Flu Shot Waiver Info Sheet - Professional Pediatric Home Care
advertisement
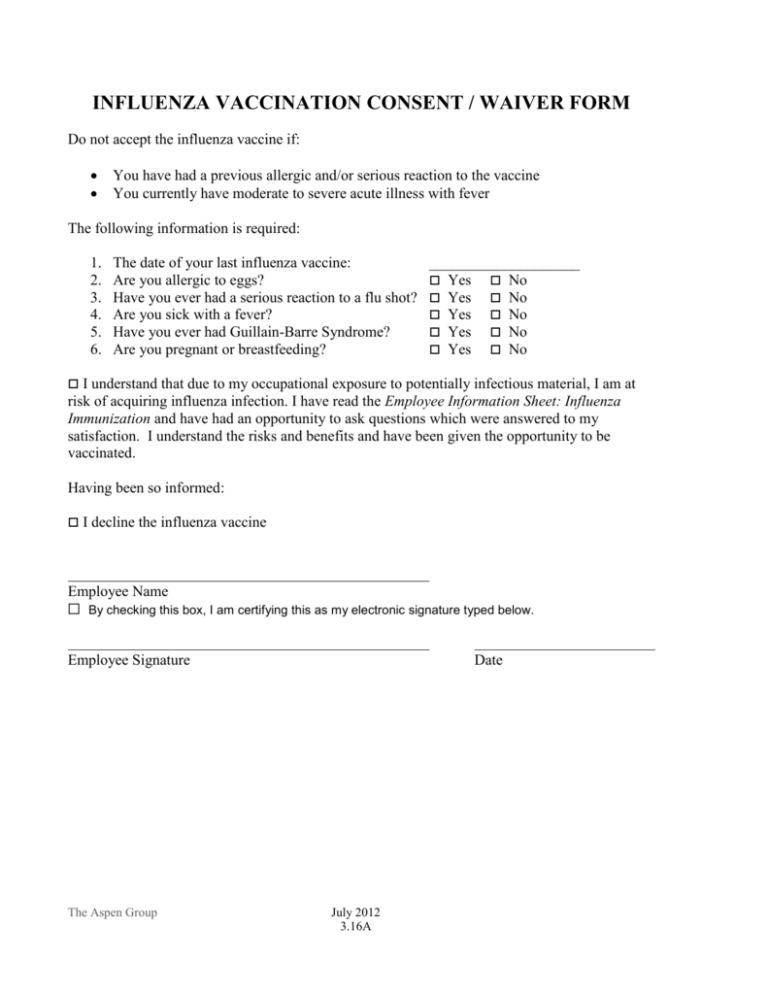
INFLUENZA VACCINATION CONSENT / WAIVER FORM Do not accept the influenza vaccine if: You have had a previous allergic and/or serious reaction to the vaccine You currently have moderate to severe acute illness with fever The following information is required: 1. 2. 3. 4. 5. 6. The date of your last influenza vaccine: Are you allergic to eggs? Have you ever had a serious reaction to a flu shot? Are you sick with a fever? Have you ever had Guillain-Barre Syndrome? Are you pregnant or breastfeeding? ____________________ Yes No Yes No Yes No Yes No Yes No I understand that due to my occupational exposure to potentially infectious material, I am at risk of acquiring influenza infection. I have read the Employee Information Sheet: Influenza Immunization and have had an opportunity to ask questions which were answered to my satisfaction. I understand the risks and benefits and have been given the opportunity to be vaccinated. Having been so informed: I decline the influenza vaccine Employee Name ☐ By checking this box, I am certifying this as my electronic signature typed below. Employee Signature The Aspen Group Date July 2012 3.16A Employee Information Sheet: Influenza Immunization Healthcare entities and healthcare workers have a shared responsibility to prevent the spread of infection and avoid causing harm to their patients by taking reasonable precautions to prevent the transmission of vaccine-preventable diseases. Vaccine programs are, therefore, an essential part of infection prevention and control for slowing or stopping the transmission of seasonal influenza viruses from adversely affecting those individuals who are most susceptible. Influenza is primarily a community-based infection that is transmitted in households and community settings. Each year, 5% to 20% of U.S. residents acquire an influenza virus infection, and many will seek medical care in ambulatory healthcare. In addition, more than 200,000 persons, on average, are hospitalized each year for influenza-related complications. Healthcare-associated influenza infections can occur in any healthcare setting and are most common when influenza is also circulating in the community. Uncomplicated influenza illness is characterized by the abrupt onset of constitutional and respiratory signs and symptoms (e.g., fever, myalgia, headache, malaise, nonproductive cough, sore throat, and rhinitis). Preventing transmission of influenza virus and other infectious agents within healthcare settings requires a multi-faceted approach. Spread of influenza virus can occur among patients, health care providers, and visitors; in addition, health care providers may acquire influenza from persons in their household or community. The most effective strategy for preventing influenza is annual vaccination. Achieving high influenza vaccination rates of health care providers and patients is a critical step in preventing healthcare transmission of influenza from health care providers to patients and from patients to health care providers. According to current national guidelines, unless contraindicated, vaccination is recommended for all people aged 6 months and older, including health care providers, patients and residents of long-term care facilities. During the care of any patient, all health care providers in every healthcare setting should adhere to standard precautions, which are the foundation for preventing transmission of infectious agents in all healthcare settings. Standard precautions assume that every person is potentially infected or colonized with a pathogen that could be transmitted in the healthcare setting. Elements of standard precautions that apply to patients with respiratory infections, including those caused by the influenza virus include, but are not limited to: Frequent hand hygiene, including before and after all patient contact, contact with potentially infectious material, and before putting on and upon removal of personal protective equipment, including gloves. Wearing gloves for any contact with potentially infectious material. Remove gloves after contact, followed by hand hygiene. Wearing gowns for any patient-care activity when contact with potentially infectious material (including respiratory) is anticipated. Remove gown and perform hand hygiene before leaving the patient's environment. The Aspen Group July 2012 3.16A Droplet precautions should be implemented for patients with suspected or confirmed influenza for 7 days after illness onset or until 24 hours after the resolution of fever and respiratory symptoms, whichever is longer. In some cases, agencies may choose to apply droplet precautions for longer periods based on clinical judgment, such as in the case of young children or severely immuno-compromised patients, who may shed influenza virus for longer periods of time. Health care providers at higher risk for complications from influenza infection include pregnant women and women up to 2 weeks postpartum, persons 65 years old and older, and persons with chronic diseases such as asthma, heart disease, diabetes, diseases that suppress the immune system, certain other chronic medical conditions, and morbid obesity. Vaccination and early treatment with antiviral medications are very important for HCP at higher risk for influenza complications because they can decrease the risk of hospitalizations and deaths. HCP at higher risk for complications should check with their healthcare provider if they become ill so that they can receive early treatment. The influenza vaccine has the potential to cause serious problems, such as severe allergic reactions. The risk of the vaccine causing serious harm, or death, is extremely small. Serious problems from influenza vaccine are very rare. The virus is inactivated, preventing transmission of influenza from the vaccine. Mild reactions: o soreness, redness, or swelling at the injection site o fever o aches o If these problems occur, they usually begin soon after the shot and last 1-2 days Severe reactions: o Life-threatening allergic reactions are very rare. If they do occur, it is usually within a few minutes to a few hours after the injection. o In 1976, a type of influenza (swine flu) vaccine was associated with Guillain-Barre Syndrome (GBS). Since then, flu vaccines have not been clearly linked to GBS. However, if there is a risk of GBS from current flu vaccines, it would be no more than 1 or 2 cases per million people vaccinated. This is much lower than the risk of severe influenza, which can be prevented by vaccination. Between October 1st and March 31st each year, the influenza vaccine is available all Agency employees who have direct contact with patients. If you have a medical condition, allergies, are pregnant or breastfeeding, please consult your physician for direction prior to receiving the vaccine. The Aspen Group July 2012 3.16A



