GENTAMICIN USE IN NEONATES: LESS OFTEN – LESS TOXIC
advertisement

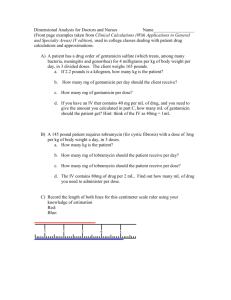
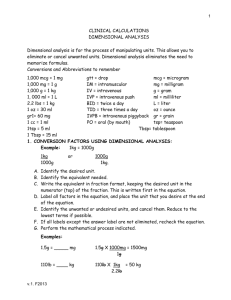
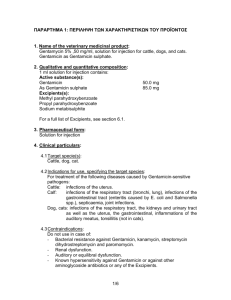
P43 GENTAMICIN USE IN NEONATES: LESS OFTEN – LESS TOXIC Davies MW, Cartwright DW The Grantley Stable Neonatal Unit, Royal Women's Hospital, Bowen Bridge Rd, Herston, Brisbane, Queensland, Australia, 4029. Objectives: Over the last decade there has been shift from giving gentamicin to neonates every 24 hours (q24hly) - rather than using shorter dosage intervals. Conflicting advice on gentamicin dosing regimens from commonly used paediatric and neonatal drug dosage booklets in Australia over the last few years has lead to the situation where neonatal house staff have been commencing neonates on varying doses and dosage intervals of gentamicin. This gave us the opportunity to assess serum gentamicin levels (SGL) at differing dosage intervals. The aim of this study was to determine the incidence of toxic trough SGLs in neonates in the first week of life, and to determine if the incidence varied with dosage interval. Methods: This was a retrospective study of all infants born between 1/7/1995 to 31/12/1995 and admitted to our neonatal unit, who received a first course of gentamicin in the first week of life. Data were collected on the infant’s birth weight, gestation, dose and dosage interval of gentamicin, the trough SGL before the third dose, serum creatinine on the day of the SGL and the urine output in the 24 hours prior. Infants were excluded from the analysis if there was evidence of impaired renal function. In our unit a trough SGL of 1.5 milligrams per litre (mg/l) was considered non-toxic and safe. A level of 1.5mg/l was considered a significant risk of toxic drug accumulation and the dosage interval of gentamicin was increased. These levels were chosen by the Department of Microbiology at the Royal Brisbane Hospital, based on the test method and to optimise safety (Faoagali J, personal communication, 1997). Results: 170 infants met the study criteria. For analysis the infants were divided into three groups: Group 1 – 21 infants from 24 to 29+6 weeks gestation. All 21 infants received gentamicin every 24 hours (q24hly). 16 (76%) infants had toxic trough SGLs. Group 2 – 83 infants from 30 to 34+6 weeks gestation. 8 infants had gentamicin every 12 hours (q12hly) and all (100%) had toxic trough SGLs. 14 infants had gentamicin every 18 hours (q18hly) and 13 (93%) had toxic trough SGLs. 61 infants had gentamicin every 24 hours and 25 (41%) had toxic trough SGLs. The differences in proportions were statistically significant. That is gentamicin given q12hly or q18hly was more likely to lead to toxic SGLs compared with gentamicin given q24hly. Group 3 – 66 infants of 35 weeks gestation. 29 infants had gentamicin q12hly and 25 (86%) had toxic trough SGLs. 6 infants had gentamicin q18hly hours and 2 (33%) had toxic trough SGLs. 31 infants had gentamicin q24hly and 4 (13%) had toxic trough SGLs. The differences in proportions comparing infants having gentamicin q12hly with those having it q24hly were statistically significant. That is gentamicin given q12hly was more likely to lead to toxic trough SGLs compared with gentamicin given q24hly. Conclusion: Starting gentamicin q12hly in infants of any gestation leads to most having toxic trough SGLs. The same can be said for infants of 30 weeks starting gentamicin q24hly. In infants of 30 weeks gestation most have safe non-toxic trough SGLs if started on gentamicin q24hly. In our unit, as a result of the above data, we recommend that gentamicin is commenced at a dose of 2.5 mg/kg q36hly for infants 30 weeks gestation and q24hly for infants 30 weeks gestation.