Travellers` Diarrhoea (TD)
advertisement

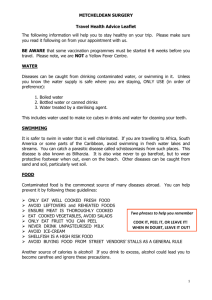
TRAVEL GUIDELINES Travellers’ Diarrhoea (TD) This is the most common illness that you will be exposed to abroad; 20-60% of travellers are affected. Although there are vaccines available for typhoid and cholera that have diarrhoea as one of their symptoms, these vaccines are not 100% effective and there are many other organisms that can cause TD. TD most commonly affects people who are travelling to a less developed country where sanitation and hygiene measures may not be adequate. Higher risk countries include - the Middle East, Africa, Central and South America and many parts of Asia. TD is caused by eating and/or drinking food and water contaminated with bacteria – such as E. coli, campylobacter; viruses – particularly norovirus and parasites which include giardia and cryptosporidium. TD is three or more loose/watery stools in a 24 hour period often accompanied by stomach cramps, nausea and fever. It usually lasts 3-4 days and whilst not a life threatening illness, it can disrupt your trip for several days. The main danger of TD is Dehydration and this, if very severe, can kill if it is not treated. Treatment Rehydration. Ensure you drink plenty of clean water- at least 200mls with each episode of diarrhoea in addition to your 2L per day in a hot climate. If you are vomiting, wait 5-10 minutes and then start drinking again, but more slowly. For example, a sip every 2-3 minutes, but making sure that your total intake is as described above. Bland foods like bread, pasta, cereals, potatoes, rice or soup eaten little and often. Avoid spicy, fatty, heavy foods, milk and dairy products until you have fully recovered. Oral Rehydration Sachet (ORS).You may also need to replace some of your lost salts. This can be achieved by taking a prepackaged ORS such as DIORALYTE® which can be bought at a pharmacy. Antidiarrhoeal tablets such as IMODIUM® should only be used if truly necessary i.e. if you have a long journey. Imodium should not be used if you have a temperature or blood in your stool. Antibiotics are unnecessary in most cases, but may be indicated if you are staying somewhere remote or where medical assistance is poor or not available, or you have a medical condition which may be compromised with a severe infection i.e. diabetes. They are effective against some bacteria agents, but will not improve diarrhoea due to other causes. You are able to buy a course of antibiotic treatment at NOMAD or STA travel clinics. There are huge problems with counterfeit medicines abroad in developing countries, so you are always encouraged to take medicines with you bought from a reliable source. February 2014 -1- STUDENTS’ HEALTH SERVICE TRAVEL GUIDELINES Non antibiotic agents (Bismuth subsalicylate), available in tablet or liquid formulation Pepto-Bismol at pharmacists, has 60% overall effect. This should not be used for >3 weeks and may cause blackening of stools and tongue. CONTACT MEDICAL HELP IF YOU Have had a temperature for more than 48 hours Are vomiting and unable to tolerate fluids Have blood or mucous in your diarrhoea Have had persistent diarrhoea for more than 72 hours Women Travellers - If you are taking the combined oral contraceptive pill, contraceptive protection maybe affected with severe diarrhoea and vomiting and extra contraceptive protection i.e. condoms should be used as per your pill guidelines leaflet. Many diseases are transmitted by what is known as the ‘faecal-oral’ route (contaminated hands to mouth) and by drinking and swimming in contaminated water. The following guidance will help prevent this. Personal Hygiene Always wash your hands with soap and clean water after; going to the toilet, any contact with animals or sick people, before handling and eating food. If finding clean water is a problem then antibacterial wet wipes or small bottles of alcohol gel (more than 60% alcohol content) are always good substitutes. Care should also be taken with potentially contaminated cutlery and crockery. Water Purification Unless you know the water supply is safe, only use: Boiled water. Water boiled for at least one minute kills all infective organisms. It is the cheapest and most reliable way of water purification. However, carrying fuel and the time and effort of boiling water render it inconvenient whilst travelling. Bottled water (always check the sell by date/for algae in the water and that the seal on the bottle is intact). Unopened canned/bottled carbonated drinks. Hot tea and coffee, beer and wine are usually safe. Water treated by a sterilising agent such as chlorine/katadyn silver and using a reliable filter. Filtration bags remove suspended solids and organic matter. However, the water will still require further chemical disinfectant for removal of pathogens. By using a fine pore size filter (≤0.2µm to 1.0µm) other organisms can be removed (to include cryptosporidium and giardia). However, some viruses may be smaller than some filters pore size. Chemical Disinfectant. The most widely used chemical agent – iodine has now been discontinued for use (September 2009) under the EU biocide regulations. Chlorine/chlorine dioxide (highly toxic in concentrated form) and katadyn silver are chemical agents currently available. Their ability to sterilise water depends on the concentration of solution, temperature of water and how long the disinfectant is left in the water. However, some viruses and cysts may be more difficult to remove. Additionally February 2014 -2- STUDENTS’ HEALTH SERVICE TRAVEL GUIDELINES filtration is required prior to disinfection to remove solids and organic matter, as these interfere with the process of chemical disinfection with chlorine in particular. Therefore a method that filters together with a chemical disinfectant is recommended. Salt (Sodium Chloride) Electrolysis via a pen size hand held purifying device claims to inactivate cryptosporidium, bacteria, giardia and viruses. Ultraviolet (UV) Reactors claim to kill cryptosporidium, bacteria and viruses. Water however needs to be clear as its effectiveness may be limited by cloudy water with solids present. Furthermore, you are highly recommended to avoid ICE CUBES and STRAWS in drinks that may have been reused and washed in contaminated water and to only use bottled or filtered/sterilised water for CLEANING YOUR TEETH. Food Only eat well cooked fresh food. Avoid leftovers and reheated foods i.e. buffet foods where food has been kept luke warm for hours or exposed to flies. Ensure meat is well cooked and eaten hot wherever possible. Vegetables should be thoroughly cooked through, and salads that may have been washed in contaminated water avoided. Avoid fruit you are unable to peel. Peel other fruits including tomatoes. Milk should be pasteurised (heat treated). Never drink unpasteurised milk (included locally made ice creams and cheeses). It is better to stick to well known brands. Fish and shellfish even if well cooked can be hazardous. Take local advice and if in doubt avoid them. Food from street traders - unless it is has been freshly prepared and is served hot on clean crockery - should be avoided. OR boil it, peel it, cook it bin it! Swimming If you are travelling to Africa, South America or the Middle East, particularly to Lake Malawi, Lake Victoria and the Nile River you can catch a parasitic disease called Schistosomiasis (Bilharzia). You are advised to avoid swimming/wading and undertaking water sports in fresh water lakes, rivers and streams. If you do happen to swim in freshwater in one of these Schistosomiasis endemic countries, then it is advisable to have Schistosomiasis screening 3 months after suspected exposure, which can be performed here at Students’ Health Service (SHS). The majority of people who contract Schistosomiasis have no symptoms, therefore screening is highly recommended if there has been possible exposure. Well chlorinated water is safe to swim in. Personal Safety Before you travel, check the Foreign and Commonwealth Office (FCO) website for any security/environmental risks at your destination. https://www.gov.uk/foreign-travel-advice. You are advised to: February 2014 -3- STUDENTS’ HEALTH SERVICE TRAVEL GUIDELINES Wear modest clothing and do not display wealth (i.e. wearing a camera around the neck/expensive jewellery). Not leave your luggage unattended or hanging on the back of chairs in restaurants. Be aware that when you stop to take photos, purchase a postcard or read a map, you become a potential target for pickpockets or robbery. Try and pick accommodation which is in a safe area. Inspect the door locks and window fasteners. Use the hotel safe to store valuables. Not travel alone at night unless you are sure of the area. Check fire exits in discos, clubs and hotels. Avoid hitchhiking. Not agree to use illegal drugs or carry them for others. Accidents The major leading causes of injury and death in young travellers are due to road traffic accidents and drowning. To help prevent them: Avoid hiring motorcycles and mopeds. Always wear a helmet. Remember which side of the road you should be driving on! If hiring a car rent a large model if possible and ensure the tyres, brakes and seat belts are in good condition. Make yourself aware of the country laws and customs. Ensure you have comprehensive, adequate travel insurance. Use reliable taxi firms. Know where emergency facilities are and the number to call. Avoid alcohol when driving, especially at night. Avoid alcohol and food before swimming. Never dive into water where the depth is uncertain. Only swim in safe water and check for currents and tides, sharks, jellyfish etc. Avoid swimming alone. Swim in approved places where there is a beach patrol or lifeguard service. Sexually Transmitted Infections (STIs) Contraception Travellers are at increased risk of contracting an STI. Use of recreational drugs and alcohol can lead to risky sexual behaviour. Many British travellers have sex with new partners abroad, a good percentage of whom do not always use a condom. Many infections have no symptoms and can be transmitted unknowingly. If you have sexual contact with a new partner abroad, always use a condom with the ‘British Kite’ or ‘CE’ mark (as above) and check the expiry. Commercial sex workers (prostitutes) have very high rates of infection. Additionally, for the blood borne infections (Hepatitis B and C, HIV and Syphilis) avoid sharing needles for intravenous drug use; also avoid tattoos, acupuncture, skin piercing and open blade shaving if you are unsure of sterile equipment. Many developing countries reuse needles and syringes and blood donated for transfusions may not be screened for blood borne viruses. Therefore avoid blood transfusions unless absolutely necessary. If staying in remote areas think about taking your own sterile needle pack (available from NOMAD and STA travel clinics). If possible observe medical staff opening packages of sterile equipment before use. If you have been at risk whilst away, sexual February 2014 -4- STUDENTS’ HEALTH SERVICE TRAVEL GUIDELINES health screening and blood tests can be performed either here at SHS or at your local sexual health clinic upon your return. If you are taking regular contraception remember to take adequate supplies with you or emergency contraception as required as these may not be easily obtained in certain countries. Insurance Cover Take out comprehensive, adequate insurance cover for your whole trip, ensuring it covers you for extreme sports, i.e. diving (check depths). It should possibly include medical repatriation - this service if needed is extremely expensive without it. If you have any pre existing medical conditions, make sure you inform the insurance company of these details and check the small print of the policy thoroughly. If you travel to a European Economic Area (EEA) country, including Switzerland, make sure you have obtained a European Health Insurance Card (EHIC) before you travel. https://www.ehic.org.uk/Internet/startApplication.do. Additional travel insurance is still advised. Air Travel To reduce the risk of blood clots during long haul flights (Deep Vein Thrombosis and Pulmonary Embolism), it is sensible to: Exercise your legs, feet and toes while sitting every half an hour or so and take short walks whenever feasible. Upper body and breathing exercises can further improve circulation. Drink plenty of water, limit caffeine consumption and alcohol intake, which in excess leads to dehydration. Additional precautions may be required if you are ‘High-Risk’ which can be discussed in your travel appointment. Sun and Heat Sunburn and heat-stroke cause serious problems in travellers. Both are preventable. The destination(s) you are visiting may be near the equator and therefore receive increased ultraviolet radiation (UVR), made up of ultraviolet B (UVB), which causes sunburn and ultraviolet A (UVA), which contributes to photo ageing. Both are carcinogenic. Precautionary guidelines are as follows: Increase sun exposure gradually, 20 minutes limit initially. Use broad spectrum sun screen with a minimum sun protection factor (SPF) of 15 to protect against UVB with additional UVA protection. Apply 20 minutes before sun exposure, every 2 hours thereafter and always after swimming and washing. Pay special attention to covering ears, neck, scalp, lips, and tops of feet and back of hands. Read manufacturers’ instructions and check expiry. Wear protective clothing, i.e. o Wide brimmed sunhats o Sunglasses with 100% UVR protection and side panels o Long-sleeves Avoid going out between 11am and 3pm, when the sun’s rays are strongest. Seek natural shade in the form of trees or other shelter. Be aware of light reflected from sand, water or light objects. February 2014 -5- STUDENTS’ HEALTH SERVICE TRAVEL GUIDELINES Drink extra fluids in a hot climate. Be aware that alcohol can make you dehydrated. Further information can be found at: http://www.sunsmart.org.uk. Altitude Sickness Acute Mountain Sickness (AMS) is a condition that affects many travellers to high altitude, especially common at heights above 2500m. Definitions of high altitude are: 2400m-3500m High Altitude (i.e. Cuzco in Peru = 3225m) 3500m-5500m Very High Altitude (i.e. La Paz in Bolivia = 3658m. Base camps of Everest in Nepal = 5500m) Above 5500m Extreme Altitude (i.e. summit of Everest 8850m) AMS is caused by a lack of oxygen as air is thinner at altitude. Effects start 1500m2000m. The main symptoms include: headache, dizziness, loss of appetite, breathlessness, vomiting, poor sleep and lethargy. If these appear, rest for a day at the same altitude. If they persist or increase, DESCEND. AMS is best prevented by acclimatisation and ascending gradually, not more than 300m per day at more than 3000m and: Don’t sleep more than 300m higher at end of day. Keep well hydrated (check urine regularly to make sure it is pale in colour). Ensure a light but high calorific diet. Avoid over/strenuous exertion. Carry only a small, light day pack. Acetazolamide (Diamox®) has been extensively studied as prevention for AMS, although it is unlicensed for treatment or prevention of AMS in the UK. We therefore do not prescribe it here at SHS, but you may purchase it from private travel clinics. Other health concerns at altitude include: hypothermia, frostbite, wind-chill, dehydration, high ultraviolet (UV) radiation= sunburn, traveller’s diarrhoea, weight loss, poor fitness, minor illness and injury. HAPE (High Altitude Pulmonary Oedema) and HACE (High Altitude Cerebral Oedema) are life threatening conditions. For more information please refer to http://www.altitude.org/home.php. Culture Shock Your trip may involve expedition/voluntary/charity work in a developing country - an incredibly fantastic personal experience, offering great insight into other cultures. However, some travellers will find it a huge culture shock and may not be able to cope with aspects of travelling and living in a developing country. Aspects you will need to consider: Living in a humid, hot climate in close proximity to strangers i.e. other travellers and local populations, where there may be little privacy. Accommodation may be very basic with shared facilities. February 2014 -6- STUDENTS’ HEALTH SERVICE TRAVEL GUIDELINES No home comforts and perhaps no running water or electricity for charging electrical equipment i.e. mobile phones/iPods. Separation from family/friends with perhaps no internet access for days/weeks at a time. Provisions may be basic and food unusual. Exposure to poverty and begging. Basic healthcare in the event of an accident/being unwell. You essentially need to be able to look after yourself. It is also important to have realistic expectations of life and travel in new cultures. If you have any unresolved problems this may make them worse. You may find adapting difficult if you have any family or social difficulties at home and psychological problems. If you are undertaking expedition/voluntary/charity work that involves living rurally with local populations you perhaps need to ask yourself: Do you understand the risks of where you are going? Are your coping strategies transferable? What are your fall back measures? An expedition or ‘working’ in a developing country is not the place to start or continue therapy. Avian and Swine Influenza Before you Go: Check the FCO website for advice on current outbreaks https://www.gov.uk/foreign-travel-advice. Ensure you have adequate travel insurance before you travel. During Travel: -Avoid visiting live animal markets and poultry farms. -Avoid contact with surfaces contaminated with animal faeces. -Do not eat or handle undercooked or raw poultry, egg or duck dishes. -Do not attempt to bring any live poultry products back to the UK. -Do not pick up or touch dead or dying birds. -Exercise good personal hygiene with frequent hand washing or use alcohol gel (more than 60% alcohol content if clean water not available). - If you become unwell with a fever (temperature 38°C or more), cough, difficulty with breathing, headache, sore throat or muscle aches, promptly seek medical attention. After travel: If you become unwell with fever and either a cough or difficulty breathing within 14 days of returning to the UK call NHS 111 or your GP before visiting the surgery. Describe your recent travel history as well as your symptoms. Recommended First Aid Kit Wound dressings (for treatment of cuts, grazes and minor injury): Remember to use clean- purified/bottle water for cleaning cuts/grazes -Assorted plasters (including Blister plasters) -Adhesive tape -Bandages -Sterile non-adherent dressings (to prevent wound sticking to dressing) -Lancets, for popping blisters (as indicated) February 2014 -7- STUDENTS’ HEALTH SERVICE TRAVEL GUIDELINES Antiseptic: -Solution for cleaning wounds -Antiseptic wipes - if clean water not available for hand washing Medication: -Analgesia (i.e. paracetamol and ibuprofen) - for treatment of pain: headache, muscle/joint pain, sunburn -Antihistamine (i.e. cetirizine) - for treatment of allergies/skin reactions, -Antidiarrhoeal (i.e. Imodium) -ORS (i.e. Dioralyte) - for replacement of salts following severe diarrhoea, vomiting and sweating -Chloramphenicol eye ointment - for treatment of minor eye infections Sterile kit: A small selection of needles and syringes to reduce the risk of blood borne viruses (kits are available at NOMAD or STA travel clinics) Other useful items: -Scissors -Tweezers -Non-sterile gloves Additional Supplies -Calamine lotion for itching after sunburn -Miconazole cream for fungal infections (especially feet) -Clotrimazole pessary for vaginal candidiasis (thrush) as medication maybe difficult to obtain -Ibuprofen gel for pain and stiffness -Aciclovir- strong sunlight, cold and wind can trigger cold sores -Lip salve with UV protection- to prevent sore, chapped lips -Ciprofloxacin- a single dose is sufficient to treat 80% of cases of traveller’s diarrhoea (available to buy from NOMAD or STA travel) -Trimethoprim- if prone to urinary tract infections Other useful items: -Antacids- heartburn and indigestion can be exacerbated by unfamiliar food -Laxatives- dehydration, dietary changes may contribute to constipation -Cold/sinus medication for treatment of viral infections and sinusitis in a cold climate Useful web site addresses: Travel Advice: http://www.fitfortravel.nhs.uk/home.aspx http://nathnac.org/travel/index.htm. NHS Immunisation Information: http://www.nhs.uk/Conditions/vaccinations/Pages/vaccination-schedule-agechecklist.aspx February 2014 -8- STUDENTS’ HEALTH SERVICE