Description
advertisement

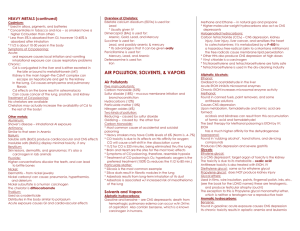
Miscellaneous Poisoning Dr Abdel Moniem G. Madbouly Hydrocarbons Poisoning Definition & Chemistry: A hydrocarbon is an organic compound made up primarily of carbon and hydrogen atoms. This includes products derived from plants (pine oil, vegetable oil), animal fats (cod liver oil), natural gas, petroleum, and coal tar. Today, the principal commercial source of hydrocarbons involves distillation of crude oil. There are three main types of hydrocarbons —aliphatic (straight or branched chains), aromatic (closed ring) and halogenated hydrocarbons. Compound Common uses Aliphatics: Gasoline Kerosene Turpentine Motor vehicle fuel Heating fuel, in lamps Paint thinner Aromatics: Benzene Toluene Solvent, gasoline additive, reagent Solvent Halogenated: Methylene chloride Carbon tetrachloride. Solvent, propellant Solvent, propellant, refrigerant Common Hydrocarbons Kerosene Poisoning Characters, Uses: One of the petroleum distillates hydrocarbons (aliphatic hydrocarbon). A volatile, colorless, irritant liquid with a characteristic odor. Used mainly as a heating fuel or in lamps. Insecticides, and other toxic chemicals may be mixed with it, and these additives can be more dangerous than kerosene itself. Circumstances (at risk groups): 1. Children, especially those younger than 5 years with unintentional exposures— they often ingest kerosene as it is a household product frequently stored at home or garage in unmarked container or soft drink bottles. 2. Workers with occupational exposures often dermal and inhalational, usually in a chronic form. Mechanism of toxicity (Pathophysiology): I- Pulmonary system: The lung is the primary target organ affected by kerosene ingestion. Pulmonary injury results from aspiration of the hydrocarbon and not from gastrointestinal absorption. 1 Miscellaneous Poisoning Dr Abdel Moniem G. Madbouly Aspiration occurs during either initial ingestion or subsequent emesis. The aspiration depends primarily on two physical properties: viscosity and volatility. Kerosene has low viscosity and low volatility. This leads to a high risk of aspiration with increasing rate of penetration into the terminal bronchioles and alveoli. Initial pulmonary damage is due to the chemical destruction of surfactant in the alveoli and distal airways. This renders the alveoli more unstable, leading to early airway closure with subsequent ventilation-perfusion mismatching and hypoxia. Kerosene also increases permeability of the vascular endothelium with subsequent leakage of plasma and blood into the alveoli. A diffuse hemorrhagic alveolitis ending in a chemical pneumonitis with frank necrosis of bronchial, bronchiolar, and alveolar tissues. II- CNS: Occasionally observed, appears to be indirect and secondary to hypoxia of pulmonary complications. If large amount ingested direct CNS depression may occur. III- Cardiac effects: Sudden cardiac death has been associated with kerosene inhalation. Severe dysrhythmia due to sensitization of the heart to circulating catecholamines; this also makes the heart more susceptible to hypoxiainduced dysrhythmia. IV- Gastrointestinal effects: Generally mild and self-limited. Due to direct local irritation (hyperemia with inflammation and superficial ulceration). Clinical picture: I- Pulmonary manifestations: 1. Characteristic smell of kerosene in breath. 2. After ingestion, a transient gasping or cyanosis may occur even in absence of aspiration, owing to volatilized vapors displacing oxygen within the alveoli. 3. Initially, cough is due to local irritation and is very common, but soon subsides. 4. Prolonged cough, gasping, or choking usually indicates aspiration which appears within 30 minutes of exposure. 5. Signs and symptoms of chemical pneumonitis progress over 24 hours, reach a plateau, and subside over 2 to 8 days: Mild toxicity consists of coughing, choking, tachypnea, irritability, and drowsiness. Moderate signs consist of grunting respirations, lethargy, or flaccidity. Signs of severe toxicity are intercostal retractions associated with Ronchi and wheezes, cyanosis, hemoptysis, coma, or seizures. 6. Fever is often present early, due to direct tissue toxicity, and usually disappears by 24 hours. Persistence of fever beyond 2 days should suggest a bacterial superinfection (Bronchopneumonia). 2 Miscellaneous Poisoning Dr Abdel Moniem G. Madbouly II- GIT manifestations: 1. Initial mouth and pharyngeal irritation and burning. 2. Vomiting with smell of kerosene in vomitus, abdominal pain, distension, and diarrhea may develop. 3. Emesis is a significant risk factor for aspiration. Therefore, vomiting, spontaneous or iatrogenic, is a common indication for hospitalization. III- Neurological manifestations: 1. CNS depression (dizziness, stupor, coma and respiratory depression). 2. Seizures. IV- Cardiac manifestations: 1. Tachycardia. 2. Atrial & ventricular dysrhythmia may occur. N.B. if other toxins as pesticides are mixed with kerosene, the clinical picture may be atypical to kerosene. Mechanism of death: 1. Death may occur within 24 hours from central respiratory failure and dysrhythmia. 2. If late in few days, death is secondary to pulmonary complications (bronchopneumonia and pulmonary edema). Diagnosis: 1. Circumstances (at risk groups). 2. Physical examination (C/P & smell). 3. Investigations: Arterial blood gases (ABG). Chest x-ray. ECG monitoring. Lab. investigations for toxic additives. Management: I- Emergency stabilization of patient (ABC): Supplemental oxygen if there is any evidence of respiratory distress. Aerosolized selective β2-adrenergic bronchodilators for bronchospasm (e.g., albuterol). Intubation and ventilatory assistance for respiratory failure. II- Decontamination: 1. Contaminated clothes should be removed and skin should be washed with soap and water, especially in children. 2. Evacuation of the stomach: In mild cases emesis and gastric lavage are contraindicated for fear of aspiration. In severe cases (large ingestion of > 1 ml/kg) or if dangerous additives (e.g., pesticides, metals, camphor, halogenated or aromatic hydrocarbons): 1. Gastric lavage is done after introduction of cuffed endotracheal tube to prevent aspiration. 3 Miscellaneous Poisoning Dr Abdel Moniem G. Madbouly 2. If syrup of ipecac is chosen, the patient must be awake, alert, and able to protect airway. 4. Activated charcoal is not effective and may cause aspiration. III- Drug therapy: 1. Corticosteroids may be used cautiously to treat chemical pneumonitis, as they may affect the immunity of the patient predisposing to infection. 2. Antibiotics may be used if bacterial pneumonia develops. IV- Prevention: 1- Educate the parents to keep toxic substances out of reach of children. 2- Familiar bottles or containers should not be used for storage of such products. 3- Safety closure for the products containing toxic materials. Strychnine Poisoning Source: Strychnine alkaloid can be found naturally in Strychnos nux vomica seeds. It is an odorless crystalline powder with a bitter taste. Uses: 1. Strychnine was first introduced as a rodenticide in 1540. 2. In the past, it was used medically as a cardiac, respiratory stimulant and as an analeptic (antidote to barbiturate). 3. Currently, strychnine is used mainly as a pesticide (rodenticide) and as a research tool for the study of glycine receptors. Circumstances: Deliberate exposure with suicidal and homicidal intent. Unintentional poisoning as with Chinese herbal medicine (Maqianzi) and medicines (tonics and cathartics). Adulteration of street drugs, the bitter taste of strychnine allows it to be substituted for heroin, and cocaine. Mechanism of action (Pathophysiology): Glycine is an inhibitory neurotransmitter in the CNS. Strychnine competitively inhibits the binding of glycine to the glycinergic chloride channel. Although strychnine affects all parts of the CNS in which glycine receptors are found, the most significant effect is in the spinal cord. With the loss of the glycine inhibition to the motor neurons in the ventral horn, there is a loss of inhibitory influence on the normally suppressed reflex arc. The result is increased impulse transmission to the muscles producing generalized muscular contractions. Clinical presentation: = Convulsion fits …….. Symptoms begin rapidly, within about 15-60 minutes of ingestion. The typical symptoms are involuntary, generalized muscular contractions resulting in neck, back, and limb pain, hyperreflexia and nystagmus. 4 Miscellaneous Poisoning Dr Abdel Moniem G. Madbouly The contractions are easily triggered by trivial stimuli (such as turning on a light) and each episode usually lasts for 30 seconds to 2 minutes. Differences in the strength of various muscle groups result in the classic signs of opisthotonus, facial trismus, and risus sardonicus (bitter smile), with flexion of the upper limbs, and extensions of lower limbs. The patient typically remains fully alert "conscious seizure" or "spinal seizure" until metabolic complications & death occur. Hyperthermia, presumably from increased muscular activity, is typical, and temperature as high as 43°C is reported. Mechanism of death: 1. Respiratory failure due to exhaustion of respiratory muscles. 2. Metabolic complications (metabolic acidosis, hyperthermia). 3. Rhabdomyolysis with renal & multiorgan failure. Differential Diagnosis: From similar muscular hyperactivity conditions: 1. Tetanus (less rapid onset and lasting much longer, a history of recent wound, a deficient record of tetanus immunization). 2. Generalized seizures due to other causes (unconsciousness or altered mental status) Management: I- Emergency stabilization of patient (ABC). II- Supportive treatment: (stop convulsion fits) At all times, unnecessary stimuli and manipulation of the patient should be avoided, as these activities trigger muscle contractions. Benzodiazepines remain the first-line treatment. If failed, barbiturates (phenobarbital, pentobarbital) are also effective. If these measures fail, a nondepolarizing neuromuscular blocking (NMB) agent should be administered but, not succinylcholine as it induces muscle contractions. If all above measures failed, general anesthesia is warranted. III- Decontamination: (only after effective control of fits) Induced vomiting is absolutely contraindicated because of the risk of aspiration. Gastric lavage should be considered on an individual basis after evaluating potential benefits and risks, with a cuffed endotracheal tube. Activated charcoal binds strychnine effectively. IV- Treatment of complications: Metabolic acidosis: stop the muscular hyperactivity as soon as possible. Hyperthermia: active cooling with ice water immersion, cooling blanket or fan. Rhabdomyolysis-induced acute renal failure: adequate fluid administration, urinary alkalinization, and temporary renal replacement therapy, if acute renal failure occurs. V- Elimination: Because strychnine has a large VD (13 L/kg), extracorporeal drug elimination procedures are unlikely to be useful. 5 Miscellaneous Poisoning Dr Abdel Moniem G. Madbouly Aconitine poisoning Source: A steroidal alkaloid found in Aconitum nepellas (monkshood) plant. The roots and flowers contain the highest concentration. Ingestion and dermal absorption can cause toxicity. Even picking the flowers of this plant has been reported to cause paresthesias of the fingers. Mechanism of action (Pathophysiology): Aconitine increases sodium permeability, enhancing myocardial contractility and automaticity and leading to digitalis-like dysrhythmia. CNS effects: stimulation followed by depression. Peripheral nerves: stimulation (paresthesia with tingling & numbness) followed by depression (anesthesia). Clinical presentation: Rapidly absorbed from the GI tract, symptoms may begin as soon as a few minutes to several hours after ingestion. Cardiac toxicity resembles that caused by cardioactive steroids, resulting in bradycardia and hypotension to tachydysrhythmias (ventricular fibrillation) and cardiac arrest. Nervous symptoms typically progress from paresthesias to CNS depression, respiratory depression and seizures. GIT: Nausea, vomiting, diarrhea, and abdominal pain. Death is usually due to cardiovascular collapse and ventricular dysrhythmia. DD: A history of paresthesias may be useful in differentiating aconitine toxicity from that caused by digitalis, but empiric use of digoxin-specific antibody fragments should not be delayed if there is any doubt. Management: Treatment is largely supportive: o Emergency stabilization of ABC. o Atropine for bradycardia. o Avoid sodium bicarbonate (it poses a theoretical risk in the setting of aconitine poisoning in which the mechanism is excessive influx at the sodium channel rather than sodium channel blockade). o Cardiac pacing. Orogastric lavage or activated charcoal. 6