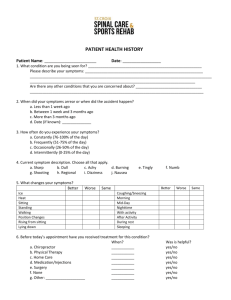
Diagnosis
advertisement
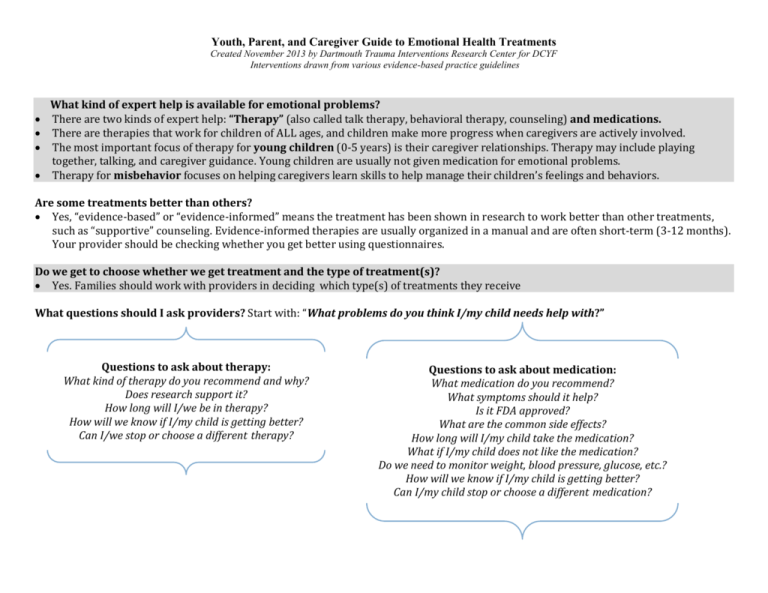
Youth, Parent, and Caregiver Guide to Emotional Health Treatments Created November 2013 by Dartmouth Trauma Interventions Research Center for DCYF Interventions drawn from various evidence-based practice guidelines What kind of expert help is available for emotional problems? There are two kinds of expert help: “Therapy” (also called talk therapy, behavioral therapy, counseling) and medications. There are therapies that work for children of ALL ages, and children make more progress when caregivers are actively involved. The most important focus of therapy for young children (0-5 years) is their caregiver relationships. Therapy may include playing together, talking, and caregiver guidance. Young children are usually not given medication for emotional problems. Therapy for misbehavior focuses on helping caregivers learn skills to help manage their children’s feelings and behaviors. Are some treatments better than others? Yes, “evidence-based” or “evidence-informed” means the treatment has been shown in research to work better than other treatments, such as “supportive” counseling. Evidence-informed therapies are usually organized in a manual and are often short-term (3-12 months). Your provider should be checking whether you get better using questionnaires. Do we get to choose whether we get treatment and the type of treatment(s)? Yes. Families should work with providers in deciding which type(s) of treatments they receive What questions should I ask providers? Start with: “What problems do you think I/my child needs help with?” Questions to ask about therapy: What kind of therapy do you recommend and why? Does research support it? How long will I/we be in therapy? How will we know if I/my child is getting better? Can I/we stop or choose a different therapy? Questions to ask about medication: What medication do you recommend? What symptoms should it help? Is it FDA approved? What are the common side effects? How long will I/my child take the medication? What if I/my child does not like the medication? Do we need to monitor weight, blood pressure, glucose, etc.? How will we know if I/my child is getting better? Can I/my child stop or choose a different medication? Youth, Parent, and Caregiver Guide to Emotional Health Treatments Created November 2013 by Dartmouth Trauma Interventions Research Center for DCYF Interventions drawn from various evidence-based practice guidelines Psychotropic medications and side effects Stimulants (e.g., Adderall, Ritalin, Concerta): headache, trouble sleeping, stomachaches, loss of appetite, weight loss. Rare: Tics (twitching of the face, blinking or throat clearing, biting finger nails), increased irritability or excitability, decreased growth (possibly an inch over 3-8 years). Please tell your doctor if your child has relatives under 50 who have died of heart problems, or your child has a history of irregular heartbeats, heart murmurs, fainting spells, chest pain, or structural heart problems. Strattera (non-stimulant for ADHD): sleepiness or insomnia, appetite loss, weight loss, nausea, stomachaches. Rare: eyes and/or skin turning yellow or changes in urine color (related to inflammation of the liver), trouble urinating, or worsening moods. The U.S. Food & Drug Association has included a “black box” warning that Strattera may increase suicidal thoughts and behaviors. Antidepressants (SSRIs, SNRIs; e.g., Prozac): headache, dizziness, stomachaches, nausea, loose stools or diarrhea, dry mouth, weight gain or loss (mild), sleepiness or insomnia. Rare: Feeling excited, irritable or more depressed. The U.S. Food and Drug Administration has put out a “black box” warning that antidepressants may increase suicidal thoughts and behaviors (about 4% of the time). Atypical Antipsychotics (e.g., Seroquel, Risperdal)/Second Generation Antipsychotics (e.g., Haldol): sleepiness, dizziness, increased appetite, weight gain with increased cholesterol, muscle stiffness, tremors (shakiness). Rare: After many years of use of these medications can lead to being overweight, high blood pressure and risk of diabetes or high blood sugar and some may develop a twitching of the face, tongue, arms or legs called tardive dyskinesia that may not always go away when the medication is stopped. Your child needs to be regularly examined (weight, blood pressure) and have regular blood tests. In extremely rare cases, these medications my cause muscle stiffness and high fevers that can be fatal. Lithium: sleepiness, tremors, weight gain, increased or decreased urination, increased thirst, worsening of acne, loose stools or diarrhea Rare: Thyroid or kidney problems, irregular heartbeat, confusion, brain injury if blood level goes to high, clumsiness and dizziness. Regular blood tests are needed to check for problems and to be sure the blood level of lithium is right. Depakote, Tegretol, Lamictal, Trileptal: sleepiness, tremors, weight gain. Rare: liver or pancreas problems, dizziness, confusion, changes in blood cell and platelet numbers, changes in vision, severe skin rash, and birth defects if taken when pregnant. Lamictal or Tegretol can cause a severe, possibly deadly allergic reaction where the skin blisters and falls off or the white blood cell count goes very low. Please let the doctor know if there are any new rashes or changes of the skin. Regular blood tests are needed to check for problems and to be sure the blood level of the medicine is right. Guanfacine, Clonidine: sleepiness, low blood pressure, dizziness, dry mouth, dry eyes, blurry vision, headache, weakness, and decreased heart rate. If your child has been taking this medication and suddenly stops it, his/her blood pressure can go up very high. If the medication needs to be stopped, you should discuss with your doctor how to go off this safely. -------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------- On-line resources: Parent medication guide: http://www.parentsmedguide.org/ Youth medication guide: http://www.nrcyd.ou.edu/learning-center/med-guide AACAP: http://www.aacap.org/AACAP/Families_and_Youth/Facts_for_Families/Home.aspx?hkey=fc8eda98-f824-4988-bb07-d49a8545e4e8