Theriogenology Exam 3 2/28/12 Viral causes of abortion: Equine
advertisement
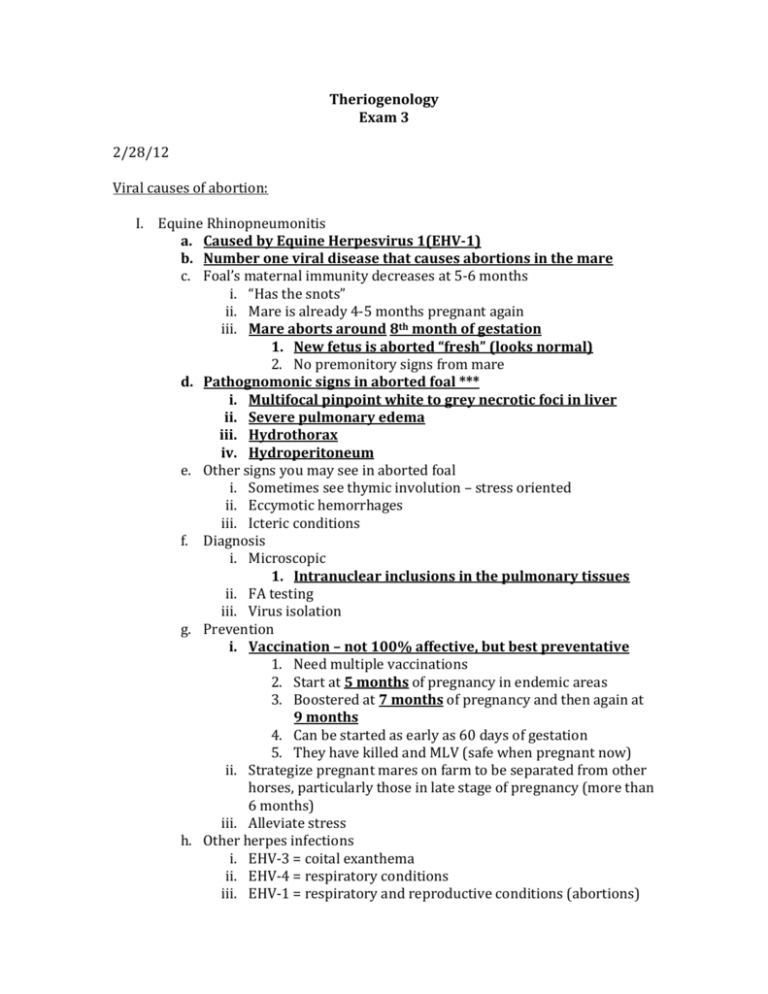
Theriogenology Exam 3 2/28/12 Viral causes of abortion: I. Equine Rhinopneumonitis a. Caused by Equine Herpesvirus 1(EHV-1) b. Number one viral disease that causes abortions in the mare c. Foal’s maternal immunity decreases at 5-6 months i. “Has the snots” ii. Mare is already 4-5 months pregnant again iii. Mare aborts around 8th month of gestation 1. New fetus is aborted “fresh” (looks normal) 2. No premonitory signs from mare d. Pathognomonic signs in aborted foal *** i. Multifocal pinpoint white to grey necrotic foci in liver ii. Severe pulmonary edema iii. Hydrothorax iv. Hydroperitoneum e. Other signs you may see in aborted foal i. Sometimes see thymic involution – stress oriented ii. Eccymotic hemorrhages iii. Icteric conditions f. Diagnosis i. Microscopic 1. Intranuclear inclusions in the pulmonary tissues ii. FA testing iii. Virus isolation g. Prevention i. Vaccination – not 100% affective, but best preventative 1. Need multiple vaccinations 2. Start at 5 months of pregnancy in endemic areas 3. Boostered at 7 months of pregnancy and then again at 9 months 4. Can be started as early as 60 days of gestation 5. They have killed and MLV (safe when pregnant now) ii. Strategize pregnant mares on farm to be separated from other horses, particularly those in late stage of pregnancy (more than 6 months) iii. Alleviate stress h. Other herpes infections i. EHV-3 = coital exanthema ii. EHV-4 = respiratory conditions iii. EHV-1 = respiratory and reproductive conditions (abortions) II. Equine Viral Arteritis a. READ ARTICLE! b. RNA virus c. Togaviridae d. Seen in all equids e. In the past it has been a relatively quiet virus and they didn’t see a lot of activity f. Recently they had outbreak in Mexico in 2006 g. Transmitted i. Respiratory system 1. Racetracks and sale barns ii. Venereal spread - MC h. Clinical signs i. Ocular and nasal discharge ii. Supraorbital edema, ventral edema, hindlimb edema iii. Stallions get edema in scrotum and prepuce iv. Photophobia i. Similar diseases based on clinical signs (rule outs) i. Equine influenza ii. Rhinopneumonitis iii. Purpera hemorrhagica j. Pathogenesis i. Pathogen enters respiratory and goes to lungs and replicates in macrophages ii. Affinity for arterioles so it produces a lot of edema 1. Metritis and edema in uterus of mare 2. Placental detachment 3. Rise in PGF2a 4. Aborted fetus can be fresh or autolytic iii. Vascular damage of lymph nodes k. Lesions i. Histologic 1. Vessels in placenta and fetus have panvasculitis l. Diagnosis i. ELISA ii. Serum neutrilization iii. Immunofluorescence iv. Viral isolation of blood’s buffy coat 1. Do not use hepranized samples because it will affect virus m. Control measures i. Management and isolation ii. Vaccination called Rabac 1. Stallions, non-pregnant mares, geldings, fillies, and foals 2. Once a year, 1 month before breeding season starts 3. Booster every year n. o. p. 3/26/12 q. iii. Test all stallions to make sure they are not carrying antibodies 1. 1:4 or higher is positive Stallions i. Carriers that harbor organism for 6 month-1 year + ii. Hides in ampulla and bulbourethral glands iii. Test them before vaccinating for the first time Mares bred to carrier stallions i. Virus survives freezing and cool shipped semen ii. Make sure mare is serologically negative and vaccinated 1. Isolated for 3 weeks iii. Do not vaccinate pregnant mares in last 2 months of pregnancy iv. Positive mares CAN be bred to positive stallions 1. She can have healthy baby because mare has immunity v. Negative mares will abort and have problems because she hasn’t been exposed to virus before and has no immunity Young horses i. Do not vaccinate horses <6 weeks of age 1. Vaccinated earlier If you have an epidemic REPORTABLE!! Venereal diseases of bovine I. Two important diseases you can diagnose sitting in your truck: a. Trichomonas i. Tritrichomonas fetus ii. Undulating membrane, 3 flagella on front of it and 1 on back iii. Protozoan 1. One cell organism iv. Seen under darkfield microscopy v. Abort in first half of gestation b. Vibriosis/Campylobacter i. Campylobacter fetus venerealis ii. Gram negative microaerophilic (needs some CO2 to grow) rod iii. Abort in 4-7 month of gestation c. History and clinical signs for both: i. MC - Cows returning to estrus ii. Post-coital/post-breeding pyometra iii. Some infertility or varying ages of gestation in pregnancy checks 1. Infertility associated with endometritis iv. Varying age of calves v. Fluid in both uterine horns without a membrane slip vi. Cows can get convalescent immunity d. e. f. g. h. 1. Breed a few times and eventually she catches and pregnancy lasts (she is exposed each time she is bred and is beuilding immunity each time) 2. Makes enough immunoglobulin to the organism and pregnancy will last a. Can produce IgA and IgM 3. Next year when she is bred to a different bull she will start the sequence over again vii. Mucopurulent vulvar discharge in cows 1. Couple weeks after bred to infected bull viii. Cows get vaginits, cervicitis, endometritis, and placentitis ix. No clinical signs in bulls 1. Bulls < 4 years old serve as transient carriers/chronic carriers a. Both organisms inhabit epithelial crypts of penis and prepuce and these bulls (<4) have deeper epithelial crypts and organisms get down in there and hang out forever Both organisms transmitted venereally, can be spread during artificial insemination Both can survive freezing (frozen semen) Both produce economic losses Differentials for both: Brucellosis, Infectious Pustular vulvovaginitis (IPV), Mycoplasma, Ureoplasma, BVD i. All can spread venereally in cow herd but Vibrio and Trich should be at top of list Diagnostics for both: i. No gross fetal lesions in fetuses that are aborted ii. Primary infections are cleared by about 90 days, if they come back and are bred by infected bull again they may calve or the degree of infection will be shorter iii. Isolation and identification of organisms: 1. Vaginal and cervical mucus samples from cow 2. Test bulls during BSE in endemic areas (prepuce sample) a. Test after a few weeks of sexual rest 3. Look at samples under darkfield microscopy, or use culture media a. Vibriosis- Clark’s media (transport media), pyroglycolate with antibiotics, brain heart infusion agar (culture media) i. Needs CO2 to grow (microaerophilic) ii. Could take 5-7 days to grow b. Trichomonas – Diamond’s media (culture media), Kupferberg’s media (transport or culture media), LRS with 5% fetal calf serum (transport media), In Pouch TF (transport media) i. Incubate at 35 C – 37 C c. Look under darkfield as early as 24 hours for undulating membrane and flagella (trich) i. Prevalence of both: i. Fl Al, out west j. Prevention and control for both: i. Management 1. Don’t bring in untested sexually active bulls 2. Avoid renting and leasing bulls from unscrupulous sources 3. Replace bulls with virgin bulls 4. Female replacements should be virgin heifers or cows already in late stages of gestation 5. Immunization a. Vaccinate cows 1 month – 6 weeks prior to breeding season II. Leptospirosis a. Spirochete b. Different serovars i. Cattle get L. hardjo c. Two types in cattle: i. Host adapted: 1. Pathogenicity is usually low 2. Infections manifest as chronic conditions 3. Stillbirths and infertility 4. May see subclinical cases or severe cases 5. L. hardjo is the host adapted species of lepto a. 2 genotypes: i. L. hardjo bovis ii. L. hardjo projetino ii. Non-host adapted: 1. Acute infections 2. Infertility and abortions 3. Organism found in other animals 4. Characterized by exposure to other animals (feral hogs) a. Feral hogs transmit L. pomona that can infect cattle d. Penetrates mucous membranes, of eye, intestinal mucosa, genital tract, and nasal cavity e. Survives for long periods of time outside of mammalian host, particularly in warm moist conditions with neutral to basic pH f. Localizes in proximal renal tubules in kidney so large amounts of organism are excreted into the urine g. Organism has been found in the bull h. i. j. k. l. m. n. o. i. L. hardjo found in testes and accessory sex glands Abortions are primarily associated with L. hardjo and L. pomona i. From 12 weeks after exposure or longer ii. Non-host adapted abortions in last trimester (L. pomona) iii. Host adapted abortions: any stage of gestation (L. hardjo) Transmission i. Direct contact of infected urine (organism survives in kidneys of host) ii. Post-abortion discharges of cows iii. Infected fetus iv. Sexual contact Incubation period i. 4-10 days Clinical signs i. Hepato-renal disease ii. Abortions 1. In host adapted species iii. Photosensitization iv. Hemolytic anemia Pathology i. Interstitial nephritis ii. Autolytic changes in fetus Diagnosis i. Take acute and convalescent serum samples of cow 1. Take one sample today and one in 3 weeks and compare the two titers 2. These method is of no diagnostic significance with this disease, titers will not change 3. Titer usually spikes before abortion occurs and then comes back down ii. Hard to culture these organism 1. Culture from: kidney, urine, thoracic fluid, aqueous humor of aborted fetus 2. Organisms don’t survive vary long in urine iii. Immunofluorescence of kidney of aborted fetus iv. Most common serologic test is microagglutination test v. Vaccination titers usually decline 1. < 1-100 vi. Best bet is to isolate organism from aborted fetus Treatment and control i. Prevent exposure to active non-host adapted animals ii. Immunization 1. Don’t prevent infection in all individuals 2. Want to develop a degree of herd immunity iii. Keep wild hogs away ZOONOTIC i. Produces chronic flu-like symptoms, meningitis, and hepatorenal disease ii. Can kill you III. Listeria a. Listeria moncytogenes b. Ruminants: i. Encephalitis ii. Abortion iii. Neonatal septicemia c. Predilection for fetal placental unit d. Produces abortions in last trimester e. Produces either sporatic or epizootic abortions i. Abortion every now and then (sporatic) ii. Every animal on farm aborting (epizootic) f. Associated with Winter g. Associated with silage feeding (improperly cured) h. Gram negative coccobacillus i. Transmission: i. Aborted fetuses ii. Placenta iii. Uterine discharges iv. Food and water sources contaminated v. Improperly cured silage (pH > 5.4) j. Pathogenesis i. Cow eats and consumes organism ii. Has affinity for Peyer’s Patches of small intestines iii. Spreads hematogenously to conceptus in placenta iv. Results in placentitis and fetal septicemia k. Pathology i. Cows maintain fetus in uterus for several days so fetus autolyzes ii. Fetus is autolyzed, may be able to see small pinpoint foci of gray-white hepatic necrosis iii. Last trimester abortion disease iv. Retained fetal membranes in cows v. Cows sick, fever, depression, weight loss, vi. Habitual abortion in some cows 1. Occurs each year in same animal l. ZOONOTIC i. Abortions in females m. Culture i. Parenchymous organs ii. Gram stain fetal tissue or fluids iii. Impression smears n. Prevention and control i. Make sure silage is not old or contaminated ii. Separate cows that are aborting and the fetuses from the rest of the herd iii. Feed therapeutic doses of tetracycline to feed or water 1. Cant do in dairy cattle because of milk residues IV. Infectious Bovine Rhinotracheitis (IBR) a. Herpesvirus – 1 i. Carrier animals b. Clinical signs i. Respiratory infections ii. Keratoconjunctivitis iii. Rhinotracheitis iv. Significant fetal pathogen c. Also produces Infectious Pustular Vulvovaginitis (IPV) i. Pustules in vulva ii. Causes abdominal posthitis in bulls 1. Inflammation of penis and prepuce iii. Enteritis and systemic disease that is fatal in calves d. Infertility associated with this virus in the cow i. Produces inflammation and necrosis in ovary, inflammation of uterus 1. Destruction of corpus luteum in pregnancy ii. Not a long lasting infertility e. Transmission i. Direct contact with upper respiratory or genital tract secretions ii. Venereal transmission in the bull iii. People can spread during AI from cow to cow f. Abortions i. Virgin or naïve herds may have significant abortion levels, endemic, 40-60% may abort (epizootic) ii. Usually occur in second half of gestation iii. Bovine abortion is autolytic with herpes, equine abortion is fresh with herpes iv. Rarely see abortions following conjunctivitis or IPV g. Diagnosis i. No significant rise in titers once you notice disease, so they are not helpful, titers will peak before abortions occur h. Prevention and control i. Vaccinations 1. MLV a. Do not use in pregnant cows – will induce abortions 2. Killed a. Use 2 injections 3-5 weeks apart V. Bovine Viral Diarrhea (BVD) a. RNA virus b. c. d. e. f. g. i. Mutate readily Clinical signs i. Abortions ii. Viral diarrhea 1. Turns into mucosal disease Acute BVD i. Affects cattle between 6 months – 2 years ii. Morbidity is high iii. Clinical signs 1. Lethargy, fever, anorexia, depression, FAD, diarrhea, ulcerative lesions in oral cavity and intestine, decreased milk production, oral erosions, blunting of oral papilla, iv. Viremia lasts 2 weeks 1. Sheds to more susceptible animals v. Most animals recover and may sero-convert and develop high titers to the virus There are two antigenically different types of this virus: i. Name from response to cell culture in the lab: 1. Non-cytopathogenic type: a. No damage to the cell culture b. Responsible for producing calves that are persistently infected (PIs) 2. Cytopathogenic type a. Produces changes in cell culture b. Acute mucosal disease form Persistently infected calves (PIs) i. Cow pregnant and exposed to non-cytopathogenic virus, virus went into fetus, fetus produced no immune response and the calf is born persistently infected 1. Pull blood sample on calf: he will have no titer and looks normal because he did not have immune response ii. Calves look normal at first, may become sick at 3-4 months of age or stay normal iii. Immunotolerant – virus does not affect calf iv. Diagnosing a PI: 1. Immunohistochemistry a. Take a piece of tissue (ear notching), drop it in formalin and send to lab for this test, they will do histological staining and diagnose it v. Cull PI from herd when it is identified Acute mucosal disease form i. Animal has diarrhea, lesions around feet (coronitis) ii. Already a PI calf and then he gets infected with cytopathogenic form BVD (both types) produces congenital anomalies: i. Cerebellar hypoplasia ii. Hydrocephalus iii. Cataracts iv. Retinal problems v. Microphthalmia (small eyes) vi. Hypotrichosis h. Infections that take place at different stages of gestation: i. Cow infected prior to 125 days: (early gestation) 1. Get PI calves a. Survive to term, look normal ii. Cow infected between 125-175 days: (mid-gestation) 1. Abortions 2. If infected with cytopathogenic type: calves will have congenital defects 3. Will get an immune response a. Pull blood samples from calf to test for antibodies 4. Cull animals with high BVD titers iii. Cow infected after 175 days: (late gestation) 1. Does not cause significant fetal disease 2. Calves have pre-colostral antibodies to BVD indicating exposure i. Diagnostics i. PCR, ELISA, fluorescent antibody testing, immunohistochemistry VI. Ureoplasm and Microplasma a. Ureoplasma diversum b. Microplasma bovogenitalium c. These organisms do not have cell wall and they are hard to culture d. Not seen a lot in the South but is significant in the North and diary country e. Clinical signs i. Granular vulvitis MC 1. Ureoplasm causes this more commonly mycoplasma can also 2. Mucopurulent discharge ii. May show no signs iii. Infertility – seen with inflammation of oviduct (salpingitis), endometritis, or cervicitis iv. Early abortions f. Both organisms found in vulva or vaginal tract, distal urethra, prepuce, semen samples g. Transmission i. Natural breeding or by artificial insemination h. Diagnosis i. Aborted fetus, cotyledons, and caruncles can be frozen immediately and sent to lab the day that you collect it ii. Special media: diacron or polyester tipped swabs must be used for vulvar secretions, transport medias are (Hayflicks for Ureaplasm) (SP4 for Mycoplasma) VII. Epizootic bovine abortion a. AKA Foothill Abortion b. Classic presentation: i. Confined to northern California foothills and far western states, mountains of Nevada and Oregon ii. History: 1. Only heifers or adult cows brought into the endemic area are affected and they abort 1 time 2. Cows are bitten by tick and shows signs of this disease iii. Thought to be transmitted by ticks iv. Abort late in gestation 1. Abort fresh calves v. Some calves born alive and unthrifty and die shortly after birth 1. One of the few conditions where you produce calves with extremely high immunoglobulin levels to organism a. IgG and IgM levels of calves who have had colostrum i. Due to the reason that they are chronically infected ii. Hyperplasia of reticuloendothelial system vi. Hereford calves can get bright red nose, conjunctiva and tongue have petechiations, ascites, enlarged nodular liver, spleens enlarged, lymph nodes enlarged c. Prevention i. Management 1. Bring heifers in area early so they can be exposed and bitten by tick and develop immunity, then breed them after 2. Bring cows in the area that are at least 6-7 months pregnant, they usually don’t abort VIII. Mycotic abortion a. Northern problem in winter or early spring b. Confined cows in barns eating hay or silage c. Most occur because cow is exposed by digestive or respiratory tract d. Causes: i. Aspergillus fumigatus MC ii. Zygomyces 1. Absinea e. Sporatic causes of abortions (10% of all abortions you will see) f. Late term abortion between 6-8 months of gestation g. Fetus expelled soon after it dies (common with Aspergillus) h. Zygomyces i. Hemorrhage and necrosis of caruncle i. Diagnosis i. Distinct placentitis 1. Cupped cotyledons – edges are thickened 2. Thickened intercotyledonary space 3. Exudate 4. Necrosis at base of caruncle ii. Fetus will have ringworm type lesions with Aspergillus (30%) iii. Use potassium hydroxide on a slide and use abomasal contents of fetus or scrape skin lesions 1. Will see fungal hyphae IX. Get BVD Handout from Anthony Goat Diseases I. H.A.A.G. (Habitual Abortion of Angora Goats) a. Condition in Angora goats i. Used for mohair production b. High incidence in S. Africa, not found in US c. Habitual abortions d. Older large does (4 yrs +) i. Goats were genetically selected for high production of mohair – more hair affects adrenal function ii. In stressful conditions they make a lot of hair and the adrenal function is not good iii. Then baby gets stressed and his adrenals become hyperplastic 1. Fetus produces high cortisol iv. Baby is aborted e. Lesions in adults i. Adrenal atrophy ii. Placentome degeneration iii. Regression of corpus luteum (CL) 1. CL is required for the entire length of gestation in the goat, NOT in the sheep f. Lesion in fetus i. Dysmaturity ii. Retarded growth iii. Anemic iv. Adrenal hyperplasia – produce too much cortisol v. Thymic atrophy Ovine Abortions (Sheep) I. Campylobacter abortion a. Campylobacter jejuni b. Campylobacter subspecies fetus c. Not a venereal disease like in cattle d. e. f. g. h. II. III. IV. V. Late term abortions Abortion storms in naïve herds only Premature lambs, weak lambs, high mortality Carrier animals are present – ewes and lambs Transmission i. Ingestion 1. Organism localizes in mucosa of gallbladder i. Lesions i. Nothing specific in adults ii. Fetus 1. Donut lesions in the liver that have raised edges, yellowish in color a. Classic sign for this diseases j. Diagnosis i. Culture or isolate organism: 1. Abomasal contents, aborted fetus, vaginal discharges ii. Microscopy (darkfield or phase contrast) iii. Fluorescent antibody testing Listeriosis a. Listeria monocytogenes b. High incidence of intestinal carriers c. Transmission i. Ingestion d. Abortion rate is 10-20% e. Lesions i. Ulcerations or erosions in larynx f. Diagnosis i. Culture cotyledons, fetal organs, vaginal discharges Leptospirosis a. Not common in sheep b. Most common if you get it is L. hardjo i. Can also get L. pomona c. Sheep seem to be more resistant than cattle d. Carrier animals e. Transmission i. Contaminated water and feed from carriers f. Clinical signs i. Weak lambs, stillborns, abortions ii. Maternal illness and death possible Other bacteria associated with abortions in sheep a. Actinomyces pyogenes – no specific signs Chlamydial abortions a. AKA Enzootic Abortion of Ewes b. Chlamydia psittici c. Pigeons, sparrows carry it d. Two strains (both caused by same organism) i. Conjunctivitis and polyarthritis strain ii. Abortion strain (what we are concerned with for exam) 1. Mummified fetuses or macerated fetuses, stillborns, weak lambs that die 2. Latent infections - carriers 3. Lambs with congenital infections e. Ewes infected in last month of pregnancy i. Abort in next pregnancy f. Ewes infected in mid-gestation abort this pregnancy g. Transmission i. Ingestion h. Classic picture i. Late abortions in last 2-3 weeks of gestation ii. Virgin and naïve herds have 50% of herd experiencing abortions iii. Ewes that abort: 1. Rear end is covered in yellowish-brown exudate iv. Retained fetal membranes v. Cotyledons are dark and mottled, red-brown exudate to them i. Diagnosis i. Intracytoplasmic inclusions on microscopic evaluation = elementary bodies ii. Fetal lesions 1. If aborted < 120 days of gestation a. Autolytic fetus 2. If aborted > 120 days a. Similar situation to Foothill Abortion in cattle b. Focal hyperplasia of reticuloendothelial system: enlarged livers, lymph nodes, and spleens iii. Microscopic evaluation of placenta, vaginal smears iv. Fluorescent antibody test on tissue v. Compliment fixation on dam’s serum j. Prevention i. Vaccination 1. Killed 2. Vaccinate ewes 8 weeks before breeding VI. READ CHAPTER 76 IN THERIO BOOK (Infectious causes of abortion)