Goals and Objectives

Neurodevelopmental Clinic and Birth Defects Clinic – Goals and Objectives
Description
Diagnosis and specialty management of congenital and early-acquired disabilities, especially motor disability affecting locomotion, manipulation and/or speech. Children with Central Nervous System (CNS) malformations, spina bifida, cerebral palsy, mental retardation, autism and related problems constitute the core populations. The ND
Program works in consultation to community-based primary care providers.
Developmental pediatricians and nurse clinicians serve as organizers/coordinators.
Consultants from orthopedics, rehabilitation medicine, social work, and nutrition attend clinic on both Tuesdays and Wednesdays. Neurosurgeons and urologists attend on
Wednesdays. Children may be scheduled for appointments with consultants in OT, PT, speech and language, psychology, and other medical/surgical sub-specialties.
Approximately 550 new children and a total of 2,000 children are seen each year. Each new referral is screened by the nursing staff. Old records are gathered as appropriate.
These records will be available at the check-in desk for review. The records should not be removed from the desk area. In clinic, patients are checked in, weighed and measured, and assigned an exam room. The room number is marked on the scheduling board in the hallway and the chart/x-rays should be by the door. The patient and family are assigned the same exam room for most of their appointments. While each professional will meet individually with the family, overlap is usually comfortable for the family and conducive to better communication among professionals. By the end of the day, the developmental pediatrician and nurse clinician are expected to be aware of the general outcome of each visit in order to plan comprehensive follow-up and communication back to sources seeking our consultation.
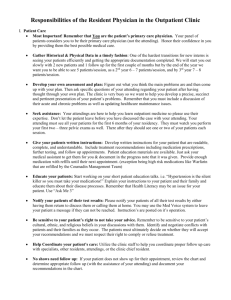
Resident Role and Expectations
Ask questions, read, see children, play with them, teach. Approach each child as a unique person in a unique family and expect the attending to do the same. The attendings will teach by example, discussion, questioning, and by encouraging independent judgment.
There is a didactic session scheduled most Tuesday mornings. Option: Initiate a unique case literature review, systematic review of a treatment or a clinical research project.
Discuss with an attending. Option: Stay in contact with the Division attending on call for the opportunity to see inpatient consults, observe surgeries or other inpatient activities.
Be on time for didactic sessions and clinic! If you have to leave early for continuity clinic, post call or night call, please let your attending know.
In clinic, you will be assigned during the rotation to work with various pediatric attendings and some of the consulting specialists. You may be assigned to follow a child and family through their entire workup. This is an especially valuable experience. You will be assigned to see new patients and returning patients. Fellows will perform a complete history and physical exam, present the child to the attending, and see the child and family together on several patients per day. Clinic notes must be dictated back to the referral sources and families on clinic day. Residents will see children jointly with attendings and will be given opportunities to take histories, do examinations, and develop a differential diagnosis and diagnostic and management plan. Most dictations will be done by attendings. Students will observe initially and then take more responsibility for history-taking and examination
If working with a consultant, you will generally follow the consultant to interact and observe, but can be active in obtaining histories and presenting to the consultants.
Documentation is essential: Use the worksheet template when gathering history.
The attending must fill out the planning sheet and a portion of the worksheet template.
This is a three-page Neurodevelopmental Clinic worksheet template on every chart to use for recording data which includes: Full Past Medical History (PMH), Social History,
Family History and Review of Systems (ROS) needed on most visits. Include allergy, current medication and immunization history. The attending will need to review and sign the worksheet, add his/her own documentation if someone else dictates.
Each chart has a planning sheet on the front. This should be filled out for every child by the attending. The planning sheet was developed to facilitate communication among disciplines, to families, and community care providers. Each discipline that comes into contact with the child is to document specific instructions and recommendations for return visits. At the end of the day, nurses need these forms to plan the next visit.
Attendings are primarily responsible for dictations. In general, residents will not be expected to dictate notes but the opportunity may arise on occasion. Students should not dictate primary notes but may be asked to write up cases for educational purposes, separate from the note that goes in the record. All clinic notes must be dictated, because most will be sent to primary care providers and families. If the attending does not do the dictation, he or she must hand write a note to document that the patient was seen personally. This documentation is essential for reimbursement and medicolegal reasons.
Required Reading:
None
Contact
Bill Walker, MD 206-987-2204, william.walker@seattlechildrens.org
Educational Goals
1.
Become familiar with the diagnostic and management strategies of childhood disability and the conditions that cause the disability.
2.
Appreciate the importance of providing excellent medical care and rehabilitation services for children with disabilities
3.
Experience the care of children with disabilities as an intellectually challenging and emotionally positive activity
4.
Promote “Medical Home” alliances with the child’s primary care provider.
Learning Objectives
Because of participating in the Neurodevelopmental Clinics, trainees will be able to: a.
Medical Knowledge
describe several diagnoses, causes, and treatments of children with cerebral palsy and related motor disorders, other developmental impairments, and their behavioral consequences.
identify the interaction of disability and child development b.
Patient Care
describe at least 2 approaches to helping families of children with chronic disabilities that support comprehensive, coordinated family-centered care and functional independence of the child and family.
demonstrate a competent pediatric evaluation of a child with or at risk for a developmental disability or congenital anomaly.
describe 3 features of effective consultants to primary care physicians, nurse practitioners, and to surgical sub specialists.
classify the roles of at least 4 professionals in the care of children with disabilities and their interdisciplinary care in an applied setting.
list 3 technologies appropriate to the care of children with disabilities.