Click here to read the full report….
advertisement
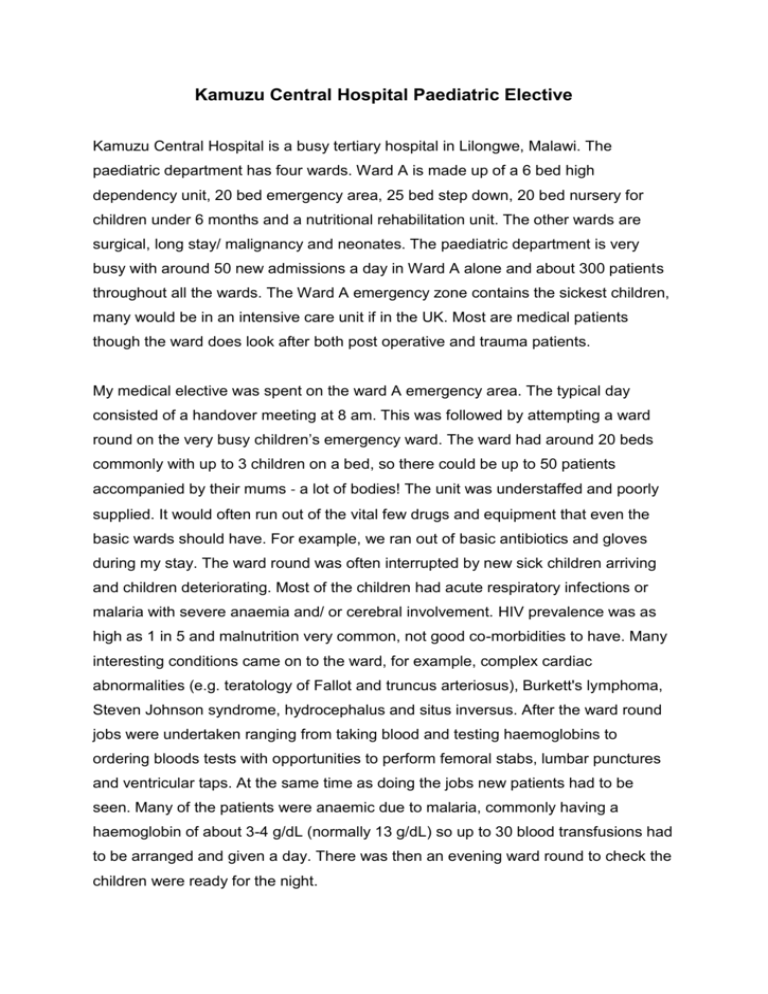
Kamuzu Central Hospital Paediatric Elective Kamuzu Central Hospital is a busy tertiary hospital in Lilongwe, Malawi. The paediatric department has four wards. Ward A is made up of a 6 bed high dependency unit, 20 bed emergency area, 25 bed step down, 20 bed nursery for children under 6 months and a nutritional rehabilitation unit. The other wards are surgical, long stay/ malignancy and neonates. The paediatric department is very busy with around 50 new admissions a day in Ward A alone and about 300 patients throughout all the wards. The Ward A emergency zone contains the sickest children, many would be in an intensive care unit if in the UK. Most are medical patients though the ward does look after both post operative and trauma patients. My medical elective was spent on the ward A emergency area. The typical day consisted of a handover meeting at 8 am. This was followed by attempting a ward round on the very busy children’s emergency ward. The ward had around 20 beds commonly with up to 3 children on a bed, so there could be up to 50 patients accompanied by their mums ‐ a lot of bodies! The unit was understaffed and poorly supplied. It would often run out of the vital few drugs and equipment that even the basic wards should have. For example, we ran out of basic antibiotics and gloves during my stay. The ward round was often interrupted by new sick children arriving and children deteriorating. Most of the children had acute respiratory infections or malaria with severe anaemia and/ or cerebral involvement. HIV prevalence was as high as 1 in 5 and malnutrition very common, not good co-morbidities to have. Many interesting conditions came on to the ward, for example, complex cardiac abnormalities (e.g. teratology of Fallot and truncus arteriosus), Burkett's lymphoma, Steven Johnson syndrome, hydrocephalus and situs inversus. After the ward round jobs were undertaken ranging from taking blood and testing haemoglobins to ordering bloods tests with opportunities to perform femoral stabs, lumbar punctures and ventricular taps. At the same time as doing the jobs new patients had to be seen. Many of the patients were anaemic due to malaria, commonly having a haemoglobin of about 3-4 g/dL (normally 13 g/dL) so up to 30 blood transfusions had to be arranged and given a day. There was then an evening ward round to check the children were ready for the night. The interprofessional team in Malawi was structured very differently to the UK. In many instances they were a bit behind with their understanding of the roles of other health professions and team working. The duties of the doctors and nurses were similar to the UK’s, however, parents played a more important role in the nursing care of their own children. On the ward we would be lucky to have two nurses. These nurses would be responsible for all the patients on the emergency ward which could be up to 50 patients, so they were very worked off their feet. This meant the parents had to get involved with their children's care, it was not uncommon for parents to feed their children via nasogastric tubes or manually ventilate a child who had been intubated. Parents also played a crucial role in identifying when their child became sick and they were encouraged to call for help. There was one physiotherapist who covered all the patients in Ward A, not just the emergency zone, so she had to work hard and this consequently meant a long wait to provide children with physiotherapy. There were no dieticians, although with all the malnutrition the paediatric department would have really benefited from this. There were a couple of specialities in Malawi that do not exist in the UK. The first were the vital signs clinicians, this profession spent their day moving from ward to ward performing and collecting vital signs on the children. This helped to relieve some of the work load of the nurses, however, there was a definite lack of communication between this profession and the other professions as children with worrying vital signs were often not handed over. The other different profession were the clinical officers. The clinical officers are similar to nurse practitioners in the UK although their training was provided through the medical school. This profession filled the gap between the nurses and doctors and revolved around performing much of the cannulation and blood collecting. The senior clinical officers were also involved with decision making similar to the doctor's responsibilities. There was a lack of effective interprofessional and even intraprofessional team working. There were often three different medical ward rounds running at the same time each with a doctor working on his own and not discussing what he had seen with the rest of the team. The doctors, nurses and clinical officers worked very independently which was in part due to culture but also due to what they had seen their seniors do. For example, in the UK we are taught that if a cardiac arrest occurs the first thing you should do is shout for help. There were many instances when I looked up and saw a health professional trying to resuscitate a child on their own. After some convincing we did improve ward rounds by including nurses and getting the doctors to work together better, however, they were still a long way off from working truly effective as a team. My work there was very demanding with long hours. The amount of sick children meant that death was sadly a common occurrence, with on average three children dying a day. I was involved with at least one cardiac arrest a week. This of course was hard to deal with but also meant that I could make a difference by recognising deteriorating children and beginning interventions that would increase their chance of survival. I was commonly responsible for my own patients, which would include their resuscitation, a steep learning curve! Help was normally available however there were times when senior help was not available. I got to perform a wide range of practical procedures, some in the UK would be performed only by more senior doctors, however, I also got to improve my nursing skills such as drawing up drugs and preparing fluids for administration. This gave me a better appreciation of the roles that other health professions have. My experiences will stay with me for a very long time and will shape me as a doctor. The lessons I learnt about effective team working has really emphasised its importance to me. I have seen how situations can go wrong when professions are not working together. I really saw firsthand how collaborative practice can improve patient care and I hope at some point to that I will be able to return to a developing country. James Selby jamespselby@gmail.com