Multiple organ dysfunction syndrome
advertisement

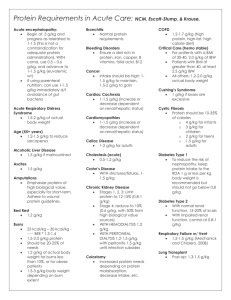
Multiple organ dysfunction syndrome Multiple organ dysfunction syndrome (MODS), previously known as multiple organ failure (MOF), is altered organ function in an acutely ill patient requiring medical intervention to achieve homeostasis. The use of "multiple organ failure" should be avoided since that term was based upon physiologic parameters to determine whether or not a particular organ was failing. Origin Originally patients were classified as having sepsis or the sepsis syndrome. This resulted in two concepts: the systemic inflammatory response syndrome (SIRS) and multiple organ dysfunction syndrome (MODS). Definition Multiple organ dysfunction syndrome is the presence of altered organ function in acutely ill patients such that homeostasis cannot be maintained without intervention. It usually involves two or more organ systems. Etiology The condition usually results from infection, injury (accident, surgery), hypoperfusion and hypermetabolism. The primary cause triggers an uncontrolled inflammatory response. In operative and non-operative patients sepsis is the most common cause. Sepsis may result in septic shock. In the absence of infection a sepsis-like disorder is termed systemic inflammatory response syndrome (SIRS). Both SIRS and sepsis could ultimately progress to multiple organ dysfunction syndrome. However, in one-third of the patients no primary focus can be found. Multiple organ dysfunction syndrome is well established as the final stage of a continuum Systemic inflammatory response syndrome -> sepsis ->severe sepsis ->Multiple organ dysfunction syndrome. Currently, investigators are looking into genetic targets for possible gene therapy to prevent the progression to Multiple organ dysfunction syndrome. Some authors have conjectured that the inactivation of the transcription factors NF-κB and AP-1 would be appropriate targets in preventing sepsis and Systemic inflammatory response syndrome. These two genes are pro-inflammatory. However, they are essential components of a normal healthy immune response, so there is risk of increasing vulnerability to infection, which can also cause clinical deterioration. Some have developed a mouse model sepsis via cecal ligation and puncture (CLP). Male Balb/c mice subjected to CLP were given an IL-10-carrying vector or an empty control vector. Lung, Liver and kidney tissue destruction were measured by assessing myeloperoxidase and malonialdehyde activity. These last two are endogenous oxidizing compounds produced during tissue inflammation. The authors assessed the level neutrophil infiltration in lung and liver tissue. IL-10 protein expression was measured using immunohistochemistry. The expression of Tumor necrosis factor-alpha mRNA was measured at 3,8, and 24 hours after CLP using reverse transcription polymerase chain reaction. Their results show significantly reduced organ damage by IL-10 gene transfer, as quantified by reduced myeloperoxidase activity in the lung, liver, and kidney. The malonialdehyde level was not affected by the transfer into the liver. The livers of the mice infected with the adenoviral vector showed reduced neutrophil activity. The lung and kidney samples in mice carrying the gene showed lower expression of Tumor necrosis factor-alpha mRNA. The investigators concluded that increased IL-10 expression significantly reduced sepsis-induced Multiple organ injury. Pathophysiology A definite explanation has not been found. Local and systemic responses are initiated by tissue damage. Respiratory failure is common in the first 72 hours after the original insult. Following this one might see hepatic failure (5-7 days), gastrointestinal bleeding (10-15 days), and renal failure (11-17 days) Gut hypothesis The most popular theory to explain MODS in critically ill patients is the gut hypothesis. Due to splanchnic hypoperfusion and the subsequent mucosal ischaemia there are structural changes and alterations in cellular function. This results in increased gut permeability, changed immune function of the gut and increased translocation of bacteria. Hepatic dysfunction leads to toxins escaping into the systemic circulation and activating an immune response. This results in tissue injury and organ dysfunction. Endotoxin macrophage theory Gram-negative infections in MODS patients are relatively common, hence endotoxins have been advanced as principal mediator in this disorder. It is thought that following the initial event cytokines are produced and released. The pro-inflammatory mediators are: tumor necrosis factor-alpha (TNF-α), interleukin-1, interleukin-6, thromboxane A2, prostacyclin, platelet activating factor, and nitric oxide. Tissue hypoxia-microvascular hypothesis As a result of macro- and microvascular changes insufficient supply of oxygen occurs. Hypoxemia causes organ dysfunction and cell death. Integrated hypothesis Since in most cases no primary cause is found, the condition could be part of a compromised homeostasis involving the previous mechanisms. Diagnosis The European Society of Intensive Care organized a consensus meeting in 1994 to create the "Sepsis-Related Organ Failure Assessment (SOFA)" score to describe and quantitate the degree of organ dysfunction in six organ systems. Using similar physiologic variables the Multiple Organ Dysfunction Score was developed. Four clinical phases have been suggested: Stage 1 the patient has increased volume requirements and mild respiratory alkalosis which is accompanied by oliguria, hyperglycemia and increased insulin requirements. Stage 2 the patient is tachypneic, hypocapnic and hypoxemic. Moderate liver dysfunction and possible hematologic abnormalities. Stage 3 the patient develops shock with azotemia and acid-base disturbances. Significant coagulation abnormalities. Stage 4 the patient is vasopressor dependent and oliguric or anuric. Ischemic colitis and lactic acidosis follow. Management At present there is no agent that can reverse the established organ failure. Therapy therefore is limited to supportive care, i.e. safeguarding hemodynamics, and respiration. Maintaining adequate tissue oxygenation is a principal target. Starting enteral nutrition within 36 hours of admission to an Intensive care unit has reduced infectious complications. Human recombinant activated protein C(activated drotrecogin alfa) can reduce 28-day mortality among patients with multiple organ dysfunction syndrome according to a randomized controlled trial. The relative risk reduction was 21.8%. For patients at similar risk to those in this study (33.9% had 28-day mortality), this leads to an absolute risk reduction of 7.4%. 13.5 patients must be treated for one to benefit. Prognosis Mortality varies from 30% to 100% where the chance of survival is diminished as the number of organs involved increases. Since the 1980s the mortality rate has not changed. See also Acute renal failure Acute respiratory distress syndrome Heart failure Intensive care Liver failure Respiratory insufficiency Shock systemic inflammatory response syndrome Acute renal failure Acute renal failure (ARF), also known as acute kidney failure or acute kidney injury, is a rapid loss of renal function due to damage to the kidneys, resulting in retention of nitrogenous (urea and creatinine) and non-nitrogenous waste products that are normally excreted by the kidney. Depending on the severity and duration of the renal dysfunction, this accumulation is accompanied by metabolic disturbances, such as metabolic acidosis (acidification of the blood) and hyperkalaemia (elevated potassium levels), changes in body fluid balance, and effects on many other organ systems. It can be characterised by oliguria or anuria (decrease or cessation of urine production), although nonoliguric ARF may occur. It is a serious disease and treated as a medical emergency. Kidney showing marked pallor of the cortex, contrasting to the darker areas of surviving medullary tissue. The patient died with acute renal failure. Causes Acute renal failure is usually categorised (as in the flowchart below) according to pre-renal, renal and post-renal causes. Pre-renal (causes in the blood supply): o hypovolemia (decreased blood volume), usually from shock or dehydration and fluid loss or excessive diuretics use. o hepatorenal syndrome in which renal perfusion is compromised in liver failure o vascular problems, such as atheroembolic disease and renal vein thrombosis (which can occur as a complication of the nephrotic syndrome) o infection usually sepsis, systemic inflammation due to infection Renal (damage to the kidney itself): o toxins or medication (e.g. some NSAIDs, aminoglycoside antibiotics, iodinated contrast, lithium, phosphate nephropathy due to bowel preparation for colonoscopy with sodium phosphates) o rhabdomyolysis (breakdown of muscle tissue) - the resultant release of myoglobin in the blood affects the kidney; it can be caused by injury (especially crush injury and extensive blunt trauma), statins, stimulants and some other drugs o hemolysis (breakdown of red blood cells) - the hemoglobin damages the tubules; it may be caused by various conditions such as sickle-cell disease, and lupus erythematosus o multiple myeloma, either due to hypercalcemia or "cast nephropathy" (multiple myeloma can also cause chronic renal failure by a different mechanism) o acute glomerulonephritis which may be due to a variety of causes, such as anti glomerular basement membrane disease/Goodpasture's syndrome, Wegener's granulomatosis or acute lupus nephritis with systemic lupus erythematosus Post-renal (obstructive causes in the urinary tract) due to: o medication interfering with normal bladder emptying. o benign prostatic hypertrophy or prostate cancer. o kidney stones. o o due to abdominal malignancy (e.g. ovarian cancer, colorectal cancer). obstructed urinary catheter. Diagnosis In general, renal failure is diagnosed when either creatinine or blood urea nitrogen tests are markedly elevated in an ill patient, especially when oliguria is present. Previous measurements of renal function may offer comparison, which is especially important if a patient is known to have chronic renal failure as well. If the cause is not apparent, a large amount of blood tests and examination of a urine specimen is typically performed to elucidate the cause of acute renal failure, medical ultrasonography of the renal tract is essential to rule out obstruction of the urinary tract. Consensus criteria[1][2] for the diagnosis of ARF are: Risk: serum creatinine increased 1.5 times OR urine production of <0.5 ml/kg body weight for 6 hours Injury: creatinine 2.0 times OR urine production <0.5 ml/kg for 12 h Failure: creatinine 3.0 times OR creatinine >355 μmol/l (with a rise of >44) or urine output below 0.3 ml/kg for 24 h Loss: persistent ARF or more than four weeks complete loss of kidney function Kidney biopsy may be performed in the setting of acute renal failure, to provide a definitive diagnosis and sometimes an idea of the prognosis, unless the cause is clear and appropriate screening investigations are reassuringly negative. Treatment Acute renal failure may be reversible if treated promptly and appropriately. Resuscitation to normotension and a normal cardiac output is key. The main interventions are monitoring fluid intake and output as closely as possible; insertion of a urinary catheter is useful for monitoring urine output as well as relieving possible bladder outlet obstruction, such as with an enlarged prostate. In the absence of fluid overload, administering intravenous fluids is typically the first step to improve renal function. Fluid administration may be monitored with the use of a central venous catheter to avoid over- or under-replacement of fluid. If the cause is obstruction of the urinary tract, relief of the obstruction (with a nephrostomy or urinary catheter) may be necessary. Metabolic acidosis and hyperkalemia, the two most serious biochemical manifestations of acute renal failure, may require medical treatment with sodium bicarbonate administration and antihyperkalemic measures, unless dialysis is required. Should hypotension prove a persistent problem in the fluid replete patient, inotropes such as norepinephrine and/or dobutamine may be given to improve cardiac output and hence renal perfusion. While a useful pressor, there is no evidence to suggest that dopamine is of any specific benefit, and at least a suggestion of possible harm. A Swan-Ganz catheter may be used, to measure pulmonary artery occlusion pressure to provide a guide to left atrial pressure (and thus left heart function) as a target for inotropic support. The use of diuretics such as furosemide, while widespread and sometimes convenient in ameliorating fluid overload, does not reduce the risk of complications and death. In practice, diuretics may simply mask things, making it more difficult to judge the adequacy of resuscitation. Lack of improvement with fluid resuscitation, therapy-resistant hyperkalemia, metabolic acidosis, or fluid overload may necessitate artificial support in the form of dialysis or hemofiltration. Depending on the cause, a proportion of patients will never regain full renal function, thus having end stage renal failure requiring lifelong dialysis or a kidney transplant. History Before the advancement of modern medicine, acute renal failure might be referred to as uremic poisoning. Uremia was the term used to describe the contamination of the blood with urine. Starting around 1847 this term was used to describe reduced urine output, now known as oliguria, which was thought to be caused by the urine's mixing with the blood instead of being voided through the urethra. Acute renal failure due to acute tubular necrosis (ATN) was recognised in the 1940s in the United Kingdom, where crush victims during the Battle of Britain developed patchy necrosis of renal tubules, leading to a sudden decrease in renal function. During the Korean and Vietnam wars, the incidence of ARF decreased due to better acute management and intravenous infusion of fluids. See also Chronic kidney disease Dialysis Hepatorenal syndrome Renal failure Acute respiratory distress syndrome Acute respiratory distress syndrome (ARDS), also known as respiratory distress syndrome (RDS) or adult respiratory distress syndrome (in contrast with IRDS) is a serious reaction to various forms of injuries to the lung. ARDS is a severe lung disease caused by a variety of direct and indirect issues. It is characterized by inflammation of the lung parenchyma leading to impaired gas exchange with concomitant systemic release of inflammatory mediators causing inflammation, hypoxemia and frequently resulting in multiple organ failure. This condition is often lethal, usually requiring mechanical ventilation and admission to an intensive care unit. A less severe form is called acute lung injury (ALI). ARDS formerly most commonly signified adult respiratory distress syndrome to differentiate it from infant respiratory distress syndrome in premature infants. However, as this type of pulmonary edema also occurs in children, ARDS has gradually shifted to mean acute rather than adult. The differences with the typical infant syndrome remain. Definition Patient presentation and diagnosis ARDS can occur within 24 to 48 hours of an injury or attack of acute illness. In such a case the patient usually presents with shortness of breath, tachypnea, and symptoms related to the underlying cause, i.e. shock. ARDS is classically associated with hypoxemia, petechiae in the axillae and neurologic abnomalities such as mental confusion.[1] Long term illnesses can also trigger it, eg malaria. The ARDS may then occur sometime after the onset of a particularly acute case of the infection. See xray of malarial ARDS. An arterial blood gas analysis and chest X-ray allow formal diagnosis by inference using the aforementioned criteria. Although severe hypoxemia is generally included, the appropriate threshold defining abnormal PaO2 has never been systematically studied. Any cardiogenic cause of pulmonary edema should be excluded. This can be done by placing a pulmonary artery catheter for measuring the pulmonary artery wedge pressure. However, this is not necessary and is now rarely done as abundant evidence has emerged demonstrating that the use of pulmonary artery catheters does not lead to improved patient outcomes in critical illness including ARDS. Plain Chest X-rays are sufficient to document bilateral alveolar infiltrates in the majority of cases. While CT scanning leads to more accurate images of the pulmonary parenchyma in ARDS, it has little utility in the clinical management of patients with ARDS, and remains largely a research tool. Pathophysiology A pathohistological image of ARDS. ARDS is characterized by a diffuse inflammation of lung parenchyma. The triggering insult to the parenchyma usually results in an initial release of cytokines and other inflammatory mediators, secreted by local epithelial and endothelial cells. Neutrophils and some T-lymphocytes quickly migrate into the inflamed lung parynchema and contribute in the amplification of the phenomenon. Typical histological presentation involves diffuse alveolar damage and hyaline membrane formation in alveolar walls. Although the triggering mechanisms are not completely understood, recent research has examined the role of inflammation and mechanical stress. Inflammation Inflammation alone, as in sepsis, causes endothelial dysfunction, fluid extravasation from the capillaries and impaired drainage of fluid from the lungs. Dysfunction of type II pulmonary epithelial cells may also be present, with a concomitant reduction in surfactant production. Elevated inspired oxygen concentration often becomes necessary at this stage, and they may facilitate a 'respiratory burst' in immune cells. In a secondary phase, endothelial dysfunction causes cells and inflammatory exudate to enter the alveoli. This pulmonary edema increases the thickness of the alveolo-capillary space, increasing the distance the oxygen must diffuse to reach blood. This impairs gas exchange leading to hypoxia, increases the work of breathing, eventually induces fibrosis of the airspace. Moreover, edema and decreased surfactant production by type II pneumocytes may cause whole alveoli to collapse, or to completely flood. This loss of aeration contributes further to the right-to-left shunt in ARDS. As the alveoli contain progressively less gas, more blood flows through them without being oxygenated resulting in massive intrapulmonary shunting. Collapsed alveoli (and small bronchi) do not allow gas exchange. It is not uncommon to see patients with a PaO2 of 60 mmHg (8.0 kPa) despite mechanical ventilation with 100% inspired oxygen. The loss of aeration may follow different patterns according to the nature of the underlying disease, and other factors. In pneumonia-induced ARDS, for example, large, more commonly causes relatively compact areas of alveolar infiltrates. These are usually distributed to the lower lobes, in their posterior segments, and they roughly correspond to the initial infected area. In sepsis or trauma-induced ARDS, infiltrates are usually more patchy and diffuse. The posterior and basal segments are always more affected, but the distribution is even less homogeneous. Loss of aeration also causes important changes in lung mechanical properties. These alterations are fundamental in the process of inflammation amplification and progression to ARDS in mechanically ventilated patients. Mechanical stress Mechanical ventilation is an essential part of the treatment of ARDS. As loss of aeration (and the underlying disease) progress, the work of breathing (WOB) eventually grows to a level incompatible with life. Thus, mechanical ventilation is initiated to relieve respiratory muscles of their work, and to protect the usually obtunded patient's airways. However, mechanical ventilation may constitute a risk factor for the development, or the worsening, of ARDS.[1] Aside from the infectious complications arising from invasive ventilation with tracheal intubation, positive-pressure ventilation directly alters lung mechanics during ARDS. The result is higher mortality, i.e. through baro-trauma, when these techniques are used.[1] In 1998, Amato et al published a paper showing substantial improvement in the outcome of patients ventilated with lower tidal volumes (Vt) (6 mL·kg-1).[1][5] This result was confirmed in a 2000 study sponsored by the NIH.[6] Although both these studies were widely criticized for several reasons, and although the authors were not the first to experiment lower-volume ventilation, they shed new light on the relationship between mechanical ventilation and ARDS. One opinion is that the forces applied to the lung by the ventilator may work as a lever to induce further damage to lung parenchyma. It appears that shear stress at the interface between collapsed and aerated units may result in the breakdown of aerated units, which inflate asymmetrically due to the 'stickiness' of surrounding flooded alveoli. The fewer such interfaces around an alveolus, the lesser the stress. Indeed, even relatively low stress forces may induce signal transduction systems at the cellular level, thus inducing the release of inflammatory mediators. This form of stress is thought to be applied by the transpulmonary pressure (gradient) (Pl) generated by the ventilator or, better, its cyclical variations. The better outcome obtained in patients ventilated with lower Vt may be interpreted as a beneficial effect of the lower Pl. Transpulmonary pressure, is an indirect function of the Vt setting on the ventilator, and only trial patients with plateau pressures (a surrogate for the actual Pl) were less than 32 cmH2O (3.1 kPa) had improved survival. The way Pl is applied on alveolar surface determines the shear stress to which lung units are exposed. ARDS is characterized by an usually inhomogeneous reduction of the airspace, and thus by a tendency towards higher Pl at the same Vt, and towards higher stress on less diseased units. The inhomogeneity of alveoli at different stages of disease is further increased by the gravitational gradient to which they are exposed, and the different perfusion pressures at which blood flows through them. Finally, abdominal pressure exerts an additional pressure on inferoposterior lung segments, favoring compression and collapse of those units. The different mechanical properties of alveoli in ARDS may be interpreted as having varying time constants (the product of alveolar compliance × resistance). A long time constant indicates an alveolus which opens slowly during tidal inflation, as a consequence of contrasting pressure around it, or altered water-air interface inside it (loss of surfactant, flooding). Slow alveoli are said to be 'kept open' using positive end-expiratory pressure, a feature of modern ventilators which maintains a positive airway pressure throughout the whole respiratory cycle. A higher mean pressure cycle-wide slows the collapse of diseased units, but it has to be weighed against the corresponding elevation in Pl/plateau pressure. The prone position also reduces the inhomogeneity in alveolar time constants induced by gravity and edema. Progression If the underlying disease or injurious factor is not removed, the amount of inflammatory mediators released by the lungs in ARDS may result in a systemic inflammatory response syndrome (or sepsis if there is lung infection).[1] The evolution towards shock and/or multiple organ failure follows paths analogous to the pathophysiology of sepsis. This adds up to the impaired oxygenation, the real mainstay of ARDS, and respiratory acidosis, often caused by the ventilation techniques indicated in ARDS. The result is a critical illness in which the 'endothelial disease' of severe sepsis/SIRS is worsened by the pulmonary dysfunction, which further impairs oxygen delivery. Treatment General Acute respiratory distress syndrome is usually treated with mechanical ventilation in the Intensive Care Unit. Ventilation is usually delivered through oro-tracheal intubation, or tracheostomy whenever prolonged ventilation (≥2 weeks) is deemed inevitable. The possibilities of non-invasive ventilation are limited to the very early period of the disease or, better, to prevention in individuals at risk for the development of the disease (atypical pneumonias, pulmonary contusion, major surgery patients). Treatment of the underlying cause is imperative, as it tends to maintain the ARDS picture. Appropriate antibiotic therapy must be administered as soon as microbiological culture results are available. Empirical therapy may be appropriate if local microbiological surveillance is efficient. More than 60% ARDS patients experience a (nosocomial) pulmonary infection either before or after the onset of lung injury. The origin of infection, when surgically treatable, must be operated on. When sepsis is diagnosed, appropriate local protocols should be enacted. Commonly used supportive therapy includes particular techniques of mechanical ventilation and pharmacological agents whose effectiveness with respect to the outcome has not yet been proven. It is now debated whether mechanical ventilation is to be considered mere supportive therapy or actual treatment, since it may substantially affect survival. Mechanical ventilation Further information: Pressure Regulated Volume Control The overall goal is to maintain acceptable gas exchange and to minimize adverse effects in its application. Three parameters are used: PEEP (positive end-expiratory pressure, to maintain maximal recruitment of alveolar units), mean airway pressure (to promote recruitment and predictor of hemodynamic effects) and plateau pressure (best predictor of alveolar overdistention). [7] Conventional therapy aimed at tidal volumes (Vt) of 12-15 ml/kg. Recent studies have shown that high tidal volumes can overstretch alveoli resulting in volutrauma (secondary lung injury). The ARDS Clinical Network, or ARDSNet, completed a landmark trial that showed improved mortality when ventilated with a tidal volume of 6 ml/kg compared to the traditional 12 ml/kg. Low tidal volumes (Vt) may cause hypercapnia and atelectasis.[1] Low tidal volume ventilation was the primary independent variable associated with reduced mortality in the NIH-sponsored ARDSnet trial of tidal volume in ARDS. Plateau pressure less than 30 cm H2O was a secondary goal, and subsequent analyses of the data from the ARDSnet trial (as well as other experimental data) demonstrate that there appears to be NO safe upper limit to plateau pressure; that is, regardless of plateau pressure, patients fare better with low tidal volumes (see Hager et al, American Journal of Respiratory and Critical Care Medicine, 2005). APRV (Airway Pressure Release Ventilation) and ARDS / ALI Although a particular ventilation mode has yet to be "proven in clinical trials"* more effective than others in treating patients with ARDS, ever increasing empirical evidence and clinical experience is showing that APRVis the primary mode of choice when ventilating a patient with ARDS or ALI (Acute Lung Injury). Advantages to APRV ventilation include: decreased airway pressures, decreased minute ventilation, decreased dead-space ventilation, promotion of spontaneous breathing, almost 24 hour a day alveolar recruitment, decreased use of sedation, near elimination of neuromuscular blockade and an often positive effect on cardiac output (due to the negative inflection from the elevated baseline with each spontaneous breath). A patient with ARDS on average spends 8 to 11 days on a mechanical ventilator; APRV may reduce this time significantly.[citation needed] *This would require a side by side study of APRV and the current ARDSNet protocol. There seems to be little political will, within the medical community, to address the need for this study, in spite of the successes seen with APRV. Positive end-expiratory pressure Positive end-expiratory pressure (PEEP) must be used in mechanically-ventilated patients in order to contrast the tendency to collapse of affected alveoli. Ideally, a 'perfect' PEEP would match the increased alveolar surface tension, caused by surfactant deficiency and external pressure (edema), thus restoring a normal time constant in all affected units. However, because of the cited inherent inhomogeneity, surface tension varies, and so do PEEP requirements for the diseased units. Furthermore, high levels of PEEP may impair venous blood return to the right heart, although the actual impact of PEEP on hemodynamics is still debated. The 'best PEEP' used to be defined as 'some' cmH2O above the lower inflection point (LIP) in the sigmoidal pressure-volume relationship curve of the lung. Recent research has shown that the LIP-point pressure is no better than any pressure above it, as recruitment of collapsed alveoli, and more importantly the overdistension of aerated units, occur throughout the whole inflation. Despite the awkwardness of most procedures used to trace the pressure-volume curve, it is still used by some to define the minimum PEEP to be applied to their patients. Some of the newest ventilators have the ability to automatically plot a pressure-volume curve. The possibility of having an 'instantaneous' tracing trigger might produce renewed interest in this analysis. PEEP may also be set empirically. Some authors suggest performing a 'recruiting maneuver' (i.e., a short time at a very high continuous positive airway pressure, such as 50 cmH2O (4.9 kPa), to recruit, or open, collapsed unit with a high distending pressure) and then to increase PEEP to a rather high level before restoring previous ventilation. The final PEEP level should be the one just before the drop in PaO2 (or peripheral blood oxygen saturation) during a step-down trial. PEEP 'stacks up' to Pl during volume-controlled ventilation. At high levels, it may cause significant overdistension of (and injury to) compliant, aerated units, and higher plateau pressures at the same Vt. Intrinsic PEEP (iPEEP), or auto-PEEP, is not detected during normal ventilation. However, when ventilating at high frequencies, its contribution may be substantial, both in its positive and negative effects. There are 'underground', unproven claims that the Amato and NIH/ARDS Network studies got a positive result because of the high iPEEP levels reached by spontaneously breathing patients in low-volume assist-control ventilation. Whether or not that is true, it is a fact that iPEEP has been measured in very few formal studies on ventilation in ARDS patients, and its entity is largely unknown. Its measurement is recommended in the treatment of ARDS patients, especially when using high-frequency (oscillatory/jet) ventilation. A compromise between the beneficial and adverse effects of PEEP is, as usual, inevitable. Prone position Distribution of lung infiltrates in acute respiratory distress syndrome is non-uniform. Repositioning into the prone position (face down) might improve oxygenation by relieving atelectasis and improving perfusion. However, although the hypoxemia is overcome there seems to be no effect on overall survival.[8][1] Fluid management Several studies have shown that pulmonary function and outcome are better in patients that lost weight or wedge pressure was lowered by diuresis or fluid restriction.[1] Corticosteroids A Meduri et al study has found significant improvement in ARDS using modest doses of corticosteroids. This is probably because of a suppression of ongoing inflammation during the fibroproliferative phase of ARDS. The initial regimen consists of methylprednisolone 2 mg/kg daily. After 3-5 days a response must be apparent. In 1-2 weeks the dose can be tapered to methylprednisolone 0.5-1.0 mg daily. Patients with ARDS do not benefit from high-dose corticosteroids.[9][1] The recent NIH-sponsored ARDSnet LAZARUS study of corticosteroids for ARDS demonstrated that they are not efficacious in ARDS. Nitric oxide Inhaled nitric oxide (NO) potentially acts as selective pulmonary vasodilator. Rapid binding to hemoglobin prevents systemic effects. It should increase perfusion of better ventilated areas. There are no large studies demonstrating positive results. Therefore its use must be considered individually. Almitrine bismesylate stimulates chemoreceptors in carotic and aortic bodies. It has been used to potentiate the effect of NO, presumably by potentiating hypoxia-induced pulmonary vasoconstriction. In case of ARDS it is not known whether this combination is useful.[1] Surfactant therapy To date no prospective controlled clinical trial has shown a significant mortality benefit of exogenous surfactant in ARDS. Complications Since ARDS is an extremely serious condition which requires invasive forms of therapy it is not without risk. Complications to be considered are: Pulmonary: barotrauma (volutrauma), pulmonary embolism (PE), pulmonary fibrosis, ventilator-associated pneumonia (VAP). Gastrointestinal: hemorrhage (ulcer), dysmotility, pneumoperitoneum, bacterial translocation. Cardiac: arrhythmias, myocardial dysfunction. Renal: acute renal failure (ARF), positive fluid balance. Mechanical: vascular injury, pneumothorax (by placing pulmonary artery catheter), tracheal injury/stenosis (result of intubation and/or irritation by endotracheal tube. Nutritional: malnutrition (catabolic state), electrolyte deficiency. Stress ulcer Stress ulcers are single or multiple mucosal defects which can become complicated by upper gastrointestinal bleeding during the physiologic stress of serious illness. Ordinary peptic ulcers are found commonly in the gastric antrum and the duodenum whereas stress ulcers are found commonly in fundic mucosa and can be located anywhere within the stomach and proximal duodenum. Risk Factors Risk factors for stress ulcer formation that have been identified are numerous and varied. However, two landmark studies and one position paper exist that addresses the topic of risk factors for stress ulcer formation: Non-critically ill medical patients with 2 or more of the following: respiratory failure, sepsis, heart failure, hepatic encephalopathy, jaundice, renal failure, stroke, hypotension, previous gastrointestinal disease and treatment with corticosteroids, NSAIDS, heparin, or warfarin. In surgical critically ill patients, only those patients who are on a mechanical ventilator for more than 48 hours and/or those with a coagulopathy. The American Society of Health-System Pharmacists guideline recommends against the practice of stress ulcer prophylaxis in non-critically ill patients. Diagnosis Stress ulcer is suspected when there is upper gastrointestinal bleeding in the appropriate clinical setting, for example, when there is upper gastrointestinal bleeding in elderly patients in a surgical intensive care unit (ICU) with heart and lung disease, or when there is upper gastrointestinal bleeding in patients in a medical ICU who require respirators. Stress ulcer can be diagnosed after the initial management of gastrointestinal bleeding, the diagnosis can be confirmed by upper GI endoscopy. The site of ulcerations The ulcerations may be superficial and confined to the mucosa, in which case they are more appropriately called erosions, or they may penetrate deeper into the submucosa. The former may cause diffuse mucosal oozing of blood, whereas the latter may erode into a submucosal vessel and produce frank hemorrhage. Lesion of stress ulcers The characteristic lesions may be multiple, superficial mucosal erosions similar to erosive gastroduodenitis. Occasionally, there may be a large acute ulcer in the duodenum (Curling’s ulcer). Generally, there are multiple lesions located mainly in the stomach and occasionally in the duodenum. They range in depth from mere shedding of the superficial epithelium (erosion) to deeper lesions that involve the entire mucosal thickness (ulceration). Stress Ulcer formation The pathogenic mechanisms are similar to those of erosive gastritis.” The pathogenesis of stress ulcer is unclear but probably is related to a reduction in mucosal blood flow or a breakdown in other normal mucosal defense mechanisms in conjunction with the injurious effects of acid and pepsin on the gastroduodenal mucosa. Stress Ulcer Prophylaxis (SUP) Prevention of this condition is far better than trying to treat it once it occurs. Prophylactic agents include antacids, H2-receptor blockers, sucralfate, proton pump inhibitors (PPIs), prostaglandin analogs, and nutrition. Antacids have been used in SUP. Numerous studies have shown them to be as effective in prevention when compared to H2-receptor blockers. However, one study has shown them to be no more effective than placebo. Thus, they are not widely used. In contrast, H2-receptor blockers are widely used in SUP. Most trials, but not all, have demonstrated their effectiveness in preventing stress ulcer formation. Sucralfate has not been shown to effectively decrease the incidence of stress ulcer formation. This was demonstrated in a large randomized, double-blinded, control trial of 1200 patients and compared sucralfate to the H2-receptor blocker, ranitidine. PPIs are also widely used in SUP. "Data regarding the efficacy and potential adverse effects of these drugs in the prevention of stress ulceration are less extensive than for antacids, H2 blockers, or sucralfate." In one study looking at omeprazole, patients were given an oral suspension by mouth followed by nasogastric tube and there were no episodes of bleeding or signs of toxicity. Similar results were reproduced in another study. Not every patient who enters the hospital needs SUP. Cook et al demonstrated that in surgical critically-ill patients the only risk factors associated with clinically significant bleeding from stress ulcers were mechanical ventilation for more than 48 hours and coagulopathy (OR 15.6 and 4.3, respectively). Management The principles of management are the same as for the chronic ulcer. The steps of management are similar as in erosive gastritis. Treatment Endoscopic means of treating stress ulceration may be ineffective and operation required. It is believed that shunting of blood away from the mucosa makes the mucous membrane ischaemic and more susceptible to injury. Treatment of stress ulceration usually begins with prevention. Careful attention to respiratory status, acid-base balance, and treatment of other illnesses helps prevent the conditions under which stress ulcers occur. Patients who develop stress ulcers typically do not secrete large quantities of gastric acid; however, acid does appear to be involved in the pathogenesis of the lesions. Thus it is reasonable either to neutralize acid or to inhibit its secretion in patients at high risk. In case of severe hemorrhagic or erosive gastritis and stress ulcers, a combination of antacids and H2-blockers may stop active bleeding and prevent re bleeding. In selected patients, either endoscopic therapy or selective infusion of vasopressin into the left gastric artery may help control the hemorrhage. Acute liver failure Acute liver failure is the appearance of severe complications rapidly after the first signs of liver disease (such as jaundice), and indicates that the liver has sustained severe damage (loss of function of 80-90% of liver cells). The complications are hepatic encephalopathy and impaired protein synthesis (as measured by the levels of serum albumin and the prothrombin time in the blood). The 1993 classification defines hyperacute as within 1 week, acute as 8-28 days and subacute as 4-12 weeks. It reflects the fact that the pace of disease evolution strongly influences prognosis. Underlying aetiology is the other significant determinant of outcome. Causes Common causes for acute liver failure are paracetamol (acetaminophen) overdose, idiosyncratic reaction to medication (e.g. tetracycline, troglitazone), excessive alcohol intake (severe alcoholic hepatitis), viral hepatitis (hepatitis A or B - it is extremely uncommon in hepatitis C), acute fatty liver of pregnancy, and idiopathic (without an obvious cause). Reye syndrome is acute liver failure in a child with a viral infection (e.g. chickenpox); it appears that aspirin use may play a significant role. Wilson's disease (hereditary copper accumulation) may infrequently present with acute liver failure. Pathology In the majority of acute liver failure (ALF) there is widespread hepatocellular necrosis beginning in the centrizonal distribution and progressing towards portal tracts. The degree of parenchymal inflammation is variable and is proportional to duration of disease. Clinical consequence Cerebral oedema and encephalopathy In ALF, cerebral oedema leads to hepatic encephalopathy, coma, brain herniation and eventually death. Detection of encephalopathy is central to the diagnosis of ALF. It may vary from subtle deficit in higher brain function (e.g. mood, concentration in grade I) to deep coma (grade IV). Patients presenting as acute and hyperacute liver failure are at greater risk of developing cerebral oedema and grade IV encephalopathy. The pathogenesis remains unclear but is likely to be a consequence of several phenomena. There is a build up of toxic substances like ammonia, mercaptan, endogenous benzodiazepines and serotonin/tryptophan in the brain. This affects neurotransmitter level and neuroreceptor activation. Autoregulation of cerebral blood flow is impaired and is associated with anaerobic glycolysis and oxidative stress. Neuronal cell astrocytes are susceptible to these changes and they swell up, resulting in increased intracranial pressure. Inflammatory mediators also play important role.[5][6][2] Unfortunately, signs of elevated intracranial pressure such as papilloedema and loss of pupillary reflexes are not reliable and occur late in the disease process. CT imaging of the brain is also unhelpful in detecting early cerebral oedema but is often performed to rule out intra-cerebral bleeding. Invasive intracranial pressure monitoring via subdural route is often recommended, however the risk of complications must be weighed against the possible benefit (1% fatal haemorrhage). The aim is to maintain intracranial pressures below 25 mmHg, cerebral perfusion pressures above 50 mm Hg. Coagulopathy Coagulopathy is another cardinal feature of ALF. Liver has central role in synthesis of almost all coagulation factors and some inhibitors of coagulation and fibrinolysis. Hepatocellular necrosis leads to impaired synthesis of many coagulation factors and their inhibitors. the former produces a prolongation in Prothrombin time which is widely used to monitor severity of hepatic injury.There is significant platelet dysfunction (with both quantitative and qualitative platelet defects). Progressive thrombocytopenia with loss of larger and more active platelet is almost universal. Thrombocytopenia with or without DIC increases risk of intracerebral bleeding. Renal failure Renal failure is common, present in more than 50% of ALF patients, either due to original insult such as paracetamol resulting in acute tubular necrosis or from hyperdynamic circulation leading to hepatorenal syndrome or functional renal failure. Because of impaired production of urea, blood urea do not represent degree of renal impairment. Inflammation and infection About 60% of all ALF patients fulfil the criteria for systemic inflammatory syndrome irrespective of presence or absence of infection. This often contributes towards multi organ failure. Impaired host defence mechanism due to impaired opsonisation, chemotaxis and intracellular killing substantially increase risk of sepsis. Bacterial sepsis mostly due to gram positive organisms and fungal sepsis are observed in up to 80% and 30% patients respectively. Metabolic derangements Hyponatraemia is almost universal finding due to water retention and shift in intracellular sodium transport from inhibition of Na/K ATPase[citation needed]. Hypoglycaemia (due to depleted hepatic glycogen store and hyperinsulinaemia), hypokalaemia, hypophosphataemia and Metabolic alkalosis are often present independent of renal function. Lactic acidosis occurs predominantly in paracetamol overdose. Haemodynamic and cardio-respiratory compromise Hyperdynamic circulation with peripheral vasodilatation from low systemic vascular resistance leads to hypotension. There is a compensatory increase in cardiac output. Adrenal insufficiency has been documented in 60% of ALF and is likely to contribute in haemodynamic compromise. There is also abnormal oxygen transport and utilization. Although delivery of oxygen to the tissues is adequate, there is a decrease in tissue oxygen uptake, resulting in tissue hypoxia and lactic acidosis. Pulmonary complications occur in up to 50% patients. Severe lung injury and hypoxemia result in high mortality. Most cases of severe lung injury is due to ARDS with or withoutsepsis. Pulmonary haemorrhage, pleural effusions, atelectasis, and intrapulmonary shunts also contribute to respiratory difficulty. Evaluation All patients with clinical or laboratory evidence of moderate to severe acute hepatitis should have immediate measurement of prothrombin time and careful evaluation of mental status. If the prothrombin time is prolonged by ≈ 4-6 seconds or more (INR ≥1.5) and there is any evidence of altered sensorium, the diagnosis of ALF should be strongly suspected and hospital admission is mandatory. Initial laboratory examination must be extensive in order to evaluate both the aetiology and severity. Initial laboratory analysis Prothrombin time/INR Complete blood count Chemistries o Liver function test: AST, ALT, alkaline phosphatase, GGT, total bilirubin, albumin o Creatinine, urea/blood urea nitrogen, sodium, potassium, chloride, bicarbonate, calcium, magnesium, phosphate o glucose o Amylase and lipase Arterial blood gas, lactate Blood type and screen Paracetamol (Acetaminophen) level, Toxicology screen Viral hepatitis serologies: anti-HAV IgM, HBSAg, anti-HBc IgM, anti-HEV Autoimmune markers: ANA, ASMA, LKMA, Immunoglobulin levels Ceruloplasmin Level ( when Wilson's disease suspected) Pregnancy test (females) Ammonia (arterial if possible) HIV status (has implication for transplantation) History taking should include careful review of possible exposures to viral infection and drugs or other toxins. From history and clinical examination possibility of underlying chronic disease should be ruled out as it may have different management. A liver biopsy done via the transjugular route because of coagulopathy is not usually necessary other than in occasional malignancies. As the evaluation continues, several important decisions have to be made such as whether to admit the patient to an ICU, or whether to transfer the patient to a transplant facility. Consultation with the transplant centre as early as possible is critical due to possibility of rapid progression of ALF. Treatment Treatment involves admission to hospital; often intensive care unit admission or very close observation are required. Supportive treatment is with adequate nutrition, optimalisation of the fluid balance, mechanical ventilation and intracranial pressure monitoring (in severe encephalopathy), and treatment aimed at removing the underlying cause (such as acetylcysteine for paracetamol poisoning). Other supportive measures may include the drainage of ascites. While many people who develop acute liver failure recover with supportive treatment, liver transplantation is often required in people who continue to deteriorate or have adverse prognostic factors. "Liver dialysis" (various measures to replace normal liver function) is evolving as a treatment modality and is gradually being introduced in the care of patients with liver failure. Prognosis Historically mortality has been unacceptably high, being in excess of 80%. In recent years the advent of liver transplantation and multidisciplinary intensive care support have improved survival significantly. At present overall short term survival with transplant is more than 65%. Several prognostic scoring systems have been devised to predict mortality and to identify who will require early liver transplant. These include kings college hospital criteria, MELD score, APACHE II and Clichy criteria. Multiple organ dysfunction syndrome (MODS) 多器官功能障碍综合征 multiple organ failure (MOF) 多器官衰竭 systemic inflammatory response syndrome (SIRS) 全身炎症反应综合征 Acute renal failure (ARF) 急性肾衰竭 acute liver failure(ALF) 急性肝功能衰竭 stress ulcer (胃、十二指肠)应激性溃疡 acute respiratory distress syndrome(ARDS) 急性呼吸窘迫综合征