to introduce screening for GBS in pregnancy. The test should be acceptable to the population A survey undertaken by ComRes14 on behalf of GBSS showed that over half (54%) the women aged 20-35 surveyed had heard of group B Strep, only 20% knew what it was P44-45 once aware of the dangers of group B Strep in pregnancy, over 90% of young women believe pregnant women should always be offered information, tests and, when the bacteria is detected, antibiotics in labour 92% believe that information on GBS should be given to all pregnant women 92% would welcome the opportunity for pregnant women to be screened for group B Strep in the later stages of pregnancy and believe that such screening should be offered to women routinely 95% believe antibiotics should be offered to women in labour with group B Strep and that they themselves would definitely or Group B Strep Support, P O Box 203, Haywards Heath, West Sussex RH16 1GF www.gbss.org.uk info@gbss.org.uk Tel: 01444 416176 Fax: 0870 803 0024 Registered Charity No: 1112065 Registered Co No: 5587535 September 2012 probably accept the offer (89%) 8. Incidence of early-onset GBS infection in babies – anticipated effect of riskbased prevention in 2003 ignored Summary P6-8 The condition should be an important health problem, EOGBS Incidence 9. Implication that any antenatal or intrapartum risk factor for earlyonset GBS infection in babies will mean mothers will be offered intravenous antibiotics in labour which does not happen in practice Presentation of EOGBS, 10. Risk of antibiotic resistance as a result of antibiotics given in labour against early-onset group B Strep infection Summary P6-8 3. All the costeffective primary prevention interventions should have been implemented as far as practicable P21-22 Antibiotic resistance P61-62 15. The benefit from the screening programme should outweigh the physical and psychological harm (caused by the test, diagnostic procedures and treatment) P9-11 P19-20 The review compares the incidence of early-onset GBS infection voluntarily reported to the Health Protection Agency in 2003 of 0.37 per 1,000 live births reported in England, Wales & Northern Ireland1 with 0.41 in 20102. This ignores the fact that the preventative strategy against EOGBS infection recommended in 2003 by the Royal College of Obstetricians & Gynaecologists15 should have reduced UK incidence by 50-60%16. The effectiveness of our existing strategy, with the relatively unchanged incidence from 2003 to 2010, must be viewed taking this into consideration. The review states that “a third of EOGBS cases might be born to women with no known risk factors for GBS, and therefore not targeted with IAP [intrapartum antibiotic prophylaxis – antibiotics given as preventative medicine in labour] in the absence of universal screening.” This presupposes that all women with any risk factor would be offered antibiotics in labour, which does not happen in practice. The Royal College of Obstetricians & Gynaecologists’ 2012 GBS guideline17 does not recommend antibiotics in labour for mothers in preterm labour or for those with prolonged rupture of membranes. Excluding these risk factors would mean that not 32% but 48% of babies with EOGBS infection in the Vergnano study18 referred to would have been born to women without known risk factors and where no prevention would take place. As a result, significantly fewer cases of EOGBS infection in babies will be prevented using the risk factor approach recommended by the Royal College of Obstetricians & Gynaecologists than the expert review suggests – almost half of all EOGBS infections in babies would still occur. Antibiotic resistance of group B Strep is of concern although is not currently an issue when the recommended penicillin is used, although there is increasing resistance with clindamycin or erythromycin. Likewise, concerns about encouraging antibiotic resistance in other organisms, such as E coli, have not been realised so long as penicillin is used. Experience from other countries shows the risk of antibiotic resistance to be very small when the recommended antibiotics are used.19 A UK study12 showed that similar percentages of women would be offered antibiotics in labour regardless of whether they were identified by screening late in pregnancy or through recognised risk factors. Therefore, the issue of antibiotic resistance is of equal concern for either strategy. However, a screening strategy would mean that the antibiotics in labour would be more accurately targeted to women actually carrying group B Strep at the time, would prevent more EOGBS infections and would minimise antibiotic use in women not carrying GBS. P63-64 Group B Strep Support, P O Box 203, Haywards Heath, West Sussex RH16 1GF www.gbss.org.uk info@gbss.org.uk Tel: 01444 416176 Fax: 0870 803 0024 Registered Charity No: 1112065 Registered Co No: 5587535 September 2012 11. Risk of anaphylaxis as a result of antibiotics given in labour against early-onset group B Strep infection Summary P6-8 5. The benefit from the screening programme should outweigh the physical and psychological harm (caused by the test, diagnostic procedures and treatment) 12. Evidence of the on-going benefit of screening in continued reduced rates of early-onset group B Strep infection in other countries Summary 13. Studies on the accuracy of the ‘gold standard’ ECM test should keep to those where the correct procedures were followed. P63-64 P6-8 Anaphylactic shock is very serious but extremely rare - EOGBS infection is both more common and more easily preventable. As for the issue of antibiotic resistance (see row above), similar percentages of women would be offered antibiotics in labour through either a risk based or screening prevention strategy, so the issue of anaphylaxis is of equal concern with each strategy. However, a screening strategy would prevent more EOGBS infections, target antibiotics at women most likely to be carrying GBS at the time of delivery and mean fewer women not carrying GBS being given antibiotics inappropriately. Again, experience from other countries shows the risk to be extremely small.Error! Bookmark not defined. The review states there has been little new evidence on the effectiveness of screening at preventing EOGBS infection. However in countries that do screen and have data from before and after the introduction of screening, their incidence has dropped by up to 86%5,6,7,8 and this has remained low20. This is new evidence showing continued benefit. The review fails to make a case why the UK should not see a similar drop in incidence were screening introduced; we can see every reason why it should and no reason why it shouldn’t. The review focuses heavily on the accuracy of the ‘gold standard’ enriched culture medium (ECM) test, but majors on studies where it has been implemented poorly, with recommended procedures not followed. Even in those cases where the ECM test is poorly done, it is still more accurate than the standard NHS test would be. When procedures are correctly followed, a positive ECM test result is 87% predictive of whether a woman will still be carrying GBS (and a negative ECM test result is 96% predictive of her still not carrying GBS) when done within 5 weeks of delivery.21 Countries which have implemented screening have seen their incidence of EOGBS infection fall dramatically (see 2 above), whilst in the UK, where a risk based strategy is used, the incidence has increased. This suggests that screening using the ECM test is enormously effective at reducing the burden of EOGBS infection even when sometimes implemented poorly. 1 Health Protection Agency, Pyogenic & non-pyogenic streptococcal bacteraemia, England, Wales &Northern Ireland: 2003, CDR Weekly Volume 14 No 16, 16 April 2004. http://www.hpa.org.uk/cdr/archives/2004/cdr1604.pdf 2 Health Protection Agency, Pyogenic &non-pyogenic streptococcal bacteraemia, England, Wales & Northern Ireland: 2010. Health Protection Report Vol. 5 No. 46, 18 Nov 2011 http://www.hpa.org.uk/webc/HPAwebFile/HPAweb_C/1317131482001 3 Health Protection Agency, Pyogenic and non-pyogenic streptococcal bacteraemia, England, Wales & Northern Ireland: 2007. Health Protection Report 2008; 2 (47): Bacteraemia http://www.hpa.org.uk/hpr/archives/2008/hpr4708.pdf#strepbact07 4 Edwards MS, Rench MA, Haffar AA, Murphy MA, Desmond MM, Baker CJ. Long-term sequelae of group B streptococcal meningitis in infants. J Pediatr 1985; 106(5):717-722 Group B Strep Support, P O Box 203, Haywards Heath, West Sussex RH16 1GF www.gbss.org.uk info@gbss.org.uk Tel: 01444 416176 Fax: 0870 803 0024 Registered Charity No: 1112065 Registered Co No: 5587535 September 2012 5 Jordan HT, Farley MM, Craig A, Mohle-Boetani J, Harrison LH, Petit S et al. Revisiting the need for vaccine prevention of late-onset neonatal group B streptococcal disease: a multistate, population-based analysis. Pediatr Infect Dis J 2008; 27(12):1057-1064. 6 Andreu A, Sanfeliu I, Vinas L, Barranco M, Bosch J, Dopico E et al. [Decreasing incidence of perinatal group B streptococcal disease (Barcelona 1994-2002). Relation with hospital prevention policies]. Enferm Infecc Microbiol Clin 2003; 21(4):174-179. 7 Daley AJ, Isaacs D. Ten-year study on the effect of intrapartum antibiotic prophylaxis on early onset group B streptococcal and Escherichia coli neonatal sepsis in Australasia. Pediatr Infect Dis J 2004; 23(7):630-634. 8 Albouy-Llaty M, Nadeau C, Descombes E, Pierre F, Migeot V. Improving perinatal Group B streptococcus screening with process indicators. J Eval Clin Pract 2011. 9 Schrag S et al. A population based comparison of strategies to prevent EOGBS disease in neonates. NEJM, Vol 347(4) July 2002. 10 Colbourn T, Asseburg C, Bojke L, Philips Z, Claxton K, Ades AE et al. Prenatal screening and treatment strategies to prevent group B streptococcal and other bacterial infections in early infancy: cost-effectiveness and expected value of information analyses. Health Technol Assess 2007; 11(29):1–226, iii 11 Kaambwa B, Bryan S, Gray J, Milner P, Daniels J, Khan KS et al. Cost-effectiveness of rapid tests and other existing strategies for screening and management of early-onset group B streptococcus during labour. BJOG 2010; 117(13):1616–1627. 12 Daniels JP, Gray J, Pattison HM, Gray R, Hills RK, Khan KS. Intrapartum tests for group B streptococcus: accuracy and acceptability of screening. BJOG 2011; 118(2):257–26.5). 13 Colbourn TE, Asseburg C, Bojke L, Philips Z, Welton NJ, Claxton K et al. Preventive strategies for group B streptococcal and other bacterial infections in early infancy: cost effectiveness and value of information analyses. BMJ 2007; 335(7621):655. 14 ComRes. Pregnancy Screening Survey. 1-11-2011. 6-6-2012 15 RCOG. Prevention of Early Onset Neonatal Group B Streptococcal Disease. Royal College of Obstetricians and Gynaecologists Guidelines 36. 2003. 16 J Med Screen. Maternal screening to prevent neonatal Group B streptococcal disease. Journal of Medical Screening 2002; 9(4). 17 RCOG. Prevention of Early Onset Neonatal Group B Streptococcal Disease. Royal College of Obstetricians and Gynaecologists Guidelines 36. 2012. http://www.rcog.org.uk/files/rcog-corp/GTG36_GBS.pdf 18 Vergnano S, Embleton N, Collinson A, Menson E, Russell AB, Heath P. Missed opportunities for preventing group B streptococcus infection. Arch Dis Child Fetal Neonatal Ed 2010; 95(1):F72-F73. 19 Law MR, Palomaki G, Alfirevic Z, Gilbert R, Heath P, McCartney C et al. The prevention of neonatal group B streptococcal disease: a report by a working group of the Medical Screening Society. J Med Screen 2005; 12(2):60-68. 20 Active Bacterial Core surveillance (ABCs) Surveillance Reports: series at http://www.cdc.gov/abcs/reports-findings/surv-reports.html 21 Yancey MK, Schuchat A, Brown LK, Ventura VL, Markenson GR. The accuracy of late antenatal screening cultures in predicting genital group B streptococcal colonization at delivery. Obstet Gynecol 1996; 88(5):811-815 Group B Strep Support, P O Box 203, Haywards Heath, West Sussex RH16 1GF www.gbss.org.uk info@gbss.org.uk Tel: 01444 416176 Fax: 0870 803 0024 Registered Charity No: 1112065 Registered Co No: 5587535 September 2012







