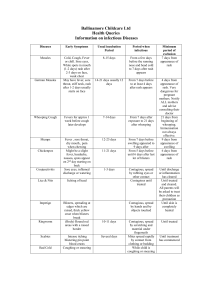
Varicella Disease History Verification Checklist
advertisement

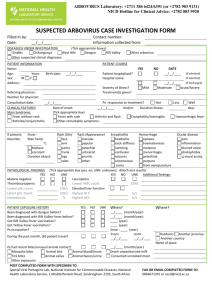
Varicella Disease History Verification Checklist This form is intended to screen for past varicella disease, not current acute varicella. Fax or mail completed form to school or child care. See reverse side for disease information. Child’s name: ________________________________________ Date of birth: _______________________ Address: _________________________________ City/town: _______________________ Zip: __________ Phone number: ______ - _____ - ________ Name of school/child care: _____________________________ Parent/guardian: ____________________________ Parent report of date of disease: _____ / ____ / ____ month General info Fever day year Was child seen by a health care provider for this illness? Yes No Unk Was a specimen collected for testing? Yes No Unk Did the child have an illness or take medication during their varicella illness that would lower the immune system? Yes No Unk Was fever present? If yes, date of onset _____/_____/_____ Yes No Unk Yes No Unk Yes No Unk Red Yes No Unk Flat (smooth) Yes No Unk Raised (bumpy) Yes No Unk Blistered (filled with fluid) Yes No Unk Crusted Yes No Unk Yes No Unk If it spread did it spread all over at once? Yes No Unk If it spread did it spread in spurts? Yes No Unk Yes No Unk Does the child have any scars from the rash? Yes No Unk Before the child’s rash developed was he/she exposed to someone who had a doctor’s diagnosis of chickenpox? Yes No Unk How long did the fever last? Rash Was there a rash? If yes, date onset _____/_____/_____ Where did the rash start? Trunk (chest, back) Hands Arms Face Feet Legs Mouth What did rash look like? (Mark “yes” to all that apply) Template Did the rash spread? Describe (or check) how the rash spread (from where to where): Trunk to trunk? Head to hands? Trunk to arms and legs? Stayed on head? Head to trunk? Was the rash itchy? How long did the rash last? I have reviewed above reported symptoms of the child named above and: (check one) _____ I verify that the child likely had varicella disease. _____ I find the child’s reported symptoms insufficient, as described, to verify varicella disease and I recommend a visit with a health care provider for further assessment. Signature of MD, NP, or PA _____________________________________________ Date ______________ Clinic name: _________________________________________________________ Phone: _____________ (8/10) Page 1 of 2 Varicella Verification Checklist Symptoms and progression of varicella disease Rash is often the first sign of varicella disease in children and fever may occur after the rash. Adults may have fatigue and fever one to two days before the rash appears. In unvaccinated individuals, the rash progresses from macules to papules to vesicular lesions before crusting – usually taking 5-7 days from onset to crusting over. Fluid may drain from vesicles before they dry and crust. Most lesions are 1 mm to 4 mm in diameter. The rash is itchy. The rash occurs in successive crops. Generally the rash distribution is centripetal, first appearing on the head then the trunk and often spreading over the entire body. Most children experience 250 to 500 itchy lesions. New crops of spots develop over several days, and spots in several stages of development are present at the same time. Post-vaccination varicella breakthrough disease A breakthrough infection is defined as a case of wild-type varicella that occurs in a person more than 42 days after vaccination following exposure to wild-type virus. Because of its modified clinical presentation, breakthrough varicella illness may be more difficult to clinically recognize by both practitioners and parents. Breakthrough disease is usually mild; patients typically have low or no fever, develop fewer than 50 skin lesions, and experience a shorter duration of illness compared to unvaccinated individuals with natural infection. The rash is more likely to be maculopapular rather than vesicular. Occasionally breakthrough cases are not mild, and patients have clinical features similar to those occurring in unvaccinated cases. The rate of breakthrough disease in one-dose vaccinees exposed to varicella is estimated to be approximately 15%-20% and does not appear to increase with length of time since vaccination. According to one study, the rate of breakthrough illness is three times less after two doses of varicella vaccine. Is laboratory confirmation of varicella cases necessary? No, not routinely. However, laboratory diagnosis can be useful if confirmation of the diagnosis or determination of susceptibility is necessary. Widespread varicella vaccination has resulted in a dramatic decrease in varicella incidence and more of the varicella cases will be occurring among vaccinated persons who may have atypical disease. This modified clinical presentation of disease makes varicella diagnosis by physicians difficult and may increase the need for laboratory confirmation. Sources: American Academy of Pediatrics. Varicella-Zoster Infections. In: Pickering LK, Baker CJ, Kimberlin DW, Long SS, eds. Red Book: 2009 Report of the Committee on Infectious Diseases. 28th ed. Elk Grove Village, IL: American Academy of Pediatrics; 2009:714-727. CDC. Epidemiology and Prevention of Vaccine-Preventable Diseases. Atkinson W, Wolfe S, Hamborsky J, McIntyre L, eds. 11th ed. Washington DC: Public Health Foundation, 2009. CDC at http://www.cdc.gov/vaccines/vpd-vac/varicella/dis-faqs-clinic.htm. Immunization Program P.O. Box 64975 St. Paul, MN 55164-0975 651-201-5503, 1-800-657-3970 www.health.state.mn.us/immunize (8/10) Page 2 of 2