PRINCE GEORGE`S HOSPITAL CENTER
advertisement

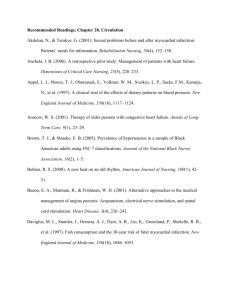
PRINCE GEORGE’S HOSPITAL CENTER INTERNAL MEDICINE RESIDENCY PROGRAM SECTION 12: GERIATRICS This section has been reviewed and approved by the Chief, Division of Geriatrics as well as the Program Director, Internal Medicine Residency Program at Prince George’s Hospital Center. ________________________ Chief, Division. Of Geriatrics ______________________________ Program Director, Residency Program I. Overview The care of older adults is a substantial and growing component health care services. The number of elderly, with their burden of chronic disease, is increasing competency in clinical geriatrics involves recognizing the difference in presentation of disease and the importance of maintaining functional independence in elderly patients. With increasing age, presentations of disease become less classic and are often muted, and timely recognition requires attentiveness to subtle signs. Appropriate management requires a balance of patient observation, judicious diagnostic intervention and acceptance of limits as defined by the patient. Effective management of problems may be complex and may necessitate an interdisciplinary approach that takes social support into account. Medical and psychological problems, acute and chronic, frequently co-exist. Many competencies of geriatrics are included within lists for other disciplines. They are repeated here to reflect the unique set of skills required to manage specific problems when they occur in the elderly. II. Principle Teaching Methods This consists of direct patient care in both inpatient and outpatient settings in area nursing homes and Geriatrician offices as well as a multidisciplinary view of care of the elderly: 1. . Issues related to end of life and hospice are taught in an area Hospice Center through lectures and patient care including home visits. 2. The residents also follow a Physiatrist and observe several evaluation techniques including swallow evaluations, cognitive evaluation, gait and balance evaluation etc. 3. In the inpatient nursing home setting the goal is to emphasize the multiple health care needs of the elderly and learn management of acute and chronic disease processes. Skilled care includes rehabilitation services (physical, occupational, and speech therapy), wound and ostomy care, patient education, certain types of intravenous and injection therapy, pain control, and medical observation. The nursing and social work staff serves a pivotal role by continually reassessing patient status and initiating appropriate changes in the treatment and discharge plans. 4. Psychiatric illnesses in the elderly can present atypically and often misdiagnosed. For example patients with depression may be diagnosed as dementia and patients with thyroid problems may be diagnosed with depression or dementia. Internists must also be aware of risk factors that cause depression in elderly like loneliness or loss of a loved one. The residents therefore round with a staff psychiatrist and learn interviewing and screening techniques for psychiatric illnesses as well as management of psychiatric disorders. 5. Ophthalmologic issues are important in the elderly. Loss of vision, its evaluation and impact on the elderly are discussed during the encounters in the area ophthalmologists office. 6. Endocrine issues related to metabolic bone disease and other endocrine abnormalities in the elderly are discussed while shadowing an area endocrinologist. The residents must make a double sided copy of their geriatrics attendance sheet at the beginning of the rotation. This sheet must be signed by the attending physician for each encounter. Topics discussed during the encounter must be marked. A completed sheet must be submitted to the program coordinator at the end of the rotation to obtain credit for the rotation. Attendance > 75% in each part of the rotation is required for satisfactory completion of the rotation. Any missed encounters must be explained in writing at the end of the month. Residents will also learn regarding the field throughout the year by taking care of geriatric patients admitted to the hospital or being followed up at the Glenridge Medical center and from a series of lectures scheduled throughout the year, conducted by geriatrician and focusing on issues like: Dementia Delirium Incontinence Decubutis Ulcers III. Strengths and Limitations Residents learn from direct interaction with the multiple subspecialties involved in the care of the elderly. At the nursing home and outpatient rehabilitation center resident learns management of multiple medical problems, polypharmacy, nutritional assessment, wound care, urinary incontinence. They also learn about a multidisciplinary approach to patient care especially with respect to nutrition, patient safety and functional ability. IV. Goals and Objectives for Geriatrics Rotation Legend for Learning Activities Learning Venues: 1. Direct patient care: supervised by attending physician 2. Management rounds at Nursing Home 3. Didactic Lectures including Core Lecture Series 4. Self Study Evaluation Methods: A. Attending evaluation B. Direct Clinical Observation C. Nursing Evaluation D. In-Training Examination Learning Venues* Evaluation Methods 1,2 A, B 1,2 A, B 1,2 A,B 1,2 A,B,D ALL A,B,D Learning Venues* Evaluation Methods ALL A,B,D ALL A,B Learning Venues* Evaluation Methods ALL A, B Meet with Program Director A, B, D Learning Venues Evaluation Methods 1,2 A,B,C ALL ALL 1,2,3 A, B, C Learning Venues* Evaluation Methods 1,2,3 A,B,C 1,2,3 A,B,C Competency: Systems-Based Practice Learning Venues Evaluation Methods Understand and utilize the multidisciplinary resources necessary to care optimally for hospitalized and out 1,2 A,B,C Competency: Patient Care Interview patients more skillfully, gathers accurate and essential information with emphasis on geriatric illness Examine patients more skillfully with competent and complete observation of normal and abnormal signs, particularly in the elderly population Define and prioritize patient’s medical problems, recognizing the special presentation of illness in the elderly Generate and prioritize differential diagnoses with appropriate testing and therapeusis Develop rational, evidence-based management strategies Competency: Medical Knowledge Expand clinically applicable knowledge base of the basic and clinical sciences underlying the care of medical service patients, both out and inpatients. Access and critically evaluate current medical information and scientific evidence relevant to geratric care Competency: Practice-Based Learning and Improvement Identify and acknowledge gaps in personal knowledge and skills in the care of hospitalized and out patients, paticularly the elderly Develop and implement strategies for filling gaps in knowledge and skills and minimize errors Competency: Interpersonal and Communication Skills Communicate effectively with patients and families, with particular emphasis on explanation of complex and multi-system illness and the testing required to confirm diagnostic possibilities Communicate effectively with physician colleagues at all levels with appropriate consultation when needed Present patient information concisely and clearly, verbally and in writing. Adhere to confidentiality. Competency: Professionalism Demonstrate respect, compassion, integrity and altruism towards patients, families, colleagues, and all members of the health care team Demonstrate sensitivity to confidentiality, gender, age, cultural differences and disabilities patients and the limitations of various practice environments. Collaborate with other members of the health care team to assure comprehensive patient care Use evidence-based, cost-conscious strategies in the care of hospitalized and outpatients 1,2 A,B,C ALL A,B,D V. Educational Content A. Physical Medicine and Rehabilitation When possible, patient’s rehabilitation sessions are schedule so that the resident can be present. Physical, occupational, and speech therapists teach the resident their assessment and treatment approaches to patient problems, both general (e.g., gait instability, cognitive impairment) and particular (e.g., hip fracture, stroke). Residents should develop an understanding of the components of a Rehabilitation Prescription, and the indications of Rehabilitation Team Referrals. They will also gain familiarity of Physical Medicine methods for management of: 1) Falls 2) Gait disorders: Understand impairment, disability and handicap terms 3) Poor safety awareness 4) Sundowning 5) :Low back pain, Radiculopathy 1) Electrodiagnostic Evaluation of the Peripheral Nervous System: Understand basics of test and its clinical indications 6) Contractures, Degenerative joint diseases 7) Cognitive dysfunction and its evaluation 8) Functional assessment Comprehensive Rehabilitation Evaluation of Function Familiarity with Quantitative Methods of Patient Functional Evaluation 9) Gait assessment 10) Home safety assessment Motor vehicle driving assessment Needs assessment on hospital discharge, including rehabilitation Audiology Neuropsychiatric testing Videofluoroscopy for swallowing problems B. Ophthalmology Eye problems are common in the elderly population. They could result as a consequence of systemic illnesses (like diabetic retinopathy) or as a result of aging itself (cataract). They are important issues that impact their ability to live and /or function independently. 1) Vision loss: acute and chronic Cataracts Glaucoma Macular degeneration Optic atrophy Visual field and acuity testing 2) Common disorders of the eyelid Blepharitis Chalazion 3) Floaters and visual phenomenon and fundoscopic evaluation (where appropriate) of: Retinal/ vitreous detachment Diabetic retinopathy Subconjunctival hemorrhage 4) Injuries Foreign bodies, external and superficial Orbital fracture 5) Infections and inflammation Conjunctivitis Uveitis Schleritis Keratitis Optic neuritis Eye involvement in giant cell arteritis Orbital or periorbital cellulitis 6) Eye pain/photophobia and work up Increased intraocular pressure Retinal artery or vein occlusion Corneal abrasion with fluorescein stain and slit lamp 7) Systemic effects of ophthalmic medications 8) Dry eye syndromes C. Psychiatry Psychiatric illnesses in the elderly can present atypically and often misdiagnosed. For example patients with depression may be diagnosed as dementia and patients with thyroid problems may be diagnosed with depression or dementia. Internists must also be aware of risk factors that cause depression in elderly like loneliness or loss of a loved one. The residents therefore round with a staff psychiatrist and learn interviewing and screening techniques for psychiatric illnesses as well as management of psychiatric disorders. 1) Substance Abuse and Related Disorders 2) Delirium 3) Delusions, Hallucinations 4) Dementia, Cognitive disorders 5) Depression, Bipolar disorder, dysthymia, Suicide risk 6) Fatigue 7) Late-onset psychotic disorders 8) Neurobehavioral disorders Agitation Psychosis Anxiety Confusion 9) Social isolation Adjustment disorders (grief, life-cycle changes) Poor hygiene or self-care 10) Personality disorders 11) Schizophrenia 12) Insomnia and other Sleep disorders 13) Humanistic Approach of Patient Care/Social Issues 14) Mental status examination, including standardized cognitive examinations (e.g. Mini Mental State Exam) when indicated. 15) Neuropsychologic evaluation D. Endocrine / metabolic Endocrine issues are common in elderly. Residents learn about special issues in management of chronic medical problems (like brittle diabetes) and issues related to problems with memory and mobility (uncontrolled blood sugars, dehydration). Wellness is also an important aspect of elder care and residents learn about important issues like osteoporosis by shadowing an endocrinologist one half day a week. 1) Dehydration Hypernatremia Hyponatremia 2) Diabetes mellitus, type 2 3) Disorders of temperature regulation 4) Thyroid Disorder Hyperthyroidism Hypothyroidism Multinodular goiter Sick euthyroid state 5) Failure to Thrive 6) Metabolic bone disease, Osteoporosis E. End of Life Care (Hospice Care) An important aspect of general internist practice is care at end of life. Resident learn how to compassionately manage patients and deal with issues related to end of life by shadowing at an area Hospice Center with a focus on: 1) Death and Dying 2) Bereavement 3) Bowel obstruction 4) Dyspnea 5) Pain Management 6) Nutrition 7) Treating the caregiver 8) Medico-legal and Ethical Issues may also be discussed like Elder Abuse Advance directives Health care proxy Unrealistic expectations of family and patient Evaluating decision making capacity The following issues will be addressed on a case by case basis by discussions with the supervising Geriatrician in the Nursing Home, Rehabilitation Center and Outpatient Offices: F. Cardiovascular 1) Angina/Myocardial infarction 2) Atrial fibrillation 3) Congestive heart failure 4) Hypertension 5) Lower-extremity edema 6) Orthostatic hypotension 7) Peripheral vascular disease G. Gastroenterology 1) Colon Cancer 2) GI bleed 3) Constipation, obstipation 4) Diverticular disease 5) Fecal incontinence 6) GERD 7) Ischemic bowel 8) Swallowing disorders H. Hematology 1) Anemia of chronic disease 2) Iron deficiency anemia 3) Leukemias and lymphproliferative disorders 4) Multiple myeloma I. Iatrogenic Disease 1) Adverse drug reactions 2) Nosocomial complications 3) Polypharmacy, drug interactions 4) Procedure complications J. Neurologic/ sensory 2) Carotid artery disease 3) Normal pressure hyprocephalus 4) Parkinson’s disease 5) Spinal stenosis 6) Stroke 7) Transient ischemic attack 8) Dementia Alzheimers Multi-infarct Thyroid disease related Infectious disease related (neurosyphilis etc.) 9) Hearing loss Cerumen impaction Presbycusis 10) Peripheral neuropathy 11) Syncope 12) Dizziness 13) Vestibular disorders 14) Sleep disorders K. Nutrition 1) Aspiration 2) Feeding disorders 3) Malnutrition, under nutrition 4) Oral health problems L. Renal/Urologic 1) Age related changes in renal function Adjusting medication dose for patient’s GFR 2) Prostate disease Benign Prostatic Hypertrophy Prostate Cancer Role of PSA 3) Sexual dysfunction 4) Urinary incontinence 5) Urinary retention Evaluating results of urodynamic studies 6) Urinary tract infection Catheter related infections M. Rheumatologic/Musculoskeletal 1) Contractures 2) Crystal diseases (gout, pseudogout) 3) Deconditioning 4) Degenerative joint disease 5) Fractures Hip Vertebral compression fracture Wrist 6) Giant cell arteritis 7) Immobility 8) Low back pain 9) Osteoporosis 10) Polymyalgia rheumatica 11) Spinal stenosis 12) Subacromial bursitis 13) Trochanteric bursitis N. Skin 1) 2) 3) 4) 5) Pressure ulcers Cancers Pruritis Seborrhic keratosis Xerosis O. Tuberculosis 1) Interpreting PPD results in nursing home patients 2) INH prophylaxis: indications, monitoring, duration 3) Treatment VI. Recommended Reading All residents are encouraged to read the Geriatrics section from the MKSAP during their month long rotation as well as read on topics on a case-by-case basis. Other resources are as follows: 1) Bentley DW, Bradley S, High K, et al. Practice guideline for evaluation of fever and infection in long-term care facilities. Clin Infect Dis. 2000; 31:640-53 2) Chang JT, Morton SC, Rubenstein LZ et al. Interventions for the prevention of falls in older adults: systematic review and meta-analysis of randomised clinical trials. BMJ. 328(7441):680, 2004 Mar 20 3) Fick DM, Cooper JW, Wade WE, et al. Updating the Beers Criteria for Potentially Inappropriate Medication Use in Older Adults. Arch Intern Med. 2003;163:2716-2724 4) Finucane TE, Christmas C, Travis K. Tube feeding in patients with advanced dementia: A review of the evidence. JAMA 1999;282(14):1365-70. 5) Matulonis UA. End of life issues in older patients. Seminars in Oncology. 31(2):27481, 2004 Apr. 6) Mui AC. The Program of All-Inclusive Care for the Elderly (PACE): an innovative long-term care model in the United States. Journal of Aging & Social Policy. 13(23):53-67, 2001. 7) Scientific Committee of the First International Consultation on Incontinence. Assessment and treatment of urinary incontinence. Lancet 355(9221):2153-2158. 8) Small GW, Rabins PV, Barry PP, et al. Diagnosis and treatment of Alzheimer disease and related disorders. Consensus statement of the American Association for Geriatric Psychiatry, the Alzheimer’s Association, and the American Geriatrics Society. JAMA 1997;278:1363-71 9) Wrenn K. Fecal Impaction. NEJM 1989;321(10):658-662 10) Practical Functional Assessment of the Elderly Person: A Primary Care Approach. Fleming KC. Mayo Clin Proc 1995.890-910. 11) Preventive Services in the Adult Aged 65 and Older. HuffmanGB. Clinics in Family Practice.June 2000. 12) The Geriatric Patient: A Systematic Approach to Maintaining Health. Miller KE. American Family Physician. February 2000.1089-1104. 13) Preventing Falls in Elderly Persons. Tinetti ME. N Engl J Med. January 2003. 42-49. 14) Falls in the Elderly. FullerGF. American Family Physician.2000.2159-68. 15) Inappropriate Medications for Elderly Patients. Chutka D Mayo Clin Proc 2004.122139. 16) The Medicare Program. www.medicare.gov 17) Constipation and Fecal Incontinence in the Elderly Population. Romero Y. Mayo Clin Proc 1996.81-92. 18) The Pathophysiology of Urinary incontinence Among Institutionalized Elderly Persons. Resnick N. N Engl J Med 1989.1-7. 19) Urinary Incontinence in the Elderly Population. Chutka D. Mayo Clin Proc 1996.93101. 20) Cancer Screening in Elderly Patients. Walter LC. JAMA. 2001.2750-56. 21) Pressure Ulcers: Prevention and Management. Evans JM. Mayo Clin Proc 1995.789799. 22) Depression in the elderly: Tailoring medical therapy to their special needs. Raj A. Postgraduate Medicine, June 2004; 115(6) 23) Delirium in Elderly Patients: Evaluation and Management. Rumnans TA. Mayo Clin Proc 1995. 989-998. 24) Alzheimer Disease. Cummings JL. JAMA 2002.2335-38. 25) Physician Evaluation and Management of Nursing Home Residents. Ouslander JG. Ann Intern Med 1994. 584-592. 26) Hazards of Hospitalization of the Elderly. Creditor MC. Ann intern Med 1993.219223. PRINCE GEORGE’S HOSPITAL CENTER INTERNAL MEDICINE RESIDENCY PROGRAM GERIATRICS ROTATION SCHEDULE SHEET Monday 8:00am 9:00am-12:00am Morning Report Psychiatry Rounds 12:00-1:00 pm 1:00pm-5:00pm Noon Conference Physical medicine 8:00am St. Thomas More Nursing & Rehab Center OAO Maryland Trade Center Tuesday 1:00pm Wednesday Thursday 7:30am Ophthalmology PGHC Conference Rm. Dr Bangura 301-437-7992 PGHC Conference Rm Dr. Kulkarni Dr. Devore Dr. Turkewitz (301) 345-5857 Dr. Malouf (301) 423-5252 1:30pm Nursing home Dr. Husain, Saadia 301-580-6732 8am-12:00 N Endocrinology Dr. Sotoudeh 301-474-0400 Multidisciplinary rounds with Dr Devore and write notes Friday 1:30pm Gladys Spellman 9:00am Urology Dr. Ajrawat, Harbhajan 301-772-3434 12:00-1:00 pm Noon Conference PGHC Conference Rm 1:30pm Glenridge clinic Weekly clinic St. Thomas More Nursing & Rehab Center Gladys Spellman Speciality Hospital 4922 LaSalle Road 2900 Mercy Lane Hyattsville, MD 20782 Cheverly, Maryland 20785 301-864-2333 301-618-2010 Dr. Turkewitz’s Office Dr F. Sotoudeh OAO Maryland Trade Center 4th Fl 7525 Greenway Center Drive, Ste 209 7500 Greenway Center Drive Greenbelt, MD 20770 Greenbelt, MD 20770 301-474-0400 301-345-5857 Dr. H. Ajrawat 6126 Landover Road Cheverly, MD 20785 301-772-3434 Dr. George Malouf 5210 Auth Road Camp Springs, MD 20746 301-423-5252 PRINCE GEORGE’S HOSPITAL CENTER INTERNAL MEDICINE RESIDENCY PROGRAM GERIATRICS ROTATION ATTENDANCE SHEET RESIDENT NAME________________________________________________________ PGY LEVEL_______________ ROTATION MONTH_____________ Psychiatry: Please discuss topics listed under the subsection of Psychiatry in the Geriatrics Curriculum. MUST DISCUSS THE MINI MENTAL EXAM Date Topic Discussed Signature Gladys Spellman Nursing Home: Please discuss topics listed under the Educational Content of the Geriatrics Curriculum Date Topics Discussed Signature St Thomas More Nursing And Rehab Center: Please discuss topics listed under the Educational Content of the Geriatrics Curriculum Date Topics Discussed Signature Dr. Turkevitz office: Please discuss topics listed under the Educational Content of the Geriatrics Curriculum Date Topic Discussed Signature RESIDENT NAME______________________________________ Dr. Malouf’s Office: Please discuss one of the topics listed under the subsection of Ophthalmology in the Geriatrics Curriculum . Date Topics Discussed Signature Dr Sotoudeh’s office: Please discuss one of the topics listed under the subsection of Endocrinology in the Geriatrics curriculum Date Topics Discussed Signature Physical Medicine: Please discuss one of the topics listed under the subsection of physical medicine in the Geriatrics curriculum. MUST DISCUSS COGNITIVE EVALUATION Date Topics Discussed Signature Urology: Please discuss some topics in urology. Especially discuss about urinary incontinence and erectile dysfuction, and prostate cancer. Date Topics Discussed Signature