North Wales Cancer Network DRAFT Feb 2007.
advertisement

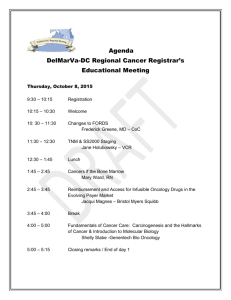
North Wales Cancer Network DRAFT Feb 2007. A Strategy for Oncology 2007 – 2014. 1) Introduction It is now six years since the opening of the North Wales Cancer Treatment Centre (NWCTC) and this passage of time, along side suggested changes to the commissioning structures in Wales, now make the need for an agreed strategy all the more urgent. This document attempts to provide stakeholders with a vision and strategy that ensures an equitable and modern service across North Wales for the next seven years. The strategy addresses the next seven years on the basis that this both broadly mirrors the time NWCTC has been opened, and, in ending in 2014 represents the date the third current linear accelerator will be in need of replacement. In this sense it provides a useful ‘line in the sand’. 2) Core Aims The following aims for the service must be evident within the strategic intentions identified within this document, 3) equity timeliness integration modernity value and sustainability Definitions Oncology for the purpose of this document refers to, Radiotherapy including the facilities and personnel required to deliver that modality. Brachytherapy Chemotherapy for all malignant disease and the supportive care resulting from that treatment All facilities and personnel related to the administration of chemotherapy including nursing and pharmacy. Treatment (only) of haematology oncology All personnel related to the above. Services out of area delivering the above to North Wales residents. 1 4) Current Provision – ‘where are we now’ 4.1) Pre 2000 Up until 2000 oncology services were in the main provided by the cancer centres in Merseyside and Manchester with only NWWT having an inpatient medical oncology based service. Outreach outpatient services from England, including chemotherapy, were hosted in C&DT and NEWT by Clatterbridge(CCO) and the Christie respectively. 4.2) Post 2000 With the opening of the North Wales Cancer Treatment Centre (NWCTC) in 2000 North Wales has developed an oncology services that includes, 3 x linear accelerators at NWCTC and associated staff 1 x basic NWCTC 40 inpatient oncology beds at NWWT and NWCTC and associated staff 8 hostel beds at NWCTC chemotherapy day units at NWWT, NWCTC and NEWT and associated staff oncology clinics at NWWT, NWCTC, NEWT and peripheral hospitals. 7 Consultant Clinical Oncologists 2 Medical Oncologists (inc a Chair in Oncology) chemotherapy reconstitution facilities in NWWT, NWCTC and NEWT and associated staff. Items above include facilities for patients with haematological malignancies though these patients are overseen by 8 Consultant Haematologists. In NEWT these patients have access to inpatient facilities within Medicine as there are no inpatient oncology beds. 4.3) The role of CCO and Christie Hospitals CCO and Christie continue to provide oncology services to the North Wales population on the basis that, The care provided is specialist and not currently available in North Wales e.g. brachytherapy. Part of a specialist pathway the main part of which is not available in North Wales e.g. radiotherapy for osteosarcoma They are the designated local oncology provider for that given population – CCO and a percentage of the Flintshire population. Limited sessions are performed by North Wales oncologists at the Christie in order to facilitate the delivery of brachytherapy to Welsh patients. No sessions are delivered by oncologists from CCO and Christie inside North Wales beyond those delivered to the Flintshire population. 2 4.4) Commissioning NWCTC services are commissioned by the Local Health Boards (LHBs) with Denbighshire LHB being the nominal lead. Services at CCO and Christies are commissioned by Health Commission Wales (HCW) and in both cases activity has diminished considerably over recent years. Activity has largely reached a plateau in 2007. 4.5) Assessment of the current provision There is no doubt that the service has developed rapidly since 2000 however issues remain that serve to shape a strategy over the next seven years. The following are known issues within the oncology service that either need to be addressed, will need a response or remain as issues for sometime in the future. 2 of the 3 linear accelerators at NWCTC are due for replacement at the end of the decade the 3 linear accelerators at NWCTC cannot be fully utilised due to incomplete staffing levels particularly within therapy radiography the Shooting Star Chemotherapy facility is under utilised and appropriate measures need to be taken to ensure this asset is fully functional the chemotherapy day units within NWWT and NWCTC are at now at capacity the oncology related elements of the pharmacy departments within all three Trusts are at, or are near to, capacity within the seven year timeframe at least three of the oncologist will have retired – possibly within the next 2-3 years. the Oncology presence within MDTs, though generally high, remains non compliant with the National Cancer Standards within a few remaining specialties recruitment to clinical trials has reduced 5) Shaping Oncology Services in the future 5.1) Demography and Geography Recent data supporting the Secondary Review (1) suggests that The demography of North Wales is predicted to change over the next 20-30 years with large growth in the numbers of older people. Tackling inequalities in health is a key issue, almost one fifth of the population living within the most deprived wards in Wales are located in North Wales. There is evidence to show that people with chronic conditions are more likely to use secondary care services. Reducing admissions requires partnership working across sectors. (1) ‘Summary Profile of the Population of Wales. A summary of the key points relevant to the North Wales region arising from currently available baseline documents - Designed for North Wales.(2005)’, 3 The birth rate in North Wales is falling with the biggest decline seen in the North West area. North Wales has a lower number of young people at all ages compared to the Welsh average. Though circulatory disease remains the main cause of death there is a significant cancer population with the known predisposing factors of increasing age, chronic illness and background poverty. It is these factors that increase the population in terms of need by approximately 100,000 (2). Geography will remain a factor though it is suggested that the population will be distributed more or less as it is now. However regarding geography the implementation of ‘Design for North Wales’ and the closure of certain community hospitals may be a factor in the provision of oncology in the future. 5.2) Trends in Cancer and Oncology The World Health Organisation have recently predicted further increases in cancer within the developed world, a world in which Wales already has some of the highest rates of certain cancers. Whilst some cancer rates are falling such as lung and stomach others are likely to increase including breast, bowel, oesophageal and skin cancer and these increases alone support the need for further developments of cancer treatment. It also noted that national screening programmes such as that for breast cancer and the forthcoming programme for bowel cancer will also detect early cancers that may well be subject to oncology based treatments (3). Recent papers suggest that though the delivery of radiotherapy may be subject to change the modality will remain as a viable treatment for cancer and in fact will increase in its application. Developments will address better targeting of radiotherapy through shaping of radiotherapy and planning of delivery as well as symptom management and tumour toxicity through ongoing debate on fractionation regimen (4). Arguably it is in the sphere of chemotherapy and supportive care where the most substantial changes may occur over the next ten years. Already two particular changes are being seen, the introduction of monoclonal antibodies such as Herceptin and the move to oral preparations such as Capectibine. Though the issue of cost is never far from the top of the agenda these developments challenge the traditional model of chemotherapy management through their inherent flexibility. Thus the trend would seem to be a definite move away from toxic regimen requiring expert administration and inpatient management to outpatient delivery and appropriate monitoring. The question is where this takes place and possibly who performs the monitoring function. (2) Population based Palliative care Needs Assessment. P Tebbit. October 2005 (3) P.Boyle, Annals of Oncology 2007. (4) Radiotherapy in Wales .WASAC 2006. 4 Regarding the last point though the current trend is for an increase in novel agents and oral versions of once intravenous drugs the fall out is an increased pressure on nurses in particular, especially as the associated reduced toxicity and increase in adjuvant usage increases the potential for use amongst a wider patient group. 5.3 The Policy Context It is suggested that at the time of writing three policy items shape the direction of an oncology strategy, National Cancer Standards - WAG 2005. Design for life – Designed to Tackle Cancer in Wales WAG Dec 2006 Design for North Wales 2006. National Cancer Standards 2005. Published in 2005 these Standards should be complied with by 2009. Each Standard has sections that relate to the delivery of radiotherapy and chemotherapy however it maybe the need to have an oncology presence at all MDTs and deliver first definitive treatment within the prescribed timescale that provide the greatest challenge in terms of meeting the standards by the deadline. Design for life – Designed to Tackle Cancer in Wales WAG Dec 2006 Provides a wider view of the direction to be taken by the Welsh Assembly Government. Design for North Wales 2006. Design for North Wales has little direct impact on oncology services other than driving the health community to rationalise its acute facilities. This rationalisation will, through its impact on support facilities such as laboratory support will influence where certain oncology services such as chemotherapy administration be developed. 6. Describing Oncology Services in 2014 – ‘where do we want to get to’ The following should be objectives that which the North Wales community wish to try and achieve by 2014 at the latest. 6.1 Radiotherapy Radiotherapy services should be sufficient to meet the needs of the population based on the evidence available in 2007.On this basis by 2014 there should be four operational linear accelerators in North Wales at NWCTC with an appropriate number of CT simulators. All four linear accelerators should be fully operational, with adequate staffing, to allow equitable access across North Wales in compliance with the waiting times targets in 2007. 5 Delivery of radiotherapy should be in line with the latest practice in the UK and be delivered in accordance with the most stringent quality programmes. North Wales should be self sufficient in therapy radiographers by 2014. 6.2 Brachytherapy Brachytherapy should continue to be delivered out of area though highly modernised simple brachytherapy should be developed for local provision if the evidence is available. Both radiotherapy and brachytherapy should continue to be offered from a single site at Glan Clwyd. 6.3 Chemotherapy Chemotherapy services should be equitable in terms of consistency, geographical access and timeliness. There should not be issues of capacity problems especially in relation to the availability of new drugs. The chemotherapy service should be modern, cohesive on a regional basis and flexible in terms where and when treatment is delivered. Pharmaceutical co-ordination and clinical management should be via software used across all three Trust sites. Pharmacies should have sufficient capacity to deliver the service and practice modified to reduce costs and expand capacity on a regional basis. The introduction of all new cancer drugs should be subject to a single process overseen by a single, relevant, group consisting of clinicians and commissioners. No new drugs should be introduced without warning sufficient to ensure resources are in place to support it. 6.4 MDTs An oncology presence should be assured at all MDTs in a manner that recognises the sub specialties of the oncologists, the need for cover and the use of current and future communication technologies. 6.5 Supportive Care All three Trusts sites should provide 24 hr inpatient supportive care facilities with appropriate staffing. 6.6 Heamatology/Oncology Haematology/oncology should be further integrated into oncology across all three sites. 6 6.7 Medical manpower Oncology medical manpower should be expanded to secure the above with specific attention being given to the role of Clinical Oncology and Medical Oncology. Manpower expansion should however, in terms of seniority, be tailored to ensure improved local access whilst not losing sight of the need to be part of a fully integrated North Wales oncology service. 6.8 Nursing Nursing should be expanded to deliver the above. 6.9 Research The availability of clinical trials should be equitable across the three Trust sites and recruitment increased, as a minimum, to equal the rest of Wales 6.10 Follow-up Oncology practice should be modernised to reduce the amount of follow-up offered by a consultant only service and viable alternatives developed using other professions in other settings. 6.11 Diagnostic support An increase in access to oncology will increase the need for diagnostic support, specifically radiological imaging. Radiology services should be expanded to cater for this expansion particularly in NEWT and NWWT. By 2014 PET-CT should be available as a fixed site service in North Wales and should be located at Glan Clwyd. 6.12 Management/co-ordination The oncology service should be both clinically and administratively managed on a North Wales basis in a fully integrated and compliant manner. This management may be located at NWCTC but should not be a formal part of that clinical organisation. NWCTC should be responsible for the co-ordination of the delivery of radiotherapy and chemotherapy on a North Wales basis and be subject to appropriate scrutiny as a result. 6.13 Commissioning There should be a single commissioner of oncology services with a single budget regardless of geographical delivery. The single commissioner should also be responsible for oncology treatment delivered in England to North Wales residents. 7 6.14 Christie and CCO The Christie and CCO should continue to be a provider of oncology services but only in accordance with the demands of the identified commissioner. 7. Delivering the future – ‘how are we going to get there’. Having identified above some ends points of how oncology services should look by 2014 what is now described below is some more detail as to how the community should progress towards achieving the strategic aims identified. 7.1 Radiotherapy – increases in capacity NWCTC has completed the submission of SOC 1a to WAG which addresses the replacement of the first two linear accelerators and the construction of two decant bunkers. SOC1b is now being developed by NWCTC and this should be supported in order to get to the four linear accelerator capacity required by the beginning of the next decade. It is noted that this strategy extends up to 2014 when the next linear accelerator will be in need of replacement .It is noted that SOC1A requires two decant bunkers to be built which if left undeveloped should leave one bunker remaining for decant purposes in 2014. 7.1.2 Physics support staff Additional physicists will be required both to commission new equipment and address an expansion in the operational equipment. The requirement for additional physics staff should be included in SOCs 1a and 1b and a recruitment process put in place to ensure sustainable radiotherapy delivery. 7.1.3 Therapy Radiographers Again SOC 1b should address the need for additional staff. However NWCTC at this time has problems maintaining adequate staffing levels for it three machines and this, with turnover and other larger units in close proximity on a similar recruitment pathway,suggests that achieving adequate staffing levels via the established routes may not deliver. NWCTC, with appropriate partners should investigate the potential for training a cadre of therapy radiographers either locally within North Wales or from other sources e.g. Eire. In addition the role of the therapy radiographer needs to be analysed further and the modernisation projects already in place built upon to see if a new type of post can be developed to assist the therapy radiographers. Either way NWCTC needs to identify how it can recruit and retain the increased number of staff it will require to utilise four linear accelerators to the maximum. 8 7.2 Brachytherapy The future of brachytherapy is unclear in terms of what is economically appropriate to be developed in North Wales. Whilst development of a service should not be ruled out it is equally the case that a sound reason for its development is required. SOC 1b may be an opportunity to develop a service as capital investment will be a major requirement and it is suggested that NWCTC take a lead on advising commissioners and stakeholders alike as to the requirement for such a service in North Wales. 7.3 Chemotherapy – increases in capacity Physical space for chemotherapy expansion should be base on three levels of provision. A minimal number of five-day bed facilities should be available on all three Trust sites for those few regimen that require overnight admission – no chemotherapy administration should take place at weekends. NEWT will be required to identify appropriate facilities probably relating to the expansion of Shooting Star to an overnight five-day facility or their haematology service where inpatient chemotherapy for solid tumour work can be co-located. This should feature in SOC2. Out-patient chemotherapy facilities should also be available on all three sites and these facilities, as with those above, should address the needs of the local population. These facilities should remain co-located with oncology outpatient facilities and provide adequate space and resources to those patients commencing chemotherapy or receiving toxic chemotherapy best delivered in that environment. No expansion of these facilities should be considered at either NWCTC or NEWT until the full utilisation of the space within NEWT has been achieved. The third level should be the localised delivery of chemotherapy to the patient using either a commercial provider such as Healthcare at Home or an equivalent competitive NHS scheme. Every opportunity should be taken to deliver the appropriate therapies in this manner by 2014 and immediate consideration should be given to scoping this development. Thus SOC 2 should establish the demands of a comprehensive chemotherapy service in North Wales, however whether this is an expansion in the hospital or community based facilities is yet to be determined, certainly no expansion of facilities within secondary care should take place until the third level of care described above has been explored as a viable clinical option. 7.3.1 Pharmacy development All three pharmacies are at capacity and development plans need to be outlined within SOC 2. Again these plans should reflect Shooting Star working to capacity and the potential development of new agents particularly the change to oral medication. Consideration should be given to a central production unit off an acute site which can mass produce chemotherapy for all three Trusts as well as those patients 9 receiving agents via other means in the community, it maybe that other commercial opportunities also exist. SOC 2 should address this option as such a development may well be more cost effective than triplicate expansion across North Wales. All three Trusts should be linked by Chemocare. 7.3.2 Nursing Support Nursing levels within the chemotherapy environment should equitable across North Wales and a single consistent approach should be taken to the education of such nurses and the standards deployed. As a result nursing standards in chemotherapy should be adopted and rigidly applied. If a community based model proves viable the nurses in the community will require appropriate training in order to deliver a specific portfolio of treatment. The nurses within the chemotherapy units must be prepared and willing to educate their colleagues and this is probably best done through adequate integration and a central consistent approach to education as previously mentioned. Once Shooting Star is working to capacity there should be a review of nursing numbers within the units and a review of the function of those nurses. 7.3.3 Introducing new cancer drugs. A single body should be established to consider the entry of new drugs into the service. This body which should be multi stakeholder in nature should have the authority and budget to act on both the providers and commissioners behalf with and explicit remit for planning for new therapies in advance and in a manner that prevents unplanned financial pressure. Core to the groups existence is consistency in practice, efficiency in process and equity in access. 7.4 Medical Manpower Medical manpower should be increased to address the following, Consultant contract requirements Radiotherapy planning sessions to maintain targets MDT participation Clinical sessions On-call Sub specialisation The manpower numbers should not only address the different specialties i.e. clinical oncology and medical oncology but also a skill mix utilising staff grades and training posts where possible. 10 Recruitment up to 2014 should reflect the WSAC (2001) report and increase the number of Consultant appointments by 4 Clinical Oncologists 3 Medical Oncologists. Noting that these recommendations preceded the outcome of the Consultant Contract negotiations in Wales these posts should be seen as a minimum. Recognising this it will be a requirement that these posts are appropriately supported by sufficient Staff grade positions. Accommodating this expansion in staff should feature in SOC2. 7.4.1 Location of Medical Manpower The location of medical manpower needs to be re-assessed in light of the commitments required of oncologists, radiotherapy capacity and changes to chemotherapy practices. As a result it is recommended that by 2014, from within the recruit profile highlighted, that the following recommendations are implemented, NWCTC has at least one Medical Oncologist on site with clinical commitments within Conwy & Denbighshire NWWT has at least one Clinical Oncologist based at NWWT who ‘reaches in’ to NWCTC. NEWT has at least one Medical Oncologist and one Clinical Oncologist who ‘reach in’ to NWCTC. The rationale for this approach is the attempt to find a balance between the need to provide planning sessions in the centre with sub specialisation versus the need to provide MDT input and chemotherapy clinical input and leadership at a local level. 7.4.2 Recruitment priorities Recruitment priorities are difficult to define as they will be dictated by the retirement or movement of the current post holders and the recruitment market place at the time. Assuming the status quo is maintained the following prioritisation is recommended. 11 Table 1. Oncology Consultant manpower – recruitment priorities. Post Med Onc 1 Location NWCTC Clin Onc 1 NWWT Clin Onc 2 Med Onc 2 NWCTC NEWT Clin Onc 3 Med Onc 3 Clin Onc 4 NWCTC NWWT NEWT 7.5 Rationale Aid chemotherapy issues Provide clinical lead for chemotherapy Provide additional support to Oncology establishment Feed into MDTs Additional support Oncology leadership with specific emphasis on chemotherapy service Additional support Additional support Provide additional support to Oncology establishment Feed into MDTs Supportive care As a result of an expansion in patients receiving both radiotherapy and chemotherapy it is likely that the need for supportive care will be increased and this may refer to drugs, rehabilitation or some other intervention. Inpatient beds and hostel beds providing supportive care for radiotherapy patients are likely to be integrated within SOC 1a but inpatient beds for other supportive needs may not be accounted for. Beds should be available on all three sites and managed by an on site designated team (see 7.4.2). Beds should be limited to patients who require symptomatic support for ongoing treatment and care should be consistent across North Wales. There should be a designated lead for supportive care who, with the identified teams, ensures consistent practice and equitable access to supportive care facilities across North Wales. 7.5.1 Psychological Care Though not the preserve of oncology designated psychological care services specifically for cancer sufferers is anchored in NWCTC and serves the populations of NWCTC and NEWT. Thus by implication there is not the same access for cancer sufferers in NWWT. The provision of psychological support should come under the umbrella of supportive care and be part of the remit of the clinical lead for that service. All patients should be assessed for their psychological state of health and care provided according to the patients need. Whilst it is reasonable that the designated psychological care services is based in NWCTC is it essential that the full development of the service as described by 12 R.Corney and J.Wilcox-Jones (2004) and supported by the Palliative Care Network is, as a minimum, implemented as part of this strategy. 7.5.2 Palliative Care Palliative care is increasingly a free-standing specialty within North Wales and rightly so. However the provision of palliative care is part of supportive care and as such links should be formalised as part of the process identified above. It is suggested that many patients within the current inpatient oncology facilities are admitted for the delivery of palliative or specialist palliative care and as part of the assessment of inpatient needs in SOCs 1a to 2 there should be the parameter that bed numbers identified reflect only those beds required for patients receiving oncological treatment or supportive care attributable to oncological treatment. Patient requiring palliative care should utilise beds resourced to deliver that care but these should not be in a treatment centre. This strategy should be shared with the Palliative Care Network with a view to gaining their insights and views on the impact of this approach. It may be that within NWCTC, NEWT and C&DT in particular, that SOC 2 includes a sub section that ensures some limited palliative care beds for those patients who need to be in an acute setting because of palliative care interventional procedures e.g. nerve blocks. Fundamentally though the Palliative Care Network needs to agree its own approach to inpatient facilities and it is assumed that these will be within the local hospices and community facilities. 7.6 Clinical Research With an expansion in medical manpower it is hoped that not only and increase in recruitment to clinical trials can take place but also that it can take place in an equitable fashion with all three locations recruiting and running trials. Whilst administrative support and Welsh Cancer Trials Network (WCTN) management should be retained at NWCTC the local units at NWWT and NEWT should be the permanent location of their local WCTN trials staff. This approach would be supported by the local oncology appointments and the supportive care teams. This, and any additional resource, should be considered as part of SOC 2.This approach should lead to equitable access to trials across North Wales. As with drugs the way in which clinical trials are adopted and implemented needs to be refined and the oncology service needs to establish a once only mechanism for consideration of trials. This will involve further development of the current WCTN approach in terms of building upon their consistent approach to streamline it into a single approach. The research leads within WCTN need to become more involved with the oncology service and the academic department of cancer at the University of Wales, Bangor and lead all those professions those working in oncology of to embrace clinical quantitative and qualitative research. 13 7.7 Education Many of the strands that support the delivery of this strategy rely on staff being adequately educated in specific elements of oncology whether this be in chemotherapy practice or as locally trained therapy radiologists. Age demographics coupled with the rest of the United Kingdom pursuing the same agenda suggests that North Wales will continue to face problems wit recruitment and retention. It would therefore seem essential that North Wales looks for alternative methods of obtaining highly skilled, appropriately educated staff and one option should be to provide enhanced education and training locally. It is suggested that each specialty investigates options for further training and education of staff and dialogue is opened up with local educational establishments as to the delivery of relevant, and possibly novel, educational programmes. It is important that some leadership is provided around this issue and it is suggested that a small multi disciplinary, multi organisational committee be formed to establish the potential educational requirements of the workforce over the next seven years in a manner that reflects the key elements of this strategy. 7.8 Modernisation All areas of oncology should be subject to modernisation with particular emphasis being given to the following, Increased efficiency within oncology pathways Wider use of nursing, pharmacy and professions allied to medicine Wider use of communication technology A particular group within the oncology environment should be tasked with analysing opportunities for modernisation and their implementation. Modernisation related developments should support the model identified for chemotherapy services, rectification of the capacity issues in chemotherapy and consistent achievement of the waiting times targets within radiotherapy. Part of achieving the above is done through the modernisation agenda being reflected in the education programme provided to the oncology service by the various academic/teaching departments. 7.9 Management It is essential that the oncology service in 2014 is seen as a Network based service that, despite being co-ordinated from NWCTC, is managed and delivered in an overtly linked and mutually supportive manner, across all three delivery sites. Thus management should exist on a number of levels. Local level Clinical management and clinical governance should be provided and assured by the clinical team established on each of the three sites. These clinical teams should be assisted by appropriate organisational management on the three sites, with both sets 14 of staff being implicitly integrated into the Network oncology service structure. Essential to this process is clinical sessions within NWCTC and clinical, practice supported by Network wide protocols. Co-ordination level A certain level of clinical co-ordination will be required especially regarding medical staff and their sessional commitment and cover requirements. The provision of chemotherapy in the primary/community care setting and clinical research will also require similar co-ordination. This co-ordination should stem from NWCTC with all oncology staff seeing this as their base or as a minimum, their administrative hub. By 2014 clinical management arrangements should be in place that reflect these responsibilities, key will be the appointment of a Clinical Director and departmental manager for Oncology on a Network basis. Network management level As mentioned above by 2014 the oncology service in North Wales should be coordinated and managed as one with the ‘management’ hub being at NWCTC. Day to day management should be delivered through the Clinical Director and departmental manager through close liaison with the site managers and resident oncologists. The service in its entirety should be accountable to a Service Board that is representative of the various delivery sites, the commissioners and users. This Board should not only oversee delivery of the service but also be the forum for delivery of the oncology strategy. This development should be delivered as soon as is practicable and the Regional Oncology Group disbanded once this level of change has been achieved. 7.10 Commissioning Building upon the model of a lead commissioning LHB and the yet to be finalised model of a Regional Commissioning Unit, there should be single commissioner of oncology services for North Wales. The single commissioner should commission all oncology services accessed by the North Wales population and have full responsibility for local provision, capital projects and any additional all Wales issues. In addition the lead commissioner should be the single source of commissioning advice on cancer drugs. By 2014 a clear understanding of oncology expenditure should be established and this investment extracted into a free standing but not ring fenced oncology budget held by the lead commissioner. The lead commissioner should have a seat on the Service Board previously mentioned. 15 7.10.1 Christies and Clatterbridge Even by 2014 it is assumed that some services will be required from Christies and Clatterbridge and these services will be commissioned by the lead commissioner rather than a single all Wales specialist commissioner as is the case at present. 8) Conclusion This strategy aims to address a vision for oncology over the next seven years on the basis that this doubles the time NWCTC will have been established and takes the community up to the next known major capital investment, replacement of the current third linear accelerator. There are several themes for the next seven years namely, expansion of treatment facilities both within the hospital setting and beyond, expansion and modernisation within the human resources available and finally a cultural shift from a hub and spoke model to a flatter equal access model. It is believed that all of these strategic objectives are desirable and with each one being achieved the service has the best chance of meeting the challenges in oncology over the next seven years. 16