Appendix
advertisement

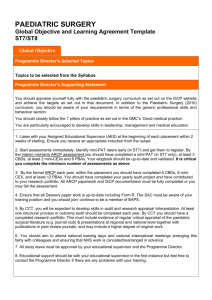
ADVANCED PAEDIATRIC UROLOGY FELLOWSHIP Global Objective and Learning Agreement template 1 – 2 YEAR PROGRAM > ST7 Global Objective Programme Director’s Selected Topics Topics to be selected from the Syllabus Programme Director’s Supporting Statement You should appraise yourself fully with the paediatric surgery curriculum as set out on the ISCP website and achieve the targets as set out in that document. In addition to the Paediatric Surgery (2010) curriculum, you should be aware of your requirements in terms of the generic professional skills and behaviour section. You should closely follow the 7 pillars of practice as set out in the GMC’s ‘Good medical practice’. You are particularly encouraged to develop skills in leadership, management and medical education. 1. Liaise with your Assigned Educational Supervisor (AES) at the beginning of each placement within 2 weeks of starting. Ensure you receive an appropriate induction from the outset. 2. Start assessments immediately. Identify mini-PAT raters (mid fellowship) and get them to register. You should meet the generic ISCP Paed Surgery WBAs pre CCT (completed 6 CBDs, 6 mini-CEX, and at least 12 PBAs ) and 6 CBDs and 12 PBAs post CCT. Your elogbook should be up-to-date and validated. It is critical you complete the minimum number of assessments as above. 3. By your formal Final fellowship assessment, you should have completed your yearly audit project and have contributed to your research portfolio. All paperwork and documentation must be fully completed or you may fail the assessment. You must have completed operative competency and deanery Purple forms. Ensure that all Deanery paper work is up-to-date including Form R. The SAC must be aware of your training position and you should join/continue to be a member of BAPU. 4. You should have completed ICB exam in Paediatric Surgery by end of first year fellowship. 5. By CCT, you will be expected to develop skills in audit and research appraisal /interpretation. At least one structure/ process or outcome audit should be completed each year. By end of fellowship you should have a completed research portfolio; this must include evidence of regular critical appraisal of the paediatric surgical literature (e.g. journal club) & presentations at regional and national level together with publications in peer review journals, and may include a higher degree of original work. 6. You should aim to attend national training days and national international meetings arranging this fairly with colleagues and ensuring that NHS work is cancelled /rearranged in advance. 7. All study leave must be approved by your educational supervisor and the Programme Director. 8. Educational support should be with your educational supervisor in the first instance but feel free to contact the Programme Director if there are any problems with your training. Learning Agreement Objective Setting Part 1: Topics to focus on during this placement Please refer to the Paediatric Surgery curriculum - Topics to be selected from the Syllabus As a guide: Aim to complete CCT (Paed Surgery)(Urology Trainees will need to refer to their Urology STC) Be pro-active in organising regular appraisals with your AES. Keep an updated educational portfolio containing CV, evidence of achievements and reflective practice Each year of fellowship should attend & present at Trainee session at BAPU By the end of Urology Fellowship: You should be able to carry out surgical procedures in the following groups (depending on placements) under supervision or independently: Example Operative Competencies Endoscopic Cystoscopy (I) Ureteroscopy (S) Mitrofanoffoscopy (I) Botox injection (I) PUV resection (I) JJ stent insertion/ removal (I) Ureterocele puncture (I) Deflux procedure (I) PCNL(O) Nephrostomy insertion (S) Urethrotomy (S) I = Independent S = Supervised O = Observed Laparoscopic Diagnostic laparoscopy (I) Laparoscopic nephrectomy (I) Laparoscopic heminephrectomy (S) Laparoscopic pyeloplasty (O) Laparoscopic varicocele ligation (I) 2-stage FS orchidopexy (I) Open/ reconstructive Bladder Cystectomy (O) Cystolithotomy (I) Augmentation cystoplasty (S) ACE procedure, (I) Mitrofanoff formation Bladder exstrophy closure (O) Bladder neck closure (O) (I) (Sling procedure (O)) Bladder neck reconstruction (S) Cloacal exstrophy repair (O) ( Kelly procedure (O)) Urinary undiversion (S) Suprapubic tube insertion (I) Vesicostomy formation/ closure (I) Genitalia Clitoral reduction (S) Buried penis repair (I) Circumcision (I) Modified circumcision (I) Chordee correction (I) Epispadias repair (O) Distal hypospadias repair (I) Proximal hypospadias repair (I) Testicular prosthesis insertion (O) UG sinus mobilisation (S) V-flap vaginoplasty (S) Orchidopexy (I) Scrotal exploration (I) Upper Tract Open Nephrectomy (I) Open heminephrectomy (I) Pyelolithotomy (S) Pyeloplasty (I) Transureteroureterostomy (O) Ureteric reimplant (I) Ureterolithotomy (S) Ureterostomy formation (I) Urethrostomy formation (I) Other PD catheter insertion (S) By the end of Fellowship Complete & present at least 1 audit (1 per year) Contribute to your research portfolio Perform the required minimum number of validated WBA (as above) Be able to manage a ward round and clinic consultations effectively Have passed the FRCS Paed and to be consolidating your factual base with regular appropriate reading. Have gained CCT Achieved expected level of operative competency in most areas (see table above) Part 2: Actions required to meet Learning Objectives Assessments Over each 12-month attachment we will aim to do at least 6 CBD and 12 PBA’s. You should aim to carry out PBAs for the same procedure on several occasions to demonstrate progress Resources Required Scheduled appraisals Attendance at local/regional Teaching Programme Time set aside for WBA’s with Educational Supervisor Learning Opportunities Insert timetable, emphasising the best opportunities incl clinics, theatres, WR, admin and MDT’s. A typical WTE weekly timetable may include: 5 consultant lead sessions per week Ward rounds, some with consultant supervision theatre sessions, at least 1 clinic, MDT Urodynamics and subspecialist clinics 1 admin session, 1 study/ teaching session, Other sessions dependent on training requirements Regional audit/ research meetings Exams FRCS Paeds – note change in regulations from 2010 ( or FRCS Urol for Urology trainees) Courses & Conferences BAPU Congress ESPU Contact paediatric@rcseng.ac.uk Audits/Research/Projects Part 3: Comments & Sign Off