Thyroid
advertisement
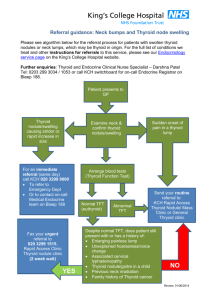
THYROID Anatomy - - - - 2 lobes joined by an isthmus, with occasionally an embryological extension of the isthmus superiorly called the pyramidal lobe. Arterial supply is from 2 arteries: o Superior thyroid A from the external carotid o Inferior thyroid A from the subclavian Drained by 3 veins: o Superior and middle thyroid veins to the internal jugular vein o Inferior thyroid vein to the innominate Why does thyroid move on swallowing? Because it is invested in the pretracheal fascia which is attached to the larynx. Where does the thyroid originate from? It originates from the foramen caecum which is located at the base of the tongue. From the there it descends into the neck, anterior to the hyoid bone, to lie in front of the trachea. The tract left behind is the thyroglossal tract. It usually closes, however a portion of its epithelial lining may persist and form a cyst – a thyroglossal cyst. This happens usually in late adolescence. The connection of the cyst to the tongue means that the cyst will move on protrusion of the tongue. If the cyst becomes infected, occasionally it can lead to a cutaneous fistula – called a thyroglossal fistula. Thyroid is intimately related to… o The recurrent laryngeal nerve – supplies the muscles of the larynx and vocal cords o The external branch of the superior laryngeal nerve – supplies the cricothyroid muscle (a tensor of the vocal cords) o The 4 parathyroid glands DDx for midline swelling in the neck: 1. Thyroid – most common by far! – moves on swallowing 2. Thyroglossal cyst – moves on swallowing and on protrusion of tongue 3. Dermoid cyst – doesn’t move on either swallowing or tongue protrusion. Thyroid mostly consists of follicular cells (controlled by TSH from anterior pituitary, take up iodine, and make thyroid hormone), but also some parafollicular cells (make calcitonin). T3 is the more active form of thyroid hormone. In the blood, most of the T4 is bound to albumin but a small proportion is free – free T4 – which is the functional constituent. In the tissues, T4 is converted to T3 which is the physiologically active hormone. Hypothyroidism is usually due to Hashimoto’s. Examination will usually reveal a small firm rubbery goiter. If a nodule if present – need to investigate to rule out malignancy. Thyroid lymphoma usually develops on a background of autoimmune hypothyroidism. Extreme hypothyroidism can present as myxoedema madness (confusion leading to coma). Investigations: TSH elevated with decreased T4/T3. Antibodies – antithyroglobulin, TPO (Ab against thyroid peroxidase enxyme). Hyperthyroidism can be caused by: - Graves disease - Toxic multinodular goiter - Solitary toxic adenoma. Grave’s disease is autoimmune thyrotoxicosis. It is caused by an antibody against the TSH receptor. Examination may reveal a moderate firm goiter, which in severe thyrotoxicosis may have a bruit and a thrill. Some patients may develop thyroid eye disease (only seen in Grave’s disease!) – lid lag, lower eyelid retraction, periorbital oedema, chemosis, exophthalmos, proptosis. Drugs to use: - Carbimazole (bad SEs – neutropenia, profuse diarrhea, hepatic failure) - Propylthyouracil - Beta-blocker, if particularly symptomatic with tremor, sweating, tachycardia If medical therapy fails – radioactive iodine. If this fails or is contraindicated – surgery. Risk of long-term hypothyroidism – will require lifelong thyroxine. Investigations – suppressed TSH with raised T4/T3. 90% will have raised TRAb (TSH receptor Ab). 70% will have TPO (Ab against thyroid peroxidase enxyme). Multinodular goiter. Most multinodualr goiters are non-toxic, however some can develop toxic multinodular goiter and be hyperthyroid – this is called Plummer’s disease. The large goiter may extend retrosternally and cause tracheal deviation and compression, occasionally leading to stridor (a low-pitched crowing noise heard on inspiration caused by narrowing of the trachea). Examination will reveal multiple nodules, either B/L or U/L. If there is a dominant nodule, it should be investigated as the risk of malignancy in this is 10%. Pemberton’s sign may be positive with retrosternal goiter – get venous congestion and stridor on elevation of the arms. Investigations: TSH will be reduced if toxic goiter. Do FNA for dominant nodule. U/S may confirm multiple nodules. Can also do Xray of thoracic inlet and CT. Treatment: - non-toxic multinodular goiter should be treated with total thyroidectomy is there is retrosternal extension, tracheal compression, or for cosmetic reasons. - Toxic multinodualr goiter should be treated with carbimazole initially and then with total thyroidectomy or radioactive iodine. Solitary toxic adenoma. Occasionally, a single thyroid adenoma may be active enough to render the patient hyperthyroid. Should investigate to r/o malignancy. TSH will be suppressed. A thyroid isotope scan will show a solitary “hot” nodule. Treatment is initially with carbimazole, followed by either thyroid lobectomy or radioactive iodine. Solitary thyroid nodule (STN) This is a common condition. Affects 5% of the female population and 5% are malignant. STN , must be investigated to differentiate between benign/malignant, as most benign ones do not require surgery. Causes of a solitary thyroid nodule: - thyroid cyst - degenerative thyroid nodule - benign follicular adenoma (including solitary toxic adenoma) - differentiated thyroid adenoma What features would suggest malignancy?... Hx of neck irradiation, hoarseness, FHx of thyroid ca. Ask about any hyperthyroid symptoms and any obstructive symptoms (stridor, dysphagia). Investigations: The important ones are TSH and FNA. Want to exclude solitary toxic adenoma (TSH would be suppressed) and malignancy (FNA would be abnormal). FNA is most useful investigation. Send aspirate to cytology, result will come back as either benign (repeat FNA in 6-12mths), suspicious (remove nodule because 30% are malignant), malignant (surgery) or inadequate specimen (repeat FNA). Other investigations may include thyroid US (solid or cystic? Is this a dominant nodule in a MNG? Also useful to guide FNA) and thyroid isotope scan (hot or cold nodule?). Slightly higher risk of malignancy in a cold nodule (10% v 5% for hot). Treatment. Benign – doesn’t require treatment unless symptomatic/cosmetically unacceptable. Repeat FNA in a year. Suspicious – lobectomy as 30% are malignant. Malignant – surgery. Thyroid malignancy Can be differentiated (papillary and follicular) or undifferenetiated (anaplastic). Can also be a medullary thyroid ca or a thyroid lymphoma. Papillary thyroid ca. Most common (70%). F>M. Present in young people (20s-40s). Metastasises to local LNs. Majority (80%) are multifocal throughout the thyroid gland. Orphan annie nuclei and psammoma bodies on histology. Excellent prognosis. Treatment – lobectomy or total thyroidectomy, +/- post op high dose radioiodine and TSH suppression therapy with thyroxine. Follicular thyroid ca. About 10% of thyroid cancers. Present in older age group (40s50s). Is slow growing and eventually spreads by haematogenous route. Prognosis depends on degree of capsular and vascular invasion, but generally good prognosis. Treatment is lobectomy or total thyroidectomy, +/- post op high dose radioiodine and TSH suppression with thyroxine For both the differentiated thyroid cancers, thyroglobulin is a useful marker to monitor patients post total thyroidectomy. Anaplastic thyroid ca. Usually in elderly females.Patients present with a rapidly enlarging thyroid mass, and symptoms of stridor/dysphagia occur early. Tumours are generally fixed and irresectable at presentation. Very poor prognosis. Radio/chemo therapy are palliative, surgery just to relieve obstructive symptoms. Medullary thyroid ca. Rare tumour of the calcitonin-secreting cells of the thyroid. Most sporadic but can be associated with MEN (MEN2). Amyloid on histology. Best treated with total thyroidectomy with central lymph node clearance. Post op, give thyroxine replacement (not suppression), and calcitonin is a useful post op marker for follow-up. Thyroid lymphoma. Rare tumour, usually presents in an elderly female with a history of Hashimoto’s thyroiditis as a rapidly growing thyroid nodule. May have obstructive symptoms and B symptoms. May be diagnosed by FNA or Trucut biopsy. Usually NHL. Stage as for all lymphomas – ie with a bone marrow aspirate and CT of thorax/abdo. If confined to thyroid – can treat with thyroid lobectomy + adjuvant radio/chemo therapy. Otherwise treat with chemoradiation alone. Complications of thyroid surgery: 1. Damage to recurrent laryngeal nerver (in 2% of thyroidectomies) hoarseness 2. Damage to external branch of superior laryngeal nerve hoarseness 3. Damage to parathyroids (in 5% of thyroidectomies) hypocalcaemia 4. Haemorrhage, potentially causing laryngeal oedema and respiratory compromise. PARATHYROIDS Embryology – develop from the 3rd and 4th pharyngeal pouches. Secrete PTH which increases serum calcium by inducing bone resorption etc. Hyperparathyroidism - Primary hyperparathyroidism – bones, stones, abdominal groans, psychic moans. However today, most are discovered incidentally. Most common cause by far is parathyroid adenoma, with four-gland hyperplasia far less frequent. Associated with MEN. Treat symptomatic patients (eg with osteoporosis) and asymptomatic young fit patient (because increased risk of cardiovascular and cerebral disease). Usually remove 3 and a half glands, leaving half. Might be transplanted to forearm for easy access. - Secondary/tertiary hyperparathyroidism is due to chronic renal failure. The inability to excrete phosphate in the urine, and the inability to absorb calcium from the gut (because decreased active Vit D) leads to a relative hypocalcaemia, which stimulates the parathyroid glands to make PTH. Most of these patients can be treated medically with oral calcium supplements, oral phosphate binders (to reduce phosphate absorption), and vitamin D. Hypoparathyroidism – usually occurs as a result of thyroidectomy, and leads to hypocalcaemia. Symptoms of hypocalcaemia may include perioral paraesthesia, digital paraesthesia, tetany, and even seizures. 2 clinical signs are characteristic – Chovstek’s sign (tap facial nerve in front of ear with mouth partially open – muscles twitch), and Trousseau’s sign – inflate BP cuff on arm to above systolic pressure causes carpopedal spasm (weird hand). Treat acute hypocalcaemia with 10ml of 10% calcium gluconate infused slowly over 10mins, with ECG monitoring. Then oral calcium supplements and vitamin D.