Pulmonary Overview
advertisement

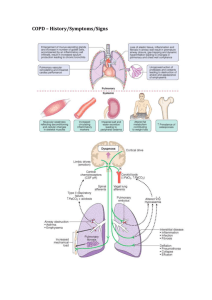
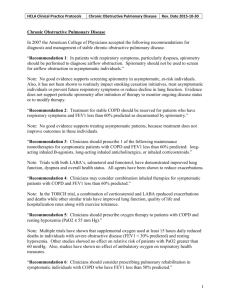
Pulmonary/COPD MS III lecture Joseph Pidala, M.D. July 12, 2005 1. Dyspnea (adapted from Dr. Schwartzstein’s discussion of dyspnea in Up to Date) i. ATS definition: "Dyspnea is a term used to characterize a subjective experience of breathing discomfort that is comprised of qualitatively distinct sensations that vary in intensity. The experience derives from interactions among multiple physiological, psychological, social, and environmental factors, and may induce secondary physiological and behavioral responses." ii. Etiology of chronic dyspnea: commonly pulmonary (asthma, COPD, interstitial lung disease) and cardiac disease (CHF, ischemia, valvular disease, pericardial disease); also anemia, deconditioning, acid/base disorders iii. Helpful to think of dyspnea in terms of respiratory controller, ventilatory pump, and gas exchanger in localizing source of dyspnea iv. Eliciting history: associated symptoms, precipitants/exercise tolerance, medical history, risk factors, social history/smoking history v. Initial evaluation for chronic dyspnea: 1. chest xray 2. cbc 3. pulmonary function testing 4. ?suspect cardiac etiology: echocardiogram, stress testing 5. further evaluation of pulmonary etiology: chest CT vi. Common causes of acute dyspnea: cardiac (ischemia, CHF, tamponade), and pulmonary (bronchospasm, PE, pneumonia, pneumothorax) vii. Use of BNP in assessment of acute dyspnea: Can help to differentiate acute dyspnea from CHF (commonly with BNP > 400) from non-CHF dyspnea (BNP < 100 has > 90% Negative predictive value) (Rapid measurement of B-type natriuretic peptide in the emergency diagnosis of heart failure. AU - Maisel AS, et al; N Engl J Med 2002 Jul 18;347(3):161-7.) o o 1. Pulmonary function testing Combining BNP with clinical indicators increased predictive accuracy Level of BNP correlated with NYHA heart failure class *indications – diagnosis/confirmatory, quantify severity of disease, evaluate disease progression a. obstructive disease i. ii. iii. iv. v. vi. vii. Examples include asthma, chronic bronchitis, emphysema, bronchiectasis, CF (asthma will demonstrate reversibility with bronchodilators) Characterized by decreased FEV1, FVC, and FEV1/FVC ratio Generally, accepted as FEV1/FVC ratio of less than 0.7 Severity according to degree of FEV1 reduction 1. > 80% normal 2. 60-80% mild 3. 40-60% moderate 4. < 40% severe (with %pred. FEV1 of 40% correlating to an FEV1 of 1liter) Asthma – shows obstructive pattern with reversibility by bronchodilator challenge Chronic bronchitis – obstructive pattern, minimal response to bronchodilators, and normal DlCO Emphysema - "" with decreased DlCO a. restrictive disease i. ii. iii. Examples include interstitial lung disease, pleural disease, obesity/chest wall, and neuromuscular disease Characterized by restrictive pattern with decreased TLC, FVC, FEV1; has normal to increased ratio of FEV1/FVC Severity by degree of reduction in TLC 1. > 80% normal 2. 60-80% mild 3. 40-60% moderate 4. < 40% severe iv. Interstitial lung disease will demonstrate decreased DlCO 1. COPD (Chronic bronchitis and emphysema) i. Burden of disease: 15million Americans, incidence of 10-15% of smokers (unlikely, but consider alpha-1 antitrypsin deficiency, especially with otherwise unexplained emphysema and cirrhosis) ii. Clinically presenting with dyspnea, cough, chronic sputum production iii. Physical exam: increased AP diameter, hyperresonance, decreased breath sounds, prolonged expiratory phase, rhonchi, wheezing iv. CXR: hyperinflation, flattened diaphragm, chronic markings, bullae v. PFT’s: obstructive pattern vi. EKG: poor R wave progression, R. heart strain vii. Chronic treatment: i. Supplemental Oxygen (if PaO2 < 55 or sat% < 89) decreases mortality (Annals of Internal Medicine. 93:391, 1980) ii. Smoking cessation iii. Ipratroprium, albuterol for symptomatic relief viii. COPD exacerbation (Acute exacerbation of Chronic Bronchitis, or AECB) i. Ipratroprium MDI/nebs, potentially albuterol MDI/nebs ii. Corticosteroids – 30% decrease in primary outcome of death, intubation, readmission for COPD or need for increased drug treatment (N Engl J Med 340:1941, 1999) iii. ?Antibiotics – no clear mortality benefit; exacerbations are commonly viral rather than bacterial. Most likely bacterial etiology includes S. pneumoniae, H. influenzae, M. catarrhalis iv. Supplemental oxygen v. Non-invasive positive pressure ventilation – Decreased need for intubation(74-26%), decreased hospital stay, decreased mortality(29-9%). (N Engl J Med 333:817, 1995) vi. Consider intubation 2. Pneumonia i. Consider acquisition – community vs. hospital vs. immunocompromised vs. aspiration ii. Microbiology i. CAP – commonly S. pneumoniae, H. influenza, M. catarrhalis, Mycoplasma (others include Legionella, gram negatives, S. aureus, strep, viruses). Usual pathogens typically will cause a lobar pneumonia, while "atypicals" like Mycoplasma, Chlamydia etc will often cause an interstitial pattern ii. Hospital acquired – more likely to include gram negatives (esp Pseudomonas), and S. aureus (consider MRSA) iii. Immunocompromised – all of the usual suspects, but also consider PCP, fungi, Nocardia, atypical mycobacteria, TB, CMV, HSV 1. PCP in AIDS patients almost uniformly when CD4 < 200 a. Presents as indolent course, dyspnea, cough, fever b. Can have multiple presentations on CXR, including normal c. Diagnosed with induced sputum, or bronchoscopy/BAL 2. PCP presentation in non-AIDS patients can be more fulminant a. Major risk factor is immunosuppression, corticosteroids iv. Aspiration – consider anaerobes iii. Manifestations i. Fever, chills, dyspnea, productive cough ii. CXR findings, consolidation, parapneumonic effusion iii. Sputum cultures (adequate specimen has > 25PMN, < 10epi) iv. Treatment i. CAP, not hospitalized – Azithromycin, or FQ ii. CAP, hospitalized – ceftriaxone/azithromycin, or FQ iii. CAP, in ICU with suspected Pseudomonas – (zosyn + FQ + azithro) iv. Hospital acquired – (IMP + FQ), or (cefepime or zosyn + tobra) v. Neutropenic pt – similar to hosp acquired; with persistent fever, consider vancomycin, then empiric antifungal coverage 3. Pleural Effusion i. Detected by decreased breath sounds, dullness to percussion ii. Seen on CXR; tap effusions layering > 1cm on lateral decubitus film iii. Consider etiology: broadly divided into transudates vs. exudates iv. Classified by Light’s criteria (overall > 90% sensitive and specific) (Light, RW, Macgregor, MI, Luchsinger, PC, Ball, WC Jr. Pleural effusions: the diagnostic separation of transudates and exudates. Ann Intern Med 1972; 77:507.) v. vi. vii. viii. ix. Exudate characterized by TPeff/TPser > 0.5, LDHeff/LDHser > 0.6, or LDH > 2/3 normal If suspicion for parapneumonic effusion, should be tapped immediately Transudates: (think imbalance of Starling forces) CHF, cirrhosis, nephrosis, sometimes PE Exudates: (think other process like inflammation, infection, malignancy, etc) Infectious, Malignancy, PE, CVD, GI disease, hemothorax, chylothorax, uremia, Meig’s syndrome, drug-induced Indications for chest tube drainage: empyema (frank pus), or complicated parapneumonic effusion (pH < 7.0, + gram stain or cultures, glc < 40, LDH > 1000)