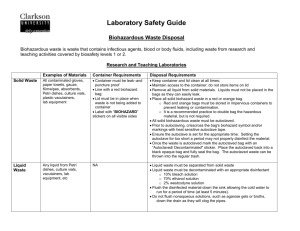
Disposal of Contaminated Sharps
advertisement

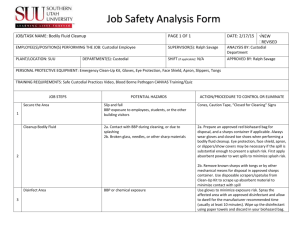
ARLINGTON FIRE DEPARTMENT STANDARD OPERATING PROCEDURES ISSUED: MARCH 2002 MEDICAL OPERATIONS INFECTION CONTROL 205.03 PURPOSE The purpose of this procedure is to provide an organizational outline for the prevention and control of infectious diseases and the reporting of potential exposures. PREVENTIVE AND CONTROL MEASURES Body Substance Isolation Because emergency services personnel are often unable to determine if body substances have the potential to be infectious, all persons should be assumed to have a communicable disease and all of their body substances should be considered infectious. AFD personnel shall use barrier techniques such as personal protective equipment (gloves, masks, gowns, etc.) to prevent contact with blood or other potentially infectious substances. Personal Protective Equipment and Supplies Gloves* - Wear disposable, nonporous gloves any time potential exists for contact with blood, body fluids, non-intact skin, or other potentially infectious material. Clean hands with soap and water as soon as possible after removing gloves, even if gloves appear intact. When wearing soiled gloves, avoid handling items such as ink pens, steering wheels, portable radios, or clipboards that will later be touched with ungloved hands. Eye Protection* - Use these any time splash contact with the face is possible. You may apply the facemask to anyone who is transported and who is/has coughing, sneezing, fever or otherwise engaging in behavior so that airborne pathogens are likely to be expelled. Gown* - Wear when a need exists to protect your clothing from contact with body fluids. Masks* - Should be worn by the caregivers or the patient for those infectious agents known to be transmitted by the airborne route (i.e., tuberculosis, chicken pox, measles, etc.). Sufficient information should be obtained to determine if a patient may have active tuberculosis (TB), recent history of TB, HIV infection, fever, recent weight loss or cough. If there is a history suggestive of active TB, caregivers should wear masks compatible with OSHA guidelines. Pocket masks with one-way valves or positive pressure ventilators should be used for artificial respiration whenever possible. * The use of gowns, masks, eye protection and gloves should be determined based on the level of exposure likely to be encountered. Disposal of Contaminated Sharps Fire Department members are responsible for protecting themselves, one another, and the public from exposure to pathogens through accidental injury by contaminated needles and other sharp objects. To accomplish this, contaminated sharps should never be left on a scene regardless of which agency may have originally been responsible for the item. Needles and other sharp objects should be considered as potentially infected and should be handled with extraordinary care. Needles should not be recapped. If it is absolutely necessary to recap a needle, use the one hand method. Needles, syringes and broken glass vials should be immediately placed in puncture-proof containers after use. The goal of this policy is to eliminate members’ carrying contaminated sharps containers in fanny packs or EMS bags, thus decreasing the risk of a container’s contents spilling. Only sharp items should be placed in sharps containers. Other contaminated items should be placed in a red, biohazard bag. Page 1 of 4 ARLINGTON FIRE DEPARTMENT STANDARD OPERATING PROCEDURES ISSUED: MARCH 2002 MEDICAL OPERATIONS INFECTION CONTROL 205.03 Single-use sharps containers Each member shall carry a single-use sharps container in the fanny pack. Single-use sharps containers may never be emptied and reused. After placing a sharp in a single use container, it shall be discarded in a multiuse container or station biohazard container as soon as possible/practical. The intent is to avoid packing several sharps in the single-use container, regardless if it is in a fanny pack or EMS equipment case, in the course of multiple incidents/responses. Multi-use sharps containers Every apparatus that responds to EMS calls will carry a multi-use sharps container. This container shall serve as a receptacle for used single-use sharps containers and contaminated sharps that will not fit in the single-use container. It shall be carried in the EMS cabinet or compartment. It shall be closed and secured in such way that the contents will not be ejected during daily activities or a vehicle accident, including an incident during which the apparatus rolls over. When a multi-use container is first placed on the apparatus, the date shall be written in plain view on the container. The container shall be discarded in the station biohazard trash and replaced when half full, 60 days after being placed in service, or 60 days after the date on the container; whichever comes first. Containers still empty after 60 days may have the date changed to reflect another 60-day period. Disposal of contaminated EMS supplies Biohazard Waste Bags Each Fire apparatus should carry a red plastic “BIOHAZARD” bag in their designated EMS compartment. Personnel shall use these plastic bags to dispose of items such as used gloves, 4” x 4”s, and other trash items from the scene of EMS runs that are contaminated with blood or other body fluids. Plastic bags that are either red in color or contain the red biohazard label. Dispose of biohazard bags and their contents by placing them in the biohazard waste containers at Fire stations or hospitals. The state law prohibits the disposal of items contained in biohazard bags along with non-medical trash. These plastic bags shall be used in the following manner: 1. The bags may be used to hold accumulated disposable items from multiple EMS runs, as long as the items placed in the bags are not contaminated with blood or other body fluids. Once the bag is full, remove it, tie it, and place it in the biohazard container at the station. 2. If items contaminated with blood or other body fluids are placed in the bag, remove and seal the bag immediately and place it in the biohazard container at the station. Under no circumstances are items contaminated with blood or other body fluids to be disposed of through routine trash containers. Contact Resource Management for removal of the biohazard waste container when it is half full. This will provide Resource Management with sufficient time to empty the container before it becomes full. Other Protective Measures Uniform Care Employees whose uniforms become soiled with blood or other body fluids should change clothes as soon as possible to prevent cross contamination. Place the dirty uniform in a biohazard bag and launder separately from other clothing using normal laundry cycles and detergent. The use of unusually hot water or bleach is not necessary. Bleach will destroy Nomex uniforms and PBI bunker gear. Page 2 of 4 ARLINGTON FIRE DEPARTMENT STANDARD OPERATING PROCEDURES ISSUED: MARCH 2002 MEDICAL OPERATIONS INFECTION CONTROL 205.03 Skin Care Covering any laceration or other area of non-intact skin with a bandage, even if later covered with gloves, will significantly decrease the risk of occupational exposure to communicable diseases. Hands should always be washed with soap and water after every patient contact even if gloved. EQUIPMENT CARE AND CLEANING A patient should never be exposed to another patient’s bodily fluids when under the care of the Arlington Fire Department. Every attempt should be made to remove blood and other contaminants from reusable EMS equipment (i.e. backboards, blood pressure cuffs, etc.) after each EMS incident in order to prevent cross contamination. Those items should be cleaned thoroughly with a 10% bleach solution or by using an equipment disinfectant supplied by Resource Management. Equipment that is unable to be cleaned of all visible blood and or body fluids should be taken out of service and replaced as soon as possible. EXPOSURES Exposures to blood and other body fluids pose a significant risk to the health and safety of EMS providers. These exposures can be a direct result of patient contact, contact with a device containing blood or body fluids used in patient care or indirect contact with a patient’s blood or body fluids. Either way, exposures of any kind must be identified and treated as quickly as possible. Post-Exposure Incident Procedures In the event a member is exposed while on duty, it is imperative that the exposed member along with his/her supervisor follows the appropriate steps in order to receive the appropriate care. Member’s Responsibilities: 1. Immediately cleanse the exposed area. a. b. For exposures to non-intact skin or a percutaneous exposure to blood or body fluids, immediately wash the exposed area thoroughly with soap and water. If soap and water is not available, immediately remove as much of the substance as possible and use an antiseptic hand cleaner. Follow with soap and water as soon as possible. For exposures to the eyes, nose, or mouth to blood or other body fluids, flush the eyes/nose with water, rinse out the mouth with water. 2. Immediately notify the Supervisor. 3. Immediately notify your on-duty Battalion Chief for referral to the appropriate facility. 4. Complete a Report of Potential Exposure Form and arrange for Notary’s signature. Return to Fire Administration. Must be completed by next business day. 5. Complete The City of Arlington Workers Compensation Injury Form (Only if associated with a needle stick or injury.) Return the original to Human Resources, a copy to Fire Administration. Must be completed by next business day. 6. Complete The City of Arlington Report of Possible Exposure of Transporter Form. Leave it with the attending physician or nurse at the hospital. 7. If contaminated sharps are involved, complete a Texas Department of Health Contaminated Sharps Reporting Form. Return to Fire Administration. Must be completed by next business day. Page 3 of 4 ARLINGTON FIRE DEPARTMENT STANDARD OPERATING PROCEDURES ISSUED: MARCH 2002 MEDICAL OPERATIONS INFECTION CONTROL 205.03 8. Complete an Exposure Pre-Alert Notification Form. completed by next business day. Return to Fire Administration. 9. Notify CIGNA Integrated Care 1-800-937-8535 10. Contact the Medical Operations Battalion Chief for follow-up care referral. Must be Battalion Chief’s Responsibilities: 1. Either transport our member to the hospital or meet our member at the hospital.* 2. Ask for the Charge Nurse. Inform them of the situation. Our member should be fast-tracked through Triage and Registration. Be discreet; we are receiving priority attention over many people in the waiting area. 3. A physician or Infection Control Nurse should see our member. The course of treatment will depend on the source patient, degree of exposure, and condition of our member. 4. Assure completion of a Report of Potential Exposure Form and arrange for Notary’s signature. Return to Fire Administration. Must be completed by next business day. 5. Assure completion of a The City of Arlington Workers’ Compensation Injury Form. (Only if associated with a needle stick or injury.) Return the original to Human Resources, a copy to Fire Administration. Must be completed by next business day. 6. Assure completion of The City of Arlington Report of Possible Exposure of Transporter Form. Leave with the attending physician or nurse at the hospital. 7. If contaminated sharps are involved, assure completion of the Texas Department of Health Contaminated Sharps Reporting Form. Return to Fire Administration. Must be completed by next business day. 8. Assure completion of an Exposure Pre-Alert Notification Form. Return to Fire Administration. Must be completed by next business day. 9. Assure notification of CIGNA Integrated Care 1-800-937-8535 10. Notify the Medical Director by pager 817-227-5888. Medical Operations Responsibilities: 1. Provide support and assistance to employee. 2. Insure all paperwork has been completed and turned in to the appropriate facility. 3. Document event in the exposure database. 4. Coordinate with hospitals and the Tarrant County Health Department. 5. Coordinate follow-up testing and treatment with the employee and appropriate facility. Note: *Our member should when possible, go to the same hospital as the source patient. If not possible, go to one of the Arlington hospitals for testing. Page 4 of 4