Copyright form
advertisement

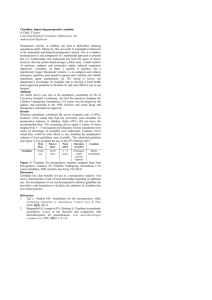
Login | Users Home | About us | Editorial board | Ahead of print | Search | Current Issue | Archives | Submit article | Instruction Contacts Search ARTICLE Volume : 7 | Issue : 1 | Page : 29-33 n with clonidine versus fentanyl for intraoperative hemodynamic stability and recovery outcome during holecystectomy under general anesthesia ta1, Mahima Lakhanpal1, Prashant K Gupta2, Atul Krishan3, Bhawna Rastogi1, Vaibhav Tiwari1 of Anaesthesiology and Critical Care, N.S.C.B. Subharti Medical College, Swami Vivekananda Subharti ubhartipuram, NH-58, Meerut, Uttar Pradesh, India of Radio diagnosis, Imaging and Interventional Radiology, N.S.C.B. Subharti Medical College, Swami Subharti University, Subhartipuram, NH-58, Meerut, Uttar Pradesh, India of Surgery, N.S.C.B. Subharti Medical College, Swami Vivekananda Subharti University, Subhartipuram, ut, Uttar Pradesh, India Publication 26-Jun-2013 nce Address: ta apuri, Shastri Nagar, Meerut - 250 004, Uttar Pradesh /0259-1162.113984 Similar in PUB Search Pu Gupta K Lakhanpa Gupta PK Krishan A Rastogi B Tiwari V Search in Scholar for Gupta K Lakhanpa Gupta PK Krishan A Rastogi B Tiwari V ct Laparoscopic cholecystectomy under general anesthesia induced intraoperative hemodynamic responses be attenuated by appropriate premedication. The present study was aimed to compare the clinical efficacy nd fentanyl premedication during laparoscopic cholecystectomy for attenuation of hemodynamic responses ative recovery outcome. Methods : In this prospective randomized double blind study 64 adult consented patients of either sex with scheduled for elective laparoscopic cholecystectomy under general anesthesia and met the inclusion allocated into two groups of 32 patients. Group C patients have received intravenous clonidine 1μg kg -1 patients have received intravenous fentanyl 2μg kg -1 5 min before induction. Anesthetic and surgical re standardized. All patients were assessed for intraoperative hemodynamic changes at specific time and recovery outcome. medication with clonidine or fentanyl has attenuated the hemodynamic responses of laryngoscopy and Clonidine was superior to fentanyl for intraoperative hemodynamic stability. No significant differences in ive recovery outcome were observed between the groups. Nausea, vomiting, shivering and respiratory re comparable between groups. Premedication with clonidine or fentanyl has effectively attenuated the intraoperative hemodynamic aparoscopic cholecystectomy. Related art Clonidine fentanyl hemodyna laparosco cholecyst laryngosc pneumope Access Statisti Email Alert * Add to My Lis * Registration re lonidine, fentanyl, hemodynamic response, laparoscopic cholecystectomy, laryngoscopy, neum his article: hanpal M, Gupta PK, Krishan A, Rastogi B, Tiwari V. Premedication with clonidine versus fentanyl for hemodynamic stability and recovery outcome during laparoscopic cholecystectomy under general nesth Essays Res 2013;7:29-33 his URL: hanpal M, Gupta PK, Krishan A, Rastogi B, Tiwari V. Premedication with clonidine versus fentanyl for hemodynamic stability and recovery outcome during laparoscopic cholecystectomy under general nesth Essays Res [serial online] 2013 [cited 2014 Aug 8];7:29-33. Available www.aeronline.org/text.asp?2013/7/1/29/113984 ction cholecystectomy provides substantial advantages of less postoperative pain with fewer pulmonary and more rapid convalescence. However the procedure is not risk free and insufflation of the abdominal rbon dioxide causes increased intra-abdominal pressure which predictably leads to increased hemodynamic In this article Abstract Introductio Results Discussion Conclusio Subjects a Reference The potential problem of hemodynamic response of pneumoperitoneum during laparoscopic surgery does al preoperative and intraoperative anesthetic care of patients. [2] Various pharmacological agents like , beta blocker and opioids were used during anesthesia to provide hemodynamic stability during and laparoscopy but with their own limitations. [3],[4],[5] 2 adrenergic agonist, has shown clinically useful drug profile due to its sympatholytic, hypnotic, sedative, algesic and anesthetic sparing effects without respiratory depression. [6],[7] In recent studies clonidine has tion of the pressor responses associated with laryngoscopy by reducing norepinephrine release. udy was aimed to compare the clinical efficacy of premedication with clonidine versus fentanyl for intraodynamic stability and postoperative recovery variables during laparoscopic cholecystectomy under esia. s and Methods l of Institutional Ethical Committee and written informed consent, 64 healthy adult patients of ASA s I and II of either sex aged 32 to 57 years, scheduled for elective laparoscopic cholecystectomy under esia from August 2011 to April 2012 were enrolled for this double blind prospective randomized study. hypertension, history of cardiac, pulmonary or renal disease, psychiatric disorder, and any drug therapy of methyldopa, and monoamine oxidase (MAO) inhibitors were excluded from the study. Other exclusion body mass index >25 and anticipated difficult airway. All patients were evaluated during pre-anesthesia e enrollment. Drug preparation was done by the resident anesthesiologist who was blinded to the n schedule and the study protocol. The observer was also blinded about the group allocations and hedule. p allocation was done by computer generated code based on a two way randomization. Group C patients (n0 d intravenous clonidine 1 μg kg -1 and Group F patients (n = 32) received fentanyl 2 μg kg -1 given over 10 to induction of general anesthesia. These doses were considered appropriate to provide adequate and inical effects. ere premedicated with oral alprazolam 0.25 mg and ranididine 150 mg night before surgery. On the day of eceived premedication of glycopyrrolate 0.2 mg intramuscularly 30 min prior to induction of anesthesia. operation room routine hemodynamic monitoring of base line heart rate, systemic arterial pressure, arterial tion (SpO 2 ), continuous ECG was performed. An intravenous infusion of ringer lactate was started in non. The premedication of clonidine 1 μg kg -1 or fentanyl 2 μg kg -1 was given over 10 minutes and 5 minutes ion according to group allocation. After premedication heart rate, arterial blood pressure, respiratory rate turation were assessed and recorded. ere given metoclopramide 10 mg and midazolam 2 mg intravenously and after preoxygenation for 3 min, was induced with propofol 2 mg kg -1 and tracheal intubation was facilitated by vecuronium 0.1mg kg -1 . as maintained with isoflurane 1-1.5% and 60% nitrous oxide in oxygen with supplementary fentanyl (50intain the heart rate and mean arterial pressure within 20% of preinduction values. The patient's lungs were ated with a tidal volume of 8 ml.kg -1 , a respiratory rate of 12 breaths per minutes, and I:E ratio of 1:2 in olled mode. Five minutes after securing the airway and abdominal insufflation, the lung mechanics were Article Fi Article Ta Article Access S Viewed Printed Emailed PDF Download Comments aintain normocapnia (EtCO2 between 35-40 mm Hg). Vecuronium 0.05 mg.kg-1 was administered during uired to maintain a train of four ratio of <25%. neum was created and maintained by insufflation of carbon dioxide. The table was tilted to about 15 o delenburg position with left side rotation to facilitate exposure of the gall bladder. Intra-abdominal pressure d between 12-15 mm Hg during the surgery. At the end of surgery, the surgeon administered 10 ml 75% in the peritoneum through the main trocar, the isoflurane and nitrous oxide were discontinued and muscular block was antagonized with neostigmine (0.05 mg kg -1 ) and atropine (0.02 mg kg -1 ). The xtubated when respiration was adequate in tidal volume and patient was able to obey simple commands. ere assessed for changes in hemodynamic parameters of heart rate and mean arterial pressure prior to , before induction, after laryngoscopy and intubation, after pneumoperitoneum, followed by every 5 min reafter every 15 min till end of surgery and after extubation. Criteria for tachycardia, bradycardia, nd hypertension were any increase or decrease more than 20% from the baseline. The intraoperative r tachycardia, hypotension or hypertension and any untoward incident requiring intervention was recorded accordingly. were transferred to post anesthesia care unit and were monitored for any hemodynamic abnormalities, pression (respiratory rate < 8 breaths/min) or hypoxemia (SpO 2 < 94%), shivering, nausea and vomiting aged as required. was based on initial pilot observation which indicated that approximately 23 to 27 patients per group were ure power 0.80 for detecting clinically meaningful reduction by 20% in heart rate and mean arterial uming a 5% dropout rate, the final sample size was set at 64 patients. The results obtained in the study are Mean ± SD in tabulated manner and Statistical analysis was done with SPSS software for windows using and Chi square test. P < 0.05 was considered statistically significant and P < 0.001 was taken as highly patients were randomly assigned to two groups of 32 patients each. Both groups were comparable with mographic and operational factors. No significant differences were found with respect to age, weight, etween premedication to anesthetic induction, duration of laryngoscopy and surgical procedure. The hnique did not differ among the study groups [Table 1]. Table 1: Demographic profile of patients Click here to view significant difference in the mean heart rate and arterial blood pressure values between groups before . Though after induction, the hemodynamics was stable in both groups but heart rate increased immediately copy in fentanyl group and maximum increase was observed after 1 min of laryngoscopy whereas no such observed in heart rate in clonidine group. It remained stabilized during intraoperative period in comparison oup [Table 2]. Table 2: Mean heart rate changes during laparoscopic cholecystectomy Click here to view difference was observed in the mean arterial pressure (MAP) before and after premedication in both tenuation of mean arterial blood pressure was observed in both groups. Clonidine group has shown more stability of hemodynamic response during pneumoperitoneum [Table 3]. Hemodynamic variables recorded mings during the study are shown in [Figure 1] and [Figure 2]. Figure 1: Showing changes in mean arterial blood pressure during laparoscopic cholecystectomy Click here to view Figure 2: Showing changes in heart rate during laparoscopic cholecystectomy Click here to view Table 3: Mean arterial blood pressure changes during laparoscopic cholecystectomy Click here to view raoperative period, heart rate and mean arterial blood pressure values were close to preoperative values ement of any other medication and remained stabilized throughout the surgery. Rapid intravenous infusion 5 patients of Group C to treat hypotension. None of the patients had persistent or severe hypotension intrahus vasoactive drugs were not used. o significant differences between groups with respect to awakening and recovery times. All patients were and able to obey verbal commands in postoperative care unit. The premedication with fentanyl allows ve recovery [Table 4]. Table 4: Recovery outcome from general anesthesia after premedication Click here to view undesirable adverse events were comparable between groups and were manageable. The postoperative miting were found in both groups and was treated with ondansetron. Eleven patients (35.2%) of fentanyl e patients (7%) of clonidine group needed tramadol 50 mg for postoperative shivering. Bradycardia of 7 reated with intravenous atropine. No significant complication has occurred after use of intravenous of clonidine or fentanyl in our study [Table 5]. Table 5: Postoperative adverse events after laparoscopic cholecystectomy Click here to view sion udy has evaluated the efficacy of intravenous premedication of clonidine versus fentanyl for intraoperative stability during laparoscopic cholecystectomy under general anesthesia. The hemodynamic pressor attenuated by clonidine and fentanyl effectively. The premedication with clonidine showed more hemodynamic stability as compared to fentanyl premedication. Near stable hemodynamic values in the was an indication of adequate analgesia and sedation with clonidine or fentanyl premedication. 2 adrenergic agonist, possesses several properties such as sedation, analgesia, bradycardia and hypotension aluable premedicant to attenuate the hemodynamic response without any deleterious effect. The results of our study were in agreement with recent studies with clonidine and fentanyl. [8],[9],[10],[11] e first described the hemodynamic response to laryngoscopy and intubation due to intense sympathetic used by stimulation of larynx. [12] These hemodynamic responses can be detrimental in elderly and ally compromised patients due to associated risk of myocardial ischemia or cerebral hemorrhage, therefore e attenuated. [13],[14],[15] Many pharmacological methods were evaluated either in premedication or during ttenuate these adverse hemodynamic responses with controversial results. The most important premedicants e, esmolol, sodium nitroprusside and opioids. [3],[4],[16] Moreover numerous techniques have also been used severity of the hemodynamic responses of laparoscopic surgery to counteract its detrimental effects. been used as anesthetic adjuvant during balanced anesthetic regimen. Its anesthetic sparing effects are well he clonidine premedication attenuates the intraoperative hemodynamic response by reducing the ansmission and decrease norepinephrine concentration in serum. In our study, clonidine 1 μg/kg given has attenuated the hemodynamic response of laryngoscopy and laparoscopy effectively. s with oral clonidine (150 μg) given 90 minutes before induction of general anesthesia have shown the modynamic response during laparoscopic surgery. Hayashi, et al. [9] and Sung, et al. [17] have concluded that vided perioperative hemodynamic stability during laparoscopic cholecystectomy. Laisalmi, et al. [18] has hat clonidine premedication blunts the stress response of surgery and reduces the requirement of narcotics agent. study, clonidine has caused intraoperative and postoperative bradycardia and subsequent use of atropine, t an anticholinergic drug should be used routinely as premedicants. Salivary and tracheobronchial mucus her necessitates prophylactic administration of an antisialagogue agent. Thus, glycopyrrolate was the ce in the present study. of nausea and vomiting after general anesthesia has been reported to be as high as 24% and after is as high as 42% due to rapid peritoneal distension. Metoclopramide has been shown to be effective and c for both prevention and treatment of nausea and vomiting. [19] In the present study, the metoclopramide emedication as it increases the tone of lower esophageal sphincter and speeds gastric emptying. Decreased ostoperative nausea and vomiting were found in the present study. m of shivering in patients recovering from anesthesia though poorly understood, but volatile anesthetic ally associated with altered temperature regulation. Regardless of its cause, shivering increases oxygen hence postoperative supplemental oxygen therapy helped to prevent hypoxemia. Clonidine group patients ased incidence of postoperative shivering when compared to fentanyl group. [20] o plays a significant role in the treatment of hypertension, delirious syndrome and withdrawal syndromes of ol and nicotine addiction. It is also used in intensive care units to facilitate weaning from long term ntilation. [21],[22] sion n with intravenous Clonidine or Fentanyl have effectively attenuated the hemodynamic responses during holecystectomy under general anesthesia. Postoperative undesirable adverse events were comparable and The intraoperative hemodynamic stability with clonidine or fentanyl premedication might enable holecystectomy in obese, hypertensive and cardiac compromised patients. nces gham AJ, Brull SJ. Laparoscopic cholecystectomy: Anesthetic implications. Anesth Analg 1993;76:1120- Anaesthesia for laparoscopic surgery. In: Miller RD. editor. Anesthesia. 7 th ed. New York: Churchill tone; 2010. p. 2185-202. , Vichitvejpaisal P, Gaines GY, White PF. Comparative effects of lidocaine, esmolol, and nitroglycerin in ng the hemodynamic response to laryngoscopy and intubation. J Clin Anesth 1995;7:5-8. KS, Sinatra RS, Halevy JD, Paige D, Silverman DG. A comparison of fentanyl, esmolol, and their ation for blunting the haemodynamic responses during rapid-sequence induction. Can J Anaesth :774-9. A, Fanelli G, Albertin A, Deni F, Danelli G, Grifoni F, et al. Small doses of remifentanil or sufentanil for g cardiovascular changes induced by tracheal intubation: A double-blind comparison. Eur J Anaesthesiol :108-12. M, Gehling M. Clonidine: A potent analgesic adjuvant. Curr Opin Anaesthesiol 2002;15:511-7. rkhana S, Gopal S. Clonidine in adults as a sedative agent in the intensive care unit. J Anaesthesiol Clin col 2010;26:439-45. ED] DC, Komal SS, Dubey SR, Doshi SM, Rawal PV. Hemodynamic stress response during laparoscopic stectomy: Effect of two different doses of intravenous clonidine premedication. J Anesth Clin Phar :475-80. y D, Manjushree R, Gauri M. Hemodynamic changes during laparoscopy cholecystectomy: Effect of oral e premedication. Ind J Anesth 2007;51:143-7. , Hoffman WE, Stechert MM, Hoffman IW, Ananda RC. Fentanyl or dexmedetomidine combined with ne for bariatric surgery. J Clin Anesth 2006;18:24-8. DE, Rosenberg H, Aukburg SJ, Bartkowski RR, Edwards MW Jr, Greenhow DE, et al. Low-dose fentanyl irculatory responses to tracheal intubation. Anesth Analg 1982;61:680-4. C, Brace DE. Irritation of the respiratory tract and its reflex effect on heart. Surg Gynae Obstet 1940;70:157- an AJ, Smith G, Achola KJ. Cardiovascular and catecholamine responses to laryngoscopy with and without intubation. Br J Anaesth 1987;59:295-9. M, Singh V, Kumar A, Wahal R, Bhatia VK. A study of cardiovascular response during laryngoscopy and on and their attenuation by ultra-short acting beta-blocker esmolol. Ind J Anaesth 2002;46:104-6. , Chiche JD, Canivet JL, Jacquet NJ, Legros JJ, Lamy ML. Hemodynamic changes induced by laparoscopy r endocrine correlates: Effects of clonidine. J Am Coll Cardiol 1998;32:1389-96. , Sakai T, Takahashi S, Matsuki A. Haemodynamic and electroencephalograph responses to intubation nduction with propofol or propofol/fentanyl. Can J Anaesth 1998;45:19-22. S, Lin SH, Chan KH, Chang WK, Chow LH, Lee TY. Effect of oral clonidine premedication on rative hemodynamic response and postoperative analgesic requirement for patients undergoing laparoscopic stectomy. Acta Anaesthesiol Sin 2000;38:23-9. i M, Koivusalo AM, Valta P, Tikkanen I, Lindgren L. Clonidine provides opioid-sparing effect, stable namics, and renal integrity during laparoscopic cholecystectomy. Surg Endosc 2001;15:1331-5. EB, Bass CS, Abrameit W, Roberson R, Smith RW. Metoclopramide versus ondansetron in prophylaxis of and vomiting for laparoscopic cholecystectomy. Surg Endosc 2001;15:1331-5. u G, Chen AA, Jonton CE, Kenny GP, Bristow GK, Giesbrecht GG. Clonidine decrease vasoconstriction vering threshold without affecting the sweating threshold. Can J Anaesth 1997;44:636-42. amashiro M, Furuya H. Clonidine as a drug for intravenous conscious sedation. Odontology 2002;90:57- M, Fairbairn J, McDonald K, Zvonar R, Cardinal P. Clonidine use in the intensive care unit of a tertiary pital: Retrospective analysis. Can J Hosp Pharm 2004;57:83-9. Figure 2] able 2], [Table 3], [Table 4], [Table 5] Sitemap | What's New | Feedback | Disclaimer © Anesthesia: Essays and Researches | Published by Medknow Online since 1st June, 2010