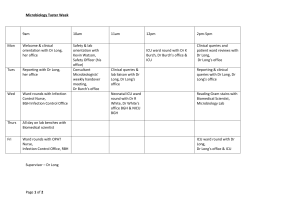
Training and Teaching specific to Microbiology
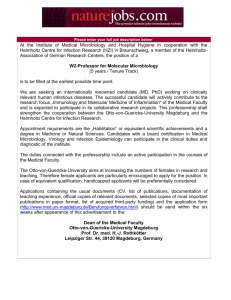
advertisement

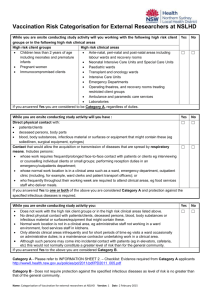
OXFORD DEANERY SPECIALTY TRAINING PROGRAMME IN INFECTIOUS DISEASES/MICROBIOLOGY and INFECTIOUS DISEASES/GENERAL INTERNAL MEDICINE About Oxford Deanery The Oxford Deanery covers the counties of Oxfordshire, Berkshire and Buckinghamshire, with Banbury and Milton Keynes in the North, to Reading and Slough in Berkshire and High Wycombe and Aylesbury in the East. The Oxford Deanery is part of the South Central Strategic Health Authority which serves a large population and covers the regions mentioned above as well as the Wessex Deanery areas of Hampshire and the Isle of Wight. The Oxford Deanery is responsible for the training of some 1500 trainees. The Oxford Deanery is a relatively small deanery with a defined geographical area which serves as a single unit of application. In the majority of cases successful candidates will be asked to preference their choice of location for either one or two years. Some programmes will require successful candidates to indicate a location and specialty. Future placements will usually be based on individual training and educational needs. Please note that applications are to the Oxford Deanery as a whole. This may mean that you may be allocated to any geographic location within the Oxford Deanery depending on training needs. These posts also have opportunities within Wessex Deanery The Infectious Diseases/Microbiology and Infectious Diseases/GIM Training Programme The Infectious Diseases and Microbiology training programme is a 6 year programme, starting at ST3. The Infectious diseases/GIM programme is a 5 year programme starting at ST3. During this time, the trainee's work will be monitored for satisfactory progress and subject to annual reviews in the form of ARCPs. Progression on the programme will be dependent upon these reviews. The posts on this rotation have been approved for Specialist Training by the Royal College of Physicians and the Royal College of Pathologists. The posts attract National Training Numbers and provide training towards a Certificate of Completion of Training (CCT). The Postgraduate Dean has confirmed that this post has the necessary educational and staffing approvals. The programme is based in several different Trusts throughout the Oxford Deanery. Opportunities also exist in Wessex deanery so trainees may find themselves placed in any of the following hospitals: Trust Hospitals and Locations John Radcliffe Hospital, Oxford Horton General Hospital, Banbury Oxford University Hospitals NHS trust Churchill Hospital, Oxford Nuffield Orthopaedic Centre, Oxford Buckinghamshire Healthcare Stoke Mandeville Hospital, Aylesbury Heatherwood and Wexham Park Hospitals Wexham Park Hospital, Slough (HWPH) University Hospital Southampton NHS Foundation Southampton General Hospital Trust Princess Anne Hospital Southampton’s Children’s Hospital Trust Information Oxford University Hospitals Oxford University Hospitals (OUH) is made up of four hospitals - the John Radcliffe Hospital (which also includes the Children's Hospital and West Wing), Churchill Hospital and the Nuffield Orthopaedic Centre, all located in Oxford, and the Horton General Hospital in the north of Oxfordshire. A wide range of clinical services is provided including specialist services such as including cardiac, cancer, musculoskeletal and neurological rehabilitation. In 2011/12 there were 727,448 outpatient appointments in the Trust's hospitals, and 22,505 inpatient admissions: 9,041 babies were delivered. The trust employs around 11,000 people and the turnover in 2011/12 was £788 million. Collaboration with the University of Oxford underpins the quality of the care that is provided to patients; to the delivery of high-quality research bringing innovation from the laboratory bench to the bedside; and the delivery of high-quality education and training of doctors. Existing collaborations include the ambitious research programmes established through the Oxford Biomedical Research Centre (BRC), funded by the National Institute for Health Research (NIHR), located on the John Radcliffe Hospital site and at the Biomedical Research Unit in musculoskeletal disease at the Nuffield Orthopaedic Centre. Buckinghamshire Healthcare NHS trust Buckinghamshire Healthcare NHS Trust is a major provider of community and hospital services in South Central England, providing care to over half a million patients from Buckinghamshire and neighbouring counties every year. It is responsible for the majority of NHS care in the county, from community health services provided in people’s homes or from one of our many local bases, to acute hospital services at Stoke Mandeville, Wycombe and Amersham. Stoke Mandeville Hospital is home to the internationally recognised National Spinal Injuries Centre, one of only 11 such centres of expertise in the UK. It is also a regional centre for burn care, plastic surgery and dermatology, and recognised nationally for urology and skin cancer services. Heatherwood and Wexham park NHS trust Heatherwood and Wexham Park Hospitals NHS Foundation Trust provides hospital services to a large and diverse population of more than 450,000 which includes Ascot, Bracknell, Maidenhead, Slough, south Buckinghamshire and Windsor. There are approximately 30 languages spoken in the area, the top six of which (excluding English) are Hindi, Polish, Urdu, Somali, Romanian and Punjabi. The Trust became a Foundation Trust in 2007 and with approximately 3,200 staff, it provides acute services that include cardiology, maternity, stroke and emergency from two main sites in Wexham Park (Slough) and Heatherwood (Ascot). It also offers a range of outpatient, breast screening and diagnostic services from four other sites: (King Edward VII Hospital in Windsor, St. Mark's Hospital in Maidenhead, Fitzwilliam House in Bracknell, Chalfonts Outpatients in Chalfont St Peter) Each year it sees approximately: 33,000 day cases and elective inpatients, 36,500 emergency inpatients , 5,500 births, 112,000 A&E attendances University Hospital Southampton NHS Foundation Trust University Hospital Southampton NHS Foundation Trust (UHSFT) is the only acute inpatient medical unit in Southampton. The Trust has approximately 1,400 beds and serves a local population of 640,000 and also provides a portfolio of highly specialist tertiary services for the local population and for a wider catchment of 3 million across central southern England and the Channel Islands. UHSFT is a designated Cancer Centre and in 2011 the Trust was designated a Major Trauma Centre and has facilities to receive critically ill patients via air ambulance. UHSFT Paediatric services will shortly be located in the newly built on-site Southampton Children’s Hospital. Obstetric and Gynaecology services are provided by the on-site Princess Anne Hospital and UHSFT is a tertiary referral centre for foetal and neonatal medicine and surgery. UHSFT has three adult (general, cardiothoracic and neurosurgical) intensive care units (ICUs) and two Paediatric (neonatal and general paediatric) ICUs. Rotation Information The objective of the post is to produce specialists with adequate training and experience to be awarded a Certificate of Completion of Training (CCT) in Medical Microbiology and Infectious Diseases or Infectious Diseases/General Internal Medicine. In agreement with the training committee, there may be opportunities for candidates to train for a career as a consultant in Communicable Disease control. Training will be in accordance with the requirements laid down by the JRCPTB/RCPath programme on joint training in Medical Microbiology/Infectious Diseases or Infectious Diseases/General Internal Medicine. There may be changes in programme requirements, curricula, work placed based assessments and knowledge based assessments when the new combined infection programme is introduced by the Royal College (anticipated date August 2014). The programme can be adjusted flexibly to meet the needs of individuals depending on previous experience. The GIM, ID and Microbiology training curricula (2010) are available on the relevant college websites. The joint training offered in Infectious Diseases/Medical Microbiology and Infectious Diseases/GIM is based in the integrated Departments of Microbiology/Infectious Diseases and GIM at the OUH, and associated district general hospitals. There are also opportunities in Wessex Deanery (Southampton). There will be flexibility allowing rotation to a variety of infection related modules. Training will be arranged in any of the following departments: 1 2 3 Medical Microbiology at the Oxford University Hospitals, Buckinghamshire Healthcare NHS Trust (High Wycombe/Aylesbury), Heatherwood and Wexham Park Hospitals (HWPH) and/or University Hospital Southampton NHS Foundation Trust. Infectious Diseases at the OUH (includes the Horton hospital in Banbury), HWPH, University Hospitals Southampton NHS Foundation Trust and the Bone Infection Unit at the NOC. General medicine at the OUH (John Radcliffe or Horton Hospitals) or University Hospital Southampton NHS Foundation Trust. LAT posts LATS will participate in the same training overall rotation as those with training numbers. LAT trainees are required to obtain competencies appropriate to their stage of training and to undergo annual review (ARCP) with other trainees. A 12 month LAT post will comprise at least six months infection consult service and up to six months direct patient care (general medicine under the supervision of an infectious diseases consultant). In addition to OUH, trainees may rotate to Buckinghamshire Healthcare NHS Trust (based in Aylesbury), Heatherwood and Wexham Park Hospitals (based in Slough) and/or University Hospital, Southampton NHS Foundation Trust NTN posts Years 1 to 4: 1) At least two years will be spent acquiring training in laboratory based infections and health protection. This may include 6-12 months at Buckinghamshire Healthcare NHS Trust, at HWPH or University Hospital Southampton NHS Foundation Trust 2) At least two years of direct patient care on the infectious diseases unit, bone infection unit and in related clinical disciplines. a) One year will be spent in Infectious Diseases (Churchill site, OUH). b) Six months on the Bone Infection Unit (NOC) c) Six months will be spent at the OUH (John Radcliffe Hospital or Horton Hospital), University Hospital Southampton NHS Foundation Trust (UHSFT) or Heatherwood and Wexham Park Hospitals NHS trust doing general medicine & Infectious diseases consults and a general medicine/infectious diseases OPD clinic. d) Three to four month’s Intensive care (OUH) is an optional but highly recommended component of the training programme. This module is usually in the first 2 years. Year 5: Up to one year of research may count towards training. Independent funding will need to be found for those undertaking dedicated periods of research, otherwise year 5 will have the same format as year 6. If doing GIM then this year will comprise of general internal medicine Year 6: (ID/Micro only) The final year will depend on the needs of the trainee and availability. It may consist of electives tailored to the needs of the individual; the aim will be to gain additional experience in subjects that can be developed further in training. Elective options Elective rotations may be available by negotiation. Options include: Infection Prevention and Control General (Internal) Medicine, Intensive Care Ward Tropical Medicine Unit Paediatric Infectious Disease, Health Protection Agency (reference & specialist laboratories, Communicable Disease Surveillance Centre and local and regional services) Genito-urinary Medicine Attachment to an established Infectious Disease/Virology unit abroad. Attachment to an HIV unit in London. Attachment to virology unit e.g. in London An example of combined training in Microbiology and Infectious Diseases. A diagram of possible training programme is given. This may be revised depending on circumstances and discussion. YEAR 1 Microbiology Bench rotation and modules in microbiology & virology. This may include 6-12 months at Buckinghamshire Healthcare Hospitals (BHH) or HWPH. RCPath Year 1 assessment and FRCPath part 1 YEAR 2 Clinical Infectious Diseases 6 months - Bone Infection Unit 6 months - Infectious Diseases ward. There may an opportunity to do a 3 months elective in ITU medicine in year 2 or 4. YEAR 3 Microbiology (This may include 6 months at BHH or HWPH Hospitals) (MRCPath Part 2 at end of year) YEAR 4 Clinical Infectious Diseases 6 months - Infectious Diseases ward and 6 months Acute Medicine. There may an opportunity to do a 3 months elective in ITU medicine in year 2 or 4. RCP Speciality Certificate Exam in Infectious Diseases early in year YEAR 5 Research, if funded, or further Microbiology & Virology/ Infectious Diseases. (or GIM) YEAR 6 Electives See above Teaching Training and courses The following training sessions are provided and are mandatory. Oxford Infection seminars: Tuesday 1pm. Specialist trainee teaching sessions: Tuesday 2.15-3.30pm: These cover a wide syllabus of subjects relevant to Clinical Microbiology, Infection Control, Infectious Diseases and Health Protection. The microbiology sessions are geared to study towards the MRCPath examination and are consistent with the RCPath curriculum in Medical Microbiology. Inter-departmental case presentations (ID, Microbiology, Virology, Bone infection, Paediatric ID, Immunology): Tuesday 4pm-5pm. Specialist registrars present cases with some discussion. During attachments in microbiology; Specialist trainee led ‘septic spot’. An issue of the week is presented. These occur on Friday mornings at 9am. Individualised bench rotations and teaching/supervision by laboratory Biomedical Scientists. During attachments in General Medicine trainees are expected to attend weekly case conferences, grand rounds and M&M meetings plus monthly audit meetings. ID/GIM trainees are expected to attend monthly all day GIM teaching sessions throughout their training. In addition, post-holders are encouraged, at appropriate stages in their training, to attend relevant medical education courses that include an epidemiology/statistics course, FRCPath exam preparation (mycology and antimicrobial courses), management courses and scientific meetings. Poster and oral presentations at such meeting are encouraged. Departmental support is available to attend scientific meetings after negotiation with TPD, ES and/or other consultant staff. Opportunities for research Post-holders will be encouraged to develop research interests. Trainees are encouraged to make applications for fellowships to extend their research experience. There is a wide range of opportunities with a large number of Research Groups in a number of different departments within the Oxford NIHR Biomedical Centre and the Medical Sciences Division of Oxford University. These include the following; Nuffield Department of Medicine Nuffield Department of Clinical Sciences including Microbiology) Paediatrics Nuffield Department of Orthopaedics Primary Care Zoology BRC Infection Theme BRC Immunity Theme BRC Vaccinology Theme These Groups include the Wellcome Trust Tropical Units in South East Asia and Africa (Prof Nick White and Prof Kevin Marsh, Prof Nick Day and Prof Jeremy Farrar). The Centre for Vaccinology (Prof Adrian Hill, Prof. Andrew Pollard, Prof Helen McShane), NDM (Prof. Derrick Crook, Prof Tim Peto), Peter Medawar Building (Prof Rodney Phillip, Prof. Philip Goulder, Prof Paul Klenerman) Weatherall Insititute of Molecular Medicine (Prof Sarah Rowland Jones). Wellcome Trust Centre for Human Genetics (Prof Dominic Kwiatowski, Prof Peter Donnelly), Nuffield Department of Orthopaedics (Philip Bejon, Matt Scarborough) Collaborations exist between Microbiology/Infectious Diseases and most of these Groups. Previous microbiology/infectious diseases trainees have been awarded Wellcome or MRC research training fellowships in many of the internationally renowned research groups working on infection. Research projects with an epidemiological flavour and linked to the HPA, will be strongly encouraged. Duties of Post Enrolment with college Specialist trainees are expected to enrol with the JRCPTB at the commencement of joint training. A copy of the enrolment is also required by the RCPath. Work Place Based assessments (WPBAs) and Knowledge Based Assessments (KBAs): At present joint trainees are required to fulfil the curriculum requirements of the RCP and the RCPath. KBAs End of year 1 (approx. May): RCPath, Year 1 assessment. After 1 year training: MRCPath Part 1 After three years training o MRCPath Part 2 o ID speciality certificate examination (Royal College of Physicians) These assessments may change after introduction of the new curriculum (possibly August 2014). WPBAs Work place based assessments should be completed in line with the ARCP requirements for both infectious diseases (JRCPTB ID curriculum) and microbiology (RCPath microbiology curriculum). Appraisal/ARCPs Specialist trainees will have regular (at least three monthly) meetings with their allocated educational supervisor and have yearly ARCPs in accordance with GMC guidelines. The ARCP requires a structured educational supervisor’s report that includes signing off the required number of work based assessments in line with the recommendations of the Royal College of Physicians and the Royal College of Pathologists. Trainees will undergo a Penultimate Year Assessment between 12 -18 months before anticipated CCT date. The CCT date for individual trainees depends on College approval for experience gained prior to entering this post and satisfactory performance during this training position. Teaching responsibilities The post holder will participate in teaching of special study module medical students and other medical students in microbiology, infectious diseases and bone infection unit. Occasionally there are elective students from other medical schools attached to the units. There are occasional sixth formers on work experience attached to the unit. The specialist registrar will be expected to take part in teaching these students, both formally and informally. In microbiology the post holder will participate in teaching for the medical student pathology course (lectures, small group teaching and practicals), foundation trainees, infection control nurses and biomedical scientists. In general medicine the post holder will be expected to actively participate in undergraduate and postgraduate teaching. First year and third year clinical students are regularly attached to the Firms. Trainees are expected to complete teaching assessment tools in line with ARCP requirements. Audit Specialist trainees are required as part of their training to be able to perform audit projects. A list of audit projects is available for specialist trainees or they may elect to look at a subject of their own choice if approved by their educational supervisor. Four times a year a trainee presents an audit of relevance to clinical microbiology or infectious diseases at the Tuesday lunchtime meeting. Trainees are expected to complete audit assessment tools in line with ARCP requirements. Leave Standard study and annual leave arrangements are available to the post-holder (see terms and conditions below). Leave must be planned in advance and is by negotiation with consultant staff in line with departmental policy (available on intranet site). On call duties The appointee will be required to live within 45 minutes travel time from their major base. OUH: The post-holder will be on call for microbiology and infectious diseases (approximately 1 in 5) except during the John Radcliffe Acute medicine/ID consults and Horton modules when the post holder will participate in the general medical on call rota. The post holder will also participate in the non-resident ID/microbiology rota and the resident ‘hospital at night’ rota (1 in 18). The overtime is banded at 1B and is EWTD compliant District hospital rotations: At Bucks Hospitals at present the post-holder will participate in the Oxford on call ID/micro rota. This is subject to review. If trainees rotate to Wexham Park or Southampton local rotas will apply. Absence of colleagues Duties will involve cover for absence of colleagues on annual and study leave. Less than full time training (LTFTT) Less than full time training may be possible either by having a slot share, applying for deanery supernumerary funding, or using part of a full time salary in a full time post. LTFTT is subject to eligibility and appropriate rotations. Career Counselling Career advice and guidance should be sought, in the first instance, from your education supervisor, who will normally be a consultant for whom you work. There are a range of services available thought the post graduate centre and deanery for further careers counselling and support. Description of individual modules: SUMMARY A. Microbiology i. Microbiology, OUH ii. Microbiology, Stoke Mandeville Hospital, Buckinghamshire Healthcare NHS Trust B. Infectious Diseases i. Infectious Diseases ward and consults, Churchill Hospital, OUH. ii. Bone Infection Unit, NOC, OUH iii. John Radcliffe Hospital and West Wing, OUH iv. Horton Hospital, OUH v. Heatherwood and Wexham park Hospitals (Slough) vi. University Hospital Southampton NHS Foundation Trust C. General Internal Medicine i. John Radcliffe Hospital, OUH ii. Horton Hospital, OUH iii. Heatherwood and Wexham park Hospitals (Slough) iv. University Hospital Southampton NHS Foundation Trust A) MICROBIOLOGY Training and Teaching specific to Microbiology and Virology The detailed training programme is given in the Royal College of Pathologists postgraduate training document. Training in preparation for the year 1 assessment and MRCPath is ongoing for all candidates. In addition, attendance at courses is encouraged and sponsored by the Trust and Dean within the constraints of finance. Support for attendance at these courses is at the discretion of the supervising consultant. Attendance on other courses may also be arranged. i. Microbiology, OUH The Department of Microbiology, based on the John Radcliffe site, provides laboratory tests for the Oxford University Hospital NHS Trust, local community hospitals, Oxford Mental Health Care Trust, district general hospitals within South Central, and Primary Care. The laboratory is CPA accredited, and approved by the RCPath for higher specialist training in Microbiology. It processes 650,000 tests per year, of which about 200,000 are virology/serology or molecular diagnostics. The laboratory is well equipped with automation for molecular diagnostics, automated bacterial identification and antibiotic susceptibility testing, and a MALDI-TOF for bacterial identification. The majority of samples for serology are processed in a multi-disciplinary core automated laboratory. The laboratory has a strong track record in demand management, training of biomedical scientists, and establishing techniques such culture of ‘sterile site’ samples. The laboratory takes an active role in supporting translational research through the Biomedical Research Centre and University. The Oxford University Hospitals NHS trust provides acute medical and surgical services for the people of Oxfordshire and also regional specialist units (e.g. solid organ (kidney, pancreas and small-bowel) transplant, bone marrow transplant, neuro-surgery, cardio-thoracic-surgery, trauma and reconstruction, bone infection unit, haemo-dialysis, cystic fibrosis unit, a dedicated Children’s hospital, infectious diseases etc.). A full range of microbiological tests is performed to support the above services and offers an excellent opportunity to acquire routine and specialist bench laboratory testing knowledge. The Virology section offers a regional service and an extensive range of virological tests is available including molecular assays. This section offers an excellent opportunity to gain experience in clinical virology. Specialist trainees The microbiology component of the post is suitable for training in Clinical Microbiology and Virology/Infectious Diseases (2 years) and also in Infectious Diseases and General Medicine (1 year). It includes modules with the following components; a) Laboratory microbiology (including virology). Includes daily AITU ward round. b) JR1& 2 microbiology consult service (gen med, gen surgery, cardiothoracic surgery, cardiothoracic ITU) c) West wing (specialist surgery, including plastics, ENT, ophthalmology, neurosurgery, plus neurology and NITU) and trauma microbiology consult service. d) Hospital infection prevention and control e) Viral hepatitis clinics It is expected that during the whole period in microbiology there will be substantial involvement and participation in practical bench microbiology. This includes virology (serology and molecular diagnostics), blood cultures, urines, swabs, pus, sterile sites, respiratory, faeces, antibiotic assays, quality control and media. There will also be close links with hospital infection prevention and control. There will be participation in the microbiology/ID on call and medical hospital at night rotas. The Clinical service offered by Clinical Microbiology is increasingly being integrated with Adult Infectious Disease, Paediatric Infectious Disease, Communicable Disease Control and Tropical Medicine. Therefore, the post holder can expect to become involved with each of these departments. Principal Responsibilities The Specialist Registrar will participate in the clinical microbiology service under the direction of a consultant. The training is organised in modules each consisting of 3 months. Trainees can extend modules depending on their training needs. The responsibilities in each module will vary and detailed module descriptions are available. They will include participating in the supervision of laboratory, review of laboratory results and responsibility for bedside consultation on infected patients. Participation in hospital infection control, control of communicable disease activities and laboratory management also forms part of the modules. There will be close involvement with the Oxford Infection Control Service, which serves all the Oxford Hospitals. It is a busy service that offers an ideal opportunity to acquire knowledge of an Infection Control service operating in a large teaching hospital offering both DGH type and specialist medical services. Daily commitment in OUH microbiology (varies according to module) Mon Tues Wed Thurs Fri AM 9am handover meeting, Bench work, enquiries, consults. Viral hepatitis clinic. Clinical plate and IC round. Bench work, enquiries, consults. Specialist Trainee AITU ward round. 9am Pharmacy/Infection Control/ID MDT Bench work, enquiries, consults. Management meeting. Infection control meeting. Clinical plate and IC round. Bench work, enquiries, consults. Clinical plate and IC round. “Septic spot” Bench work, enquiries, consults. Clinical plate and IC rounds. 10am Pharmacy/Infection Control/ID MDT PM Consultant ward rounds. Consultant ITU and Neuro ITU ward rounds. 3pm Cardiothoracic MDT. Registrar teaching half day at JR 1pm Academic meeting, 2.15pm registrar teaching, 4pm departmental meeting Consultant ward round. Consultant ITU ward round. Grand Round, Neuro ITU ward round. Trainee ITU ward round. Consultant ward rounds. Consultant ward round. Consultant ITU ward round. Office facilities Ample computer facilities are available for the use by the appointee, secretarial support is available and shared office space is provided. ii. Microbiology, Stoke Mandeville Hospital, Buckinghamshire Healthcare NHS Trust Monday Tuesday Wednesday Thursday Friday AM Link with BMS staff in laboratory; gain bench skills in variety of areas of microbiology. Accept first clinical consults and queries from Trust clinical staff on telephone. Help to complete daily ITU microbiology charts for rounds held later in day. Join consultant microbiologist for “bench round” when performed. PM As Wednesday – Friday Registrar teaching half day at JR. 1.00 pm Academic meeting 2.15 pm Registrar teaching 4.00 pm Departmental meeting If required, gain experience in initial processing of samples received in laboratory. Join consultant microbiologist for daily ITU ward round and visit patients on other wards requiring clinical microbiology input. Liaise with local GPs/Public Health regarding important results which merit urgent attention. Trainees are encouraged from an early stage to be the first contact for clinical hospital based consults telephoned through to the Microbiology Department. After due training and observation, trainees may also answer GP enquiries and telephone results to primary care surgeries. Participation when required at any “Grand Round” presentation is encouraged and the trainee will be able to attend various meetings, whenever possible. These include meetings such as the Infection Prevention and Control Committee or specific outbreak investigation meetings. Participation in audit in both Microbiology and Infection Control departments or where contributing to another directorate’s audit, is strongly encouraged. The trainee will help with Infection Control surveillance work where appropriate. Since Spring 2011, the Microbiology Dept of Buckinghamshire Healthcare Hospitals (BHH) has been merged onto one site at Stoke Mandeville Hospital. The trainee will therefore spend the vast majority of time at this site. In addition the Trust’s reconfiguration plans taking place since 2011 have resulted in most major clinical services orientating to the Aylesbury end of the district. Buckinghamshire Healthcare Trust offers tertiary referral specialist units for both spinal injury and burns patients. The trainee should therefore gain some specific experience in microbiological issues related to these clinical areas. Whilst attached to BHH, trainees will be allowed to return to OUH for lectures and formal teaching sessions on Tuesday afternoons unless specifically requested to remain at BHH for clinical service reasons due to colleague absence etc. B) INFECTIOUS DISEASES i. Infectious Diseases ward, Churchill Hospital, OUH. The Infectious Diseases Unit, is based at the John Warin Ward which is a 20-bedded unit. This ward admits acutely ill adults with community acquired infections and imported diseases and also provides the only in-patient service for HIV positive patients in the district. There are 18 single rooms so that the ward can provide isolation facilities for nosocomial infections that require isolation and for tuberculosis. The ward also houses an outpatient service for fever, HIV disease and infectious diseases. An active intravenous antibiotic service is provided for patients who can be treated either as outpatients or in their own homes for a variety of bacterial infections. Experience in the following specialist clinics is available: HIV infection, Chronic fatigue, Travel medicine and Genitourinary medicine. There is also a very active consultation service across the Churchill dealing with complex infective issues in Immunocompromised patients (e.g. renal, pancreas and small bowel transplant patients, haematology-oncology) and other patient groups (e.g. in the diabetic centre, surgical units and Churchill adult ICU) This part of the post is suitable for training in Infectious Diseases and Microbiology or Infectious Diseases and General Internal Medicine. The post provides clinical experience in a wide range of infections including unselected community infections, HIV/AIDS, imported infections. There are also infection outpatients including a travel clinic. Trainee will also participate in a clinical consult service at the Churchill Hospital (including ITU, general surgery, renal, urology, haematologyoncology and Transplant patients). The main duties and responsibilities of the post are for the day-to-day supervision of ward inpatients on the infectious diseases ward, review of consults on the Churchill site, ITU ward rounds and participation in infectious diseases clinics. The specialist registrar will also be involved in assessing referrals made in the infectious diseases department from other hospitals in Oxford. Daily commitments will be roughly as outlined in the following timetable. Daily Commitment (2 registrars): Monday AM Ward work/consults, CICU ward round PM Ward Work/Consults/Travel Clinic Tuesday Consultant ward round. CICU WR Wednesday ID Outpatients Clinic, CICU WR Registrar teaching half day at JR 1pm Academic meeting, 2.15pm registrar teaching, 4pm departmental meeting Ward work/Consults. TB clinic Thursday Dept of Med meeting, CICU WR Grand Round/Ward work/Consults ID Outpatients clinic X-ray meeting, Multidisciplinary 2pm transplant meeting meeting, Consultant ward round, CICU Ward work/Consults WR Friday Administration/Management There is a doctor’s office on the ward with appropriate computer facilities, including electronic access to laboratory results and medical literature searching. There is a full-time secretary/administrator on the ward and a part-time typist for clinical letters and discharge summaries. During their tenure, the specialist registrar will have the opportunity to attend management courses in the region. ii. Bone Infection Unit, NOC The Bone Infection Unit (BIU) at the Nuffield Orthopaedic NHS Trust is unique in the UK and consists of a 26-bed unit admitting patients with bone infections. The clinical service provided by the BIU team includes caring for the medical aspects of all the BIU patients, providing infection consults at the Nuffield Orthopaedic hospital and participating in the home IV and bone infection out-patients. This part of the post is suitable for training in Infectious Diseases and Microbiology or Infectious Diseases and General Medicine. The main duties and responsibilities of the post are for the day-to-day supervision of ward inpatients on the Bone Infection Unit, and the participation in the Bone Infection clinic on Thursdays and the Home Intravenous Therapy clinic on Wednesdays. The specialist registrar will also be involved in assessing referrals made in the Bone Infection Unit from other hospitals in Oxford. Daily commitments will be roughly as outlined in the following timetable. Daily Commitment: Monday AM Ward work (ID consults) PM Multi-disciplinary ward round Tuesday Consultant ward round Wednesday Ward work (ID consults) Registrar teaching half day at JR 1pm Academic meeting, 2.15pm registrar teaching, 4pm departmental meeting Home IV Clinic Thursday Bone Infection Clinic Friday Consultant ward round Medical Grand Round, Radiology case conference, Ward work. 1.30pm Hip and Knee MDT, Ward work Administration/Management There is a doctor’s office with appropriate computer facilities, including electronic access to laboratory results and medical literature searching. There is full secretarial support for clinical letters and discharge summaries. iii. John Radcliffe Hospital, OUH (Acute medicine and ID consults. Also for GIM training) The John Radcliffe Hospital is the only acute hospital for South Oxfordshire. The acute medical firms admit about 10,000 patients per year with unselected medical problems. There are 160 medical beds including an emergency assessment unit and short stay ward. The unit is staffed by consultant firms, with a majority of patients being admitted and discharged by the same team. Patients staying in hospital are transferred to one of four general medicine wards (each consultant firm looks after half of a general medicine ward). This part of the post is suitable for training in Infectious Diseases and General Medicine. Trainees will be attached for the relevant period to do acute on-take medicine at the John Radcliffe Hospital to secure accreditation in general internal medicine. There are 8 active consultant firms at any one time. Each firm has a consultant, an St3+ , an F2/CMT and 2 FY1s. There are three "takes" a day, (9am-4pm, 4pm-9pm, 9pm-9am) with the hospital at night team covering overnight admissions (one of the consultant firms undertakes a round of these patients from 0800, and takes over their ongoing care. In any 12 consecutive weeks, a St3+ will do 8 weeks of day time work including 1 in 4 weekday long days and weekends, and during the subsequent 4 weeks they only do either 4 weekday nights or 3 weekend nights. Leave is incorporated into the rota. Trainees are paid at IA. Specialist Trainees are expected to provide medical input to their patients on ITU. Apart from daily ward rounds and 1 in 4 take rounds, trainees are expected to attend weekly case conferences, grand rounds, weekly M&M meetings, monthly audit meetings and all day teaching sessions. Outpatient duties and participation The trainees will participate in a weekly general medicine outpatient clinic Principal Responsibilities of Post Day-to-day management of general medicine inpatients under the care of consultants of the firm. Responsibility for acute "on-take" patients, general medical outpatients work (one-two clinics per week depending on firm). Supervision of SHO's and foundation year doctors. Teaching – as described in the general section of this document. iv. Horton Hospital, OUH (Infectious Diseases and GIM) The Horton attachment is suitable for training in Infectious Diseases and General Medicine. Trainees will be attached to one of four firms, each of which has two consultants, two specialist trainees and at least one SHO and one HO. The Horton Hospital operates a ward based system for medical staff. Patients whose primary medical problem is infection will be admitted preferentially to the clinical infection firm when possible. As a result of the ward based system, there is usually capacity for new patients to be admitted under the firm’s care on a daily basis. The firm also provides ongoing care to medical outliers on surgical wards who are admitted during the team’s take period. Medical takes are shared equally between the firms. Currently there are two consultant led posttake ward rounds in any 24 hour period. There is a formal handover meeting at 9am each week day for which attendance is mandatory The module will give the trainee experience in unselected medical admissions, domestic and imported infections presenting to acute general medicine, surgical site infections, infections relating to trauma and orthopaedics and hospital infection control. Weekly timetable: Monday Tuesday Wednesday Thursday Friday am Handover, ITU round, ward round, Handover, ward round, consults Handover, ITU round, ward work, MDT meeting Handover, ward round, X-ray meeting Handover, ITU ward round, ward work Pm Journal club, OP clinic, consults Registrar teaching half day at JR 1pm Academic meeting, 2.15pm registrar teaching, 4pm departmental meeting Consults, infection control, administration Case conference, consults, teaching and infection control Ward work, consults Outpatient clinics The trainees will have the opportunity to participate in a weekly clinical infection outpatient clinic Principal Responsibilities of Post Specialist trainees will be responsible for day-to-day management of general medicine inpatients under the care of consultants of the firm, acute "on-take" patients, and the supervision of SHO's and foundation year doctors. Trainees in clinical infection will contribute to the infection consult service, regular ITU/CCU ward rounds and the promotion of good clinical practice in relation to antibiotic guidelines, antimicrobial stewardship and infection control. v. Heatherwood and Wexham Park Hospitals (Infectious Diseases and GIM training) The Wexham Park attachment is suitable for training in Infectious Diseases and General Medicine. Trainees will be attached to Ward 9 Respiratory and General medicine. Wexham Park has an active clinical microbiology and infectious disease service comprising two consultants in infectious diseases, 1 consultant microbiology/infectious diseases and one consultant microbiologist. The infectious diseases team have close links with respiratory who manage inpatient care. The TB service is led by Dr Sarah Menzies (Consultant Respiratory Physician) with input from Dr Jane Democratis (Consultant Infectious Diseases). There is a weekly TB MDT before TB clinic and 3 monthly TB/HIV and TB/paediatric MDT’s. Inpatients with suspected TB, HIV related illness and imported infections are preferentially housed on ward 9. The infection service is a consult based service with three outpatient clinics: General infectious diseases, OHPAT and Viral hepatitis and weekly MDT meetings with haem/onc, the diabetic foot team, HIV, and TB. There are twice weekly antimicrobial stewardship ward rounds and a daily ICU ward round. Principal Responsibilities of Post Specialist trainees will be responsible for day-to-day management of general medicine inpatients under the care of the respiratory consultants, acute "on-take" patients, and the supervision of SHO's and foundation year doctors. Ward 9 has an F1 and an F2 trainee on a combined infectious diseases/respiratory rotation. The infectious diseases/GIM trainee will be involved in TB and respiratory consults, TB MDT and TB and general respiratory clinics shared with the other 2-3 respiratory registrars. There are optional opportunities to further ID training experience with the infection team in the outpatient clinics, MDT, antimicrobial stewardship ward rounds, infection control and audit at Wexham Park. Tuesday afternoon registrar teaching takes place in Oxford. In both cases attendance must with prior agreement from the respiratory team. There is an unselected medical take. Patients are admitted from A and E to MAU (wards 7 and 8) and the medical wards thereafter. New post take patients come to the ward daily. There are two consultant led post take rounds a day. Trainees are paid band 2B. Outpatient duties and participation There is a weekly TB clinic at King Edward VII hospital, Windsor Monday Tuesday am Micro weekend handover 1pm Medical meeting Journal club Ward work/consults Wednesday Ward work/consults Thursday Friday Consultant ward round Ward work/consults Radiology MDT pm Consultant ward round Registrar teaching half day at JR 1pm Academic meeting, 2.15pm registrar teaching, 4pm departmental meeting TB MDT followed by TB Clinic (King Edward VII) Respiratory OPD(King Edward VII) Ward work/consults vi University Hospital Southampton NHS Foundation Trust (UHSFT) (Infectious Diseases and General Medicine) Approximately 15,000 adult patients per annum are admitted via the acute medicine service into 250 beds and around 20% of patients admitted through acute medicine have infections. Consequently, UHSFT continually provides care to a large number of challenging and complex infection cases, across an extremely wide spectrum of clinical specialties, both in inpatient and outpatient settings. Trainees undertaking this post in Infectious Diseases will be provided with a wealth of excellent training and learning opportunities, enabling them to gain valuable experience in managing all aspects of community and hospital acquired infection and to gain all appropriate competencies specified by the national curriculum for Infectious Diseases. The Trust is committed to further developing its clinical infection services and the trainee will play an active and closely supervised role in this process and the ongoing development of the UHSFT Department of Infection. All consultants and trainees in infection at UHSFT maintain close working links with the Health Protection Agency (HPA) microbiology laboratory sited within UHSFT. The laboratory processes in excess of 600,000 specimens per annum. The laboratory provides a comprehensive diagnostic service in bacteriology, mycobacteriology, mycology, virology and parasitology and has a wellequipped molecular facility providing diagnostics for a wide range of viral and bacterial pathogens. The joint training provided in Infectious Diseases and Medical Microbiology/Virology at UHSFT is based in the integrated Department of Infection, incorporating Infectious Diseases, Medical Microbiology, Medical Virology and Infection Prevention and Control. Inpatient ID service The Infectious Diseases Firm is one of the medical specialty firms within the Division of Emergency and Specialist Medicine. Patients are triaged by acute medical admission services, and those with community acquired infections or imported infections are then managed by three ID Physicians (a fourth is to be appointed by April 2013). Each morning, there is a daily consultant-led ID ward round, to include pick up of new cases of community acquired or imported infection on the acute medicine unit (AMU). Whilst inpatients are admitted initially to AMU, those whose length of stay is anticipated to exceed 72 hours are usually transferred to other inpatient medical beds. Side rooms are utilised where necessary but patients requiring isolation, including some with respiratory infections, are managed in the 15 bed Infectious Disease Unit. This ID Firm is supported by 2 Foundation trainees/SHOs, and Infectious Diseases specialty registrars will provide middle grade care of these patients who will be managed by the ID team from admission-to-discharge, including outpatient follow-up where necessary. The Infectious Diseases Firm has close links with respiratory physicians (Drs Ben Marshall, Anindo Banerjee, Rachel Limbrey and Paul Elkington) who care for inpatients with TB and inpatients with complications of HIV. In the future it is envisaged that the ID Firm will have an increasing involvement in the management of inpatients with opportunistic infections and complications of HIV. Infection consult service UHSFT Consultants in Medical Microbiology, Medical Virology and Infectious Disease provide a comprehensive infection consult service for inpatients. Specialty trainees in ID will receive training from, and contribute to this service, and will be supervised in providing ward based consults across all major medical and surgical specialties. UHSFT provides specialist tertiary clinical infection services in Bone Marrow Transplant (autologous and allogeneic), Cardiothoracic Surgery, Neurosurgery and Paediatrics including Paediatric Infectious Diseases/Immunology and Foetal Medicine. Specialty trainees will be provided with excellent opportunities to attain all relevant competencies during modular attachments to the Infection services in these areas, typically during modules in either years 5 and/or 6. The spectrum of patients will also include respiratory, (including cystic fibrosis), cardiology, hepatology, gastroenterology, rheumatology, HIV/GUM, and orthopaedic, gastrointestinal and vascular surgery, ENT and Urology. There is a dedicated Paediatric Microbiology and ID service and trainees will have the opportunity to gain experience in Paediatric Infectious Diseases if required. Overall Infectious Diseases trainees will be exposed to abundant learning opportunities across this spectrum including the opportunity to provide infection advice in complex infections and in a variety of immunocompromised patients. Trainees will have the opportunity to incorporate particular aspects of the Infection consult service into their weekly timetabled ward consult time (see specimen weekly timetable below). These modules will typically be undertaken for a period of 3-6 months each, in addition to providing care for the ID Firm inpatients and twice weekly clinic attendance. Modules providing ward-based consult advice include: Cancer care (Haematology and Oncology, incorporating experience in bone marrow transplant patients) Paediatric Infectious Diseases, Allergy and Immunology Cardiothoracics and Cardiology (incorporating experience in native and prosthetic valve endocarditis and sternal wound infections) Neurosciences (incorporating experience in the management of cerebral abscess and neurosurgical infection such as intra-ventricular shunt infections) Trauma and Orthopaedic surgery (incorporating experience in managing septic arthritis, osteomyelitis and prosthetic joint infection) Obstetrics and Gynaecology Surgery including upper gastrointestinal surgery, Vascular surgery, ENT and Urology (incorporating experience in complex patients including those with intestinal failure, intraabdominal collections and infections associated with prosthetic material or implants) General Medicine and Elderly Care Additional modules include but are not limited to: Infection prevention and control ICU medicine Adult Immunology Infection Clinics During the post in Infectious Diseases specialty trainees will attend two infection outpatient clinics per week. The following specialist infection clinics are available: Infection Clinic Supervising Consultants General Infectious Diseases Tuberculosis * Professor Rob Read and Drs Sarah Glover and Julian Sutton Professor Salim Khakoo, Drs Katherine Nash, Nick Sherron and Mark Wright Drs Ben Marshall, Anindo Banerjee and Paul Elkington HIV & Genitourinary medicine * Drs David Rowen, Elizabeth Foley and Sam Samraj Viral hepatitis * The Tuberculosis and HIV/GUM clinics are based at the Royal South Hants Hospital (RSH). In addition, UHSFT has an active outpatient parenteral intravenous antimicrobial therapy (OPAT) service, provided for patients with a variety of bacterial infections who are treated either as daily hospital attenders, or alternatively in their own homes. Clinical Supervision in post A team of ten Consultants in Infection (three accredited in Infectious Diseases, seven accredited either singularly or jointly in Medical Microbiology and two accredited in Medical Virology) will provide close clinical supervision for Infectious Diseases specialty trainees on a daily basis. The Consultant supervisors accredited in Infectious Diseases with direct responsibility for ID inpatient care are Professor Rob Read, Dr Sarah Glover and Dr Julian Sutton. A further ID-accredited consultant trainer will be appointed in 2013. Close daily consultant supervision will include daily Consultant-led ward rounds of ID inpatients and ID consults, twice weekly Consultant-led ID clinics and Consultant attendance and participation in teaching sessions and MDTs (e.g. educational seminars and Infection radiology meetings). Teaching sessions The following regular training sessions are provided and trainees will be expected to attend: Weekly formal education seminar (internal and external speakers) These cover a wide spectrum of subjects relevant to Clinical Microbiology and Virology, Infection Control, Infectious Diseases and Health Protection. Infectious Disease sessions will be tailored to prepare trainees for the RCP ID specialty exam. Weekly case-based (‘grey case’) meeting Weekly Infection X-ray conference. This is a service-oriented session; trainees will attend and present relevant cases Weekly Medical Grand Round Monthly Wessex regional Infection training days Monthly Infection Forum meetings (UHSFT/UoS/HPA multidisciplinary clinical-academic presentations, including Adult Infectious Diseases, Medical Microbiology, Medical Virology, Paediatric Infectious Diseases, Immunology, HIV medicine, Respiratory Hepatology etc.) In addition, numerous opportunities exist to attend specialty educational meetings (such as those provided in paediatrics, ICU medicine, medical and surgical specialties). Weekly University of Southampton (UoS) Clinical Experimental Sciences open seminars are also available. Opportunities to gain teaching experience Trainees will be encouraged and given the opportunity to participate in undergraduate and postgraduate teaching and to develop their presentation and teaching skills. Opportunities include lectures/seminars, bedside teaching and participation in Departmental and Trust meetings listed above. Research at UHSFT The UHSFT Department of Infection has strong links with a number of research groups in the University of Southampton (UoS). In particular, UoS academics in collaboration with UHSFT colleagues have a national and international reputation in respiratory disease including respiratory infections, nutrition and gastrointestinal disease and there are strong clinical research outputs in cardiology, orthopaedics and neurosciences. Research projects with an epidemiological flavour (e.g. molecular epidemiology) in collaboration with the HPA, or in infectious disease vaccinology/pathogenesis in collaboration with UoS academics will be actively encouraged. IT, office and library facilities and secretarial support Appropriate office space for trainees and IT facilities including dedicated terminals for internet access and access to relevant UHSFT information services will be provided to all specialty trainees. Meeting rooms for presentations, educational and training meetings will be provided as will access to the large, well-stocked medical library which subscribes to national and international e-journals and databases. There is a secretary/administrator attached to the ID Firm for clinical letters, outpatient appointments and discharge summaries. Each ward has appropriate computer facilities, including electronic access to laboratory results and medical literature searching. Laboratory results and the electronic patient record can be accessed by secure Wi-Fi from both Department of Infection offices and remotely on the wards. Summary of trainee’s overall role and principal responsibilities in Infectious Diseases The main duties and responsibilities of the post are for the day-to-day supervision of infectious diseases inpatients on AMU, the ID unit and the inpatient medical unit, review of consults across the UHSFT site and participation in two outpatient clinics per week, one of which will usually be the General Infectious Diseases clinic. The specialty registrar will also be involved in assessing referrals from other hospitals in Wessex and potentially supra-regional referrals. Daily commitments will be roughly as outlined in the timetable below. Illustration of weekly timetable for Specialty Registrar in Infectious Diseases: Monday AM Clinical handover meeting Consultant ward round Tuesday Consultant ward round Wednesday Consultant ward round TB clinic Case presentation meeting PM Inpatient ward work Ward consults Hepatitis clinic Ward consults OPAT clinic Infection radiology MDT Inpatient ward work Ward consults Thursday Consultant ward round Friday Consultant ward round HIV clinic Medical Grand Round General ID clinic Ward consults Education seminar Inpatient ward work Ward consults Trainees will normally participate in the weekly general Infectious Diseases clinic and one other specialty infection clinic per week. (All available clinics are shown purely for illustration). When not attending an outpatient clinic, Consultant ward round or other meeting as specified, the major duties of the specialty registrar will be in inpatient ward work and ward consults. When a trainee is undertaking a specific additional ‘module’, for example inpatient ward consults for patients with cardiothoracic infection, this clinical liaison work will be accommodated within ‘ward consults’ in the above illustrative timetable. On call at UHSFT The post holder will participate in the UHSFT Infection (Medical Microbiology/Virology and ID) oncall rota (approximately 1 in 7). Who’s Who? CONSULTANTS IN MICROBIOLOGY /INFECTIOUS DISEASES Oxford University Hospitals NHS trust Dr Brian Angus, Dr Bridget Atkins, Dr Philip Bejon, Dr Tony Berendt, Dr Ian Bowler, Dr Ivor Byren, Dr Chris Conlon, Prof. Derrick Crook, Dr Katie Jeffery, Dr Nicky Jones, Prof. Paul Klenerman, Prof. Tim Peto, Dr Sarah Rowland-Jones, Dr Matthew Scarborough, Dr Andrew Woodhouse. Paediatric ID: Dr Andrew Pollard, Dr Shelley Segal, Dr Dominic Kelly Buckinghamshire Healthcare NHS Trust: Dr David Waghorn, Dr Rubi Devi, Dr Jean O’Driscoll, Dr Kathy Cann. Heatherwood and Wexham Park Hospitals NHS trust Dr Jane Democratis, Dr Albert Lessing, Dr Veronica Garcia University Hospitals Southampton NHS Foundation Trust: Drs Sarah Glover and Julian Sutton Paediatric ID: Drs Saul Faust and Sanjay Patel CONSULTANTS IN ID/GENERAL INTERNAL MEDICINE Oxford University Hospitals NHS trust Dr Brian Angus, Dr Philip Bejon, Dr Ivor Byren, Dr Chris Conlon, Prof. Nick Day, Dr John Frater, Dr Nicky Jones, Prof Tim Peto, Dr Matt Scarborough, Prof Nick White, Dr Andrew Woodhouse. University Hospitals Southampton NHS Foundation Trust: Professor Robert Read, Drs Ben Marshall and Patrick Sharp; Senior Lecturer in Infectious Diseases (to be appointed) SPECIALIST TRAINEES ID/micro and ID/GIM Trainees in the Deanery consist of NHS STs, LATS, University clinical lecturer, Academic Clinical Fellows and Academic Clinical Lecturers. These include a number of part-time trainees. In addition there are trainees ‘Out of Programme’ doing research. There are currently 4 ‘F2s/CMT’s (3 Infectious Diseases, 1 Bone Infection) and 1 F1 (bone infection) THAMES VALLEY HPU Dr Eamonn O’Moore, Dr Noel McCarthy PROGRAMME DIRECTOR Dr Bridget Atkins (Clinical microbiology/infectious diseases) Dr Ian Reckless (General internal Medicine) EDUCATIONAL SUPERVISOR To be allocated on appointment Main Conditions of Service Appointments to this programme are subject to the Terms and Conditions of Service (TCS) for Hospital Medical and Dental Staff (England and Wales). In addition appointments are subject to: Applicants having the right to work in the UK Registration with the General Medical Council Pre-employment checks carried out by the Trust HR department, including CRB checks and occupational health clearance. The employing Trust’s offer of employment is expected to be on the following nationally agreed terms: Hours – your duty hours will be up to 48 hours per week averaged over 17 weeks(part-time staff pro rata) in accordance with the European Working Time Directive. Your hours will depend on the pattern of work offered by the employer and may include work in the evenings, at night and weekends. Pay – you should be paid monthly at the rates set out in the national terms and conditions of service for hospital medical and dental staff and doctors in public health medicine and the community health service (England and Wales), “the TCS”, as amended from time to time. The payscales are reviewed annually. Current rates of pay may be viewed at http://www.nhsemployers.org/PayAndContracts/Pay%20circulars/Pages/PayCircularsMedicalandD ental.aspx Pay supplement –depending upon the working pattern and hours of duty you are contracted to undertake by the employer you should be paid a monthly additional pay supplement at the rates set out in paragraph 22 of the TCS. The current payscales may be viewed at http://www.nhsemployers.org/PayAndContracts/Pay%20circulars/Pages/PayCircularsMedicalandD ental.aspx . The pay supplement is not reckonable for NHS pension purposes. The pay supplement will be determined by the employer and should be made clear in their offer of employment and subject to monitoring. Pension – you will be entitled to join or continue as a member of the NHS Pension Scheme, subject to its terms and rules, which may be amended from time to time. If you leave the programme for out of programme experience you may have a gap in your pension contributions. More information can be found at http://www.nhsbsa.nhs.uk/pensions Annual Leave – your entitlement to annual leave will be five or six weeks per annum depending on your previous service/incremental point, as set out in paragraphs 205-206 of the TCS. The TCS may be viewed at http://www.nhsemployers.org/PAYANDCONTRACTS/JUNIORDOCTORSDENTISTSGPREG/Page s/DoctorsInTraining-JuniorDoctorsTermsAndConditions150908.aspx Sick pay – entitlements are outlined in paragraph 225 of the TCS. Notice –you will be required to give your employer and entitled to receive from them notice in accordance with paragraphs 195-196 of the TCS. Study Leave –the employer is expected to offer study leave in accordance with paragraphs 250254 of the TCS. Local policy and procedure will be explained at induction. Travel Expenses – the employer is expected to offer travel expenses in accordance with paragraphs 277-308 of the TCS for journeys incurred in performing your duties. Local policy and procedure should be explained at induction. Subsistence expenses – the employer is expected to offer subsistence expenses in accordance with paragraph 311 of the TCS. Local policy and procedure should be explained at induction. Relocation expenses – the employer will have a local policy for relocation expenses based on paragraphs 314 – 315 of the TCS and national guidance at http://www.nhsemployers.org/PAYANDCONTRACTS/JUNIORDOCTORSDENTISTSGPREG/Page s/DoctorsInTraining-JuniorDoctorsTermsAndConditions150908.aspx. You are advised to check eligibility and confirm any entitlement with the employer before incurring any expenditure. Pre-employment checks – all NHS employers are required to undertake pre-employment checks. The employer will confirm their local arrangements, which are expected to be in line with national guidance at http://www.nhsemployers.org/RecruitmentAndRetention/Employmentchecks/Pages/Employment-checks.aspx Professional registration – it will be a requirement of employment that you have professional registration with the GMC for the duration of your employment. Though the post is covered by NHS Indemnity, you are strongly advised to register with the MPS for professional indemnity. Health and Safety – all employers have a duty to protect their workers from harm. You should be advised by the employer of local policies and procedures intended to protect your health and safety and expected to comply with these. Disciplinary and grievance procedures – the employer will have local policies and procedures for dealing with any disciplinary concerns or grievances you may have. They should advise you how to access these, not later than eight weeks after commencement of employment. Educational Supervisor – the employer or a nominated deputy (usually the Director of Medical Education) will confirm your supervisor on commencement. General information on the Deanery’s management of Specialty Training programmes, including issues such as taking time out of programme and dealing with concerns or complaints, is available at www.oxforddeanery.nhs.uk and in the national ‘Gold guide’ to Specialty Training at http://www.mmc.nhs.uk 25/01/2013