Medication use among acutely hospitalised medical patients

Medication use among acutely hospitalised medical patients
Patient’s self-reported use versus pharmacy records and drug analyses
PhD thesis
Bente Glintborg, MD
Copenhagen 2008
_______________________________________________________________________________
This PhD dissertation was accepted by the Faculty of Health Sciences of the University of
Copenhagen, and was defended on January 18 th , 2008.
Official opponents: Christian Torp-Pedersen, Jesper Hallas, Birgitte Brock
Tutors: Kim Dalhoff, Henrik Enghusen Poulsen
Correspondance: Bente Glintborg, Hybenvej 46, 2830 Virum. Email: glintborg@dadlnet.dk
List of contents
1.3. The quality of medication histories among hospitalised patients ........................... 10
1.7. Secondary medication interview among in-hospital patients ................................. 14
1
Preface
The data collection and the writing of this PhD thesis took place during my fellowship at
Department of Clinical Pharmacology, Q7642 at Rigshospitalet, Copenhagen, from 2004-2007.
The making of the thesis is not entirely my own work. Many colleagues have helped me during this process and I would like to take this opportunity to thank some of them. First and foremost, thanks to my skilled and experienced supervisors Professor Henrik Enghusen Poulsen,
Department of Clinical Pharmacology, Rigshospitalet and Senior Resident Kim Dalhoff, Clinical
Pharmacologic Unit, Bispebjerg Hospital. They have both unremittingly been available for professional guidance. Without the financial support provided by Henrik E. Poulsen this work would not have been possible.
Thanks to the staff at Department of Clinical Pharmacology, Rigshospitalet. I would especially like to thank the chemists Peter R. Hillestrøm and Lenette Holm Olsen and the technical staff Bodil Mathiassen and Senia Scharling for their work done in the laboratory. But also to the long line of physicians and colleagues who have worked in the department through my employment for their social and professional inspiration. Thanks to Kristian Linnet, Section of
Forensic Chemistry, University of Copenhagen for verification analysis of drug screenings.
Associate professor Thomas Scheike and associate professor Lene Theil Skovgaard, Department of
Biostatistics, Kommunehospitalet provided professional guidance with the selection of appropriate statistical analyses.
I am thankful to all patients willing to participate in the study. Thank you to the staff at acute medical department, Bispebjerg Hospital for their help during data collection; especially Hanne Lund and her nurses, and Grith Ingemann and her secretaries. Thank you to the secretaries Annette Ring and Tina Hansted Olsen at Medical Department, Bispebjerg hospital for their help retrieving hospital files. The cooperativeness and help from Solveig Wittenburg and her laboratory technicians at Department of Clinical Biochemistry, Bispebjerg Hospital during blood sampling was invaluable.
Thanks to Rigshospitalets Forskningsudvalg and H:S Direktionen for financial support.
2
Dansk resumé
En ufuldstændig medicinanamnese giver ved hospitalsindlæggelser bl.a. risiko for behandlingssvigt, medicineringsfejl, lægemiddelinteraktioner og mistolkning af symptomer.
Strukturerede lægemiddelinterviews forbedrer anamnesen, men der findes ingen guld-standard metode som med sikkerhed beskriver patientens totale forbrug. Formålet med denne afhandling var at beskrive anvendelsen af patient interviews, receptdata og medikamentanalyser til at opnå en nøjagtig medicinanamnese. Et delformål var at vurdere, om nogle patient-karakteristika kunne identificere patienter, som var bedre til at selvrapportere, og om brugen af nogle lægemidler rapporteredes bedre end andre.
Metode 500 patienter indlagt på et akut medicinsk modtageafsnit blev interviewet på indlæggelsesdagen om deres lægemiddelforbrug i ugen før indlæggelsen, og urin og blodprøver blev indsamlet. Blandt patienter, som rapporterede brug af 5 på forhånd udvalgte kardiovaskulære eller antidiabetiske lægemidler (amlodipin, bendroflumethiazid, digoxin, glimepirid, simvastatin), blev yderligere et interview foretaget 1 måned efter udskrivelsen i patientens hjem. Der blev atter indsamlet blod- og urinprøver. Patienternes selv-rapporterede lægemiddelforbrug blev sammenlignet med receptdata (PR) tilgængelige via www.medicinprofilen.dk
. Alle indsamlede blodprøver blev analyseret for indhold af amlodipin, bendroflumethiazid, glimepirid og simvastatin, hvorimod digoxin-analyser kun blev udført blandt brugere af de 5 på forhånd udvalgte lægemidler. Blandt en stikprøve på 100 patienter blev urinprøver fra indlæggelsen analyseret for indhold af amfetamin, barbiturat, benzodiazepin, cannabis, kokain, metadon og opiat (toksikologi screening). Alle analyseresultater blev sammenlignet med interview data.
Resultater De inkluderede patienter havde medianalder 72 år, 60% var kvinder. Patienterne rapporterede et medianforbrug på 3 receptpligtige lægemidler (POM) op til indlæggelsen. Når registreringerne i PR blev sammenlignet med interview data blev 19% (95% CI: 15-23%) af POM registreret i PR ugen forinden, og 27% (24-29%) købt måneden forinden ikke rapporterede af patienten ved indlæggelsen. Hjertemedicin (ATC gruppe C) var den medicintype, som blev rapporteret i højest overensstemmelse med PR. Dette i modsætning til bl.a. dermatologiske lægemidler som ofte blev underrapporteret. Patienter med høj alder underrapporterede hyppigere.
Ved hjemmebesøgene blev 11% (6-18%) af POM købt ugen forinden og 18% (15-22%) af POM købt måneden forinden ikke rapporterede af patienten ved interviewet. Igen blev hjertemedicin rapporteret hyppigst (p<0,05). Patienterne rapporterede i højere overensstemmelse med PR ved hjemmebesøgene sammenlignet med ved indlæggelsen (p<0,05).
Overensstemmelsen mellem selvrapporteret forbrug af amlodipin, bendroflumethiazid, digoxin, simvastatin og glimepirid vs. resultat af blodprøveanalyser var høj for alle 5 lægemidler ved både indlæggelse og hjemmebesøg (alle kappa-værdier >0,79, p<0,05). I alt 36 patienter (7%, 5-10%)
3
rapporterede dog i uoverensstemmelse med blodprøve resultaterne, disse patienter adskilte sig ikke køn- eller aldersmæssigt fra patienter med overensstemmende resultater.
Forbrugs-prævalensen af illegale stoffer var lav og ingen patienter havde positiv screening for amfetamin eller kokain. I alt 12 patienter (12%, 6-20%) havde en toksikologi screening positiv for stoffer, som ikke var blevet rapporteret ved interviewet (cannabis: 5 patienter, benzodiazepin: 7 patienter). Dette gav en sensitivitet af selvrapporteret forbrug på 66% (48-81%). Patienterne var generelt troværdige, når de benægtede brug af de enkelte stoffer (negativ prædiktiv værdi >92%).
Diskussion Uoverensstemmelser mellem PR og interviews skyldes ikke nødvendigvis underrapportering men kan alternativt forklares som non-adherence eller ændringer i medicinerings-regimet.
Konklusion På trods af fokuserede medicin-interviews tyder receptdata på, at der sker underrapportering af lægemiddelforbruget - selv når interviewene foretages i patientens eget hjem.
Hjertemedicin rapporteres tilsyneladende bedst, og der er stor overensstemmelse mellem selvrapporteret brug, receptdata og medikamentanalyser for denne lægemiddelgruppe.
Lægemidler med misbrugspotentiale og illegale stoffer anvendes kun af få patienter – imidlertid underrapporterer en del patienter brugen af benzodiazepin og cannabis.
Perspektiver Medicininterviews giver ikke den fulde information om patientens medicinforbrug.
Da receptdata er let tilgængelige i elektronisk form i Danmark, kunne disse sandsynligvis med fordel anvendes til forbedring af medicinanamnesen - specielt hos ældre patienter. Medikament og rusmiddel-analyser er ressourcekrævende og ikke altid praktisk tilgængelige, men kan overvejes ved diagnostisk uafklarede patenter. Den praktiske implementering af forbedrede procedurer til indhentning af medicinoplysninger, herunder medicinafstemning (reconciliation), samt effekten af disse på forekomsten af medicineringsfejl, bivirkninger, øget patienttilfredshed og lign. er på nuværende tidspunkt uafklaret.
4
Abstract
Upon hospitalisations, a complete medication history is of value for the correct interpretation of symptoms and the safe prescription of drugs. A major reason for medication errors and adverse drug effects is lack of knowledge of the patient’s in home medication use. Secondary medication interviews improve the medication history compared to the history routinely written in hospital files. However, even secondary medication interviews may be subjected to patient’s recall bias.
The aim of the present thesis was to describe secondary medication interviews, pharmacy records and drug analysis as methods to obtain a reliable medication history. Furthermore, to identify if some patient characteristics were predictive of poor self-reporting and if use of some drug types were reported poorer than others.
Methods 500 patients admitted to an acute medical department were interviewed about their medication use within the preceding week. Patients provided blood and urine samples. Home visits were performed 1 month after discharge among the patients reporting use of one of 5 predefined antidiabetic and cardiovascular drugs upon admission (amlodipin, bendroflumethiazide, digoxin, glimepiride, simvastatin). During the home visit, patients clarified recent medication use based on drugs in the home inventory. The patients provided additional blood and urine samples. The patients’ self-reported medication use was compared to prescription data (pharmacy records, PR) available from www.medicinprofilen.dk
. Blood samples drawn among users of the 5 before-mentioned drugs were analysed for digoxin contents. All available blood samples were analysed for contents of amlodipin, bendroflumethiazide, glimepiride and simvastatin. A subset of 100 urine samples collected upon admission was screened for contents of amphetamine, barbiturates, benzodiazepines, cannabinoids, cocaine, methadone and opiates
(=toxicology screening). All analysis results were compared to patients’ self-reported use.
Results Included patients had median age 72 years and 60% were women. Median drug use upon admission was 3 prescription only medications (POM). When comparing data from PR vs. self-reported drug use, 19% (95% CI: 15-23%) of POM purchased 0-7 days before admission and
27% (24-29%) of POM purchased 0-30 days before admission was unreported during the interview. Congruence between PR and self-reports was highest for cardiovascular drugs (p<0.05) whereas dermatologicals frequently were underreported. Younger patient age was the only patient characteristic predictive of higher congruence. Patients reported with higher congruence upon the home-visits (p<0.05), but still 11% (6-18%) of POM purchased during the preceding week and 18%
(15-22%) purchased the preceding month was unreported.
Overall, the patients’ self-reported use of the 5 cardiovascular/antidiabetic drugs was in high agreement with medication analysis (all Kappa>0.79, p<0.05). However, 36 patients (7%, 5-10%) reported in disagreement with analysis results. These patients had similar age and sex distribution as patients with congruent data.
5
The using prevalence of illicit drugs was low and no patients had screenings positive for amphetamine or cocaine. Among 12 patients (12%, 6-20%), the toxicology screening was positive for drugs not reported during the interview (cannabinoids: 5 patients, benzodiazepine: 7 patients).
This gave an overall sensitivity of self-reported drug use of 66% (48-81%). The predictive value of self-reported non-use of a drug was high (all negative predictive values >92%).
Discussion The inconsistencies between PR and self-reported drug use indicate underreporting - but non-adherence or alterations in regimen has to be considered.
Conclusion Despite interviews solely focusing on medication use, patients seem to underreport their medication use even when the interviews are performed in the patient’s own home. The use of cardiovascular drugs is however reported with high reliability. Illicit drug use seemed a minor problem but several patients underreported use of cannabinoids and benzodiazepines.
Perspectives PR might be useful in order to detect errors in the medication history upon hospital admissions – especially among the elderly. PR are available directly online to treating physicians.
The implementation of PR during medication reconciliation procedures might improve the medication history and subsequently prevent medication errors and adverse drug effects. Despite the accessibility of PR, any implementation still demands extra time and resources. The cost effectiveness of these procedures remains to be established. Drug analysis and toxicology screens are resource demanding and must be limited to complicated cases.
6
Abbreviations
ADR Adverse drug reaction
ATC
CI
Anatomical therapeutic chemical classification system
Confidence interval
GC
GP
LC
MS
NPV
OTC
POM
PPV
PR
UPLC
Gas chromatography
General practitioner
Liquid chromatography
Mass spectrometry
Negative predictive value
Over-the-counter products
Prescription only medication
Positive predictive value
Pharmacy records
Ultra high pressure liquid chromatography
7
I
Publication list
This thesis is based on the following manuscripts
Glintborg B, Poulsen HE, Dalhoff K
The use of nationwide on-line prescription records improves the drug history in hospitalized patients
British Journal of Clinical Pharmacology, Published online August 2007
II
Glintborg B, Hillestrøm PR, Olsen LH, Dalhoff K, Poulsen HE
Are patients reliable when self-reporting medication use? Validation of structured drug interviews and home visits by drug analysis and prescription data in acutely hospitalized patients
Journal of Clinical Pharmacology, 2007 Nov;47(11):1440-9
III
Glintborg B, Olsen LH, Linnet K, Poulsen HE, Dalhoff K
The reliability of self-reported use of amphetamine, barbiturates, benzodiazepines, cannabinoids, cocaine, methadone and opiates among acutely hospitalised elderly medical patients
Accepted for publication in Clinical Toxicology, July 2007
The manuscripts are available through www.pubmed.gov
8
1. Background
1.1. The medication history
The medication history is a list of the medications currently used by the patient.
1 The adverb currently emphasizes that the medication list is changeable and alters over time. Hence, the history should be updated when changes have occurred or when necessary e.g. at transitions in care or other situations where responsibility of care is handed off.
2;3
Upon hospitalisations, a detailed and updated medication history is often of relevance. This history should include: name of all used drugs including prescription drugs, herbals, over-the-counter products and vitamins; dosing regimen; and route of administration.
3
Optimally, indication for use, adherence to regimen, and when the last dose was taken should also be registered.
4
1.2. Why do we need a medication history?
Some authors have described the medication history as being a portrait of the patient’s health because it gives information about the patient’s diagnoses and health status.
5 Knowledge of the patient’s medication use is beneficial for diagnostic and therapeutic purposes: medication related issues might itself have prompted the patient to approach the health care system due to symptoms caused by e.g. under- or over-treatment, drug interactions or adverse drug reactions
(ADRs).
6-9 Furthermore, an important prerequisite before new medications are prescribed or drug regimens are altered is knowledge of which drugs the patient is already taking in order to avoid double-prescribing or inappropriate drug-drug interactions. Not only drug names but also drug doses are important in order to up-titrate introductory doses properly.
10;11
Insufficient medication histories may cause misinterpretation of symptoms and sub optimal treatment, and lack of knowledge of a patient’s current medication use is an important cause of medication prescribing errors.
12-14 Only 1% of medication prescribing errors actually cause harm.
15 However, it is estimated that medication errors and adverse drug effects contribute to more than half of the adverse events occurring in connection to hospitalisations.
16 The incidence of serious ADRs among hospitalised American patients is reported as 6.7% in a recent metaanalysis, 17 but is likely to be even higher among elderly and patients at increased risk due to e.g. decreased renal or hepatic function.
12;18;19 Approximately 6-8% of admissions to medical departments are attributable to ADRs.
9;20 ADRs are often preventable.
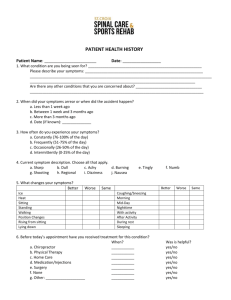
21 Causes and consequences of prescribing errors are schematically shown in Figure A.
12;15;21
Thus, an updated medication history in congruence with the patient’s current medication use is one of the prerequisites of safe drug prescribing.
8;22
9
Figure A. Causes and consequences of medication prescribing errors
Causes of prescribing errors:
Calculation of drug dose
Medications with similar names
Use of abbreviations
Unusual route of administration
Uncommon regimen
Complicated dosage regimen
Poor patient history taking
Medication history
Allergies
Chronic conditions
Medication prescribing errors
Potential harm
No potential harm
ADR (1%)
1.3. The quality of medication histories among hospitalised patients
The ideal health care system is seamless and allows unhindered transfer of information between health care sectors.
23 For practical purposes, this is difficult to achieve and every time information is communicated from one person to another, knowledge is potentially lost or distorted.
Vulnerability is especially present upon transitions in care (hand-offs), e.g. upon hospital admissions, transfer between departments, discharge to primary care, change of practitioner or changed level of care.
3;20
The quality of the medication histories in hospital files is known to be poor: up to
83% of patients have at least one error in their history registered upon admission.
1;8;24 These errors are often unintended and clinically important.
24-26 It is estimated that 27% of prescribing errors are caused by insufficient medication histories.
14
Misunderstandings and flaws occur when patients communicate with health care professionals or when information is transferred between carers.
1;23;27 Several barriers exist in the hand-off process e.g. physical barriers (noise, interruptions), social barriers (discomfort due to status and interpersonal power differences), language barriers, inconvenient medium of communication (communication in writing is less effective than verbal communication), or lack of time.
23 Furthermore, patients may be poor at reporting their medication use due to disorientation, acute illness, poor memory or aphasia.
1 Special problems apply to over-the-counter products, herbal medical products and dietary supplements which some physicians and patients fail to consider as medications and therefore neglect from the medication history.
28;29
Once a list is wrongly recorded, the mistake may be transferred unnoticed when the patient is discharged or referred.
11;30 Furthermore, alterations in therapy during hospitalisation may not be correctly noted in the discharge letters – or the discharge letter may be completely missing or lacking a medication list.
31-35
Errors in the medication lists are more frequently omission errors (failures of action) rather than errors of commission (incorrect actions).
8;24;36;37 Examples of omission errors are lacking registration of regularly used drugs upon hospital admissions 38 or unintended
10
discontinuation of long-term therapies.
39 Commission errors are the erroneous adding of medications to the medication lists despite not being used by the patient.
8
There is room for improvement when it comes to securing the hand-off processes in the health care system. Improved medication lists would minimize information loss and enhance supervision of treatment.
14;40
1.4. Terminology confusion
The medication history describes the drugs currently used by the patient. This must not be confused with listings of drugs prescribed for the individual patient, as these are not necessarily identical.
22;40-48 Reasons for lacking identity between the list of prescribed drugs and the list of used drugs may be found with the prescriber (lacking update of lists, involvement of multiple prescribers) or with the patient (non-adherence, misinterpretation of prescribed regimen).
49;50
Indeed, insufficient patient-physician communication about drug regimen sometimes result in conflicting perceptions of the prescribed drug regimen.
46;49;51
Medication adherence describes the extent to which the patient follows a prescribed regimen.
50;52 Adherence is also denoted compliance, and these terms are in the following used as synonyms. A prerequisite before even talking about adherence is knowledge of which regimen the patient should adhere to – that is, the regimen actually prescribed. In this respect, a medication list precedes any discussion of adherence. Where adherence rates describe medication use over a certain period of time, the medication list is a cross sectional description: which medications do the patient take at this time point or within this limited time span.
The fields of adherence and medication history taking may be perceived as two aspects of medication-taking behaviour, and although they in some ways differ, they are also closely interweaved and in many ways related. Many of the methods used in adherence research are also applicable when the aim is to construct a medication list as will be discussed below.
50;52-55
1.5. Methodologies available for data collection
Several methods may be used in order to obtain a medication history among hospitalised patients.
The patient’s self-reported drug use is important as only the patient himself is capable of accounting for non-adherence, self-medication, and use of medications on demand.
24;56 In hospital settings, the medication histories are often based on patients’ self-reports.
11;57 In research settings, the researchers often perform additional medication interviews with systematic focus on the patient’s medication use.
1;22;58 These interviews are traditionally performed at a later time point during the hospitalisation and may be used to confirm data obtained previously or may include data from other sources.
24;58-60 Often a semi-structured or structured technique is applied or pre-designed forms or questionnaires are included.
25;59;61-64 Photographs of tablets or prompting
11
with proprietary names may be used to enhance recall. 57;64-67 This interview-method is sometimes called secondary, structured, focused or comprehensive medication interviews.
Various other methodologies and aids are sometimes included in order to reduce patient’s recall bias and oppose the patient’s potential difficulty in remembering drug names:
Medication lists from treating doctors provide information about prescribed drugs. Upon hospitalisations, the lists from doctors in primary care (general practitioners or specialists) but also secondary care (previous hospital admissions, emergency room contacts) may be of relevance.
Lacking updates and involvement of multiple prescribers potentially make the lists mutually conflicting or incorrect.
22;41;42;44;68;69 Thus, the lists may serve as supplements and not as solitary source. The patient may be asked to collect all their medication containers in a bag and bring them upon the consultation (brown bag/medication bag method).
10;70 This procedure demands cooperation and preparation from the patient – but the patients seem willing to do this if they are properly informed in advance.
40;44;71 Ultimately, medication interviews performed in the patient’s home allow direct inspection of medication bottles and vials stored in the patient’s medication inventory.
42;72-74 Home visits are resource demanding but is thought to surpass bringing medications upon consultations.
72 Pharmacy records (PR) give information about the medications prescribed and dispensed for the individual patient.
43;75;76 Where physician records reflect the prescribed regimen, PR are one step ahead and show whether a prescription is actually redeemed - and how often.
47 Therefore, PR may be used to detect primary non-adherence or other adherence problems.
43;77-79 In pharmacoepidemiological research, the records are estimated valid as proxies for drug exposure.
75;80 Only little experience is available on how to implement pharmacy records directly on the patient level.
16;81 The accessibility of the records limits their practical use, and in most countries, the records are only available in local pharmacies.
24;75;82 If the patients attend more than one pharmacy, this renders the medication profiles of individual pharmacies incomplete.
47;70;83 Denmark is perhaps the only country that provides one common database based on pharmacy records from every national pharmacy - and that furthermore allows extraction of data on the individual patient level. The availability directly online makes the record of use to treating physicians in clinical settings.
68;84;85 Drug analysis where the occurrence of drugs is measured in blood or urine samples is a way to confirm which medication or drugs the patient is actually taking.
86;87 This method has especially been used in adherence research in order to validate self-reports.
86;88-90
Similar to the tradition in adherence research, strengths and weaknesses of the above mentioned methodologies may be outlined as in Table A.
50;52;91
12
Table A. Methods applicable when constructing medication histories. Advantages and disadvantages
Method
Self-report
Information from relatives
Medication bag
Home visits
Description
Patient-interview about drug use.
Structured techniques or directed recall may be used to enhance information
Of relevance among patients having recall bias or otherwise unable to provide a medication history
(children, demented, unconscious etc.)
The patient or relatives bring medication vials and bottles
Advantages
Immediately available
Necessary in order to validate information from other sources
Disadvantages
Recall bias
Influenced by interviewer-skills
Recall bias
Relatives might not be properly informed about drug changes etc.
Minimizes recall bias Demands cooperation from patient or relatives
Minimize recall bias Resource demanding
List of prescribed drugs
Visits in the patient’s home and inspection of medication vials
List of drugs prescribed by physicians in primary or secondary care
Medication list from district nurse
List of drugs dispensed from the district nurse
Pharmacy records List of all drugs dispensed from a pharmacy
Drug analysis Analysis of blood or urine for drug contents
Often readily available
Not always updated
Not necessarily in agreement with the patient’s actions
Minimizes recall bias Not always updated
Not necessarily in agreement with the
Illustrates long term
Objective drug use
Objective
Illustrates short term drug use patient’s current medication use
Prescribed regimen may have altered since the prescription was issued.
Refilled drugs are not necessarily used
OTC are not included
Requires closed pharmacy system
Resource demanding
Not always available
Only recent drug use verified
Result influenced by patient specific kinetics
Resource demanding
1.6. The gold standard – the perfect medication history
Unfortunately, we have no scale on which we can measure the quality of an actual medication list, and there is no gold standard list or method that with certainty includes all the patient’s currently used drugs.
70;76;92 This unfortunate problem is solved in various ways in the literature. Some authors decline from stating the yardstick and instead report the discrepancies between available lists as this indirectly implies problematic recording.
82;93
Most authors directly or indirectly state a gold standard. Some have used physician interviews, 46 medical records, or pharmacy data as the gold standard.
65;66;76;94-96 However, focused medication interviews are generally perceived as the most accurate method to obtain medication information.
47 The medication interviews may be performed face-to-face either upon hospital contacts 1;22;97 or in the patient’s own home; 30;42;47;64;66;72;74-76;98;99 or by telephone.
11;65;74;100
Although structured medication interviews improve the traditional medication history written in hospital files, the structured interview does not necessarily include 100% of used drugs for several reasons. Firstly, despite the efforts to reduce the patient’s recall bias, forgetfulness cannot be completely ruled out.
24;28;29;40;53 Secondly, patients may underreport use of medications that they not consider important, e.g. over-the-counter products, tranquillisers, minor analgesics or drugs used on demand.
28;29;101;102 Thirdly, patient’s might deliberately
13
underreport use of drugs with misuse potential 103 or psychotrophic medications 104 due to embarrassment.
The gold standard method is perhaps a combination of various methodologies.
47 The more sources available, the better the chance of detecting all prescribed medications and reducing recall bias.
56 The most valid records are probably obtained by combining patient’s review of existing data with inputs from patient providers.
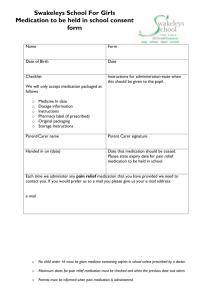
11 The theoretical way towards a complete medication history is illustrated in Figure B.
Figure B. How to improve the medication history.
Schematic presentation of methods and sources that improve the medication history
The patient’s selfreported medication use
Drug analyses
Medication list from district nurse
Home visits, home inventory
Pharmacy records
MEDICATION
HISTORY
Medication bag
Information from relatives
Medication list from GP or other prescribing doctors
Previous hospital files
1.7. Secondary medication interview among in-hospital patients
Several studies have applied secondary medication interviews among hospitalised patients in order to detect errors in the traditional medication history. Table B is a listing of such studies identified through a PubMed Medline search.
105 The table is partly based on a recent systematic review covering the frequency and clinical importance of medication history errors at admission to hospital.
8 The authors Tam et al. found 22 studies that compared the traditional medication history obtained at the time of hospital admission (referential method) versus a comprehensive medication interview among adult inpatients. The authors outlined their search strategy in www.cmaj.ca/cgi/content/full/173/5/510/DC1 . We imitated the authors’ search in order to identify recent publications. We found 5 of the 22 studies given by Tam et al. unidentified during the search, and we found no additional studies using the search strategy. This illustrates the lack of uniformity of chosen keywords in this area of research. However, by reviewing “Related articles, links” in PubMed of all 22 studies listed in the publication and by hand-searching references, we found 6 additional studies.
22;41;60;106-108 Furthermore, we identified 2 studies published in
Danish.
68;85 One of these used the medication list provided by GP as the referential method.
68
14
Table B. Secondary medication interviews among in-hospital patients.
Overview of the methodologies used, profession of interviewer, and the percentage of patients identified with erroneous medication histories. 1;25;26;48;58;61;62;106;107;109-119
The column OTC included indicates whether over-the-counter drugs are included in the given percentages and results.
Country Ref. no.
N Patient category included
Methodology Patients with errors, %
Other results
P
DK
Australia
Canada
Holland
UK
USA
22
68
85
41
24
81
100
48
64
151
Medical
Medical
Medical
Elderly
Medical
63 43 Medical
59 80 Medical
Surgical
120 304 Medical
60 80 Medical
48 60 Medical
109 80 Medical
108 222 Medical
110 60 Medical
111 328 Medical
Surgical
R - + - - Ph/MD
+ - R - - ?
R + + + - Ph
R - + - - ?
R + - - + Ph/
MDSt/
PhSt
R - - - - Ph
R - - - - Ph
R
R
R
R
R
R
R
+
?
-
-
-
-
-
-
?
+
+
+
-
-
-
?
-
-
+
-
-
-
?
+
-
+
-
-
PhSt/MD 67 -
Ph
Ph
Ph
Ph
Ph
Ph
112 1053 Surgical
113 33 Elderly
58 86 Medical
R - - - - MD
R - + - - Ph
62 146 Gynecol. R - - - - Ph
61 109 Psychiatry R + + - - Ph
25 50 Medical R - - - - Ph/
Nurse
R - - - - Ph
91 -
63 -
69 -
36 -
54 -
- -
57 -
40 -
48 -
34 -
54 - - ?
42 - - +
- - - - More items identified
10 -
73 -
-
-
-
-
61 -
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
+
-
-
-
-
- More items identified
-
-
-
+
+
-
+
+ 31% more items identified
+
+ 2 times more POM and 10times more OTC identified
- 3.2 additional POM identified per patient
114
1
186
122
Medical
Elderly
115 58 Medical
Surgical
26 204 Medical
Surgical
116 100 Males
R
R
R
-
-
-
-
-
-
-
-
-
-
-
-
Ph
?
Ph
75 - - +
60 52 - -
- - - - 2.7 more POM identified per patient
R + - - - Ph/PhSt 55 - - +
107 252 Trauma centre
R - - - - Ph
R + - + + Ph
-
-
-
-
-
-
- 42% more items identified
? 34% more items identified
117 50 Psychiatry R - - - - Ph/PhSt - 24 16 -
118 247 Various R + - - - Ph - - - - More items identified
106 100 Various
119 205 ?
R + + - - Ph
R + + + + Ph
- - - - More discrepancies identified
- - - + 87% more items identified
Abbreviations, table B:
R: referential method
?: not reported
+: method included
MD: physician
-: method not included
Ph: pharmacist St: student
15
Although the articles included various patient groups and used different terminologies and methods in order to describe any discrepancies, the uniform conclusion was that medication interviews provided more accurate medication lists compared to the standard lists.
We scrutinized the articles with specific focus on which methods that had been applied during the data-collection. As shown in the table, 9 studies included data from pharmacy records whereof 5 of these included the records as routine 61;85;118-120 and 4 studies only used PR in selected cases.
24;26;106;107 Medication bags and medication lists from prescribing doctors or district nurses were included to a various degree. None of the studies included drug analyses. This illustrates onemajor problem in this field: despite the widespread acknowledgement of secondary medication interviews, little is known of how the method most optimally is applied. Is the inclusion of specific data sources of particular interest? Which sources contribute additional information – and which patient groups deserve extra attention?
Secondary medication interviews are to an increasing extent used in clinical settings with the aim to improve patient management and reduce medication errors.
121-123 This underscores the need for method-validation even further.
The few studies that have questioned the validity of patient’s self-reported medication use during structured medication interviews have mainly addressed ambulatory patients: In a study by Psaty et al., the patients’ self-reported use of beta-blockers and betaagonists guided by drugs stored in the home-inventory was associated with heart rate whereas structured questioning alone was not.
124 Smith et al. showed that ambulatory elderly included in a cardiovascular study reported in high congruence with drug analyses.
86 The interviews were performed during a clinic visit and were guided by the patient’s medication bag. In another study performed in primary care, the authors compared data on theofylline use obtained by physician interview, patient interview, chart audits and videotaped observations in patients with obstructive pulmonary disease. They found frequent disagreements between the methods and used an iterative procedure to identify the “truth” best capturing data. Based on this approach, they concluded that the patients over-reported drug use and that physician interviews were more accurate.
102 One study validated a questionnaire technique by use of 6 actors with a predefined medication history simulating to be patients.
59 Kelly et al. performed duplicate interviews among
510 hospitalised patients.
125 Self-reported medication use was considered reliable if the patient reported concordantly during the two interviews. The authors concluded the patients to report medications used for longer durations of time (oral contraceptives) more consistently than drugs taken intermittently (aspirin, penicillin).
Thus, although the methodological difficulties and the lack of gold standards of this area seem widely acknowledged, few have specifically aimed to test the reliability of structured medication interviews and the potential benefit of including other data sources. There especially seem to be a noticeable lack of studies addressing in-hospital patients.
16
1.8. Factors affecting reliability of self-reported medication use
The methodology of data collection is one main reason for invalid information about medication use. However, patient characteristics are a second possible contributor of non-random error.
74
It would be convenient if patient characteristics revealed the patients having most difficulties self-reporting their drug use. Various factors might be suggested e.g. gender, poor vision (impair ability to read writing on pill boxes), poor memory, need of help from others during drug-dispensing, social status, multiple drug use, complexity of regimens, multiple prescribers or older age (correlated to multiple drug use, poor vision and poor memory).
8;41;44-46;126;127 Health literacy and the ability to read, understand and act on health information is another factor potentially affecting medication taking behaviour.
53 The application of various methodologies and endpoints makes interpretation across studies difficult, and where some studies find special attention necessary especially among elderly, 94 impaired 74 using polypharmacy 45;126 - others find these factors of no significance.
49;72
Similarly, drug characteristics might influence the reliability of self-reporting. As previously mentioned, patients tend to underreport medications used on demand, tranquillisers, antidepressants, weak analgesics and over-the-counter products.
28;29;101;104 On the other hand, cardiovascular drugs 86 and drugs prescribed for serious conditions 70 seem to be reported with higher reliability.
1.9. Background summary
In short, the background for performing the following study was:
1.
Insufficient medication lists and lack of knowledge of the patient’s current medication use are important causes of medication errors and ADRs
2.
There is no gold standard method that with certainty measures the patient’s current medication use
3.
Structured secondary medication interviews improve the medication lists compared to the routine medication histories written in hospital files
4.
Secondary medication interviews are widely used, but the benefits of including additional data from drug analysis or pharmacy records is sparsely known
5.
The reliability of secondary interviews might vary according to drug types or patient characteristics
6.
Knowledge of the reliability of patient’s self-reported medication use is of interest for research purposes but also in the daily clinical practise
17
2. Aims and hypotheses
The aim of this thesis was
To describe secondary medication interviews, pharmacy data and drug analysis as methods for the construction of a reliable medication history among acutely hospitalised medical patients
The thesis was based on the following hypotheses
Patient’s self-reported medication use during secondary medication interviews is subjected to recall bias
Recall bias may be detected if the data obtained during the interviews is compared to pharmacy records or drug analysis
The reliability of patient’s self-reported medication use varies according to drug and patient characteristics
Patients report with less recall bias during visits in their own homes compared to in hospital
Pharmacy records and drug analysis may be useful in daily clinical practise in order to detect and minimize recall bias and to reduce medication errors.
18
3. Materials and methods
The materials and methods are described in details in Appendix I-III. In the following sections, the motives for choosing various methodologies are discussed.
3.1. Study sample
The study was conducted at the acute medical emergency ward at Bispebjerg University hospital in Copenhagen. This ward was chosen because it accepted patients with a wide range of medical diseases directly from primary care. Therefore, our results could possibly be generalized to similar settings. On the other hand, if the study had been performed at Rigshospitalet, not many other settings would be expected to be similar as this hospital mainly accepts carefully selected patients from secondary care or patients with predefined diagnoses.
Medical in-patients were selected as it is of particular importance to obtain a comprehensive and complete medication history in these patients: the hospitalisation may be immediately induced by medication related problems.
6;9;18;83;128-132 The medication list often needs revision or adding of further drugs and undisclosed medication use implies risk of unintended drug interactions or adverse drug effects.
14;106;113 Medical patients are often elderly and treated with polypharmacy and this gives specific problems with recall bias.
1;124 Thus, the process of medication history taking is of special interest and implies special problems among medical patients.
133
3.2. Patient characteristics
A number of factors are potentially related to medication taking behaviour.
53;134 Thus, for each patient, the following characteristics were recorded: sex (male/female), age (years), social status
(single/cohabit), housing (nursing home yes/no), need of help when dispensing medicines (no/yes relatives/yes district nurse), use of compliance aids e.g. boxes or containers for the dispensing of appropriate pills (yes/no), educational level measured as years of schooling (<=9 years/>10 years), current employment (working/unemployed/retired).
During the home visit, the patient’s vision was tested with a reading board when the patient was wearing usual glasses or lenses (poor/normal vision). Cognitive status was roughly measured by clock-drawing test (correct/not correct) and the patient’s ability to remember three words after diversion (yes: three words remembered/no: 0-2 words remembered).
135;136
3.3. Medication history
Data from several sources was included in order to describe the patient’s medication use:
Upon admission: The drug history written in the hospital file
A focused medication interview
Drug analyses
19
After discharge:
Pharmacy records
A focused medication interview performed in the patient’s home
Drug analyses
Pharmacy records
Motives for the inclusion of individual sources are described in detail below.
3.3.1 Hospital files
The medication history routinely written in the hospital files was used as supplementary to data obtained during the structured interviews in order to describe the over-all knowledge about the patients medication use upon the hospitalisation. We did not explicitly aim to describe the validity of the hospital files because this has previously been done in detail (Table B). Hospital files were not available until the data-processing stage and the files were not included during the interview.
Therefore, the patients were not confronted with any inconsistencies and were not asked to verify these data.
3.3.2. Medication interview upon admission
A physician (BG) performed all the medication interviews. The optimal profession and educational background of interviewers when medication information is gathered is a matter of debate.
25 Most agree that counselling skills and medication knowledge are necessary 26 and that the interviewer must have necessary training or must be a health care professional (e.g. nurse, pharmacist, physician). However, in many previous studies, the detection of omission errors in the routine medication histories has included a secondary medication interview performed by a pharmacist
(e.g. several of the studies shown in Table B). This has lead some to conclude that pharmacists are better than physicians when it comes to the construction of the list of currently used drugs, 58;62;108;111;118;119;137 and that patients prefer to report non-adherence and any use of OTCs or illicit drugs to a pharmacist.
62;110;117 However, focus on medication related issues and more time may be the important elements of the process.
117;138 In clinical settings, it has been shown that although physicians widely appreciate the patient’s medical history as an important source during the diagnostic process, 133 they often fail to record the information correctly.
139;140 Proper education and attention among physicians might improve the medication histories.
112;141 Qualitative studies and appropriate study designs are necessary in order to make valid statements about preferred interviewer profession.
118 To our knowledge, no such studies exist and we were of the opinion that focus and time was of higher importance than profession. Furthermore, BG had interviewer skills and experience from previous studies.
30
It was emphasised to the patient that BG had all the time necessary and had a specific interest in learning more about the patient’s medication use. The patient was encouraged to speak freely, and it was stressed that BG came from another hospital and was not involved in the patient’s treatment. This was in order to make the patient feel as comfortable as possible. A
20
semi-structured interview technique was used; open-ended questions were followed by closedended in order to minimize the patient’s recall bias.
46;51 Patients were prompted to mention drugs applied locally on skin, eye drops, nose drops, inhaled medications and over-the-counter products. Furthermore, the patients were asked if they ever used cannabinoids or other illicit drugs. Specifically made forms were filled during the interview in order to secure a complete dataset. The interview was guided by the patient’s personal in-home medication list, list of prescribed drugs from referring doctor, or listings of dispensed drugs from district nurse - if any of the lists were available. The patient was asked to verify any use of the listed drugs. We made no efforts to gather additional lists. The overall objective was to obtain the optimal conditions for the patient’s to self-report their drug use - but only with use of the data-sources already available.
3.3.3. Medication interview after discharge
Home-visits are resource demanding and time consuming. Therefore, we chose during the designing phase of the study only to perform visits in a subset of patients. Cardiovascular and antidiabetic drugs are among the most frequently used drugs in Denmark.
84 Diabetics and patients with cardiovascular disease often use numerous drugs daily – and several of these drugs are used for diseases and risk factors that only cause limited symptoms e.g. hypertension and hypercholesterolemia. Thus, we expected these categories of patients to have specific problems correctly reporting a complete medication list.
46;102 We decided only to perform home-visits in the subgroup of patients reporting use of digoxin, bendroflumethiazide, amlodipine, simvastatin and/or glimepiride upon admission. Analytical and pharmacokinetic considerations were additional decisive factors: the drugs should be practically measurable in our laboratory and the drugs should have an elimination time long enough to make them detectable 12-24 hours after intake.
86;142
During the home visit, the patient was asked to present all the drugs stored in their home. Based on the drugs stored in their home inventory, patients accounted for current and recent medication use again using a semi-structured interview procedure.
3.3.4. Pharmacy records
Information on all drugs acquired on prescription from any Danish pharmacy during the preceding 2 years was obtained from www.medicinprofilen.dk
. This represents real-time data as the handling of prescriptions includes direct electronic reporting on-line to the central database.
84
We calculated the time interval between the registration in PR and the patient interview for individual drugs as number of days between the two dates. Generic drugs were only included once per patient, and the time interval was given according to the registration date in PR closest to the interview.
Methodological considerations are important in order to identify the relevant records from PR. It is difficult to determine length of treatment periods and the currently used regimen
21
from PR alone. Two approaches are traditionally used: 1) fixed time windows: all records registered within a predefined time interval before the interview are considered relevant 2) calculation of legend times based on package size, prescribed regimen or DDD where drugs prescribed before the interview and with theoretical end-dates in close proximity to the interview date or later are considered relevant.
47;75;120 During the first approach, long time windows ensure high sensitivity: more of the drugs currently used by the patient are included from PR. However, the longer the time window, the lower the positive predictive value (PPV) and fewer of the drugs identified in PR are actually used by the patient. The second approach also imply complications e.g. the drug may be used less/more frequently than prescribed which leads to a altered treatment period, prescribed regimens may be changed by treating doctors, or the drug may be prescribed according to agreement or on demand.
75;143
When we accessed the Danish PR, we discovered that many regimens were stated as either according to agreement or were not stated at all. Therefore, we chose to apply the fixed time window method where the time window was related to the interview date and relevant records were included retrospectively from this date. This method is perhaps also easier to apply and understand within a clinical setting. In order to obtain a high PPV, we chose short time windows of one week and one month when estimating omission errors. On the other hand, a 2-year time window was applied in the description of commission errors in order to ensure a high sensitivity.
3.3.5. Drug analysis on blood and urine samples
Blood and urine samples for drug analysis were obtained upon admission and during the subsequent home visit.
Plasma contents of amlodipine, simvastatin, glimepiride and bendroflumethiazide were measured semi-quantatively on all blood samples available. These analyses were performed in our own laboratory at Department of Clinical Pharmacology, Rigshospitalet. Analyses were not available as routine and had to be developed especially for this project. This development was performed by two of the department’s chemists (Lenette Holm Olsen and Peter Hillestrøm). A major challenge was that drugs used in therapeutic doses are only present in plasma in low concentrations.
144-147 Eventually, the UPLC (ultra high pressure liquid chromatography) method was the only method capable of measuring drug levels in plasma with sufficient sensitivity. For description of extraction, separation and detection methodology see Methods Supplementary
(written by LH Olsen and P Hillestrøm).
Analyses for the plasma contents of digoxin were performed with a quantitative, immunoassay procedure (Elecsys, Roche) at Department of Clinical Biochemistry, Rigshospitalet.
Due to the resource demanding nature of this externally performed analysis, we limited the analysis to patients considered of particular interest. Therefore, plasma-digoxin was only measured in samples drawn among the patients reporting use of digoxin, bendroflumethiazide, amlodipine, simvastatin or glimepiride upon admission. This selection would exclude mainly non-
22
users, but we would still include both users and non-users of the individual drugs. Subsequently, we could calculate both negative (NPV) and PPV, sensitivity and specificity of self-reported medication use, where NPV=reliability of stated non-use, PPV=reliability of stated use, sensitivity=the ability of self-reports to identify medication use, specificity=the ability of selfreports to preclude medication use.
Among a randomly selected sub sample of 100 patients where urine samples were available upon admission, we performed a toxicology screening for urine contents of amphetamine, barbiturates, benzodiazepines, cannabinoids, cocaine, methadone and opiates.
This screening is available and set up as a routine analysis. Toxicology screenings unexpectedly positive for drug contents as compared to the interview data were verified by substance specific analysis either in our own department by urine-GC-MS method or at Department of Forensic
Chemistry by plasma-LC-MS/MS method. The urine verification analysis was advantageous in detecting use of illicit drugs over longer periods of times and was used for the substance specific analysis of amphetamine, cannabinoids and cocaine. On the other hand, plasma verification analysis indicated only very recent drug use and was used for the analysis of benzodiazepines, barbiturates, methadone and opiates.
3.4. Statistical analyses
The use of drugs was reported using descriptive statistics. Independent groups of data were compared by Chi square tests (for categorical data) and t-tests (for continuous data). We used multiple logistic regression analysis in the comparison of pharmacy data and self-reported drug use. We used a generalized estimating equation (GEE) model due to possible clustering of data at patient level. Thus, each record described data regarding one drug, but as the patients’ often used several drugs, the information on each patient consisted of several records. The model was constructed in collaboration with the Department of Biostatistics, Kommunehospitalet.
Kappa analysis was used as an estimator of agreement in the comparison of drug analysis (amlodipine, bendroflumethiazide, digoxin, glimepiride or simvastatin) and self-reported drug use in order to include both false negative (drugs detected but not reported used) and false positive results (drugs not detected but reported used). The comparison of self-reported use of amphetamine, barbiturates, benzodiazepines, cannabinoids, cocaine, methadone and opiates versus drug analysis was reported using sensitivity and negative predictive values instead of kappa in order to emphasize false negative self-reporting (underreporting)and not false positives.
Statistical tests were considered significant for p<0.05.
23
4. Results
The patient characteristics are shown in Table C.
Table C. Patient characteristics
Characteristic
Age, years (range)
Male
Female
Social status Single
Cohabit
Nursing home resident
Help with dispensing medicines
Yes
No
No
Yes, relative
Yes, nurse
Use of compliance aids
Educational level
Current employment
Yes
No
<=9 years
>10 years
Working
Unemployed
Retired
Vision. Reading test Poor vision (<=0.2)
Normal vision (>0.2)
Memory. Correct clock drawing test
Yes
No
Missing
Memory. Remembers tree words
Yes
No
Missing
Number of patients
Admission*
N=500
72 (17-97)
Home visit **
N=115
77 (22-96)
202
298
305
195
39
76
81
34
13
487
369
31
100
169
331
340
160
105
16
379
-
-
-
-
-
-
-
-
54
43
18¤
47
61
7¤¤
4
111
70
5
40
68
47
74
41
11
1
103
10
105
*) Status upon admission
**) Status upon home visit
Patients with home visits are included in both columns.
¤) Blind, hemiparetic, or did not wish to participate
¤¤) Did not wish to participate
As shown in Table D, a complete set of data (interview, PR, hospital files, blood and urine samples) was not available in all patients. A total of 495 patients provided blood samples upon admission; all samples were drawn within 1 hour after hospitalisation. In 10 patients, all sample material was spent for digoxin analyses or toxicology verification analyses. Therefore, only
485 admission samples were available for the analysis of bendroflumethiazide, amlodipine, simvastatin or glimepiride.
Table D. Data available upon admission and during home visit
Data type
Hospital file
Secondary interview
Blood sample
Urine sample
Pharmacy record
Admission
N=500 patients
Available Not available
500
500
495
246
493
0
0
5
254
7
Home visit
N=115 patients
Available Not available
-
115
111
90
115
-
0
4
25
0
24
It proved difficult to obtain urine samples upon admission. The samples were most conveniently collected immediately following the medication interview for two reasons. Firstly, the interview was performed shortly after the patient’s admission and therefore, the number of patients that had received treatment within the hospital would be minimal. This was important, as the urine analysis should represent medications used before hospitalisation. Secondly, if the patient provided the sample on BG’s request, then BG could personally mark the samples as an alternative to various nursing staff collecting and marking the samples. However, several patients were unable to produce a urine sample on request mostly due to sparse fluid intake, incontinence or inability to attend the toilet facilities. Consequently, urine samples were only available in half of the patients included.
Urine sampling was more successful during the home visits where 90 of 115 patients
(78%) provided a urine sample. The patients were seldom bed confined, they were feeling well and had had regular fluid intake. However, these samples have not been used for drug analysis at present.
4.1. Sequence of reporting
We mainly report data on the use of prescription only medications (POM) defined as medications only available on prescription and categorised according to the ATC-system.
148 This is opposed to over-the-counter medications (OTC), which are ATC coded but available without prescription, and herbal remedies and dietary supplements which have no ATC code.
28;84
We aimed to describe the methods of medication interviews, drug analysis and pharmacy records in the construction of complete medication histories. In order to detect recall bias and to test the reliability of medication interviews, data obtained by this method was compared to data from drug analysis and pharmacy records. The reliability of self-reports might vary depending on drug type, and we therefore reported the results in several parts corresponding to method used and drug type investigated. These parts correspond to the three manuscripts
(Appendix I-III). The sequence of reporting is illustrated in Table E.
Table E. Methods and results reported in manuscript I, II and III
I
II
Manus Drug types investigated
III
All POM
Amlodipine, bendroflumethiazide, digoxin, glimepiride, simvastatin
Amphetamine, barbiturates, benzodiazepines, cannabinoids, cocaine, methadone, opiates
Time point Method 1 >< Method 2 Supplementary methods
Admission
Home visit
Admission
Home visit
Admission
Self-reports
Self-reports
Self-reports
PR
Drug analysis
(blood)
Drug analysis
(urine- and blood)
Hospital files
Hospital files
PR
PR
25
4.2. Overall drug use
During the medication interview performed upon admission, the 500 patients reported use of
1818 POM (median 3 different generic drugs per patient, range 0-14) either daily or on demand during the preceding week. As shown in Table F, the drugs most frequently reported were cardiovascular drugs and drugs from ATC group N (e.g. analgesics and anxiolytics).
There was not complete agreement between the drug use reported during the medication interview compared to the medication list in the hospital files. A total of 140 POM were only mentioned in hospital files and 352 POM were only recorded during the interview. This yielded 1958 drugs mentioned one place or the other.
The 115 patients visited in their home reported use of 663 POM (median 6 drugs per patient, range 1-14) during the week preceding the visit. As the patients were selected based on their antidiabetic and cardiovascular drug use, drugs from ATC group C were not surprisingly the most frequently used (Table F).
Table F. Number of drugs reported as being used during the medication interview upon admission and home visit. By ATC group
ATC Drug category Admission Home visit
A
B
C
D
G
H
Alimentary tract and metabolism
Blood and bloodforming organs
Cardiovascular system
Dermatologicals
J
L
Genito urinary system and sex hormones
Systemic hormonal preparations, excluding sex hormones
General antiinfectives for systemic use
Antineoplastic and immunomodulating agents
Musculo-skeletal system M
N
R
S
Others
Total
Nervous system
Respiratory system
Sensory organs
Number of used drugs
Percent, %
(95% CI)
186 10 (9-11)
84 5 (4-6)
581 32 (30-34)
10 1 (0-1)
60
24
3 (2-4)
1 (1-2)
81
14
4 (3-5)
1 (0-1)
71 4 (2-8)
398 22 (20-24)
275 15 (13-17)
29 2 (1-2)
5
1818
0 (0-0)
100
Number of used drugs
Percent, %
(95% CI)
76 11 (9-14)
44 7 (5-9)
287 43 (39-47)
4 1 (0-2)
15
8
2 (1-4)
1 (1-2)
10
8
2 (1-3)
1 (1-2)
20 3 (2-5)
107 16 (13-19)
73 11 (9-14)
8 1 (1-2)
3
663
0 (0-1)
99
4.3. Prescription data from pharmacy records
The patient’s self-reported drug use upon admission was compared to the registrations in PR: among the 1958 POM reported used according to either hospital files or interviews, 114 POM where unregistered in PR (6%, 95% CI 5-7%). Among the 1818 POM only reported during the secondary interview, a similar proportion was reported (p>0.05) and 95 POM (5%) were unregistered (78 patients). Probable reasons for the lacking registrations might be errors of
26
commission, or that the drugs were acquired outside the pharmacy system. The unregistered drugs came from various ATC groups without any apparent trend.
Half of the POM reported used during the medication interview was registered in PR
0-34 days previously, but 27 patients reported use of drugs dispensed more than one year previously. This illustrates that if one wishes to detect the patient’s entire drug use from PRs, a very wide time window has to be applied. On the other hand, a large proportion of drugs are detected by use of e.g. a 0-2 month’s time window. This pattern may be of use if the PR’s were to be applied in a clinical setting for example in demented, unconscious, or intoxicated patients unable to provide a medication history.
Subsequently, we compared the registrations in PR to the self-reported drug use. If the patients omitted to mention use of drugs otherwise registered in PR, this might be due to an error of omission (the patient forgets to mention a currently used drug). Alternatively, the drug was no longer used (discontinuation of therapy by health care professional or by the patient himself (non-adherence)). In order to obtain results as conservative as possible, drugs were considered reported by the patient if mentioned either during the medication interview or in the medication history in the hospital file. The results are reported in Appendix I. A total of 61 patients (12%) did not report use of one or more drugs registered in PR 0-7 days before admission whereas 180 (36%) omitted to mention drugs purchased within the preceding month.
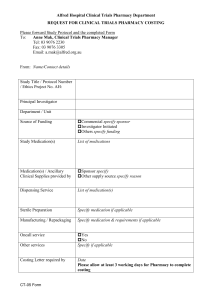
As shown in Figure C, the proportion of POM registered in PR but not reported upon admission varied according to the selected time window. For example, 56% of POM bought 80 to
90 days before admission were unreported whereas 22% of POM bought during the 10 days preceding admission were unreported.
Figure C. Proportion of drugs registered in pharmacy records but not registered in either hospital file nor reported used upon admission
Proportion of drugs not registered
0,6
0,5
0,4
0,3
0,2
0,1
0
0-10 11-20 21-30 31-40 41-50 51-60 61-70 71-80 81-90
Time interval, days, between pharmacy registration and admission
27
According to logistic regression analysis, ATC group was predictive of whether drugs registered in PR 0-30 days before admission were actually reported upon admission (p<0.05): cardiovascular drugs were reported most frequently whereas the odds of reporting drugs from ATC group N, A, R, S, M, J, D were significantly lower (corrected for patient sex and age). Drugs dispensed several times in the preceding 6 months were more likely to be reported, but inclusion of this variable in the analysis only slightly affected the odds ratios coupled to the effect of ATC group. The detailed results of the logistic regression analysis are shown in Appendix I.
A total of 363 patients had purchased one or more drugs from a pharmacy in the month preceding hospitalisation. Patients not reporting one or more of these drugs upon admission were significantly older than patients reporting all prescribed drugs (72 vs. 68 years, p=0.02), whereas there were no sex differences (37 vs. 38% males, p>0.05). Social status, residence, help with dispensing medicines, use of compliance aids, educational level, employment, vision, memory or number of used drugs did not affect reporting level.
The registration percentages upon admission compared to home visits were calculated and compared for two different time windows: 1) For a time window of 0-30 days, 801 of the 1153 POM (69%) purchased from a pharmacy were reported upon hospitalisation whereas during the home-visit, 278 of 340 POM were reported (82%). 2) For a time window of 0-7days, 305 of 400 POM (76%) were reported upon admission and 99 of 111 POM (89%) were reported during the home visit. For both these time windows, the reporting rate was significantly higher during the home interview compared to upon hospitalisation (both p<0.05). This indicated that home interviews were superior and reduced omission errors compared to interviews performed inhospital.
4.4. Drug analyses on blood and urine samples
4.4.1. Amlodipine, bendroflumethiazide, digoxin, glimepiride and simvastatin
The drug analyses for blood contents of amlodipine, bendroflumethiazide, digoxin, glimepiride or simvastatin were in high agreement with the patient’s self-reported drug use during the 0-24h preceding admission, and all the lower bounds of the 95% confidence interval for Kappa exceeded
0.79. Overall, there were 42 occurrences where the self-reported drug use was incongruent with drug analyses upon admission or during home visit (36 patients, 7% of patients). These 36 patients had similar age and sex distribution as patients with congruent data (both p>0.05). In total, 9 patients (2%) reported use of drugs that were not detected in their blood samples and in
29 patients (6%), the blood samples contained drugs not reported during the medication interview
(2 patients are counted in both categories). Inconsistencies occurred both upon admissions as well as during home visits.
Among the drugs detected in blood but not reported by the patient during the interview (30 drugs in 29 patients), 13 (43%) were registered in the patient’s PR. These registrations all occurred within 10-68 days preceding the interviews. In 5 patients, the
28
unreported drugs were registered in the hospital files. When categorizing a medication user as a patient having the drug present in their blood sample, the sensitivity of interviews, hospital files and PR in detecting users was all over 80% with no significant differences between the 3 methods.
Further details are shown in Appendix II.
4.4.2. Amphetamine, barbiturates, benzodiazepines, cannabinoids, cocaine, methadone and opiates
These drug analyses and the comparison to self-reported use was only performed on data acquired upon admission. The self-reported prevalence of illicit drug use was low, and among the
500 study participants, none reported use of amphetamine or cocaine whereas 8 patients (2%) reported occasional use of cannabinoids.
A total of 4 patients (1%) reported use of barbiturates in the week preceding admission, 65 patients (13%) used benzodiazepines, 8 patients (2%) used methadone, and 103 patients (21%) used opiates.
The 100 patients randomly selected for drug analysis had similar age and sex distribution as all patients included (p>0.05). Overall, 12 patients had not reported use of a drug
(cannabinoids or benzodiazepine) that was subsequently detected by drug analysis. This yielded an overall sensitivity of drug interviews in identifying drug use of 66% (95% CI: 48-81%) The 12 patients underreporting drug use had similar age and sex distribution compared to all screened patients (p>0.05).
Among 1 of the 7 patients underreporting benzodiazepine use, a benzodiazepinecontaining drug was registered in the patient’s PR 50 days before admission.
The NPV when a patient denied use of a drug was high for all 7 drugs screened indicating that the patients were reliable when they denied use of the drugs screened. The low frequency of use of individual drugs was however a major attributor to the NPV (many true negatives). See Appendix III for further details.
4.5. Over-the-counter products
It was not a primary aim of this thesis to describe the patients’ use of OTC as this has previously been done in detail.
28;29 However, a major concern when the use of pharmacy records is discussed, is the lacking registration of over-the-counter products. Therefore, it is of relevance to describe a few details on this subject.
In Denmark, OTC are despite their over-the-counter status sometimes prescribed for the patients due to reimbursement regulations and less patient self-payment.
84 Prescribed OTC are of course registered in the PR. In the present study, patients reported use of 995 OTC (median
2, range 0-8) during the admission interview. The drugs most frequently reported were from ATC group N (weak analgesics) and A (laxatives, potassium). Among the 506 OTC reported used every day in the preceding week, 310 were registered in PR (61%) whereas 221 of the 489 OTC (46%) not used daily were registered in PR. Thus apparently, the OTC used daily were more frequently acquired on prescription (p<0.05). The high prescription rate of over-the-counter products may
29
possibly be explained by reimbursing of e.g. acetylicsalicylicacid and acetaminophen-containing products when prescribed to senior citizens. In these populations, PR might provide valuable information of OTC-use – at least in Denmark and countries with similar reimbursing policies.
When comparing the registrations in PR to patients’ self reported use upon admission (in either hospital file or during interview), 84 OTC were dispensed 0-7 days before admission whereof 18 were not reported (21%). Similarly, 272 OTC were dispensed 0-30 days before admission whereof 77 (28%) were not reported. These reporting rates were not different compared to reporting of POM (p>0.05). Thus, patients appeared not to distinguish between OTC acquired on prescription compared to POM.
The patients reported use of 361 vitamins and herbal remedies (median 0, range 0-
8). Multivitamins were the remedy used most frequently. These drugs are not recorded in PR.
30
5. Discussion
5.1. Main results
Focused medication interviews provided reliable information about the patient’s very recent use of cardiovascular drugs as estimated by PR and drug analysis. This applied if the interview was performed upon admission or after discharge in the patient’s own home.
When it came to over-all drug use, younger patients were better at reporting than older, and self-reporting during home visits was superior to in-hospital interviews. Apart from age, no other patient characteristic was predictive of the reliability of self-reports. Even home visits did not eliminate omission errors as 1 in 10 drugs dispensed from pharmacy within the preceding week and 1 in 5 drugs dispensed within the preceding month were unreported. Commission errors seemed a minor problem, and only 6% of the POM reported used by the patients were not recoded in PR.
The reliability when a patient denied illicit drug use or use of drugs potentially causing dependence was high. However, some patients underreported their use of cannabinoids and benzodiazepines.
Medication interviews may not uncritically be applied as the gold standard, and omission errors occur especially among elderly. Supplementary information from pharmacy records might be of relevance especially when it comes to detecting use of non-cardiovascular drugs.
5.2. Strengths of study. Methodological considerations
Focused medication interviews are often used for research purposes, but the method is also to an increasing extent implemented in clinical settings. Although knowledge of the reliability of the method is of importance, only few authors have addressed this issue. The tradition in the field is to compare two information sources and to describe the discrepancies. The present work provides additional information by including a wider range of information sources (hospital files, inhospital interviews, home-interviews with inspection of medication vials, pharmacy data and drug analyses) in order to nuance the methodological discussion even further.
We find the Danish PR data highly valid and accurate when it comes to measuring the prescription drugs available to the individual patient. Denmark has a monopolized pharmacy system, and reimbursement regulations make it unfavourable to acquire medications outside this system. In the present study, only few patients reported use of POM provided directly from hospitals (e.g. chemotherapeutics) or from relatives, and none reported use of POM acquired over the Internet. Thus, the requirement of a closed pharmacy system seems fulfilled in a Danish setting. Denmark has with www.medicinprofilen.dk
a unique possibility of applying pharmacy data in the daily clinical setting. The tedious intermediary link of pharmacy personnel to extract
31
data has become needless. Therefore, our data are not only of interest for research purposes but will hopefully attract attention from clinicians.
The approach to use drug analysis in order to test the reliability of the medication history in a hospital setting is new.
149 Drug analysis may be as close as we can get to an objective measurement of the patient’s very recent medication use, and the results therefore represent an interesting yardstick for the comparison of results obtained by other measures. Thus, our finding that patient’s are reliable when reporting their recent use of the 5 cardiovascular and antidiabetic drugs seems a highly valid statement. The drug analyses used in the present study are not immediately recommendable outside a research setting, as they are expensive, tedious and not available as routine. In clinical settings, drug analyses may be used to monitor treatments with e.g. antiretroviral agents where plasma drug levels are coupled to treatment effects and where low drug levels might indicate non-adherence.
150;151
The same can be said about the toxicology screening – although this method cannot be recommended used as a routine, our results give interesting and valid knowledge about the patient’s willingness to self-report use of the drugs tested. The toxicology screening is available as a standardized method at Department of Clinical Pharmacology, Rigshospitalet - and in similar forms elsewhere in the country.
152 Therefore, screenings may be considered in troublesome clinical cases for diagnostic or therapeutic purposes.
5.3. Study weaknesses. Methodological considerations
An important weakness of our study design was the lacking confrontation of the patients with any inconsistencies between the medication interviews versus the drug analysis/hospital files/pharmacy records. Such a confrontation might have clarified whether inconsistencies were attributable to forgetfulness, misunderstandings, adherence problems, errors or alterations in regimens. It would also have been of interest to question the patients that had occurrence of POM
(e.g. bendroflumethiazide) in their blood samples without reporting use of the drug or without the drug being registered in PR. These drugs must have been provided outside the pharmacy system e.g. from relatives or treating doctors. Similarly, the 6% of medications being reported by the patient but not registered in PR were possibly acquired outside the pharmacy system although commission errors were a likely alternative. Practical difficulties influenced our study design as we only obtained access to PR several weeks after study inclusion had begun. Furthermore, drug analysis was not performed until 1 year after study inclusion due to the high efforts required in the laboratory.
The Danish pharmacy records have longitudinal registrations of all drugs dispensed to the individual patient during the preceding 2 years. However, the construction of a medication history imply a cross sectional description of the medication use at a given date or within a given time period. Thus, although PR data may be considered more objective than self-reporting, any use of the records involve several methodological considerations.
47;70;75;92;143 Identification of
32
relevant records is one important issue and our decision to use fixed time windows may have influenced our results. On one hand, we may have overestimated the frequency of omission errors that involved medications only used for a short period of time e.g. acute illness.
75 These records were identified within the 0-30 day window but were unlikely to be reported if the treatment had finished upon the interview. Short-term treatments are often dispensed once or few times (e.g. antibiotics) whereas chronic treatments are dispensed several times. Therefore, we introduced number of pharmacy dispensings in the statistical model to correct this possible error. It was reassuring for the interpretation of analysis, that ATC group was a main predictor of reporting irrespective of the number of dispensings.
On the other hand, we did not detect if drugs purchased more than one month previously were underreported and this might have lead to an underestimate of the omission error frequency. This problem may be significant as the patients frequently used drugs dispensed several months or even one year previously.
Similarly, drug analysis may be perceived more objective than self-reporting, but methodological considerations are still necessary.
86;104 For example, non-detection of a drug otherwise reported as being used may be explained either by lacking use – or by actual use but lacking detection due to fast elimination, short half-life or low daily dose.
86 Even congruent findings must be interpreted with caution: non-detection of a drug not reported used does not preclude use, and the drug may be present but in concentrations below detection limit.
Furthermore, detection of a drug reported as being used gives no insight into long-term use and adherence rates.
153
5.4. Consequences of insufficient medication histories
It was beyond the scope of this thesis to describe the clinical impact of an improved medication history, and we did not evaluate the possible consequences of unreported drug use. Thus, the legitimacy of reporting these indirect parameters rely on knowledge from literature where inadequate medication histories are linked to adverse drug effects and harmful events.
12;14;15;154
No medications are without risk, and a full medication history constitutes the optimal fundament for prescribing and monitoring.
8;14
It is potentially time-consuming and difficult to bring the medication history up to a
100% correctness. At a certain point, the extra workload must be weighed against the clinical importance of any additional information.
56 In the present study, the patient’s reported use/nonuse of amlodipin, bendroflumethiazide, digoxin, glimepiride and simvastatin generally was in high congruence with drug analyses, and the self-reported use of drugs from ATC group C was highly congruent with pharmacy records. On the other hand, antibiotics (ATC J), dermatologicals (D), musculoscleletal (M), sensory (S), and respiratorical (R) medications were reported in poorer congruence with pharmacy data, and benzodiazepine-use was sometimes underreported according to the toxicology screening. Apparently, extra efforts are necessary in order to detect
33
recent use of these apparently underreported drugs. Several aspects may be discussed and considered regarding the clinical importance of undeclared use of the individual drug types.
According to previous studies, antibiotics, analgesics, antirheumatics and psychotropic drugs are often involved in the ADRs causing hospital admissions.
9;132 This emphasises the advantage of obtaining knowledge of any use of these drugs in order to detect the harmful effects. Currently, community-acquired ADRs often pass unnoticed upon hospitalisations 130 and the number of admissions attributable to undesired drug effects might be even larger than currently anticipated in clinical settings.
A recent systematic review included 6 studies who evaluated the significance of the additional knowledge obtained during secondary interviews.
8 The investigators concluded that 11-
59% of the medication history errors were of clinical relevance. Benzodiazepines and analgesics were reported as some of the drug categories often involved in medication errors. This again underscores the importance of detecting use of these drugs.
If a patient is deprived the usual drugs upon admission, this might cause lack of an otherwise well indicated treatment and breakthrough of symptoms, e. g. epileptic seizures in epileptics not receiving regular therapy, or glaucoma in patients not receiving prescribed eyedrops.
14 Insufficient communication between health care professionals regarding chronic diagnoses augments this problem.
155 According to our own data, patients sometimes used drugs with indications that did not match any of the patients’ diseases (Appendix II). If a drug omitted from the medication history is used to treat a disease that is not even known to the hospital physician, then the physician has no chance of detecting the mistake.
In adherence research, drugs are considered forgiving if prolonged activity ensures therapeutic coverage despite missing doses.
156 The effect of missed doses depends on duration of drug action (pharmacodynamic processes and elimination half life) compared to dosing regimen.
157 By use of this terminology, omission of non-forgiving drugs from the medication history might theoretically provoke immediate symptoms, lack of treatment effect or withdrawal symptoms. In this respect, the omission of benzodiazepines from the medication history poses a problem. Other drugs considered non-forgiving are e.g. anti-retroviral drugs and oral contraception.
150 Examples of drugs with longer elimination time and better forgiveness are aspirin, antihypertensive treatment with bendroflumethiazide, trandolapril and amlodipine, cholesterol-lowering atorvastatin and the antidepressant fluoxetin.
157-159
Drugs available over-the-counter, herbal drugs, drugs used in low doses, and drugs used on demand are sometimes perceived as low-risk by physicians and patients and therefore omitted from the medication history.
160-162 However, these drug categories are often subjected to self-medication and are potentially used in the wrong doses or for the wrong reasons, and extra attention might therefore be necessary.
163;164
34
Thus, our study showed that some patients omitted potentially important drug use from their medication history and that PR in several cases might have improved the medication information by raising suspicion of the drug use. It is however disappointing that no patient characteristics apart from patient age was of use to identify the patients in need of specific attention.
5.5. Comparison with previously published studies
5.5.1.Use of pharmacy data
Several studies have previously compared data from PR vs. self-reported medication histories.
47;64-
66;70;76;96;98-100;165-170 Although these prior studies mainly include patients from ambulatory settings, the results are widely congruent with our findings: The reliability of self-reports depends on drug type, and especially cardiovascular drug use is reported with high reliability.
70;76;99;100;165-
167;169;170 Underreporting and omission errors are more frequent than commission errors.
65 High age 65;70;165 or multiple drug use 64 may be related to poor self-reporting.
Previous studies have shown recall enhancement strategies beneficial (showing pills, photographs and prompting with proprietary names) in order to reduce recall bias – especially when it comes to drugs used in the past.
57;67 Thus, PR data might serve as such a recall enhancer if available when the medication history was obtained.
81 Some of the studies shown in Table B used PR during the assembly of a medication history among in-hospital patients but without any further description of how the data was used and how PR benefited the medication history.
24;26;61;85;106;107;118;119
A single study performed systematic questioning of 304 in-hospital patients based on data from their PR.
120 The patients reported use of 1606 drugs whereof 26% only were identified through PR. Among the 518 drugs possibly used according to PR, patients admitted to use the 410 (79%) – they had just forgotten to mention them. Benzodiazepines and NSAIDs were the drugs most frequently omitted. The patients were not questioned about drugs registered in PR if the drugs were not considered potentially used according to calculation of legend time. This possibly caused the authors to underestimate the frequency of omission errors. Commission errors only happened in 3% of drugs registered in the hospital files.
One Danish study detected 85 medication errors among 67 hospitalised patients, 12 of these errors were detected by use of PR.
85 In a casuistic report, pharmacy data helped to identify a wrong medication regimen and an erroneous medication history in 3 patients.
171
Thus, our study seems to add to the current knowledge that PR are valuable sources when a medication history is obtained. However, we need more information on how to use pharmacy data as a recall enhancing strategy in clinical settings.
35
5.5.2. Use of medication analyses
In literature, drug analyses are frequently used in order to describe the patient’s adherence rate to a known and pre-specified long-term treatment.
78;88-90;172-179 This is not immediately comparable to our study design, where we made no assumptions about the patient’s medication regimen beforehand. Instead, we applied drug analysis in order to distinguish users of specific drugs from non-users. The results were then used to validate if self-reports correctly identified drug users.
However, some other authors have used an approach similar to ours and have tested the reliability of self-reported drug use in different population groups. Toxicology screenings with the aim to detect use of illicit drugs or drugs with misuse potential are traditionally applied in high-risk populations where the prevalence of drug use is high, e.g. during drug rehabilitation, among prison inmates or arrestees.
180-182 In these populations, patients appear to report with higher reliability upon inclusion in rehabilitation programmes, and smoking of marijuana is the drug use reported most accurately.
183 Alcohol, benzodiazepines and illicit drugs are frequently detected during screenings among trauma patients.
152;184 Undeclared drug use has also been described in low-risk populations: Among 530 American pregnant women presenting in a prenatal clinic, 8% had a positive toxicology screening whereof 66% denied their drug use.
185 Similarly, 5% of blood donors have unexpectedly positive toxicology screens.
104;186;187
In-hospital patients are often elderly, chronically ill, and treated with polypharmacy.
Thus, other drug usage patterns might be expected. Lilja et al reported a positive benzodiazepine screening among 31 of 198 (16%) in-hospital patients whereof 21 (68%) had not disclosed their use.
149 This is not far from our findings where 8 of 15 (53%) patients with a positive benzodiazepine screening had not declared their use.
Our study indicated that some patients underreported their use of codeinecontaining analgesics. Other studies have previously described underreporting of weak analgesics.
188 Among blood donors, 4-8% have blood screenings unexpectedly positive for salicylate 189;190 or acetaminophen contents.
191;192 Eleven of 122 (9%) female patients attending an outpatient clinic had a urine test indicating recent use of paracetamol-containing analgesics, 9
(82%) denied use.
101
Only few studies have described how to use cardiovascular drug analyses as a means to distinguish users from non-users in a cross sectional manner. Smith et al performed a study among US elderly included in a cardiovascular health study.
86 Similar to our results, the authors described high reliability of self-reported digoxin, propranolol and hydrochlorothiazide use. On the other hand, aspirin use appeared over-reported possibly due to short drug elimination half-life and patient fasting.
Conclusively, no matter the setting, some patients underreport their drug intake.
The consequences potentially vary, and situations where other individuals are potentially harmed may be perceived more serious. This is exemplified by blood donors, where undisclosed medication use potentially causes anaphylaxia or adverse reactions in the recipient due to
36
residual antigenic material in the donor blood.
190-194 Thus, extraordinary precautions may be necessary in some situations.
5.5.3. Medication lists and adherence research
The patient’s ability to correctly report current medication use does not necessarily overlap with the patient’s ability to report medication adherence. However it might be speculated if medication taking behaviour and adherence rates affect the patients’ ability or willingness to correctly report their current medication use.
50;53;86;195 The discrepancies between the self-reported drug use and drug analysis/PR found in the present study might be attributable to adherence problems e.g. if the patients deliberately misinformed to please the interviewer and to camouflage medicationproblems.
53;86 The difficulties of measuring adherence rates accurately is well known.
50;52;53;55;196
Especially the reliability of self-reported medication adherence has been questioned, and some authors describe a tendency towards an underreporting of adherence problems.
66;89;178
Interviewer-technique and –skills may also affect the reliability of self-reports.
46;51;53;55;88;89;153;175
Therefore, if medication adherence affected reporting, we would have expected over-reporting of drug use to occur more frequently than underreporting. This theory was not supported by the data from drug analysis or from PR where the patients more frequently seemed to underreport use of a drug otherwise present in their blood samples or registered in PR rather than overreport.
When it comes to the collection of correct medication information, simple forgetfulness and inability to remember drug names seem to be a more likely problem rather than deliberate underreporting. Patients may think that all pills look alike, and the collective term
unidentified round objects may be well chosen.
57;197 This explains the higher frequency of omission errors compared to errors of commission and again stresses the importance of using recall enhancement.
57
37
6. Future perspectives
More accurate records of current treatment might be achieved by having a computerized database which could be accessed and updated by both general practitioners and hospital doctors.
36
The same said by Price in 1985 might be said today, more than 20 years later. However, the importance of identifying errors in the medication histories at time of hospital admission and discharge is increasingly acknowledged.
16 Worldwide, systems and procedures capable of detecting and reducing errors are being introduced.
3;10;198;199
Medication reconciliation is a term gradually implemented and accepted during the last decade. The process of reconciliation suggests a systematic approach when medication information is collected in order to prevent discrepancy-related ADRs - that is: ADRs caused by discrepancies and errors in the prescribed drug regimens.
3;16;81;200 Reconciliation is especially relevant at hand-offs. Upon hospitalisations, the patient’s in-home medication use is compared to the medications prescribed according to the hospital file. Inconsistencies are discussed before a common medication list is prepared.
2;4;201 In 2004, the Joint Commission on Accreditation of
Healthcare Organizations (JCAHO) declared medication reconciliation a national patient safety goal in order to ensure patient safety across the continuum of care.
3;200 In Denmark, the term
medicinafstemning is included as part of the Operation Lives campaign introduced in 2007 with the aim to prevent deaths in the Danish health care system.
4;56;201
Although a secondary medication interview is a low-technology procedure, it is resource demanding due to the extra time consumed. Similarly, pharmacy records are easily accessible – at least in Denmark, but the extra time needed to access the records is not necessarily well spent for the busy clinician. Encouraging the patients to bring drugs upon consultations, the inspection of the drugs end ultimately the performance of home visits are also resource-demanding procedures. Methods suitable for research purposes may be too timeconsuming to implement in clinical practise. We need more information on how to reconcile with high efficiency, low cost and minimum workload. 2;3;16;81;122 Many authors stress the importance of including the patient in the process of medication prescribing and in the monitoring of treatment.
If the patient feels co-responsible, this might improve communication and medication adherence.
2;46;122;200
In conclusion, the introduction of the term medication reconciliation is promising for an impending improvement of the medication prescribing process and the reduction of medication errors. The methodologies most suitable for research or in a clinical setting remain to be established. To a great extent, patient’s self-reported medication use during a focused interview provides a reliable medication history - perhaps especially when supplemented with pharmacy data.
38
7. Reference List
Reference List
(1) Beers MH, Munekata M, Storrie M. The accuracy of medication histories in the hospital medical records of elderly persons. J Am Geriatr Soc 1990; 38(11):1183-1187.
(2) Boockvar KS, Carlson LH, Giambanco V, Fridman B, Siu A. Medication reconciliation for reducing drug-discrepancy adverse events. Am J Geriatr Pharmacother 2006; 4(3):236-
243.
(3) Using medication reconciliation to prevent errors. Sentinel Event Alert 2006;(35):1-4.
(4) Operation Life Denmark www.operationlife.dk, www.trygpatient.dk
. 2008
(5) Beers MH. The medication list--a portrait of a patient's health. J Gerontol A Biol Sci Med
Sci 2000; 55(10):M549.
(6) Davidsen F, Haghfelt T, Gram LF, Brosen K. Adverse drug reactions and drug noncompliance as primary causes of admission to a cardiology department. Eur J Clin
Pharmacol 1988; 34(1):83-86.
(7) Col N, Fanale JE, Kronholm P. The role of medication noncompliance and adverse drug reactions in hospitalizations of the elderly. Arch Intern Med 1990; 150(4):841-845.
(8) Tam VC, Knowles SR, Cornish PL, Fine N, Marchesano R, Etchells EE. Frequency, type and clinical importance of medication history errors at admission to hospital: a systematic review. CMAJ 2005; 173(5):510-515.
(9) Hallas J. Drug related hospital admissions in subspecialities of internal medicine.
Thesis/dissertation 1995.
(10) Keeble W, Cobbe SM. Patient recall of medication details in the outpatient clinic. Audit and assessment of the value of printed instructions requesting patients to bring medications to clinic. Postgrad Med J 2002; 78(922):479-482.
(11) Porter SC, Kohane IS, Goldmann DA. Parents as partners in obtaining the medication history. J Am Med Inform Assoc 2005; 12(3):299-305.
(12) Lesar TS, Briceland L, Stein DS. Factors related to errors in medication prescribing. JAMA
1997; 277(4):312-317.
(13) Leape LL, Bates DW, Cullen DJ, Cooper J, Demonaco HJ, Gallivan T et al. Systems analysis of adverse drug events. ADE Prevention Study Group. JAMA 1995; 274(1):35-43.
(14) Dobrzanski S, Hammond I, Khan G, Holdsworth H. The nature of hospital prescribing errors. British Journal of Clinical Governance 2002; 7(3):187-193.
(15) Bates DW, Boyle DL, Vander Vliet MB, Schneider J, Leape L. Relationship between medication errors and adverse drug events. J Gen Intern Med 1995; 10(4):199-205.
(16) Vira T, Colquhoun M, Etchells E. Reconcilable differences: correcting medication errors at hospital admission and discharge. Qual Saf Health Care 2006; 15(2):122-126.
39
(17) Lazarou J, Pomeranz BH, Corey PN. Incidence of adverse drug reactions in hospitalized patients: a meta-analysis of prospective studies. JAMA 1998; 279(15):1200-1205.
(18) Mannesse CK, Derkx FH, de Ridder MA, Man in 't Veld AJ, van der Cammen TJ.
Contribution of adverse drug reactions to hospital admission of older patients. Age Ageing
2000; 29(1):35-39.
(19) Bates DW, Miller EB, Cullen DJ, Burdick L, Williams L, Laird N et al. Patient risk factors for adverse drug events in hospitalized patients. ADE Prevention Study Group. Arch Intern
Med 1999; 159(21):2553-2560.
(20) Moore C, Wisnivesky J, Williams S, McGinn T. Medical errors related to discontinuity of care from an inpatient to an outpatient setting. J Gen Intern Med 2003; 18(8):646-651.
(21) Bates DW, Cullen DJ, Laird N, Petersen LA, Small SD, Servi D et al. Incidence of adverse drug events and potential adverse drug events. Implications for prevention. ADE
Prevention Study Group. JAMA 1995; 274(1):29-34.
(22) Andersen SE, Pedersen AB, Bach KF. Medication history on internal medicine wards: assessment of extra information collected from second drug interviews and GP lists.
Pharmacoepidemiol Drug Saf 2003; 12(6):491-498.
(23) Solet DJ, Norvell JM, Rutan GH, Frankel RM. Lost in translation: challenges and opportunities in physician-to-physician communication during patient handoffs. Acad Med
2005; 80(12):1094-1099.
(24) Cornish PL, Knowles SR, Marchesano R, Tam V, Shadowitz S, Juurlink DN et al.
Unintended medication discrepancies at the time of hospital admission. Arch Intern Med
2005; 165(4):424-429.
(25) Barger RC, Barger J. Pharmacist, nurse cooperate in taking drug histories. Hospitals
1976; 50(17):93-94.
(26) Gleason KM, Groszek JM, Sullivan C, Rooney D, Barnard C, Noskin GA. Reconciliation of discrepancies in medication histories and admission orders of newly hospitalized patients.
Am J Health Syst Pharm 2004; 61(16):1689-1695.
(27) Gandhi TK. Fumbled handoffs: one dropped ball after another. Ann Intern Med 2005;
142(5):352-358.
(28) Glintborg B, Andersen SE, Spang-Hanssen E, Dalhoff K. Disregarded use of herbal medical products and dietary supplements among surgical and medical patients as estimated by home inspection and interview. Pharmacoepidemiol Drug Saf 2005; 14(9):639-645.
(29) Glintborg B, Andersen SE, Spang-Hanssen E, Dalhoff K. The use of over-the-counter drugs among surgical and medical patients. Eur J Clin Pharmacol 2004; 60(6):431-437.
(30) Glintborg B, Andersen SE, Dalhoff K. Insufficient communication about medication use at the interface between hospital and primary care. Qual Saf Health Care 2007; 16(1):34-39.
(31) Himmel W, Tabache M, Kochen MM. What happens to long-term medication when general practice patients are referred to hospital? Eur J Clin Pharmacol 1996; 50(4):253-257.
(32) Corry M, Bonner G, McEntee S, Dugan J, MacAuley D. Hospitals do not inform GPs about medication that should be monitored. Fam Pract 2000; 17(3):268-271.
40
(33) Williams EI, Fitton F. General practitioner response to elderly patients discharged from hospital. BMJ 1990; 300(6718):159-161.
(34) Bourke JL, Bjeldbak-Olesen I, Nielsen PM, Munck LK. [Joint charts in drug handling.
Toward increased drug safety]. Ugeskr Laeger 2001; 163(39):5356-5360.
(35) Burns JM, Sneddon I, Lovell M, McLean A, Martin BJ. Elderly patients and their medication: a post-discharge follow-up study. Age Ageing 1992; 21(3):178-181.
(36) Price D, Cooke J, Singleton S, Feely M. Doctors' unawareness of the drugs their patients are taking: a major cause of overprescribing? Br Med J (Clin Res Ed) 1986; 292(6513):99-
100.
(37) Hayward RA, Asch SM, Hogan MM, Hofer TP, Kerr EA. Sins of omission: getting too little medical care may be the greatest threat to patient safety. J Gen Intern Med 2005;
20(8):686-691.
(38) Weingart SN, Wilson RM, Gibberd RW, Harrison B. Epidemiology of medical error. BMJ
2000; 320(7237):774-777.
(39) Bell CM, Bajcar J, Bierman AS, Li P, Mamdani MM, Urbach DR. Potentially unintended discontinuation of long-term medication use after elective surgical procedures. Arch Intern
Med 2006; 166(22):2525-2531.
(40) Feely M, Singleton S, McGibney D. The inadequacies of information on current drug therapy in out-patients' records. J R Coll Physicians Lond 1984; 18(4):222-224.
(41) Gonski PN, Stathers GM, Freiman JS, Smith T. A critical review of admission and discharge medications in an elderly Australian population. Drugs Aging 1993; 3(4):358-
362.
(42) Barat I, Andreasen F, Damsgaard EM. The consumption of drugs by 75-year-old individuals living in their own homes. Eur J Clin Pharmacol 2000; 56(6-7):501-509.
(43) Tobi H, van den Heuvel NJ, de Jong-van den Berg LT. Does uncollected medication reduce the validity of pharmacy dispensing data? Pharmacoepidemiol Drug Saf 2004; 13(7):497-
500.
(44) Claoue C, Elkington AR. Informing the hospital of patients' drug regimens. Br Med J (Clin
Res Ed) 1986; 292(6513):101.
(45) Barat I, Andreasen F, Damsgaard EM. Drug therapy in the elderly: what doctors believe and patients actually do. Br J Clin Pharmacol 2001; 51(6):615-622.
(46) Hulka BS, Cassel JC, Kupper LL, Burdette JA. Communication, compliance, and concordance between physicians and patients with prescribed medications. Am J Public
Health 1976; 66(9):847-853.
(47) Leister KA, Edwards WA, Christensen DB, Clark H. A comparison of patient drug regimens as viewed by the physician, pharmacist and patient. Med Care 1981; 19(6):658-664.
(48) Cohen J. Improve drug history taking. Pharmacy in Practice 1998;(1):13-16.
(49) Bikowski RM, Ripsin CM, Lorraine VL. Physician-patient congruence regarding medication regimens. J Am Geriatr Soc 2001; 49(10):1353-1357.
41
(50) Farmer KC. Methods for measuring and monitoring medication regimen adherence in clinical trials and clinical practice. Clin Ther 1999; 21(6):1074-1090.
(51) Sleath B, Rubin RH, Campbell W, Gwyther L, Clark T. Physician-patient communication about over-the-counter medications. Soc Sci Med 2001; 53(3):357-369.
(52) Osterberg L, Blaschke T. Adherence to medication. N Engl J Med 2005; 353(5):487-497.
(53) MacLaughlin EJ, Raehl CL, Treadway AK, Sterling TL, Zoller DP, Bond CA. Assessing medication adherence in the elderly: which tools to use in clinical practice? Drugs Aging
2005; 22(3):231-255.
(54) Rudd P. In search of the gold standard for compliance measurement. Arch Intern Med
1979; 139(6):627-628.
(55) Bond WS, Hussar DA. Detection methods and strategies for improving medication compliance. Am J Hosp Pharm 1991; 48(9):1978-1988.
(56) Nissen Å. Medicinafstemning. Dansk Selskab for Patientsikkerhed. www.patientsikkerhed.dk
. 2008
(57) Bellamy N, Grace E, Hanna B, Grant E, Tugwell P, Buchanan WW. Clinical evaluation of two strategies for improving patient recall of prior drug therapy. Br J Clin Pharmacol 1984;
17(6):769-772.
(58) Gurwich EL. Comparison of medication histories acquired by pharmacists and physicians.
Am J Hosp Pharm 1983; 40(9):1541-1542.
(59) Badowski SA, Rosenbloom D, Dawson PH. Clinical importance of pharmacist-obtained medication histories using a validated questionnaire. Am J Hosp Pharm 1984; 41(4):731-
732.
(60) Cattell R, Wooller S, O'Mahoney S. Obtaining the correct drug history. Postgrad Med J
1997; 73(858):255.
(61) Brookes K, Scott MG, McConnell JB. The benefits of a hospital based community services liaison pharmacist. Pharm World Sci 2000; 22(2):33-38.
(62) Dodds LJ. An objective assessment of the role of the pharmacist in medication and compliance history taking. British Journal of Pharmaceutical Practice 2002; July:12-24.
(63) Montpetit LM, Roy MT. Evaluation of a patient-completed versus health professionalconducted medication history. Drug Intell Clin Pharm 1988; 22(12):964-969.
(64) de Jong-van den Berg LT, Waardenburg CM, Haaijer-Ruskamp FM, Dukes MN, Wesseling
H. Drug use in pregnancy: a comparative appraisal of data collecting methods. Eur J Clin
Pharmacol 1993; 45(1):9-14.
(65) West SL, Savitz DA, Koch G, Strom BL, Guess HA, Hartzema A. Recall accuracy for prescription medications: self-report compared with database information. Am J Epidemiol
1995; 142(10):1103-1112.
(66) Norell SE. Accuracy of patient interviews and estimates by clinical staff in determining medication compliance. Soc Sci Med [E ] 1981; 15(1):57-61.
42
(67) Rosenberg MJ, Layde PM, Ory HW, Strauss LT, Rooks JB, Rubin GL. Agreement between women's histories of oral contraceptive use and physician records. Int J Epidemiol 1983;
12(1):84-87.
(68) Rabol R, Arroe GR, Folke F, Madsen KR, Langergaard MT, Larsen AH et al. [Disagreement between physicians' medication records and information given by patients]. Ugeskr Laeger
2006; 168(13):1307-1310.
(69) Foss S, Schmidt JR, Andersen T, Rasmussen JJ, Damsgaard J, Schaefer K et al.
Congruence on medication between patients and physicians involved in patient course.
Eur J Clin Pharmacol 2004; 59(11):841-847.
(70) Caskie GI, Willis SL. Congruence of self-reported medications with pharmacy prescription records in low-income older adults. Gerontologist 2004; 44(2):176-185.
(71) Manley HJ, Drayer DK, McClaran M, Bender W, Muther RS. Drug record discrepancies in an outpatient electronic medical record: frequency, type, and potential impact on patient care at a hemodialysis center. Pharmacotherapy 2003; 23(2):231-239.
(72) Yang JC, Tomlinson G, Naglie G. Medication lists for elderly patients: clinic-derived versus in-home inspection and interview. J Gen Intern Med 2001; 16(2):112-115.
(73) Atkin PA, Stringer RS, Duffy JB, Elion C, Ferraris CS, Misrachi SR et al. The influence of information provided by patients on the accuracy of medication records. Med J Aust 1998;
169(2):85-88.
(74) Landry JA, Smyer MA, Tubman JG, Lago DJ, Roberts J, Simonson W. Validation of two methods of data collection of self-reported medicine use among the elderly. Gerontologist
1988; 28(5):672-676.
(75) Lau HS, De Boer A, Beuning KS, Porsius A. Validation of pharmacy records in drug exposure assessment. J Clin Epidemiol 1997; 50(5):619-625.
(76) Heerdink ER, Leufkens HG, Koppedraaijer C, Bakker A. Information on drug use in the elderly: a comparison of pharmacy, general-practitioner and patient data. Pharm World Sci
1995; 17(1):20-24.
(77) Steiner JF, Prochazka AV. The assessment of refill compliance using pharmacy records: methods, validity, and applications. J Clin Epidemiol 1997; 50(1):105-116.
(78) Steiner JF, Koepsell TD, Fihn SD, Inui TS. A general method of compliance assessment using centralized pharmacy records. Description and validation. Med Care 1988;
26(8):814-823.
(79) Ekedahl A, Mansson N. Unclaimed prescriptions after automated prescription transmittals to pharmacies. Pharm World Sci 2004; 26(1):26-31.
(80) Wetzels GE, Nelemans PJ, Schouten JS, van Wijk BL, Prins MH. All that glisters is not gold: a comparison of electronic monitoring versus filled prescriptions--an observational study. BMC Health Serv Res 2006; 6:8.
(81) Pronovost P, Weast B, Schwarz M, Wyskiel RM, Prow D, Milanovich SN et al. Medication reconciliation: a practical tool to reduce the risk of medication errors. J Crit Care 2003;
18(4):201-205.
43
(82) Baum C, Forbes MB, Kennedy DL, Jones JK. Patient drug profiles and medical records as sources of hospital drug-use information. Am J Hosp Pharm 1983; 40(12):2191-2193.
(83) Frisk PA, Cooper JW, Jr., Campbell NA. Community-hospital pharmacist detection of drug-related problems upon patient admission to small hospitals. Am J Hosp Pharm 1977;
34(7):738-742.
(84) Danish Medicines Agency. www.laegemiddelstyrelsen.dk. 2008
(85) Larsen MD, Nielsen LP, Jeffery L, Staehr ME. [Medication errors on hospital admission].
Ugeskr Laeger 2006; 168(35):2887-2890.
(86) Smith NL, Psaty BM, Heckbert SR, Tracy RP, Cornell ES. The reliability of medication inventory methods compared to serum levels of cardiovascular drugs in the elderly. J Clin
Epidemiol 1999; 52(2):143-146.
(87) Gogtay NJ, Jakhere SG, Waingankar SP, Dalvi SS, Kshirsagar NA. Therapeutic drug monitoring as a tool to identify medication errors. Drug Saf 2004; 27(2):143-144.
(88) BERGMAN AB, WERNER RJ. Failure of children to receive penicillin by mouth. N Engl J
Med 1963; 268:1334-1338.
(89) Gordis L, Markowitz M, Lilienfeld AM. The inaccuracy in using interviews to estimate patient reliability in taking medications at home. Med Care 1969; 7(1):49-54.
(90) Weintraub M, Au WY, Lasagna L. Compliance as a determinant of serum digoxin concentration. JAMA 1973; 224(4):481-485.
(91) Rand CS, Wise RA. Measuring adherence to asthma medication regimens. Am J Respir
Crit Care Med 1994; 149(2 Pt 2):S69-S76.
(92) Christensen DB, Williams B, Goldberg HI, Martin DP, Engelberg R, LoGerfo JP.
Comparison of prescription and medical records in reflecting patient antihypertensive drug therapy. Ann Pharmacother 1994; 28(1):99-104.
(93) Burda SA, Hobson D, Pronovost PJ. What is the patient really taking? Discrepancies between surgery and anesthesiology preoperative medication histories. Qual Saf Health
Care 2005; 14(6):414-416.
(94) West SL, Strom BL, Freundlich B, Normand E, Koch G, Savitz DA. Completeness of prescription recording in outpatient medical records from a health maintenance organization. J Clin Epidemiol 1994; 47(2):165-171.
(95) Monson RA, Bond CA. The accuracy of the medical record as an index of outpatient drug therapy. JAMA 1978; 240(20):2182-2184.
(96) Boudreau DM, Doescher MP, Saver BG, Jackson JE, Fishman PA. Reliability of Group
Health Cooperative automated pharmacy data by drug benefit status. Pharmacoepidemiol
Drug Saf 2005; 14(12):877-884.
(97) Opdycke RAC, Ascione FJ, Shimp LA, Boyd EL, Malloch CK. Comparison of Pharmacist-
Obtained Comprehensive Medication Histories and Medical Records in Geriatric Patients.
Journal of Geriatric Drug Therapy 2004; 9(2):19-39.
44
(98) Torrible SJ, Hogan DB. Medication use and rural seniors. Who really knows what they are taking? Can Fam Physician 1997; 43:893-898.
(99) Johnson RE, Vollmer WM. Comparing sources of drug data about the elderly. J Am Geriatr
Soc 1991; 39(11):1079-1084.
(100) Olesen C, Sondergaard C, Thrane N, Nielsen GL, de Jong-van den Berg, Olsen J. Do pregnant women report use of dispensed medications? Epidemiology 2001; 12(5):497-501.
(101) Schwarz A, Faber U, Borner K, Keller F, Offermann G, Molzahn M. Reliability of drug history in analgesic users. Lancet 1984; 2(8412):1163-1164.
(102) Gerbert B, Stone G, Stulbarg M, Gullion DS, Greenfield S. Agreement among physician assessment methods. Searching for the truth among fallible methods. Med Care 1988;
26(6):519-535.
(103) Rockett IR, Putnam SL, Jia H, Smith GS. Declared and undeclared substance use among emergency department patients: a population-based study. Addiction 2006; 101(5):706-
712.
(104) Melanson SE, Stowell CP, Flood JG, Lewandrowski EL, Zak RJ, Lewandrowski KB. Does blood donor history accurately reflect the use of prescription medications? A comparison of donor history and serum toxicologic analysis. Transfusion 2006; 46(8):1402-1407.
(105) The National Library of Medicine and the National Institutes of Health.http:, www.ncbi.nlm.nih.gov/sites/entrez/ . 2008
(106) Nester TM, Hale LS. Effectiveness of a pharmacist-acquired medication history in promoting patient safety. Am J Health Syst Pharm 2002; 59(22):2221-2225.
(107) Carter MK, Allin DM, Scott LA, Grauer D. Pharmacist-acquired medication histories in a university hospital emergency department. Am J Health Syst Pharm 2006; 63(24):2500-
2503.
(108) Lawrence J, Wilcock M. Importance of accurate medication histories. Am J Health Syst
Pharm 2003; 60(6):615.
(109) Drewett NM. Stop regular medicine errors. Pharmacy in Practice 1998; May.
(110) Massey C. An evaluation of the benefits of pharmacist-acquired drug histories. Proc Guild
Hosp Pharm 1987; 25:80-81.
(111) Nicholls M, Horler K, Campbell D, Conroy C, Cattell R. Peace in a POD. Health Service
Journal 2001;(July).
(112) Hocking G, Kalyanaraman R, deMello WF. Better drug history taking: an assessment of the
DRUGS mnemonic. J R Soc Med 1998; 91(6):305-306.
(113) Akwagyriam I, Goodyer LI, Harding L, Khakoo S, Millington H. Drug history taking and the identification of drug related problems in an accident and emergency department. J Accid
Emerg Med 1996; 13(3):166-168.
(114) Truitt CA, Longe RL, Taylor AT. An evaluation of a medication history method. Drug Intell
Clin Pharm 1982; 16(7-8):592-596.
45
(115) Covington TR, Pfeiffer FG. The pharmacist-acquired medication history. Am J Hosp Pharm
1972; 29(8):692-695.
(116) Wilson RS, Kabat HF. Pharmacist initiated patient drug histories. Am J Hosp Pharm 1971;
28(1):49-53.
(117) Dobbs JH. Drug histories obtained by pharmacists from psychiatric inpatients. Hosp
Community Psychiatry 1981; 32(9):639-640.
(118) Walchle RD, McKercher PL, Cooper JW. Physician-, nurse-, and pharmacist-conducted patient drug histories. Contemp Pharm Pract 1980; 3(2):75-78.
(119) La VS. Evaluation of drug history program. Hospitals 1973; 47(15):106.
(120) Lau HS, Florax C, Porsius AJ, De Boer A. The completeness of medication histories in hospital medical records of patients admitted to general internal medicine wards. Br J Clin
Pharmacol 2000; 49(6):597-603.
(121) Ketchum K, Grass CA, Padwojski A. Medication reconciliation: verifying medication orders and clarifying discrepancies should be standard practice. Am J Nurs 2005; 105(11):78-2,
84.
(122) Whittington J, Cohen H. OSF healthcare's journey in patient safety. Qual Manag Health
Care 2004; 13(1):53-59.
(123) Fertleman M, Barnett N, Patel T. Improving medication management for patients: the effect of a pharmacist on post-admission ward rounds. Qual Saf Health Care 2005; 14(3):207-
211.
(124) Psaty BM, Lee M, Savage PJ, Rutan GH, German PS, Lyles M. Assessing the use of medications in the elderly: methods and initial experience in the Cardiovascular Health
Study. The Cardiovascular Health Study Collaborative Research Group. J Clin Epidemiol
1992; 45(6):683-692.
(125) Kelly JP, Rosenberg L, Kaufman DW, Shapiro S. Reliability of personal interview data in a hospital-based case-control study. Am J Epidemiol 1990; 131(1):79-90.
(126) Bedell SE, Jabbour S, Goldberg R, Glaser H, Gobble S, Young-Xu Y et al. Discrepancies in the use of medications: their extent and predictors in an outpatient practice. Arch Intern
Med 2000; 160(14):2129-2134.
(127) Spagnoli A, Ostino G, Borga AD, D'Ambrosio R, Maggiorotti P, Todisco E et al. Drug compliance and unreported drugs in the elderly. J Am Geriatr Soc 1989; 37(7):619-624.
(128) Malhotra S, Karan RS, Pandhi P, Jain S. Drug related medical emergencies in the elderly: role of adverse drug reactions and non-compliance. Postgrad Med J 2001; 77(913):703-
707.
(129) van Kraaij DJ, Haagsma CJ, Go IH, Gribnau FW. Drug use and adverse drug reactions in
105 elderly patients admitted to a general medical ward. Neth J Med 1994; 44(5):166-173.
(130) Dormann H, Criegee-Rieck M, Neubert A, Egger T, Geise A, Krebs S et al. Lack of awareness of community-acquired adverse drug reactions upon hospital admission : dimensions and consequences of a dilemma. Drug Saf 2003; 26(5):353-362.
46
(131) Pirmohamed M, James S, Meakin S, Green C, Scott AK, Walley TJ et al. Adverse drug reactions as cause of admission to hospital: prospective analysis of 18 820 patients. BMJ
2004; 329(7456):15-19.
(132) Grymonpre RE, Mitenko PA, Sitar DS, Aoki FY, Montgomery PR. Drug-associated hospital admissions in older medical patients. J Am Geriatr Soc 1988; 36(12):1092-1098.
(133) Rich EC, Crowson TW, Harris IB. The diagnostic value of the medical history. Perceptions of internal medicine physicians. Arch Intern Med 1987; 147(11):1957-1960.
(134) Baker DW, Gazmararian JA, Sudano J, Patterson M. The association between age and health literacy among elderly persons. J Gerontol B Psychol Sci Soc Sci 2000; 55(6):S368-
S374.
(135) Sundhedsstyrelsen.Danish National Board of Health. Rapport fra arbejdsgruppen vedr. forslag til vurdering af kognitiv funktion ved lægeundersøgelse i forbindelse med kørekortsfornyelse fra det 70. år. 2003.
(136) Dansk selskab for almen medicin. Klinisk vejledning. Identifikation og udredning af demens og demenslignende tilstande i almen praksis. 1999.
(137) Trudeau T, Oleen M. How drug histories obtained by pharmacists help the hospitalized patient. Pharm Times 1978; 44(2):65-67.
(138) Cohen AF, Kroon R, Schoemaker HC, Breimer DD, Vliet-Verbeek A, Brandenburg HC. The bioavailability of digoxin from three oral formulations measured by a specific h.p.l.c. assay.
Br J Clin Pharmacol 1993; 35(2):136-142.
(139) Moran MT, Wiser TH, Nanda J, Gross H. Measuring medical residents' chartdocumentation practices. J Med Educ 1988; 63(11):859-865.
(140) Romm FJ, Putnam SM. The validity of the medical record. Med Care 1981; 19(3):310-315.
(141) Hocking G, deMello WF. Taking a 'drugs' history. Anaesthesia 1997; 52(9):904-905.
(142) Moffat AC, Osselton MD, Widdop B. Clarke's analysis of Drugs and Poisons. 3rd ed.
London Pharmaceutical Press; 2003.
(143) Christensen DB, Williams B, Goldberg HI, Martin DP, Engelberg R, LoGerfo JP. Assessing compliance to antihypertensive medications using computer-based pharmacy records. Med
Care 1997; 35(11):1164-1170.
(144) Badian M, Korn A, Lehr KH, Malerczyk V, Waldhausl W. Absolute bioavailability of glimepiride (Amaryl) after oral administration. Drug Metabol Drug Interact 1994;
11(4):331-339.
(145) Najib NM, Idkaidek N, Adel A, Admour I, Astigarraga RE, Nucci GD et al. Pharmacokinetics and bioequivalence evaluation of two simvastatin 40 mg tablets (Simvast and Zocor) in healthy human volunteers. Biopharm Drug Dispos 2003; 24(5):183-189.
(146) Scandinavian medical Information MD. www.SMI.dk. 2008
47
(147) Beermann B. Aspects on pharmacokinetics of some diuretics. Acta Pharmacol Toxicol
(Copenh) 1984; 54 Suppl 1:17-29.
(148) WHO Collaborating Centre for Drug Statistics Methology. Guidelines for ATC-classification and DDD assignment (2 edn.). 1998. Oslo.
(149) Lilja M, Arvela P, Klintrup HE, Jounela AJ. Intake of alcohol and benzodiazepines and reliability of drug history in patients admitted to hospital. Hum Toxicol 1986; 5(4):281-
282.
(150) Burger DM, Aarnoutse RE, Hugen PW. Pros and cons of therapeutic drug monitoring of antiretroviral agents. Curr Opin Infect Dis 2002; 15(1):17-22.
(151) Durant J, Clevenbergh P, Garraffo R, Halfon P, Icard S, Del GP et al. Importance of protease inhibitor plasma levels in HIV-infected patients treated with genotypic-guided therapy: pharmacological data from the Viradapt Study. AIDS 2000; 14(10):1333-1339.
(152) Deutch SR, Christian C, Hoyer S, Christensen EF, Dragsholt C, Hansen AC et al. Drug and alcohol use among patients admitted to a Danish trauma centre: a prospective study from a regional trauma centre in Scandinavia. Eur J Emerg Med 2004; 11(6):318-322.
(153) Cramer JA, Mattson RH, Prevey ML, Scheyer RD, Ouellette VL. How often is medication taken as prescribed? A novel assessment technique. JAMA 1989; 261(22):3273-3277.
(154) Bond CA, Raehl CL, Franke T. Clinical pharmacy services and hospital mortality rates.
Pharmacotherapy 1999; 19(5):556-564.
(155) Kljakovic M, Abernethy D, de R, I. Quality of diagnostic coding and information flow from hospital to general practice. Inform Prim Care 2004; 12(4):227-234.
(156) Boissel JP, Nony P. Using pharmacokinetic-pharmacodynamic relationships to predict the effect of poor compliance. Clin Pharmacokinet 2002; 41(1):1-6.
(157) Hughes DA, Walley T. Predicting "real world" effectiveness by integrating adherence with pharmacodynamic modeling. Clin Pharmacol Ther 2003; 74(1):1-8.
(158) Elliott HL, Elawad M, Wilkinson R, Singh SP. Persistence of antihypertensive efficacy after missed doses: comparison of amlodipine and nifedipine gastrointestinal therapeutic system. J Hypertens 2002; 20(2):333-338.
(159) Girvin BG, Johnston GD. Comparison of the effects of a 7-day period of non-compliance on blood pressure control using three different antihypertensive agents. J Hypertens 2004;
22(7):1409-1414.
(160) Benrimoj SI, Langford JH, Bowden MG, Triggs EJ. Switching drug availability from prescription only to over-the-counter status. Are elderly patients at increased risk? Drugs
Aging 1995; 7(4):255-265.
(161) Honig PK, Gillespie BK. Clinical significance of pharmacokinetic drug interactions with over-the-counter (OTC) drugs. Clin Pharmacokinet 1998; 35(3):167-171.
(162) Lamy PP. Over-the-counter medication: the drug interactions we overlook. J Am Geriatr
Soc 1982; 30(11 Suppl):S69-S75.
48
(163) Davies P, Fattah H, Clee MD. Undisclosed self-medication--a clinical pitfall. Br J Clin Pract
1994; 48(6):333.
(164) Gude A-BJ, Hoegberg LCG, Pedersen M, Nielsen J, Angelo HR, Christensen HR.
Forgiftningsmønstre hos 355 konsekutivt indlagte akutte patienter på Bispebjerg Hospital i
2001. Ugeskr Laeger 2007; 169(19):1793-1797.
(165) Van den Brandt PA, Petri H, Dorant E, Goldbohm RA, Van de CS. Comparison of questionnaire information and pharmacy data on drug use. Pharm Weekbl Sci 1991;
13(2):91-96.
(166) Klungel OH, de BA, Paes AH, Herings RM, Seidell JC, Bakker A. Agreement between selfreported antihypertensive drug use and pharmacy records in a population-based study in
The Netherlands. Pharm World Sci 1999; 21(5):217-220.
(167) Klungel OH, de BA, Paes AH, Herings RM, Seidell JC, Bakker A. Influence of question structure on the recall of self-reported drug use. J Clin Epidemiol 2000; 53(3):273-277.
(168) Al-Windi A. The validity of a questionnaire on medicines used in health care practice: comparison of a questionnaire and computerized medical record survey. Eur J Clin
Pharmacol 2003; 59(4):321-329.
(169) Boudreau DM, Daling JR, Malone KE, Gardner JS, Blough DK, Heckbert SR. A validation study of patient interview data and pharmacy records for antihypertensive, statin, and antidepressant medication use among older women. Am J Epidemiol 2004; 159(3):308-
317.
(170) Sjahid SI, van der Linden PD, Stricker BH. Agreement between the pharmacy medication history and patient interview for cardiovascular drugs: the Rotterdam elderly study. Br J
Clin Pharmacol 1998; 45(6):591-595.
(171) Jacobson J. Ensuring continuity of care and accuracy of patients' medication history on hospital admission. Am J Health Syst Pharm 2002; 59(11):1054-1055.
(172) Black DM, Brand RJ, Greenlick M, Hughes G, Smith J. Compliance to treatment for hypertension in elderly patients: the SHEP pilot study. Systolic Hypertension in the Elderly
Program. J Gerontol 1987; 42(5):552-557.
(173) Macintyre CR, Goebel K, Brown GV. Patient knows best: blinded assessment of nonadherence with antituberculous therapy by physicians, nurses, and patients compared with urine drug levels. Prev Med 2005; 40(1):41-45.
(174) Haynes RB, Taylor DW, Sackett DL, Gibson ES, Bernholz CD, Mukherjee J. Can simple clinical measurements detect patient noncompliance? Hypertension 1980; 2(6):757-764.
(175) Butler JA, Peveler RC, Roderick P, Horne R, Mason JC. Measuring compliance with drug regimens after renal transplantation: comparison of self-report and clinician rating with electronic monitoring. Transplantation 2004; 77(5):786-789.
(176) George CF, Peveler RC, Heiliger S, Thompson C. Compliance with tricyclic antidepressants: the value of four different methods of assessment. Br J Clin Pharmacol 2000; 50(2):166-
171.
(177) Fletcher SW, Pappius EM, Harper SJ. Measurement of medication compliance in a clinical setting. Comparison of three methods in patients prescribed digoxin. Arch Intern Med
1979; 139(6):635-638.
49
(178) Craig HM. Accuracy of indirect measures of medication compliance in hypertension. Res
Nurs Health 1985; 8(1):61-66.
(179) Cramer JA, Scheyer RD, Mattson RH. Compliance declines between clinic visits. Arch
Intern Med 1990; 150(7):1509-1510.
(180) Jain R, Tripathi BM, Varghese ST, Kumar N, Kumar M. Can you trust self-reports among injectable drug users in clinical setting? Journal of Substance Use 2006; 11(6):431-436.
(181) Yacoubian GS, Jr., Urbach BJ. To pee or not to pee: reconsidering the need for urinalysis.
J Drug Educ 2002; 32(4):261-270.
(182) Zanis DA, McLellan AT, Randall M. Can you trust patient self-reports of drug use during treatment? Drug Alcohol Depend 1994; 35(2):127-132.
(183) Magura S, Kang SY. Validity of self-reported drug use in high risk populations: a metaanalytical review. Subst Use Misuse 1996; 31(9):1131-1153.
(184) Levy RS, Hebert CK, Munn BG, Barrack RL. Drug and alcohol use in orthopedic trauma patients: a prospective study. J Orthop Trauma 1996; 10(1):21-27.
(185) Ashling K, Gross AH, Coghlin DT, Sweeney PJ. Prevalence of positive urine drug screens in a prenatal clinic: correlation with patients' self-report of drug use. R I Med 1994;
77(11):371-373.
(186) Mahl MA, Hirsch M, Sugg U. Verification of the drug history given by potential blood donors: results of drug screening that combines hair and urine analysis. Transfusion
2000; 40(6):637-641.
(187) Mahnovski V, Cheng MH, Lipsey AI, Keyomarsi K. Drugs in blood donors. Clin Chem 1987;
33(1):189.
(188) Joubert PH, Clark EC, Otto AC, Pannall PR. Unreliable drug histories, analgesics, and changes in renal function. S Afr Med J 1977; 52(3):107-109.
(189) Sharon R, Frutkoff I, Kidroni G, Menczel J. Applicability and significance of salicylate screening in sera of voluntary blood donors: evaluation of two analytical methods. J Clin
Pathol 1982; 35(1):59-62.
(190) Sharon R, Kidroni G, Michel J. Presence of aspirin in blood units. Vox Sang 1980;
38(5):284-287.
(191) MacIntyre A, Gray JD, Gorelick M, Renton K. Salicylate and acetaminophen in donated blood. CMAJ 1986; 135(3):215-216.
(192) Sharon R, Menczel J, Kidroni G. Incidence of acetaminophen in donated blood. Vox Sang
1982; 43(3):138-141.
(193) Michel J, Sharon R. Presence of antibacterial agents in blood units collected from healthy voluntary donors. Chemotherapy 1981; 27(2):114-116.
(194) Michel J, Sharon R. Detection of penicillins in the sera of 'healthy' blood donors. Vox Sang
1980; 38(1):19-21.
50
(195) Rudd P, Byyny RL, Zachary V, LoVerde ME, Titus C, Mitchell WD et al. The natural history of medication compliance in a drug trial: limitations of pill counts. Clin Pharmacol Ther
1989; 46(2):169-176.
(196) Wright EC. Non-compliance--or how many aunts has Matilda? Lancet 1993;
342(8876):909-913.
(197) Biron P. Chromoconfusion and unidentified round objects. Can Med Assoc J 1977;
117(7):732-733.
(198) Longo DR, Hewett JE, Ge B, Schubert S. The long road to patient safety: a status report on patient safety systems. JAMA 2005; 294(22):2858-2865.
(199) Sanson-Fisher RW, Clover K. Compliance in the treatment of hypertension. A need for action. Am J Hypertens 1995; 8(10 Pt 2):82S-88S.
(200) Barnsteiner JH. Medication Reconciliation: Transfer of medication information across settings-keeping it free from error. Am J Nurs 2005; 105(3 Suppl):31-36.
(201) Steenberger A. Kampagne for de optimale rutiner. Ugeskr Laeger 2007; 169(16):1416.
51
8. Methods supplementary. Development of analytical assays
By Peter Rene Hillestrøm, MSc and Lenette Holm Olsen, MSc.
Department of Clinical Pharmacology, Rigshospitalet
Materials
Glacial acetic acid and formic acid were supplied from Merck KgaA (Darmstadt, Germany) while acetonitrile and 25% aqueous ammonia were from J.T. Baker (Deventer, the Netherlands). Purified water was obtained from a Milli-Q Gradient A10 system (Millipore, Bedford, MA). All other solvents were of analytical grade. The following standards and internal standards were used: Amlodipine and UK 52.829 (Pfizer Aps Denmark and Pfizer England), Simvastatin and Lovastatin (Merck
Sharp & Dohme), Glimepiride and Glibenclamide (Aventis Pharma Deutschland GmbH),
Bendroflumethiazide (LEO Pharma Denmark) and Cyclopenthiazide (Norvartis Healthcare A/S
UK).
Liquid Chromatography
Chromatographic separation of the analytes from matrix constituents was performed on an UPLC system (Waters, Milford, MS, USA) consisting of Binary Solvent Manager, Sample Manager and
Column Compartment. The column used was with a Zorbax XDB-C
18
column (50x2.1mm 1.8µm,
Agilent, Palo Alto, CA, USA) protected with in-line filter (0.2µm 2.1mm). Solvents were 1 mM ammonium acetate buffer, adjusted to pH 4.75 with glacial acetic acid (eluent A) and acetonitrile
(eluent B); the used solvent compositions are given in Table A1.
Table A1. Solvent composition programs for the UPLC methods
UPLC method 1 UPLC method 2 UPLC method 3
Time
(min)
0.0
2.5
Flow
(µl/min)
325
325
Solvent
(%A) (%B)
60
60
40
40
Time
(min)
0.00
1.75
1.80
3.90
4.00
5.00
Flow
(µl/min)
400
400
200
200
400
400
Solvent
(%A) (%B)
50 50 0.0
45 55 2.4
30
20
50
50
70
80
50
50
Time
(min)
Flow
(µl/min)
350
350
Solvent
(%A) (%B)
57.5 42.5
57.5 42.5
Mass Spectrometry
The mass spectrometer used was an API 3000 triple quadrupole (Sciex, Toronto, Canada) equipped with an ESI source (Turbospray ). The vaporizer temperature was 500 C. Nitrogen was used as nebulizer-, auxiliary- and collision gas. Interface settings and gas pressures were
52
manually optimized at the chromatographic conditions prevailing when the analyte in question elutes into the mass spectrometer. Detections were performed in multiple reaction monitoring
(MRM) mode; the used transitions are given in Table A2. “High resolution mode” corresponding to a peak width of 0.5 amu at half the maximum peak height (0.5 FWHM), was used in both the first and the third quadrupole.
Table A2. Transitions in multiple reaction monitoring (MRM) mode
Analyte Name Ionization Mode MRM transition
Amlodipine
UK 52.829
Simvastatin
Lovastatin
Glimepiride
Glibenclamide
Bendroflumethiazide
Cyclopenthiazide
Positive
Positive
Positive
Positive
Positive
Positive
Negative
Negative
m/z 409→238
m/z 443→272
m/z 419→199
m/z 405→199
m/z 491→352
m/z 494→369
m/z 420→289
m/z 378→205
Sample handling
Solid phase extraction (SPE) was used for pre-treatment of plasma samples. A schematic overview of the analytical workflow is shown in Figure A1. The frozen plasma was thawed and centrifuged
(3000 rpm for 5 minutes). Aliquots of 1 ml were added 20 µl of conc. phosphoric acid and diluted
1:1 in phosphate buffer. A mixture of the four internal standards (ISTD) was added to all samples, which were loaded onto a Bond Elut-Certify cartridge (Varian, Darmstadt, Germany). The SPEcolumn (130 mg/6 ml) had been pre-conditioned with 3 ml of methanol and 3 ml of H
2
O. Sample application was performed slowly under gravity flow. The column was washed with 2.5 ml of water, followed by 1.25 ml of 0.01 M acetic acid. The analytes were eluted in two consecutive steps. First fraction was eluted with 2.5 ml of methanol, and the second fraction was eluted with
5 ml of 5 % (v/v) 25 % aqueous ammonia in ethyl acetate. The individual fractions were vacuumcentrifuged to dryness. The residue of fraction 1 was redissolved in 200 µl of 40 % acetonitrile in
1mM ammonium acetate buffer (pH 4.75), while the residue of fraction 2 was redissolved in 200 µl of 25 % acetonitrile in 75% 25mM ammonium formate buffer (pH 2.75).
Positive-negative cut-off levels for blood samples containing a drug were based on lower limit of quantification (LLOQ), which were 0.50 µg/l, 0.25 µg/l, 0.25 µg/l, and 0.10 µg/l for amlodipine, bendroflumethiazide, glimepiride and simvastatin, respectively.
Chromatograms of relevant plasma samples spiked at LLOQ levels are shown in
Figure A2.1, A2.2 and A2.3.
53
Figure A1. Schematic overview of the analytical workflow
Solid Phase Extraction
Bond Elut-Certify (130 mg/6ml, Varian)
Conditioning 3 ml methanol
3 ml phosphate buffer
Sample application
1 ml plasma (centrifuged 5 min at 3000 rpm), 20 µl ISTD, 20 µl concentrated phosphoric acid, 1 ml phosphate buffer
Wash 2,5 ml milli-Q water
1,25 ml 0,01 M acetic acid
Elution steps 1 and 2
Fraction 1
2.5 ml methanol
Evaporation
Reconstitution
To dryness
200 µl of 40 % acetonitrile in 1 mM ammonium acetate (pH 4.75)
UPLC method
Method 1 Method 2
Injection volume
Drugs detected
10 µl
20 µl
Bendroflumethiazide
Cyclopenthiazide
Glimepiride
Glibenclamide
Simvastatin
Lovastatin
Fraction 2
5 ml of 5 % (v/v) 25 % aqueous ammonia in ethyl acetate
To dryness
200 µl of 25 % acetonitrile in 25 mM ammonium formate (pH 2.75)
Method 3
15 µl
Amlodipine
UK 52.829
54
Figure A2.1. Chromatogram of the MRM transitions from UPLC method 1 of Bendroflumethiazide
(plasma sample spiked at LLOQ) and its internal standard Cyclopenthiazide
Bendroflumethiazide
Cyclopenthiazide
Figure A2.2 Left: Chromatogram of the MRM transitions from UPLC method 2 of Glimipiride
(plasma sample spiked at LLOQ level) and its internal standard Glibenclamide.
Right: Simvastatin (plasma sample spiked at LLOQ level) and its internal standard Lovastatin
Glimepiride
Simvastatin
Glibenclamide
Lovastatin
55
Figure A2.3 Chromatogram of the MRM transitions from UPLC method 3 of Amlopidine (plasma sample spiked at LLOQ level) and its internal standard UK 52.829
Amlodipine
UK 52.829
Abbreviations used in this section
Amu
ESI
FWHM
ISTD
LLOQ
M
Atomic mass unit
Electrospray ionization
Full width at half height
Internal standards m / z
MRM rpm
SPE
UPLC
Lower limit of quantification
Moles per litre
Mass to charge ratio
Multiple reaction monitoring
Rounds per minute
Solid phase extraction
Ultra high pressure liquid chromatography
56