Syllabus - College of Nursing
advertisement

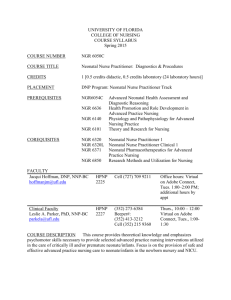
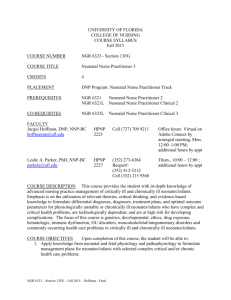
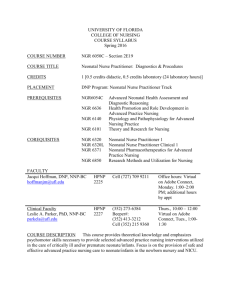
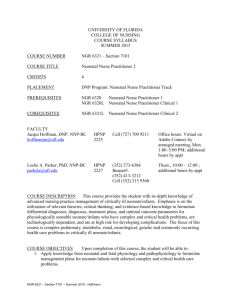
COLLEGE OF NURSING COURSE SYLLABUS Fall 2011 COURSE NUMBER NGR 6320C section 7740 COURSE TITLE Neonatal Care I CREDITS 2 PLACEMENT First Course in Neonatal Care Track PRE/Co-REQUISITE NGR 6101: Theory and Research for Nursing NGR 6020C: Advanced Neonatal Health Assessment and Diagnostic Reasoning NGR 6140: Physiology and Pathophysiology for Advanced Nursing Practice NGR 6636: Health Promotion and Role Development in Advanced Practice Nursing (1 credit didactic, 1 credit laboratory) FACULTY (352) 273-6384 Beeper#: (352) 413-3212 Cell (352) 215 9360 Thurs., 10:00 – 12:00 Virtual on elluminate Tues., 12:00-12:30 Sheryl Montrowl, MSN, NNP-BC montrsj@peds.ufl.edu Beeper# 352 413-2619 Available by appt Julie Schultz, MSN, NNP Julieannschultz@yahoo.com Cell: 954 260 0071 Available by appt Jacqui Hoffman, DNP, NNP-BC Hoffmanjm@ufl.edu Cell (727) 709 9211 Available by appt Office 352-273-6366 Available by appt Leslie A. Parker, PhD, NNP-BC parkela@ufl.edu DEPARTMENT CHAIR Susan Schaffer, PhD, ARNP-BC Department Chair sdschaf@ufl.edu Gainesville Campus HPNP 2227 HPNP 2229 NGR 6320C COURSE OUTLINE PAGE 2 CAMPUS DIRECTOR JAX Andrea Gregg, DSN, RN Associate Professor greggac@nursing.ufl.edu Jacksonville Campus JAX LRC, 3rd Floor Office: 904-244-5172 Fax: 352-273-6568 Available by appt COURSE DESCRIPTION This course provides advanced study of neonatal intensive care nursing for low risk term and preterm neonates. Emphasis will be on fetal growth and development, neonatal nursing care, and the role of the neonatal nurse practitioner in low risk neonatal care. COURSE OBJECTIVES Upon completion of this course, the student will be able to: 1. Analyze the genetic and environmental variables associated with congenital defects and/or spontaneous abortion. 2. Integrate theory and current research findings pertaining to fetal and neonatal physiology and pathophysiology, perinatal development, low risk term and preterm neonates and families, and therapeutic approaches for the management of neonatal health problems. 3. Direct the care of low risk term and preterm neonates, in collaboration with other members of the health care term. 4. Provide care to low risk term and preterm neonates in neonatal intensive care settings. 5. Analyze the influence of ethical, legal, political, economic, and sociocultural factors on the provision of care to neonates and their families. COURSE SCHEDULE Class Day On-line Time Room Tuesday 8-12 on elluminate Clinicals: TBA E-Learning in Sakai is the course management system that you will use for this course. ELearning in Sakai is accessed by using your Gatorlink account name and password at http://lss.at.ufl.edu. There are several tutorials and student help links on the E-Learning login site. If you have technical questions call the UF Computer Help Desk at 352-392-HELP or send email to helpdesk@ufl.edu. It is important that you regularly check your Gatorlink account email for College and University NGR 6320C COURSE OUTLINE PAGE 3 wide information and the course E-Learning site for announcements and notifications. Course websites are generally made available on the Friday before the first day of classes. ATTENDANCE Students are expected to be present for all scheduled classes, other learning experiences, and examinations. Students who have extraordinary circumstances preventing attendance should explain these circumstances to the course instructor prior to the scheduled class or as soon as possible thereafter. Instructors will then make an effort to accommodate reasonable requests. A grade penalty may be assigned for late assignments, including tests. Students are responsible for responding to online assignments as part of their attendance. Make-up exams may not be available in all courses. Students are expected to be present for all scheduled clinical practice experiences and seminars. Students who have extraordinary circumstances preventing attendance should explain these circumstances to the course instructor prior to the scheduled clinical practice experience or seminar. Instructors will then make an effort to accommodate reasonable requests. A grade penalty may be assigned for unexcused seminar or clinical absences. The faculty member will advise the method of notification for absences to the clinical site e.g. phone, email, and notification of facility. Graduate students are required to submit a written calendar of planned clinical practice dates and times to the course faculty member prior to beginning the clinical rotation. Any changes to the calendar (dates and times) must be submitted in writing to the course faculty member before the change is planned to occur. Clinical hours accrued without prior knowledge of the faculty member will not be counted toward the total number of clinical hours required for the course. ACCOMMODATIONS DUE TO DISABILITY Each semester, students are responsible for requesting a memorandum from the Disability Resource Center to notify faculty of their requested individual accommodations. This should be done at the start of the semester. STUDENT HANDBOOK Students are to refer to the College of Nursing Student Handbook for information about College of Nursing policies, honor code, and professional behavior. TOPICAL OUTLINE 1. Patterns of embryological and fetal growth and development and the genetic and environmental variables which influence those patterns (Obj.# 2,3,4) NGR 6320C COURSE OUTLINE PAGE 4 2. 3. 4. 5. Health maintenance and anticipatory care of the low risk term and preterm neonate, pharmacologic and nutritional variations related to those clients (Obj.# 4,5,6) Intrapartal adaption from intrauterine fetal physiology, resuscitation measures at time of delivery (Obj.# 1,4,5) The perinatal family and their adaptation to the crisis of the birth and possible hospitalization of a healthy neonate (Obj.# 4,5) Immunological factors related to the neonate, neonatal sepsis, antibiotic therapy, and infection control in neonatal care units (Obj.# 1,2,4,5) TEACHING METHODS Lecture, discussion, case studies and case presentations, faculty supervised clinical practice, written materials, computer assisted instruction and audiovisual materials, and individual conferences. LEARNING ACTIVITIES Case studies and case presentations, discussions, exams, faculty supervised clinical practice EVALUATION Minimum Required Contact Hours: 48 Clinical experience will be evaluated through faculty observation, verbal communication with the student, written work, and agency staff reports using a College of Nursing Clinical Evaluation Form. Faculty reserve the right to alter clinical experiences, including removal from client care areas, of any student to maintain patient safety and to provide instructional experiences to support student learning. Clinical evaluation will be based on achievement of course and program objectives using a College of Nursing Clinical Evaluation Form. All areas are to be rated. A rating of Satisfactory represents satisfactory performance and a rating of Unsatisfactory represents unsatisfactory performance. The student must achieve a rating of Satisfactory in each area by completion of the semester in order to achieve a passing grade for the course. A rating of less than satisfactory in any of the areas at semester end will constitute a course grade of E. Regardless of the classroom grade, the student receiving an Unsatisfactory evaluation in the clinical component of the course will be assigned a course grade of E or U. The faculty member will hold evaluation conferences with the student and clinical preceptor, if applicable, at each site visit. The faculty member will document or summarize each conference on the Clinical Evaluation Form or Incidental Advisement Record. This summary will be signed by the faculty member and student. Mid-rotation evaluation conferences will be made available to each student. Final evaluation conferences with the faculty member are mandatory and will be held during the last week of each semester. A student may request additional conferences at any time by contacting the faculty member. NGR 6320C COURSE OUTLINE PAGE 5 Students enrolled in advanced practice courses with a clinical component will use Clinical Experience Form F to document clinical experience including hours, practice location and preceptor for their personal records. Students also assess their learning experiences using Clinical Site Assessment Form G. Completed Form G is collected by the faculty member and submitted to the Coordinator of Clinical Resources at the College. At the end of the clinical experience the student completes a self-evaluation and the faculty member completes a student evaluation using the College of Nursing Clinical Evaluation Form. Course work will be evaluated by written examinations and written assignments. Clinical performance will be graded on satisfactory/unsatisfactory basis. Students must achieve a satisfactory grade in the clinical area in order to successfully complete the course. Test I Test II Test III Class Participation 25% 25% 25% 25% September 27th 2:00 November 8th 2:00 December 13th 2:00 Testing must be scheduled and proctored through a testing center such as Sylvan or proctored by a UF faculty person. All tests will be graded and returned to the student within 2 weeks. CRITERIA FOR CLASS PARTICIPATION You are expected to complete the following assignments. 1. Logs A weekly log is expected and is due each Friday by 5:00pm on the course Sakai web site. This log should include: a. b. c. d. e. f. g. A short description of your patients What care you provided each patient Procedures Ethical dilemmas (if any were encountered) Problems with staff, preceptor, faculty Problems which may need discussion with faculty preceptor Goals for next week Assigned clinical faculty will respond to each log on the Sakai web site. It is expected that you respond via Sakai E-mail to all Questions. Failure to complete logs in a timely manner may result in an unsatisfactory Clinical evaluation. NGR 6320C COURSE OUTLINE PAGE 6 2. Case Studies There will be (5) case study assignments which you will be required to analyze. I will distribute these via e-mail on the following dates: September 5th, September 26th, October 3rd, October 17th, and November 7th. You will have 2 weeks to complete. This is a clinical tool; therefore, there is no need for APA format. Please answer the questions as if you were the NNP caring for the patient. Each student will return this assignment for feedback from the instructors. The student will then incorporate this feedback into the case study. This process will continue until the case study is in an acceptable format. 3. You will also be required to place an entry at least 4 times per week on the Sakai discussion board. This may include submitting new items for discussion or to discuss an issue already introduced. This is a required aspect of the class participation grade. 4. The student’s attendance sheet must be completed and returned prior to ALL scheduled evaluations. 5. All clinical experiences need to be scheduled through me. If you schedule clinical on an unauthorized day you will not receive credit for those hours. GRADING SCALE A AB+ B BC+ 95-100 (4.0) 93-94 (3.67) 91- 92 (3.33) 84-90 (3.0) 82-83 (2.67) 80-81 (2.33) C CD+ D DE 74-79* (2.0) 72-73 (1.67) 70-71 (1.33) 64-69 (1.0) 62-63 (0.67) 61 or below (0.0) * 74 is the minimal passing grade REQUIRED TEXTS Kenner, C. and Lott J.W. (2007). Comprehensive Neonatal Care. (5th ed). Elsevier. ISBN:978-1-4160-2942-7 Gomella, T. L. , Cunninham, M.D., & Eyal, F.G. (2003). Neonatology management, procedures, on call problems, diseases and drugs. McGraw-Hill Professional Publishing. ISBN: 9780071389181. Moore, K. Persuad, T.V.D. (2008). The developing human (8th ed.). Elsevier. ISBN: 10-0721601316. NGR 6320C COURSE OUTLINE PAGE 7 WEEKLY CLASS SCHEDULE Date Topic Reading/ Online Lectures August 15th , 16th and 17th (All day classes) Orientation Week 1-3 August 23rd and 30th Sept 6th THE PREGNANCY AT RISK: Perinatal Risk Factors, Evaluation of Fetal Maturity and Well-Being, Fetal Distress, Intrauterine Resuscitation, Congenital Infections Askin, D.F. (2001). Intrauterine infections. Neonatal Network. 23(5). 23-30. Chang, M.H. (2007). Hepatitis B virus infection. Seminars in Fetal and Neonatal Medicine. 12(3), 160-167. Kenner and Lott Chpt 37 Gomella. Chapter 1, 61. Walker (2007). Congenital syphilis: a continuing but neglected problem. Seminars in fetal and neonatal medicine, 12(3), 198 Week 4-6 Sept 13th, 20st, and 27th NEONATAL SEPSIS: Risk Factors, Immune Response, Early and Late Onset, Infection Control in NICUs Human Development: The beginnings of human development: The first week Clark, R. (2004). Prevention and treatment of nosocomial infections. Journal of Perinatoology, 24, 446-453/ Kenner and Lott chp 9 Gomella. Chapter 61. Enright, (2002) Neonatal herpes infection: diagnosis, treatment & prevention. Seminars in neonatology 7 283-291 Moore: Chp 1 and 2 Procedure lab NGR 6320C COURSE OUTLINE PAGE 8 Week 7,9,10 Oct 4th, 18th, 25th MANAGEMENT OF RESPIRATORY PROBLEMS I: Respiratory Function; Problem Identification, Management, and Evaluation; Respiratory Distress Syndrome; Meconium Aspiration; TTN; Airleaks. Embryology: Formation of the bilaminar embryonic disc and chorionic sac: The second wk Kenner and Lott chp 1 Gomella. Chapters 6, 9, 67.Moore: Chapter 3 Wiedemann (2008). Meconium aspiration syndrome. Neonatal Network, 27(2), 81-7. Aly, H. (2004). Respiratory Disorders in the Newborn: Identification and Diagnosis. Pediatr. Rev. 25, 201-208 Week 8 October 11th No Class: Work on Case studies FANNP Conference Week 11, 12, 13 Nov 1st, 8th and 15th PERINATAL ADAPTATION: Delivery Room Resuscitation, Transition to Extrauterine Life, Kenner and Lott Chpt 38 Gomella. Chapter 2. Moore Chapter 4 Sansoucie,(1997). Transition from fetal to extrauterine circulation. Neonatal Network, 16(2), 5-12. Parker, L. (2005). Early recognition and treatment of birth trauma: injuries to the head and face. Advances in Neonatal Care. 5(6):288-97. Bradshaw (2006). A nurses guide to early detection of UVC catheter complications in infants. Advances in Neonatal Care, 6(3), 127-138 Human Development: Formation of germ layers and early tissue and organ differentiation: The third week Week 14, 15, 16 Nov 22nd, 29th, Dec 6th PROBLEMS OF IMMATURITY: Nutritional Support, Health Maintenance, Apnea, PDA. Chow, (2008). Fluid and electrolyte management in the premature infant, Neonatal Network, 27(6), 379 Evans, N. (2003) . Current D:\106735468.doc NGR 6320C COURSE OUTLINE PAGE 9 Human Development: The organogenic period controversies in the diagnosis and treatment of patent ductus arteriosus in preterm infants. Adv Neonatal Care. 2003, 3(4):168-77. Kenner and Lott chpt 15 Gomella. Chapters 7, 8, 10. Moore Chpt 5 Stokowski, (2005). A primer on apnea of prematurity. Adv Neonatal Care.5(3), 155-70. Hantroll, G. Basic principles and practical steps in the management of fluid balance in the newborn. Seminars in neonatology 2003. 8, 307-313 Kuzma-O’reilly (2003). Evaluation, development and implementation of potentially better practices in neonatal intensive care nutrition. Pediatrics, 111(4). E461. Week 17 Week of Dec 12th Finals week D:\106735468.doc NGR 6320C COURSE OUTLINE PAGE 10 Student Attendance Sheet Name: Date Hours in Clinical Unit # of Critically Ill Patients # of moderately ill infants # of Stable Patients # of convalescing infants Preceptor Signature D:\106735468.doc NGR 6320C COURSE OUTLINE PAGE 11 Definitions for types of patients cared for 1. Convalescing infant: An infant requiring minimal care. Examples: infants on full feedings, newborn infants, full term infants on antibiotic therapy, late preterm infants working on po feedings, stable infants with uncomplicated hyperbilirubinemia 2. Stable infants: An infant requiring critical care but is stable. Examples: Infants on nasal cannula, infants on nasal cannula and TPN. 3. Moderately ill infants: An infant requiring significant amounts of critical care: post op infants, infants admitted with significant illness. Examples: infants on CPAP, infants on stable vent settings 4. Critically ill infants: An infant requiring extensive care. Examples: infants on ventilators requiring frequent vent changes, infants on pressor support, infants with rapidly changing clinical status D:\106735468.doc NGR 6320C COURSE OUTLINE PAGE 12 Procedure Log Procedure Date/preceptor initial Intubation UAC placement UVC placement CT insertion Needle aspiration of pneumothorax Suprapubic bladder aspiration Delivery room attendance PICC line placement Lumbar puncture PAL placement Arterial blood draw D:\106735468.doc