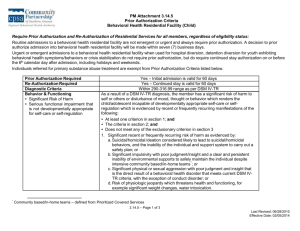
BNET - South Florida Behavioral Health Network
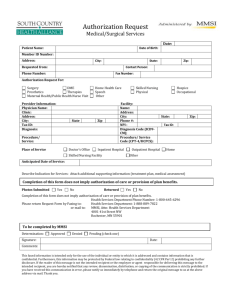
advertisement

SOUTH FLORIDA BEHAVIORAL HEALTH NETWORK UTILIZATION MANAGEMENT MANUAL Table of Contents Table of Contents ...................................................................................................................................... - 1 Glossary of Terms ..................................................................................................................................... - 2 Utilization Management Overview ............................................................................................................. - 9 Children’s System of Care ....................................................................................................................... - 11 Behavioral Health Network (BNET) ......................................................................................................... - 12 Children’s Crisis Response Team (CCRT) .............................................................................................. - 20 Children’s Crisis Stabilization Unit (CCSU) ............................................................................................. - 25 Families and Communities Empowered for Success (FACES) ............................................................... - 27 Functional Family Therapy (FFT) ............................................................................................................ - 35 Specialized Therapeutic Group Care ...................................................................................................... - 39 Statewide Inpatient Psychiatric Program (SIPP) ..................................................................................... - 43 Juvenile Addictions Receiving Facilities (JARF) ...................................................................................... - 55 Children’s Residential Substance Abuse Services .................................................................................. - 57 Adult System of Care ............................................................................................................................... - 64 Crisis Stabilization Units (CSUs) ............................................................................................................. - 65 Florida Assertive Community Treatment Team (FACT) .......................................................................... - 68 State Treatment Facilities ........................................................................................................................ - 71 Incidental Expenses ................................................................................................................................. - 73 Short-term Residential Treatment (SRT) Program - Civil ....................................................................... - 74 Short-term Residential Treatment (SRT) Forensic Program .................................................................. - 76 Short-term Residential Treatment (SRT) ................................................................................................. - 79 Miami-Dade Forensic Alternative Center ................................................................................................. - 79 Adult Residential Level II Mental Health .................................................................................................. - 82 Adult Forensic Services ........................................................................................................................... - 86 Indigent Drug Program (IDP) ................................................................................................................... - 87 Projects for Assistance in Transition from Homelessness (PATH) ......................................................... - 88 Family Intervention Specialists (FIS) ....................................................................................................... - 89 Adult Residential Levels I-II Substance Abuse ........................................................................................ - 91 General .................................................................................................................................................... - 99 Temporary Assistance for Needy Families (TANF) ............................................................................... - 100 Reporting and Compliance Reviews ..................................................................................................... - 103 Authorizations & Denials ........................................................................................................................ - 105 Reconsiderations ................................................................................................................................... - 106 Forms ..................................................................................................................................................... - 109 Data Sharing & Consent to Release and Exchange Information .......................................................... - 113 - ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 -1- Glossary of Terms DEFINITION OF TERMS: 1. Accessible: Children, families and community members should be helped to become knowledgeable about how to ask for and receive services that are timely, comprehensive and family-friendly without facing unreasonable barriers. Access to services meets individualized needs of the consumer (i.e., physical, emotional, and social needs), and are timely and geographically appropriate. Consumers have access to services regardless of race, language, cultural background, sexual orientation, age or developmental level, psychological characteristics, physical condition, spiritual beliefs, social preferences, gender or ability to pay. This also includes accessibility needs of consumers, funders, provider representatives, care practitioners, family members, volunteers, visitors, employees and community stakeholders to services contracted through and facilities operated by SFBHN. 2. Actuarial Study: Analysis of past utilization data for specific groups in order to estimate future costs. Built upon assumptions where necessary, the final analysis combines all estimates to compute the cost per member per month (PMPM). 3. American Society of Addiction Medicine Patient Placement Criteria For the Treatment of Substance Related Disorders Second Edition (ASAM PPC-2): As part of the State of Florida’s movement toward a comprehensive system of managed behavioral health care, the Department of Children and Family Services Substance Abuse Program Office implemented the American Society of Addiction Medicine Patient Placement Criteria for the Treatment of Substance-Related Disorders, Second Edition (ASAM PPC-2) and the Florida Supplement, on July 1, 1997. All contracted State of Florida substance abuse providers are required to use the ASAM PPC-2R, Florida Supplement, and its accompanying forms. The primary purpose of the Florida Supplement, as an extension of the ASAM PPC-2R, is to provide clinicians with an abbreviated reference document to assist them in documenting their placement decisions in accordance with Florida’s system of licensable services. 4. Alternative Services: Services outside of the department’s Integrated Data System cost centers that are deemed necessary to meet the objectives outlined in a consumer's treatment plan. 5. Assessment: The systematic collection and integrated review of individual-specific data and completion of evaluations for determining clinical eligibility and treatment planning. 6. Assessment Instrument: A tool used for collection of detailed information concerning an individual’s substance abuse, emotional and physical health, social roles, and other areas that may reflect the severity of the individual’s abuse of alcohol or drugs, as a basis for identifying an appropriate treatment regimen. 7. Average Length of Stay (ALOS): Duration of treatment in a treatment setting, expressed in units of service. Measure is calculated by dividing the sum of total days enrolled in a specific service or setting over a specific date range by the total number of consumers admitted during a same time period. 8. Behavioral Health Network (BNET): means the statewide network of Providers of Behavioral Health Services who serve non-Medicaid eligible children with mental or substance-related disorders who are determined eligible for the Title XXI part of the KidCare Program. This network includes providers who are managed behavioral health care organizations, private and state funded mental health and substance-related disorders providers. The Behavioral Health Network is administered by the Department of Children and Families, Children's Mental Health State Program Office to provide a comprehensive behavioral health benefits package for children with serious mental or substancerelated disorders. ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 -2- 9. Behavioral Health Services: Mental health services and substance abuse prevention and treatment services as defined in chapters 394, 397 and 916, F.S. which are provided using state and federal funds. 10. Case Management: This service includes assessment, coordination of service linkages, referral, and follow-up of clinically indicated treatment services required for a consumer within a holistic and costeffective system of care. This process includes coordinating all of consumers’ care and advocating for consumers’ needs. 11. Child Global Assessment Scale (CGAS): The scale used to report the clinical judgment of a child’s overall level of functioning as based on and as described in the Diagnostic and Statistical Manual of Mental Disorders, Most Current edition (DSM Axis V). 12. The Children's Functional Assessment Rating Scale (CFARS): A method of documenting and standardizing impressions from clinical evaluations or mental status exams of children that assess cognitive, social and role functioning. 13. Consumer: Person who receives substance abuse and/or mental health services. Consumer, patient, and consumer are used interchangeably. 14. Clinical Assessment: The collection of detailed information concerning an individual’s behavioral health, emotional and physical health, social roles, and other areas that may reflect the individual’s overall health as a basis for identifying an appropriate treatment regimen. 15. Clinically Necessary: Services deemed appropriate and necessary to treat protect and enhance the health status of consumers based on consumers’ symptoms and diagnoses and if services are not provided could adversely affect the consumer. All services are to be provided in accordance with accepted standards of practice. 16. Behavioral Health Clinician: A substance abuse or mental health professional that provides one or more of the following services: assessment; individual, group, or family counseling services; or case management. 17. Community-Based Services: Behavioral health services provided outside of a state facility. 18. Community-Focused: The process of planning, management and decision-making to ensure resources are designed to build on the unique strengths and meet the specific needs of the local community. 19. Concurrent Review: Specific methodology and practices utilized periodically during the course of treatment to verify that the treatment is clinically necessary and progressing at an appropriate pace. 20. Continued Stay: An extension of services at the same level of care. A Continued Stay may be clinically indicated where consumers have not completed treatment goals and have not reached the necessary level of functioning for the next least restrictive level of care. 21. Continuous Quality Improvement: Continuous internal improvements in service provision and administrative functions. Continuous improvement is an ongoing effort to improve services and/or processes. These efforts can seek “incremental” improvement over time or “breakthrough” improvement all at once. 22. Continuum of Services: Recovery-oriented systems of care will offer a full array of services, including prevention, pretreatment, treatment, continuing care and support throughout recovery. Individuals will have a full range of stage-appropriate services from which to choose at any point in the recovery process. ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 -3- 23. Co-occurring Disorder: Consumers with co-occurring disorders (COD) have one or more disorders relating to the use of alcohol and/or other drugs of abuse as well as one or more mental disorders. A diagnosis of co-occurring disorders occurs when at least one disorder of each type can be established independent of the other and is not simply a cluster of symptoms resulting from the one disorder. 24. Co-occurring Disorder Service Capability: The ability of any program to coordinate every aspect of its program infrastructure (policies, procedures, practices, documentation, and/or staff competencies), within its existing resources, to be able to provide and/or coordinate appropriately matched, integrated services to the individuals and families with co-occurring disorders that are routinely presenting for care in that program. 25. Covered Days: The authorized service units for which the Department of Children & Families, Medicaid, HMOs, and other managed care companies will reimburse for services rendered. Units of measure may be limited per episode of illness, per year, or per lifetime. 26. Criteria: Predetermined elements related to particular health care services with which aspects of the quality, clinical necessity, and appropriateness of a health care service may be assessed by health care professionals. 27. Data Management: Activities that use data elements to track cost, utilization, quality of care and access to services within the network of providers. “CFP 155-2 Department of Children & Families, Pamphlet 155-2 - Mental Health and Substance Abuse Measurement and Data, effective August 20011 (10th edition, version 2)”, or the latest revised edition thereof means a document promulgated by the department that contains required data-reporting elements for substance abuse and mental health services, hereafter referred to as “CFP 155-2”, and which can be found at: http://www.dcf.state.fl.us/mentalhealth/publications/index.shtml. 28. Day or Night Treatment: A therapeutic environment wherein services and activities are generally provided a minimum of 4 consecutive hours three or more days per week. 29. Denial: An adverse determination by the Utilization Management Program resulting in a denial of authorization for requested services. Denials are based upon a lack of clinical necessity and reasonableness and/or appropriateness of the requested treatment service. Denials may also be based on eligibility criteria and the availability of coverage days. 30. Discharge Planning: Advance preparations for assuring the continuity of care for moving a consumer from one level of care to another within or outside the current agency. 31. Discharge Summary: A narrative summary of consumer treatment records which describes the consumer’s accomplishments or lack thereof during the treatment episode. The summary includes the treatment interventions and activities provided and consumer’s responses to the interventions, progress made, problems encountered, and reason(s) for discharge and referrals and/or treatment recommendations provided. 32. Evidence-Based Practices: Those practices that are based on accepted practices in the profession and are supported by research, field recognition, or published practice guidelines. 33. Family Intervention Specialists/Adult Intervention Specialists (FIS). Individuals employed to provide adult behavioral health outreach, screening, intervention, and case management to families involved in the child welfare system and/or the Abuse Hotline. 34. Family Intervention Specialist Service. Services designed to reduce the incidence of child abuse and neglect resulting from parents’ or caregivers’ behavioral health and to improve outcomes for families in ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 -4- the child welfare system and/or community based care. 35. Forensic Mental Health Services: Forensic Mental Health Services provide services to individuals with mental illness pursuant to Chapter 916, Florida Statutes. 36. Global Assessment of Individual Needs (GAIN): One of the Department approved evidenced-based assessment instruments. Information regarding this instrument is available from the following website: http://www.chestnut.org/LI/gain/ 37. HIPAA: The acronym for Health Insurance Portability and Accountability Act of 1996. Privacy Act included in 45 CFR Parts 160 and 164. 38. High-Risk: Consumer presenting with a profile that includes a multitude of treatment requirements with at least one problem area identified as ‘severe’. Cases with Child Welfare System involvement and cases in which the consumer is either pregnant and/or an Intravenous (IV) drug user are also identified as High-Risk. High-Risk suggests increased risk that the consumer may not successfully complete the treatment episode and/or may have a poor prognosis. 39. High-Utilizer: Consumer with three or more admissions to residential level I or level 2 substance abuse treatment in a 2 year time period. 40. Incidental Cost Center: This cost center provides for incidental expenses, such as clothing, medical care, educational needs, developmental services, FACT Team housing subsidies and pharmaceuticals and other approved costs. All incidental expenses must have prior written authorization by the SFBHN’s authorized staff member or be authorized in the contract. 41. Incompetent to Proceed (ITP): Unable to proceed at any material stage of a criminal proceeding, which shall include trial of the case, pretrial hearings involving questions of fact on which the defendant might be expected to testify, entry of a plea, proceedings for violation of probation or violation of community control, sentencing, and hearings on issues regarding a defendant's failure to comply with court orders or conditions or other matters in which the mental competence of the defendant is necessary for a just resolution of the issues being considered as outline in Chapter 916 of Florida Statutes. 42. Indigent Drug Program (IDP): The program that allows the Department of Children and Families to purchase medications for individuals who are indigent. 43. Individual(s) Served: Any individual who is receiving services in any substance abuse treatment or prevention program or mental health treatment program whose cost of care is paid, in part or in whole, by the Department, Medicaid, Medicaid capitated managed care entities, or local match. 44. Inmate of a public institution: An individual that is serving time for a criminal offense or confined involuntarily in state or federal prisons, jails, detention facilities, or other penal facilities. A facility is a public institution when it is under the responsibility of a governmental unit or when a governmental unit exercises administrative control. 45. Intensive Outpatient: A planned and organized service where substance abuse agency staff provides regularly scheduled sessions within a structured program, with a minimum of nine treatment hours per week. Examples include day or evening programs in which consumers attend a full spectrum of treatment programming but also spend time outside the treatment setting including residing outside of the facility. 46. Interim Service:. In cases where consumers are on the wait list for behavioral health treatment, services are provided to reduce adverse effects to the consumer and the community. These services are provided until the consumer is admitted into the recommended treatment program and/or level of ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 -5- care. Interim Services may include placement into a lower level of care pending entry into recommended level of care. Interim Services may also include peer support services such as drop in centers and/or linkages to recovery support services. Interim services also may include a combination of services that are provided to meet the needs and desires of the individual while waiting for services. 47. Juvenile Incompetent to Proceed (JITP): A "child" or "juvenile" or "youth" as defined in chapter 985, F.S., as any unmarried person under the age of 18 who has not been emancipated by order of the court and who has been found or alleged to be dependent, in need of services, or from a family in need of services; or any married or unmarried person who is charged with a violation of law occurring prior to the time that person reached the age of 18 years deemed incompetent to proceed by virtue of mental illness. 48. Managing Entity (ME): A corporation that is organized in the State of Florida, is designated or filed as a non-profit organization under section 501(c)(3) of the Internal Revenue Code, and is under contract to the department to manage the day-to-day operational delivery of behavioral health services through an organized system of care. 49. Monitoring Subcontracts: The process whereby the managing entity conducts a systematic organized review of a network provider’s performance in order to give reasonable assurance that the network provider is complying with subcontract requirements, rules, regulations and laws applicable to contract performance. 50. Outcome: The results/effects obtained as a result of a measured performance. 51. Outcome Measurement: State-Mandated and/or SFBHN required behavioral health consumer outcomes. 52. Outpatient Treatment: A therapeutic environment wherein services are provided by appointment during scheduled operating hours. Services are generally provided via individual, family and/or group sessions where the consumer does not reside at the facility. 53. Passive Authorization: passive utilization management for all other cost centers not specified in other sections of this manual. SFBHN specifies the limitations associated by each cost center that SFBHN will reimburse the provider for. 54. Prior Authorization: The authorization required for services identified by Utilization Management Program. Authorizations are necessary for reimbursement for designated State-Funded treatment services. 55. Program Reviews: Reviews conducted by the Utilization Management Program to ensure compliance with Departmental and State requirements, as applicable. Program Reviews also ensure quality-ofcare. 56. Participant: Any individual who takes part in targeted substance abuse prevention programs, activities or services which are paid, in part or in whole, by the department. 57. Performance Measures: Quantitative indicators, outcomes and outputs that are required by the contracted and implemented by the organization to objectively measure performance of the ME and subcontractors and are used by the ME and network subcontractors to improve services. 58. Program: A structured Schedule of Activities designed so that participants will attain so far as possible, certain educational, attitudinal, social and behavioral objectives. This is an unduplicated count of participants. ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 -6- 59. Projects for Assistance in Transition from Homelessness (PATH): The Federal grant to support homeless individuals with behavioral health needs. 60. Promising Practices: The use of practices that incorporate the best objective information available regarding effectiveness and acceptability. 61. Protected Health Information: Any information whether oral or recorded in any form or medium that is created or received by a health care provider, health plan, public health authority, employer, life insurer, school or university, or health care clearinghouse; and relates to the past, present, or future physical or mental health or condition of an individual; the provision of health care to an individual; or the past, present, or future payment for the provision of health care to an individual. 62. Provider Network: The direct service agencies that are under contract with a managing entity and that together constitute a comprehensive array of emergency, acute care, residential, outpatient, recovery support, and consumer support services or other services as designated by this contract. See section 394.9082, F.S. 63. Residential Treatment: A therapeutic intervention processes for individuals who cannot or do not function satisfactorily in their own home environments. Typically, this is a structured, live-in environment within a non-hospital setting which includes, at a minimum, a range of assessment, rehabilitation, and treatment services. Access to ancillary services are also provided when indicated. 64. Quality Assurance: A systematic monitoring and evaluation of the various aspects of a project, service or facility to maximize the probability that minimum standards of quality are being attained by the production process. 65. Quality Improvement: A management technique to assess and improve internal operations and network services. It focuses on organizational systems rather than individual performance and seeks to continuously improve quality. The process involves setting goals implementing systematic changes, measuring outcomes, and making subsequent appropriate improvements. Quality assurance activities will assess compliance with contract requirements, state and Federal law and associated administrative rules, regulations, and operating procedures and validate quality improvement systems and findings. 66. Recovery: An on-going process which enables a person with behavioral health issues to live a meaningful life in a community of his or her choosing while striving to achieve his or her potential. This allows individuals to improve their health, wellness, and quality of life. 67. Recovery Based: Based upon a personal process of overcoming the negative impact of substance abuse addiction or mental illness. A system of care provides treatment and supports that promote recovery and functioning in the community. 68. Retrospective Review: Review of cases retrospectively for evaluating clinical processes and outcomes, consumer satisfaction, efficiency of services and quality of care. 69. Temporary Assistance to Needy Families (TANF): Any family receiving cash assistance payments or TANF diversion services from the state program pursuant to the provisions of section 414.045, F.S., and Part A of Title IV of the Social Security Act. 70. TANF Participant: A person or family member of that person defined in 45 CFR Part 260.30 and section 414.1585 and subsection 414.0252(9), F.S. 71. Transfer Summary: A written justification of the circumstances to transfer a consumer from one treatment component to another or from one provider agency to another. ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 -7- 72. Treatment Plan: A plan developed by the treatment team with the consumer that details measurable goals and objectives for the consumer’s treatment. The plan shall include the type and frequency of treatment interventions and the projected target dates for each objective. Treatment Plans address all indicated treatment needs. Some goals may be deferred until a later time as indicated. 73. Treatment Plan Reviews: An amendment of the original treatment plan which updates the consumer’s progress in treatment and denotes any deficiencies and issues still to be addressed in treatment. 74. Substance Abuse and Mental Health (SAMH): The Substance Abuse and Mental Health Program within the Department of Children and Families. 75. SOAR (SSI/SSDI Outreach, Access and Recovery): A technical assistance initiative. This strategy helps States and communities increase access to SSI and SSDI for people through training, technical assistance and strategic planning. 76. “Stakeholder” means individuals/groups with an interest in the provision of behavioral health services. 77. Statewide Inpatient Psychiatric Programs (SIPP): Residential inpatient facilities under contract with the Agency for Health Care Administration under the Medicaid IMD waiver for children under age 18 to provide diagnostic and active treatment services in a secure setting. 78. Substance Abuse and Mental Health Information System (SAMHIS): The department's online data system which providers are required to use to collect and report data and performance outcomes on persons served whose services are paid for, in part or in whole, by the department's Substance Abuse and Mental Health (SAMH) contract, Medicaid, or local match. Instructions on how to access the system can be found in CFP 155-2. 79. System of Care: Behavioral health services that are coordinated and developed into an integrated network of services accessible and responsive to the needs of individuals served, their families, and community stakeholders. 80. Unit of Measure: The billing component services. The unit of measure for residential levels I and II is a ‘bed-day’, for Day/Night it is a ‘day’, and for Outpatient it is a ‘contact hour’. All units of measure can be found in 65E-14 of Florida Administrative Codes. 81. Utilization Management: Is a system for the evaluation of the appropriateness, clinical need and efficiency of behavioral health services procedures and facilities according to established criteria and/or guidelines. Typically it includes new activities or decisions based upon the analysis of a case and includes discharge planning, concurrent planning, and preauthorization, for some services as well as retrospective reviews and focused reviews of individual cases. It also covers proactive processes, such as concurrent clinical reviews and peer reviews, as well as appeals introduced by a consumer or subcontractor. 82. Wait List: This list includes consumers identified as waiting for placement into a behavioral health treatment program. Wait Lists are used when programs are at full capacity and unable to admit additional consumers into the prescribed service. ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 -8- Utilization Management Overview Utilization Management (UM) is a system for the evaluation of the appropriateness, clinical need and efficiency of behavioral health services, procedures and facilities according to established criteria and/or guidelines. For the purposes of this manual, the specific goals of utilization management include elimination/management of wait lists, the maximum utilization of treatment resources, and the delivery of clinically appropriate services in the least restrictive setting and most cost effective manner. Utilization management systems include preauthorization for some services as well as passive authorization with retrospective reviews and focused reviews of individuals receiving services and subcontractors whose utilization of services is outside of expected parameters. Utilization management includes methods used to manage the system of care to ensure access to the appropriate level of care, at the right frequency and for the appropriate duration. It also includes financial screening to ensure maximization of fiscal resources including other third party payors such as, but not limited to KidCare, Medicaid, Medicare, and other HMOs. These methods may include programs of intervention and/or diversion. Utilization management includes not only managerial and supervisory strategies, methods and tools to ensure timely access to care, but also includes processes to promote continuous improvement to manage resources. As the Managing Entity for South Florida, South Florida Behavioral Health Network (SFBHN) is enhancing our automated utilization management system to include additional treatment authorization and management reports for the system of care. The SFBHN conducts oversight, reporting and management of the behavioral health services for individuals served. In the event that waiting lists do develop, the managing entity implements procedures for managing the substance abuse and mental health waiting list for all applicable levels of care including provision of interim services through utilization management strategies. SFBHN strives to ensure that its core values and principles are incorporated on every level of the System of Care (SOC). One of the mechanisms SFBHN utilizes to ensure that these core values and principles are embedded into the SOC is its Utilization Management Program. SFBHN’s applies its UM processes to ensure those values and principles are intrinsic to the services provided and are integrated and reflected at every level and/or entry point. These core principles and values are: Consumer Guided Individualized to meet the needs of the Consumer Family Driven Community Based Culturally and Linguistically Competent Transparent Recovery and Resiliency Focused SFBHN subcontractors are required to ensure SFBHN is the payor of last resort and as such has adopted DCF CFOP 155-2. SFBHN subcontractors are required to adhere to DCF CFOP 155-2 which specifies that services are only to be furnished to eligible individuals and families with mental health, substance abuse, and/or co-occurring disorders, subject to the availability of funds. Further sections in this manual specify additional criteria that must be met for various services. In accordance to Attachment I the Managing Entity shall not bill the Department for services provided to: (a) Individuals who have third party insurance coverage when the services provided are covered under the insurance plan; or (b) Medicaid enrollees or recipients of another publically funded health benefits assistance program, when the services provided are covered by said program regardless of limitation. The SFBHN conducts initial and continued stay authorizations for applicable levels of care as described in the contract with the Department in order to ensure timely access to behavioral health services and ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 -9- minimize the wait lists. The authorization processes include: Timeliness standards for authorization review: All authorization reviews must adhere to timeline standards for the services provided and departmental, statutory, and judicial regulations or requirements. Processes for communicating UM decision-making criteria to practitioners including any standardized tools and assessments for use in determining placement and/or level of care. Provisions for providing timely reconsiderations, or second opinions, when a request for authorization for a particular service is denied. (Reconsideration differs from a grievance in that grievances are used when a recipient or member of the covered population believes that he or she has been treated improperly, whereas reconsideration is a request to review authorization or reauthorization for a particular service.) The second opinion shall be obtained according to the timeliness standards for the service in question as outlines in the Reconsiderations section of this manual. SFBHN collaborates with community partners to leverage and enhance services described throughout UM Manual. SFBHN collaborative include partnerships with DCF Child Protective Investigations (CPI), Community-based Care (CBC) organizations, Court Systems, etc. SFBHN has formalized MOUs with collaborating partners and is continually engaging new systems partners to enhance and leverage services for consumers served. This manual establishes written utilization management procedures inclusive of and not limited to agreed upon behavioral health services. These procedures meet the Department’s requirements and defines the processes to be utilized to minimize over- and underutilization of services. ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 10 - Children’s System of Care ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 11 - Section: 1 Children’s Mental Health Behavioral Health Network (BNET) POLICY: Behavioral Health Network (BNET) is a statewide network of Providers of Behavioral Health Services who serve non-Medicaid eligible children with mental or substance-related disorders who are determined eligible for the Title XXI part of the KidCare Program. This network includes providers who are managed behavioral health organizations, private and state funded mental health and substance-related disorders providers, and Lead Agencies. PURPOSE: To define the procedures necessary for eligibility determination, assessment, and access to BNET services. PROCEDURE: I. Ensuring Continuity of Services for Children Transferring Between Districts/Regions/Providers: A. SFBHN’s BNET Coordinator will ensure that the region’s behavioral health liaison from the sending provider shall contact the receiving region’s Title XXI region coordinator, the Children’s Medical Services liaison, and Behavioral Health Network HQ in Tallahassee and that the behavioral health liaison shall provide the receiving region the child’s name, social security number, effective date of transfer, and the county to which the child will be transferring. Additionally, the child’s parent or guardian should be given the name, phone number, and address of the new behavioral health liaison. B. Copies of the child’s current treatment plan, demographic information, and all other pertinent information should be sent to the receiving provider prior to the child’s transfer. Electronically transmitted confidential information shall follow established guidelines to ensure the confidentiality of this information is maintained. C. If applicable, the child should also be given enough medication to hold the child over until the receiving provider has had an opportunity to conduct their own assessment of the child’s needs based on his or her presenting condition. II. Slot Transfer Scenarios: A. A child transfers from one open slot from a sending region into another open slot in the receiving region. B. Child from a sending provider transfers into receiving provider slot sometime after the current enrollment month begins. There will be no change in either region’s slot allocation. C. A contract amendment is not required since the receiving provider has an available slot. D. A child transfers to a receiving region that has no available slots. E. If a slot is not available in the receiving region, the slot from the sending region will follow the child into the receiving region and will remain there until the first available slot in the receiving region becomes open. F. Children will be moved into the next available slot based on their official Children’s Medical Services start date. G. Once the child is enrolled, the slot returns as a vacant slot to the sending provider. H. A contract amendment is not required since the cost of service is billed to the sending provider. I. An enrolled waiting child transfers to a region with available slots. J. An enrolled waiting child will transfer from enrolled waiting status to enrolled status taking one of the receiving region’s available slots. ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 12 - K. A contract amendment is not required as enrolled waiting children are not considered officially enrolled in the Behavioral Health Network. L. An enrolled waiting child transfers to a region with no available slots. M. An enrolled waiting child will transfer from enrolled waiting status in the sending region to enrolled waiting status in receiving region. N. Enrolled waiting children will be moved into the next available slot based on their official CMS start date. III. Payment for Services During Transfers: A. SFBHN’s BNET Coordinator (in conjunction with the SFBHN contract manager, if different) must approve the prorated and/or capitation distribution and any capitation payment invoices prior to the distribution of funds. B. Conditions for payment for services when a child transfers prior to next enrollment month. C. The sending provider retains a pro-rata share of the capitation for the month up to and including the actual date of transfer. D. The pro-rata share shall be determined by dividing the monthly capitation rate by the number of days in the current enrollment month. For example $1,000/30 = $33.33 per day. If the child moves out of the district/region on the 15th day, the sending provider would receive $499.95 for that child. The remaining balance of the capitation ($500.05) is paid to the receiving provider. E. SFBHN’s BNET Coordinator (in conjunction with the SFBHN contract manager, if different) should ensure the child is still eligible and enrolled prior to the approval of the invoice. If the child is still enrolled the SFBHN’s BNET coordinator (in conjunction with the SFBHN contract manager, if different) will approve the invoice as prescribed by local region practice. F. Once approved and processed the sending SFBHN’s BNET coordinator or SFBHN contract manager will complete an invoice to the receiving Title XXI region coordinator that will include the child’s name, social security number, month of service, and the prorated amounts to be paid to both the sending and receiving providers. G. The receiving Title XXI region coordinator will provide their network provider with a copy of the invoice. H. Conditions for payment for services after the initial transfer when there are still no available slots in the receiving district/region. I. At the end of the current enrollment month, the receiving provider will prepare an invoice with only the child’s name, social security number, and month of service and send to SFBHN’s BNET coordinator for signature and approval. J. SFBHN’s Title XXI BNET coordinator (or SFBHN contract manager if not the same) should ensure the child is still eligible and enrolled prior to the approval of the invoice. If the child is still enrolled the SFBHN’s BNET coordinator (or SFBHN contract manager) will approve the invoice and send back to the sending provider in order to process the invoice for payment as prescribed by region practice. K. Upon receipt, the sending provider will pay the receiving provider the entire monthly capitation rate based on the approved invoice from the sending provider. L. Payment for services for enrolled waiting children is done by invoicing the receiving region’s local Children’s Medical Services office if the provider is serving these children. SFBHN is not involved in these transactions. Enrolled waiting children’s expenditures should not be reported to the SFBHN data system. SFBHN encourages its Title XXI providers to develop an agreement with their local Children’s Medical Services office to be the behavioral health services provider for these children. IV. Initial Eligibility Determination and Assessment: A. Every child referred to the Behavioral Health Network shall be screened as a first step in determining the child's clinical eligibility for services. If the screening indicates the child ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 13 - has the potential to meet the Behavioral Health Network clinical eligibility criteria described in this section, an assessment shall be conducted. B. A child shall be considered eligible for behavioral health services from the Behavioral Health Network when the child is determined to be Title XXI eligible for the Florida KidCare Program, be at least five (5) years of age and not yet nineteen (19) years of age; and, 1. The child requires a level of care not available in other KidCare programs; and, 2. The child is expected to show improvement or achieve stability as a direct result of the services to be rendered under the benefit package specified in Chapter 65E11, Florida Administrative Code; and, 3. At the time of assessment, the child requires no more than 30 days of residential treatment; and, 4. The child's family indicates a willingness to participate in the goals and objectives outlined in the child's treatment plan; and, 5. The child meets the Title XXI Behavioral Health Network’s clinical eligibility criteria. C. SFBHN’s BNET coordinator is responsible for ensuring “The Behavioral Health Network Screening and Eligibility Tracking Form” is properly completed prior to approval and submission to the Title XXI Behavioral Health Unit in Tallahassee. Each of the following items must be legibly filled out. 1. Provider Information and Referral Source Section. The following must be indicated: a. Who is filling out the form. b. This person’s phone number with area code. c. Name of lead agency that is responsible for child. d. The referral source is circled or checked. e. If this is a Florida Healthy Kids referral, the Florida Healthy Kid account number is provided. 2. Demographic Section: a. The child’s social security number, last name, first name, date of birth and county of residence are indicated. b. The legal custodian’s last name and first name are noted. 3. Part I – Initial Screening: a. The box indicating whether or not the child meets the Title XXI Behavioral Health Network treatability criteria is checked or circled. b. The box indicating whether or not the child’s parents have signed the Statement of Understanding is checked or circled. A child will not be considered for enrollment until such time that the child’s custodian has signed the Statement of Understanding. c. Person conducting the screening has indicated the date of the screening and their initials are indicated. 4. Part II – Assessment Clinical Eligibility. The person conducting the assessment has indicated that the child meets the following Title XXI Behavioral Health Network clinical criteria: a. The child has a DSM-IV-R Axis I clinical classification of mental disorder or substance-related disorder. b. Attention-Deficit Disorders are excluded as DSM-IV-TR Axis I mental disorders in determining clinical eligibility for the Behavioral Health Network: c. The child is experiencing significant functional impairment as a result of his or her condition as demonstrated by a CGAS score of 50 or below. d. The date of the assessment and initials of the person conducting the assessment are indicated. ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 14 - e. If all of the above is correctly filled out, SFBHN’s BNet Coordinator signs the form, makes two copies with one going back to the liaison and one going to the Title XXI Behavioral Health staff at the Children’s Mental Health state program office. V. The Statement of Understanding: A. The Statement of Understanding is intended to be used by the Behavioral Health Liaison as a tool to facilitate understanding by parents/guardians of key points about the program and their responsibilities to their child as an enrollee in the Behavioral Health Network. The form needs to be completed only once per child unless the responsible parent/guardian changes. B. The Behavioral Health Liaison should plan to complete the Statement of Understanding sometime during the process of explaining the program to the parent/guardian and completing the screening/assessment instrument. The procedure requires that: 1. Each point of the Statement of Understanding is explained to, and is initialed by, the parent/guardian. 2. The form be signed and dated by the parent/guardian and signed by the Behavioral Health Liaison. 3. The form becomes part of the file maintained by the Behavioral Health Liaison on the child. 4. A copy of the completed form be provided to the SFBHN’s BNet Coordinator along with the screening/assessment instrument. 5. A copy of the signed and dated form is provided to the parent/guardian. VI. Re-verification and Request for Disenrollment Form: A. SFBHN’s BNET coordinator is responsible for ensuring “The Behavioral Health Network Re-verification and Request for Disenrollment Form” is properly completed prior to approval and submitted to the Title XXI Behavioral Health staff at the Children’s Mental Health state program office. Re-verification occurs every six months. Each of the following items must be legibly filled out. 1. Provider Information and Referral Source Section. The following must be indicated. a. The person who is filling out the form. b. This person’s phone number with area code. c. Name of lead agency that is responsible for child 2. Demographic Section a. The child’s social security number, last name, first name, date of birth, and county of residence are indicated. b. The legal custodian’s last name and first name are noted. 3. Part I – Assessment – Re-verification. The person conducting the assessment has indicated that the child meets the following Title XXI Behavioral Health Network clinical criteria: a. The child has a DSM-IV-R Axis I clinical classification of mental disorder or substance-related disorder. b. Attention-Deficit Disorders are excluded as DSM-IV-R Axis I mental disorders in determining clinical eligibility for the Behavioral Health Network: c. The child is experiencing significant functional impairment as a result of his or her condition as demonstrated by a CGAS score of 50 or below. d. The date of the assessment and the initials of the person conducting the assessment are indicated. 4. Part II – Assessment – Request for Disenrollment. The person conducting the assessment has indicated at least one of the following: a. The parent has neglected to pay the premium; or, ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 15 - b. c. d. e. The child has turned 19 years of age; or, The child is Medicaid eligible or obtained other insurance coverage; or, The child has moved out-of-state; or, The child has been placed in residential treatment exceeding thirty days; or, f. The child is an inmate of a public institution; or, g. At re-verification, the child no longer meets the Title XXI Behavioral Health Network’s clinical or treatability eligibility criteria (completes treatment, refuses services, noncompliance, CGAS score above 50). VII. Applicant Eligibility and Ineligibility Letters: A. Applicants for the Behavioral Health Network should receive written notification that the child for whom the application was filed has been found clinically eligible or ineligible for enrollment. This notification should be consistent throughout the state and not conflict with notification requirements and letters used by KidCare. Also, confusion and enrollment delay can result if the applicant does not understand the next steps in the process. The model letters to which this procedure applies satisfy all of the necessary criteria. B. The model letters are used statewide to inform Behavioral Health Network applicants that they have been screened and assessed and found to be either clinically eligible or ineligible to enroll in the network. If eligible the letter sent to the parents will briefly describe the enrollment process remaining. The ineligibility letter will describe the reasons for the child’s ineligibility and briefly describe how the parent can enroll in other KidCare programs. No other language is to be substituted for the language used in the model letter. 1. The letter should be sent on lead agency letterhead by the Behavioral Health Liaison within five working days following the date that clinical eligibility/ineligibility is determined. 2. A copy of the dated and signed letter must be filed in the applicant’s enrollment file retained by the Liaison. 3. A copy of the letter must be forwarded by the Liaison to the attention of the member services representative in the local Children’s Medical Services Network office at the same time that the letter is sent to the applicant. VIII. Alternative Services Reporting: A. As a part of the Title XXI Behavioral Health Network benefits package, children are eligible to receive services that are not a part of the traditional state cost center/service event matrix. These services include, but are not limited to professional consultation, medication, recreation, parent assistance, home management, respite, wrap around services and other discretionary activities. B. The services allowable under this provision, and the corresponding reimbursement rates, will be reviewed by SFBHN’s BNET coordinator. 1. Alternative Services shall be approved so long as they are identified as part of the child’s individualized treatment plan. The treatment plan shall be based on strength based assessment and Alternative Services shall be used to enhance services that will enable the child to remain in the community and to meet the unique individualized needs of the child. 2. Documentation of approved Alternative Services shall include the name of the SFBHN’s Title XXI BNET Coordinator with signature and shall contain the following elements: a. Region identifier; b. Provider name; c. Provider federal Identification number (FID); d. Description of Alternative Service; ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 16 - e. Unit type; and, f. Unit cost. 3. To track the provision of Pharmaceutical and approved Alternative Services, documentation shall contain the following elements: a. County in which service was provided; b. Provider federal Identification number (FID); c. Client social security number; d. Date of services; e. Name of medication, strength, and schedule if applicable; f. Units; and , g. Unit cost. 4. The number of units for a prescribed drug depends on how the unit cost is reported. If the unit cost reported is the prescription price, the number of units would be one (1). If the unit cost reported is the price per dose, the number of units would be the number of doses in the prescription. In either case, the number of units multiplied by the unit cost should equal the total cost of the prescribed drug. 5. Once received, SFBHN’s BNET coordinator is required to forward the Alternative Services Reports to the Behavioral Health Network central office in Tallahassee. IX. Quality Assurance Monitoring: A. The Children’s Mental Health Central Office Title XXI unit is responsible for Behavioral Health Network (BNET) policy development and for liaison with Children’s Medical Services Network in accomplishing the BNET enrollment process. The unit has no direct, contractual relationship with any region lead agency provider. At the same time, as BNET is a statewide program with all regions sharing common operational requirements specified by central office, it is incumbent upon the central office Title XXI unit to review BNET operations in each region periodically and to render technical assistance where appropriate. It is a goal of the central office unit to routinely review each region at least once each fiscal year. B. The Department has established a common protocol for use throughout the state by central office staff. The reviews are intended to supplement the administrative and performance reviews conducted by region contract management staff, and to focus on those elements of program operations that are unique to BNET and/or essential to successful contractor performance. C. Preparation. 1. Notification and Scheduling. Approximately 15 workdays prior to establishing a firm review date, the SFBHN’s BNET Coordinator shall be apprised by email of an impending review visit. The email should provide an approximate date and request information on the coordinator’s availability to some extent participate in the review on the approximate date(s) in question. The coordinator should be requested to determine the availability of key agency personnel, including the behavioral health liaison, on the proposed review date(s). Details of the review schedule should be worked out among all affected parties. It is important that SFBHN’s Title XXI BNET coordinator and the Behavioral Health Liaison be present or available at specific times during the review. 2. Sample Considerations. Approximately two weeks prior to the agreed-upon review date, the central office Title XXI unit will query the BNET enrollment database to identify enrollees and enrollment/disenrollment dates in the region to be reviewed. Depending on criteria to be discussed below, a sample of approximately 10 enrollees should be selected for chart review. The department’s data system will be queried to capture a sample of the service events to be matched with chart entries to validate the accuracy of the data system reporting. The query should span the portion of the enrollment period selected for review. Multiple service ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 17 - dates subsequent to the last review conducted should be reviewed for each record. Likewise, the alternative services database should be queried to identify the alternative services provided to the selected enrollees during the period selected for review. a. If the lead agency has been the region contractor for the entire period to be sampled and reviewed, any enrollee of that region should provide usable service encounters. If the contractor is relatively new to BNET in the region, the sample will be most productive if the period reviewed is that in which the current contractor has held the contract. The focus should normally be on understanding and correcting problems with current operations. b. If the contractor has not been reporting to the data system as required, some of the sample should include records of relatively long term enrollees with few or no service events on file with data system. The focus of reviewing those charts will be to see if appropriate services have been provided, despite the lack of service event reporting. If the contractor has reported to data system as required, service dates of active records should span the enrollment period. A sample of these will demonstrate the consistency and accuracy of records keeping, as well as the maintenance of regular contact with each client. 3. Review Logistics. It should be determined beforehand whether the charts to be reviewed are in one location, can be gathered by the contractor to one location, or if the reviewer must travel to multiple locations to review charts. If the latter is the case, the review will take longer and more time may have to be scheduled for the review. Also, it should be determined whether the charts to be made available by the contractor are clinical charts or case management charts or both. It may be that the contractor is the case management entity and provides few or no direct clinical services. The provider network may be dispersed throughout the community and may provide only limited documentation to the lead agency, principally as related to billing. a. If the clinical charts are not filed in the lead agency contractor’s location, it should be determined: 1) Whether it will be possible to view the charts; and, 2) How and where that may be accomplished. The reviewer must decide on the practical feasibility of the process in the time available. b. All of the above relates to the lead time to be given the provider in pulling the charts to be reviewed. Ideally, the sample should be provided to the lead agency contractor 48 hours, excluding weekends and holidays, before the reviewer’s scheduled arrival. However, if charts must be gathered from multiple locations, more time must be allowed the contractor. D. Recording Findings. 1. Chart Review Instrument. The review sample of service events resulting from the data system query should be entered on the standardized BNET Chart Review Instrument, one client per instrument. The data system query may be exported as an Excel file, allowing cutting and pasting from the Excel file to the review instrument file, which is available in either Excel or MS Word. 2. Other Review Instruments. In addition to the chart review instrument, other standard review materials include a Lead Agency Provider Questionnaire, a BNET Review Questionnaire –Children’s Medical Services Network, and a Participants List. The Behavioral Health Liaison must be asked to identify the Children’s Medical Services Network locations and staff normally involved with BNET. The ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 18 - reviewer should make contact, either face-to-face or by telephone, with those locations and people and should complete the Children’s Medical Services Network questionnaire with them. If face to face contact is not feasible on site, the form can be completed by telephone before or during the review, or after return to central office. a. The Participants List is intended to facilitate recording the identity, affiliation and contact telephone number of everyone encountered during the review. The information is essential to creating a complete record of the review and for writing the review report. b. The Lead Agency Provider Questionnaire is intended to ensure that all pertinent information is collected from the lead agency. However, the reviewer should not be limited to only the information requested by the questionnaire. The questionnaire asks a series of questions intended to create an understanding of how the agency manages the Behavioral Health Network in its region, and also provides ready contractor background information for the reviewer. 3. Several of each type form should be taken to the review site. With the exception of the Chart Review Instrument, the other forms are set up as tables to facilitate on line data entry, i.e., the space on each line for data entry will expand until the Enter key is pressed. Unless a laptop computer containing these forms is carried on site, copies of the forms should be expanded and printed in advance to facilitate hand written entries. Following return to central office, the information collected on the forms should be converted to word processing entries for easily read attachments to the review report and a permanent electronic record. 4. Review Report to Report Findings. The review report should be completed in draft for internal review within 30 calendar days of the final date of the review and should be organized as follows: a. Table containing a summary of the district/region and contractor demographics, including all review participants. b. Standard description of the BNET program. c. Description of the district/region organization, demographics, contractor organization and BNET-related processes. d. Description of the review process actually followed. e. Review findings. 5. Recommendations a. Cover Letter. A review cover letter addressed to the region office program supervisor should be developed for the bureau chief’s signature. It should recommend that the region require a corrective action plan of the contractor for any recommendations that require action by the contractor. The review letter should also request that reports of the contractor’s corrective action (planned and actual) be copied to the bureau chief’s attention. Subsequent on-site reviews should partially focus on the accomplishment of corrective action planned or claimed in a contractor’s report of corrective action. ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 19 - Section: 2 Children’s Mental Health Children’s Crisis Response Team (CCRT) POLICY: The Children’s Crisis Response Team (CCRT) is a crisis mobile team that is attached to the Children’s Crisis Stabilization Unit. The team is comprised of a licensed psychologist, behavior analyst, individual therapist, family therapist and a case manager. When an unfunded child is referred to The Southern Region (a child that does not have insurance or ability to pay for services) for residential treatment the team is sent out to perform an assessment and determine if the child can be maintained in a nonresidential, community based setting. If nonresidential, community based services are judged to be able to adequately meet the child’s needs, the CCRT may provide an intense array of services oriented to the goal of stabilization of the child and family. The CCRT may at times provide non-Medicaid eligible services to Medicaid recipients. PURPOSE: To define the procedures necessary for eligibility determination, assessment and provision of services including stabilization by the Children’s Crisis Response Team (CCRT). PROCEDURE: I. Referral Process: A. A representative from SFBHN’S Children’s System of Care Team will e-mail a referral for CCRT assessment to the Referral and Tracking Department and copy via email the CCRT Clinical Coordinator. B. The Referral and Tracking Department will verify the eligibility for funding and status of consumer and forward this information to the CCRT Clinical Coordinator. C. The CCRT Coordinator will contact the family to schedule a community based assessment. D. The referral will be denied and SFBHN’S Children’s System of Care Team will be notified in writing if: 1. The legal guardian cannot be contacted after three failed attempts or 2. The legal guardian refuses services. II. Eligibility Criteria: A. Child or adolescent is 17 years old or less. B. Child or adolescent has been referred for residential treatment. C. Child or adolescent does not have insurance or ability to pay for services. III. Assessment Process: A. If an assessment is scheduled, the CCRT Coordinator will meet with the consumer and family to perform the assessment. This assessment shall include at a minimum, but not limited to: 1. Assessment of the child’s mental status, 2. Assessment of the family dynamics 3. Obtaining information from collateral contacts. Information may be obtained from collateral contacts which may include but are not limited to, the child’s current treatment providers, targeted case manager, juvenile probation officer and school (if available and as appropriate). 4. For active consumers, the CCRT Coordinator will complete the following: a. Authorization for Release and Exchange of Protected Health Information (complete one for SFBHN’S Children’s System of Care Team and all other relevant agencies) ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 20 - b. Consumer Registration Form (if updates are needed) c. Consumer Financial Form (if updates are needed) d. CCRT Clinical Documentation Form e. Outcome Measures Form, as applicable f. CFARS, if due g. Internal Referral Form, as applicable 5. For inactive consumers, the CCRT Coordinator will complete the following: a. Authorization for Release and Exchange of Protected Health Information (complete one for SFBHN’S Children’s System of Care Team and all other relevant agencies) b. Consumer Registration Form c. Consumer Financial Form d. CCRT Clinical Documentation Form e. Outcome Measures Form f. CFARS g. Internal Referral Form, as applicable h. Expressed and Informed Consent for Treatment i. Consumer Rights and Responsibilities j. Notice of Privacy Practices k. Medical History l. Diagnostic Interview 6. Once the disposition of the referral is determined, the information is sent to the CCRT’s Program Referral and Tracking Department for input into the data system. 7. The CCRT Clinical Coordinator will send a copy of the Diagnostic Interview report (including diagnostic impressions, treatment history and treatment recommendations) to the referring staff from SFBHN’s Children’s System of Care Department within 5 business days for crisis/emergency cases and 10 business days for all others cases after the initial assessment unless otherwise indicated. IV. V. Admission Criteria. The following criteria must be met for a child or adolescent to be admitted for treatment with the CCRT: A. The child or adolescent presents with a clinical problem that is the focus of treatment. B. The child or adolescent’s needs are judged to be adequately met with the provision of nonresidential, community based services. C. The CCRT is able to provide and/or coordinate the necessary services to stabilize the child and family. Review Provision of Services Process: Upon completion of the Assessment Process, the CCRT Coordinator will recommend one of the following: A. If the CCRT Clinical Coordinator determines the individual meets criteria for involuntary examination pursuant to F.S. Chapter 394, the Coordinator will: 1. Initiate Baker Act procedures. 2. The CCRT designated staff will follow up with the family upon the consumer’s discharge from the relevant receiving facility and will make appropriate referrals. B. If the individual does not meet the criteria for involuntary examination, is not receiving any therapeutic services, and may benefit from outpatient services, the CCRT staff will notify SFBHN’S Children’s System of Care Team of recommendations for immediate linkage to outpatient services. 1. A representative from SFBHN’S Children’s System of Care Team will facilitate referrals for follow-up services with designated mental health providers. 2. When deemed necessary and appropriate by the CCRT Coordinator, the CCRT staff will provide short term follow-up services in order to stabilize the home environment of the consumer until consumer is successfully linked to other services. ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 21 - 3. The CCRT designated staff will conduct a follow-up phone call to the family 30 days from the initial assessment to verify the implementation of recommended services. 4. If consumer was successfully linked to another provider, the case shall be closed. 5. If consumer was not successfully linked CCRT staff will provide clinical services until linkage with another agency is achieved. 6. It is the responsibility of the provider to notify the SFBHN’S Children’s System of Care Team of all updates. 7. The CCRT will conduct a follow-up phone call with the family two months from the time of the initial assessment to monitor the status of the case. Based on the status of the consumer at the 60 day follow-up phone call, one of the following recommendations will be made: a. If the consumer’s functioning has deteriorated, the CCRT will contact SFBHN’S Children’s System of Care Team to determine whether a case staffing (to include all involved parties) may be necessary. b. If the consumer’s functioning has not improved or deteriorated as compared to the original assessment, the CCRT will contact SFBHN’S Children’s System of Care Team to determine whether an additional followup meeting in 30 days or a case staffing will be necessary. 8. If the consumer’s functioning improves, the CCRT will follow-up with the family via a telephone call in 60 days. 9. If the individual does not meet the criteria for involuntary examination and is receiving therapeutic services, the CCRT will notify SFBHN’S Children’s System of Care Team of a recommendation for an increase in the intensity or frequency of therapeutic services. A representative from Children’s System of Care will facilitate referrals for increased intensity of services with designated behavioral health providers. 10. If the individual meets CCRT eligibility criteria and it is therapeutically indicated, the CCRT will provide clinically indicated intensive in-home services. 11. If the individual does not meet CCRT eligibility criteria, the CCRT will recommend an increase in therapeutic services to SFBHN’S Children’s System of Care Team Staff who will determine the appropriate community agency to provide behavioral health services. a. The CCRT will conduct a follow-up phone call to the family 14 days (two weeks) from the initial assessment to verify the implementation of recommended services. b. The CCRT will also conduct a follow-up meeting with the family 60 days from the initial assessment to monitor the status of the case. c. Based on the status of the consumer at the 60 day follow-up meeting, one of the following recommendations will be made: i. If the consumer’s functioning has deteriorated, the CCRT clinician will contact SFBHN’S Children’s System of Care Team to determine whether a case staffing (to include all involved parties) may be necessary. ii. If the consumer’s functioning has not improved or deteriorated as compared to the initial assessment, the CCRT clinician will contact SFBHN’S Children’s System of Care Team to determine whether an additional follow-up meeting in 30 days or a case staffing will be necessary. iii. If the consumer’s functioning improves, the CCRT will follow-up with the family via a telephone call in 60 days. 12. If CCRT deems a more restrictive placement may be necessary, the CCRT will recommend a residential treatment assessment for residential placement. a. The CCRT will attend a pre-admission staffing with SFBHN’S Children’s ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 22 - System of Care Team (including all involved parties) to discuss expectations of the residential program. b. The CCRT team will continue to provide support services with those consumers who meet eligibility criteria and are admitted into a residential program. c. The CCRT clinician will collaborate with the residential program treatment team on treatment goals and discharge planning. d. The CCRT may provide intensive family services beginning within 45 days of residential placement discharge. Community-based services will be provided until the family has achieved maximum benefit, at which time the CCRT will transfer the case to the appropriate community provider. As needed, for Medicaid community children referred to CCRT by SFBHN’S Children’s System of Care Team, an initial assessment will be conducted and recommendations reported to SFBHN’S Children’s System of Care Team. If the child’s parent(s) refuse the recommendation made, SFBHN’S Children’s System of Care Team will schedule a Child and Family Staffing (CFS) to include the CCRT evaluator. For dispositions that result in successful linkages to external agencies/providers, the CCRT Targeted Case Manager will complete a program discharge form. IV. Length of Stay: The provider shall involve the child and the child’s parent or guardian to the fullest extent possible at all stages of treatment planning and discharge planning toward the goal of stepping down to a lower level of care. The child’s discharge plan shall be reviewed and, if necessary, revised during each review of the treatment plan. The provider shall design individualized services and treatment for the child to address the child’s presenting problems on admission with a goal of discharge to a step-down program within 90 days of admission. V. Initial Authorization: A. An authorization number is generated if consumer meets criteria based admission criteria as identified in Section 2.III. B. The authorization will become effective only upon admission into the treatment agency. C. Authorizations generated are for a specified length of stay with a specified start and end date. D. Reimbursement will only be provided for service dates covered by the authorization. E. Initial Authorization Length of Stay: Initial authorization length of stay for children entering CCRT is 90 days. VI. Continued Stay Criteria: A. The child must continue to meet Admission Criteria as identified in Section 2. IV. B. The child or adolescent has demonstrated the ability to benefit from nonresidential, community based treatment. VII. Continued Stay Authorization: 1. For consumers who require treatment beyond the initial authorization period, the provider must complete and submit a “Continued Stay Authorization Request Form” to the CSOC Department for review and determination. 2. The request must be received by the CSOC Department no later than 30 days prior to the expiration date of the current authorization. 3. The CSOC Department will review the “‘Continued Stay Authorization Request” and notify the Provider in writing within 5 working days of decision to authorize or deny payment for continued residential treatment. 4. Should Continuation of Stay be denied, see Section 26 and 27 of UM Manual for ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 23 - denial and reconsideration protocols. C. Procedures for Continued Stay Request: The Provider must review consumer’s information and determine the primary clinical reasoning for extending services at the same level of care. The provider must submit: 1. The initial individualized treatment plan along with all revisions and updates. (This will show what goals the consumer has not achieved as well as goals for continued stay period). 2. A clearly written summary explaining the clinical justification(s) for the continued stay request. The summary should include both the consumer’s need (s) and planned staff intervention. (Include specific consumer symptoms and/or behaviors to illustrate consumer’s clinical presentation and reasons for unmet goals). 3. The summary should be typed on the Provider’s letterhead stationery and include: a. Date b. Consumer’s name and I.D. c. Clinician’s printed name and legible signature with date & credentials. d. The staff person’s name and phone number and e-mail address available for discussing the request and providing additional information as needed. 4. Requests are due 30 days prior the expiration of the previous authorization. 5. It is the responsibility of the provider to ensure that all submitted documentation has been received by the CSOC Specialist. 6. Once all required documentation has been received, the request will be processed within 5 business days. Once the request is processed, the authorization or denial will be forwarded via e-mail to the designated contact person. Reconsideration and Denial Policies can be found in Sections 26 and 27 of this UM Manual. a. CSOC Specialist may request a case staffing as needed for review of the Continued Stay Request with the CCRT. 7. Continued Stays are provided in 90-day intervals. Alternate authorization time intervals may be considered on a case by case basis. ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 24 - Section: 3 Children’s Mental Health Children’s Crisis Stabilization Unit (CCSU) POLICY: A Crisis Stabilization Unit (CSU) is a state-supported mental health service or program which functions as a short-term alternative to inpatient psychiatric hospitalization and an integrated part of a designated public receiving facility under the authority of Chapter 394, F.S. A CSU provides brief intensive services for individuals who are presented as acutely mentally ill on a 24-hour-a-day, 7-day-a-week basis, under the licensing authority of the Agency for Healthcare Administration (AHCA). The purpose of a CSU is to examine, stabilize and redirect people to the most appropriate and least restrictive treatment settings consistent with their needs. PURPOSE: To describe the eligibility, admission and criteria for provision of services in a CSU. PROCEDURE: I. CCSU Eligibility Criteria: A. Each CCSU shall develop and utilize policies and procedures pursuant to Chapter 394, F.S., for the intake, screening, admission, referral, disposition, and notification of guardians or representatives of individuals seeking treatment. There shall be adequate intake procedures to ensure that individuals being received from an emergency room, agency, facility, or other referral source shall have all the required paperwork and documentation for admission. Persons receiving services, or significant others, shall be informed of their eligibility or ineligibility status for publicly paid CCSU services, either at admission or shortly thereafter, pursuant to Chapters 65E-5 and 65E-14, F.A.C. II. Consumer Admission Criteria: A. A child meeting the requirements for voluntary admission for mental health treatment under s. 394.4625. B. An child meeting the criteria for involuntary examination for mental illness under s. 394.463. III. Program Protocol: A. The SFBHN collects monthly information on the utilization of beds and consumer recidivism rate of the Public Baker Act Receiving Facilities and CCSU’s. The information is analyzed and reported to the Department of Children and Families, SAMH Program Office and the SFBHN Adult System of Care Management Staff. B. The SFBHN reviews the monthly report for the utilization of beds from each provider. The report is based on the number of beds used daily divided by the number of beds days available. SFBHN tracks the recidivism rate. This rate is the number of re-admissions within 30 days of discharge divided by total of admissions. Information reported is to be submitted to the SFBHN’s QA/QI Department for analysis. The QI/QA Department will trend and report data to the appropriate stakeholder groups and/or committee for recommendations. C. Bed Availability: The CCSU provider will update bed availability on a daily basis and report availability to the CSOC Specialist. Provider agencies are responsible for updating the bed list for their agency on a daily basis ensuring the CSOC Specialist has updated bed availability information. ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 25 - IV. Continuation of Stay Criteria: A. The child or adolescent continues to meet the admission criteria as specified in Section 3.II.A and 3.II.B. B. The child or adolescent has demonstrated the ability to benefit from CCSU treatment. V. Authorization (Initial & Continued): A. CCSU providers are required to seek initial authorization for any consumer remaining in the CCSU past the initial 5 day stabilization period. B. An authorization number is generated if consumer meets criteria based on the documentation received that the consumer needs longer than the initial 5 days. 1. Authorizations are for a specified length of stay with a start and end date. 2. Initial authorization length for children in CCSU is 5 days after initial 5 day stabilization for a total of a possible 10 days. The CSOC Specialist may provide authorization for an alternative length if indicated, on an individual basis. 3. Should the consumer need continued C CSU services after the initial authorization period, the CCSU provider must resubmit documentation and follow authorization process as outlined in Section 3-IV.B.1-2. VI. Tracking, Review, and Corrective Action A. The SFBHN also tracks: 1. Average Length of stay 2. Total of number Admissions and Discharges 3. Number of licensed beds 4. Number of contracted beds 5. Timely access of transfer from private and public receiving facilities (as issues are identified) 6. High System Utilizers for linkage into community services a. SFBHN reviews high system utilizers amongst SOC and CQI Departments b. SOC staff coordinates for linkage of high system utilizers amongst treatment agencies including linkages into CCRT. c. SOC staff follows-up with providers for appropriate linkages including, but not limited to participation in interagency staffings and review of discharge plans B. The SFBHN reports any discrepancy or major change in the CCSU Utilization Report and immediately notifies and follows–up with the provider. The follow-up could consist of discussions of findings and/or monitoring visit. C. The SFBHN will require corrective action from the provider if discrepancies or major changes in the CCSU Utilization Report are not in compliance with applicable laws/requirements. Corrective action plans will be reviewed by the SFBHN and a plan of action will be generated. The provider will be required to resubmit their CCSU Utilization Report to achieve compliance. If approved, SFBHN will ensure the timely and accurate compliance with the approved document. ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 26 - Section: 4 Children’s Mental Health Families and Communities Empowered for Success (FACES) POLICY: Families and Communities Empowered for Success (FACES) is a collaborative effort to enhance, expand and strengthen existing community-based services in Miami-Dade County, in order to better serve youth who have serious emotional disorders (SED) and co-occurring substance abuse disorders and their families. FACES is supported by a strong system of care infrastructure and accompanying philosophical framework that will guide its day to day operation and the way in which services should be delivered to children and their families. PURPOSE: To describe the eligibility, admission and criteria for provision of services in FACES. PROCEDURE: FACES will transform and build upon the existing continuum of services by offering a comprehensive range of integrated treatment services, made possible by a cross county, cross systems interagency collaboration. The implementation of best practices coupled with “System of care” values will transform the children’s mental health system into a recovery-oriented system of care for children with serious emotional disorders and their families. Services are intended to restore the individual’s function and participation in the community. The services are designed to assist and guide individuals achieving recovering and maintaining stability within the community setting The focus is on the individual’s/family’s strengths and resources as well as their readiness and phase of recovery. A team approach for delivery of services will be used to guide and support the children and families served with development of a recovery plan focusing on the areas of individual and family living, learning, and socialization with the expectation is that therapy will be determined by the clinical needs of the child and family. I. Youth served through FACES: Two categories of youth are served through the outpatient services, with minimum number of children/youth assigned to each category. The maximum number of children/youth served at any given time by the outpatient team cannot exceed fifty (50). A. Youth served through FACES – The FACES outpatient provider must serve a minimum of fifteen (15) youth but no more than twenty (20) youth at any one time. FACES providers offer services to both the unfunded and funded population. All services provided to the unfunded youth are billed to corresponding cost centers. These include Assessment, Case Management, Outpatient, Medical and Incidental. If the services provided by an outpatient team member are a Medicaid reimbursable services and the individual served is Medicaid eligible, the services must be reported and billed to Medicaid, and it must not be reported or billed to SFBHN. The total hours billed for each team member must not exceed the hours billed to the department and the hours billed to Medicaid, and the service documentation must support all units for staff time: 1. Unfunded youth requiring mental health and or substance abuse services who are not eligible for services through FACES – The outpatient provider must serve a minimum of twenty (20) children/youth but no more than thirty (30) children/youth at any one time. II. Eligibility Criteria for Services through FACES: A. Youth aged 12-17 who are residing in Miami-Dade County. B. Youth who are identified by a full clinical assessment which includes the GAIN with cooccurring (SAMH) disorders and serious emotional diagnosis. ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 27 - C. Youth who are identified by a full clinical assessment with a mental health disorder, serious emotional diagnosis, and are using or at risk of using substances D. The full clinical assessment determines such diagnosis has existed for at least 1 year. E. The youth and the parent/guardian are willing to participate in an orientation of the national evaluation process. III. Access to Services through FACES: It is the goal of FACES to ensure youth who meet the established criteria for services have unrestricted access to the system of care. By collaborating with providers, system partners, and key stakeholders FACES will ensure that youth, regardless of their point of access, geographic location, ethnicity or primary language spoken, will have access to needed services. The following outlines most of the points of access through which services can be accessed: A. Child serving agencies/providers B. Children’s Crisis Response Team (CCRT) C. Miami-Dade Public Schools D. Department of Juvenile Justice E. Our Kids of Miami-Dade/Monroe Counties F. Residential Treatment Providers G. Crisis Stabilization Units (CSU) H. Self- referrals I. Community Partners IV. Referral Process: A. All referrals for services through FACES must be directed to the FACES contracted providers. B. A referral is initiated by completing and submitting a FACES referral and enrollment form (see Attachment ) The form must be faxed or submitted electronically to the supervisor listed on the contact list. C. Youth and families seeking services (self-referrals) through a FACES child serving agency/provider may also initiate a referral by contacting the provider directly to request services. The agency must complete a referral and enrollment form on behalf of the parent/youth and schedule the youth for a complete assessment. D. A full clinical assessment which includes the Global Assessment of Individual Need (GAIN) must be completed by the youth and within the time lines outlined in the GAIN Policy 002. E. The supervisor must schedule the youth for a GAIN assessment within two working days of receiving the referral if it appears that the youth meets criteria for services through FACES. F. The youth is eligible for services through FACES if the level of care suggested by the clinical assessment identifies any of the following levels of care or service needs: 1. Intensive Outpatient Treatment 2. Day Treatment 3. Residential Treatment (this includes Statewide Inpatient Psychiatric Program, Specialized Therapeutic Group Care, Residential Substance Abuse Treatment.) 4. Specialized Therapeutic Foster Care 5. Addiction Receiving Facility 6. Detoxification G. If the results of the agency’s full clinical assessment indicate that the youth does not meet criteria for services through FACES, the agency must work in partnership with the youth and family to either address the service needs identified by the family/youth and the assessment, or link the youth and family to services of their choice. ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 28 - V. Enrollment: A. A youth can be enrolled in FACES after the following steps have been established: 1. The youth has received a GAIN I assessment and has met the eligibility criteria for services through FACES. 2. The youth and the parent/guardian have agreed to participate in the treatment and an orientation of the national evaluation process. B. The FACES supervisor must submit an initial enrollment form to SFBHN for approval. C. Once all eligibility criteria have been met an enrollment number will be issued. D. Within 48 hours of receipt of the request for an enrollment number, SFBHN must send the enrollment number to the FACES supervisor and the evaluation team. VIII. Length of Stay: The child’s discharge plan shall be reviewed and, if necessary, revised during each review of the treatment plan. The provider shall design individualized services and treatment for the child to address the child’s presenting problems on admission with a goal of discharge to a step-down program within 60 days of admission. IX. Initial Authorization: A. An authorization number is generated if consumer meets criteria based admission criteria as identified in Section 4.II. B. The authorization will become effective only upon admission into FACES intensive outpatient. C. Authorizations generated are for a specified length of stay with a specified start and end date. D. Reimbursement will only be provided for service dates covered by the authorization. E. Initial Authorization Length of Stay: Initial authorization length of stay for children entering FACES is 60 days. X. Continued Stay Criteria: A. The child must continue to meet admission criteria as identified in Section 4.II. B. The child or adolescent has demonstrated the ability to benefit from treatment services provided through FACES. X. Continued Stay Authorization: A. For consumers who require treatment beyond the initial authorization period, the provider must complete and submit a “Continued Stay Authorization Request Form” to the CSOC Department for review and determination. B. The request must be received by the CSOC Department no later than 14 days prior to the expiration date of the current authorization. C. The CSOC Department will review the “‘Continued Stay Authorization Request” and notify the Provider in writing within 5 working days of decision to authorize or deny payment for continued residential treatment. D. Should continue Stay be denied, see Section 26 and 27 of UM Manual for denial and reconsideration protocols. E. Procedures for Continued Stay Request: The Provider must review consumer’s information and determine the primary clinical reasoning for extending services at the same level of care. The provider must submit: 1.The initial individualized treatment plan along with all revisions and updates. (This will show what goals the consumer has not achieved as well as goals for continued stay period). 2. A clearly written summary explaining the clinical justification(s) for the continued stay request. The summary should include both the consumer’s need (s) and planned staff intervention. (Include specific consumer symptoms and/or behaviors to ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 29 - illustrate consumer’s clinical presentation and reasons for unmet goals). 3. The summary should be typed on the Provider’s letterhead stationery and include: a. Date b. Consumer’s name and I.D. c. Clinician’s printed name and legible signature with date & credentials. d. The staff person’s name and phone number and e-mail address available for discussing the request and providing additional information as needed. 4. Requests are due 14 days prior the expiration of the previous authorization. 5. It is the responsibility of the provider to ensure that all submitted documentation has been received by the CSOC Specialist. 6. Once all required documentation has been received, the request will be processed within 5 business days. Once the request is processed, the authorization or denial will be forwarded via e-mail to the designated contact person. Reconsideration and Denial Policies can be found in Sections 26 and 27 of this UM Manual. e. CSOC Specialist may request a case staffing as needed for review of the Continued Stay Request with the FACES Team. 7. Continued Stays are provided in 30-day intervals. Alternate authorization time intervals may be considered on a case by case basis. XI. Evaluation Study: A. Upon completion of the enrollment process SFBHN will notify the evaluation team of the youth’s enrollment in FACES via e-mail. B. The following activities are required for every youth and family who are receiving services through a FACES provider and who are participating in the evaluation study. 1. Contact the youth and parent/guardian to acquire informed consent to participate in the evaluation study. 2. Contact the FACES provider to schedule a case record review (Enrollment and Demographic Information Form/EDIF). 3. The evaluation team will complete the EDIF within the first thirty days of the youth’s enrollment into FACES 4. Within 72 hours of completion of the Youth and Family Wraparound plan the FACES provider must notify SFBHN and the evaluator. 5. Within 30 days of the development of the Youth and Family Wraparound plan the evaluator must complete an initial interview with the youth and family. 6. After initial baseline interview, the Evaluation Team will re-contact and obtain further consent from the youth and caregiver to participate in a series of follow-up interviews. 7. Follow-up interviews will be conducted every 6 months up to a period of 24 months. The Evaluation Team will also conduct a record review at each follow-up data collection point. XII. Wraparound Flexible Funding: A. For youth enrolled in FACES wraparound, flexible dollars are available to purchase services and supports that are not currently available through any other funding mechanism. In addition, the Child and Family Team have established a clinical need for the services. The incidental cost center allows the provider the flexibility needed to purchase non funded supports and services needed by the youth in order to achieve the goals listed on the Youth and Family Plan. B. Prior to using the flexible wraparound funding the providers must exhaust all funding sources which includes, but is not limited to, community collaborations, networks and or service partnerships such as those funded by The Children’s Trust. ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 30 - C. The ability of the FACES provider to cover the cost of supports and services through this cost center is strictly based on the availability of funding. D. The Wraparound flexible funds can be used to provide the following supports and services: 1. One to One Supervision Services – A provider of one-to-one supervision services is required to have a minimum of 40 hours of training in behavioral techniques. 2. Certified Behavioral Analysis – In keeping with Florida Administrative Rule Code 65E-9, Certified Behavioral Analysis is the science in which procedures derived from the principles of behavior are systematically applied to increase skill acquisition and reduce problematic behavior, to improve socially significant behavior to a meaningful degree and to demonstrate experimentally that the procedures used were responsible for the improvement in behavior. Anyone providing these services must be certified as defined in statute and provides services outlined in 65E-9. 3. Respite Care – Any individual providing respite care is required to have a minimum of 40 hours of training in behavioral techniques. 4. Therapeutic Recreational Activities – Therapeutic Recreational Activities are any activities and or supports that assist the youth to achieve the goals on the treatment plan. An example of such activities includes but is not limited to karate, which can be used to assist the youth with impulse control, or music to help enhance selfesteem. XIII. Authorization Process for Flexible Funds: A two tier authorization process has been established to ensure the appropriate allocation of services and use of flexible funds (incidental cost center). A. Tier I - Provider level Authorization Process: 1. Each provider will internally review and manage the use of Wraparound flexible dollars up to $499.99 per youth and or family. 2. A youth and family team meeting must be held to identify the support and services needed. The Care Coordinator will ensure that services and or supports requested are not funded through any other source. 3. The Care Coordinator must submit a formal request to the Agency’s Outpatient Supervisor. The Supervisor must review and ensure that services and or supports requested are not funded through any other source prior to approval and submission of the request to the agency’s Clinical Director or the designee. 4. Upon review of the request by the Outpatient Supervisor, the agency’s Clinical Director or the designee must provide final approval prior to the purchase and implementation of the service requested. 5. The provider must consistently demonstrate that all supports and services requested and authorized were directly used to address specific needs in order to achieve the goals listed on the Youth and Family Plan. B. Tier II - SFBHN, CMH Authorization Process: South Florida Behavioral Health Network has established a two level authorization process to ensure that the clinical needs of youth requiring further supports and services being addressed. 1. Level I a. South Florida’s Behavioral Health’s level I authorization process allows the Children’s Mental Health representative working with the provider to clinically review the case and authorize from $500 through $999.99 in Wraparound Flexible funding per youth and family. b. Once the amount requested exceeds a total of $1,000 of wraparound flexible funding, the request will be elevated to the level II review and authorization process. The $1,000 limit includes the monies authorized via the provider’s ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 31 - authorization process. Should a youth and or family require supports and or services that exceed the $499.99 provider’s authorization process, the agency’s Clinical Director or the designee must submit a request (attachment A) for funding to the Children’s Mental Health representative. The following information / documentation must be submitted with Attachment A: The type of supports and/or services needed. Duration of supports and services requested. Steps taken to address the youth’s needs through alternative sources of funding. Documentation outlining the continued review and approval of the services and or supports requested by the youth and youth and family team meeting. The provider must consistently demonstrate that all supports and services requested and authorized were directly related used to address specific needs in order to achieve the goals listed on the Youth and Family Plan. 2. Level II a. The Level II authorization process will be completed by the Children’s Mental Health Supervisor for those youth and families requiring ongoing intensive supports and services. b. The goal of the level II authorization process will be to ensure that all stakeholder collaborations are in place, and that clinical resources are provided at the level required to support the youth safely in the community. c. Should a youth and family require ongoing supports and or services that exceed the SFBHN level I authorization process, the Clinical Director or the designee must submit a request (attachment A) for funding to the Children’s Mental Health Supervisor. The following information / documentation must be submitted with Attachment A: i. The type of supports and/or services needed. ii. Duration of supports and services requested. iii. Steps taken to address the youth’s needs through alternative sources of funding. iv. A history of the supports and services provided to the youth. v. Need for ongoing supports and or services. vi. Most recent Youth and Family Plan. d. Upon receipt of a request for authorization for flexible funding, the Children’s Mental Health Supervisor or their designee will submit a response to the provider with two working days. XIV. Discharge/Disenrollment/Inactive Status: A. It is the policy of FACES to ensure that youth who meet the established criteria for services continue to receive ongoing supports and services until it has been determined by the Youth and Family Team that the intensity of services and supports offered through FACES are no longer clinically required. There are two ways in which a youth can exit services. In specific instances services can be temporarily suspended. The policy outlines the guidelines for discharge, disenrollment and suspension of services. First, a youth can be discharged from FACES once the discharge criteria have been met. Second, a youth may be dis-enrolled from FACES if the youth is unable to consistently participate in services. Third, services may be suspended when a youth is unavailable for a pre-determined period of time. B. Reasons for Discharge - A youth can be discharged from FACES once the established criteria for discharge has been met and the intensity of supports and services offered through FACES is no longer required. A youth must meet all of the following discharge criteria: ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 32 - 1. The behaviors identified at the initiation of services have diminished and no longer significantly impact the youth’s daily functioning. The youth must be assessed to have CGAS of 65 or over for a minimum of sixty (60) days to be eligible for discharge. 2. The youth must be linked to appropriate services designated on the Youth and Family Plan. 3. The family is stable for more than sixty (60) days. 4. There is documented evidence of natural supports on the team and available to the youth and family. XV. Guidelines for Discharge: Prior discharge from FACES the following steps must be completed: 1. Discharge planning must be completed. Discharge planning is a continuous, begins during the first Youth and Family Team meeting and continues throughout the treatment episode. The Youth and Family Team must establish clear measureable discharge goals. These goals must be listed on the Wraparound plan. 2. Youth and Family Discharge Meeting – A discharge meeting must be held with the Youth and Family Team at least thirty (30) days prior to the youth’s discharge from FACES. The purpose of the meeting is to identify the support and services needed to maintain the youth in the community. 3. Service and Support Linkage – Following the Youth and Family meeting the Care Coordinator will link the youth to the identified supports and services identified by the Youth and Family Team. Linking a youth to services means, that the Care Coordinator will secure an appointment for the youth and family to the receiving provider(s) for the identified supports and or services. In addition, the Care Coordinator must follow up with the youth and family after the appointment with the new provider(s) to ensure that services and or supports were initiated. 4. Post Discharge Staffing – Following the discharge of the youth the FACES provider will attend the case staffing held at the receiving provider to ensure the appropriate transfer of the case and provide any additional information that may be needed to support the transition of the case. XVI. Reasons for Disenrollment: A youth maybe dis-enrolled for the following reasons: A. The youth and or family is moving out of Miami-Dade County B. The youth and family no longer wish to received services and supports through FACES C. The youth ran away and has not been available for services and or supports for at least thirty (30) days. XVII. Guidelines for Disenrollment: D. Discharge planning must begin during the first Youth and Family Team meeting and continue through the treatment episode. The Youth and Family Team must establish clear measureable discharge goals. These goals must be listed on the Wraparound plan. E. In instances where youth are present at disenrollment, a meeting must be held with the Youth and Family Team prior to the youth’s disenrollment from FACES. The purpose of the meeting is to identify the support and services needed to maintain the youth in the community. F. Service and Support Linkage – Following the Youth and Family meeting the Care Coordinator will link the youth to the identified supports and services identified by the Youth and Family Team. Linking a youth to services means, that the Care Coordinator will secure an appointment for the youth and family to the receiving provider(s) for the identified supports and or services. In addition, the Care Coordinator must follow up with the youth and family after the appointment with the new provider(s) to ensure that services ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 33 - and or supports were initiated. G. In instances when the youth are not present at the time of the disenrollment, the Care coordinator must provide the parent/guardian with the names and contact information of resources in the community that can offer the needed supports and or services to the youth. Following the disenrollment the provider shall complete and document at least two contacts with the parent/guardian to ensure that the youth and family were linked to needed services and supports. XVIII. Reasons for Suspended Services: In certain circumstance services may be suspended for a specific period of time. Services may be suspended for the following reasons: H. The youth has been hospitalized, requires extended medical treatment and is unable to participate in services. I. The youth is ordered to enter a Juvenile Justice facility for a specific period of time. J. The youth has entered a mental health or substance abuse residential treatment facility and will be discharged to FACES upon the completion of treatment. XIX. Guidelines for Suspension of Services: K. A Youth and Family meeting must be held to determine the reason for the suspension of services and the length of time that services will be suspended. L. The FACES provider shall request a suspension of service (submit attached form) at least two weeks prior to youth’s admission to the facility. M. The FACES team will maintain monthly contact with the youth and family throughout the suspension of services. N. In instances where the youth has entered a mental health or substance abuse residential treatment facility, the FACES team can work collaboratively with the residential treatment facility by continuing to provide supports and services to the family (e.g., family therapy). In these cases, the FACES provider must attend treatment team meeting held by the residential provider and work closely with the residential provider during the discharge phase. O. For youth in residential mental health or substance abuse facilities, the Care Coordinator will meet with the youth and family at least sixty (60) days prior to the youth’s discharge for the program. In addition, the Care Coordinator will attend staffings/meetings from that time forward held at the facility and ensure that the services and supports identified by the treating facility are provided upon discharge from the facility. XX. Notification of South Florida Behavioral Health: P. Within twenty-four (24) hours of discharge or disenrollment from FACES the provider must submit the discharge/disenrollment form (see attached) to SFBHN. The form can be submitted electronically to faces@sfbhn.org or faxed to 305-860-4869. Q. Upon receipt of the discharge/disenrollment form, SFBHN will complete the discharge or disenrollment form and notify the evaluation team electronically of the provider’s request. R. Upon receipt of the request for the suspension of services, SFBHN will review the request and respond to the FACES provider within forty –eight (48) hours of the receipt of the request. The evaluation team will be notified electronically of all approved suspension of services. * Changes to FACES Procedures are subject to approval by the FACES Governance Board and review by the FACES Program Subcommittee ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 34 - Section: 5 Children’s Mental Health Functional Family Therapy (FFT) POLICY: Family Functional Therapy (FFT) is a family-focused, community-based treatment for youth who are either “at risk” for, or who manifest, antisocial behavioral problems such as conduct disorder, oppositional defiant disorder, disruptive behavior disorder, violent acting-out and/or substance abuse disorders. Co-morbid behavioral or emotional problems, such as anxiety or depression, may also exist as well as family problems, such as communication and conflict issues. PURPOSE: To describe the eligibility, admission and criteria for provision of Functional Family Therapy services. PROCEDURE: FFT has been applied to a wide range of families with at-risk, pre-adolescent and adolescent youth in various multi-ethnic, multicultural contexts. Interventions are conducted at home, in school, in juvenile court, in community-based clinic or outpatient settings and at times of transition from institutional placement. FFT therapists recognize that solutions to behavioral health problems require an integration of high quality science, tested theoretical principles and extensive clinical experience to accomplish the achievement of specific functional goals for the youth and family. FFT incorporates specific intervention phases which include engagement, motivation, assessment, behavior change and generalization. Each phase includes a description of goals, requisite therapist characteristics and techniques. The intervention phases enable clinicians to maintain focus in the context of considerable family and individual disruption. The range of treatment is 3 to 30 sessions over a three month period with an average of 8 to 12 sessions. FFT is available to the community through three children’s agencies, Institute for Child and Family Health, Citrus Health Network and The Village South. Oversight and management of referrals and FFT services will be conducted by South Florida Behavioral Health Network. I. Population of Focus: A. Eligibility Criteria: Youth are eligible for Functional Family Therapy if: 1. At the time of the referral the youth is aged 10-17, 2. Residing in Miami-Dade County, 3. Has received a full clinical assessment and, 4. The family is available and has agreed to participate in all sessions. B. Admission Criteria: Evidence of behavioral symptoms consistent with a serious emotional diagnosis and the diagnosis is expected to last for at least 1 year. Specifically, the youth must exhibit at least two of the following behavioral difficulties: 1. The youth is physically aggressive at home, at school or in the community. 2. The youth is at imminent risk of out-of-home placement due to his/her behavioral problems. 3. The youth is adjudicated delinquent and or in the child welfare system. 4. The youth manifests substance abuse issues in the context of the behavioral problems. 5. The youth is transitioning from an institutional placement and his/her behavioral challenges threaten the success of the transition. 6. School truancy or suspension 7. Rule breaking and parent/child conflict ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 35 - 8. Legal issues such as prior and/or current offenses, failures to comply, probation, juvenile detention, running away. C. In general, youth receiving FFT typically exhibit symptoms associated with any of the following DSM-IV –TR diagnosis and/or categories: 1. Attention Deficit/ Hyperactivity Disorder & Disruptive Behavior Disorders 2. Co-Occurring Diagnosis (i.e., Axis I mental health and substance related disorders) 3. Posttraumatic Stress Disorder (PTSD) 4. Mood Disorders D. In instances where youth presents with a diagnosis that is not listed above, the clinical team will make a determination of the youth and family’s appropriateness for FFT services. This decision will be based on a full clinical assessment and any collateral information available to the clinical team at the time of the determination. II. Point of Access: A. The following outlines most of the points of access through which FFT services can be accessed 1. Child serving agencies/providers 2. Children’s Crisis Response Team (CCRT) 3. Miami-Dade Public Schools 4. Department of Juvenile Justice 5. Our Kids of Miami-Dade/Monroe Counties 6. Residential Treatment Providers 7. Crisis Stabilization Units (CSU) 8. Self-referrals 9. Community Partners III. Referral: A. All referrals for FFT services that are not immediately assigned to a therapist for intake must be directed to the Children System of Care (CSOC) Department at SFBHN. B. The referral must be sent to the CSOC Department at SFBHN within 2 days of determining that FFT services are currently unavailable at the agency. The referral must contain at a minimum the name of the youth in need of services, the parent(s)/guardian(s), residential address, telephone numbers(s), and if applicable, past arrest information. C. Upon receipt of the FFT referral the Children’s Specialist will add the referral information to the FFT tracking log. D. Once an opening becomes available at any of the FFT agencies, the CSOC Department at SFBHN will send a referral to the agency E. If the results of a the agency’s full clinical assessment indicates that the youth does not meet criteria for FFT, the agency must work in partnership with the youth and family to either address the service needs identified by the family/youth and the assessment, or link the youth and family to services of their choice. XI. Length of Stay: The child’s discharge plan shall be reviewed and, if necessary, revised during each review of the treatment plan. The provider shall design individualized services and treatment for the child to address the child’s presenting problems on admission with a goal of discharge to an alternate program within 120 days of admission. XII. Initial Authorization: A. An authorization number is generated if consumer meets criteria based admission criteria as identified in Section I. B. The authorization will become effective only upon admission into the treatment agency. C. Authorizations generated are for a specified length of stay with a specified start and end ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 36 - date. D. Reimbursement will only be provided for service dates covered by the authorization. E. Initial Authorization Length of Stay: Initial authorization length of stay for children entering FFT is 120 days. XIII. Continued Stay Criteria: D. The child must continue to meet Admission Criteria as identified in Section 5.I.B. E. The child or adolescent has demonstrated the ability to benefit from treatment services provided through FFT. XIII. Continued Stay Authorization: A. For consumers who require treatment beyond the initial authorization period, the provider must complete and submit a “Continued Stay Authorization Request Form” to the CSOC Department for review and determination. B. The request must be received by the CSOC Department no later than 30 days prior to the expiration date of the current authorization. C. The CSOC Department will review the “‘Continued Stay Authorization Request” and notify the Provider in writing within 5 working days of decision to authorize or deny payment for continued residential treatment. D. Should the Continued Stay be denied, see Sections 26 and 27 of UM Manual for denial and reconsideration protocols. E. Procedures for Continued Stay Request: The Provider must review consumer’s information and determine the primary clinical reasoning for extending services at the same level of care. The provider must submit: 1. The initial individualized treatment plan along with all revisions and updates. (This will show what goals the consumer has not achieved as well as goals for continued stay period). 2. A clearly written summary explaining the clinical justification(s) for the continued stay request. The summary should include both the consumer’s need (s) and planned staff intervention. (Include specific consumer symptoms and/or behaviors to illustrate consumer’s clinical presentation and reasons for unmet goals). 3. The summary should be typed on the Provider’s letterhead stationery and include: a. Date b. Consumer’s name and I.D. c. Clinician’s printed name and legible signature with date & credentials. d. The staff person’s name and phone number and e-mail address available for discussing the request and providing additional information as needed. 4. Requests are due 3- days prior the expiration of the previous authorization. 5. It is the responsibility of the provider to ensure that all submitted documentation has been received by the CSOC Specialist. 6. Once all required documentation has been received, the request will be processed within 5 business days. Once the request is processed, the authorization or denial will be forwarded via e-mail to the designated contact person. Reconsideration and Denial Policies can be found in Sections 26 and 27 of this UM Manual. a. CSOC Specialist may request a case staffing as needed for review of the Continued Stay Request with the treatment team. 7. Continued Stay authorizations are provided in 30-day intervals. Alternate authorization time intervals may be considered on a case by case basis. IV. Waitlist: A. If a wait list becomes necessary, SFBHN will maintain and manage the wait list. In order to ensure that all therapeutic slots are filled in a timely manner. Agencies are to submit monthly reports to the CSOC Department at SFBHN. The report must list the therapist, all ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 37 - active open cases, and their discharge date. At least two weeks before a youth and family is discharged from FFT, the agency must notify the CSOC Department at SFBHN in order to ensure that referrals are provided timely. ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 38 - Section: 6 Children’s Mental Health Specialized Therapeutic Group Care POLICY: Specialized Therapeutic Group Care is a Medicaid funded intensive community based psychiatric program residential treatment services designed for children and adolescents with moderate to severe emotional disturbances. Specialized Therapeutic Group Homes (STGH) must be licensed under charpter409.175, F.S. and 65 C-13 or 65 C-14, F.AC, by district, Family Safety Program Office. The program must also be licensed by AHCA, as required under Chapter 65 E 9, F.AC when promulgated. PURPOSE: To describe the eligibility, admission and criteria for provision of Specialized Therapeutic Group Care services. PROCEDURE: Specialized Therapeutic Group Care services are provided in a licensed residential group home setting serving no more than 5 children and adolescents. The children and adolescents are supervised on a 24 hour basis by trained staff that assist them in personal and social adjustment and provide for their routine daily needs. I. Referral Process: A. The referral source initiates an application for residential program. The referral sources can include: targeted case managers, community behavioral health providers (including licensed psychologists or psychiatrists, social workers), Crisis Stabilization Units. B. Applications submitted to the Children’s System of Care (SFBHN), must include a residential treatment evaluation in accordance with FL Administrative Rule 65E-9. C. Upon receipt of a complete residential treatment application, a Child and Family Staffing is conducted. Less restrictive options are explored and preferred residential treatment programs are discussed. D. The completed application is submitted to the STGH providers who review the information for clinical appropriateness. E. Once a STGH provider determines the child is clinically appropriate for admission to their program, the District Medicaid Office conducts their own review for approval of funding. F. Upon completion of clinical approval by the provider and funding approval by the District Medicaid Office, placement into program may occur. II. Program Standards: A. Admissions: Acceptance of a child for residential treatment in a residential treatment center, including a therapeutic group home, shall be based on the assessed needs of the child, family, or guardian, recommendations, and the determination that the child requires treatment of a comprehensive and intensive nature and the provider’s ability to meet those needs. Children referred by the Department and funded in full or in part by state, Medicaid, or local matching funds, shall be admitted only after they have been personally examined, assessed for suitability for residential treatment and upon recommendation by the appropriate multidisciplinary team. For children in departmental custody, the assessment must be performed by a qualified evaluator as defined in Section 39.407(6)(b), F.S., Children in parental custody must be ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 39 - assessed by a clinical psychologist or by a psychiatrist licensed to practice in the State of Florida, with experience or training in children’s disorders. For children currently in residential placement, recommendations of the facility treatment team may serve as authorization for placement in therapeutic group homes. The assessment must result in a report whose written findings support the Admission Criteria as defined in Section 6.!!.B. B. Admission Criteria: 1. The child presents with an emotional disturbance as defined in Section 394.492(5), F.S. or serious emotional disturbance as defined in Section 394.492(6), F.S. that requires treatment in a residential treatment center; 2. All available treatment that is less restrictive than residential treatment has been considered or is unavailable; 3. The treatment provided in the residential treatment center is reasonably likely to improve the child’s presenting problems as identified by the qualified evaluator; 4. The provider is qualified as determined by employing staff, program and equipment to deliver the care and treatment required by the child’s condition, age and cognitive ability; 5. The child is under the age of 18; and 6. The nature, purpose and expected length of the treatment have been explained to the child and the child’s parent or guardian and Guardian ad Litem. 7. Children in the legal custody of the Department shall be placed in accordance with Section 39.407, F.S., and the Amendment to the Rules of Juvenile Procedure, FLA. R. JUV. P. 8.350. 8. The provider may establish additional admission criteria to ensure that the program admits only children the program is capable of serving. III. Treatment planning: A. Treatment planning includes treatment and support services, goals and objectives designed to enable children being served to transition to a less restrictive level of care and/or be reunited with their family. B. Within fourteen business days after admission, a written treatment plan shall be developed with input from, interpreted and provided to, and signed and dated by: 1. child, 2. the child’s parent(s) or guardian, 3. child welfare or community based care case manager, 4. foster parents 5. Guardian ad Litem, if applicable, and 6. any other party involved in the development of the plan. C. If a child is determined to be incapable of signing the treatment plan, a written justification of the determination must be documented in the child’s record. D. Treatment modalities and services shall be in accordance with the child’s psychiatric, behavioral, emotional and social needs and be incorporated into their individualized treatment plan and discharge plan. IV. Education: The provider shall arrange for or provide an educational program for children that complies with the State Board of Education, Rule 6A-6.0361, F.A.C., effective date 2-18-93, hereby incorporated by reference. ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 40 - V. Health, medical, and emergency medical and psychiatric services: The provider shall develop and implement on an ongoing basis written procedures for health, medical, and emergency medical and psychiatric services describing how the provider obtains or provides general and specialized medical, psychiatric, nursing, pharmaceutical and dental services. VI. Length of stay: The provider shall design individualized services and treatment for the child to address the child’s presenting problems on admission with a goal of discharge to the community or to a step-down program within 120 days of admission for residential treatment centers and 365 days for therapeutic group homes. VII. Discharge Planning: A. Discharge planning shall begin at the time of admission. B. A discharge plan shall be developed, written and interpreted in collaboration with the child, parent or guardian, department, foster parents and Guardian ad Litem, if applicable, within ten days of admission, and a projected date for discharge shall be included in the child’s treatment plan. C. A copy of the discharge plan shall be given to the parent or guardian, the Guardian ad Litem, and SFBHN. D. Discharge planning may include a period of transition into the community, such as home visits and meetings with community mental health service providers. E. A summary of treatment and services which have been provided, the outcomes of treatment in relation to the child’s presenting problem on admission, and identification of needs for continuing treatment and services in the community following discharge must be part of the notification of discharge submitted to SFBHN 45 days prior to discharge. VIII. Rights of Children: The provider shall protect children’s rights under the federal and state constitutions and as specified in Sections 394.459 and 394.4615, F.S. - refer to rule 65E-9.012 IX. Staffing: A. The provider shall have an agreement with a pediatrician, family care physician, medical group or prepaid health plan to provide primary medical coverage to children in the facility. B. A registered nurse shall supervise the nursing staff during the times that the children are present in the facility and normally awake, the nursing staff to child ratio shall be no less than 1:30, and during normal sleeping hours, the nursing staff to child ratio shall be no less than 1:40. For therapeutic group homes that do not use restraint or seclusion in their program, the provider is not required to have a registered nurse or other nursing staff on duty, but shall have definitive written agreements for obtaining necessary nursing services. C. Each provider shall have on staff or under contract, at a minimum, one licensed psychologist or have definitive written agreements with an individual psychologist or psychological organization to provide such services as needed. D. At a minimum, two (2) direct care staff shall be awake and on duty at all times. E. In addition, the following direct care staff-to-child ratios shall be provided and maintained: 1. During hours when children are present in the facility and normally awake, the direct care staff to child ratio shall be no less than 1:4; and 2. During hours when the children are normally asleep, the direct care staff to child ratio shall be no less than 1:6; and ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 41 - 3. While residents are away from the facility, the staffing ratio for those residents shall be no less than 1:4. The need for more intensive staffing will be determined by the child's physician; and 4. Direct care staff shall not divide time on their shift between programs located in other areas of the facility or other buildings; and 5. While transporting residents of residential treatment centers other than group homes, the driver shall not be counted as the direct care staff providing care, assistance or supervision of the child. For therapeutic group home residents, prior to a single staff person transporting one or more children in a motor vehicle, children must be assessed to ensure the safety of the children and staff. The provider shall be able to demonstrate and provide as necessary, upon request, the ability to acquire and the past uses of the consultation services of dieticians, speech, hearing and language specialists, recreation therapists, and other specialists, when same will be or has been needed. See rule 65-E.9007 for further details NOTE: This is a general summary of the program. Refer to rule 65E-9 for details. ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 42 - Section: 7 Children’s Mental Health Statewide Inpatient Psychiatric Program (SIPP) POLICY: Statewide Inpatient Psychiatric Programs (SIPP) provides intensive therapeutic services to children with very serious emotional disturbance. Children placed in these facilities, especially in psychiatric hospitals, are generally those who require continuous medical treatment. PURPOSE: To describe the eligibility, admission and criteria for provision of services in a SIPP. PROCEDURE: These programs provide 24 hour staff supervision in a restrictive environment that limits the child’s interaction with the community. Staff is trained to provide necessary therapeutic interventions with the children, who often require one-on-one therapy and supervision. Staff also works with the child’s family to prepare for the child’s return home. Educational services are coordinated with the public school program according to the child’s Individualized Educational Plan. Residential Treatment centers are licensed under either Chapters 65M-9 or 59A-3, Florida Administrative Code. Psychiatric Hospitals are licensed under Chapter 59A-3. The following is a general summary of rule 65E-9. Refer to the Rule for full details. I. Referral Process: A. The referral source initiates an application for the residential program. The referral source can be: targeted case manager, community behavioral health provider (including licensed psychologist or psychiatrist, social worker), or Crisis Stabilization Units. B. Referrals are submitted to the Children’s System of Care (SFBHN), with a residential treatment evaluation according to Rule 65E-9. C. Upon receiving a complete residential treatment application, a Child and Family Staffing is conducted. Less restrictive options are explored and parent/legal guardian input on the preferred residential program is discussed. D. A submission of completed referral to SIPP providers takes place for review of clinical appropriateness. E. The completed referral application is submitted to the SIPP provider who reviews the information for clinical appropriateness. F. Once a SIPP provider determines the child is clinically appropriate for admission to their program, the District Medicaid Office conducts their own review for approval of funding. G. Upon completion of clinical approval by the provider and funding approval by the District Medicaid Office, placement into program may occurs. H. Refer to the Admission Section for children who are adjudicated dependent. II. Administrative Enforcement: Provider staff shall cooperate with the Agency, Department, and/or SFBHN personnel during surveys, complaint investigations, monitoring visits, implementation of correction plans, license application and renewal procedures, and other activities necessary to ensure compliance with this rule and Chapter 394, F.S. III. Program Standards: A. Physical restraints as outlined in 65E-9.013 of F.A.C.: Physical restraint may be applied only during potential emergency or crisis situations for no longer than 30 minutes. If the use of physical restraint is required during the child’s stay, the treatment team shall formally review the child’s treatment plan, at least monthly, and revise at the time of the review if determined necessary, to actively address and eliminate its use. As part of its ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 43 - B. C. D. E. F. IV. review, the treatment team will determine whether implementation of an individual behavior plan is necessary, considering such factors as the frequency and duration of the physical restraint, incidents and the age and cognitive ability of the child. Treatment and services shall be individualized, child and family centered, culturally competent, and based on the child’s assessed strengths, needs, and presenting problems that precipitated admission to the program. Activities: The facility shall have a written plan for a range of age-appropriate indoor and outdoor recreational and leisure activities provided for children, including activities for evenings and weekends. Such activities shall be based on the group and individual interests and developmental needs of the children in care. Health, medical, and emergency medical and psychiatric services: The provider shall develop and implement on an ongoing basis written procedures for health, medical, and emergency medical and psychiatric services describing how the provider obtains or provides general and specialized medical, psychiatric, nursing, pharmaceutical and dental services. Child’s record: The provider shall have written procedures regarding children’s records, including provisions to ensure that clinical records are maintained in accordance with Section 394.4615, F.S. Quality assurance program. The provider shall develop and follow a written procedure for a systematic approach to assessing, monitoring and evaluating its quality of care and treatment, improving its performance, ensuring compliance with standards, and disseminating results. Quality Assurance program: Identification of current and potential problems in service delivery and strategies for addressing the problems. This includes discharge planning (refer to the discharge planning section for more details). The program should have written measurable criteria and norms assessing, evaluating, and monitoring quality of care and treatment. Staffing: A. Psychiatrist: For residential treatment centers, the provider shall employ or contract a psychiatrist, licensed under Chapter 458 or 459, F.S., who is board certified or board eligible in child and adolescent psychiatry to serve as the medical director for the program. The medical director shall oversee the development and revision of the treatment plan and the provision of mental health services provided to children. A similarly qualified psychiatrist who consults with the medical director may provide back-up coverage. A psychiatrist shall be available and on call “24 hours-a-day”, seven “days-a-week”, and shall participate in staffings. For children committed under Section 985.19, F.S., a psychologist as defined in paragraph 65E-9.007(3)(d), F.A.C., may be used in lieu of the medical director to oversee the development and revision of the treatment plan and the provision of mental health services provided to children. B. Psychologist. Each provider shall employ or contract, at a minimum, one licensed psychologist or have definitive written agreements with an individual psychologist or psychological organization(s) to provide such services as needed. C. Direct care staff. At a minimum, two (2) direct care staff shall be awake and on duty at all times. In addition, the following direct care staff-to-child ratios shall be provided and maintained: 1. During hours when children are present in the facility and normally awake, the direct care staff to child ratio shall be no less than 1:4; and 2. During hours when the children are normally asleep, the direct care staff to child ratio shall be no less than 1:6; and 3. While residents are away from the facility, the staffing ratio for those residents shall be no less than 1:4. The need for more intensive staffing will be determined by the child's physician; 4. Direct care staff shall not divide time on their shift between programs located in ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 44 - other areas of the facility or other buildings; 5. If the provider’s program includes behavior analysis services, a certified behavior analyst, a master’s level practitioner, or professionals licensed under Chapter 490 or 491, F.S., with documented training and experience in behavior management program design and implementation shall be employed on staff or under contract, either full-or part-time, to provide ongoing staff training and quality assurance in the use of the behavior management techniques, which may include, but are not limited to those listed in sub-subparagraph 65E-9.007(5)(e)4.c., F.A.C V. Treatment services: A. Provide individualized treatment that is culturally competent; B. Provide specialized treatment that addresses child’s needs, including but not limited to, issues involving sexual or physical abuse, abandonment, domestic violence, separation, divorce, or adoption; C. Provide behavior management techniques that include, but are not limited to: preventing problem behavior, defining and teaching expectations, teaching and encouraging the child’s long-term use of new skills as alternative behaviors, contingency management, teaching and promoting choice making and self-management skills, time-out, point systems or level systems, de-escalation procedures, and crisis prevention and intervention; D. Develop and implement treatment plans; E. Provide treatment that supports the child’s permanency goals; and F. Ensure ongoing training, and be able to produce documentation of such training, on the use of restraint and seclusion, physical escort, time-out, de-escalation procedures and crisis prevention and intervention VI. Admission: A. Acceptance of a child for residential treatment in a residential treatment center, shall be based on the assessed needs of the child, family, or guardian recommendations, and the determination that the child requires treatment of a comprehensive and intensive nature and the provider’s ability to meet those needs. Children placed by the Department and funded in full or in part by state, Medicaid, or local matching funds shall be admitted only after they have on recommendation of the appropriate multidisciplinary team, been personally examined and assessed for suitability for residential treatment. For children in departmental custody, the assessment must be by a qualified evaluator as defined in Section 39.407(6)(b), F.S., Children in parental custody must be assessed by a clinical psychologist or by a psychiatrist licensed to practice in the State of Florida, with experience or training in children’s disorders. For children currently in residential placement, recommendations of the facility treatment team may serve as authorization for placement in therapeutic group homes. The assessment must result in a report whose written findings support the Admission Criteria as defined in Section 7.VI.B. B. Admission Criteria: 1. The child has an emotional disturbance as defined in Section 394.492(5), F.S., or a serious emotional disturbance as defined in Section 394.492(6), F.S.; 2. The emotional disturbance or serious emotional disturbance requires treatment in a residential treatment center; 3. All available treatment that is less restrictive than residential treatment has been considered or is unavailable; 4. The treatment provided in the residential treatment center is reasonably likely to improve the child’s presenting problems as identified by the qualified evaluator; 5. The provider is qualified by staff, program and equipment to give the care and treatment required by the child’s condition, age and cognitive ability; 6. The child is under the age of 18; and 7. The nature, purpose and expected length of the treatment have been explained to ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 45 - the child and the child’s parent or guardian and Guardian ad Litem. 8. Children in the legal custody of the department shall be placed in accordance with Section 39.407, F.S., and the Amendment to the Rules of Juvenile Procedure, FLA. R. JUV. P. 8.350. The Agency Our Kids is the primary contact for such placements. Once all legal requirements have been met, an Our Kids representative forwards the referral to SFBHN for processing and placement. 9. The provider may establish additional admission criteria to ensure that the program admits only children the program is capable of serving. VII. Admission packet: The provider shall require documentation in the child’s admission packet, including: A. The child’s parent or guardian has given expressed and informed consent to treatment; B. A funding source has been secured for the expected duration of the treatment. If the Department is the funding source, there shall be written authorization from the Department’s mental health program office that approved the funding; C. The admission packet shall request the identification of a discharge placement for the child upon their completion of treatment and the identification of a contact person who will participate in the treatment and discharge planning; D. The location of the parent or legal guardian or court ordered custodian with responsibility for medical and dental care, including consent for medical and surgical care and treatment. A statement signed by the parent or legal guardian, and a copy given to the parent or legal guardian, requiring the parent or legal guardian to notify the provider of any change in the parent’s or legal guardian’s address or telephone number. VIII. Treatment Planning: Within fourteen business days after admission a written treatment plan shall be developed with input from, interpreted and provided to, and signed and dated by: A. The child, B. The child’s parent(s) or guardian, C. The child welfare or community based care case manager, D. The foster parents, E. Guardian ad Litem, and F. If applicable, and any other party involved in the development of the plan. If a child is determined to be incapable of signing the treatment plan, a written justification of the determination must be documented in the child’s record. IX. Length of Stay: The provider shall involve the child and the child’s parent or guardian to the fullest extent possible at all stages of treatment planning and discharge planning toward the goal of reintegrating the child into the community. The child’s discharge plan shall be reviewed and, if necessary, revised during each review of the treatment plan. The provider shall design individualized services and treatment for the child to address the child’s presenting problems on admission with a goal of discharge to the community or to a step-down program within 120 days of admission. X. Initial Authorization: A. An authorization number is generated if consumer meets criteria based admission criteria as identified in Section VI.B. B. The authorization will become effective only upon admission into the treatment agency. C. Authorizations generated are for a specified length of stay with a specified start and end date. D. Reimbursement will only be provided for service dates covered by the authorization. E. Initial Authorization Length of Stay: Initial authorization length of stay for children entering SIPP is 120 days. ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 46 - XI. Continued Stay Criteria: A. The child must continue to meet admission criteria as identified in Section 7.VI and 7.VII. B. Continued Stay Authorization: 1. For consumers who require treatment beyond the initial authorization period, the provider must complete and submit a “Continued Stay Authorization Request Form” to the CSOC Department for review and determination. 2. The request must be received by the CSOC Department no later than 30 days prior to the expiration date of the current authorization. 3. The CSOC Department will review the “‘Continued Stay Authorization Request” and notify the Provider in writing within 5 working days of decision to authorize or deny payment for continued residential treatment. 4. Should continue Stay be denied, see Sections 26 and 27 of UM Manual for denial and reconsideration protocols. C. Procedures for Continued Stay Request: The Provider must review consumer’s information and determine the primary clinical reasoning for extending services at the same level of care. The provider must submit: 1. The initial individualized treatment plan along with all revisions and updates. (This will show what goals the consumer has not achieved as well as goals for continued stay period). 2. A clearly written summary explaining the clinical justification(s) for the continued stay request. The summary should include both the consumer’s need (s) and planned staff intervention. (Include specific consumer symptoms and/or behaviors to illustrate consumer’s clinical presentation and reasons for unmet goals). 3. The summary should be typed on the Provider’s letterhead stationery and include: a. Date b. Consumer’s name and I.D. c. Clinician’s printed name and legible signature with date & credentials. d. The staff person’s name and phone number and e-mail address available for discussing the request and providing additional information as needed. 4. Requests are due 30 days prior the expiration of the previous authorization. 5. It is the responsibility of the provider to ensure that all submitted documentation has been received by the UM Specialist. 6. Once all required documentation has been received, the request will be processed within 5 business days. Once the request is processed, the authorization or denial will be forwarded via e-mail to the designated contact person. Reconsideration and Denial Policies can be found in Sections 26 and 27 of this UM Manual. 7. Continued Stays are provided in 30-day intervals. Alternate authorization time intervals may be considered on a case by case basis. XII. Discharge and Discharge Planning: A. The provider shall develop and utilize a written procedure on discharge planning and aftercare services that specifies the availability of services and the persons responsible for implementation of the aftercare plan. Discharge planning shall begin at the time of admission and is an ongoing process throughout the stay. Within ten days of admission. B. A discharge plan shall be developed, written and interpreted in collaboration with the child, parent or guardian, Department, foster parents and Guardian ad Litem, if applicable. A projected date for discharge shall be included in the child’s treatment plan. C. A copy of the discharge plan shall be given to the parent or guardian, the Guardian ad Litem, and the Department. D. The provider shall finalize the discharge summary and have it approved and signed by the treatment team. At least 30 days prior to the projected discharge, a copy of the discharge summary shall be sent to SFBHN. ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 47 - E. The provider and SFBHN shall coordinate with each other to assist in the development of the discharge plan based on the provider’s recommendations for services after discharge. Linkage to recommended services, including names of providers, appointment dates and times must be provided at the Utilization Management Team Meeting prior to discharge. XIII. XIV. Rights of Children: The provider shall protect children’s rights under the federal and state constitutions and as specified in Sections 394.459 and 394.4615, F.S. Restraint, Seclusion, and Time-Out: A. Restraint or seclusion shall not result in harm or injury to the child and shall be used only: 1. To ensure the safety of the child or others during an emergency safety situation; and 2. Until the emergency safety situation has ceased and the child’s safety and the safety of others can be ensured, even if the restraint or seclusion order has not expired. B. Restraint or seclusion shall not be used for purposes of punishment, coercion, discipline, convenience, or retaliation by staff or to compensate for inadequate staffing. C. An order for restraint or seclusion shall not be issued as a standing order or on an asneeded basis. D. Restraint or seclusion shall be used in a manner that is safe and proportionate to the severity of the behavior and the child’s chronological and developmental age; size; gender; physical, medical and psychiatric condition, including current medications; and personal history, including history of physical or sexual abuse. E. Only staff who have completed a competency-based training program that prepares them to properly use restraint or seclusion shall apply these procedures to children. F. Restraint that impedes respiration (e.g., choke hold or basket hold), places weight on the child’s upper torso, neck, chest or back, or restricts blood flow to the head is prohibited. G. Ambulatory or walking restraints (e.g., shackles that bind the ankles and waist-wrist shackles) may only be used during transportation under the supervision of trained staff. The use of ambulatory or walking restraints is prohibited except for purposes of offpremise transportation. H. The provider’s medical or clinical director shall be responsible for providing oversight of ongoing monitoring, quality improvement and staff training in the use of restraint and seclusion and in the use of less intrusive, alternative interventions. I. Provider procedures. The provider’s procedures shall address the use of restraint, seclusion and time-out. A copy of the procedures shall be provided to children and their parents or guardians, foster parents and Guardian ad Litem, if applicable, upon admission, to all staff, and to the Department. The procedures shall include provisions for implementing the requirements of this section and the provider’s strategies to: 1. Reduce and strive to eliminate the need for and use of restraint and seclusion; 2. Prevent situations that might lead to the use of restraint or seclusion; 3. Use alternative, non-intrusive techniques in the prevention and management of challenging behavior; 4. Train staff on how restraint and seclusion are experienced by children and the effect they have on children with a history of trauma; and 5. Preserve the child’s safety and dignity when restraint or seclusion is used J. Authorization of restraint or seclusion: 1. Restraint or seclusion shall be used and continued only pursuant to an order by the child’s treatment team physician who should be a board certified or board eligible psychiatrist licensed under Chapters 458 or 459, F.S., or licensed physician with specialized training and experience in diagnosing and treating mental disorders. If the child’s treatment team physician is unavailable, the covering physician must also meet these qualifications. Physicians allowed to order seclusion and restraint, pursuant to this rule, must be trained in the use of ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 48 - emergency safety interventions prior to ordering them. 2. The ordering physician shall order the least restrictive intervention that is most likely to be effective in resolving the emergency safety situation. 3. If the ordering physician is not available on-site to order the use of restraint or seclusion, a verbal telephone order shall be obtained by, at a minimum, a registered nurse or other licensed staff, such as a licensed practical nurse (LPN), at the time the restraint or seclusion is initiated or immediately after it ends. At the time the order is received, the registered nurse or other licensed staff, such as an LPN, shall consult with the ordering physician about the child’s physical and psychological condition. The order and consultation shall be documented in the child’s treatment record. If an emergency exists where restraint or seclusion is needed but the physician is not present or available by telephone, a psychiatric nurse, advanced nurse practitioner, physician assistant, or registered nurse may apply the restraint or place the child in seclusion, with follow up information provided to the physician as soon as is reasonably possible. 4. The verbal order given by the physician shall be followed with their signature verifying the verbal order within seven calendar days and the signed verification shall be maintained in the child’s treatment record. 5. The ordering physician shall be available to staff for consultation, at least by telephone, throughout the period of the intervention. 6. Each order for restraint or seclusion shall: a. Be limited to no longer than the duration of the emergency safety situation; b. Not exceed two hours for children or adolescents ages nine through seventeen or one hour for children under age nine; and c. Be documented and maintained in the child’s treatment record. 7. If restraint or seclusion exceeds a total of six hours within a 24-hour period for a child age nine through seventeen or a total of three hours for a child under age nine, the treatment record should include written justification as to why the child was not transferred to a more acute program. 8. If a child requires the use of seclusion or restraint at any time during their stay, the treatment team shall formally review and actively address their use during the child's regularly scheduled treatment team review meetings, no less frequently than two times per month, until deemed no longer necessary. The reviews shall assess the frequency, patterns and trends, and identify ways to prevent the need for seclusion and restraint use. The treatment team's review of and efforts to eliminate seclusion and restraint use with a specific child shall be documented as part of the child's treatment team review. In addition, if a child is restrained a total of two times within a thirty day period, or is in seclusion a total of three times within a thirty day period, the treatment team will oversee the development and monitor the implementation of a formal child-specific plan to aggressively address the need for seclusion and restraint use with that child. 9. Within one hour of the initiation of restraint or seclusion, the ordering physician or other licensed practitioner, as permitted by the state and facility, (including a psychiatric nurse, advanced nurse practitioner, physician assistant, or registered nurse) trained in the use of emergency safety interventions, shall conduct a faceto-face assessment of the physical and psychological well-being of the child. This face-to-face assessment shall include at a minimum: a. The child’s physical and psychological status; b. The child’s current behavior; c. The appropriateness of the intervention measures; and d. Any physical or psychological complications resulting from the intervention. ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 49 - Each order for restraint or seclusion shall include: a. The ordering physician’s name; b. The date and time the order was obtained; and c. The emergency safety intervention ordered, including the length of time for which the physician authorized its use. The length of time for restraint or seclusion orders shall not exceed the time limits set forth in subsection 65E-9.013(3)(f)1.-.3, F.A.C. K. Documentation: Staff shall document the intervention in the child’s treatment record, with documentation completed by the end of each shift during which the intervention begins and continues. Documentation shall include for each order for restraint or seclusion; 1. The time the emergency safety intervention began and ended; 2. The specific circumstances of the emergency safety situation, the rationale for the type of intervention selected, the less intrusive interventions that were considered or attempted and the results of those interventions; 3. Time-specific assessments of the child’s physical and psychological condition; 4. The name, position, and credentials of all staff involved in or witnessing the emergency safety intervention; 5. Time and date of notification of the child’s parent, guardian and Guardian ad Litem; 6. The behavioral criteria and assistance provided by staff to help the child meet the criteria for discontinuation of restraint or seclusion; 7. Summary of debriefing of the child with staff; 8. Description of any injuries sustained by the child during or as a result of the restraint or emergency safety intervention and treatment received for those injuries; 9. Review and revise, if necessary, the child’s treatment plan, including a description of procedures designed to prevent the future need for and use of restraint or seclusion; and 10. Before restraint or seclusion were ordered for the child, the ordering physician assessed whether there were pre-existing medical conditions or physical disabilities, history of sexual or physical abuse, or current use of psychotropic medication that could present a risk to the child. Results of such review are documented in the order for restraint or seclusion and the child’s record. 11. Consultation with treatment team physician. If the physician ordering the use of restraint or seclusion is not the child’s treatment team physician, the staff person authorized to receive the verbal order shall: a. Consult with the child’s treatment team physician as soon as possible and inform the team physician of the emergency safety situation that required the child to be restrained or placed in seclusion; and b. Document in the child’s record the date and time the team physician was consulted. L. Notification: 1. Notification upon admission. At admission, the provider shall: a. Explain and provide a written copy of the provider’s procedures regarding the use of restraint and seclusion to the child, the child’s parent or ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 50 - guardian, and Guardian ad Litem, if applicable. The provider shall document that the child and the parent or guardian, and Guardian ad Litem were informed of the provider’s policies on the use of restraint and seclusion. This documentation shall be maintained in the child’s treatment record. b. Communicate the procedures in a language the child and the parent or guardian understand, including American Sign Language or through an interpreter or translator if needed. c. Include in the procedures contact information, including phone number and mailing address, of the Advocacy Center for Persons with Disabilities, Inc. d. Consult with the child’s parent or guardian and foster parent and Guardian ad Litem, if applicable to determine if there are any known physical or psychological risks that would rule out the use of such interventions for the child. The results of such interview shall be documented in the child’s treatment record. 2. Notification of use of restraint or seclusion. a. As soon as possible, but no later than 24 hours after the initiation of each emergency safety intervention, the provider shall notify the parent or guardian that the child has been restrained or placed in seclusion. b. The provider shall document in the child’s record that the parent or guardian was notified, including the date and time of notification and the name of the staff person providing the notification. M. Monitoring of the child during and immediately after restraint: 1. Staff trained in the use of emergency safety interventions shall be physically present and continually visually assessing and monitoring the physical and psychological well-being of the child and the safe use of restraint throughout the duration of the emergency safety intervention. 2. If the emergency safety situation continues beyond the time limit of the physician’s order for the use of restraint, the staff person authorized to receive the verbal order, as identified in paragraph 65E-9.013(4)(c), F.A.C., shall immediately contact the ordering physician to receive further instructions or new orders for the use of restraint and shall document such notification in the child’s treatment record. 3. A physician, or other licensed staff member as identified in paragraph 65E9.013(4)(i), F.A.C., trained in the use of emergency safety interventions, shall evaluate and record the child’s physical condition and psychological well-being immediately after the restraint is removed. N. Monitoring of the child during and immediately after seclusion: 1. Staff trained in the use of emergency safety interventions and in assessment of suicide risk shall be physically present in or immediately outside the seclusion room, continually visually assessing, monitoring, and evaluating the physical and psychological well-being of the child in seclusion. Video or auditory monitoring shall not be used as substitutes for this requirement. 2. If the emergency safety situation continues beyond the time limit of the physician’s order for the use of seclusion, the staff person authorized to receive the verbal order, as identified in paragraph 65E-9.013(3)(c), F.A.C., shall immediately ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 51 - contact the ordering physician to receive further instructions or new orders for the use of seclusion and such notification shall be documented and maintained in the child’s treatment record. 3. A physician or other licensed staff member, as identified in paragraph 65E9.013(3)(i), F.A.C., trained in the use of emergency safety interventions, shall evaluate the child’s physical condition and psychological well-being immediately after the child is removed from seclusion and documentation of such evaluation shall be maintained in the child’s treatment record. 4. Staff shall immediately obtain medical treatment from qualified medical personnel for a child injured during or as a result of an emergency safety intervention. 5. Discontinuation of restraint or seclusion. As early as feasible in the restraint or seclusion process, the child shall be told the rationale for restraint or seclusion and the behavior criteria necessary for its discontinuation that ensures the safety of the child and others. Restraint or seclusion shall be discontinued as soon as the child meets the behavioral criteria. O. Post-restraint or seclusion practices: 1. After the use of restraint or seclusion, staff involved in an emergency safety intervention and the child shall engage in a face-to-face discussion, or debriefing. Whenever possible, subject to staff scheduling, this discussion shall include all staff involved in the intervention. The child’s parent or guardian shall be invited to participate in the discussion. The provider shall conduct the discussion in a language that is understood by the child and the child’s parent or guardian. The discussion shall provide both the child and staff the opportunity to process the circumstances resulting in the use of restraint or seclusion and strategies to be used by the staff, the child, or others to prevent the need for the future use of restraint or seclusion. The discussion must occur within 24 hours of the emergency intervention, subject to the following exceptions: a. Allowances may be made to accommodate the schedules of the parent(s) or legal guardian(s) of the child when they request an opportunity to participate in the debriefing and when staff deem their participation appropriate. b. Allowances may be made to accommodate shift changes, vacation schedules, illnesses, and all applicable federal, state, and local labor laws and regulations. d. The emergency safety situation that required the intervention, including a discussion of the factors that caused or preceded the intervention; e. Alternative, less intrusive techniques that might have prevented the need for the restraint or seclusion; f. The procedures, if any, that staff are to implement in the future to prevent any recurrence of the use of restraint or seclusion; and 2. The outcome of the intervention, including any injuries that resulted from the use of restraint or seclusion and the treatment provided for those injuries 3. After the use of restraint or seclusion, the staff involved in the emergency safety intervention, and appropriate supervisory and administrative staff, shall conduct a debriefing session that includes a review and discussion of: a. Staff shall document in the child’s treatment record that both debriefing sessions took place and shall include in that documentation the names of staff present for the debriefing, names of staff excused from the ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 52 - debriefing, and any changes to the child’s treatment plan or facility procedures that resulted from the debriefings. b. The provider shall maintain a record of each emergency safety situation, the interventions used, and their outcomes. These records shall be maintained in a manner that allows for the collection and analysis of data for agency monitoring and provider performance improvement and shall be available for such purposes upon request. c. Staff shall document in the child’s treatment record all injuries that occur during or as a result of an emergency safety intervention, including injuries to staff resulting from that intervention. 4. Staff involved in an emergency safety intervention that results in an injury to a child or staff shall meet with supervisory staff and evaluate the circumstances that caused the injury and develop a plan to prevent future injuries. The provider shall immediately notify the child’s parent or guardian of any serious occurrence, including a child’s death, a serious injury to a child, or a suicide attempt. The provider shall also report the serious occurrence to the Department, the agency, and the state advocacy council the same day or no later than close of business the next business day for a serious occurrence that occurs after 5:00 p.m. or over a weekend. The report shall include the name of the child involved in the serious occurrence, a description of the occurrence, and the name, street address, and telephone number of the facility. P. Time-out: 1. Time-out shall be used only for the purpose of providing a child with the opportunity to regain self-control and not as a consequence or punishment. 2. When time-out is utilized, the treatment team shall consider the child’s age, maturity, health, and other factors and develop and document in the treatment plan childspecific guidelines for the use and duration of time-out. In addition, the child’s parent or guardian shall sign an informed consent form detailing the circumstances under which time-out will be used and how the procedure is to be implemented. 3. Time-out shall be initiated only by staff who have completed competency-based training in the use of time-out and such training shall be documented in their personnel record. 4. Time-out may take place either in or away from the area of activity or other children, such as in the child’s room. 5. The designated area shall be a room or area that is part of the living environment the child normally inhabits or has access to during routinely scheduled activities and from which the child is not physically prevented from leaving. 6. If the child requires physical contact in order to move to the area or room, staff shall end the contact immediately once the child is in the designated area. 7. The child shall not be physically prevented from leaving the time-out area. 8. The criteria for terminating time-out without further intervention shall be specified to the child in a neutral manner at the initiation of the time-out. 9. Time-out shall be terminated after the child meets the behavioral criterion for the specified time period, which shall not exceed 5 minutes at a time. If the child meets the criterion earlier, staff shall end the intervention immediately. 10. If the child has not been able to meet the criterion for exiting time-out within 30 minutes, staff shall notify the ranking clinician on duty or on-call, who shall assess how the procedure was implemented, assess the child’s condition, and determine whether to end the procedure, reduce the exit criterion, or continue the procedure. 11. When time-out is implemented, staff shall directly and continuously observe the child. 12. The child’s treatment team shall review the use of time-out during that child’s treatment team meetings, but no less frequently than two times per month. This review shall consist of assessing the frequency, patterns and trends, questioning the ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 53 - function(s) of the behavior(s) that resulted in the use of time-out, possible ways to prevent the behavior(s) and the appropriateness of the exit criteria used. 13. For each instance that time-out is utilized, the staff member who initiates the intervention shall document in the child’s record: a. The circumstances leading to the use of time-out; b. The specific behavior criteria explained to the child that would allow for discontinuation of time-out; c. When and how the child was informed of the behavior criteria; d. The time the procedure started and ended; and e. Any injuries sustained and treatment provided for those injuries. f. The shift; g. The staff who initiated the process; h. The time the procedure started and ended; i. The date and day of the week of each episode; j. The age and gender of the child; and k. Consumer ID. XV. Medication Administration and Psychotropic Medications: The provider shall develop, implement and maintain written policies and procedures governing the administration of medication and the supervision of and assistance with self-administered medication. These policies and procedures shall include, but not be limited to, management of the medication administration program, training, inventory control, accounting, and disposal of medications. In addition, these policies and procedures shall be consistent with the Comprehensive Drug Abuse Prevention and Control Act of 1970, 21 U.S.C.; Chapter 893, F.S., the Drug Abuse and Prevention and Control Act; DEA compliance policy guidelines on disposal of controlled substances, C.F.R. 21, Title 21, Section 1307.21, Disposal of Controlled Substances, and related department rules and regulations. ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 54 - Section: 9 Children’s Substance Abuse Juvenile Addictions Receiving Facilities (JARF) POLICY: A Juvenile Addictions Receiving Facility (JARF) is a secure, acute-care, residential facility operated 24 hours-per-day, 7 days-per-week, designated by the department to serve adolescents found to be substance abuse impaired as described in Section 397.675, F.S., and who meet the placement criteria for this component. PURPOSE: To describe the eligibility, admission and criteria for provision of services in a JARF. PROCEDURE: I. Assessment Procedures: Consumers who are determined to require JARF services, and who are eligible for Department of Children and Families (DCF) funds, are required to receive the Global Appraisal of Individual Needs – Quick (GAIN-Q) within 3 calendar days to determine level of care upon completion of JARF treatment episode. The assessment must include 5 axis diagnosis and level of care recommendation. II. III. IV. Consumer Eligibility: A. A person under 18 years of age who wishes to enter treatment for substance abuse and applies to a service provider for voluntary admission, pursuant to 397.601, F.S. B. A person under 18 years of age who meets the criteria for examination or admission under paragraph (A) or paragraph (B) and has a coexisting mental health and substance abuse disorder. Admission Criteria: A. Voluntary Criteria: There is good faith reason to believe the person is substance abuse impaired pursuant to 397.675, F.S. and, because of such impairment: 1. Has lost the power of self-control with respect to substance use; and 2. Has inflicted, or threatened or attempted to inflict, or unless admitted is likely to inflict, physical harm on himself or herself or another; or B. Involuntary Criteria: There is good faith reason to believe the person is substance abuse impaired pursuant to 397.675, F.S. and, because of such impairment: 1. Has lost the power of self-control with respect to substance use; and 2. Has inflicted, or threatened or attempted to inflict, or unless admitted is likely to inflict, physical harm on himself or herself or another; or 3. Is in need of substance abuse services and, by reason of substance abuse impairment, his or her judgment has been so impaired that the person is incapable of appreciating his or her need for such services and of making a rational decision in regard thereto; however, mere refusal to receive such services does not constitute evidence of lack of judgment with respect to his or her need for such services. Protocols All Admissions: A. Daily census and waitlist typed & e-mailed among SFBHN and JARF facilities must occur on a daily basis. B. RECORDS: JARF agencies must comply with rule 65D-30 and Section 397 F.S. for documentation standards as specified. ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 55 - V. VII. VIII. JARF Procedures –Involuntary: A. Court orders child into JARF via the Marchman Act (Section 397, F.S.) B. Court orders specifies primary JARF and/or secondary JARF provider should the primary provider be full. The court order must include both providers and their full addresses. C. JARF providers communicate availability for placement to the court. D. The child is transported to facility that has availability. E. All agencies must follow JARF protocols as identified in Section 9-III. A-B. Authorization (Initial & Continued): A. JARF providers are required to seek initial authorization for any consumer remaining in the JARF past the initial 15 day stabilization period. B. An authorization number is generated if consumer meets criteria based on the documentation received that the consumer needs longer than the initial 15 days. 1. Authorizations are for a specified length of stay with a start and end date. 2. Initial authorization length for children in JARF is 15 days after initial 15 day stabilization for a total of a possible 30 days. The CSOC Specialist may provide authorization for an alternative length if indicated, on an individual basis. 3. Should the consumer need continued JARF services after the initial authorization period, the JARF provider must resubmit documentation and follow authorization process as outlined in Section 9-VI.B.1-2. Tracking, Review, and Corrective Action A. The SFBHN also tracks: 1. Average Length of stay 2. Total of number Admissions and Discharges 3. Number of licensed beds 4. Number of contracted beds 5. High System Utilizers for linkage into community services B. The SFBHN reports any discrepancy or major change in the DETOX (JARF) Utilization Report and immediately notifies and follows–up with the provider. The follow-up could consist of discussions of findings and/or monitoring visit. C. The SFBHN will require corrective action from the provider if discrepancies or major changes in the DETOX (JARF) Utilization Report are not in compliance with applicable laws/requirements. Corrective action plans will be reviewed by the SFBHN and a plan of action will be generated. The provider will be required to resubmit their DETOX (JARF) Utilization Report to achieve compliance. If approved, SFBHN will ensure the timely and accurate compliance with the approved document. ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 56 - Section: 10 Children’s Substance Abuse Children’s Residential Substance Abuse Services POLICY: Residential Treatment is provided 24 hours-per-day, 7 days-per-week, and is intended for children and adolescents who meet the placement criteria for this component. PURPOSE: To define the procedures necessary for eligibility determination, assessment and utilization of services of the Children’s Residential Substance Abuse Services For the purposes of this manual, two levels of residential treatment are managed (Residential Levels I & II). Residential Level I: Level 1 programs provide services on a short-term basis. This level of care is appropriate for persons who have sub-acute biomedical problems or behavioral, emotional, or cognitive problems that are severe enough that they require inpatient treatment, but do not require the full resources of an acute care general hospital or a medically managed inpatient treatment program. Typically, consumers are enrolled in school, may be employed and have a home to support their recovery upon completion of this level of care. The emphasis is clearly on an intensive regimen of clinical services using a multidisciplinary team approach. Services may include some medical services based on the needs of the consumer. Level 1 programs shall provide consumers with services each week in accordance with subsection 65D30.007(3), F.A.C., including at least 14 hours of counseling per week. Residential Level II: Level 2 programs provide more intensive and comprehensive services and longer lengths of stay than Level I programs. These programs are generally referred to as therapeutic communities or some variation of therapeutic communities. This level of residential care is appropriate for persons characterized as having chaotic and often abusive interpersonal relationships, extensive juvenile justice histories, prior treatment episodes in less restrictive levels of care, inconsistent educational experiences, and anti-social behavior. In addition to clinical services, considerable emphasis is placed on services that address the consumer’s educational and vocational needs, socially dysfunctional behavior, and need for stable housing upon discharge. They also include services that assist the consumer in remaining abstinent upon returning to the community. Level 2 programs shall provide consumers with services each week in accordance with subsection 65D30.007(3), F.A.C., including at least 10 hours of counseling per week. PROCEDURE: I. Assessment Procedures: Consumers who are determined to require residential Level I or level II substance abuse treatment, and who are eligible for Department of Children and Families (DCF) funds, are required to receive the following assessments prior to placement on the circuit centralized wait list and prior to placement into a DCF funded bed: A. Screening: The Global Appraisal of Individual Needs -Quick (GAIN-Q) ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 57 - B. Admission: The Global Appraisal of Individual Needs-Initial (GAIN-I) II. Obtaining Consent: Prior to conducting the above outlined screening/assessment, provider agencies are required to obtain consent from the child, parents or guardians. The required consent form shall be provided by the Department of Children & Families (the Department) and South Florida Behavioral Health Network (SFBHN). Consent for mutual exchange of information shall be obtained to ensure coordinated quality care with the Department, SFBHN and any other entities requiring access. All entities privileged to access the assessment are identified on the consent form appendix. The consent form is available in the ‘Forms’ section of this manual. III. Completion of the GAIN: The GAIN must be fully completed. For sections in which items are identified as being a clinical concern, the clinicians conducting the assessment must utilize the comment section to provide further detail. Complete and edited GAIN Q-RRS and G-RRS must be submitted for placement onto the waitlist and/or admission into treatment. A. The GAIN-Q is valid for 90 days unless consumer has been residing in a controlled environment. If the consumer was not residing in a controlled environment and more than 90 days has lapsed since the last assessment, the consumer must be re-screened prior to placement in order to ensure appropriateness of services. B. Additional information: Assessment must also include information regarding Medicaid or other benefits, target population, and high-user status (3 or more admissions to a residential program in the past 2 years). C. For consumers in a controlled environment (e.g., jail or hospital), the length of time for which the assessment remains valid is determined on an individual basis. If upon assessment, the provider agency determines that the consumer requires a different level of care other than residential level I or level II or requires another type of treatment, (i.e.: medical, crisis, etc.) the provider agency is responsible for making the appropriate referral and linkage. IV. Criteria for Admission: An adolescent appropriately placed in to a Children’s Substance Abuse Residential Treatment Program (RTP) meets specifications in 2 of the following dimensional criteria as specified in ASAMPPC: A. Youth must be between the ages of 12-17. 1. Youth aging out of the CSA system will be authorized on a case by case basis and will be determined by the SFBHN UM Specialist. B. Dimension 1: Acute Intoxication and/or Withdrawal: The adolescent’s status is characterized by the following: 1. Adolescent is free from intoxication or withdrawal symptoms/risks; or 2. The risk of withdrawal is present, however, withdrawal is manageable. C. Dimension 2: Biomedical conditions and Complications: The adolescent’s status is characterized by 1 the following: 1. Adolescent’s continued alcohol/drug use places them in imminent danger of serious damage to their physical health or related biomedical conditions; or 2. Biomedical complications require medical monitoring or concurrent biomedical illness requires monitoring but not acute care. D. Dimension 3: Emotional, Behavioral or Cognitive Conditions and Complications; The adolescent’s status is characterized by 1 of the following: 1. Dangerousness/Lethality; Adolescent is at risk for dangerous consequences because of lack of a stable living environment. 2. Interference with Addiction Recovery Efforts: Adolescent needs a stable living environment to promote a sustained focus on recovery tasks. ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 58 - 3. Social Functioning: Adolescent’s emotional, behavioral or cognitive problem results in moderate impairment in social functioning requiring limited 24-hour supervision. 4. Ability for Self-Care: Adolescent has moderate impairment in their ability to manage their ADLs and thus needs 24-hour supervision. 5. Course of Illness: Adolescent’s history and present situation suggest that an emotional, behavioral or cognitive condition would become unstable without 24-hour supervision; or the adolescent’s emotional, behavioral or cognitive conditions suggests the need for low-intensity and/or longer term reinforcement and practice of recovery skills in a controlled environment. E. Dimension 4: Readiness to Change: The adolescent’s status is characterized by both of the following: 1. Adolescent is open to recovery but requires limited 24-hour supervision to promote or sustain progress through the stages of change; 2. Adolescent is cooperative and likely to engage in treatment at this level of care. F. Dimension 5: Relapse/Continued Use Potential: The adolescent’s status is characterized by 1 of the following: 1. Lack of monitoring and supervision between treatment encounters at a less intensive level of care has been a major barrier to abstinence of the achievement of recovery goals. Adolescent’s continued substance use poses a high risk of serious impairment in the absence of 24-hour monitoring and structured support; or 2. The adolescent’s recovery skills are not sufficient to overcome environmental triggers such as peer substance use or internal triggers such as craving; or 3. The adolescent’s history of chronic substance use, repeated relapse and/or resistance to treatment predicts continued use or relapse without residential treatment and a structure programmatic setting; or 4. The adolescent’s likelihood of relapse and/or continued use poses a high risk of serious impairment in the absence of a 24-hour monitoring and structure support. Adolescent may be at risk for relapse/continued use due to ongoing exposure to substances in the context of trafficking, gang involvement or other delinquent of drug involved peers. G. Dimension 6: Recovery Environment: The adolescent’s status is characterized by 1 of the following: 1. Adolescent’s environment is not conducive to successful treatment at less intensive levels of care; or 2. Adolescent’s parents or legal guardian(s) are unable to provide the consistent participation necessary to support treatment in a less restrictive setting; or 3. Logistical impediments (such as lack of transportation) impede participation in treatment at less intensive levels of care; or 4. There is a danger of physical, sexual, and/or severe emotional attack or victimization in the adolescents’ current living environment, which makes recovery unlikely. Thus, the consumer must be removed from that environment. V. Procedures for Residential Placement: A. Assessment: Prior to Residential Level I or II placement, all consumers receive an assessment as defined in Section 10-I-III. The consumer’s assessment information is entered into the GAIN ABS Application. Providers participating in the Substance Abuse Utilization Management (SAUM) Program utilize the GAIN ABS Application. B. Referral and Placement: Following the completion of the assessment, the provider will notify SFBHN of the referral. SFBHN will attempt to find placement for the consumer within the network of treatment facilities that provide Residential Level 1 or 2 treatment services. C. Bed Availability: 1. The provider will update bed availability and report availability to a UM Specialist ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 59 - on a daily basis. 2. If a placement is not immediately available, SFBHN will maintain contact with consumers on the waiting list. SFBHN contacts consumers in order of priority. Attempts to contact a consumer are documented by SFBHN. After 3 unsuccessful attempts, a consumer may be removed from the waitlist. 3. The SFBHN validates placements through ongoing on-site monitoring. D. Interim Services: If there are no available placements in residential treatment, the provider shall provide non-residential services to the consumer to engage the consumer until a placement becomes available. E. Wait list: The consumer is also placed on the Centralized Wait List. The screening agency shall obtain a completed Release of Information form from the consumer and guardian as described in the GAIN ABS Application updates records daily to incorporate newly added consumers to the wait list. F. Target Populations: These populations are given priority status when placing consumers in available residential beds, due to the nature and severity of their substance abuse. A consumer is designated as being part of the target population through the Assessment process. Priority Target Populations include: 1. Children involved in the Child Welfare System 2. Pregnant, Intravenous (IV) drug users 3. Other pregnant substance users 4. Other intravenous (IV) drug users 5. Involved with the juvenile justice system 6. Dually diagnosed / Consumers with co-occurring disorders VI. Initial Authorization: A. An authorization number is generated if consumer meets criteria based on the GAIN-I assessment completed by admitting agency. The authorization will become effective only upon admission into the treatment agency. B. Authorizations are for a specified length of stay with a specified start and end date. C. Reimbursement will only be provided for service dates covered by the authorization. D. The admitting agency will receive an admission 5-day authorization based on the GAIN-Q Screening. In those 5 days, the admitting agency must complete a full GAIN-I in order to receive the full authorization. E. Initial Authorization Length of Stay: Initial authorizations for adolescents are valid for 120 days upon completion of the GAIN-I. VII. Continued Stay Criteria: In addition to meeting all the criteria outlined in Section 9-IV on a continuing basis, the following criteria must also be met: A. An individualized plan of active treatment is required. This plan should contain at a minimum, clinical evidence of therapeutic goals that must be met before the adolescent can return to a previous or other living situation. B. Evidence of continued support 24 hours a day through a therapeutic living situation. C. Evidence of coordination and access to active therapeutic interventions and services directed at the alleviation of clinical symptoms that are interfering with the adolescent’s ability to return to a less intensive level of care. VIII. Procedures for Continued Stay Request: The Provider must review consumer’s information and determine the primary clinical reasoning for extending services at the same level of care. A. The provider must submit to the UM Department for review and determination: 1. A “Continued Stay Authorization Request Form” 2. The initial individualized treatment plan along with all revisions and updates. (To demonstrate what goals the consumer has not achieved as well as goals for the ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 60 - B. C. D. E. continued stay period). 3. A clearly written summary explaining the clinical justification(s) for the continued stay request. The summary should include both the consumer’s need (s) and planned staff intervention. (Include specific consumer symptoms and/or behaviors to illustrate consumer’s clinical presentation and reasons for unmet goals). The summary should be typed on the Provider’s letterhead stationery and include: a. Date b. Consumer’s name and I.D. c. Clinician’s printed name and legible signature with date & credentials. d. The staff person’s name and phone number and e-mail address available for discussing the request and providing additional information as needed. The request must be received by the UM Department no later than 30 days PRIOR to the expiration date of the current authorization. 1. Providers may request a continued stay after the 30 day interval for special circumstances (i.e. consumer relapse). These requests will be considered on an individual basis. It is the responsibility of the provider to ensure that all submitted documentation has been received by the UM Specialist. Once all of the required documentation has been received, the UM Department will review the request and notify the Provider in writing and/or email within 5 business days of the decision to authorize or deny payment for continued residential treatment. Appeal and Reconsideration Procedures can be found in Section 27 of UM Manual. Continued Stays are provided in 30-day intervals. Alternate authorization time intervals may be considered on a case by case basis. IX. High Risk/High Utilizer Consumers: A. A High-Risk/High Utilizer Consumer is defined as the following: 1. High-Risk: Consumers presenting with multiple service needs with at least one of the problem areas identified as ‘severe’. Pregnant consumers, IV drug users, and consumers with involvement in the Child Welfare System are also identified as HighRisk. 2. High-Utilizer: Consumers with three or more placements in residential Level I or level 2 treatments within a 2 year period are identified as High-Users. B. High-Risk & High-Utilizer Follow-Up: The UM Specialists will monitor High-Risk & HighUtilizer consumers. Monitoring may include clinical record review and observational participation in case staffing. Information gathered may include the following: common traits among High-Risk consumers, services provided, consumers’ responses to treatment interventions utilized, coordination between provider and Child Welfare System, when applicable, and significant areas identified on a case by case basis. Information gathered regarding High Risk and High Utilizers will be trended and analyzed through SFBHN’s QA/QI Department for treatment recommendations. X. Documentation Requirements: The following documents will be maintained by the Treatment Provider for all consumers placed in residential care and submitted to SFBHN: A. A copy GAIN-Q, GAIN-I, and/or GAIN-M90* if the forms are not in the GAIN ABS Database B. Psychiatric Evaluation or Detoxification Clearance (if necessary) C. Initial Treatment Plan D. Continued Stay Request Letter** E. Continued Stay ASAM-PPC-2-R F. The most up-to-date Treatment Plan Review** *Providers only need to submit “**” indicated documents to SFBHN if seeking continued stays or if ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 61 - the determined necessary by the program specialist. XI. Billing Validation: A. The UM Department will monitor invoices submitted by providers on a monthly basis to ensure that the billing is in congruence with the authorization period granted to each consumer for residential services. The invoice should reflect the period of time for which the consumer was authorized. B. Upon completion of the monthly review, the provider will be notified of any discrepancies and the invoice will be adjusted accordingly. ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 62 - ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 63 - Adult System of Care ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 64 - Section: 11 Adult Mental Health Crisis Stabilization Units (CSUs) POLICY: A Crisis Stabilization Unit (CSU) is a state-supported mental health service or program which functions as a short-term alternative to inpatient psychiatric hospitalization and an integrated part of a designated public receiving facility under the authority of Chapter 394, F.S. A CSU provides brief intensive services for individuals who are presented as acutely mentally ill on a 24-hour-a-day, 7-day-a-week basis, under the licensing authority of the Agency for Healthcare Administration (AHCA). The purpose of a CSU is to examine, stabilize and redirect people to the most appropriate and least restrictive treatment settings consistent with their needs. PURPOSE: To describe the eligibility, admission and criteria for provision of services in a CSU. PROCEDURE: I. CSU Eligibility Criteria: A. Each CSU shall develop and utilize policies and procedures pursuant to Chapter 394, F.S., for the intake, screening, admission, referral, disposition, and notification of guardians or representatives of individuals seeking treatment. There shall be adequate intake procedures to ensure that individuals being received from an emergency room, agency, facility, or other referral source shall have all the required paperwork and documentation for admission. Persons receiving services, or significant others, shall be informed of their eligibility or ineligibility status for publicly paid CSU services, either at admission or shortly thereafter, pursuant to Chapters 65E-5 and 65E-14, F.A.C. II. CSU Admission Criteria: A. An adult meeting the requirements for voluntary admission for mental health treatment under s. 394.4625. Per Statute: “If found to show evidence of mental illness, to be competent to provide express and informed consent, and to be suitable for treatment, such person 18 years of age or older may be admitted to the facility.” B. An adult meeting the criteria for involuntary examination for mental illness under s. 394.463. Per Statute: “A person may be taken to a receiving facility for involuntary examination if there is reason to believe that the person has a mental illness and because of his or her mental illness: (a) 1. The person has refused voluntary examination after conscientious explanation and disclosure of the purpose of the examination; or 2. The person is unable to determine for himself or herself whether examination is necessary; and (b) 1. Without care or treatment, the person is likely to suffer from neglect or refuse to care for himself or herself; such neglect or refusal poses a real and present threat of substantial harm to his or her well-being; and it is not apparent that such harm may be avoided through the help of willing family members or friends or the provision of other services; or 2. There is a substantial likelihood that without care or treatment the person will cause ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 65 - serious bodily harm to himself or herself or others in the near future, as evidenced by recent behavior.” III. Program Protocol: A. The SFBHN collects monthly information on the utilization of beds and consumer recidivism rate of the Public Baker Act Receiving Facilities and CSU’s. The information is analyzed and reported to the Department of Children and Families, SAMH Program Office and the SFBHN Adult System of Care Management Staff. B. The SFBHN reviews the monthly report for the utilization of beds from each provider. The report is based on the number of beds used daily divided by the number of beds days available. SFBHN tracks the recidivism rate. This rate is the number of re-admissions within 30 days of discharge divided by total of admissions. Information reported is to be submitted to the SFBHN’s QA/QI Department for analysis. The QI/QA Department will trend and report data to the appropriate stakeholder groups and/or committee for recommendations. C. Bed Availability: The CSU provider will update bed availability on a daily basis at agreed upon specified time such as 12:00 pm and report availability to the ASOC Specialist. Provider agencies are responsible for updating the bed list for their agency on a daily basis ensuring the ASOC Specialist has updated bed availability information. IV. Continuation of Stay Criteria: A. The consumer continues to meet the admission criteria as specified in Section 3.II.A and 3.II.B. B. The consumer has demonstrated the ability to benefit from CSU treatment. Per FS 394.4625 (Vol): “Who has sufficiently improved so that retention in the facility is no longer desirable.” V. Authorization (Initial & Continued): A. CSU providers are required to seek continued authorization for any consumer remaining in the CSU past the initial 5-day stabilization period. B. An authorization number is generated if consumer meets criteria based on the documentation received with notification that the consumer needs longer than the initial 5 days. 1. Authorizations are for a specified length of stay with a start and end date. 2. Initial authorization length for adult consumers in CSU is 5 days after initial 5 day stabilization for a total of a possible 10 days. The ASOC Specialist may provide authorization for an alternative length if indicated, on an individual basis. 3. Should the consumer need continued CSU services after the initial authorization period, the CSU provider must resubmit documentation and follow authorization process as outlined in Section 11-.V.B.1-2. VI. Tracking, Review, and Corrective Action A. The SFBHN also tracks: 1. Average Length of stay 2. Total of number Admissions and Discharges 3. Number of licensed beds 4. Number of contracted beds 5. Timely access of transfer from private and public receiving facilities (as issues are identified) 6. Management of jail/prison system access to CSU beds through Prison Aftercare program 7. High System Utilizers for linkage into community services ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 66 - a. SFBHN reviews high system utilizers amongst SOC and CQI Departments b. SOC staff coordinates for linkage of high system utilizers amongst treatment agencies including linkages to wrap around services. c. SOC staff follows-up with providers for appropriate linkages including, but not limited to participation in interagency staffings and review of discharge plans B. The SFBHN reports any discrepancy or major change in the CSU Utilization Report and immediately notifies and follows–up with the provider. The follow-up could consist of discussions of findings and/or monitoring visit. C. The SFBHN will require corrective action from the provider if discrepancies or major changes in the CSU Utilization Report are not in compliance with applicable laws/requirements. Corrective action plans will be reviewed by the SFBHN and a plan of action will be generated. The provider will be required to resubmit their CSU Utilization Report to achieve compliance. If approved, SFBHN will ensure the timely and accurate compliance with the approved document. ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 67 - Section: 12 Adult Mental Health Florida Assertive Community Treatment Team (FACT) POLICY; Florida Assertive Community Treatment (FACT) Teams provide intensive, assertive communitybased treatment that includes rehabilitation and support services for persons with psychiatric disabilities. These disabilities typically include schizophrenia, other psychotic disorders (e.g., schizoaffective disorder), mood disorders, such as bipolar disorders and major depression, personality disorders, such as borderline personality disorder, obsessive-compulsive disorder, posttraumatic stress disorder, anorexia nervosa, and dissociative identity disorders. Individuals must first meet the definition of mental illness as defined in Chapter 394, F.S., and be in one of the target groups included under the auspices of the Departmental performance measures as required by the Government Performance and Accountability Act of 1994. PURPOSE: To describe the eligibility, admission and criteria for provision of services by a FACT team as outlined in Assertive Community Treatment (ACT) Start-Up Manual published by The National Alliance on Mental Illness (NAMI). PROCEDURE: I. Admission Criteria: An applicant may be admitted to the FACT program if they meet the following criteria: A. Have repeated crisis stabilization admissions(>3 admissions within the past year) AND B. Either: 1. Demonstrate a high risk for hospital admission or readmission OR 2. Present with a history of prolonged inpatient length of stays (>90 days) AND C. The applicant must meet at least THREE of the following six characteristics: 1. Unable to consistently perform the range of Activities of Daily Living (ADLs) tasks except with significant support or assistance from others. 2. Unable to engage in regular productive activity such as employment, volunteer work, school, or homemaker responsibilities. 3. Unable to retain permanent housing due to repeated evictions or loss of housing. 4. Presents with a co-occurring Substance Abuse disorder of significant duration. 5. Exhibits destructive behavior to self or others. D. Demonstrates high risk for legal involvement or has a recent legal history E. The person has been referred to outpatient mental health services and has either failed to benefit or has been non-adherent. II. Program Thresholds: A. FACT teams must comply with the following parameters when at full capacity or while achieving full capacity: 1. At least 50% (50%) of FACT members enrolled must be directly discharged from the state hospital serving the circuit if adequate referrals by the state hospital are made to the FACT team. 2. At least 60 percent (60%) of all persons served by the FACT program shall be eligible for Medicaid. As Health Maintenance Organizations (HMOs) are capitated for Community Behavioral Health Services and Targeted Case Management, FACT teams must be aware of Medicaid procedures for enrollment and disenrollment from managed care plans. ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 68 - III. Program Protocol: A. SFBHN is the single point of contact for FACT referrals. SFBHN reviews referrals for eligibility within 24 hours of receiving the referral, and logs eligible referrals in a centralized list and assigns to the appropriate FACT team based upon availability. If a referred client does not meet criteria, SFBHN will contact the referral source within 72 hours for explanation as to reason the referral was deemed inappropriate for FACT. B. SFBHN provides technical assistance and ensures those FACT team meet their performance measure as stipulated in their contracts. C. SFBHN conducts subcontractor monitoring as specified in master contract. D. On a monthly basis SFBHN monitors the census of the FACT teams to ensure that they remain at or near capacity. When a FACT Team has the ability to accept a new referral, SFBHN staff assigns the person based on their waitlist status. A referred person may be passed over on the waiting list if: 1. The referred person requests treatment with a specific provider. In these instances SBHN staff contacts the person and informs him/her of the availability of treatment with the particular FACT provider. He/she will be again given the option of accepting treatment with the available provider. Declining will result in being passed over on the wait list. AND 2. The referred person is not a Medicaid recipient or Medicaid eligible and the team with availability cannot accept another non-Medicaid funded person.–NOTE: FACT Team censuses are required to be comprised of 60% Medicaid recipients and 40% non-Medicaid receiving consumers. E. SFBHN maintains a log of the assigned referral, date of assignment and the team that it was assigned. In the case that there is not a waitlist for FACT team services, referrals deemed appropriate for FACT will be assigned to a team within 48 hours. In the case where a wait list exist for FACT team services, SFBHN will contact referral sources and advise them that consumer must be linked to intensive interim services while they wait for FACT team services. This log is reviewed at least weekly to ensure that the teams maintain ongoing communication with SFBHN about the status of the referrals. Once a referral is assigned to a team, SFBHN monitors the engagement process to ensure that it is timely and the FACT teams employed all the recognized best practices techniques to engage the referred person into services. SFBHN requires FACT teams to continue efforts to enroll a referred person into services. If the submitted disposition for a referral is accepted by SFBHN, it is logged. If the team did not enroll the person and a vacant spot remains in the team another referral will be assigned. F. Management of referral from submission to SFBHN, including timeliness for engagement, acceptance, or denial by team. The assigned FACT team should first contact the referral source in order to gain the most updated information regarding consumer whereabouts. The assigned FACT team then has to begin the engagement process and within 30 days must report to SFBHN all contact attempts and status of engagement through submission of the disposition form. *an extension in engagement period will be reviewed on a case by case basis. G. SFBHN reviews the Quarterly Reports to identify opportunities for improvement and follow up with the provider as trends/areas are identified. H. SFBHN receives, reviews, and monitors performance through monthly reports. In addition, FACT teams are required to submit Quarterly Reports to the DCF Central Office. The Central Office compiles data from all Florida ACT teams and sends it back to the Regions. This data is used for comparison purposes and used to determine areas needing technical assistance. SFBHN provides the necessary assistance/support to the teams. Through its CQI and SOC Divisions SFBHN reviews and identifies opportunities for improvement and follow-up with FACT providers. ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 69 - Florida Assertive Community Treatment Services Flowchart Referral submitted to our office Referral reviewed for completeness and appropriateness by Adult System of Care Specialist (ASOCS) – within 24 hrs If completed and appropriate If inappropriate and/or incomplete Person is placed in waiting list by ASOCS Referral source is informed of the disposition by ASOCS – within 72 hrs FACT Teams submits completed disposition – within 30 days of assignment Person is assigned to FACT Team by ASOCS with 72 hrs (if waitlist does not exist) Disposition is reviewed by AMHS FACT Team beings (continue) engagement – within 72 hours of receipt of assigned referral Person is not enrolled in FACT Person is enrolled in FACT FACT Teams submits completed disposition within 30 days of assignment Disposition is logged by ASOCS Disposition accepted as submitted Disposition is logged by ASOCS Disposition not accepted FACT Team informed by ASOCS that further action is required ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 70 - Section: 13 Adult Mental Health State Treatment Facilities POLICY: State Treatment Facilities include any state-owned, state-operated, or state-supported hospital, center, or clinic designated by the Department of Children and Families for extended treatment and hospitalization, beyond that provided for by a receiving facility, of persons who have a mental illness and need mental health treatment and services in a highly structured, in-patient residential setting. All admissions to civil state treatment facilities are governed under Chapter 394, Florida Statutes. PURPOSE: To describe the SFBHN management functions related to state treatment facilities. PROCEDURE: Geo Care, Inc., through a Management Agreement with the Department of Children and Families, operates South Florida State Hospital, a State Mental Health Treatment Facility serving individuals from Circuits Seven, Eleven, Twelve, Thirteen, Fifteen, Sixteen, Seventeen, Eighteen, Nineteen and Twenty. I. Admissions to State Treatment Facilities: A. Receiving facilities must obtain approval from the state treatment facility prior to the transfer of a person. A state treatment facility shall be permitted to accept persons for transfer from a receiving facility if the administrator of the receiving facility has provided the following documentation, which documentation shall be retained in the person’s clinical record: 1. Recommended form CF-MH 7000, Jan. 98, “State Mental Health Facility Admission Form,” with all required attachments, which is hereby incorporated by reference and may be obtained pursuant to Rule 65E-5.120, F.A.C., of this rule chapter; 2. Recommended forms CF-MH 3040, Feb. 05, “Application for Voluntary Admission,” which is incorporated by reference and may be obtained pursuant to Rule 65E-5.120, F.A.C., of this rule chapter, or CF-MH 3008, Feb. 05, “Order for Involuntary Inpatient Placement,” which is incorporated by reference and may be obtained pursuant to Rule 65E-5.120, F.A.C., of this rule chapter; and 3. Mandatory form CF-MH 3089, “Transfer Evaluation” as referenced in subsection 65E-5.1301(1), F.A.C. B. Use of recommended form CF-MH 7002, Feb. 05, “Physician to Physician Transfer,” which is incorporated by reference and may be obtained pursuant to Rule 65E-5.120, F.A.C., of this rule chapter may be used for documentation when completed by the referring physician or in the absence of the referring physician the physician’s designee within state law and approved facility protocols and practice guidelines, at the time of transfer. The form shall accompany the person to the state treatment facility and upon arrival shall be presented to admitting staff. C. If a person awaiting transfer to a state treatment facility improves to the degree that he or she no longer meets the criteria for involuntary placement or that such transfer is unnecessary, the receiving facility shall discharge the person as specified in Section 394.469, F.S. II. SFBHN coordinates with the state mental health treatment facilities (civil and forensic), regarding the utilization of said facilities, which includes at a minimum, working together to address the admission process, on-going communication during treatment, and the discharge/aftercare process regarding: ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 71 - A. Annual bed utilization reduction as a percentage of total beds in the applicable state mental health treatment facilities (civil and forensic); and B. Annual reduction of average length of stay as the average number of days in the applicable state mental health treatment facilities (civil and forensic). III. SFBHN Management of the CIVIL state treatment facilities include: A. Coordinates and analyzes the tracking and provision of monthly reports on admissions, discharges and unmet needs for persons served B. Oversees Circuit reports on individuals in receiving facilities who are awaiting admission into State Treatment Facilities C. Attends the Quarterly Utilization Review and Stakeholders meetings D. Coordinates and facilitates monthly discharge tracking meetings E. Assists Liaisons/Case Management with difficult placements F. Acts as the liaison for all community relate issues G. Responsible for coordinating Circuit transfers H. Assist in the implementation of the Continuity of Care Guidelines as agreed upon by the Department and the state treatment facilities. I. Manages the efficiencies of network providers for discharging civil and forensic consumers from state hospital within 30 days of being placed on the seeking placement list J. Oversees individuals ready to be discharged from state hospital including utilization of incidental funds for individuals. ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 72 - Section: 14 Adult Mental Health Incidental Expenses POLICY: This cost center provides for incidental expenses, such as clothing, medical care, educational needs, developmental services, FACT Team housing subsidies and pharmaceuticals, and other approved costs. All incidental expenses must have prior written authorization by the department’s authorized staff member or be authorized in the contract. PURPOSE: To describe the process for accessing incidental expenses and the SFBHN management of those funds. PROCEDURE: I. Contract Requirements: A. The network provider agrees to use incidental funds allocated under their contract for housing, medication and other emergency expenses for indigent clients. B. The network provider must maintain in the consumers’ file a record of all consumer expenses charged against the funds. C. The network provider keeps a record to log all incidental funds expenditures as specified in contract. D. The ME reserves the right to reduce the contract amount by the incidental funds projected surplus. II. System Management A. SFBHN monitors the use of incidental expenses through monthly lapse reports generated by the fiscal department. B. Surplus and lapses are reported to providers on an ongoing basis to ensure proper utilization of funds. C. SFBHN provides technical assistance ensure compliance with contract requirements and proper use of incidental funds. ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 73 - Section: 15 Adult Mental Health Short-term Residential Treatment (SRT) Program - Civil POLICY: A Short-term Residential Treatment (SRT) Program is a state-supported acute care 24-hour-aday, 7-day-a-week residential alternative service, typically with lengths of stay of 90 days or less, and which is an integrated part of a designated public receiving facility and receiving state mental health funds under the authority of Chapter 394, F.S. The purpose of an SRT is to provide intensive short-term treatment to individuals who are temporarily in need of a 24-hour-a-day structured therapeutic setting in a less restrictive, but longer-stay alternative to hospitalization. PURPOSE: To describe admission criteria and the SFBHN management functions related to SRT. PROCEDURE: I. Admission Criteria: Admission to an SRT requires the individual meet the following criteria: A. Person be at least 18 years old and diagnosed with a severe and persistent mental illness, with or without co-occurring disorders B. Person is at risk of institutionalization or incarceration for mental health reasons C. All individuals shall be admitted pursuant to Chapter 394 (voluntary or involuntary), Part I, F.S., and Chapter 65E-5, F.A.C., and only on the order of a physician. D. Individuals must present as acutely mentally ill and in need of intensive staff supervision, support and assistance, as documented in a psychiatric or psychological evaluation. E. Individuals must be continent, ambulatory or capable of self-transfer. II. Exclusion Criteria: A. Individuals presenting with major medical conditions requiring ongoing 24 hours per day, 7 day per week nursing services as determined by the Southern Region's Medical Exclusionary Guidelines for Crisis Stabilization Units and Stand Alone Receiving Facilities for CSU 2009. B. Individuals presenting with physically aggressive, suicidal, or homicidal behavior (past history will be evaluated on a case by case basis). III. Admission Requirements: A. The individual receives a psychiatric or psychological evaluation, and B. The individual is referred from a CSU, inpatient psychiatric unit (including county jail psychiatric units. IV. System Management: A. SFBHN is the single point of contact for SRT Program referrals. B. SFBHN reviews referrals for eligibility; logs eligible referrals in a centralized list and forwards to the program for screening within 24 hours having received the referral. C. SFBHN coordinates the screening of the referred person within three (3) days of the program having received the referral. D. SFBHN actively participates with the program in the approval of a referral. E. For approved referrals, SFBHN assigns an authorization number for 90 days of treatment. V. Bed Availability: ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 74 - A. The provider will update bed availability on a daily basis and report availability to the ASOC Specialist. B. If a placement is not immediately available, the SFBHN will immediately inform the referral source that individuals will be placed on a waiting list. VI. Continued Stay Criteria: In addition to meeting all the criteria outlines in Section 15-I on a continuing basis, the following criteria must also be met: A. An individualized plan of active treatment is required. This plan should contain at a minimum, clinical evidence of therapeutic goals that must be met before the consumer can return to a less restrictive level of care. B. Evidence of continued need for acute and post-acute treatment 24 hours a day as defined in 65E-12, F.A.C C. Evidence of coordination and access to active therapeutic interventions and services directed at the alleviation of clinical symptoms that are interfering with the consumer’s ability to return to a less restrictive level of care. VII. Procedures for Continued Stay Request: A. The provider must review consumer’s information and determine the primary clinical reasoning for extending services at the same level of care B. The provider must submit to the ASOC Department for review and determination: 1. Adult Mental Health ‘Continued Stay Authorization Request Form” containing the following: a. Consumer’s name and information. b. Date of request. c. Date current authorization expires on. d. The staff person’s name and phone number and e-mail address available for discussing the request and providing additional information as needed. e. Clearly written summary explaining the consumer’s presenting problem(s), Diagnosis, progress in treatment, barriers to progress and justification for continued stay. (Include specific consumer symptoms and/or behaviors to illustrate consumer’s clinical presentation and reasons for unmet goals). f. Clinician’s printed name and legible signature with date and credentials. C. The initial individualized treatment plan along with all revisions and updates. (This will demonstrate which goals the consumer has not achieved as well as goals for the continued stay period). D. Requests are due 30 days prior to the expiration of the previous authorization. E. It is the responsibility of the provider to ensure that all submitted documentation has been received by the ASOC Specialist. Once all required documentation has been received, the request will be processed within 5 business days of the decision to authorize or deny continued stay. D. Continued Stays are provided in 30-day intervals. Alternate authorization time intervals may be considered on an individual basis. E. Appeal and Denial Policies can be found in Sections 26 and 27 of this UM Manual. ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 75 - Section: 16 Adult Mental Health Short-term Residential Treatment (SRT) Forensic Program POLICY: A Short-term Residential Treatment (SRT) Program is a state-supported acute care 24-hour-aday, 7-day-a-week residential alternative service, typically with lengths of stay of 90 days* or less, and which is an integrated part of a designated public receiving facility and receiving state mental health funds under the authority of Chapter 394, F.S. The purpose of a Forensic SRT is to provide intensive short-term treatment, competency restoration and rehabilitative skills to individuals who are temporarily in need of a 24-hour-a-day structured therapeutic setting in less restrictive environment than a state forensic hospital. PURPOSE: To describe admission criteria and the SFBHN management functions related to SRT. PROCEDURE: I. Admission Criteria: A. Individuals must be at least 18 years of age B. Individuals shall be charged with a felony in any of the state’s twenty Circuit Courts C. Individuals shall be free of any major medical conditions or shall have stable medical conditions as determined by the Southern Region's Medical Exclusionary Guidelines for Crisis Stabilization Units and Stand Alone Receiving Facilities for CSU 2009. D. Individuals must be continent, ambulatory or capable of self-transfer E. Individuals display with physically aggressive, suicidal, or homicidal behavior (past history will be evaluated on a case by case basis) F. Individuals must present as acutely mentally ill and in need of intensive staff supervision, support and assistance, as documented in a psychiatric or psychological evaluation G. All individuals shall be admitted pursuant to Chapter 916, F.S. (voluntary or involuntary), Part I, F.S., and Chapter 65E-5, F.A.C., and 1. Have received at least two psychiatric or psychological evaluations finding that the individual has a mental illness as defined by Chapter 916.106 (13), F.S. and with: a. That at least two independent evaluators opine that the person is unable to proceed at any material state of a criminal proceeding and b. That with treatment there is a probability that the defendant will attain competence to proceed in the foreseeable future. 2. Or found not guilty by reason of insanity and a. Has been refer from a CSU, inpatient psychiatric unit (including county jail psychiatric units in Dade and Monroe), or a designated public or private receiving facility. II. System Management: A. The Forensic Team is the single point of contact for Forensic SRT Program referrals. B. The Forensic Team in conjunction with SFBHN reviews referrals for eligibility, logs eligible referrals in a centralized list, and screens the person within 72 hours of having received the referral. C. The Forensic team and SFBHN actively participate with the program in the approval of a referral. 1. For approved referrals, The Forensic Team assigns an authorization number for 120 days of treatment. ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 76 - D. For approved referrals, SFBHN monitors and coordinates the admission of the person into the program. E. SFBHN provides ongoing monitoring of the program to ensure compliance with length of stay (LOS), discharge procedures and staffing of difficult individuals admitted to the program. F. SFBHN provides program technical assistance ensure compliance with contract requirements and applicable laws and regulations. G. SFBHN provides technical assistance and coordination with other community providers to ensure that individuals being discharged from the Forensic SRT have access to less restrictive residential levels of care. H. SFBHN acts a liaison to the program and assist in the elimination of barriers to discharge for individuals served in the program. III. Length of Stay: A. Forensic SRT aims to transition individuals in 120 days or less. However, length of stay is contingent upon communication and approval from the courts. IV. Bed Availability: A. The provider will update bed availability on a daily basis and report availability to the Forensic Team. B. If a placement is not immediately available, the Forensic Team will immediately inform the referral source that individuals will be placed on a waiting list. V. Continued Stay Criteria: In addition to meeting all the criteria outlined in Section 16-I on a continuing basis, the following criteria must also be met: A. An individualized plan of active treatment is required. This plan should contain at a minimum, clinical evidence of therapeutic goals that must be met before the consumer can return to a less restrictive level of care. B. Evidence of continued need for acute and post-acute treatment 24 hours a day as defined in 65E-12, F.A.C. C. Evidence of coordination and access to active therapeutic interventions and services directed at the alleviation of clinical symptoms that are interfering with the consumer’s ability to return to a less restrictive level of care. VI. Procedures for Continued Stay Request: A. The provider must review consumer’s information and determine the primary clinical reasoning for extending services at the same level of care B. The provider must submit to the Forensic Team for review and determination: 1. Adult Mental Health ‘Continued Stay Authorization Request Form” containing the following: a. Consumer’s name and information. b. Date of request. c. Date current authorization expires on. d. The staff person’s name and phone number and e-mail address available for discussing the request and providing additional information as needed. e. Clearly written summary explaining the consumer’s presenting problem(s), Diagnosis, progress in treatment, barriers to progress and justification for continued stay. (Include specific consumer symptoms and/or behaviors to illustrate consumer’s clinical presentation and reasons for unmet goals). f. Clinician’s printed name and legible signature with date and credentials. C. The initial individualized treatment plan along with all revisions and updates. (This will demonstrate which goals the consumer has not achieved as well as goals for the ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 77 - continued stay period). D. Requests are due 30 days prior to the expiration of the previous authorization. E. It is the responsibility of the provider to ensure that all submitted documentation has been received by the Forensic Team. Once all required documentation has been received, the request will be processed within 5 business days of the decision to authorize or deny continued stay. F. Continued Stay authorizations are provided in 30-day intervals. Alternate authorization time intervals may be considered on an individual basis. G. Appeal and Denial Policies can be found in Sections 26 and 27 of this UM Manual. ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 78 - Section: 17 Adult Mental Health Short-term Residential Treatment (SRT) Miami-Dade Forensic Alternative Center (MD FAC) POLICY: A Short-term Residential Treatment (SRT) Program is a state-supported acute care 24-hour-aday, 7-day-a-week residential alternative service, typically with lengths of stay of 90 days or less, and which is an integrated part of a designated public receiving facility and receiving state mental health funds under the authority of Chapter 394, F.S. The purpose of the MD FAC is to provide intensive short-term treatment, rehabilitation and competency restoration to individuals who are temporarily in need of a 24hour-a-day structured therapeutic setting in a less restrictive setting alternative to hospitalization and to facilitate community reintegration and follow-up services. PURPOSE: To describe admission criteria and the SFBHN management functions related to MD FAC. PROCEDURE: I. Admission Criteria: A. Individuals must be at least 18 years of age, B. Individuals shall be charged with a felony in 11th Judicial Circuit Court C. Individuals shall be free of any major medical conditions or shall have stable medical conditions as determined by the Southern Region's Medical Exclusionary Guidelines for Crisis Stabilization Units and Stand Alone Receiving Facilities for CSU 2009 D. Individuals must be continent, ambulatory or capable of self-transfer E. Individuals must present as acutely mentally ill and in need of intensive staff supervision, support and assistance, as documented in a psychiatric or psychological evaluation. 1. All individuals shall be admitted pursuant to Chapter 916, F.S. II. Exclusion Criteria: A. The program shall not admit an individual who is incompetent to proceed, or has previously been convicted of, found incompetent to proceed on, or found not guilty by reason of insanity of one of the following criminal offenses: 1. Homicide of any kind 2. Domestic battery by strangulation, as defined in section 784.041, F.S. 3. Kidnapping 4. Sexual battery of any kind, except as provided in section 794.05, F.S. 5. Lewd or lascivious battery 6. Lewd or lascivious molestation 7. Arson or any offense related to fire bombs or explosive devices 8. Home invasion robbery 9. Aggravated child abuse 10. Aggravated abuse of an elderly person or disable adult 11. Aggravated stalking III. System Management: A. The Mental Health Administrative Office of the Courts (MHAOC) makes the referral to the Forensic Team B. The Forensic Team reviews the referral packet for admission criteria and forwards on to ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 79 - MD FAC for their review C. MD FAC staff screens the referred person and submit written disposition to the MHAOC. D. The presiding judge is informed of the person’s eligibility for the program E. The 11th Judicial Circuit courts commitments the individual to the Department of Children and Families F. The 11th Judicial Circuit court orders the Department of Corrections to transport the person to MDFAC G. The Forensic Team is the single point of contact for SRT-MDFAC Program referrals H. The Forensic Team and SFBHN actively participates in the approval of a referral with the input of the treatment team I. For approved referrals, SFBHN monitors and coordinates the admission of the person into the program J. SFBHN provides ongoing monitoring of the program to ensure compliance with length of stay (LOS), discharge procedures and staffing of difficult individuals admitted to the program K. SFBHN provides program technical assistance to ensure compliance with contract requirements and applicable laws and regulations. L. SFBHN provides technical assistance and coordination with other community providers to ensure that individuals being discharged from the MD FAC have access to less restrictive residential levels of care. M. SFBHN acts a liaison to the program and assists in the elimination of barriers to discharge for individuals served in the program. IV. Length of Stay: A. MD FAC aims to transition individuals in 90 days or less. However, length of stay is contingent upon communication and approval from the courts. VII. Bed Availability: A. The provider will update bed availability on a daily basis and report availability to the Forensic Team. B. If a placement is not immediately available, the Forensic Team will immediately inform the referral source that individuals will be placed on a waiting list. VIII. Continued Stay Criteria: In addition to meeting all the criteria outlined in Section 17.I on a continuing basis, the following criteria must also be met: A. An individualized plan of active treatment is required. This plan should contain at a minimum, clinical evidence of therapeutic goals that must be met before the consumer can return to a less restrictive level of care. B. Evidence of continued need for acute and post-acute treatment 24 hours a day as defined in 65E-12, F.A.C. C. Evidence of coordination and access to active therapeutic interventions and services directed at the alleviation of clinical symptoms that are interfering with the consumer’s ability to return to a less restrictive level of care. IX. Procedures for Continued Stay Request: A. The provider must review consumer’s information and determine the primary clinical reasoning for extending services at the same level of care B. The provider must submit to the Forensic Team for review and determination: 1. Adult Mental Health ‘Continued Stay Authorization Request Form” containing the following: a. Consumer’s name and information. b. Date of request. c. Date current authorization expires on. ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 80 - C. D. E. F. G. d. The staff person’s name and phone number and e-mail address available for discussing the request and providing additional information as needed. e. Clearly written summary explaining the consumer’s presenting problem(s), Diagnosis, progress in treatment, barriers to progress and justification for continued stay. (Include specific consumer symptoms and/or behaviors to illustrate consumer’s clinical presentation and reasons for unmet goals). f. Clinician’s printed name and legible signature with date and credentials. The initial individualized treatment plan along with all revisions and updates. (This will demonstrate which goals the consumer has not achieved as well as goals for the continued stay period). Requests are due 30 days prior to the expiration of the previous authorization. It is the responsibility of the provider to ensure that all submitted documentation has been received by the Forensic Team. Once all required documentation has been received, the request will be processed within 5 business days of the decision to authorize or deny continued stay. Continued Stays are provided in 30-day intervals. Alternate authorization time intervals may be considered on an individual basis. Appeal and Denial Policies can be found in Sections 26 and 27 of this UM Manual. ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 81 - Section: 18 Adult Mental Health Adult Residential Level II Mental Health POLICY: A Level II residential treatment facility provides a structured group treatment setting with 24 hour per day, 7 days per week supervision for five or more residents who range from those who have significant deficits in independent living skills and need extensive supervision, support and assistance to those who have achieved a limited capacity for independent living, but who require frequent supervision, support and assistance. PURPOSE: To describe the eligibility, admission and criteria for provision of services for adult mental health residential treatment facilities. DESCRIPTION: Level II Mental Health Residential Treatment Facilities provide a long term, residential environment that provides care, support, assistance and limited supervision in daily living to adults diagnosed with a serious and persistent major mental illness who do not have another primary residence. A residential treatment facility under 65E-4.016 must sustain a 60 day average or greater length of stay of residents. For level II, each consumer shall receive services each week in accordance with subsection 65E-4.016(c) F.A.C. PROCEDURE: I. Assessment Procedure: Consumers seeking Adult Residential Level II Mental Health Treatment, and who are eligible for Department of Children and Families (DCF) funds, are required to receive an assessment prior to placement on the circuit centralized wait list and placement into a DCF funded bed. A referral is required, including referral form, recent psychiatric evaluation and any other clinical information if available. II. Obtaining Consent: Prior to conducting the above outlined screening/assessment, provider agencies are required to obtain consent from consumers. The consent form used is provided by the Department and South Florida Behavioral Health Network (SFBHN). The consent shall include authorization for sharing the information gathered in the assessment with the Department, SFBHN and any other entities requiring access to ensure coordinated quality care. All entities privileged to access the assessment are identified on the consent form appendix. The consent form is available in the ‘Forms’ section of this manual. III. Criteria for Admission A. Persons who enter Level II residential treatment facilities must meet the following minimum criteria: 1. Diagnosed as having a severe and persistent mental illness; 2. Age 18 or older; 3. Ambulatory or capable of self-transfer; 4. Able to participate in treatment programming and services; 5. Free of major medical conditions requiring ongoing 24 hours per day, 7 days per week nursing services; 6. Self-administers medication with staff supervision, 7. Does not exhibit chronic inappropriate behavior which disrupts the facility’s activities or is harmful to self or others. 8. Maintain personal hygiene and grooming with staff supervision, ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 82 - 9. Initiate and participates in social interaction with staff supervision, 10. Perform assigned household chores with staff supervision, and 11. Is capable of self-preservation in accordance with subparagraph 65E-4.016(17) (b) 2, F.A.C. 12. Additional admission criteria may be developed if such criteria are needed to insure that individuals admitted by the facility are compatible with the facility’s capability to serve them, or to further delineate the minimum skills or behaviors that a person needs to function in the facility’s environment. IV. Procedures for Residential Placement: A. Assessment: Prior to placement, all consumers undergo an assessment that includes a Diagnostic and Statistical Manual (DSM) Axis I-V diagnosis, current mental status exam, history, and clinical impression as to appropriateness for level of care. *upon system development, a universal assessment tool will be utilized. B. Referral and Placement: Following the completion of the assessment, the provider will notify SFBHN of the referral. SFBHN will determine if the information available supports the Admission Criteria as defined in Section III. SFBHN will attempt to find placement for the consumer within the network of Mental Health Residential Treatment Facilities. C. Bed Availability: 1. The provider will update bed availability on a weekly basis and report availability to the UM Specialist. Provider agencies are responsible for updating the bed list for their agency on a daily basis ensuring the ASOC Specialist has updated bed availability information. 2. If a placement is not immediately available, the SFBHN will maintain contact with the referral source for individuals on the waiting list while providing interim services Contacts are made in order of priority. Contact attempts are documented by SFBHN. After 3 unsuccessful attempts of contacting the referral source, a consumer may be bypassed on the waitlist, but may remain on the waitlist if still in need of services. D. Interim Services: The consumer should be enrolled in services by the assessing provider until residential placement is available. These services seek to provide engagement opportunities to the consumer until a placement becomes available, at which time the continued need for residential services will be evaluated. E. Waitlist: The consumer is also placed on the Centralized Wait List for Residential Services. A consumer release of information would continue to be obtained by the screening agency. If a placement is not immediately available, SFBHN will maintain a waitlist and will communicate with the referral source and the provider. F. Target Populations: Targeted consumers are individuals being served by the SAMH system who generally have a long-term involvement with that system, have multiple problems and needs, and require multiple services or resources to meet these needs. 1. Persons at least 18 years old diagnosed with a severe and persistent mental illness, with or without co-occurring disorders, with one of the following characteristics are priority clients: a. Persons who are been discharged from a state treatment facility; b. Persons who are forensic consumers (have an incompetent to proceed or a not guilty by reason of insanity court order); c. Persons who are at risk of institutionalization or incarceration for mental health reasons; d. Persons who have had three (3) or more admissions to a crisis stabilization unit (CSU), short-term residential facility (SRT), or inpatient psychiatric unit; e. Persons who are experiencing long-term or serious acute episodes of mental impairment that may put them at risk of requiring more intensive services. ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 83 - V. Initial Authorization: A. An authorization number is generated if consumer meets criteria based on the documentation received with referral. The authorization will become effective only upon admission into the treatment agency. B. Authorizations are for a specified length of stay with a start and end date. C. Reimbursement will only be provided for service dates covered by the authorization. D. The admitting agency will receive an initial 30 day authorization. In those 30 days a comprehensive assessment must be completed to receive continued authorization. E. Initial authorization length for adult consumers in residential Level II care is 12 months. The ASOC Specialist may provide authorization for an alternative length if indicated, on an individual basis. F. The authorization will become effective only upon admission into the treatment agency. G. The ASOC Specialist may provide authorization for an alternative length if indicated, on an individual basis as identified by ASOC Department. VI. Continued Stay Criteria: In addition to meeting all the criteria outlined in Section 18.IV on a continuing basis, the following criteria must also be met: A. An individualized plan of active treatment is required. This plan should contain at a minimum, clinical evidence of therapeutic goals that must be met before the consumer can return to a previous or other living situation. B. Evidence of continued need for support 24 hours a day through a therapeutic living situation. C. Evidence of coordination and access to active therapeutic interventions and services directed at the alleviation of clinical symptoms that are interfering with the consumer’s ability to return to a less intensive level of care. VII. Procedures for Continued Stay Request: The provider must review consumer’s information and determine the primary clinical reasoning for extending services at the same level of care. A. The provider must submit to the ASOC Department for review and determination: 1. Adult Mental Health ‘Continued Stay Authorization Request Form” containing the following: a. Consumer’s name and information b. Date of request c. Date current authorization expires on d. The staff person’s name and phone number and e-mail address available for discussing the request and providing additional information as needed e. Clearly written summary explaining the consumer’s presenting problem(s), Diagnosis, progress in treatment, barriers to progress and justification for continued stay. (Include specific consumer symptoms and/or behaviors to illustrate consumer’s clinical presentation and reasons for unmet goals). f. Clinician’s printed name and legible signature with date and credentials. 2. The initial individualized treatment plan along with all revisions and updates. (This will demonstrate which goals the consumer has not achieved as well as goals for the continued stay period). 3. A comprehensive assessment is completed within 30 days of admission. 4. Requests are due 30 days prior the expiration of the previous authorization. B. It is the responsibility of the provider to ensure that all submitted documentation has been received by the ASOC Specialist. Once all required documentation has been received, the request will be processed within 5 business days of the decision to authorize or deny payment for continued residential treatment. ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 84 - C. Denial and Reconsideration Policies and Procedures can be found in Sections 26 and 27 of this UM Manual. D. Continued Stay authorizations are provided in 90-day intervals. Alternate authorization time intervals may be considered on an individual basis. VIII. Billing Validation: A. The ASOC Department will monitor invoices submitted by providers on a monthly basis to ensure that the billing is in congruence with the authorization period granted to each consumer for residential services. The invoice should reflect the period of time for which the consumer’s stay was authorized. B. Upon completion of the monthly review, the provider will be notified of any discrepancies and the invoice will be adjusted accordingly. IX. System Management: A. SFBHN is the single point of contact for MH Residential Level II Treatment Facility referrals. B. SFBHN reviews referrals for eligibility; logs eligible referrals in a centralized list and forwards to the program for screening within 24 hours of having received the referral. C. SFBHN coordinates the screening of the referred person within three (3) days of the program having received the referral. D. SFBHN actively participates with the program in the approval of a referral. E. For approved referrals, SFBHN monitors and coordinates with the program the admission of the person into the program. F. SFBHN provides ongoing monitoring of the program to ensure compliance with length of stay (LOS), discharge procedures and staffing of difficult individuals admitted to the program. G. SFBHN provides technical assistance to ensure compliance with contract requirements and applicable laws and regulations. H. SFBHN provides technical assistance and coordination with other community providers to ensure that individuals being discharged from the program have access to less restrictive residential levels of care. I. SFBHN acts a liaison to the program and assists in the elimination of barriers to discharge for individuals served in the program. ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 85 - Section: 19 Adult Mental Health Adult Forensic Services POLICY: Forensic services are responsible for a service delivery system of mental health and substance abuse for adults age 18 and over who are diagnosed with a severe and persistent mental illness and because of their mental illness have a legal status indicating that they were found under Chapter 916 to be Not Guilty by Reason of Insanity (NGI) or Incompetent to Proceed (ITP). PURPOSE: To describe the mental health and substance abuse services available for adults within the legal system who were deemed Not Guilty by Reason of Insanity or Incompetent to Proceed. PROCEDURE: I. Program Protocol: The South Florida Behavioral Health Network (SFBHN) in partnership with the judiciary, criminal justice and social services, state treatment facilities and correctional institutions and subcontracted mental health and substance abuse providers, facilitate the timely delivery of effective services in the least restrictive environment possible. II. Forensic Service Continuum: The continuum includes access to a full array of services including acute care, residential treatment programs and outreach services, which are provided in a variety of settings including county jails, state treatment facilities and the local community. The various services available include: A. Centralized Forensic Specialist Team 1. Assessments 2. Discharge planning 3. Coordination of services 4. Conditional release monitoring and intervention B. Competency Restoration Program 1. Weekly onsite competency groups (5 locations) 2. Individual competency classes – jail, designated locations 3. Competency evaluations C. Forensic Residential Treatment Services 1. Short Term Residential Treatment (SRT) 2. Miami Dade Forensic Alternative Center (MDFAC) 3. Residential Treatment Level II 4. Crisis Support/ Emergency D. Outpatient Services III. System Management: A. SFBHN is responsible for submission of up-to-date tracking of individuals on conditional release and ongoing communication with the program office. B. SFBHN participates on bimonthly Forensic Team meeting and facilities discussion about difficult to serve individuals and facilitate services for those discussed. SFBHN also participates in the treatment team meetings for the MD FAC and SRT programs. SFBHN participation aims to ensure that individuals being served are clinically appropriate for the level of care and that transition to less restrictive level of care are facilitated. C. SFBHN will hold quarterly Forensic Stakeholder meetings to manage the expectations of the criminal justice system and that of the adult forensic mental health system of care identified above. ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 86 - Section: 20 Adult Mental Health Indigent Drug Program (IDP) POLICY: SFBHN provides oversight, monitoring, and service validation for the Indigent Drug Program (IDP) network providers to ensure that all funds allocated are utilized for purchasing psychotropic medications or medications accessed through the “Line of Credit” from the Indigent Drug Program (IDP) as per the state’s existing allocations as delineated in the master contract. PURPOSE: To describe the eligibility criteria for provision of services through the IDP. PROCEDURE: I. Eligibility Criteria: Individuals who meet ANY of the following criteria are eligible for IDP funds: A. Have an annual income that is at or below 150% of the Federal Poverty Income Guidelines, as published annually in the Federal Register. B. If the individual has third party insurance for psychotropic medications but has temporarily been denied benefits for these medications, they may receive IDP medications until such time as eligibility has been reestablished. II. Exclusion Criteria: A. The individual has third-party insurance or other source of psychotropic medications available. B. The individual is a participant in a program where psychotropic medications are paid for by any other funding source. III. IDP Program Management: SFBHN manages the IDP allotment as follows: A. Disseminates IDP Year-To-Date (YTD) Activity Reports to all providers and the Department as received from Florida State Hospital. B. Monitors providers to ensure utilization to prevent lapsed funds and take appropriate action for under or over utilization. C. Monitors subcontractors to ensure utilization for eligible individuals. ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 87 - Section: 21 Adult Mental Health Projects for Assistance in Transition from Homelessness (PATH) POLICY: The Projects for Assistance in Transition from Homelessness (PATH) Program is administered by the Center for Mental Health Services, of the Substance Abuse and Mental Health Services Administration (SAMHSA), within the U.S. Department of Health and Human Services are authorized by the Stewart B. McKinney Homeless Assistance Amendments Act of 1990. PATH funds community-based outreach, mental health and substance abuse services, case management, and limited housing services for people experiencing serious mental illnesses—including those with co-occurring substance use disorders—who are experiencing homelessness or are at risk of becoming homeless. PURPOSE: To describe the eligibility criteria for provision of services through the PATH Program. PROCEDURE: I. PATH Eligibility Criteria: A. Homeless or imminent risk of becoming homeless; and B. Suspected of having a serious mental illness; and C. Not in the custody/guardianship of the State of Florida; and D. Not receiving a similar service. II. PATH Program Management: A. SFBHN manages PATH services and ensures dissemination of deliverables as set forth and described in each approved and signed Local Intended Use Application. 1. Oversees the Annual reapplication process for the PATH Grant 2. Compiles Annual report information and sends a final draft to the Southern Region SAMH Program Office for approval. 3. Ensures providers submit final Annual report to Tallahassee. B. Eligible PATH local matching funds must be expended in the provision of PATH eligible services to PATH eligible persons. The expenditures must match the types of services outlined in the Local Intended Use Plan. The formula to be followed is cited in Section 524 of the Public Health Services Act, as amended by Public Law 101-645. ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 88 - Section: 22 Adult Substance Abuse Family Intervention Specialists (FIS) POLICY: Family Intervention Specialists (FIS) services are designed to reduce the incidence of child abuse and neglect resulting from parents’ or caregivers’ behavioral health and to improve outcomes for families in the child welfare system and/or community based care. PURPOSE: To describe the eligibility, admission and criteria for provision of services by FIS. PROCEDURE: I. Program Protocol: A. All FIS funded agencies will adhere to Florida Guidelines for Family Intervention Specialists (FIS) (most current edition): http://www.dcf.state.fl.us/programs/samh/SubstanceAbuse/docs/FIS_Guidelines_07-0110.pdf B. SFBHN will monitor all subcontracted agencies to ensure compliance with FIS guidelines through Monitoring. C. SFBHN conducts subcontractor monitoring as specified in master contract. II. FIS Eligibility Criteria: Eligible FIS referrals are parents/caregivers, significant others, household residents and their children referred by child welfare, protective investigations, or a dependency court. Referred family members are those for whom substance abuse is suspected as a contributing factor to the abuse/neglect situation. III. FIS Referrals: A. A referral can be made when the Child Protective Investigator (CPI) suspects that parent(s)/caregiver(s) alcohol and/or drug use/abuse may be contributing factors in a situation where a child's safety or well-being is at risk. B. Referrals may be made during the initial child abuse/neglect investigation or at any point during child protective supervision or out-of-home care. C. In the event that a person or family is in need of screening or referral, the CPI worker should inform the family member that a recommendation will be made to the FIS for a substance abuse screening and obtain the appropriate release of information. The case should then be discussed with the FIS and the CPI worker should provide the FIS with a referral packet. D. The provider agency and the FIS are responsible for determining what constitutes a complete referral package and conveying these requirements to the referral agents. This will likely include copies of any relevant assessments, contact information, and recommendations or background information that may be of use to the FIS in conducting the substance abuse screening. E. The FIS will attempt contact with the consumer within three (3) working days of receipt of the complete referral package. IV. Contingency Funds: A. Limited discretionary funds in each region are available to be used to support successful outcomes for families receiving FIS services. Funds are used for the purpose of removing barriers to person's successful participation and completion of treatment and to support the substance abuse treatment plan. These funds should only be utilized if no other funding source can be identified. Examples of appropriate use include the provision of childcare, transportation, storage of personal belongings during short-term residential ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 89 - B. C. D. E. treatment, educational/ vocational assistance, support for housing/utility costs, and clothing. Use of discretionary funds should be determined on an individual basis. Some consumers are especially needy of this type of support and may require a greater share of the available funds from this resource than other families in the FIS caseload. Any expenditure of contingency funds should be documented in the individual’s clinical record. Procedures: 1. FIS funded subcontractors are to contact their SFBHN FIS Program Manager when requesting FIS contingency funds. 2. The fund request form should be submitted to SFBHN for requisitioning of contingency funds. 3. The SFBHN FIS Program Manager will review the request and make a determination of approval or denial of funding within 48 hours of receipt of the request. 4. The SFBHN FIS Program Manager shall notify via fax the FIS funded subcontractors of the decision to approve or deny funding. 5. Should further information or clarification be needed, the SFBHN FIS Program Manager will contact the FIS funded provider for further information/clarification. 6. Upon receiving any additional information, the SFBHN Program Manager shall determine if funding is partially approved or denied, will make such notation on form and fax back the form to the provider. A monthly report will be generated detailing year-to-date expenditures, the balance of the FIS provider’s contingency fund account, and the corresponding incidental/contingency form request submitted to the SFBHN FIS Program Manager for reimbursement. Substance abuse incidental/contingency funds expenditures will be reflected under the incidental expense cost center section on the monthly invoice. Requests for incidental/contingency funds MUST include the following information: 1. FIS accessing funds 2. Funds spent on behalf of (consumer name) 3. Referral type (protective investigation/supervision) 4. Date of request 5. Description of goods/services requested 6. How the purchase is related directly to the FIS intervention plan 7. Goal/reason for purchase amount requested 8. FIS and approving authority signature with date ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 90 - Section: 23 Adult Substance Abuse Adult Residential Levels I-II Substance Abuse POLICY: Residential substance abuse treatment is provided 24 hours-per-day, 7 days-per-week, and is intended for consumers who meet the placement criteria for this level of care. PURPOSE: To describe the eligibility, admission and criteria for provision of services for adult residential substance abuse. For the purpose of this manual, residential treatment is comprised of two levels (Residential Levels I & II). Residential Level I: Level I programs provide services on a short-term basis. This level of care is appropriate for persons who have sub-acute biomedical problems or behavioral, emotional, or cognitive problems that are severe enough that they require inpatient treatment, but do not need the full resources of an acute care general hospital or a medically managed inpatient treatment program. Typically, consumers have a job and a home to support their recovery upon completion of this level of care. The emphasis is clearly on an intensive regimen of clinical services using a multidisciplinary team approach. Services may include some medical services based on the needs of the consumer. Level I services include, at least 14 hours of counseling per week Each consumer shall receive services each week in accordance with subsection 65D-30.007(3), F.A.C. Residential Level II: Level II programs include those that are referred to as therapeutic communities or some variation of therapeutic communities. Duration of treatment is longer than level II. This level is appropriate for persons characterized as having chaotic and often abusive interpersonal relationships, extensive criminal justice histories, prior treatment episodes in less restrictive levels of care, inconsistent work histories and educational experiences, and anti-social behavior. In addition to clinical services, considerable emphasis is placed on services that address the consumer’s educational and vocational needs, socially dysfunctional behavior, and need for stable housing upon discharge. It also includes services that assist the consumer in remaining abstinent upon returning to the community. For level II, each consumer shall receive services each week in accordance with subsection 65D30.007(3), F.A.C., including at least 10 hours of counseling per week PROCEDURE: I. Assessment Procedure: Consumers who may require residential Level I or Level II substance abuse treatment, and who are eligible for Department of Children and Families (DCF) funds, are required to receive the following assessments prior to placement on the circuit centralized wait list and placement into a DCF funded bed. A. Screening: The Global Appraisal of Individual Needs -Quick (GAIN-Q) B. Admission: The Global Appraisal of Individual Needs-Initial (GAIN-I) II. Obtaining Consent: Prior to conducting the above outlined screening/assessment, provider ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 91 - agencies are required to obtain consent from consumers. The consent form used is provided by South Florida Behavioral Health Network (SFBHN). The consent shall include authorization for sharing the information gathered in the assessment with the Department, SFBHN and any other entities requiring access to ensure coordinated quality care. All entities privileged to access the assessment are identified on the consent form appendix. The consent form is available in the ‘Forms’ section of this manual. III. Completion of the GAIN: The GAIN must be completed fully. For sections in which items are identified as being a clinical concern, the clinicians conducting the assessment must utilize the comment section to provide further detail. Completed and edited GAIN Q-RRS and G-RRS must be submitted for placement onto the waitlist and/or admission into treatment. A. The GAIN-Q is valid for 90 days unless consumer has been placed in a controlled environment. To ensure appropriateness of services, if the consumer was not in a controlled environment and more than 90 days have lapsed since the last assessment, the consumer must be re-screened prior to placement. B. Additional Information: Assessment must also include information regarding Medicaid or other benefits, target population, and high-user status (3 or more admissions to a residential program in the past 2 years). C. For consumers in a controlled environment (e.g., jail or hospital), the length of time for which the assessment remains valid is determined on an individual basis. If upon assessment, the provider agency determines that the consumer requires a level of care other than residential substance abuse Level I or Level II placement or requires another type of treatment (medical, crisis stabilization, etc.), the provider agency is responsible for generating the appropriate referral. IV. Criteria for Admission: The consumer must meet specifications in each of the six dimensions: A. Dimension 1: Acute Intoxication and/or Withdrawal. 1. Consumer has no signs or symptoms of withdrawal, or his or her withdrawal needs can be safely managed in a Level I or II setting. B. Dimension 2: Biomedical Conditions and Complications: 1. Biomedical problems, if any, are stable and do not require 24-hour monitoring and the consumer is capable of self-administering any prescribed medications; or 2. A current biomedical condition is not severe enough to warrant inpatient treatment but is sufficient to distract from treatment or recovery efforts. The biomedical problem requires monitoring, which can be provided by the program or through an arrangement with another provider. C. Dimension 3: Emotional, Behavioral, Cognitive Conditions and Complications: (If any of these conditions are present, consumer must be in a Dual Diagnosis Capable or Enhanced Program). The consumer’s status is characterized by 1 of the following: 1. Consumer’s psychiatric condition is stabilizing. However, the consumer is unable to control use of alcohol or other drugs and/or antisocial behaviors, with probability of harm to self or others. The resulting level of dysfunction is so severe that the consumer is unable to participate in a less structured or intensive level of care. 2. Consumer demonstrates repeated inability to control impulses to use alcohol or other drugs and/or engage in antisocial behavior, with likelihood of harm to self or others. The resulting level of dysfunction is so severe that the consumer is unable to participate in treatment in the absence of the 24-hour support and structure of a Level I or II program. 3. Consumer demonstrates antisocial behaviors that have led or could lead to significant criminal justice problems, lack of concerns for others and extreme lack or regard for authority, and which the consumer is unable to participate in a less structured or intensive level of care. ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 92 - 4. Consumer has significant functional deficits, which are likely to respond to staff interventions. However, the consumer is not likely to maintain mental stability and/or abstinence if treatment is provided in a non-residential program. 5. Consumer’s related personality disorders are of such severity that the accompanying dysfunctional behaviors require continuous boundary-setting interventions. 6. Consumer’s mental status is assessed as sufficiently stable to permit the consumer to participate in therapeutic interventions and to benefit from treatment. D. Dimension 4: Readiness to Change: The consumer’s status is characterized by 1 of the following: 1. Because of the intensity of the addictive disorder or the mental health problem, the consumer has little awareness of the need for continuous care, the existence of substance use or mental health problem and need for treatment and thus has limited readiness to change. 2. Despite serious consequences, the consumer has difficulty in understanding the relationship between the substance use, addiction, mental health or life problems, their impaired coping skills and level of functioning, often blaming others for their problems. 3. Consumer demonstrates passive or active opposition to addressing the severity of their mental or addiction problem, or does not recognize the need for treatment. This poses a danger of harm to self or others. However, assessment indicates that treatment interventions available at Level I or II may increase the consumer’s degree of readiness to change. 4. Consumer requires structured therapy and 24-hour program setting to promote treatment progress/recovery because other interventions have failed at a less intensive level of care and are not likely to succeed in the future at a less intensive level of care. 5. Consumer’s perspective impairs their ability to make behavior changes without repeated, structure, clinically directed motivational interventions, delivered in a 24hour program setting. E. Dimension 5: Relapse, Continued Use or Continued Problem Potential: the consumer’s status is characterized by 1 of the following: 1. Consumer does not recognize relapse triggers and is not committed to continuing care. Continued substance use poses an imminent danger of harm to self or others without 24-hour monitoring and structured support. 2. Consumer’s psychiatric condition is stabilizing. However, despite efforts, consumer is unable to control use and/or antisocial behaviors with a probability of harm to self or others. Continued substance use poses an imminent danger of harm to self or others without 24-hour monitoring and structured support. 3. Consumer’s cognitive impairment has limited their ability to identify or cope with relapse triggers and high-risk situations. Consumer requires relapse prevention activities that are delivered at a slower pace and in a setting that provides 24-hour structure and support to prevent imminent danger or dangerous consequences. 4. Consumer is in imminent danger of relapse, with dangerous emotional, behavioral or cognitive consequences, because of a crisis situation. 5. Despite recent participation in treatment at a less intensive level of care, the consumer continues to use or to deteriorate psychiatrically, with imminent serious consequences and is at high-risk for continued use and deterioration without 24hour monitoring and treatment. F. Dimension 6: Recovery Environment: the consumer’s status is characterized by 1 of the following: 1. Consumer has been living in an environment that is characterized by a moderately high of initiation or repetition of physical, sexual or emotional abuse, or substance use where the consumer is assessed as being unable to obtain or ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 93 - maintain recovery in a less intensive setting. 2. Consumer is in danger of victimization and requires 24-hour supervision. 3. Consumer’s social network is characterized by social isolation/withdrawal, such that recovery goals are unachievable at a less intensive setting. 4. Consumer’s social network involves living with an individual who is a regular user, abuser or dealer of drugs, or the living environment is highly invested in alcohol or drug use that their recovery goals are unachievable. 5. Due to cognitive limitations, consumer is in danger of victimization by another and requires 24-hour supervision. 6. Consumer’s living environment is characterized by criminal behavior, victimization and other antisocial norms and values. V. Procedures for Residential Placement: A. Assessment: Prior to Residential Level I or II placement, all consumers undergo an assessment that includes the GAIN. The consumer’s assessment is entered into the GAIN ABS Application. Providers participating in the Substance Abuse Utilization Management (SAUM) Program utilize the GAIN ABS Application. B. Referral and Placement: Following the completion of the assessment, the provider will notify SFBHN of the referral. SFBHN will review the available information to confirm that the criteria for admission are met. If the documentation supports admission, SFBHN will attempt to find placement for the consumer within the network of treatment facilities that provide Residential Level I or II treatment services. If the documentation does not support admission, SFBHN will notify the provider and consumer of the denial. C. Bed Availability: 1. The provider will update bed availability on a daily basis and report availability to the UM Specialist. Provider agencies are responsible for updating the bed list for their agency on a daily basis ensuring the UM Specialist has updated bed availability information. 2. If a placement is not immediately available, the SFBHN will maintain contact with consumers on the waiting list for up to 30 days. After 3 unsuccessful attempts, a consumer may be removed from the waitlist. The SFBHN validates placements through ongoing on-site monitoring. 3. The SFBHN contacts consumers in order of priority. Attempts to contact a consumer are documented by the SFBHN. D. Interim Services: The consumer will be offered interim services by the assessing provider if residential placement is not available. Interim services seek to provide engagement opportunities to the consumer until a placement becomes available, at which time the continued need for services will be evaluated. E. Waitlist: The consumer is also placed on the Centralized Wait List for Residential Services. A consumer release of information would continue to be obtained by the screening agency. The GAIN ABS Application updates records daily to incorporate newly added consumers to the wait list. 1. Homeless Consumers: The provider must provide homeless consumers with instructions to begin calling the UM Specialist for placement within two business days. Providers will inform homeless consumers at the point of initial assessment of their waitlist status. The instructions given to the consumer must include the toll free contact number and hours (see below). Although homelessness is not a circuit target population, efforts are made to provide immediate placement when possible in order to minimize loss of contact. Homelessness is defined by DCF Pamphlet 155-2 as “an individual who lacks housing (without regard to whether the individual is a member of a family), including an individual whose primary residence during the night is a supervised public or private facility that provides temporary overnight ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 94 - shelter. Temporary overnight shelter being defined as a facility where the individual has a place to stay during the night and is required to leave during daytime hours.” Homeless consumers, if not placed, would require referral to shelter or other temporary housing arrangements. Consumers living with friends and/or relatives are not classified as homeless. Note that the target population consumers are prioritized. The provider gives the consumer the contact number, 1-866-833-7477, and instructs them to contact the UM Specialist daily between the hours of 10:00am and 2:00pm for placement or linkage to interim services. F. Target Populations: These populations are given priority status when placing consumers in available residential beds, due to the nature and severity of their substance abuse. A consumer is designated as being part of the target population through the assessment process. Priority Target Populations include: 1. Pregnant, injecting drug users 2. Other pregnant substance users 3. Other injecting drug users 4. Women with dependent children (including those involved in Child Welfare System) 5. Other parents putting children at risk (including those involved in Child Welfare System) 6. Consumers involved with the criminal justice system 7. Dual diagnosed / Consumers with co-occurring disorders VI. Initial Authorization: A. An authorization number is generated if consumer meets criteria based on the GAIN-I assessment completed by admitting agency. The authorization will become effective only upon admission into the treatment agency. B. Authorizations are for a specified length of stay with a start and end date. C. Reimbursement will only be provided for service dates covered by the authorization. D. The admitting agency will receive an initial 5 day authorization, in those 5 days based on the GAIN-Q Screening, The admitting agency must complete a full GAIN-I in order to receive continued authorization. E. Initial authorization length for adult consumers in residential Level I or II care is 61 days and 90 days for High-Risk/High-Utilizer Consumers. The UM Specialist may provide authorization for an alternative length if indicated, on an individual basis. VII. Continued Stay Criteria: In addition to meeting all the criteria outlines in Section 23.IV on a continuing basis, the following criteria must also be met: A. An individualized plan of active treatment is required. This plan should contain at a minimum, clinical evidence of therapeutic goals that must be met before the consumer can return to a previous or other living situation. B. Evidence of continued support 24 hours a day through a therapeutic living situation. C. Evidence of coordination and access to active therapeutic interventions and services directed at the alleviation of clinical symptoms that are interfering with the consumer’s ability to return to a less intensive level of care. VIII. Procedures for Continued Stay Request: The provider must review consumer’s information and determine the primary clinical reasoning for extending services at the same level of care. A. The provider must submit to the UM Department for review and determination: 1. A ‘Continued Stay Authorization Request Form” 2. The initial individualized treatment plan along with all revisions and updates. (This will demonstrate which goals the consumer has not achieved as well as goals for ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 95 - B. C. D. E. the continued stay period). 3. A clearly written summary explaining clinical justification for the continued stay request. Include both the consumer’s need (s) and planned staff intervention. (Include specific consumer symptoms and/or behaviors to illustrate consumer’s clinical presentation and reasons for unmet goals). The summary should be typed on the Provider’s letterhead stationery and include: a. Date b. Consumer’s name and I.D. c. Clinician’s printed name and legible signature with date and credentials. d. The staff person’s name and phone number and e-mail address available for discussing the request and providing additional information as needed. e. Requests are due 30 days prior the expiration of the previous authorization. The request must be received by the Utilization Management Department no later than 14 days prior to the expiration date of the current authorization. 1. Providers may request a continued stay after the 14 day interval for special circumstances (i.e. consumer relapse). These requests will be considered on an individual basis. It is the responsibility of the provider to ensure that all submitted documentation has been received by the UM Specialist. Once all required documentation has been received, the request will be processed within 5 business days of the decision to authorize or deny payment for continued residential treatment. Appeal and Denial Policies can be found in Sections 26 and 27 of this UM Manual. Continued Stays are provided in 30-day intervals. Alternate authorization time intervals may be considered on an individual basis. IX. High Risk/High Utilizer Consumers: A. High-Risk/High Utilizer Consumers are defined as the following: 1. High-Risk: Consumers presenting with multiple service needs with at least one of the problem areas identified as ‘severe’. Pregnant consumers, IV drug users, and consumers with involvement in the Child Welfare System are also identified as HighRisk. 2. High-User: Consumers with three or more placements in residential level I or level 2 treatments within a 2 year period are identified as High-Users. B. High-Risk & High-Utilizer Follow-Up: The UM Specialists will follow-up and gather data on high-risk & high-user consumers. Follow-up may include clinical record review and observational participation in case staffing. Information gathered may include the following: common traits among high-risk consumers, services provided, consumers’ responses to treatment interventions utilized, coordination between provider and Child Welfare System, when applicable, and significant areas identified on a case by case basis. Information gathered on high risk and high users will be trended and analyzed through SFBHN’s QA/QI department for treatment recommendations. X. Documentation Requirements: The following documents will be maintained by the Treatment Provider for all consumers placed in residential care: A. A copy GAIN-Q,GAIN-I, and/or GAIN-M90* if the forms are not in the GAIN ABS Database B. Psychiatric Evaluation or Detoxification Clearance (if necessary) C. Initial Treatment Plan* D. Continued Stay Request Letter* E. Continued Stay ASAM-PPC-2-R F. The most up-to-date Treatment Plan Review* *Providers only need to submit “*” indicated documents to SFBHN if seeking a continued stay ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 96 - authorization or if the consumer was identified as a high-risk/high-user consumer. XI. Billing Validation: A. The UM Department will monitor invoices submitted by providers on a monthly basis to ensure that the billing is in congruence with the authorization period granted to each consumer for residential services. The invoice should reflect the period of time for which the consumer’s stay was authorized. B. Upon completion of the monthly review, the provider will be notified of any discrepancies and the invoice will be adjusted accordingly. ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 97 - ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 98 - General ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 99 - Section: 24 General Temporary Assistance for Needy Families (TANF) POLICY: Temporary Assistance for Needy Families (TANF) is cash assistance for families, including any family receiving cash assistance payments or TANF diversion services from the state program pursuant to the provisions of section 414.045, F.S., and Part A of Title IV of the Social Security Act. PURPOSE: To describe the eligibility and criteria for provision of services through the TANF Program. PROCEDURE: I. TANF Eligibility: SFBHN manages TANF services and ensures consumer eligibility as set forth and described in The TANF Guidelines issued by the State of Florida. Subcontractors are required to comply with the provisions of the TANF Guidelines for any disbursement of TANF funds. TANF Guidelines can be found at the following web site: http://www.dcf.state.fl.us/programs/samh/contract/tanf.pdf II. TANF Specialists: TANF Specialists provide technical assistance to agencies as needed, identifying outreach services, and promoting interagency collaboration for linkages in the communities. TANF Specialists ensures that all TANF Guidelines requirements are consistently utilized with services performed for the consumers at the Provider Agencies. III. Procedure for TANF Services Determination: A. The provider must complete a screening to determine if the consumer is eligible for TANF services as outlined in the TANF Guidelines. B. The provider agency completes the TANF SAMH EZ-1 Authorization Form, certifies the consumer eligible or ineligible, and sends the form via the TANF database to the TANF Specialist for authorization of TANF services. After the consumer has completed the screening process, the Provider Outreach staff must: 1. Log all required information on the Log of Outreach Activities Form, 2. Submit the Log of Outreach Activities form and 3. Submit the Billing Invoice to SFBHN. C. To obtain an authorization confirmation number: 1. The TANF Specialists will click on provider agency’s consumers’ SSN to view the consumer’s complete record, 2. Proceed to the Edit Screen where they will add the Acknowledgment Date, 3. The Confirmation Number (authorization number) will be automatically added. These Confirmation Numbers are unique to each district in Florida. D. Consumer eligibility must be pre-certified by the provider agency before sending to TANF Specialist for authorization to ensure proper billing for TANF SAMH services. 1. Recertification will be performed annually each July for the participants who recertify themselves for continuing TANF eligibility status. E. A copy of the TANF SAMH EZ-1 Eligibility Form must be secured to ensure confidentiality and kept in the following files: 1. TANF Provider Agency a. Consumer File 2. Referral Agency (i.e., South Florida Workforce (SFW), Family Safety Program ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 100 - (FSP), Department of Juvenile Justice (DJJ)) a. Case Manager File IV. TANF Confirmation Number: A. Confirmation numbers are randomly assigned numbers generated through TANF Database. B. The TANF Specialist provides a confirmation number for each TCA consumer, Non-TCA consumer, and CO consumer requesting TANF SAMH services. C. Providers will be able to see all of their agency’s consumers that are pending approval from the TANF Specialist. D. Providers will use this screen to notify the appropriate TANF Specialist of the pending consumers via email. E. The consumer will not be considered eligible for payment if they do not have a confirmation number. F. The provider agency must log each consumer confirmation number on the TANF SAMH Monthly Consumer Log and submit the Billing Invoice to SFBHN SAMH Contract Office. V. TANF Discharge Goals Assessment: A. All TANF Provider agencies submit the TANF SAMH Discharge Goals Assessment to the TANF Specialist via the TANF Database within 10 days after discharge of consumers. B. SFBHN tracks receipts of discharge goals assessment through TANF logs. SFBHN notifies providers of pending discharge goals assessments through monthly calls placed to delinquent providers. C. The first two goals must be clearly identified with dates and date of completed treatment. VI. TANF Contingency Funds: A. The following procedures are required to determine a consumer’s eligibility for TANF Contingency funds: 1. TANF provider must identify eligible the TANF consumer and submit the TANF Services and One-Time Payment Request and Approval Form to the TANF specialist. B. The TANF Services and One-Time Payment Form must include: 1. Consumer Name 2. Number of Days (24 hours) per month in rental housing unit (Census Log) 3. The goals for SAMH TANF 4. Description of treatment services received each month 5. Rental Receipt (Back-up Documentation) 6. Approving authority signature with date C. Funds requested by TANF provider may not exceed a one hundred twenty (120) day time period. D. TANF Specialist will review submitted TANF Services & One-Time Payment Request/Approval form. 1. If approval is granted, SFBHN will complete the approval section of the form and fax back to the provider identifying the total funds approved. 2. If approval is denied, SFBHN will complete the disapproval section of the form and identify the reason(s) for disapproval and fax back to the provider. a. Prior to disapproving any request, SFBHN will contact the TANF provider for further clarification and/or documentation. After contact with the TANF provider the TANF specialist shall determine if the TANF consumer meets the eligibility requirements for approval of TANF Contingency funds. E. SFBHN will monitor TANF providers through monitoring to ensure compliance with TANF contingency funds. VII. TANF Billing Validation: ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 101 - A. The TANF Department will monitor invoices submitted by providers on a monthly basis to ensure that the billing is in congruence with the certification period granted to each consumer for TANF services. The invoice should reflect the period of time for which the consumer’s stay was certified. B. Upon completion of the monthly review, the provider will be notified of any discrepancies and the invoice will be adjusted accordingly. VIII. TANF Monitoring: A. There will be continuous program reviews and monitoring through the SAMH data warehouse and other integrated data systems for TANF participants’ eligibility authorization and system coordination. B. Annual record reviews will be performed at the treatment providers to assure that TANF requirements are being followed. When providers are being monitored for programmatic quality assurance, TANF Staff randomly selected files and look within the progress notes and treatment plans for evidence that participants are pursuing the TANF goals as part of their treatment. The SFBHN Monitor will check, among other items, if the TANF strengthsbased goals are documented as the TANF participants’ wants with the objectives being what the individuals need. For a complete list of what is to be monitored, please refer to TANF SAMH Policy Handbook: http://www.dcf.state.fl.us/programs/access/docs/TANF%20101%20final.pdf. ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 102 - Section: 25 General Reporting and Compliance Reviews POLICY: South Florida Behavioral Health Network (SFBHN) submits operations information to its System of Care (SOC) / Quality Improvement (QI) Committee (SOC/QI) for stakeholder, provider, and consumer feedback and recommendations. The SOC/QI Committee is a subcommittee of the Board of Directors which is tasked to recommend goals to the full Board to improve and transform system of care, utilization management processes and the QI program. PURPOSE: To describe the reporting and compliance functions of the SOC/QI Committee. PROCEDURE: I. SOC/QI Committee membership shall be determined by the Chair of the Board with representation from the provider network and include a minimum of one consumer or a family member of a consumer. Recommendations are reviewed by SFBHN staff through its Continuous Quality Improvement (CQI) structure to ensure proper utilization management and functioning of the system of care. II. SFBHN is contractually obligated to submit monthly and/or quarterly utilization management reports to the Department. These reports include utilization activity relative to utilization goals, program compliance, and corrective actions. III. See individual program sections for specified programmatic reports. IV. As part of the quality improvement program, the SFBHN provides or coordinates reviews of service compliance with criteria and practice guidelines, such as retrospective reviews, to ensure the level of placement of consumers is appropriate. The SFBHN takes corrective action to resolve situations in which the subcontracted providers are not following the guidelines or working to help the system meet its utilization goals. V. SFBHN staff submits the following reports to its SOC/QI Committee: A. Overall System of Care Reports: 1. Performance Measures Report (Exhibit D) 2. Provider Report Cards 3. Invoice Validation Report 4. Incident Reports 5. Linkage to System of Care Services (Residential to Outpatient) B. Children’s System of Care Reports: 1. Children’s System – Residential Services Report 2. Juvenile Incompetent to Proceed (JITP) Waiting List Report 3. Families and Communities Empowered for Success (FACES) Census Report 4. FACES Incidental Report C. Adult System of Care Reports: 1. Residential Services Report – Substance Abuse 2. Residential Services Report – Mental Health 3. Short-Term Residential Services Report 4. Crisis Stabilization Unit Utilization Report ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 103 - 7. 8. 9. 10. VI. 5. Florida Assertive Community Treatment (FACT) Reports 6. Indigent Drug Program (IDP) Utilization Report State Treatment Facilities Admissions & Discharge Report Detox & CSU Utilization Reports Lapse Reports (including incidental expenditures) Temporary Assistance for Needy Families (TANF) Report SFBHN utilizes the above outlined reports to ensure program compliance and utilization and to ensure its core SOC values and principles are integrated to the provided services that are being managed through its Utilization Management Programs. ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 104 - Section: 26 General Authorizations & Denials POLICY: South Florida Behavioral Health Network (SFBHN) is committed to employing evidence based criteria and procedures for approving and authorizing of payment for care. Our Utilization Management (UM) staff is accessible to practitioners and consumers to discuss UM and related issues as appropriate. These guidelines are meant to structure and direct the process of authorization of behavioral health treatment. They do not in any way dictate or replace sound clinical care by each of the providers. Medical necessity of care is based on the principles of improved symptom severity and functioning. In situations where chronicity exists the goal is the maintenance of ability and prevention of deterioration. PURPOSE: To define the procedures for which decisions are made to authorize payment for services. PROCEDURE: I. Eligibility Determination: Every consumer referred for behavioral health services shall be screened as a first step in determining the consumer's clinical eligibility for services. Please refer to each specific section for program specific eligibility criteria. II. Authorizations: Procedures for obtaining authorization for payment are specified in each program area. Please refer to the appropriate section of each program for details. Authorizations and denials for payment for services are made by the UM staff member assigned to each program. III. Denials by SFBHN: A. Denials of payment for services shall be communicated in writing to the consumer and provider. B. The reasons for the denial shall be clearly documented in the communication. C. All denial notifications shall outline the process for reconsiderations. D. All denials for payments for services are staffed by the UM Committee. IV. Denials by Providers: A. Denials shall be communicated in writing by the provider to the consumer and SFBHN. B. The reasons for the denial shall be clearly documented in the communication. C. All denials by providers are staffed by the UM Committee. D. The UM Committee will review the denial and may determine: 1. Uphold the provider denial 2. Staff the denial with the provider for additional information 3. Overturn the provider denial E. The UM Committee shall communicate their determination in writing to the provider and consumer. ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 105 - Section: 27 General Reconsiderations POLICY: Behavioral health treatment is a multifaceted and complex process. A request to reevaluate a decision by the Utilization Management (UM) Committee to deny authorization for payment is considered a reconsideration. Reconsiderations are applicable only to South Florida Behavioral Health Network (SFBHN) funded services and placements; it does not pertain to services funded by other agencies. Procedures for reconsiderations are developed to afford consumers and providers opportunities to have denials reexamined. PURPOSE: To define the guidelines for which consumers and providers can request a denial for payment of services be reconsidered. PROCEDURE: I. UM Committee: The UM Committee is comprised of the SFBHN Vice President of Behavioral Health Services, the Medical Director and two UM staff persons (A child and adult representative). The UM Committee meets routinely on a bimonthly basis or more frequently as needed. This Committee performs the following functions: A. Oversees the development and maintenance of the UM Polices, Procedures and Manual. B. Evaluates, updates and approves the UM manual annually for adoption by the SFBHN Board of Directors C. Reviews all denials of payments. D. Reviews all requests for reconsiderations of authorizations for payments. E. Establishes procedures for evaluating member and provider satisfaction of the UM process. II. Types of reconsiderations: A. Concurrent: 1. Reconsiderations of a denial are considered concurrent if services are currently still being provided to the consumer. Decisions are made within 30 working days of receipt of the request. Requests received after the 30 working day period will be managed as a retrospective request. 2. Expedited concurrent reconsiderations may be requested when a delay in decision-making might jeopardize the life or health status of the claimant because of the clinical urgency of their situation. Decisions are made within 3 working days of the request. B. Retrospective: 1. Request for reconsiderations may be initiated up to 180 days after the denial is made. These requests include post-service requests. III. Initiation of a request for reconsideration: A. A claimant can initiate a reconsideration request. A claimant includes: 1. Consumer 2. Consumer’s physician with the Consumer's consent 3. Consumer’s designee or agent (relative, friend, attorney, etc.). The Consumer must provide SFBHN with the written designation at the time of the appeal. The designation must be signed by the Consumer, or by the Consumer's guardian, if the Consumer is a minor. ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 106 - B. During the reconsideration process the decision to maintain the Consumer in the current level of care and receive ongoing services is made by the provider. IV. Participating Provider Appeal: Participating providers include professional and institutional providers. These appeals are made consistent with the participating provider's contractual obligations with SFBHN and are not done on behalf of the Consumer. V. How to initiate a request for a First Level Reconsiderations: A. A claimant who is dissatisfied with a denial may initiate a request for reconsideration. B. The claimant contacts the SFBHN UM staff person who issued the denial. C. The SFBHN UM staff person: 1. Requests that the Claimant submit additional written information (preferably via email) that was not available at the time of the initial UM review. 2. Notifies the Claimant of their rights, procedures and time frames for processing reconsiderations. VI. First Level Reconsiderations: A. First Level Reconsiderations involve the request and submission of additional written information that was not available to the UM staff person at the time of the UM review. First Level Reconsiderations should be scheduled by the UM staff person for presentation to the UM Committee no later than 30 working days after the request is received. 1. The UM Committee will review the additional information provided and determine if authorization for payment is indicated or to uphold the denial. 2. The decision of the UM Committee shall be transmitted in writing to the Claimant within 3 working days. 3. If a denial is upheld, all denial notifications shall include: a. The reasons for upholding the denial. b. A description and delineation of procedures for Second Level Reconsiderations. c. A list of titles and qualifications of individuals participating in the appeal review (participant names do not need to be included in the written notification to Claimants). B. Expedited First Level Reconsiderations should be scheduled by the UM staff person for presentation to the UM Committee no later than 3 working days after the request is received. 1. The UM Committee will review the additional information provided and make a determination if authorization for payment is indicated or to uphold the denial. 2. The decision of the UM Committee shall be transmitted in writing to the Claimant the day of the decision. 3. If a denial is upheld, all denial notifications shall include: a. The reasons for upholding the denial. b. A description and delineation of procedures for Second Level Reconsiderations. c. A list of titles and qualifications of individuals participating in the appeal review (participant names do not need to be included in the written notification to Claimants). VII. Second Level Reconsiderations: A. If a Claimant is dissatisfied with the UM Committee’s First Level Reconsideration decision, a written request for a Second Level Reconsideration can be submitted. This written request must be received by the UM Committee within 14 working days of notification of the First Level Reconsideration. ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 107 - B. Within 30 working days of receiving the written request for a Second Level Reconsideration, the UM Committee will arrange for a second opinion consultation of the consumer’s level of care and treatment needs. This evaluation may include examination of any available records and documents and consultation with provider staff, guardian or other interested parties. This evaluation shall be performed by a physician with specialization in the field in question and should not be an employee of SFBHN. C. The second opinion consultation report will be submitted to the UM Committee no later than 14 working days after it is requested. D. The UM Committee will review the results of the second opinion consultation and reconsider the recommendation for authorization for payment for services within 45 days of the receipt of the Claimant’s request for a Second Level Reconsideration. E. The decision of the UM Committee shall be transmitted in writing to the Claimant within 3 working days. F. All denial notifications shall include: 1. The reasons for upholding the denial. 2. A list of the title and qualifications of the individual participating in the appeal review (the consultant’s name does not need to be included in the written notification to Claimants). VIII. Grievance Protocols: A. SFBHN values the concerns of the complainant and offers a process by which to express and address complaints and concerns regarding subcontractor related issues, including the option to formally file a complaint. B. Should the complainant go through the reconsideration process and require the grievance protocols, the SFBHN grievance policy can be found on its website at: http://www.sfbhn.org/pdf/External%20Complaint-Grievance%20Policy.pdf. ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 108 - Passive Utilization Management ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 109 - Section: Passive Utilization Management Description & Limitations POLICY: SFBHN utilizes passive utilization management for all other cost centers not specified in other sections of this manual. SFBHN specifies the limitations associated by each cost center that SFBHN will reimburse the provider for. PURPOSE: To define cost centers which passive utilization management applies and describe limitations. PROCEDURE: I. II. III. IV. V. VI. Aftercare - Aftercare services, including but not limited to relapse prevention, are a vital part of recovery in every treatment level. Aftercare activities include client participation in daily activity functions that were adversely affected by mental illness and/or substance abuse impairments. New directional goals such as vocational education or re-building relationships are often priorities. Relapse prevention issues are key in assisting the client’s recognition of triggers and warning signs of regression. A. Limitations: 1. Individual -Maximum of 104 quarter-hour units, per recipient, per fiscal year 2. Group - Maximum of 156 quarter-hour units of group services, per recipient, per fiscal year Assessment - Assessment services assess, evaluate, and provide assistance to individuals and families to determine level of care, motivation, and the need for services and supports to assist individuals and families identify their strengths. A. Limitations: One bio-psychosocial evaluation, per recipient, per state fiscal year. Crisis Support/Emergency - These acute care services, on a twenty-four (24) hours per day, seven (7) days per week basis, provide brief, intensive mental health residential treatment services. These services meet the needs of individuals who are experiencing an acute crisis and who, in the absence of a suitable alternative, would require hospitalization. A. Day/Night - Day-Night services provide a structured schedule of non-residential services for four (4) or more consecutive hours per day. Activities for children and adult mental health programs are designed to assist individuals to attain skills and behaviors needed to function successfully in living, learning, work, and social environments. Generally, a person receives three (3) or more services a week. Activities for substance abuse programs emphasize rehabilitation, treatment, and education services, using multidisciplinary teams to provide integrated programs of academic, therapeutic, and family services. A. Limitations: Maximum of 190-hour units, per recipient, per fiscal year In-Home and On-Site - Therapeutic services and supports are rendered in non-provider settings such as nursing homes, alternative living facilities (ALF), residences, school, detention centers, commitment settings, foster homes, and other community settings. A. Limitations: Maximum combined limit of a total of 36, 15-minute units per month, per recipient, per fiscal year. Intervention - Intervention services focus on reducing risk factors generally associated with the progression of substance abuse and mental health problems. Intervention is accomplished through early identification of persons at risk, performing basic individual assessments, and providing supportive services, which emphasize short-term counseling and referral. These services are targeted toward individuals and families. A. Limitations: ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 110 - VII. VIII. 1. Individual -Maximum of 104 quarter-hour units, per recipient, per fiscal year 2. Group - Maximum of 156 quarter-hour units of group services, per recipient, per fiscal year Medical Services - Medical services provide primary medical care, therapy, and medication administration to improve the functioning or prevent further deterioration of persons with mental health or substance abuse problems. Included is psychiatric mental status assessment. For adults with mental illness, medical services are usually provided on a regular schedule, with arrangements for non-scheduled visits during times of increased stress or crisis. This service includes medication administration of psychotropic drugs, including new medications, and psychiatric services. A. Limitations: 1. Medication Management - As medically necessary 2. Medical Therapy – Maximum of 16 quarter-hour units of brief individual medical psychotherapy, per recipient, per fiscal year Outpatient - Outpatient services provide a therapeutic environment, which is designed to improve the functioning or prevent further deterioration of persons with mental health and/or substance abuse problems. These services are usually provided on a regularly scheduled basis by appointment, with arrangements made for non-scheduled visits during times of increased stress or crisis. Outpatient services may be provided to an individual or in a group setting. The group size limitations applicable to the Medicaid program shall apply to all Outpatient services funded through a state substance abuse and mental health program contract. A. Limitations: 1. Individual -Maximum of 104 quarter-hour units, per recipient, per fiscal year 2. Group - Maximum of 156 quarter-hour units of group services, per recipient, per fiscal year ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 111 - Forms ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 112 - Section: 28 Forms Data Sharing & Consent to Release and Exchange Information PATIENT AUTHORIZATION FORM FOR DISCLOSURE OF HEALTH INFORMATION ***PLEASE READ THE ENTIRE FORM, ALL THREE PAGES, BEFORE SIGNING BELOW*** Individual (name and information of person whose health information is being disclosed): Name (First Middle Last): Date of Birth (mm/dd/yyyy): Address: ____________________________City: State: ___________ Zip:_____________ You may use this form to allow full or limited access to and use of your health information by certain persons for certain purposes. Your choice on whether to sign this form will not affect your ability to get medical treatment, payment for medical treatment, or health insurance enrollment or eligibility for benefits. By signing this form, I voluntarily authorize, give my permission, and allow use and disclosure (including paper, oral and electronic interchange): OF WHAT: (initial one) ALL MY HEALTH INFORMATION including information about sensitive conditions (if any). Health information includes, but is not limited to, all records and other information regarding my health history, treatment, hospitalization, tests, residential and outpatient care. This includes my specific permission to release any and all of the following information: a. Drug, alcohol, or substance abuse b. Psychological, psychiatric or other mental impairment(s) or developmental disabilities (excludes “psychotherapy notes” as defined in HIPAA at 45 CFR 164.501) c. Sickle cell anemia d. Birth control and family planning e. Records which may indicate the presence of a communicable disease or noncommunicable disease; and tests for or records of HIV/AIDS or sexually transmitted diseases or tuberculosis f. Genetic (inherited) diseases or tests ONLY THE INFORMATION INDICATED BELOW (initial next to all that you want disclosed): History and Physical Operation Reports Discharge Summary Radiology Reports & Images Pathology Reports EKG Reports Progress Notes Consultation Reports Lab Results Physician’s Orders Drug, Alcohol or Substance Abuse Records Family Planning Records Prenatal Records Mental Health Records (excluding “psychotherapy notes” as defined in HIPAA at 45 CFR 164.501) Diagnostic Test Reports (specify type of test): Other (please specify): Note: Information created before or after the date of this form may be disclosed, unless you specify a date range of records here: From (mm/dd/yyyy): To (mm/dd/yyyy) : . ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 113 - FROM WHOM: (choose one) All information sources, including but not limited to medical and clinical sources (hospitals, clinics, labs, pharmacies, physicians, psychologists, etc.) including mental health, correctional, addiction treatment, Veterans Affairs health care facilities, state registries and other state programs, social workers, rehabilitation counselors, insurance companies, health plans, health maintenance organizations, employers, pharmacy benefit managers, worker’s compensation programs, state Medicaid, Medicare and any other governmental program. Only the following specific sources of my health information: Person/Organization Name: Phone: ( ) Address: Fax: ( ) Person/Organization Name: Phone: ( ) Address: Fax: ( ) Person/Organization Name: Phone: ( ) Address: Fax: ( ) Person/Organization Name: Phone: ( ) Address: Fax: ( ) Person/Organization Name: Phone: ( ) Address: _ _ __ _ _ _ _ _ __ _ _ _ _ _ Fax: ( ) TO WHOM: (check one) South Florida Behavioral Health Network and its service providers listed in Attachment I. Specific person(s) or organization(s) permitted to receive my information: Person/Organization Name: Address: Person/Organization Name: Address: Person/Organization Name: Address: Person/Organization Name: Address: Person/Organization Name: Address: Person/Organization Name: Address: Phone: ( Fax: Phone: Fax: Phone: Fax: Phone: Fax: Phone: Fax: Phone: Fax: ( ) ( ( ( ( ( ( ( ( ( ( ) ) ) ) ) ) ) ) ) ) ) PURPOSE: (select full or limited) Full Access: To provide me with medical treatment and related services and products, and to evaluate and improve patient safety and the quality of medical care provided to all patients. By selecting this option, you are also authorizing the use of your personal information for aggregated data reporting purposes. Your personal information, along with data from other patients/consumers, may be used to create non-identifiable aggregate data such as reports, and as part of group statistical research and analysis. The research and analysis will not contain any information that could be used to contact or identify you. Or Limited Access (check all that apply) My medical treatment and related services and products To evaluate and improve patient safety and the quality of medical care provided to all patients Payment (as defined in HIPAA at 45 CFR 164.501) Eligibility for certain health care services (e.g., hospice)(please specify: Eligibility for clinical trials (if limited, please specify here: Scientific research with proper Institutional Review Board approval or waiver Personal Health Record for my use Personal use ) ) ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 114 - Other, please specify: EFFECTIVE PERIOD: This authorization/permission form will remain in effect until (check one): The day I withdraw my permission or the date of my death A specific date (mm/dd/yyyy): A specific event. Please specify: REVOKING YOUR PERMISSION: I can revoke my permission at any time by giving written notice to the person or organization to whom I originally gave this form. In addition: I authorize the use of a copy (including electronic copy) of this form for the disclosure of the information described above. I understand that there are some circumstances in which this information may be redisclosed to other parties (see page 4 for details). I understand that refusing to sign this form does not stop disclosure of my health information that is otherwise permitted by law without my specific authorization or permission. I have read all pages of this form and agree to the disclosures above from the types of sources listed. X Signature of Patient or Patient’s Legal Representative Date Signed (mm/dd/yyyy) Print Name of Legal Representative (if applicable) Check one to describe the relationship of Legal Representative to Patient (if applicable): Parent of minor Guardian Other personal representative (explain: ) This form is invalid if modified. You are entitled to get a copy of this form after you sign it. ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 115 - Explanation of “Patient Authorization Form for Disclosure of Health Information” Laws and regulations require that some sources of personal information have a signed authorization or permission form before releasing it. Also, some laws require specific authorization for the release of information about certain conditions. Definitions: In this form, the term “treatment,” “healthcare operations,” “psychotherapy notes,” and “protected health information” are as defined in HIPAA (45 CFR 164.501). Note on Mental Health Records: If you are requesting a copy of your mental health records with this form, Florida allows such access, unless such access is determined by your physician to be harmful to you. For more information, see Florida Statute 394.4615(10). “To Whom”: If you specified a healthcare provider in the “TO WHOM” section above, this permission would also include physicians, other health care providers (such as nurses) and medical staff who are involved in your medical care at that organization’s facility or that person’s office, and health care providers who are covering or on call for the specified person or organization, and staff members or agents (such as business associates or qualified services organizations) who carry out activities and purpose(s) permitted by this form for that organization or person that you specified. If you specified an organization other than a healthcare provider in the “TO WHOM” section above, this permission would also include that organization’s staff or agents and subcontractors who carry out activities and purpose(s) permitted by this form for that organization that you specified. Revocation: You have the right to revoke this authorization and withdraw your permission at any time regarding future uses by giving written notice. You should understand that organizations that had your permission to access your health information may copy or include your information in their own records. These organizations, in many circumstances, are not required to return any information that they were provided nor are they required to remove it from their own records. Re-disclosure of Information: Any health information about you may be re-disclosed to others only to the extent permitted by state and federal laws and regulations. You understand that once your information is disclosed, it may be subject to lawful re-disclosure, in accordance with applicable state and federal law, and in some cases, may no longer be protected by federal privacy law. Limitations of this Form: This form does not obligate your health care provider or other person/organization listed in the “From Whom” or “To Whom” section to seek out the information you specified in the “Of What” section from other sources. ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 116 - Attachment I South Florida Behavioral Health Network Providers: Banyan Community Health Foundation, Inc. Key West HMA LLC (d.b.a.) Lower Keys Medical Center Better Way of Miami, Inc. King David Foundation, Inc./CLAPA Camillus House, Inc. Kristi House, Inc. Carrfour Supportive Housing Inc. MDC-Community Action and Human Services Dept. (MDC-CAHSD) Catholic Charities of The Archdiocese of Miami, Inc. Miami-Dade County Juvenile Services Department (MD-JSD) Citrus Health Network, Inc. Miami-Dade Homeless Trust (MDHT) Community AIDS Resource, Inc. (d.b.a.) CARE Resource Monroe County Coalition, Inc. Community Health of South Florida Inc. (CHI) New Hope C.O.R.P.S., Inc. Comprehensive Treatment Centers of South Florida, Inc. (CTC) New Hope Drop-In Center, Inc. Concept Health Systems, Inc. New Horizons Community Mental Health Center, Inc. Douglas Gardens Community Mental Health Center of Miami Beach, Inc. Non-Violence Project USA Drug Free Youth In Town (DFYIT) Our Children, Our Future, Inc. Family & Children Faith Coalition, Inc. Passageway Residence of Dade County, Inc. Family Counseling Services of Greater Miami, Inc. (FCS) Psychosocial Rehabilitation Center, Inc., d.b.a, Fellowship House Family Resource Center of South Florida, Inc. Public Treat of Miami-Dade County d.b.a Jackson Health Systems (JHS) Federation of Families/ Miami-Dade Chapter, Inc. Recapturing the Vision, International, Inc. (RTV) Florida International University (FACES Consulting Contract) Regis House, Inc. Fresh Start of Miami-Dade, Inc. Sembrando Flores, Inc. Gang Alternative, Inc. South Florida Jail Ministries, Inc. (d.b.a.) Agape Family Ministries Guidance Care Center, Inc. (GCC) Switchboard of Miami, Inc. Guidance Care Center, Inc. (GCC) Emergency Contract The Abriendo Puertas Governing Board of East Little Havana, Inc. Here's Help, Inc. The Center for Family and Child Enrichment, Inc. (CFCE) Human Services Associates (HAS) The Key Clubhouse of South Florida, Inc. Hosanna Community Foundation, Inc. The Miami Coalition For a Safe and Drug-Free Community, Inc. Institute for Child and Family Health, Inc. (ICFH) The Village South, Inc. /The Miami Beach Coalition Informed Families, The Florida Partnership Volunteers of America of Florida, Inc. Jessie Trice Community Health Center, Inc. ______________________________________________________________________________________________________________________ Date Approved: Date Modified: 09-30-2013 - 117 -