DysGeneExpDis2009
advertisement

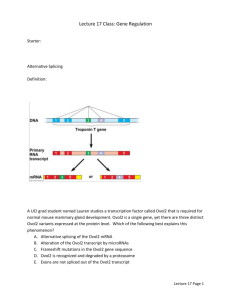
Dysregulation of Gene Expression in Disease States Cell Pathology December 7, 2009 Dr. Coffman I. Gene expression – more than just transcription A. Components of gene expression 1. Transcription a. Synthesis or pre-mRNA b. Transcription factors c. Chromatin structure supporting or repressing transcription (epigenetics) 2. Post-transcriptional modifications a. RNA splicing b. Transcript stability c. Capping and tailing 3. Translation a. Initiation, elongation, termination b. Transcript utilization c. Proper folding (proteasome degradation of misfolded proteins) 4. Post-translational modification a. Protease cleavage b. Phosphorylation, methylation, acetylation, ADP ribosylation, glycosylation, and other covalent additions c. Assembly of multisubunit proteins (identical and different subunits) 5. Secretion and other spatial concerns a. Protein trafficking to membrane or vesicle b. Compartmentalization of proteins in the cytoplasm or nucleus B. Common dysregulations of gene expression 1. Over and underexpression of specific proteins or RNA a. Too much or too little of a particular macromolecule 2. Expression of mutant RNA or protein a. Loss of function b. Loss of normal regulation 3. Altered modification or processing 4. Incorrect localization or trafficking of proteins C. Disturbing a complex web 1. Relationships among signaling and regulatory pathways 2. Alterations of one gene product lead to alterations in other gene products 3. Extra copies of normal chromosomes disrupt normal relationships 4. Overactive responses often create more serious consequences than the initial problem II. Dysregulation of transcription A. Transcription of mutant genes 1. Neoplasias a. erbB/neu b. bcr-abl c. p53 2. Sickle cell anemia a. Glutamic acid to valine substitution causes hemoglobin aggregation b. Diminished glutathione allows disulfide bonds to form in spectrin filament network that freeze erythrocytes in aberrant shape c. Heterozygote carriers have resistance to malaria 3. Cystic fibrosis a. Defect in chloride channel causes aberrant ion secretion b. Heterozygote carriers have resistance to cholera 4. Marfan’s syndrome a. Family of diseases caused by defect in collagen expression b. Most serious defect creates weak aortic walls that can rupture 5. Duchennes muscular dystrophy a. Defect in dystrophin gene on X chromosome (male get the disease, females are carriers) b. Dystrophin is part of T-tubule network and is involved in calcium release c. Disease causes progressive muscle weakness and muscle atrophy, patients usually die before age 20 B. Abnormal production of normal gene products 1. Large changes due to mutations in gene promoters a. Cancer-related c-myc and N-myc upregulations 2. Subtle changes due to promoter polymorphisms 3. Diseases related to epigenetics a. Prader-Willi Syndrome 1) Due to deletion on paternal chromosome 15 2) Homologous region on maternal chromosome 15 silenced b. Fragile X – an epigenetic disease 1) Expansion of trinucleotide repeat from 40 (normal) to 80 (threshold of disease) to many thousands (severe disease) 2) Over 200 repeats results in chromatin methylation and gene silencing 3) Wide range of symptoms – more repeats corresponds with more severe disease 4) Protein product is RNA-binding protein FMR1, likely affects transcription of other genes C. Molecular misreading - production of mutant gene products from normal (wild-type) genes 1, Dinucleotide deletions result in +1 proteins 2. +1 APP and UBB proteins found in Alzheimer’s Disease plaques III. Between transcription and translation A. Splicing errors 1. Splicing mechanism requires DNA sequences and specific binding proteins 2. Mutations in either splicing proteins or DNA splicing sites results in truncated or nonsense proteins 3. Alternative splicing – can make several proteins from a single gene a. Over 70% of human genes can be alternatively spliced b. Myotonic Dystrophy – a disease of dysregulated alternative splicing B. Message stability and degradation 1. Regulated by proteins binding to AU-rich elements in 3’ untranslated region C. Capping and polyA addition 1. mRNA cap-binding protein eIF4E upregulated by c-myc IV. Translation and beyond A. Protein synthesis 1. Misincorporations result in misfolded protein that is degraded 2. More efficient than halting translation after misincorporation B. Protein folding and misfolding 1. Chaperone roles in protein folding 2. Misfolded proteins and disease C. Protein modifications 1. Disease states produce signature changes in patterns of post-translational modifications D. Protein transport and localization 1. Overexpressed proteins exist in inappropriate places 2. Transformed cells express inappropriate proteins V. Extra copies of normal chromosomal A. Trisomy 21 (Down Syndrome) 1. Extra copy of chromosome 21 2. Small region of chromosome (containing perhaps 20-30 genes) responsible for the syndrome (21q22) ` 3. Symptoms (partial list) - moderate to severe mental retardation (IQ 40-45), cranial and facial abnormalities, epicanthic folds, short fingers, absence of whorl on ball of foot, cardiac murmur (50%), mitral valve prolapse, seizure disorder, conduct disorders (self-talk), Alzheimer’s Disease prevalence (30-75% by age 60), increased chance of leukemia B. Trisomy 18 (Edward’s Syndrome) 1. Extra copy of chromosome 18, occurrence 1/3000 live births 2. 90% die within the first year 3. Symptoms a. Heart defects: hole between upper or lower heart chambers b. Microcephaly c. Abnormalities of lungs, diaphragm, kidneys, ureter C. Trisomy 13 (Patau Syndrome) 1. Extra copy of chromosome 13, occurrence 1/5000 live births 2. 50% die within first month 3. Symptoms a. Severe mental retardation b. Seizures c. Microcephaly D. Klinefelter’s Syndrome 1. XXY sex chromosome complement 2. Most common chromosomal aneuploidy VI. Inflammation and repair – changes in gene expression in response to infection A. Changes in gene expression with the inflammatory response 1. Proinflammatory cytokines - TNF, IL-I, IL-6 2. Release of small molecules – histamine, prostaglandins and leukotrienes B. Septic shock – fatal reaction to bacterial infection 1. Bacterial superantigen activates T cells to produce IL-1 2. IL-1 and bacterial LPS induce macrophage TNF release 3. High systemic TNF leads to systemic vascular permeability and plummeting blood pressure