Implementing a Smoke-Free Environment in Mental Health Services
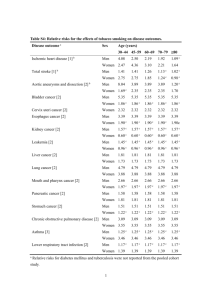
advertisement

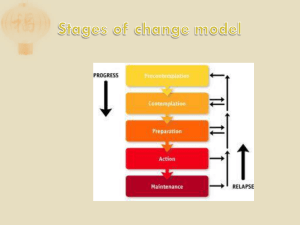
IMPLEMENTING A SMOKE-FREE ENVIRONMENT IN MENTAL HEALTH SERVICES July 2004 For more information, contact: Sonja Goldsack Mental Health Commission (04) 917 8922 sgoldsack@mhc.govt.nz LETTER TO DISTRICT HEALTH BOARDS The introduction of the Amendment to the Smoke-free Environments Act 1990 on August 1st 2004 has implications for District Health Boards, not least of these being the effect on Mental Health Acute Inpatient Units. Some DHBs have asked for the Commission’s views on implementing a smoke-free environment in acute inpatient units. The Mental Health Commission is fully committed to an eventual smoke-free environment within mental health services, with recent evidence suggesting that the incidence of smoking amongst service users remains at unacceptably high levels. However issues surrounding implementation of a smoking ban are wide-ranging and complex. In this respect, the Mental Health Commission’s position is as follows: Exemptions under the Smoke-free Amendments Act 2003 should be used by all acute inpatient services. Acute services provide care and treatment for individuals in acute states of unwellness and vulnerability. Clinically, this is neither the time nor the environment for smoking cessation to be imposed. While all efforts to introduce a smoke-free environment in mental health services are encouraged, the dignity, rights and safety of service users are paramount. All attempts to change smoking behaviour should have service users as leaders and participants in the process. Mental health services need to remove institutional inducements to smoke including the distribution and use of tobacco products as rewards, prizes or tools of control and privilege or behaviour management. This practice is particularly prevalent in acute inpatient units. DHBs must work to close the gap between rates of smoking for service users and the general population. The basis for this position is attached in this paper. In October 2004, the Commission will be following up on DHB responses to the introduction of the Smoke-free Amendments Act. Sonja Goldsack (Advisor, Service User Issues) is available for comment, advice and information on the issues outlined in this paper. Sonja is available on 04 917 8922 or at sgoldsack@mhc.govt.nz. Yours sincerely Jan Dowland Chair IMPLEMENTING A SMOKE-FREE ENVIRONMENT IN MENTAL HEALTH SERVICES INTRODUCTION An amendment to the Smoke-free Environments Act 1990 comes into effect on 1st August 2004. The purpose of the Act (1990) as amended is “to prevent the detrimental effect of other people’s smoking on the health of people in workplaces, or in certain public enclosed areas, who do not smoke or do not wish to smoke there”1 The purpose therefore, is primarily to prevent the detrimental effect on non-smoking individuals and workers, rather than an express purpose to make services smoke-free. Acute services are therefore required to become smoke-free. However, in recognition of the specific needs of individuals in these services, the use of a “dedicated smoking room” is permitted. Strict requirements must be met if this option is to be used. Smoking is only permitted where: (a) the smoking takes place only in one or more dedicated smoking rooms; and (b) each dedicated smoking room is equipped with or connected to a mechanical ventilation system that takes air from the room to a place outside the workplace; and (c) all reasonably practical steps are taken to minimise the escape of smoke from the dedicated smoking rooms into any part of the workplace that is not a dedicated smoking room; and (d) for each dedicated smoking room, there is available for patients and residents who wish to socialise in a smoke-free atmosphere an adequate equivalent room2. Therefore, hospitals, rest homes and residential care institutions may ban smoking, but where they choose to allow smoking, only patients or residents (not staff, volunteers, or members of the public) may smoke in a dedicated smoking room. While the amendment to the Smoke-free Environments Act allows for the use of a dedicated smoking room within inpatient units and mental health residential units, most other mental health services will be required to be smoke-free. There are several key stakeholder views to be taken into account in discussing the impact of the Amendment on acute inpatient units. These include: service users staff working within acute inpatient units managers. International evidence shows that smoking for service users remains one of the highest clinical risk factors relating to poor physical health3,4. This, alongside evidence suggesting that physical ill health is commonplace for most mental health service users, should be 1 Smoke-free Environments Act Amendment 2003 2 Smoke-free Environments Act Amendment 2003 s6 3 Lasser, K et al. (2000) Smoking and Mental Illness. A population based prevalence study. Journal of the American Medical Association Vol284; 4 Mental Health Commission (2004) Our physical health… who cares? Occasional Paper No.5. Wellington, New Zealand. sufficient reason for mental health services to commit to smoking reduction within their services. However, nicotine is a highly addictive drug and cessation brings with it significant personal and clinical issues which need to be considered before any action is taken on smoke-free initiatives. THE ISSUES Clinical implications International literature reports a clear differential in the uptake of some drugs, in particular antipsychotics, during a reduction in smoking5,6. Abrupt withdrawal will affect therapeutic doses almost immediately, with increased agitation also likely to occur as a result. In services where people are acutely unwell, both nicotine reduction and cessation would need to be carefully managed to ensure that individuals are not subject to ineffective or potentially dangerous drug regimes. In order to work within the bounds of clinical accountability, staff working with service users must have a full and thorough appreciation of, and education on, the clinical issues around smoking cessation and its effects on individuals. International advice suggests that cessation treatment “should not be offered when the mental illness is florid or very active”7. Addiction behaviours often increase during times of stress and it would be unreasonable for inpatient or acute care units to expect any form of smoking cessation during the initial stages of a person’s admission. The signs and behaviours of nicotine withdrawal often are similar to, and can mirror, the symptoms of psychiatric illness, giving rise to complication of diagnosis, medication prescribing and symptom observation. Smoking as a coping strategy Service users in acute services are often in vulnerable and stressed states where there are strong demands and challenges to individuals’ coping strategies. At this time, smoking cessation is an unnecessary additional stressor, which could further burden coping strategies. For many service users, smoking itself is a coping strategy. Attempts to cease smoking would possibly further worsen what, for many, is already a traumatising experience. Practices encouraging smoking Often practices within mental health services both passively and actively encourage smoking. The practice of staff handing out cigarettes on the hour (a practice used in many inpatient units, particularly intensive care units) reinforces the belief that smoking is a privilege and something to be desired. The use of cigarettes as prizes or rewards within some residential units not only further supports this belief, but also does little to promote healthy practices within mental health services. Often this leads to the initiation of smoking for those who entered the service as non-smokers, along with increased rates of smoking by those who are ongoing smokers. An identification of these practices and their immediate cessation is the first and most important step in providing an environment that discourages smoking. A DHB 5 Symposium Report on Smoking and Mental Health (2001) London, Pg 22 6 Nicotine interacts with nicotinic receptors on nerves throughout the body and brain. Chronic nicotine use causes inactivation of the receptors causing a subsequent increase in their number and leading to an increased number of high affinity nicotinic receptors. Consequently, nicotine use affects the release of different neurotransmitters, including acetylcholine, dopamine, norepinephrine (or noradrenaline), serotonin (5-HT), glutamate and aminobutyric acid (GABA). Whitireia Community Polytechnic (2004) Psychopharmacology. A Handbook for New Zealand Health Professionals, Wellington, NZ 7 Symposium Report on Smoking and Mental Health (2001) London whose practices within mental health services both foster and encourage smoking amongst service users and who also runs a public health smoke-free campaign is at odds with itself. Smoking and socialising Service users tend to smoke more than the general population across most diagnoses. Evidence suggests that the inpatient unit, as well as other service environments, are often major contributors to high levels of service user smoking8. Smoking often plays a large role in the social interactions of clients within these units where “if people went into hospital as nonsmokers, in all probability they would leave as smokers, literally because of peer pressure to smoke, the lack of other activities to occupy them while there, and reinforcement by the institution” 9. The smoking room of the acute inpatient unit and similar rooms in other mental health services are where many introductions and social interactions occur10,11. Inpatient units that offer little else in terms of entertainment, structure and activities often leave little alternative for clients who desire relief from the boredom of the ward and a platform for interaction with others. This leaves non-smokers more vulnerable to taking up smoking. The requirement of an equivalent room for non-smokers as outlined in section 6 of the Amendment is an acknowledgement of the need to provide a smoke-free room in which people can congregate and socialise. WORKING WITH SERVICE USERS AND STAFF TO CHANGE THE ENVIRONMENT Leading the change Some DHBs have employed staff specifically to oversee the implementation of a smoke-free environment in non-acute mental health services. This ensures that there is consistency in the implementation of tactics used as well as streamlining the delivery of training. Where this implementation is not led by service users, the staff involved in this implementation should be aware of issues around smoking cessation or reduction which are particular to service users. Where steering groups are used, they should include an appropriate representation of service users and consumer advisors, preferably as the leaders of this process. Reducing use of the smoking room Restricting access to the designated smoking room in all mental health services may be the first step in removing the attraction of smoking as a means of socialising, although this should be weighed up against the rights of the service users who may view these services as their current ‘home’. Slow, but sure introductions of closure have worked well in some services12. Successful ideas around reducing use might include: 1. Giving notice that a smoking room will be used only for limited hours, if at all. 2. Allowing only one person at a time. 3. Eventually closing the ‘smoking’ room altogether, with service users smoking outside where practicable. 8 Lawrie, S (1995) Cigarette Smoking in Psychiatric Units. Journal of the Royal Society of Medicine Vol 88, p59 9 McNeill, A (2001) Smoking and mental health – a review of the literature. Smokefree London Programme, United Kingdom. 10 Goldsack, S (2004) Advice to DHBs on Cessation of Smoking in Mental Health Service Acute Inpatient Units. Paper prepared for the Mental Health Commission. 11 Porter, S (2004) Service User Perspectives on the Proposal to Ban Smoking on all DHB Facilities and Grounds. Paper prepared for the Mental Health Commission. 12 McDonald, G (2004) Personal Communication, Wakari Hospital. Otago District Health Board. Staff need to be aware that there may be situations in the initial stage of the closure where the smoking room needs to be re-opened. Flexibility around this, particularly where the safety of either a service user or staff member is compromised, should be exercised. Changing the physical environment An outside smoking space accessible to all within the immediate area protects staff and nonsmokers from the effects of smoking and actively discourages smoking by reducing social interaction. The provision of an outdoor space for service users to smoke must ensure that the health of individuals is not compromised. The area provided should be secure and protected from bad weather, and not directly in the space of other non-smoking service users. Individuals standing in the rain or in freezing temperatures in order to smoke is unacceptable. In some services, the design of the unit may not lend itself to an outside smoking area. In these instances, services may be able to provide an escort for client to a suitable place not located directly within the service in order to reduce use of the smoking room. However staff ratios and clinical issues can all affect this practice, which should be seen as a last resort. Including smoking status on service user information files and recovery care plans Given the strong anecdotal evidence that smoking for service users is often initiated or increased within mental health services, attempts to prevent such behaviour is worthwhile. Gathering information on tobacco use will allow for assessments and ongoing plans to be made for each client who is keen to work towards smoking reduction or cessation. Steps toward smoking reduction or cessation should be instigated and led by the service user themselves. As with all steps toward recovery, small practicable goals should be first identified by the service user and then supported by mental health service staff to be achieved. Assessment processes Most DHBs have staff trained to assess with the individual, their readiness for smoking cessation and / or reduction and consequently, which Nicotine Replacement Therapy could be used in this process. Mental health staff will often need to contribute to this assessment to provide a clear idea of a person’s mental wellness to undertake smoking cessation. Subsidised community programmes and nicotine replacement therapy Most communities have smoke-free programmes and initiatives available, many with subsidies for people on benefits or who have community services cards. Several smoke-free initiatives are underway through public health services. The Ministry of Health Smoking Cessation Services has recently published a Smoking Cessation Directory, which details all Government funded cessation programmes within New Zealand13. International evidence states that support programmes should be set up specifically for service users, as they often feel excluded from mainstream smoking cessation programmes14. Many service user-friendly programmes exist throughout New Zealand and have proven to be worthwhile. A range of nicotine replacement therapies (NRT) for service users who are being encouraged to reduce smoking by DHB services should be available. Nicotine patches, inhalers, nasal 13 Ministry of Health (2004) Smoking Cessation Directory. Public Health Directorate, Wellington New Zealand 14 McNeill, A (2001) Smoking and mental health – a review of the literature. Smokefree London Programme, United Kingdom p4 sprays, sublingual tablets, lozenges and gum are all forms of NRT. Many cessation programmes offer free nicotine replacement therapy for various population groups. Promoting healthy lifestyle alternatives Smoking is an addiction and like all other addictions, often needs to be replaced with other activities. It is not surprising given the stressful nature of mental illness and often, mental health services themselves, that smoking is particularly high amongst this client group15. Most individuals who give up smoking report huge demands on other parts of their lives as the result of smoking cessation. Often dietary concerns are raised as people replace smoking with a higher intake of comfort food often leading to weight gain and poor nutritional status. CONCLUSION Mental health services will need to make accommodations according to the nature of the service being provided and the service users involved when working towards a smoke-free environment. Many mental health services will still be required to become smoke-free under the Smoke-free Environments Act. Specialist mental health services, NGO residences and services where service users are contained under the Mental Health Act16 may need to adapt to cater for particular needs of their clients. Service user leadership and involvement in this process will enhance effectiveness and promote recovery. All mental health services need to be aware and mindful of the human rights of service users to continue to smoke, should they so choose, and weigh this alongside the requirements of the Act. While the Mental Health Commission is supportive of strategies to increase the physical health of all population groups within New Zealand, these must be balanced alongside the need to uphold the rights, dignity and respect of individuals. Any undue coercion or enforcement of smoking cessation challenges this balance and is in direct contrast to the aims and philosophies of the Smoke-free Environments Act and the recovery approach to mental illness. For further information, contact: Sonja Goldsack Mental Health Commission (04) 917 8922 sgoldsack@mhc.govt.nz July 2004 15 ibid. 16 Mental Health (Compulsory Assessment and Treatment) Act 1992