N210 Control Lab/Clilnical Folder
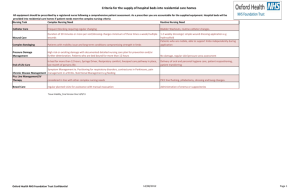
advertisement
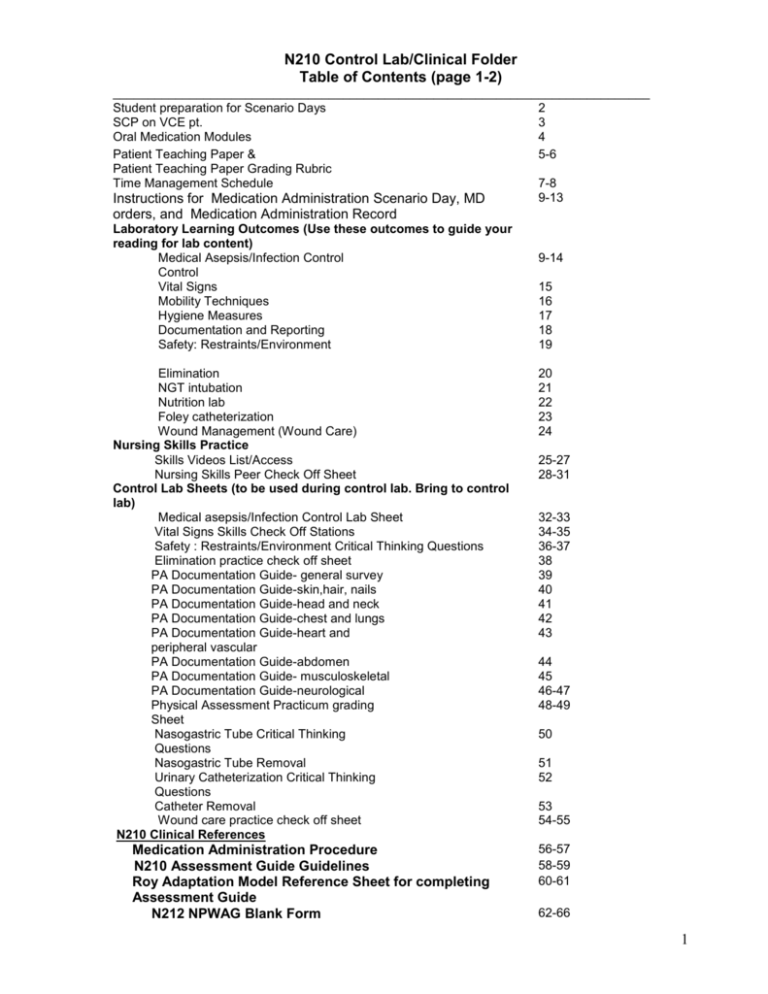
N210 Control Lab/Clinical Folder Table of Contents (page 1-2) _____________________________________________________________________________ Student preparation for Scenario Days 2 SCP on VCE pt. 3 Oral Medication Modules 4 Patient Teaching Paper & 5-6 Patient Teaching Paper Grading Rubric Time Management Schedule 7-8 9-13 Instructions for Medication Administration Scenario Day, MD orders, and Medication Administration Record Laboratory Learning Outcomes (Use these outcomes to guide your reading for lab content) Medical Asepsis/Infection Control Control Vital Signs Mobility Techniques Hygiene Measures Documentation and Reporting Safety: Restraints/Environment Elimination NGT intubation Nutrition lab Foley catheterization Wound Management (Wound Care) Nursing Skills Practice Skills Videos List/Access Nursing Skills Peer Check Off Sheet Control Lab Sheets (to be used during control lab. Bring to control lab) Medical asepsis/Infection Control Lab Sheet Vital Signs Skills Check Off Stations Safety : Restraints/Environment Critical Thinking Questions Elimination practice check off sheet PA Documentation Guide- general survey PA Documentation Guide-skin,hair, nails PA Documentation Guide-head and neck PA Documentation Guide-chest and lungs PA Documentation Guide-heart and peripheral vascular PA Documentation Guide-abdomen PA Documentation Guide- musculoskeletal PA Documentation Guide-neurological Physical Assessment Practicum grading Sheet Nasogastric Tube Critical Thinking Questions Nasogastric Tube Removal Urinary Catheterization Critical Thinking Questions Catheter Removal Wound care practice check off sheet N210 Clinical References Medication Administration Procedure N210 Assessment Guide Guidelines Roy Adaptation Model Reference Sheet for completing Assessment Guide N212 NPWAG Blank Form 9-14 15 16 17 18 19 20 21 22 23 24 25-27 28-31 32-33 34-35 36-37 38 39 40 41 42 43 44 45 46-47 48-49 50 51 52 53 54-55 56-57 58-59 60-61 62-66 1 Nursing Caremap Instructions Sample Caremap Template N212 Medication Sheet (for Non-Med Days) N212 Medication Sheet (for Scheduled Med Days) Sample Med Sheet for Non-Med Days N210 Clinical Course Evaluation Guidelines for Clinical Performance Evaluation Tool Approved abbreviations Unapproved abbreviations N210 Clinical Schedule Long TermCare Clinical Absence Make-up guidelines CPE Sheet ___________________________________________________________ 67 68 69 70 71 72-78 79-83 84-86 87 88-90 91 92-99 Student Preparation for Control Lab/Scenario Days in Skills Lab Review all previously taught skills Bring Taylor’s Fundamentals of Nursing textbook Wear complete uniform and name tag References for documentation (class notes, abbreviation list, pen, etc.) Personal Hygiene Measures Control Lab Day (Week 2 Wednesday) Bring: 2 towels, 2 washcloth sports bra and shorts (for females) 1 soap (bar or liquid) shorts for males (boxer or briefs 1 lotion to wear underneath patient plastic bag to hold your wet gowns are unacceptable) towels after lab Scenario Day #1 Bring: Shorts and tank top or sports bra Soap Lotion Toothbrush Toothpaste Stethoscope Washcloth and towel Patient gown Scenario Day #2 Bring: o Shorts and tank top or sports bra o Stethoscope o Isolation gown and mask o Patient gown 2 Cerritos N210 Medical Surgical Nursing Long Term/Acute Care Clinical Rotation STANDARD CLINICAL PREPARATION: Nursing Process Worksheet Preparation This activity will introduce you on how to navigate through the chart to gather patient information while filling out your Nursing Process Worksheet (NPW). You will need the following materials: DVD on Standard Clinical Preparation (access online via N210 TalonNet site) Virtual Clinical Excursion (VCE) DVD-Rom. Complete the VCE patient assigned to you by your instructor. TBA. A blank NPW form Instructions: 1. 2. Watch the v ideo on Standard Clinical Preparation. (You may check out from the library or watch online via TalonNet). 3. Take notes for your reference. 4. Using the VCE DVD-Rom, Go through the Virtual Clinical Excursion (VCE) and practice looking through a patient’s chart. Choose the assigned patient from the VCE e.g. Harry George, Piya Jordan and fill out a blank NPW form with the patient information. 5. Fill out the blank NPW as you go through the VCE chart (follow the steps as shown in the Standard Clinical Preparation). 6. Pay attention to “Course of Events in the hospital”. FILL OUT AND COMPLETE THE PATIENT PREPARATION THINKING TOOL ON PAGES ______ ON THIS CONTROL LAB FOLDER to assist you with the course of events in the hospital. You will need to summarize this in your NPW as shown in the Standard Clinical Preparation video. 7. Turn in the completed NPW including lab data (significant normal lab results and all abnormal lab results (NO NEED TO complete “Reason for Abnormal Values” portion) of the NPW) of your VCE patient to your instructor by week 1 (THURSDAY) of N212. 8. Practice with as many patients as you’d like. You may do this in pairs. Each student is required to turn in 1 complete NPW for a VCE patient. 3 Name_________________ Lab___________________ Cerritos College Nursing Department N212: Medical Surgical Nursing Oral Medication Module Instructions: Complete 2 “patient” medication preparation scenarios by the medication scenario day. You may work individually or in groups of two. You may complete as many scenarios as you wish, but only two are required. PLEASE DO NOT OPEN THE MEDICATION PACKAGES!!!!!!!!!! 1. Choose one patient. 2. Gather the MAR, physician’s order sheet and pull the medication drawer from the medication cart for the patient you have chosen. 3. Review the physician’s order sheet and the MAR and check for accuracy. Note any errors found. 4. Using your Mosby drug book, look up all of the medications ordered in preparation for administration (despite times ordered). 5. Note any errors found. 6. Note any information you would need to gather before administering the medication: why is this medication given (look at diagnosis and history), dosage and range, nursing considerations (ex: antihypertensive medication, check BP before administration) and common side effects (try to group side effects if possible (Ex: nausea/vomiting/diarrhea should be GI distress). Complete dosage calculation if needed. 7. Remove the medications from the medication drawer in preparation for administration (5 “rights”). Note any errors or concerns. 8. Review the steps for administration that you would complete at the patient’s bedside (5 “rights”) 9. Complete the documentation below 10. Review the errors/concerns found with the N47 faculty member or N47 student worker and have him/her sign below verifying completion. 11. Repeat the above steps for a second patient. Date Patient Name Faculty/Staff Signature *Submit this form (completed with faculty/staff signatures) on assigned DUE DATE to your clinical instructor. Failure to do so will result in an advisement note. 4 Patient Teaching Paper (Taylor Chapter 22) Each student will complete a Patient Teaching on an actual client that the student has cared for in this clinical rotation. Patient Teaching Paper will be a written essay of your patient teaching experience. It should be submitted with a minimum of 1 page and a maximum of 2 pages (typed and double spaced). You may include and submit brochures or handouts to enhance your teaching. Use different teaching strategies or tool to deliver effective patient teaching. Be creative! Patient Teaching Paper Guidelines Requirements: The Patient Teaching Paper should include the following: Read the chapter readings on Patient Teaching (Taylor, Ch 22 Teacher and Counselor) Patient Teaching Paper should be Nursing focused (i.e. teaching provided should be in the role of the Nurse, not physician, radiologist, dietician, pharmacist, etc.) 1. A complete NPW on the client including med sheets and assessment guide (do not include concept maps). 2. Please read Chapter 22 of Taylor and write a paragraph describing the client you taught which includes the following: a. A brief history of present illness (HPI) b. A description of client characteristics including details about any client variables/factors that may affect the teaching/learning experience. b. Identify the patient’s “learning need” (see Taylor Ch 22- the content that the patient needs to learn; patient’s learning style; developmental level, literacy level, language barrier if applicable c. Identify the client’s readiness to learn (discuss the patient’s physiologic and psychological readiness, willingness to make changes and participate, etc.) d. Identify any unique socioeconomic, cultural, and ethnic aspects (look at your client’s ethnic background and consider any cultural factors that may affect the client’s learning and/or health care practices. If identified, identify how you will tailor your patient teaching.) 3.What specific content taught based on the patient’s learning need? 4.Identify a specific “Patient Learning Outcome” for your patient (see page 480 Taylor). 5.What specific teaching strategies (e.g. demonstration, video, verbal, written or a combination) did you use in patient teaching appropriate for your patient and situation and state the rationale for choosing the specific strategy/ies. 6.Include an evaluation of your patient teaching. How did you evaluate the effectiveness of your teaching? State specific client behaviors that demonstrates the effectiveness or ineffectiveness of your patient teaching. If the teaching was ineffective, state the rationale and how you would approach the client for a more effective teaching. 7.Attach your client’s completed NPW and Assessment Guide to your paper (Required). Attach the Grading rubric when you submit this paper. 8.Include at least 2 references in the back of your paper. – must have at least 2 sources (e.g., Taylor, Iggy, credible internet sites, etc.) 5 Patient Teaching Paper Grading Criteria (Pass or Fail: 3/5 pts or greater= Pass) Grading Rubric : Patient Teaching Paper Student Name: ________________________________________ Clinical Instructor Name: 1 0.75 0.5 0.25 Content Accuracy All content throughout the paper is accurate. There are no factual errors. Information is shortened to simple phrases. Most of the content is accurate but there is one piece of information that might be inaccurate. Information is presented in long paragraphs. The content is generally accurate, but one piece of information is clearly flawed or inaccurate. Content is typically confusing or contains more than one factual error. There is little or no information. Creativity Student used several teaching strategies and showed considerable work/creativity and which made the patient teaching very effective Student used 1 teaching strategy that showed considerable work/creativity and which made the patient teaching effective. Student used 1 teaching strategy which made the patient teaching somewhat effective. Student used ineffective or inappropriate teaching strategy/ies that made the patient teaching ineffective. Relevance Student assessed the patient’s learning needs. The content taught to patient was relevant to patient’s learning needs and condition/situation. Student assessed patient’s learning needs. The content/s taught to patient was somewhat relevant to the patient’s learning needs. Some content/s included where unnecessary. Student did not assess the patient’s learning needs and taught on content that was lacking relevance to patient’s learning needs and situation. Student did not assess the patient’s learning needs. The content taught was not at all relevant to patient’s learning needs or situation. Clarity Content of patient teaching presented clearly in relation to patient’s ability to understand information Content of patient teaching presented somewhat clearly in relation to patient’s ability to understand information. Needs few clarifications. Content of patient Content presented teaching not presented confusing and needs clearly in relation to major clarifications. patient’s ability to understand information. Needs several clarifications. Thoroughness And Completeness Content is presented and explained completely. All areas of teaching paper #1,2,3, 4 &5 addressed thoroughly Content is presented and explained somewhat completely (Missing some areas (subcontent i.e., #1 a, b, c, d) of the teaching paper). Content presentation and explanation incomplete (Missing 1 major area (#1,2,3,4 &5) of the teaching paper). CATEGORY Lacking in Content presentation and explanation (Missing more than 1 major area (#1,2,3,4 &5) of the teaching project). This grading rubric serves only as a guide to evaluate if the paper earned a Pass or Fail. There are no points assigned to this assignment that will be included in the final course grades. Final grade will be rounded to the nearest whole number.** 6 Time Management Schedule Time management will be a key issue for you if you are to successfully transition to nursing school. Complete the two assignments listed below as tools to assist you in planning for this new adventure. Think about the connection between time management and prioritizing tasks. 1. Time Management Schedule Fill in the prototype weekly calendar. This is what you “plan” to do every week. (Not what you did last week). Hints: Begin by filling in all inflexible times (classes, work) Guide for study time: 2 hours of study per 1 hour of lecture and 1 hour of study per 1 hour of laboratory/clinic) Write in your place of study (home, library, skills lab) Use color or design if this helps you organize Remember to add: Sleep (particularly the night before clinical) Travel time (to and from school, work, childcare) Personal hygiene time Grocery shopping, cooking, eating Family responsibilities Family togetherness time Exercise “Don’t forget your spouse/significant other” time Relaxing time Telephone/internet 2. Mantra Mantra have been used throughout time, beginning in India many centuries ago, as a method of focusing the mind. Mantras are considered to have powerful effects on those who use them. Literally the word mantra means “the thought that liberates or protects”. Repeating a mantra can help you overcome fear, increase your creativity, give you energy when you are tired, and inspire you to keep going when you want to quit. Many of us are familiar with mantras but may not realize it. Our lives are filled with such mantras as “No pain, no gain”, or “The teacher is out to get me”, or “This is too hard, I might as well quit now” or “Practice, makes perfect”. In some spiritual traditions, mantras are given to students by their teachers. However, it is possible to make up your own mantra and use it as an antidote to other negative mantras you may already be using. Design a mantra for your personal use in nursing school. This mantra will be a simple phrase that you will recite over and over. Be creative and have some fun. Be inspired. 7 Time Management Schedule and Mantra Student Name__________________Lab Group_______________________ Time 04 05 06 07 Monday Tuesday Wednesday Thursday Friday Saturday Sunday Study: Work: Sleep: Study: Work: Sleep: Study: Work: Sleep: Study: Work: Sleep: Study: Work: Sleep: Study: Work: Sleep: Study: Work: Sleep: 08 09 10 11 12 1 2 3 4 5 6 7 8 9 10 11 12 01 02 03 Add up Hours Mantra: __________________________________________________ 8 Instructions for Medication Administration Scenario 1. Research all the necessary information to be prepared to administer the medications during the Med Administration scenario day. 2. In preparation for Medication Administration Scenarios, you must complete the following: a. complete your N210 Medication Sheet (For Scheduled Med Days) for all the medications listed in the MD orders and Medication Administration Record following this instruction page. **You must have looked up all the medications listed in the MD orders and MARs. b. Watch the following Taylor Videos from www.ThePoint.lww.com (log in as a new user or return user) and complete Skills Video notes (will be checked by instructor) Ch. 29 : Medications, Watch and Learn: Medications: 3 Checks and Rights of Medication Administration Ch. 29 : Medications, Watch and Learn: Medications: Preparing Unit-Dose Packaged Medications 3. Review Medication Administration chapter readings (Ch. 29) and lecture. 4. Bring your skills video notes and completed N210 Medication Sheet (For Scheduled Med Days), MAR, and MD orders, and the “Medication Administration Procedure” from this packet to the Medication Administration Scenario Day. ******Guidelines for Administration (See Taylor textbook)****** Oral meds: • NEVER crush sustained release, controlled release or enteric-coated pills. • Capsules can not be split • Scored tabs can be split in half • Place into plastic/paper administration cup without touching the med. • May use pudding or applesauce for patient’s with difficulty swallowing • Stay with patient until all medications are taken. Never leave meds at bedside. Topical meds: • Make sure previous dose is removed, before applying new dose. • Apply patches to non-hairy areas of the body • Take care not to touch topical medications with ungloved hands 9 Enteral tube administration: • Use liquid form if possible • Crush pills individually and mix with 20-30 mL of warm water. • If medication should be given on empty stomach-stop feeding for 2030 minutes before and after med administration • √ Placement, Flush with water, administer medication, flush with water, administer medication, flush with water 10 Health Occupations Skills Lab Physician’s Orders Date Time Complete top portion with each Level of Care change. Indicate order with a Check Mark. Outpatient Procedure for Place in Outpatient Observation Services for yesterday 1400 Admit as Inpatient for R/O gangrene Physician Signature Date yesterday Time 1400 Additional Orders: (Dates/Times required) 20. Accucheck ACHS 21. Humulin N 20 units SQ q am and 20 units SQ q pm 22. Sliding Scale with Regular insulin as follows: If BS level: Give: 150-200 2 units 201-250 4 units 251-300 6 units 301-350 8 units 351-400 10 units and And call MD. Allergies & Sensitivities Patient Name: Ibuprofen Medical Record: Grumpy Weight Height Diagnosis 110 lbs 3’3” R/O PNA vs. CHF, fracture left humerus 0000003 Bed Number: SL123 11 Health Occupations Skills Lab MAR MAR TODAY Date Site Codes: 1. Right Abdomen 3. Right Upper Arm 7. Right Anterior Thigh 2. Left Abdomen 4. Left Upper Arm Drug Name, Strength, Dosage Start Stop Time Period (upper outer quadrant) 8. Left Anterior Thigh Form Time Time Dose Rate Route Schedule Demerol 75 mg IM q4 hours prn pain Vistaril 25 mg IM q4hours prn pain. Give with Demerol. Date Date today discharge today discharge Claforan IV 1 g Q 12 hours today discharge Tylenol 650 mg PO q4 hours prn temperature > 101.0 today discharge Albuterol nebulizer 1 unit dose/0.5 mL NS q6h today Proventil nebulizer 1 unit dose/0.5 mL NS q6h Page 1 of 1 5. Right Buttock (upper outer quadrant) 0700To1459 Time/Init./Site Time Period 1500 To 2259 Time/Init./Site 0800 2000 discharge 0600 1200 1800 today discharge 0600 1200 Digoxin 0.125 mg PO QD today discharge 1000 Lasix 20 mg PO QD today discharge 1000 Colace 100 mg PO BID today discharge 1000 2200 Motrin 600 mg PO TID today discharge 1000 1400 2000 Ultram 100 mg PO BID today discharge 1000 2200 Neurontin 300 mg PO BID today discharge 1000 2200 D5 0.45% NS at 75 mL/hr today discharge Zestril 10 mg PO QD. Hold if SBP <100 today discharge 1000 Xarelto 20 mg PO daily today discharge 1000 Humulin N 20 units SQ q am and 20 units SQ q pm today discharge 0730 Signature Initials Signature Patient Name Patient No. Grumpy 0000003 Room Age SL 123 56 Diagnosis Pt. Weight 6. Left Buttock Time Period 2300 To 0659 Time/Init./Site 0000 1800 0000 1730 Initials Signature Initials Allergies: Ibuprofen Pt. Height 3’3” 110 lbs R/O PNA vs CHF exac., fracture L humerus Physician’s Name Dr.Suess 24 Hour MAR 12 Health Occupations Skills Lab MAR MAR TODAY Date Site Codes: 1. Right Abdomen 3. Right Upper Arm 7. Right Anterior Thigh 2. Left Abdomen 4. Left Upper Arm Drug Name, Strength, Start Stop (upper outer quadrant) 8. Left Anterior Thigh Time Period Dosage Form Time Time Dose Rate Route Schedule Date Date Accucheck ACHS today discharge Sliding Scale with Regular insulin as follows: today discharge If BS level: Give: 150-200 2 units 201-250 4 units 251-300 6 units 301-350 8 units 351-401 10 units and And call MD. Signature Initials Signature Patient Name Patient No. Grumpy 0000003 Room Age SL 123 56 Diagnosis Pt. Weight 0700To1459 Time/Init./Site 0600 1200 Initials 1 Page 1 of 5. Right Buttock (upper outer quadrant) Time Period 1500 To 2259 Time/Init./Site 6. Left Buttock Time Period 2300 To 0659 Time/Init./Site 1800 2100 Signature Initials 24 Hour MAR Pt. Height 3’3” 110 lbs R/O PNA vs CHF exac., fracture L humerus Allergies NKA Physician’s Name Dr. Suess 13 Laboratory Learning Outcomes: Medical Asepsis/Infection Control (Ch. 27) After studying this content, you should be able to: 1. Describe and demonstrate correct hand washing techniques. 2. List all possible situations when hand washing should be performed. 3. Discuss the use of alcohol based antibacterial hand gels. 4. State the personal hygiene guidelines related to hair, fingernails and jewelry. 5. Describe and draw the six steps in the chain of infection 6. List and describe conditions that predispose clients to infection 7. Describe what is meant by the term nosocomial infection (now known as hospital acquired infection) and discuss one intervention that will help prevent it 8. List the major organisms responsible for nosocomial infections 9. Define the term surgical asepsis and medical asepsis 10. Implement recommended techniques for medical and surgical asepsis. 11. Describe how and when personal protective equipment should be used. 12. Demonstrate and outline the steps in donning and removing personal protective equipment according to the Centers for Disease Control 13. Describe the strategies for implementing the CDC guidelines for standard and transmission based precautions. 14. Discuss the purpose of neutropenic precautions/ isolation and the measures that should be followed with this type of isolation. 15. Discuss multidrug resistant organisms and nursing implications 16. List interventions that might be used to meet psychological needs of a patient in isolation. 17. Describe the contents and care of an isolation room. Skills: Application and Removal of personal protective equipment Demonstrate proper hand hygiene techniques Demonstrate proper application and removal of sterile gloves and nonsterile gloves 14 Laboratory Learning Outcomes: Vital Signs (Ch. 24) After studying this content, you should be able to: 1. Define the terminology relating to vital signs 2. Explain physiologic processes involved in homeostatic regulation of temperature, pulse, respirations, and blood pressure. 3. Compare and contrast factors that increase or decrease body temperature, pulse, respirations, and blood pressure. 4. Identify sites for assessing temperature, pulse, and blood pressure. 5. Discuss the steps to accurately obtaining temperature, pulse, respirations, and blood pressure. 6. Discuss the factors that contribute to false readings for blood, pressure. 7. Discuss the normal ranges for body temperature, pulse, respirations, and blood pressure. 8. Demonstrate documentation of vital signs. 9. Discuss the steps to obtaining an orthostatic blood pressure and pulse as well as their indications. Skills: blood pressure, orthostatic blood pressure, radial pulse, apical pulse, respirations and oral temperature, pulse oximetry 15 Laboratory Learning Outcomes: Mobility Techniques (Ch. 33,34) After studying this content, you should be able to: 1. State nursing guidelines and rationale for use of proper body mechanics. 2. Identify variables that influence body alignment. 3. Describe common patient positions. 4. Demonstrate supine, lateral and Fowler’s positions. 5. Discuss positioning and protective devices and indications for use. 6. List nursing guidelines and rationales for patient transfer and ambulation. 7. Demonstrate patient transfer using a gait belt: bed to wheelchair and wheelchair to bed. 8. Describe the effects of exercise and immobility on major body systems 9. Assess body alignment, mobility, and activity tolerance, using appropriate interview questions and physical assessment skills. 10. Relate nursing guidelines and rationales for performing range of motion exercises. 11. Demonstrate appropriate range of motion exercises to all body joints. 12. Document range of motion procedure. 13. Compare comfort, rest and sleep. 14. Relate spiritual needs to comfort. 15. Differentiate between NREM and REM sleep. 16. State the relationship of age to sleep requirements. 17. Examine sleep promoting and sleep suppressing factors. 18. Review drugs that affect sleep. Skills: transfer patient from bed to wheelchair and from wheelchair to bed with and without a gait belt, perform passive range of motion on all joints, positioning of a patient in bed, moving a patient up in bed, ambulating a patient with and without a gait belt 16 Laboratory Learning Outcomes: Hygiene Measures (Ch. 31) After studying this content, you should be able to: 1. Discuss the characteristics of healthy skin, mucous membranes, nails, hair and teeth. 2. List nursing guidelines for bathing patients. 3. Demonstrate techniques for assisting patients with hygiene measures, including those used when administering different types of baths and those used when cleaning each part of the body. 4. State the types of therapeutic baths and the purpose for each. 5. Describe interventions for care of patient’s teeth and mouth (including dentures and bridges), eyes, ears, nose, fingernails, feet, toenails and hair. 6. Describe how to shave male patients and list any nursing precautions. 7. 8. List medical asepsis guidelines related to handling of linen and the disposition of contaminated articles. Skills: hand hygiene, non-sterile gloving, bed bath, making occupied bed 17 Laboratory Learning Outcomes: Documentation and Reporting (Ch. 17) After studying this content, you should be able to: 1. State at least 4 uses of documentation in a medical record and recognize when documentation is used inappropriately. 2. Define and apply the following types of nurse’s notes documentation (narrative, SOAPIE, Focus [DAR], PIE, and charting by exception) 3. Discuss the pros and cons of using flowsheets for documentation. 4. Name the components and use of a nursing care plan. 5. Discuss the pros/cons of computerized charting 6. Apply the “Golden Rules” of documentation 7. Recognize and utilize medical abbreviations, both approved and from the “Do Not Use” list. 8. Convert traditional time to military time 18 Laboratory Learning Outcomes: Safety/ Restraints/ Environment (Ch. 26) After studying this content, you should be able to: Restraints 1. 2. 3. 4. 5. 6. 7. 8. Outline strategies to provide a safe patient environment Identify clients who are at high risk of falls Discuss the benefits and risks of using physical restraints Explain the basis for enacting restraint legislation and National Patient Safety Goals (NPSG) standards. Demonstrate proper application of restraints Discuss nursing responsibilities related to use of restraints Differentiate between a restraint and a restraint alternative List 5 restraint alternatives Skills: Apply vest and wrist restraint to patient in bed, and application of vest to patient in wheelchair. 19 Laboratory Learning Outcomes: Elimination (Ch. 37,38) After studying this content, you should be able to: Urinary Elimination 1. Describe the physiology of the urinary system. 2. Identify variables that influence urination. 3. Describe how the nurse would assist the patient with toileting, use of a bedpan, a urinal, bedside commode and a condom catheter. 4. Describe the care and management of an indwelling catheter and external urinary catheter. 5. State the rationale for measuring and recording the patient’s urinary output. 6. Discuss the use of a “hat” in a commode and graduated cylinder to measure urine output. 7. Describe the process of emptying a foley catheter drainage bag. 8. Describe how the collection of the following urine specimens are obtained and give the reasons for why they are collected: A. Midstream B. 24 hour D. Indwelling catheter. Bowel Elimination 1. 2. 3. 4. Review normal anatomy and physiology related to elimination. Describe the characteristics of normal bowel elimination and stool. Identify nursing interventions for patients with diarrhea or constipation. Discuss the steps for the following procedures: removing fecal impaction; rectal suppository, administering a large volume enema; administering a small volume enema. 5. Identify nursing interventions if signs and symptoms of vagal response occurs 6. Describe how stool specimens are collected and give the various reasons why they are collected. Skills: Enema Administration, applying a condom catheter, emptying a Foley drainage bag, placing a patient on a bedpan/fracture pan, assisting a patient with use of a urinal, emptying a BSC, providing pericare and foley catheter care, obtaining a specimen from an indwelling foley catheter, changing a incontinence brief 20 Laboratory Learning Outcomes: Nasogastric Intubation (Ch. 36) After studying this content, you should be able to: 1. Discuss reasons for nasogastric intubation 2. Describe the process of nasogastric tube insertion and removal including equipment needed. 3. Describe various methods to check placement of a nasogastric tube. 4. Discuss nursing interventions related to promoting patient comfort and maintaining a nasogastric tube. 5. Compare and contrast the Salem sump and Levin gastric tubes 6. Discuss nursing management of the NGT attached to suction 7. Identify the purpose of NGT to suction. 8. Discuss the steps to discontinuing an nasogastric tube Skills: Insertion and removal of a nasogastric tube; attaching NGT to suction; discontinuing an NGT 21 Laboratory Learning Objectives : Nutrition Lab (Nix Chapter readings) After studying this content, you should be able to: 1. Discuss the assessment of a patient’s normal nutritional status. 2. Discuss cultural influences related to meeting nutritional needs. 3. Describe how to feed a patient with special needs. 4. Describe commonly ordered therapeutic diets. 5. Demonstrate meal percentage and oral fluid intake measurement and record. 6. List interventions to assist the patient who is on restricted fluids. 7. Discuss reasons for nasogastric and gastric intubation 8. Describe the process of administering a continuous and intermittent nasogastric and gastrostomy tube feeding. 9. Demonstrate the process of administering a water bolus via an NGT or gastrostomy feeding tube. 10. Discuss how nasogastric and gastrostomy feedings are measured and recorded. 11. Compare the risks and benefits of gastric feeding versus total parenteral nutrition. Skill: Administering intermittent and continuous tube feeding; Administering a water flush of an NGT/G tube.; How to measure and document percentages of food tray consumed, and measuring fluid intake. 22 Laboratory Learning Outcomes: Foley Catheterization (Ch. 37) After studying this content, you should be able to: 1. Demonstrate the insertion of a Foley catheter using sterile technique 2. Explain the procedure for removal of an indwelling catheter 3. Discuss patient teaching related to maintaining a foley catheter. 4. Discuss the patient teaching related to post foley catheter removal. 5. Identify unexpected outcomes that may occur during foley catheter insertion and recommended nursing interventions. Skill: Insertion and removal of an indwelling urinary catheter 23 Laboratory Learning Outcomes: Wound Care (Ch. 32) After studying this content, you should be able to: 1. Identify the three stages of wound healing 2. Discuss the difference between primary, secondary and tertiary intention wound healing. 3. List the factors that can affect wound healing to include nutrition, medications, and health status. 4. Identify the signs and symptoms of a wound infection. 5. Identify the solutions used for wound irrigation and rationale for use. 6. Describe various types of wound drainage. 7. Describe the different types of wound treatments: e.g. transparent, hydrocolloid, wound vac, hydrogel, calcium alginate and foams. 8. Discuss the indication for use of transparent and hydrocolloid wound dressings. 9. Discuss the wound closure devices: staples, sutures, retention sutures steristrips, dermabond and Montgomery straps, wound-vac. 10. Identify and discuss the mechanism of action of the following wound drainage devices: penrose, Jackson-Pratt and hemovac . 11. State the guidelines for maintaining a sterile field 12. Describe the steps (and rationale for each step) for performing a sterile wet to moist dressing. 13. Demonstrate a wet to moist sterile dressing change. Bandages and Binders 1. State the purposes of bandages and binders. 2. Discuss the general guidelines for application and removal of bandages and binders. 3. Demonstrate application of the following: A. An abdominal binder B. An ace bandage using the spiral turn, recurrent, and figure of eight turn Thermal Therapy 1. List the common uses for both heat and cold as therapeutic modalities. 2. Describe techniques and related nursing responsibilities for heat and cold applications. Skills: wet to moist sterile dressing change 24 Taylor & TalonNet SKILLS VIDEOS You are required to view the following skills demonstrations online (from any internet access computer or the skills lab computers in SL 121, 122, 123, 110) prior to assigned control lab days at The Point (Taylor website access to stuent Wath & Learn Videos) and http://talonnet.cerritos.edu/osp-portal (TalonNet) TheTalonNet videos were developed as an instructional aide by your instructors for beginning nursing students. Enter username (7 digit student ID number) and password (6 digit birthdate) Click on My Projects (top menu bar) Click on My Video Links Click on Nursing Skills Videos; click “I Agree” on the copyright; Choose your video links according to assigned labs and view the videos (click on broadband if you have high speed internet; click on 56K if you have dialup internet) Content Name of Skills Medical Asepsis Nonsterile Gloving GlovingNSterile Sterile Gloving GlovingSterile Vital Signs Taylor Watch and Learn Video (Use access code on inside cover of Taylor textbook to access videos) Hand hygiene Ch. 27 Asepsis & Infection Control, Watch & Learn: Asepsis, Performing Hand Hygiene Vital signs Ch 24: Vital Signs, Watch and Learn: Measuring oral Temp, Radial pulse, resp rate and blood pressure Ch 24: Vital Signs, Watch and Learn: Measuring an apical pulse TalonNet Video Link VitalSigns ApicalPulse PulseOximetry RectalTemp TymAxTemp 25 Content Name of Skills Taylor Watch and Learn Video (Use access code on inside cover of Taylor textbook to access videos) TalonNet Video Link Activity and Rest Ambulating a patient AmbPatient Bed Mechanics BedMech Moving a Patient up in bed MovingPatient PassiveRange ROM exercises PositionPatient Positioning a Patient TransPatient Transferring a Patient Personal Hygiene Measures See TalonNet Video OR See Taylor Videos Ch: 31: Hygiene, Watch and Learn: Giving a Bedbath No video required prior to lab Assessment Lab2 No video required prior to lab Assessment Lab3 No video required prior to lab B/B/Teds/Restraints/Thermal Bandages and Therm Binders/Teds/Restraints /Thermal Therapy Bed_Bath (includes occupied bed change) Assessment Lab1 Elimination Enema Collecting a Urine Specimen Bandages (view only applying bandages and restraints; NOT binders and NOT Teds) Ch. 37: Bowel Elimination: Enema Watch & Learn: Administering a Cleansing UrineSpecimen Enema Ch. 37: Bowel Elimination: Watch & Learn: Urinary 26 Elimination: Applying a Condom catheter Scenarios Review previously learned skills videos NGT Insertion VS Competency Testing Review Vital Signs videos Scenarios Review all previously learned skills videos Nutrition Lab Foley Catheterization Wound Care Foley Catheter Wound Care See Taylor Video-Ch. 36: Nutrition, Watch and Learn: Inserting a Nasogastric tube NGTube Ch. 36: Nutrition: Watch & Learn: Nutrition: Administering a continuous tube feeding: Using a feeding pump and a prefilled closed tube feeding set-up Ch. 37 Urinary Elimination: Watch & Learn: Urinary Elimination: Catheterizing a male urinary bladder ONLY: Indwelling and Intermittent catheters. Live demo in control lab Catheter draping Catheter (watch the female urinary catheterization ONLY) WoundCare 27 N210 Fundamentals of Nursing Nursing Skills Peer Check Off Following independent practice, demonstrate proper technique of the following nursing skills to your classmates three (3) separate times. Obtain peer signatures/dates indicating that you have demonstrated proper technique in performing the skills. If you need help, please refer to the videos online, your skills book, and/or see a skills lab instructor during open lab. This sheet is to be completed prior to Skills CPE and submitted to clinical instructor on Skills CPE testing day (week 8). Any student who fails to turn in a completed sheet to the instructor will receive an advisement note and will not be allowed to test for CPE. Arrangements will be made with the instructor to test for CPE on a different day. If a student fails the CPE, a skills lab referral will be given for the failed skill and the student is to complete the Skills Lab referral within 1 week of the referral date. 28 Nursing Skills Peer Check Off Student___________________________ Clinical Instructor_____________________ Skill Bed Bath And Occupied Bed Making Peer Name (PRINT) 1. _______________ 2. _______________ 3. _______________ Signature 1. _____________ 2. _____________ 3. _____________ Handwashing 1. _______________ 2. _______________ 3. _______________ 1. _____________ 2. _____________ 3. _____________ Sterile And Nonsterile Gloving 1. _______________ 2. _______________ 3. _______________ 1. _____________ 2. _____________ 3. _____________ Denture Care 1. _______________ 2. _______________ 3. _______________ 1. _____________ 2. _____________ 3. _____________ Applying And Removing PPE 1. _______________ 2. _______________ 3. _______________ 1. _____________ 2. _____________ 3. _____________ Taking Full Set Of Vital Signs Temp (Oral, Ax, Tymp, Rectal); Pulse (Radial and AP), Resp, BP 1. _______________ 2. _______________ 3. _______________ 1. _____________ 2. _____________ 3. _____________ Patient Transfer From Bed To Chair 1. _______________ 2. _______________ 3. _______________ 1. _____________ 2. _____________ 3. _____________ Positioning A Patient In Bed 1. _______________ 1. _____________ Date 1. _______ 2. _______ 3. _______ 1. _______ 2. _______ 3. _______ 1. _______ 2. _______ 3. _______ 1. _______ 2. _______ 3. _______ 1. _______ 2. _______ 3. _______ 1. _______ 2. _______ 3. _______ 1. _______ 2. _______ 3. _______ 1. 29 2. _______________ 3. _______________ 2. _____________ 3. _____________ Ambulating A Patient 1. _______________ 2. _______________ 3. _______________ 1. _____________ 2. _____________ 3. _____________ Applying Bandages, Binders, Restraints, Anti-Embolism Stockings, Thermal Therapy 1. _______________ 2. _______________ 3. _______________ 1. _____________ 2. _____________ 3. _____________ Enema Administration 1. _______________ 2. _______________ 3. _______________ 1. _____________ 2. _____________ 3. _____________ Collecting Urine Specimen From A Urinary Catheter 1. _______________ 2. _______________ 3. _______________ 1. _____________ 2. _____________ 3. _____________ Sterile Wet-Moist Dressing Change 1. _______________ 2. _______________ 3. _______________ 1. _____________ 2. _____________ 3. _____________ Urinary Catheterization (Male & Female) Requires 2 peer and 1 Skills Lab Personnel (instructor or student worker) signature Nasogastric Tube Insertion 1. _______________ 2. _______________ 1. _____________ 2. _____________ 3. _______________ 3. _____________ 1. _______________ 2. _______________ 3. _______________ 1. _____________ 2. _____________ 3. _____________ Water Bolus Via 1. _______________ 1. _____________ _______ 2. _______ 3. _______ 1. _______ 2. _______ 3. _______ 1. _______ 2. _______ 3. _______ 1. _______ 2. _______ 3. _______ 1. _______ 2. _______ 3. _______ 1. _______ 2. _______ 3. _______ 1. _______ 2. _______ 3. _______ 1. _______ 2. _______ 3. _______ 1. 30 Nasogastric Tube 2. _______________ 3. _______________ 2. _____________ 3. _____________ Moving A Patient Up In Bed 1. _______________ 2. _______________ 3. _______________ 1. _____________ 2. _____________ 3. _____________ Range of Motion Exercises 1. _______________ 2. _______________ 3. _______________ 1. _____________ 2. _____________ 3. _____________ _______ 2. _______ 3. _______ 1. _______ 2. _______ 3. _______ 1. _______ 2. _______ 3. _______ REMINDER: This sheet is to be completed prior to Skills CPE and submitted to clinical instructor on Skills CPE testing day (week 8). Any student who fails to turn in a completed sheet to the instructor will receive an advisement note and will not be allowed to test for CPE. Arrangements will be made with the instructor to test for CPE on a different day. If a student fails the CPE, a skills lab referral will be given for the failed skill and the student is to complete the Skills Lab referral within 1 week of the referral date. 31 Infection Control Control Lab Sheet Chain of Infection 1. Discuss the chains of infection (reservoir, portal of entry, mode of transmission, etc.) then give examples that apply to each chain (e.g. mode of transmission = direct contact, droplet). See Chain of Infection Illustration. 2. Scenarios A. Scenario 1: The spread of Infection An elderly patient, hospitalized with a gastrointestinal disorder, was on bedrest and required assistance for activities of daily living. The patient had frequent uncontrolled diarrhea stools and the nurse provided excellent care to maintain cleanliness and comfort. While cleaning the patient, the soiled linens touched the nurse’s uniform. The nurse placed the soiled linens on a chair and left the room. Following 1 episode of cleaning the patient and changing the bed linen, the nurse immediately went to a second patient to provide am care and assist with the morning meal. The nurse’s hands were not washed prior to assisting the second patient. 2 days later, the second patient developed diarrhea. His stool cultures showed positive for Vancomycin Resistant Enteroccocus (VRE). Let’s examine the chain of infection as it applies to this situation Question#1 What is the: Susceptible host Infectious agent Portal of entry Mode of transmission Reservoir Portal of exit Answer Question #2 Answer Break the Chain of Infection… What should the nurse do to prevent the spread of infection? Which PPE should be worn? 32 B. Scenario 2: The Nurse Breaks the Chain A patient assigned for morning care has an open wound on her left lower leg. The wound is draining and when last cultured, the microorganism MRSA was identified. In preparation for bed making, the hands of the nurses were washed. Clean linen and a bag for soiled linen were gathered from the linen room and placed on the patient’s clean bedside stand. To remove the soiled linen from the bed, the following procedure was followed: Hands washed Gloves worn Each side of the soiled linen ends folded towards the middle of bed Soiled linen held away from the nurses’ uniform Soiled linen placed in the linen bag for later discard Protective gloves removed Hands washed Let’s examine the chain of infection as it applies to this situation Question#1 What is the: Infectious agent Reservoir Portal of exit Question #2 a. How did the nurse break the chain of infection? b. Which chains where broken? c. Which PPE should be worn? Answer Answer 33 N210 Fundamentals of Nursing Vital Signs Skills Check Off Stations Lab Groups Lab A & B Lab C & D Lab E & F Room Assignment SL 105 SL 122 SL 123 ACTIVITY Check when completed Temperature Practice taking temperature on another student: Oral axillary tympanic Practice taking temperature on a manikin: rectal (using manikin) __________ Set of Vital Signs Take a full set of vital signs (temp., pulse & respirations, apical pulse, blood pressure) on 3 clients & document on the graphic sheet Vital Signs Manikin Apical Pulse Listen to apical pulse on manikin. Identify the rhythm and write on the back of this sheet. Orthostatic Vital Signs Practice taking orthostatic vital signs on another student Answer orthostatic vital signs questions on the poster. Use the back of this sheet. VS Special Considerations (SL 121) Assess the client and answer Measuring Blood Pressure questions on the poster. Use the back of this sheet. Complete this sheet by the end of week 2. 34 Vital Signs Questions Apical Pulse Identify the rhythm on the VS manikin. ______________ Orthostatic Vital Signs 1. How would you take orthostatic VS on a patient? 2. How would you take orthostatic VS on a patient who is dehydrated and is experiencing some dizziness upon rising from a lying position? Measuring Blood Pressure (VS Special Considerations) 1. You are caring for a post left-mastectomy patient. Where would you take the patient’s blood pressure? 2. You received report from the previous shift’s nurse that your patient has an atrio-venous graft (AV dialysis graft) on her right arm. Where would you take the patient’s blood pressure? 35 N210: Fundamentals of Nursing Safety: Restraints/ Environment Critical Thinking Questions 1. Discuss the components of an environmental assessment. 2. Perform and verbalize an environmental assessment on your assigned patient. 3. How often does the physician’s order need to be renewed for a client on restraints? 4. When initiating restraints without a physician’s order, what is the time frame in which the physician’s order needs to be signed? 5. How often do you release restraints on a client? 6. What are your nursing responsibilities when releasing a client from restraints? 7. What would you need to monitor on a client who is on restraints and how often would you do this? 8. How often should the need for continuation or termination of restraint use be determined? 9. What would you need to assess after applying an abdominal binder on a client? 10. What would you need to assess after applying anti-embolism stockings? 11. What are restraint alternatives? Give examples of these. 12. How would you prevent thermal injury on a client using a heating pad or hot compress? 36 N210: Fundamentals of Nursing Safety: Restraints/ Environment Scenario: As you enter your female client’s room, you find her with one leg over the side rail, making attempts to get out of bed unassisted. Your client is an 82-yearold female with a history of congestive heart failure (CHF). When you question what she is doing, she tells you, “I need to go to the bathroom.” She also tells you she is sure her dog needs to be let out because she hasn’t been able to get out of bed all morning. This is your second day caring for your client. Your initial assessment on admission 2 days ago included her being oriented to person, place, time, and purpose. The night shift did report off saying she was disoriented all night. 1. What is your first nursing action? Provide rationale for your response. 2. What additional priority nursing actions are justified for your client? 3. What additional information do you need to gather to determine the next step in her plan of care? 4. If it is determined that your client needs to be closely monitored for possible falls, what interventions, by priority, will you implement? 5. Identify the legal requirements that must be implemented when a client is placed on restraints. (Read the procedure, Managing a client of restraints) 6. What documentation must be provided when a client is placed on restraints? 37 N210: Fundamentals of Nursing Elimination Practice Station Check-off Station 1 Emptying Foley catheter bag______________________________ Specimen from foley catheter______________________________ Station 2 Assisting with urinal _____________________________________ Place a fellow student on a bedpan_________________________ Changing a brief________________________________________ Station 3 Enema Administration___________________________________ Station 4 Pericare on female manikin_________________________________ Emptying a BSC__________________________________________ Foley catheter care________________________________________ Station 5 (self station) Condom catheter________________________________________ 38 Physical Assessment Documentation Guide Student____________________________ Date ________________ Client/Patient Initials________Age ________Sex__________ General State of Health Subjective Data: (Obtain all info under “General State of Health” from Review of Systems page 5 of Jarvis) Objective Data: Appearance Posture (relaxed, erect, tripod position, slumped, leaning to one side) Overall hygiene and grooming (clean, well groomed, unkempt) Any apparent signs of distress Dress (appropriately for situation) Behavior Level of consciousness (awake, asleep, lethargic, comatose) Mood and affect/ Facial expressions (appropriate for situation) Cognition Orientation (person, place, time, and purpose-X4) Speech (clear, garbled, slurred, incomprehensible) Responsiveness (follows directions and responds appropriately) Documentations: (Include both Subjective and Objective Data in Narrative Form) 39 Physical Assessment Documentation Guide Student____________________________ Date ________________ Client/Patient Initials________Age ________Sex__________ Assessment of the Skin, Hair, and Nails Subjective Data: (Obtain all info under “Skin”, “Hair”, & “Nails” from Review of Systems page 5 Jarvis) Objective Data: Inspection and palpation of the skin Color(pink, cyanotic, jaundiced, erythematous), Pigmentation (even, hyper/hypopigmentation) Lesions (Describe 3) Description – size & color Structure - type of lesion (macule, papule, nodule etc.) Anatomical Distribution Hydration – skin turgor (immediate recoil, tenting) Temperature & Moisture (warm/dry, cool/clammy) Inspection and palpation of the hair Color & condition Quantity, distribution, & texture (abundant; balding/receding vs. bald patches, smooth or course) Inspection and palpation of the fingernails Color of nail bed Firmness, texture, ridging, or irregularities Clubbing: Palpate for firm nail matrix Estimate nail angle (160 degrees or less; >160 degrees) Documentation: (Include both Subjective and Objective Data in Narrative Form) 40 Physical Assessment Documentation Guide Student____________________________ Date ________________ Client/Patient Initials________Age ________Sex__________ Assessment of the Head and Neck Subjective Data: (Obtain all info under “Head, Eyes, Ears, Nose, Mouth and Neck” from Review of Systems page 5-6 Jarvis) Objective Data: Inspection and palpation of the head and face Skull for symmetry & tenderness Face (includes eyes, ears, nose, mouth, and neck) Symmetry Discoloration Lesions Drainage Distention of neck Oral mucous membranes –color, hydration(dry/moist), lesions Documentation: (Include both Subjective and Objective Data in Narrative Form) 41 Physical Assessment Documentation Guide Student____________________________ Date ________________ Client/Patient Initials________Age ________Sex__________ Assessment of the Chest and Lungs Subjective Data: (Obtain all info under Respiratory from Review of Systems in Jarvis page 6) Objective Data Inspect chest wall Color, Configuration (symmetry) and Lesions Movement Respiratory rate, depth, and effort Auscultate systematically for quality of lung sounds Assessment of lung sounds and location (Clear, diminished, absent) Identify adventitious sounds if present: Wheezes (sibilant or sonorous rhonchi) Crackles (fine or course) Documentation: (Include both Subjective and Objective Data in Narrative Form) 42 Physical Assessment Documentation Guide Student____________________________ Date ________________ Client/Patient Initials________Age ________Sex__________ Assessment of the Heart and Peripheral Vascular System Subjective Data: (Obtain all info under Cardiovascular, Peripheral Vascular from Review of Systems page 6 Jarvis) Objective Data HEART Inspection Pulsations, lifts, heave JVD with chest at 35-45 degree angle Auscultation Rhythm assessment of S1 and S2 (Regular/Irregular) Assess all auscultatory sites: APETM Count Apical Heart Rate PERIPHERAL VASCULAR SYSTEM Palpation of Peripheral Pulses Radial Femoral Posterior Tibial Dorsalis Pedis Skin color – extremities (upper and lower) Capillary refill after blanching (secs) Fingers/toes Presence of Edema- depress for 5 seconds (grade if pitting) **Practice the following skills: Use of Doppler; applying antiembolism stockings; applying Sequential compression Device** Documentation: (Include both Subjective and Objective Data in Narrative Form) 43 Physical Assessment Documentation Guide Student____________________________ Date ________________ Client/Patient Initials________Age ________Sex__________ Assessment of the Abdomen Subjective Data: (Obtain all info under Gastronintestinal, Genitourinary from Review of Systems page 6-7 Jarvis) Objective Data Inspection Contour Lesions Scars Distention Pulsations Hernia (while patient lifts head) Auscultation (all quadrants) Bowel sounds Palpation Light palpation Tension of abdominal wall (soft, firm, hard) Tenderness Masses Deep palpation Tenderness Masses Enlarged organs Percussion CVA tenderness Documentation: (Include both Subjective and Objective Data in Narrative Form) 44 Physical Assessment Documentation Guide Student____________________________ Date ________________ Client/Patient Initials________Age ________Sex__________ Assessment of the Musculoskeletal System Subjective Data: (Obtain info from Review of Systems under Musculoskeletal in Jarvis) Objective Data Muscle strength Check each muscle group against resistance Compare right with left: Upper extremities Triceps Biceps Adduction arms Abduction arms Wrists – flexion, extension Lower extremities Quadriceps Hamstrings Abduction knees Adduction knees Plantar flexion feet Dorsiflexion feet Documentation: (Include both Subjective and Objective Data in Narrative Form) 45 Physical Assessment Documentation Guide Student____________________________ Date ________________ Client/Patient Initials________Age ________Sex__________ Neurological Assessment Subjective Data: (Obtain info from Review of Systems under Neurological in Jarvis) Objective Data Mental Status Examination Appearance (posture, body movement, dress appropriate for setting, grooming/hygiene) Behavior (level of consciousness, facial expression, mood and affect) Cognition (orientation x4, responsiveness, speech) Thought Processes (thought content for consistency and logic, perceptions consistency with reality, any suicidal thought) Pupillary Reaction (equality, size, shape, reaction to direct and consensual light) Sensory system (assess for intactness of the following sensory functions) Light touch Pain and temperature (only unable to feel light touch) Vibration Kinesthesia/Proprioception (position sense) Stereognosis Graphesthesia Two-point discrimination Motor function (assess for strength) Hand grips (ask client which is dominant hand) Foot pushes( plantar flexion) 46 Deep tendon reflexes (Grade) Biceps (optional) Triceps (optional) Brachioradialis (optional) Quadriceps or Patellar Achilles (optional) Cerebellar Functions Balance Gait Gross motor coordination – heel to toe walking Romberg Coordination Finger to Nose (eyes closed) Rapid Alternating Movements (RAM) Documentation: (Include both Subjective and Objective Data in Narrative Form) 47 PHYSICAL ASSESSMENT PRACTICUM Student____________________________ Date ________________ **Starred ** items are critical elements and must be passed by the student. Technique (5) Organization (5) Clear Instructions(2) Description Accurate (4) General Survey: Appearance (posture, grooming, hygiene, apparent signs of distress, dress) Behavior (attitude, mood and affect, facial expressions) Cognition (mental status, speech, level of orientation) Skin Color (pink, cyanotic, jaundice, dusky, pale/appropriate for race) Hydration – skin turgor Temp. and Moisture (warm/cool, dry/clammy) Lesions (describes morphology, size, color, pattern of arrangement, and distribution) (Describe two lesions) Neurological Pupils - equal, round, reactive to direct and consensual light Head and Neck Visual Inspection of skull, face (eyes, ears, nose, mouth, and neck) Include oral mucous membranes (color, moist/dry, lesions) Assess for drainage, lesions, distention, discoloration, and symmetry Lungs Performs inspection before auscultation Assess respiratory effort and rate Assess for symmetry of chest wall movement Auscultate for breath sounds (anterior or posterior chest) in a systematic order Heart Identify auscultatory sites: Aortic – 2nd right ICS Pulmonic – 2nd left ICS Tricuspic – Left 5th ICS sternal border or midsternal line Mitral – left 5th ICS midclavicular line **Auscultate S1 and S2 - assess rhythm (S1 S2 Reg./irreg.) assess for extra heart sounds & murmurs Identify PMI (left 5th ICS midclavicular line) Count Apical heart rate (BPM) for 1 full minute 48 Technique (5) Organization (5) Clear Instruction (2) Description Accurate (4) Peripheral Vascular Palpates for pulses together: Radial, Pedal Capillary refill (secs) (hands) **Assess for edema (depresses medial malleolus & pretibial area for 5 seconds) Abdomen ** Auscultation before Palpation Inspect for contour,lesions,distention Ausculate all 4 quadrants for bowel sounds Count in each quadrant for 1 full minute Light palpation all quadrants (bend knees before palpation) (begins at RLQ and proceeds clockwise) Motor - Assess hand grips and foot pushes bilaterally _______________________________________________________________________________________________________________ Musculoskeletal ROM and Motor strength against resistance: If unable to assess patient’s ability to move in the bed during the assessment, then test specific muscle sets: Upper extremities (arms only – biceps, triceps) Lower extremities (legs only – quadriceps, hamstrings) Performance HIPIE X Worked from head to toe Professional behavior (verbal and nonverbal communication, draping of patient) TOTAL SCORE: COMMENTS: _____/149 /50 /45 X /18 X /36 __________SATISFACTORY (95% or better= 141/149 points) __________NEEDS INPROVEMENT (90-94% = 133-140/149- Skills Lab Referral for head to toe physical assessment) __________UNSATISFACTORY (<90% or 132/149: Advisement note and retest with instructor).*** Failure to pass retest will result in requirement to complete N251 course prior to Fall semester N220 course or concurrent with Spring semester N220 course. 49 Nasogastric Tube Insertion Critical Thinking Questions Act out the most appropriate nursing actions for the following patient situations while you practice with the manikins. 1. Name nursing interventions/actions appropriate for a nasogastric tube that is difficult to advance 2. What nursing action is appropriate if the client coughs, is unable to speak, and becomes cyanotic during NGT insertion? 3. During advancement of the NGT, passed the nasopharynx, the client gags and coughs, but remains pink and is able to speak. What is the nurse’s next appropriate action? 4. Your client has a history of dysphagia from a previous stroke. The physician has ordered the client to remain NPO (nothing by mouth) and to insert a nasogastric tube. How would you proceed to instruct the patient to assist in advancing the NG tube once you have passed the nasopharynx. 5. If a Salem Sump pigtail leaks gastric contents, what should the nurse do? 6. Your client who has an NG tube connected to suction suddenly vomits around the tube. What is the appropriate action the nurse should take next? 7. Your client who is receiving a bolus NG-tube feeding is due for his morning medications. As you proceed to assess placement (by flushing with air and aspirating for gastric contents), you feel resistance and are unable to push the plunger. What may be the cause of the resistance and what is your most next appropriate action? 8. Your 72 year old male client has had a left sided stroke and is receiving a continuous G-tube feeding at 60 mL/hr. a. In considering the client’s diagnosis and treatment, what is he most at risk for? b. What is the most appropriate nursing intervention to prevent this risk? c. You are checking the client’s residual and you obtain no residual. What does this mean and what actions will you take? d. You are checking the client’s residual and you obtain 12 mL of residual volume. What does this mean and what action will you take? 9. Practice connecting the tubing for the Kangaroo pump and priming the tubing prior to connecting to the end of the NG tube or G-tube. 50 Nasogastric Tube Removal (AIR-WATER-AIR) 1. Check physician’s order for NG tube removal 2. Gather equipment: Towel, paper towel, stethoscope, container of sterile normal saline (or tap water), 60 mL syringe with catheter tip, tissues, clean gloves, tube plug 3. Assess client to determine presence of bowel sounds. Signs more indicative of GI function include passage of flatus, bowel movement, absence of nausea and vomiting, and presence of hunger. 4. Perform IPIE. Explain to client that removal may cause some nasal discomfort, coughing, sneezing, or gagging. 5. Place towel over client’s chest 6. Disconnect NG tube from suction tubing of feeding machine if indicated 7. AIR: Flush tube with a 15-20 mL bolus of air (to displace the tube from the gastric mucosa) then aspirate gastric contents to check for placement 8. WATER: Flush NG tube with 20 mL of NS or tap water (To clear tube so that GI contents do not inadvertently drain into the esophagus during tube removal) 9. AIR: Follow saline or water flush with a 20 mL bolus of air (to clear saline or water from tube and to free tube from stomach or intestinal lining) 10. Unpin tube from client’s gown and loosen tape that secures tube to client’s nose. 11. Plug tube or clamp it by folding it over in your gloved hand 12. Pinch tube to client’s nares, have client take a deep breath and hold it while you withdraw the tube (Holding breath closes glottis and helps prevent aspiration) 13. Wrap tube in paper towel and remove from client’s view 14. Offer oral and nasal hygiene 15. Empty and record amount and character or drainage if applicable 16. Discard equipment and clean up 17. Remove gloves and perform hand hygiene 51 Urinary Catheterization Critical Thinking Questions 1. Catheter is inserted into the female client’s vagina. What is the next most appropriate action by the nurse? (Role play this during practice and discuss your options with your fellow classmates). 2. Difficulty inserting catheter into a male client. a. Name two or three reasons a catheter would be difficult to insert in a male client. b. Identify appropriate nursing actions if experiencing this difficulty. 3. As you are inserting an indwelling catheter into your male client, he begins to have an erection. What is the most appropriate nursing action at this time? 4. As you insert an indwelling catheter into your male patient, there is no urine return. What are possible causes and what are appropriate actions by the nurse in this case? 5. Demonstrate and practice the steps to removing a catheter. See back page (Catheter Removal). 6. What appropriate nursing assessments and client teachings would you perform for a client who has had his/her catheter remove/discontinued? 7. Continuous Bladder Irrigation (CBI) – see CBI station and do the following as a group. a. Discuss the purpose of a CBI b. Discuss the procedure of initiating a CBI on your patient c. What color and consistency of urine output would you expect to see on the urine drainage bag immediately after a TURP-Transurethral Resection of the Prostate; and just before discontinuing the continuous bladder irrigation? ACCEPTABLE Alternative method during catheter insertion: Once the unine flows, you may choose to keep the sterile dominant hand holding the catheter and use your nonsterile /nondominant hand to inflate the balloon. NOTE: Preferred methods 1. You may also place the waste receptacle (cath kit bag) on the side of the patient instead of at the foot of the bed. 2. There is no need to pretest the catheter balloon if already pretested by the manufacturer. E.g. BARD catheter Kits have pretested balloons therefore do not need to test the catheter balloon. 52 N210 Fundamentals of Nursing CATHETER REMOVAL SKILLS CHECKLIST Recommended Technique N.I. S Comments U CHECK physician’s orders (and when last changed if requiring changing) WASH hands ASSEMBLE equipment: syringe, unsterile gloves Identify (armband) Explain Privacy POSITION: -Male: none required -Female: legs slightly apart REMOVAL: -empty FC drainage bag and discard urine. -empty catheter baloon by withdrawing fluid with syringe until resistance felt (balloon empty); note location of meatus in female if F/C being changed -Gently pull on F/C near meatus while pinching tube; inspect F/C for intactness (tip sent for C&S in some agencies) CLEAN perineum; provide patient comfort MEASURE urine; record I&O DISCARD equipment DOCUMENT procedure -Time -Patient’s response TEACHING: -2500 cc fluid/day, possibly acidifying liquids (cranberry juice) -Dribbling can occur for several hours -Need to void within 6-8 hrs; report if unable urge/fullness ASSESSMENT: -First void after d/c (If no void, include in shift report) -Frequency -Burning -Hesitation -Dribbling -Cloudiness or any other color or change in characteristics Rev. Fall’07 53 Wound Care Practice Station Check Off N210: Fundamentals of Nursing Station 1 Identify the wound pictures. Identify the wound as red/yellow/black. Stage the pressure ulcer. Picture 1_____________________________ Picture 2_____________________________ Picture 3_____________________________ Picture 4_____________________________ Station 2 Identify the name of each treatment and what type of wounds each treatment is used for. pg 924 and 925 as a reference) (use Transparent dressing_______________________________________________ Hydrocolloid dressing_______________________________________________ Wound vac_______________________________________________________ Hydrogel_________________________________________________________ Alginate__________________________________________________________ Foams___________________________________________________________ Station 3 Identify which wound is healing by primary intention and which wound is healing by secondary intention. Pay special attention to statement on tertiary healing in page 1189 -1190 of Taylor’s textbook. Primary _________________________ Secondary_______________________ Tertiary _________________________ Station 4 Identify each drainage device. The JP and Hemovac work by negative pressure- when compressed the drainage is PULLED into the collection area. Penrose__________________________________________________ Jackson-Pratt______________________________________________ Hemovac__________________________________________________ Station 5 Identify each of wound closure device 54 Staples_____________________________________________________ Retention sutures_____________________________________________ Sutures_____________________________________________________ Dermabond__________________________________________________ Steristrips____________________________________________________ Montgomery straps____________________________________________ Station 6 Identify each of the following types of wound drainage Serous__________________________________________________________ Sanguineous_____________________________________________________ Serosanguineous__________________________________________________ Purulent_________________________________________________________ Station 7 Check your answers on the study guide Station 8 (optional) Remove sutures Station 9 Practice a sterile wet to moist dressing change. 55 Cerritos College N212 Medication Administration Procedure 1. You will be assigned by your clinical instructor to administer scheduled medications to 1 patient on 2 consecutive days (2 days of care). 2. You MUST choose a patient that you will administer meds to the night before clinical and throughly complete the Schedule Med Day Medication Sheet for all the patient’s meds. 3. Choose a patient that has scheduled meds. Do not choose to give meds to a patient who has none or only 1 scheduled med (PO, SQ, IM, Inh., PR, Top.) 4. On the day of your scheduled Med Administration, you will administer all scheduled meds (PO, SQ, IM, Inh., PR, Top., etc.) to your patient with instructor supervision. 5. You and any other student (not scheduled to give meds) may give PRN IM/SQ meds with instructor supervision upon instructor availability. 6. You will not administer any scheduled IV fluids or IVPB medications. 7. If your patient has any scheduled IV/IVPB, be sure to remind your RN that you are not administering these. 8. Inform your RN that you will be administering all scheduled meds for your patient (except IV/IVPB) and obtain the patient’s Medication Administration Record (MAR). 9. Inform your clinical instructor regarding the scheduled times that you are to administer the medications. 10. Check the MAR against MD orders for all scheduled meds you will be administering to your patient. 11. Check the patient’s medication cassette for all scheduled meds as early as possible when you begin your shift. Practice doing the five rights at this time. 12. If a medication is missing from the patient’s cassette, send a “missing medication” form to the pharmacy before the scheduled time to give the medication (Ask your instructor for assistance in filling out the facility’s form). NOTE: It takes pharmacy time to get the medications up on the floor, so do it early….The earlier, the better. 56 Cerritos College N212 Medication Administration Procedure 12. Students should be prepared with appropriate data (VS, labs, and patient assessment) necessary prior to administering scheduled medications e.g. check BP before administering a BP med e.g. K+ level before administering Lasix • • Prepare the medications: • Calculate drug dosage • Prepare one medication at a time • Leave medications in packages if possible. • Use appropriate measuring devices to prepare medications. Be prepared to do the five rights in the presence of your instructor. 13. Be prepared to answer questions about the medication you are to administer Know why the patient is receiving the particular medication (you may need to look at the admission diagnosis or chronic illnesses from the H&P, or MD progress notes – Ask your instructor for guidance if you are having trouble with this). You should know the medications’ use/effect, adverse effects, nursing considerations, patient teaching, & pertinent drug-drug interactions. 14. Go into your patient’s room with your clinical instructor, patient’s scheduled meds, and MAR. 15. Wash hands and perform IPIE. 16. Identify your patient by comparing the armband against MAR using 2 identifiers: Medical record or patient number and patient’s name. Ask for allergies. 17. Open all meds at the patient’s bedside and proceed to administer the medications as ordered. 18. Perform basic patient teaching (medication, dose, and indication). • Always tell patient: (Name of medication, Dosage, & Indication for use) Ex: “Here is your atenolol 25mg, it is t o help control your blood pressure.” 19. Document on MAR a. As soon as possible AFTER administration b. Document time administered c. Initials d. Make sure signature/initials are in signature section of MAR 20. Document client response a. Narrative note b. Flowsheet c. Especially document for PRN medications and first time a new medication is administered 21. Document if refused or held a. Circle time b. Initial c. Reason not administered 22. Monitor patient for therapeutic effects. 57 NPW and Assessment Guide Guidelines General Instructions: All work must be neat and legible NPW to be completed on EVERY patient cared for in the clinical setting BEFORE you provide nursing care to the patient Complete an assessment guide for ONE patient and submit each week Staple any additional papers Highlight any abnormal findings on the Assessment Guide Make extra blank copies and keep them in your clinical folder If no order can be found, write “no order”. NPW Page 1 Student: write your full name Date: date(s) caring for patient Co-Assigned Nurse/NA: Nurse and nursing assistant assigned to the patient Patient Initials: Remember HIPPA regulations and only put the patient’s initials Room #: The room number of the patient Age: Age of the patient Admit date: The date the patient was admitted to the facility Surgery date: If applicable, state the date the patient had surgery relevant for the current admission Code Status: The resuscitation status for the patient. Ex: DNR, No Code, Full Code, No CPR Allergies: State all allergies to medications, food, environment Admitting diagnosis: State the diagnosis given as reason for admission. Ex: Pneumonia. May not have admitting diagnosis in long term care. May only have chronic diagnoses. Ask your instructor for assistance as necessary. History of present illness: Describe the events that occurred from time of onset of illness to time of admission. May not have in long term care. Course of events in hospital: What major events occurred from the time of admission to the time you assume care. Ex: Admitted with R/O Myocardial Infarction. That diagnosis was ruled out. Patient was found to have a hiatal hernia causing him chest pain and is schedule for surgery (fundoplication) to repair the hiatal hernia. Will not complete in long term care. Hx: State the patient’s significant past medical and surgical history. Ex: History of COPD, osteoarthritis, cataracts in the right eye MD Orders *ONLY MD ORDERS FROM THE ORDER SECTION OF THE CHART ARE ENTERED IN THIS SECTION Vital Signs: Frequency ordered Ex: every 4 hours. Diet/Feedings: Diet ordered and/or tube feedings (name of solution, volume to be administered, continuous vs. intermittent) Activity: The activity level ordered IVF: Intravenous fluids ordered for continuous infusion only. Ex: D5.45NS @ 100 ml/hr. Any piggyback solutions are written under medications Blood glucose monitoring: Frequency ordered Ex: QAC and HS (before meals and before bedtime). Treatments/Nursing Orders: This section should include any additional orders for the patient. Ex: strict I/O, wet to dry dressing change every 8 hours, Foley catheter, O2 at 2L NC. Diagnostic Results Should be the most recent lab results Record the normal range for each lab result -Urine: specify which urine test you are referring to. Ex: culture normal (-), patient result is + for E.Coli 58 -X-ray: specify which X-ray is done. Ex: CXR normal is (-) and patient result is right lower lobe infiltrate Record the reason for patient values. -If normal: state WNL. If this normal is unexpected, also state this and why Ex: WBC is normal for a patient admitted with pneumonia is an abnormal finding, but could be explained in a patient that is immunocompromised -If abnormal: state the reason the value is abnormal. Ex: Elevated WBC in a patient with pneumonia occurs because of response to inflammation and infection. NPW Page 2 Create two concept maps to represent the following information: pathophysiology, signs and symptoms, medical treatment and nursing interventions. In long term care, you may create concept maps for chronic medical problems. Ideally ones that have signs and symptoms you can observe and that have nursing interventions you can implement. In N212, you will need a concept map for every admitting medical/surgical diagnosis and additional concept maps if the patient has diabetes, hypertension, COPD and/or chronic renal failure (ESRD, CRD, is on dialysis). Medications Page 3 Drug Names: State the trade (one) and the generic name of the medication Class: State both the functional and chemical class for each drug. Dosage and range: State the normal dosage range for this person (ex: elderly) and the dosage ordered for the patient Route: State the route ordered for the patient. Ex: oral, intramuscular, subcutaneous, etc. Indication for use for this patient and nursing implications: Why is this medication ordered for this patient? State any nursing implications for the administration of this medication. Ex: Check BP before administering an antihypertensive. Time and frequency: State when the drug is ordered to be administered and the frequency of administration. Ex: Ordered twice a day and the administration times are 0900 and 2100 Attach additional paper if needed Assessment Guide (AG) Page 4 The Assessment Guide is based on the diagnostic divisions based on the Roy Adaptation Model. The RAM diagnostic divisions page should be used as a guide to assist you in figuring out what information should be included in each section. This page is arranged in a stepwise approach, addressing each piece of information as you complete the Assessment Guide chart. Eventually this will become second nature and you will not have to refer to the diagnostic divisions page for reference. Once the data collection is completed, you will be directed from your clinical instructor on how many complete diagnostic divisions should be thoroughly completed, starting with one, adding more sections as you become more proficient. AG Psychosocial & Documentation Page 5 Use this area for documentation as directed by your clinical instructor. You may be instructed to document a narrative, DAR, SOAPIE note or any variation that may be used by your facility. 59 Roy Adaptation Model Reference Sheet for Completing the Assessment Guide Neurological Neurological Function -Subjective Data Obj: LOC, GCS (eye opening, verbal response, motor response), seizures (describe, timing), altered mental status, aphasia, intellectual functioning -Lab results: radiology (EEG, MRI, etc) -Interventions: seizure precautions, etc. Include Sensation -Subjective Data -Pain (location, intensity, character, onset and duration), vision, hearing, response to sensory overload -Interventions: PCA pump, special devices (glasses, hearing aid) Protection Protection -Subjective Data, immunization status -Obj: Temperature, Shivering, Diaphoresis, Skin/Hair/Nails (describe), Lesions (describe, location), Incisions (describe, location), IV site (describe, location), AV shunt (describe) -Lab results: WBC, C&S (specify source: wound, sputum) -Interventions: Wound dressing (location, describe), drainage tubes (type, site, describe), Isolation, Siderails, Bed position, Restraints (Type, reason) Oxygenation-gas exchange Oxygenation-gas transport Focused Assessment Plan Oxygenation : Gas Exchange -Subjective Data -Obj: Respiratory Rate, Depth, Effort, Breath Sounds (describe, location), Cough (describe), Sputum production (describe) -Lab results: Sputum C&S, radiology results, ABG -Interventions: positioning, turning, DB&C, oxygen (flow rate and method), pulse oximetery (% on how much oxygen), incentive spirometer (volume, frequency of use), suctioning (type, frequency, response) Nutrition Nutrition -Subjective Data -Obj: Height, Weight, Ideal body weight, Nutrition intake, NPO status and reason, food intolerances , nausea, emesis (describe), swallowing ability, gag reflex, oral cavity (inspect and describe), cultural preferences -Lab results: Cholesterol (HDL, LDL), blood sugar, Ca, K, Na, Albumin -Interventions: Diet; Enteral feedings (tube type, formula and flow rate), TPN/Lipids F&E Fluid and Electrolytes -Subjective Data -Obj: Changes in weight, LOC, thirst, 24 hour intake/output, abnormal loss (edema, drainage, diuresis, diaphoresis, tachypnea, diarrhea, emesis), tissue turgor, mucous membranes) -Lab results: Na; Cl; K; ABG: HCO3, pH; Urine specific gravity -Interventions: IVF (solution, tonicity of solution, flow rate), NG drainage (amount, describe) Oxygenation: Gas Transportation -Subjective Data -Obj: Blood pressure, apical pulse, peripheral pulses (location, rhythm and strength), edema (degree, location), capillary refill (location), skin/mucous membranes, Homan’s sign (if appropriate) -Lab results: Hgb, Hct, RBC, platelets, PT/PTT, INR Bowel/Urinary Elim Bowel/Urinary Elimination -Subjective Data -Obj: Abdomen (inspection, auscultation, palpation), urine (describe), Flatus, Stool (describe), last bowel movement -Lab results: Urinalysis/Culture, Serum: BUN, creatinine, RBCs, WBCs, stool specimen results, radiological studies -Interventions: catheter, colostomy/ileostomy, bladder irrigation Act & Rest Endocrine Activity and Rest -Subjective Data -Obj: Activity level and tolerance -Muscle and joints (description, movement, strength, coordination), posture/gait (describe), circulation/sensation/movement (describe), rest and sleep patterns (describe) -Lab results: Ca, Phos, Mg, radiological results -Interventions (assistive equipment-cast, trapeze, traction, CPM, etc), special beds (type) Endocrine Function -Subjective Data -Diabetes Mellitus, Thyroid, Parathyroid, Reproductive function (last menstrual period, menopause, infertility, changes in sexual function) -Lab results: Thyroid (TSH, T3, T4), blood sugar, estrogen, other 60 Assessment Guide-Psychosocial Interdependence: -Interdependence: Significant others and support systems: Does patient have families/significant others/friends who can assist them? Assess for safety concerns regarding their behaviors and ability to care for self both in the hospital and when they go home. Assess the patient’s ability to accept assistance and care from their healthcare team. Assess and document if the patient is exhibiting inappropriate dependent or independent behaviors affecting patient safety. Role Function -Role Function: Focus on assessment of patient chronic diseases and their acceptance, knowledge and home management. Focus on how the patient is adapting to their acute illness and hospitalization. Are they participating in their care, or refusing care? Assess for body image concerns in patients who have removal of organs, incisions or tubes, disfiguring procedures and surgeries such as amputations or removal of a breast or prostrate? Date/Time Focus Cultural Considerations Cultural: Health care beliefs (pain, nutrition, disease, health, family and gender roles). Language (barriers) and Communication considerations; cultural considerations re: eye contact, touch, & space. Self Concept -Self Concept: Focus on how the patient views themselves. Do they have positive or negative self-esteem? Do they feel good about themselves? Are they out going or withdrawn? Are they experiencing any fear, anxiety, anger or grief regarding their life situation? How are they coping? What spiritual concerns might they have and are spiritual needs being met? Any problems with sexuality? Documentation 61 Assessment Guide Patient Initial: _______ Room#: ______ Date: __________ Neurological Subj: “My hands ache, it must be raining outside” Obj: AAOX4, GCS 15 Pain 5/10 Bil. hands, aching, onsetupon waking, Motrin ↓’d pain to 1/10 Protection Subj: Flu shot in the fall, Pneumovax 1 year ago Obj: Temp 100.5 F, No chills Fluid and Electrolytes Subj: Obj: 2 lb wt loss since admission Skin: intact, ,pink, warm and dry Lesion: R heel stage III. 1cmX 1cm, red, serous discharge. IV site: R AC. No s/s infection or infiltration. 2/5/05 I: 1500 ml/ O: 2200ml Tissue turgor: good MM: dry Labs: Na: 144, K: 4.0; Cl: 102 Labs: WBC: 18 Labs: NA Oxygenation: Gas Exchange Subj: “I can’t breathe” Obj: RR 24, even and labored. Focused Assessment Plan Oxygenation: Gas Transport Obj: BP 142/85 lying; Apical: O2@ 2L NC with O2 Sat. of 95%. Breath sounds: crackles BLL. Cough productive of mod. amt of thick green/yellow sputum. Labs: CXR: BLL infiltrate 105 S1S2 irregular;Radial/pedal 2+ Bil., irregular Edema: none; Cap refill BUE/BLE 2 sec Skin color: pink; Skin temp: warm ; MM: pink/dry Labs: H/H: 16/48; RBC: 5.2; platelet: 200,000; PT: 12; PTT: 62; INR: 2.3 Nutrition Subj: “I’m not hungry” Obj: Ht: 5’11” Wt. 176 lbs Bowel/Urinary Subj: Obj: Abdomen non-distended, soft, IBW: 166 lbs Intake: Breakfast 30%, Lunch 40% Oral cavity: full dentition, Tongue: pink/dry, no lesions; Gums: pink/dry Labs: 205; Ca: 8.5; K: 4.0; Na 144: Albumin: 3.8 nontender, BS X4-hypoactive. LBM 2/1/05. States “I usually have a bowel movement every day after I eat my bran cereal. I feel constipated” Urine: clear, yellow Activity/Rest Subj: “I feel weak” Obj: BRP, Endocrine Subj: “I’ve been a type II Muscle/Joints: no contractures, morning stiffness in B hands. Movement limited in hands. Strength: strong BUE, BLE Coordination: smooth Posture/gait: kyphotic/ steady CSM: Feet cool, sensation intact, movement intact Sleeps 6 hours a night with one wakening for bathroom Obj: Labs: Ca: Labs: UA: negative 2/4/05 BUN: 11, Creat: 0.6 diabetic for 5 years” Labs: Serum glucose: 205 Fingerstick BS (0730) 198, (1130) 213 8.5 62 Assessment Guide-Psychosocial Interdependence Significant Others Subj: Wife and children Obj: Rec: Accepts calls and visits from family. Giving: Returns affection of wife, calls wife Psychosocial: Role Function Cultural Considerations Self Concept Primary Role: Psychosocial Self Concept Sex M Age 68 Ego integrity vs. Despair Secondary Role: Role: Diabetic Instr: Check BS 4X/day at home. Asks about glucose reading. Tries to follow diet Expr: “I know I have to keep my BS under control, I don’t want to loose a limb.” Role: Husband Instr: Calls wife every day Exp: “I have to get home and be with my wife, she misses me” Tertiary Role: Role: Pneumonia patient Instr: Takes breathing treatments and oral meds, Performs TCDS exercises Exp: “I want to get my breathing back to normal” Role: Masonic member Instr: Attends monthly meetings. Chairperson of fundraising Exp: “It feels good to be a member of a group.” Date/Time 02/02/12 1400 Focus Resp Physical Self: Body sensation Subj: “My hands ache” “I don’t like to wear this oxygen, it makes me feel old” “Am I going to have to wear this oxygen forever?” “I just want to go back to my normal self” “I believe that God will help me through this. “ Obj: wearing O2 al 2L per NC Rubbing hands together.Tears in eyes Performs TCDB exercises, verbalizes desire to learn about medications and treatments to improve. Prays in room. Asks for chaplain to visit Documentation S: “I can’t breathe”---------------------------------------------------------------------------O: Resp shallow, labored, 30/min. Intercostal retractions present. BS c coarse crackles BLL and sibilant wheezes BUL. O2 @ 2L NC c pulse ox 90%.A: Impaired gas exchange-------------------------------------------------------------------P: Administer prn bronchodilator---------------------------------------------------------I: Administered Albuterol unit dose via face mask @ 1340 ---------------------E: States “My breathing is better now” Resp regular, unlabored, 22/min. No intercostals retractions. Remains on O2@2L NC c pulse ox 95%. BS c coarse crackles BLL. No wheezing noted. . No apparent distress noted. ________________________________________________N.Nurse SNCC 63 Lab Group _____ N212 Nursing Process Worksheet-NPW Student:____________________________ Date(s):____________ Co-Assigned Nurse/Nursing assistant:_____________________ Patient Initials:_________ Room #_________Age/Sex_______ Admit Date:___________ Surgery Date:__________________ Code Status:___________ Allergies:_______________________________________________________________________________ Admitting Dx: History of present illness: PMH: Course of events in hospital: MD Orders from Physician Order Section of Chart Vital Signs (Frequency) Treatments/ Nursing Orders: (Restraints, Fluid Restriction, PT etc) Diet/Feedings: Activity: O2 Foley Glucose Testing Times: Tests & Procedures: IV & Rate: Wound Care & Dressing Change Result and (↓ ↑) Admit Na+ K+ ClCa+ Albumin Creatinine BUN Glucose WBC RBC Hgb Hct Platelets PT PTT aPTT INR Urine X-ray Normal Range Result (↓↑) Tuesday Result (↓↑) Wednesday I&O NGT JP Lab Result Summary: Discuss abnormal lab values and diagnostics and relate them to the admitting diagnosis or chronic/concurrent diseases Comments (Monitoring , Actions, Notified MD) 136-145 3.5-5.0 98-106 9.0-10.5 3.5-5.0 (M) 0.6-1.2 (F)0.5-1.1 10-20 70-150 5000-10000 (M)4.7-6.1 (F)4.2-5.4 (M)14-18 (F)12-16 (M)42-52 (F)37-47 150000-400000 11-12.5 60-70 30-40 0.9-1.2 NEG NEG 64 Assessment Guide Patient Initial: _______ Room#: ______ Date: __________ Neurological Subj: Subj: Protection F&E Subj: Obj: Obj: Obj: Labs: Labs: Labs: NIC: NIC: NIC: Oxygenation-gas exchange Subj: Focused Assessment Plan Oxygenation-gas transport Subj: Obj: Obj: Labs: Labs: NIC: NIC: Nutrition Bowel/Urinary Elim Subj: Subj: Obj: Obj: Labs: Labs: NIC: NIC: Act & Rest Endocrine Subj: Subj: Obj: Obj: Labs: Labs: NIC: NIC: 65 Assessment Guide-Psychosocial Interdependence: Subj: Obj: Role Function Cultural Considerations Self Concept Subj: Subj: Obj: Obj: Date/Time Focus Documentation 66 Nursing CareMaps Identify the MAIN medical/ surgical diagnosis and all chronic medical diagnosis. Construct a Caremap (See CareMap Guidelines) that includes the following: 1. 2. 3. 4. 5. 6. Define and explain the pathophysiology of the Medical diagnosis. Identify all signs and symptoms pertinent for the medical diagnosis. List nursing interventions appropriate for the medical diagnosis. List all treatments including pharmacological and non-pharmacological modalities for the medical diagnosis List all the diagnostic tests and laboratory tests pertinent to this medical diagnosis. List all possible nursing diagnoses appropriate for this medical diagnosis. 67 Nursing Diagnoses: SAMPLE CAREMAP TEMPLATE Nursing Interventions Signs and Symptoms Medical Diagnosis Pathophysiology Pharmacological Treatment Diagnostic tests: 68 MEDICATION SHEET (for Non-Med Days) MEDICATION: Generic / Trade Classification (Functional/Chemical) DOSE /ROUTE/ FREQUENCY: Reason why THIS Patient is receiving 69 Medication Sheet for Med Days MEDICATION: ROUTE/DOSE / Generic / Trade FREQUENCY: Classification (Functional/Chemical) Safe Dose Range ACTION & SIDE EFFECTS: Most common and life threatening NURSING CONSIDERATIONS: ASSESSMENTS / LABS PT TEACHING NEEDED: Reason why my pt is receiving this 70 SAMPLE MEDICATION SHEET FOR NON-MED DAYS Drug Names (trade/generic) Class (functional/chemical) Apo-Pen VK/ penicillin V potassium F: Broad spectrum antiinfective C: natural penicillin Cleocin/ clindamycin HCL F: antiinfective-misc C: Lincomycin derivative Percocet Proventil/albuterol F: Bronchodilator C: Adrenergic B2-agonist, sympathomimetic, bronchodilator Oxycodone F: Opiate analgesic C: Semisynthetic derivative Tylenol/ acetaminophen F: Nonopiod analgesic C: nonsalicylate, paraminophenol derivative Cardura/ doxazosin F: Alpha Blocker, antihypertensive C: Quinazoline Dose Route Time Frequency Why is my patient receiving this 400mg IV QID 1200,0600, 1800,2400 600 mg IV BID 0900, 2100 2.5mg/ml unit dose Inhaled QID PRN - Bacterial pneumonia (gram + cocci) - Bacterial pneumonia - Bronchodilation to assist breathing difficulty from pneumonia 5mg PO Q 4 hours PRN 325mg PO Q 4 hours PRN - Reduce pain caused by osteoarthritis and pleuritic chest pain - Fever and could be used for pain management for the osteoarthritis and pleurtic chest pain 2mg PO Once a Day - To lower blood pressure (hx of HTN) 2.5mg PO Once a Day 1600 - Prevent embolus formation from atrial fibrillation RISS/SC QAC, HS 0730,1130,1700,2100 - Lower blood sugar (Hx of diabetes ) 0900 Coumadin/ warfarin F: Anticoagulant Humulin R/ regular insulin F: pancreatic hormone C: exogenous unmodified insulin 71 Student ____________________________ ___Fall____Spring _____Year Cerritos College Health Occupations Division Associate Degree Nursing Program Clinical Performance Evaluation Nursing 210 This evaluation tool will be used for measurement of the clinical course objectives. Evaluation of the clinical performance will be based on behaviors identified in the evaluation key and the accompanying guidelines. Professional nursing requires competency in both theoretical knowledge and application to clinical practice. Clinical Competency must be demonstrated by meeting all Critical Clinical Competencies, as well as a “satisfactory” or “needs improvement” marking at the end of the clinical tool to pass the clinical component of this nursing course. CRITICAL CLINICAL COMPETENCIES: MASTERY MUST BE DEMONSTRATED IN ALL OF THE FOLLOWING CRITICAL CLINICAL COMPETENCIES AT ALL TIMES. A CRITICAL BEHAVIOR IN ONE OF THE FOLLOWING AREAS WILL CONSTITUTE AN IMMEDIATE CLINICAL FAILURE. Demonstrates safe practice of designated nursing skills. Provides for physical safety of patient. Protects patients from emotional harm. Communicates clearly both verbally and in writing Seeks assistance from instructor or other healthcare members for care which is beyond the student’s level of knowledge or experience. Calls attentions to own errors and reports situations accurately. Maintains confidentiality. Complies with college and agency policies and procedures. Submits required graded papers. Passes Medication Calculation Exam Other behaviors that will result in clinical failure include: Dishonesty including but not limited to cheating, plagiarism, fabrication, and misrepresentation. Violent or aggressive behavior Disrespectful and/or abusive language or behavior Use of drugs or alcohol (legal or otherwise) in clinical setting Stealing Conviction of felony 72 0 OUTSTANDING: Consistently above-average performance and self-directed. Requires minimum guidance. S SATISFACTORY: Overall satisfactory, occasionally requires some guidance NI NEEDS IMPROVEMENT: Inconsistent performance requires repeated guidance and supervision. Nursing 210 Clinical Evaluation Tool Overall Clinical Performance Evaluation: There are (8) Major Areas of clinical performance for evaluation: Professional Behaviors, Communication, Critical Thinking and Clinical Decision Making, Nursing Process, Caring, Teaching and Learning, Clinical Skills, and Managing Care. I. Three or more needs improvement “NI” in one major area will result in an “overall needs improvement” for that major area. (ex: 3 “NI”s out of the 8 criteria in the area of Professional Behaviors will result in an overall NI for Professional Behaviors). A student may progress to the next clinical with an overall “NI” in only one major area. In this case, the student will receive an overall “Needs Improvement” in clinical and an Advisement Notice for the major area of Needs Improvement. II. A student who receives an “overall needs improvement” in more than one major area will fail clinically. (ex: overall “NI” in Communication and overall “NI” in Nursing Process). III. A student who has a “needs improvement” marking in eight or more single, isolated boxes throughout the entire tool will fail clinically. IV. For less than eight single “needs improvements” throughout the entire tool, the student can progress to the next clinical with an overall “Satisfactory” or “Needs Improvement” (with an Advisement Notice attached) based upon instructor evaluation and anecdotal. 73 Core Clinical Competencies PROFESSIONAL BEHAVIORS: Practices safe professional behaviors consistent with ethical, legal and regulatory standards of professional nursing practice when providing client care. O S NI O S NI 1. Complies with college, nursing department, and facility regulations and policies. 2. Arrives at clinical prepared for patient care. Submits all assignments within designated time frame, including referrals and make-up assignments. 3. Notifies instructor when unable to attend clinical or will be late. 4. Demonstrates responsibility and accountability for one’s actions. a. Calls attention to errors and reports situations to clinical instructor. b. Reports unsafe practices. c. Maintains professional boundaries in the nurse-client relationship. 5. Practices within guidelines of N210; individual knowledge and expertise; and seeks assistance for care beyond level of knowledge. 6. Abides by HIPPA standards 7. Follows universal precautions. 8. Demonstrates professional behavior such as a positive attitude, punctuality, self-direction, and an appropriate appearance (follows dress code – ref. student handbook). OVERALL EVALUATION ON PROFESSIONAL BEHAVIORS: COMMUNICATION: Communicates effectively with nursing staff, various members of the healthcare team, patients and family members. 1. Communicates verbally in a clear and concise manner in English. 2. Writes in a clear and concise manner in English. 3. Begins to utilize therapeutic communication when interacting with patients, family and significant others. 4. Verbalizes assessment, interventions and evaluations using appropriate medical terminology at a beginning level. 5. Begins to communicate with the healthcare team: providing patient updates in a timely manner to staff nurse and instructor. OVERALL EVALUATION ON COMMUNICATION: 74 CRITICAL THINKING AND CLINICAL DECISION MAKING: Uses critical thinking when performing all steps of the nursing process with patients in the clinical setting. O S NI O S NI O S NI 1. Begins to make clinical judgment decisions to ensure safe and effective care when providing patient care with instructor support. 2. Begins to organize plan of care and prioritize total patient care for one patient. 3. Demonstrates, at a beginning level, the ability to apply theory to clinical situations, stating scientific rationale, incorporating best practices. OVERALL EVALUATION ON CRITICAL THINKING / DECISION MAKING: NURSING PROCESS: Applies the Nursing Process in implementing care. 1. Begins to utilize appropriate sources to elicit data about the patient. 2. Performs and documents a physical assessment, demonstrating appropriate use of medical terminology and approved abbreviations, at a beginning level. 3. Initiates an environmental assessment. 4. Begins to identify appropriate nursing problems / nursing diagnosis. 5. Begins to develop patient-specific interventions. 6. Begins to evaluate patient response to care and revises patient care as needed. OVERALL EVALUATION ON NURSING PROCESS: CARING INTERVENTIONS: Demonstrates caring behaviors towards the patient and significant others. 1. Assists the patient to obtain optimum comfort and functioning. 2. Provides a safe physical and psychological environment protecting the patient from undue harm, maintaining dignity and respect. 3. Identifies and adapts care to honor the patient’s values and customs, and the emotional, cultural, and spiritual needs. 4. Advocates for the patient. 75 5. Demonstrates empathy when providing nursing care. OVERALL EVALUATION ON CARING BEHAVIORS: TEACHING AND LEARNING: Demonstrates application of teachinglearning principles. O S NI O S NI O S NI 1. Provides simple explanations and instruction to patients prior to interventions and / or procedures. OVERALL EVALUATION ON TEACHING AND LEARNING: CLINICAL SKILLS: Competently performs technical skills with patients in the health care setting. 1. Demonstrates safe practice of designated nursing skills for N210 in clinical and/or skills lab. 2. Seeks out patients that provide varied learning and skills opportunities. OVERALL EVALUATION ON CLINICAL SKILLS: MANAGING CARE AND COLLABORATION: Effectively manages patient care in collaboration with other members of the healthcare team, patient and significant others. 1. Begins to work cooperatively with health care team members, peers, faculty, patients and their significant others toward common patient-centered outcomes. 2. Manages the patient assignment in an organized and efficient manner completing care within allotted time frame. OVERALL EVALUATION ON MANAGING CARE: 76 N210 Nursing Skills Competency Check box for each skill: S= Satisfactory, NI= Needs Improvement, LP= lab Performance only, LO= Lack of opportunity to evaluate S NI LP LO Performs skills necessary to meet activity and rest needs including: Utilizing body mechanics, positioning, ambulation, and transfer activities Utilizing active and passive range of motion and isometric exercises Making unoccupied and occupied beds Performs skills necessary to meet nutritional needs including: Feeding patients orally Feeding patients via nasogastric and/or gastrostomy tubes (H20 flush/placement check) Inserting nasogastric tube Assessing nutritional status (% of meal consumed and recording oral intake) Performs skills necessary to meet elimination needs including: Assisting with toileting Inserting and maintaining catheters Assessing and recording fluid output Administering an enema or Harris flush Inserting rectal tube and/or suppository Collecting specimens Performs skills necessary to meet oxygenation needs including: Performing, assessing and recording vital signs (temperature, pulse [apical and radial], respirations, pulse oximetry and blood pressure) Performs skills necessary to meet protection needs including: Hand hygiene Provide personal hygiene measures (bath, oral care) Gowning and gloving Applying isolation techniques Applying bandages, binders, restraints and anti-embolism stockings Maintaining a sterile field Providing wound care Assessing level of pain Performs physical assessment practicum (Pass/Fail) Pass random skill testing within 2 tries. Failure to pass within 2 attempts will be reflected in your overall clinical evaluation. List all skills the student performed in this clinical rotation: 77 N 210 Overall Clinical Competency 0 S NI OUTSTANDING: Meets all Critical Clinical Competencies. Consistently aboveaverage performance and self-directed. Requires minimum guidance. SATISFACTORY: Meets all Critical Clinical Competencies. Overall satisfactory, occasionally requires some guidance NEEDS IMPROVEMENT: Meets all Critical Clinical Competencies. Inconsistent performance requires repeated guidance and supervision. 1) Overall “NI” in only one major area OR 2) Fewer than eight single needs improvement throughout the clinical tool U *Advisement Notice Required for students with an overall “Needs Improvement” UNSATISFACTORY: Unsatisfactory performance. 1) Fails to meet one or more critical clinical competency OR 2) Receives more than one “overall needs improvement” in a major area OR 3) Receives a single “needs improvement” in eight or more single boxes throughout the entire tool. *Results in clinical failure. Midterm Evaluation (as needed): _________ Needs Improvement ___________ Unsatisfactory Comments: Instructor Signature:___________________________ Date:_____________ Student Signature:_____________________________ Date:_____________ Final Overall Evaluation: ____Outstanding _____Satisfactory _____Needs Improvement _____Unsatisfactory Comments: Instructor Signature:___________________________ Date:_____________ Student Signature:_____________________________ Date:_____________ 78 Cerritos College Health Occupations Department of Nursing Guidelines for Clinical Performance Evaluation Tool Professional Behavior Students will practice safe professional behaviors consistent with ethical, legal and regulatory standards of professional nursing practice when providing client care. Students are held accountable to standards of practice for nursing care. Policies and procedures should be used to guide practice and be upheld. Students must notify instructor of any clinical absence or tardiness. Failure to do so will result in a clinical failure. Tardiness is not an accepted clinical behavior. The first tardy will result in a verbal warning, the second will result in an advisement note and the third tardy will result in a clinical failure. Two or more absences may result in a clinical failure. All clinical hours will be made up according to individual course policy. Students are to arrive at the clinical site in a timely manner with written assignments completed and equipped with the knowledge necessary to give safe competent care. Failure to do so will result in adjustment of the patient care assignment, up to and including being sent home. Students are expected to demonstrate consistency in growth in both written assignments and clinical performance. The ability to follow directions and guidelines is imperative in the practice of professional nursing. Students are expected to adhere to all directions and guidelines, both in the care of the patient and in preparation of written assignments. It is the responsibility of the student to seek clarification, if unclear about expectations. Assessment of the ability to follow guidelines and directives extends to the policies and procedures of the clinical facility to which the student is assigned. Practices within guidelines of N210 and individual knowledge and expertise and seeks assistance for care beyond level of knowledge. Clinical instructors recognize that students are learning. Students are to acknowledge the limitations of their knowledge and seek to correct areas of knowledge deficit. Assistance should be sought as needed; failure to do so may jeopardize the patient, the student or others. Students are expected to verify dependent nursing interventions in the physician’s orders prior to implementation. This includes all treatments and medications. In addition the student is responsible to check the physicians’ orders regularly to determine if existing orders have been altered or new orders have been written. Students represent not only themselves and their families, but Cerritos College, the clinical facility to which they are assigned and the profession of nursing as a whole. Physicians, patients, families and other health care 79 team members judge nursing care by the behavior and appearance of the nurse. The expectation is that students will role model the highest standards of professionalism, including adherence to the Student Dress Code policy. A professional demeanor is to be maintained at all times. A component of action and behavior on the part of the professional is the ability to be self-directed, and example of which is to use clinical time wisely by seeking learning experiences. Students are expected to participate in shared learning experiences, including group conferences. Development of awareness and understanding of how personal/professional behavior influences patient care is expected of each student. Students are to demonstrate knowledge of and competency in infection control measures appropriate to the clinical site and the needs of each patient. These include but are not limited to: hand hygiene, wiping down equipment, and proper use of personal protective equipment. Students are expected to maintain the confidentiality of all personal health information in accordance with HIPPA. Identifying data must be removed from all documents leaving the clinical site. Communication Students will communicates effectively with nursing staff, various members of the healthcare team, patients and family members. Students are expected to communicate clearly in English at all times and use appropriate medical terminology. Bilingual students may communicate with their patients in the patient’s preferred language. The student should be able to communicate a clear and concise verbal report of their patients. Students are expected to communicate with their patients while providing care. Written assignments should be legible and grammatically correct. Students are expected to show improvement in their documentation and verbal skills as they progress in clinical. Ability to communicate following proper lines of authority will be included in the evaluation. Students are expected to clarify their role responsibilities with the RN and CNA prior to assuming care. Verbal Report First Semester Students Students should begin to formulate a verbal report that includes patient condition, pertinent assessment findings and priority care needs. Second semester students Students are expected to provide an organized verbal and written report. Second Year Level Students Students are expected to provide an organized verbal report reflecting patient condition, pertinent assessment findings and priority care needs. Critical Thinking and Clinical Decision Making Student will use critical thinking when performing all steps of the nursing process with patients in the clinical setting. 80 Nursing Process Worksheets (NPWs) are to be completed on all patients prior to clinical. Arriving to clinical unprepared will result in adjustment of the patient care assignment, up to and including being sent home. Being sent home warrants an advisement note and the student is required to complete a clinical make-up assignment. . Students are expected to show progression in critical thinking and problem solving skills. Students are expected to function within the scope of practice within their respective course. Unsafe clinical behaviors/judgment will result in a clinical failure. Students are expected to transfer and apply knowledge from previous and current courses. Students must show progression in the application of scientific rationale. Students are expected to show a progression in the ability to synthesis data and develop an understanding of the patient’s clinical situation. Students should show a progression in being able to recognize the relationship between assessment data (physical assessment findings, diagnostic tests, and medications). Problem Solving First Year Level Students will begin to apply problem solving with support from the clinical instructor. Students should present problem issues to the clinical instructor armed with possible solutions to the problem at hand that demonstrate critical thinking. Second Year Level Students will apply problem solving while providing care for more complex and increased number of patients with increased confidence. Students should begin to anticipate possible outcomes prior to deciding nursing actions. They will validate decisions with the instructor and require less direction and dependency throughout the clinical rotation. Their level of independence remains within the student role but allows for a safe and smooth transition to the next course. NURSING PROCESS Student will apply the Nursing Process in implementing patient care. Students will utilize the nursing process when assessing, implementing and evaluating care. The Roy Adaptation Model will be used to collect and organize assessment data. Assessment data should include subjective and objective data. Objective data may include but not limited to diagnostic tests, lab values, past medical history, physical assessment, medications, physician orders and interdisciplinary treatments. Students are expected to use NANDA approved nursing diagnoses provided in the course packet. (N/A at N210) 81 The ability to formulate a nursing care plan that reflects the priority nursing problems for a patient is critical to the function of a nurse. Failure to achieve 75% on the Nursing Care Plan/Concept Map will result in an advisement note. Failure of a Nursing Care Plan/Concept Map in a subsequent course will result in a clinical failure in that course. (N/A at N210) Students are encouraged to seek instructor assistance and/or guidance prior to submission of the Nursing Care Plan/Concept Map. (N/A at N210) Caring Interventions Student will demonstrate caring behaviors towards the patient, significant others, peers and members of the healthcare team. Students are expected to: Protect and promote the patient dignity. Identify psychosocial needs. Provide for the privacy of patients at all times. Protect the patient from physical harm by identifying potential or actual threats and act to correct them. Examples of unacceptable behaviors include: leaving side-rails down when patient is at risk for falling, leaving syringes with needles in the room, not recognizing breaks in sterile technique, picking up items off the floor and using in patient care, not discriminating clean versus unclean, not using gloves when needed when protecting self or others, not utilizing hand hygiene, not recognizing when contamination occurs and taking appropriate corrective actions or not adhering to isolation policies. Protect the patient from emotional harm by identifying potential or actual threats and act to correct them. Examples of unacceptable behaviors include: ignoring patient concerns; failure to psychologically prepare patients before procedures; making statements that instill fear or anxiety; using inappropriate “slang” language or inappropriate terms of endearment such as “honey” or “sweetie”; sexual innuendos; not promoting an environment that allows the patient to express their feelings; not demonstrating empathy while caring for patients and performing procedures; not seeking guidance if unsure of course of action; failure to report abnormal findings or change in condition. Teaching and Learning Students will demonstrate application of teaching-learning principles. Students are expected to: Document patient teaching on NPW and patient record as indicated. Include teaching in the care of their patients and families from the first clinical course and throughout the program. Demonstrate the ability to prepare and present educational needs of the patient as well as evaluate the effectiveness of the teaching. 82 Utilize patient teaching opportunities with medication administration. (N/A at N210) Assess the patient’s understanding of clinical situation or disease process. Assess patient’s management of chronic conditions. Respond to patient questions appropriate to their level. Managing Care/Collaboration Students will effectively manage patient care in collaboration with other members of the healthcare team. Students are expected to interact in a professional and collegial manner with all members of the healthcare team. The student team coordinator obtains pertinent data from team members on all patients assigned to the team. (N/A at N210) The team coordinator gives a complete report to the clinical instructor on the status of patients assigned to the team. (N/A at N210) All students are to utilize appropriate channels of communication (assigned staff nurse, student team coordinator, and instructor) when providing patient care. Students are expected to report to appropriate staff and instructor pertinent abnormal patient information or when patient situations change. Examples: abnormal VS, respiratory distress, unrelieved pain, low urine output, abnormal labs, signs of bleeding, changes in level of consciousness and inappropriate behavior. Students are to assist fellow students and staff as needed. Students are expected to answer all patient call lights and requests for assistance even if the student is not assigned to the patient. Students should relay requests to appropriate staff nurse. Students will delegate aspects of nursing care to the appropriate members of the student team according to Team Role Guidelines. (N/A in N210) Students are expected to begin developing leadership and assertiveness skills and show initiative in solving problems and meeting patient needs. Examples: Following up on missing food trays, medications, checking orders, providing education, asking MD questions, volunteering to assist MDs, seeking out learning opportunities, and developing communication skills. 83 Approved Abbreviations i ii ∆ ° ā AAOx4 abd ABG AC a.c. ADA ADL ad lib AFA aka AKA alb ALOC AMA amb amt ant as tol ASA ASHD Ax bid BKA BLE BM BMP B/P or BP BPH BR BRBPR BRP BS one two change degrees or hours before awake, alert, and oriented X4 abdomen arterial blood gas antecubital before meals American Diabetes Association activities of daily living as desired appropriate for age also known as above knee amputation albumin altered level of consciousness against medical advice ambulate amount anterior as tolerated aspirin arteriosclerotic heart disease axillary twice a day below knee amputation bilateral lower extremities bowel movement basic metabolic panel blood pressure benign prostatic hypertrophy bedrest bright red blood per rectum bathroom privileges bedside BS BSC BUN BX ℅ c Ca CA CABG CAD cap cath CBC CDB C/D/ I CHF cm CMP CMS CNS COPD CP CPM C&S CT CTA CVA CVD CXR DAT DJD DKA DM DOB DOE bowel sounds bedside commode blood urea nitrogen biopsy complains of, complaints of with calcium cancer coronary artery bypass graft coronary artery disease capsule catheter complete blood count cough and deep breath clean, dry, intact congestive heart failure centimeters complete metabolic panel circulation, movement, sensation central nervous system chronic obstructive pulmonary disease chest pain continuous passive motion culture and sensitivity computerized tomography clear to auscultation cerebrovascular accident cardiovascular disease chest X-ray diet as tolerated degenerative joint disease diabetic ketoacidosis diabetes mellitus date of birth dyspnea on exertion 84 DP dorsalis pedis drsg dressing DSD dry sterile dressing DVT deep vein thrombosis DX diagnosis ECF extended care facility ECG/EKG electrocardiogram ED emergency department EGDesophagogastroduodenoscopy ESRD end stage renal disease FA forearm FBS fasting blood sugar FC foley catheter FFP fresh frozen plasma F/U follow up FUO fever of undetermined origin FWB full weight bearing fx fracture GCS Glasgow coma scale GI gastrointestinal G-tube gastrostomy tube GU genitourinary HA headache Hct hematocrit HD hemodialysis Hgb hemoglobin H&H hemoglobin and hematocrit HOB head of bed HOH hard of hearing H&P history and physical HR heart rate hs at bedtime HTN hypertension I&D incision and drainage IDDM insulin dependent diabetes mellitus inc incontinent IM intramuscular I&O intake and output IS incentive spirometer IV intravenous J-tube jejunostomy tube JVD jugular vein distention K KCL KVO KUB L LE lg LLL LLQ LMP LUL LVN MAE mg MOM MRI MRSA MAR ml MM MVA Na NAD NCP NGT NIDDM NKA NS Nsg NPO N/V/D NWB O2 OA OBS OOB ORIF p potassium potassium chloride keep vein open kidneys, ureters, and bladder x-ray left lower extremity large left lower lobe (lung) left lower quadrant last menstrual period left upper lobe (lung) licensed vocational nurse moves all extremities milligrams milk of magnesia magnetic resonance imaging methicillin-resistant Staphylococcus aureus medication administration records milliliter mucous membranes motor vehicle accident sodium no apparent distress nursing care plan nasogastric tube non-insulin dependent diabetes mellitus no known allergies normal saline nursing nothing by mouth nausea, vomiting, diarrhea non-weight bearing oxygen osteoarthritis organic brain syndrome out of bed open reduction and internal fixation after 85 pc per PCN PCXR PEG PERL PERLA PERRLA PICC PMH po POD post pre PR PRN Pt PT PVD PWB q2h R R/O RR RUL RUQ Rx s sat SL SNF SOB S/P spec S/S SSE after meals by, or through Penicillin portable chest X-ray percutaneous endoscopic gastrostomy pupils equal and reactive to light pupils equal and reactive to light and accommodation pupils equal, round, reactive to light and accommodation peripherally inserted central catheter past medical history by mouth postoperative day after before per rectum as needed patient physical therapy peripheral vascular disease partial weight bearing every 2 hours right rule out regular rhythm right upper lobe (lung) right upper quadrant prescription without saturation sublingual skilled nursing facility shortness of breath status post specimen signs and symptoms soap suds enema SSRI STAT SW sx TCDB TDWB THA THR TIA T.O tol TWE TPN TSH TURP Tx UA UE UGI UO URI US UTI VO VRE WBAT WBC W/C W&D WNL VS selective serotonin reuptake inhibitor at once social worker symptom turn, cough, deep breathe touch down weight bearing total hip arthroplasty total hip replacement transient ischemic attack telephone order tolerated tap water enema total parentral nutrition thyroid stimulating hormone transurethral resection of the prostate treatment urinalysis upper extremity upper gastrointestinal urine output upper respiratory infection ultrasound urinary tract infection verbal order vancomycin-resistant enterococcus weight bearing as tolerated white blood cell wheelchair warm and dry within normal limits vital signs 86 Unapproved Abbreviations DO NOT USE AU cc D/C, DC IU MgSO4 MS MR HCTZ q qhs, qd, qod SQ or SC U or u µg OD OS OU per os ss each ear cubic centimeter discharge, discontinue international units Magnesium Sulfate Morphine Sulfate, Multiple Sclerosis, Mitral Stenosis Mitral Regurgitation, may repeat, medial record Hydrochlorothiazide every every hour sleep, every day, every other day subcutaneous unit microgram right eye left eye both eyes orally sliding scale Do not use slash marks to separate doses (/) (ex: 25 units/100ml). Use “per” Do not use “greater than” (>) or “less than” (<) marks. Spell out greater than or less than. When writing dosages, do not use zeros after the decimal point for doses in whole numbers (ex. 1mg). Always use a zero before the decimal point when the dose is less than a whole number (0.5mg) **For a complete list of Error –Prone abbreviations, visit the Institute of Safe Medication Practices website http://www.ismp.org/Tools/errorproneabbreviations.pdf 87 CERRITOS COLLEGE NURSING PROGRAM N210 CLINICAL SCHEDULE LONG TERM CARE WK DATE ASSIGNMENT EXPERIENCES 0800-1100 LTC Orientation Tour, Scavenger Hunt Facility information, Fire/disaster codes, clinical expectations, Clinical evaluation tool NPW/ Assessment Guide; Clinical Schedule and Student Assignments POSTCONFERENCE What is due? 6 1200-1500 PA Practicum Nothing 6 0650-1150 Caremaps and Meds for COPD Due Buddy with C.N.A. By the end of the day, choose 1 patient (1 diagnosis) for next week’s assignment and complete front and back page of NPW (include concept map); No Lab data Skills: baths, beds, feeding, assist with transfers, ROM, VS, NGT/GT feedings, positioning, hot/cold applications, bandages/binders, TED hose, restraints, enemas, isolation, Physical Assessment Foley Cath, Wound Care, NGT 1100-1150 NPW / Assessment Guide: sample/blank Clinical Experiences NPW: page 1 and page 2 including concept map due next Tuesday in pre-conference. Charting: VS, I&O 1330-1530 PA Practicum 88 7 0650-1250 Care of 1 patient NPW due in pre-conference Skills: baths, beds, feeding, assist with transfers, ROM, VS, NGT/GT feedings, positioning, hot/cold applications, bandages/binders, TED hose, restraints, enemas, isolation, Physical Assessment Foley Cath, Wound Care, NGT 1100-1150 Nothing NPW/ Assessment Guide Physical Assessment techniques Clinical Experiences and observations Charting: VS, I&O 7 0650-1250 SCP/NPW on VCE patient Due By the end of the day, choose 1 patient (2 Diagnoses) for next week’s assignment and complete front and back pages of NPW (include concept map) + medications; No Lab data Skills: Same as above 1100-1150 NPW / Assessment Guide: sample/blank Clinical Experiences NPW: page 1, & 2 including concept map, and page 4 (documentation) for the patient cared for this week due on Wed postconference 89 8 0650-1250 Skills: Same as above 1100-1150 NPW/ Assessment Guide Physical Assessment techniques Care of 1 patient NPW due in pre-conference By the end of the day, choose 1 patient (2 diagnoses) for next week’s assignment and complete front and back pages of NPW (include concept map) + medications and Lab data NPW: page 1-5 for patient cared for this week AND Assessment guide: all sections for physical mode for patient cared for this week due on Tues postconference SL 121 0700-1600 CPE: All skills Full Uniform 8 Nothing 9 0650-1250 Show this week’s completed NPW/AG to clinical instructor by end of day for feedback CPE Retesting Arrange Hours with Instructor 9 Skills: Same as above 1100-1150 NPW/ Assessment Guide Physical Assessment techniques Clinical Experiences and observations No Clinical All NPWs due in pre-conference to your clinical instructors which will be returned to you during clinical 90 Clinical Absence Make-Up Guidelines Make-up for any clinical absence in N210: 1. The student will be assigned by the instructor to write a paper on one of the diagnoses of the patient(s) that the student would have cared for on the missed day. 2. The student is to research the diagnosis using the library or internet to find a recent nursing journal (within last 5 years) about the diagnosis. 3. The article should include the following information related to: An explanation of the diagnosis Signs and Symptoms Risk factors/causes Diagnostic tests/measures Medical and Nursing treatment Evaluation of Outcomes 4. The student is to summarize the article, including in the summary all of the data stated in #3 (if possible). 5. The paper is to be typed. The paper and a copy of the article are to be turned in to the clinical instructor. If the absence is due to illness, the paper is to be turned in on the Monday after the illness. If the absence is due to being sent home for not being prepared, the paper is to be turned in the next day (ie: for a Tuesday absence, the paper is due on Wednesday) 6. The student may be asked to present the paper in post conference. 91 Cerritos College Department of Nursing NURS 210: Competency Performance Examination (CPE) Official Record of Student Performance Name of Student______________________________________ Vital Signs Competency Date________ Name of Clinical Examiner_______________________________ Pass___________ Fail_____________ Comments_____________________________________________ Retest Date___________Pass ___________Fail ______________ Comments _____________________________________________ Comprehensive Skill Competency Date___________ Name of Clinical Examiner_________________________________ Pass__________ Fail_______________ Check ALL competencies examined in this CPE: ___Universal competencies ___Occupied bed making ___Positioning of Patient ___Ambulating a patient ___Applying Bandages ___Applying Binders ___Applying antiembolism stockings ___Administering an enema ___NGT insertion +/- suction ___Sterile wet to moist dressing change ___Bed bath ___Range of Motion ___Transfer of Patient from bed to chair ___Moving a Patient up in bed ___Applying restraints ___Applying and removing PPE ___Irrigation (flush) of NGT/Gtube ___Administering intermittent/continuous tube feeding ___ Foley catheter insertion Legal Validation of Failure to Meet Critical Elements: In the case of failure of the comprehensive skill CPE, the examiner must cite the specific critical element(s) that the student did not pass and write the objective description of the reason for failure, using the space below (use additional lines as needed). ______________________________________________________________________ ______________________________________________________________________ ______________________________________________________________________ ______________________________________________________________________ Retest date_________________________ Pass_______ Fail________ Outcome of performance_________________________________________________ ______________________________________________________________________ ______________________________________________________________________ ______________________________________________________________________ 92 Cerritos College Department of Nursing The Universal Competencies and related clinical elements are supplied in all aspects of client care. The Universal Competencies which will be evaluated in N210 include: safety and security, standard precautions (asepsis), comfort and documentation. At the end of the clinical rotation, the student will be able to perform the following competencies and related critical elements: Universals: Safety and Security 1. Physical safety and security: Any action or inaction on the part of the student that threatens the patient’s well being or is in violation of the patient’s physical security. 2. Emotional security: Any action or inaction which threatens the emotional well being of the patient or significant others or is a violation of the patient’s emotional security. It is important to realize that all potential failures to protect the patient from harm can not be described here. Met ___ Not Met _______ ___ ________ ___ _____ Critical Elements 1. Identify assigned patient by reading ID bracelet before initiating care 2. Protect the patient from physical harm at all times, such as the following: a. Side rails are raised when indicated b. Bed is left in low position c. Patient’s ability to ambulate safely is assessed before beginning ambulation d. Restraints are secure, when required, without injuring patient 3. Protect the patient and significant other from psychological harm by the following actions: a. Refer to the patient by designated or preferred name b. Communicate verbally and non-verbally in professional manner c. Communicate verbally and non-verbally in a manner that does NOT express anger, distrust, abuse, familiarity or demeaning behaviors to the patient and/or significant others. d. Provide accurate information to patient and/or significant others e. Keep all patient-related information professionally confidential f. Maintain patient’s personal privacy at all times g. Explain procedure to patient prior to initiating skill 93 Standard Precautions: The prevention of the introduction or transfer of organisms Met ___ Not Met _______ ___ ________ ___ ___ ___ ___ ________ ________ _______ ________ ___ ________ Critical Elements 1. Wash hands before initiating direct contact with patient and whenever hands are contaminated by patient’s body secretions or substances. (During an examination wash hands in presence of examiner before beginning care.) 2. Wear gloves whenever coming in contact with human secretions 3. Protect patient from contamination. 4. Protect self and others from contamination 5. Confine contaminated material to contaminated areas. 6. Dispose of contaminated materials in designated containers, 7. Implement any designated special precautions as required Comfort: The assessment of and interventions related to the patient’s tolerance of the procedure. Met ___ Not Met _______ ___ _______ Critical Elements 1. Assess the patient’s comfort level before, during and after a potentially uncomfortable procedure. 2. Provide interventions to increase the patient’s comfort level Documentation: The recording of data required by, or pertinent to, the designated situation. Met ___ Not Met _______ ___ ________ ___ ________ ___ _______ Critical Elements 1. Document patient care using the following methods, as designated: a. assessment forms, flow graphs, or other standard clinical forms b. narrative process recording 2. Document patient changes and responses to care in designated records. 3. Use language, terms, and abbreviations that are consistent with professional standards, agency protocols, and other specific guidelines 4. Record data so that entries are: a. clear b. accurate c. precise d. pertinent/relevant 94 Competencies Specific to N210: Fundamentals of Nursing 1. Vital Signs: to measure the blood pressure, pulse, respirations, temperature and pulse oximetry of a patient Met Not Met Critical Elements: ___ _______ ___ ___ ___ ___ ___ ______ ______ ______ ______ ______ 1. Measure vital signs accurately a. within +/- 4 mmHg of systolic and diastolic blood pressure b. within +/- 4 bpm of pulse c. within +/- 2 of respirations per minute 2. Prepare and place thermometer correctly 3. Count irregular and apical pulse for one minute 4. Count irregular respiration for one minute 5. Use correct size blood pressure cuff 6. Correctly identify location of apical pulse 2. Handwashing: reducing microbial load on hands with the use of water and soap. Met Not Met Critical Elements: ___ ___ _______ _______ ___ ___ _______ _______ 1. Regulate water temperature and flow 2. Lather with soap covering all aspects of hands and wrists for appropriate length of time 3. Dry hands 4. Maintain medical asepsis and do not contaminate self 3. Occupied bedmaking: to change the soiled sheets on a bed occupied by a patient Met Not Met Critical Elements: ___ ___ ___ ___ _______ _______ _______ _______ 1. 2. 3. 4. ___ ___ _______ _______ ___ _______ Maintain medical asepsis of linen Place bed at working level for height Keep patient covered at all times Maintain proper positioning of patient and body mechanics of nurse. 5. Create mitered corner and foot tent 6. Center top sheet and bedspread to hang equally on both sides 7. Place clean pillowcase on pillow 4. Range of Motion: to move patient’s joints actively or passively through set movements Met Not Met Critical Elements: ___ ___ ___ _______ _______ _______ 1. Proceed systematically from head to toe 2. Support joint being exercised 3. Perform exercise 3-5 times 95 5. Transfer of patient from bed to chair: assisting a patient to change locations Met Not Met ___ _______ ___ ___ _______ _______ ___ ___ ___ _______ _______ _______ Critical Elements: 1. Assess patient’s ability to assist; presence of weaknesses or paralysis; cognitive function 2. Maintain use of good body mechanics by the nurse 3. Maintain proper body alignment of the patient during Changes in position by supporting weak limbs 4. Position bed at working level for height 5. Demonstrate appropriate use of gait belt 6. Position wheelchair at appropriate angle and locked 6. Moving a patient up in bed: assisting a patient to a higher position in a hospital bed, so that the patient bends at the appropriate place Met Not Met ___ ___ ___ ___ _______ _______ _______ _______ Critical Elements: 1. 2. 3. 4. Assess the patient’s ability to assist Position a draw sheet under the patient appropriately Use proper body mechanics Properly instruct the patient how to assist 7. Applying restraints : Apply a device that limits movements of an extremity or body part Met Not Met ___ ___ ___ ___ _______ ________ ________ ________ ___ ________ Critical Elements: 1. 2. 3. 4. Assess CSM or any contraindications to use Explain rationale to patient and/or family Apply restraint properly Secure restraint to proper location on bed or wheelchair as appropriate 5. Assess at frequency dictated by agency policies 8. Applying and removing personal protective equipment: use of materials that are worn to decrease the transmission of microbes Met Not Met ___ ___ ___ _______ _______ _______ Critical Elements: 1. Identify needed equipment 2. Apply appropriate equipment in proper order 3. After use, remove protective equipment in proper order to Prevent contamination 9. Administering an Enema: instilling a solution per rectum Met ___ ___ ___ ___ Not Met _______ _______ _______ _______ Critical Elements: 1. Use warm water 2. Position patient to facilitate flow 3. Regulate flow of water to appropriate rate 4. Offer and place patient on bedpan after instillation 96 10. Nasogastric tube insertion +/- suction to insert a catheter through the nose into the stomach and attach to suction if ordered Met Not Met ___ ___ ___ _______ _______ _______ ___ ___ ___ ___ ___ _______ _______ _______ _______ _______ Critical Elements: 1. Measure tube for appropriate positioning 2. Lubricate the tube 3. Instruct the patient regarding procedure and patient participation 4. Facilitate chin tuck when appropriate 5. Insert the tube to the appropriate place 6. Check placement 7. Secure the tube 8. Attach tube to suction appropriately 11. Sterile Wet to moist dressing change: Met Not Met ___ ___ ___ ___ ___ ___ _______ _______ _______ _______ _______ ______ Critical Elements: 1. 2. 3. 4. 5. 6. Remove and assess old dressing Assess wound and drainage thoroughly and accurately Establish sterile field & properly apply sterile gloves Cleanse wound correctly using sterile technique Pack wound and apply dressing using sterile technique Secure dressing 12. Bed bath: to clean the body of a patient that remains in bed Met Not Met Critical Elements: ___ ___ _______ _______ ___ _______ ___ ___ _______ _______ 1. Prepare supplies using medical asepsis 2. Maintain proper body positioning of the patient and good body mechanics of the nurse; minimizing movements of the patient and nurse 3. Keep patient covered to maintain modesty and prevent chilling 4. Clean from head to toe; perineal area last 5. Change water when appropriate 13. Positioning a Patient: assisting a patient into positions used therapeutically in nursing practice Met Not Met ___ _______ ___ ___ _______ _______ Critical Elements: 1. Maintain use of good body mechanics for the nurse and patient 2. Use pillows appropriately for support 3. Support body during position changes as appropriate 97 14. Ambulating a patient: providing a one person assistance to walk Met Not Met ___ ___ _______ _______ ___ _______ Critical Elements: 1. Assess patient’s ability to ambulate 2. Correctly position self and arms to provide for assistance and safety 3. Evaluate patient’s gait, distance and tolerance of exercise 15. Applying bandages : Apply a device that provides support to a designated area/joint Met Not Met ___ ___ ___ ___ ___ ___ ___ _______ _______ _______ ______ _______ _______ ______ Critical Elements: 1. 2. 3. 4. 5. 6. 7. Assess CSM Position body part in neutral, elevated position if possible Apply bandage using equal distance and equal pressure Use the proper wrapping technique for the body part Wrap the extremity distal to proximal Secure appropriately Reassess CSM 16. Applying binders : Apply a device that provides support to the abdomen and/or torso Met Not Met ___ ___ ___ _______ _______ _______ Critical Elements: 1. Choose proper sized binder for the patient 2. Position the binder appropriately 3. Assess for potential breathing or skin impairment 17. Applying antiembolism stockings : Apply a device that promotes the return of blood to the heart Met Not Met ___ ___ ___ _______ _______ _______ Critical Elements: 1. Measure patient for proper fit 2. Apply the stocking appropriately 3. Assess CSM and presence of wrinkles in stockings 18. Intermittent and continuous tube feeding administration: administering a set amount of tube feeding solution via a NGT, G-tube, or J-tube. Met Not Met ___ ___ ___ ___ ___ _______ _______ _______ _______ ______ Critical Elements: 1. 2. 3. 4. 5. Position HOB at least 30º unless contraindicated Check placement and patency of tube Perform residual check; hold if residual >100 mL Administer correct type and amount at prescribed rate Keep HOB at least 30° for at least 1 hour after feeding for intermittent feedings and maintain HOB always at least 30°for continuous feedings 98 19. Foley catheter insertion: to insert a catheter into bladder utilizing sterile technique Met Not Met ___ ___ ___ ___ ___ ___ ______ _______ _______ _______ _______ _______ Critical Elements: 1. 2. 2. 3. 4. 5. Establish sterile field Properly apply sterile gloves Check foley balloon (optional if using BARD catheter kit) Cleanse perineum correctly Insert catheter maintaining sterile technique Inflate foley bulb at appropriate location & holds on to catheter during inflation 20. Irrigation (flush) of NGT/Gtube to instill water or saline into NGT/Gtube Met ___ ___ ___ ___ ___ Not Met ______ _______ _______ _______ _______ 1. 2. 3. 4. 5. Critical Elements: Stop current feeding or suction (as applicable) Check tube placement Aspirate for residual Instill prescribed solution and amount using appropriate method Resume feeding or suction (as applicable) 99