Analysis of Symptom
advertisement

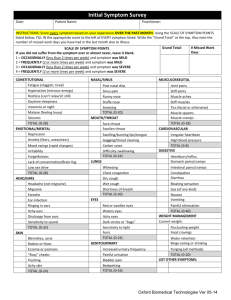
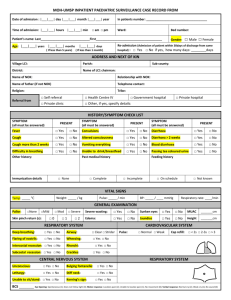
Analysis of symptom 1 MENNONITE COLLEGE OF NURSING AT ILLINOIS STATE UNIVERSITY NUR 431 Diagnostic Reasoning for Advanced Nursing Practice ANALYSIS OF SYMPTOM CHIEF COMPLAINT The interviewer first determines the patient’s chief complaint. Examples include: “Stomachache and diarrhea for three weeks” “I’ve been wheezing and I can’t seem to catch my breath.” o NOTE: This chief complaint was obtained after the patient had said “Asthma for 12 hours.” This is a diagnosis, not a chief complaint. Thus, the interviewer then elicited the chief complaint by asking the patient what had been occurring to make him say this. This then lead the patient to state he had been wheezing and couldn’t catch his breath. Note: At times, the patient is not ill, but rather is having a preventative health care. The “chief complaint” would then be replaced as follows: o Reason for presenting: Desires yearly checkup and pre-employment physical. After determination of the chief complaint, the interviewer then analyzes the problem further using an analytical, organized approach. HISTORY OF PRESENT ILLNESS OR PRESENT STATE OF HEALTH This section of the history contains a thorough investigation of the chief complaint or a more detailed description of the well client’s health status. The components of the history of present illness (HPI) or present state of health are as follows: A. Introduction 1. Description of client 2. Usual health B. Chronological investigation of symptoms 1. Course of symptomatology: incidence, duration and manner 2. Symptom analysis: aggravating, alleviating, and associated factors; location; quality; quantity; and setting C. Pertinent negatives--what it is not! D. Relevant family history, psychological, social, cultural, spiritual data E. Assessment of disability F. Related medications including OTC. Analysis of symptom 2 Each of these components will now be discussed in further detail. Introduction The introduction is a brief biographical section including age, sex, marital status, occupation, and employment status. It also includes the number of visits to the interviewer’s facility and the number of hospital admission for the problem identified in the chief complaint, or for any other problem. In addition, it contains information about the client’s usual health status and any previous or present health problems. Examples of an introduction are the following: Introduction: First visit; 17-year-old; unmarried, black female high-school student. Is healthy and has never had serious health problem. Introduction: First hospital admission for this 30-yr.-old Mexican American, a separated father of four and self-employed brick layer. Health has always been good until two years ago, when burning in stomach began. Unable to go to work today because of weakness, vomiting, and severe stomach pain. Chronological Investigation of Symptoms For every problem or “chief complaint” the patient presents with, a symptom analysis is done. The following characteristics of a symptom are always analyzed. Onset o Date of onset/duration o Manner of onset o Precipitating and disposing factors related to onset Characteristics o Location and radiation (of pain) (where is it located, is it in one location, diffuse, or does it radiate?) o Quality (What is it like--for example, is the pain dull, sharp, throbbing?) o Quantity/severity or intensity (on a scale of 1-10 what is your pain like?, how it affects daily activities or family relations--how bad is it?) o Timing/setting (circumstances under which it occurs--environment, personal activities, emotional reactions) o Aggravating and alleviating (relieving) factors (What makes it better or worse?) o Associated factors (other related symptoms--review of the appropriate body system(s), or a directed review of systems) Course o Incidence (single or recurrent episode, predictable?) o Progress o Effect of therapy o Hospitalizations In addition, pertinent (related to the system) past health history, personal/social/occupational history and family history are included in the symptom analysis. The meaning of some of the above-mentioned terms is: Analysis of symptom 3 Onset describes when the symptom first occurred and may be sudden or gradual. Incidence refers to the frequency of the symptom. Duration applies to the amount of time the symptom lasts. o Note: Onset and duration are documented in standard terms, for example, upon awakening in the morning, 30 minutes after meals, twice a day, and for three hours. Terms such as frequently, a lot, and often are inexact and confusing. Manner describes the nature of the system over time, for example, intermittent, constant, continually worsening, and crescendo-decrescendo. The location applies to the specific place where a symptom is experienced. Most frequently it is used for pinpointing an area where pain occurs and includes the origin and any radiation to other areas. The quality of the symptom is described in the client’s words as specifically as possible. Sometimes it is helpful to ask the client if it feels like anything experienced before. An example is the feeling of pressure or chest constriction during a myocardial infarction. Patients often describe this feeling as if the weight of an elephant were sitting on the chest. There are at least 50 words in the English language for pain; however, the most commonly used ones are aching, burning, dull, sharp, stabbing, stinging, and throbbing. The quantity is the amount experienced in concrete, measurable terms, such as minutes, hours, days, or weeks. For instance, the client related, “My heart was racing. My pulse was up to 200 for 15 minutes.” The setting refers to the circumstances surrounding the symptom. This applies to who was present, where it occurred, and during what kind of activity. The following is an example of the family nurse practitioner’s process of seeking clarification of a general statement: o Client: My husband and I are having marital problems. o NP: Tell me more about that. o Client: We fight a lot. o NP: You’re fighting more than you used to? o Client: It seems like we fight all the time. Whenever we are in the same room, one of us seems to get mad at the other. o NP: Is there anything else going on that seems related to these fights? o Client: Well, my husband lost his job three months ago because of funding cuts. I guess we’re both really worried about finances. o NP: Anything else? o Client: I’m afraid I’ll get pregnant again, so I haven’t been too interested in bed. o NP: Has anything helped your problems? o Client: We used to go out once a week until the job layoff. That gave us a chance to talk and be close without the kids. Now we can’t afford it. An aggravating factor seems to increase the intensity of a symptom, while an alleviating factor seems to produce a lessening effect. An associated factor appears to be related to the feeling being discussed or seems to occur at the same time. For example, o Interviewer: Did you notice any other changes during the headache? Analysis of symptom 4 o Client: Well, as a matter of fact, I felt sick to my stomach and was afraid that I would vomit. Of course, for the well client, the chronological investigation of symptoms is usually omitted. If later in the interview, usually during the ROS, a symptom is uncovered, it would then be discussed. For example, when a client presents for a routine checkup and later mentions amenorrhea for two months, this symptom is fully investigated and recorded in the present illness section, proceeding from the most remote to the most recent symptom as follows: Five years ago: Menarche-age 13, menses every 29-31 days, lasting 4-5 days with moderate blood flow (saturates 5-6 tampons/day). Mild cramping on second day that usually responds to aspirin, grains 10, bid. (NOTE: menstrual cramping usually not responsive to Tylenol.) Two years ago: Began having unprotected sexual relations with steady boyfriend about twice/month. Has never practiced contraception because it would ruin naturalness of sex. One week ago: Noticed breast tenderness and fullness and began to experience nausea every evening. The chief complaint is changed to say. “Desires routine check up and thinks she is pregnant.” LMP 12/4. Pertinent Negatives A negative response to certain questions about symptoms is just as important as a positive response in assessment. This is referred to as a pertinent negative. The items can be symptoms, as well as information, from any other section of history (family, psychosocial, socioeconomic, or nutritional history) that could have significance in the overall course of health or illness. Hence the descriptive word pertinent is used. Some relationships are obvious; for example, persons with respiratory system symptoms are asked about their smoking history and persons with vascular changes such as cold extremities or intermittent claudication are asked about family history of angina, arrhythmias, arteriosclerosis, hypertension, and myocardial infarction. A good rule of thumb for beginning interviews is to ask all of the review of system questions for a given system or region when symptoms of that system or region are mentioned in the history of present illness. Disability An assessment of disability indicates what changes in lifestyle the client has made as a result of the symptoms discussed in the history of present illness. For example, a client who related recent difficulties in walking to work (a distance of 1 mile) due to shortness of breath and fatigue has made a quantitative statement about the effects of declining health on life style. Disability also includes financial constraints and physical limitations imposed by illness or injury. Analysis of symptom 5 Medications All related medications taken by the client are recorded in this manner: drug’s name, dosage, frequency of administration, and description of the effect of the drug and any untoward reactions. Over-the-counter drugs including vitamins, aspirin, and cold remedies are also listed. Medications unrelated to the current problem are usually listed in a designated section of the patient’s record and verified for accuracy with each visit. Documentation Tips When writing the symptom analysis (history of present illness), integrate this information using appropriate indentations and paragraphs--do not label categories or list items as you would in other parts of the complete history. In your written notes, use appropriate abbreviations, symbols, and non-wordy, but meaningful sentences. Do not use excess adverbs. Documentation Example The following is an example of a completed history of present illness for a client with burning pains in the stomach: Denies diarrhea, melena, belching, nausea, jaundice, dysphagia, bloating, constipation, and hemorrhoids. Paternal grandfather died of stomach hemorrhage at age 45. Father, age 64, three hospital admissions for bleeding peptic ulcers. Well since ulcer surgery 5 years ago. Smokes two packs of cigarettes/day for 15 years. Stopped drinking coffee and cola 2 yrs. ago. Drinks six pack beer with buddies q. Friday night. Fights with wife about 2x/wk. over children. Business slow. Maalox, 2 tabs, 30 mins., after meals and between meals up to 20/day, provides relief for only 30 mins. Uninsured. Worried about loss of income during hospitalization and about ability to pay for medical expenses.