Study Title Here - The University of North Carolina at Chapel Hill
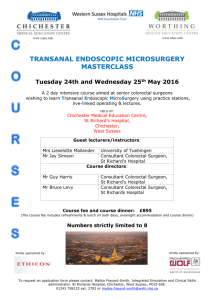
advertisement

Amendment #3 December 2005 A Population-Based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 December 2005 Cancer Care Outcomes Research and Surveillance Consortium (CanCORS) PRIMARY DATA COLLECTION AND RESEARCH (PDCR) SITES University of Alabama at Birmingham (UAB) University of California at Los Angeles (UCLA)/RAND Dana-Farber Cancer Institute (DFCI)/Cancer Research Network (CRN) Harvard Medical School (HMS)/Northern California Cancer Center (NCCC) University of Iowa (UI) University of North Carolina at Chapel Hill (UNC) Veterans Affairs Health Services Research /Duke and University of Minnesota (VA) CANCORS STATISTICAL COORDINATING CENTER Dana-Farber Cancer Institute (DFCI)/Frontier Science and Technology Research Foundation (FSTRF) Protocol 001 Amendment #3, December 2005 PDCR Site Principal Investigators John Ayanian, MD, MPP Harvard Medical School Dept. of Health Care Policy 180 Longwood Ave. Boston, MA 02115 Mona Fouad, MD, MPH University of Alabama at Birmingham Div. of Preventative Medicine 1530 3rd Ave., South MT 618 Birmingham, AL 35294-4410 Katherine Kahn, MD RAND Corporation P.O. Box 2138 1700 Main St., M-10 Santa Monica, CA 90407 Ph: (617) 432-3455 Fax: (617) 432-0173 ayanian@hcp.med.harvard.edu Ph: (205) 934-2125 Fax: (205) 934-7959 mfouad@dopm.uab.edu Ph: (310) 393-0411 ext. 7706 Fax: (310) 393-4818 kkahn@mednet.ucla.edu Robert Sandler, MD, MPH University of North Carolina Div. of Digestive Diseases and Nutrition CB#7080 719 Burnett Womack Bldg. Chapel Hill, NC 27599-7080 Robert Wallace, MD University of Iowa Dept. of Epidemiology College of Public Health 200 Hawkins Drive C21N General Hospital Iowa City, IA 52242 Jane Weeks, MD Dana-Farber Cancer Institute Center for Outcomes and Policy Research 44 Binney St. Boston, MA 02115 Ph: (919) 966-0090 Fax: (919) 966-2478 rsandler@med.unc.edu Ph: (617) 632-2509 Fax: (617) 632-2270 jane_weeks@dfci.harvard.edu Ph: (319) 384-5005 Fax: (319) 384-5004 robert-wallace@uiowa.edu Dawn Provenzale, M.D, M.Sc. Colorectal Cancer Quality Enhancement Research Initiative, Durham VAMC & Duke University School of Medicine 508 Fulton Street Durham, NC 27705 Michelle van Ryn, Ph.D. Colorectal Cancer Quality Enhancement Research Initiative, Minneapolis VAMC and University of Minnesota School of Public Health 152/2E, One Veterans Place Minneapolis MN 55417 Ph: (919) 286-2287 Fax: (919) 416-5839 prove002@mc.duke.edu Ph: (612) 467-3406 Fax: (612) 727-5699 michelle.vanryn@med.va.gov CanCORS Statistical Coordinating Center (SCC) Principal Investigator David Harrington, PhD Dana-Farber Cancer Institute Dept. of Biostatistical Science 44 Binney St. Boston, MA 02115 Ph: (617) 632-3012 Fax: (617) 632-2444 harrington.david@jimmy.harvard.edu CanCORS Statistical Coordinating Center (SCC) Protocol Information Contact CATI Coordinating Center (CCC) Contact Maryse Roudier, MPH Project Manager CanCORS Statistical Coordinating Center Frontier Science 900 Commonwealth Ave. Boston, MA 02215 Laural Hill Project Leader RAND Corporation P.O. Box 2138 Santa Monica, CA 90407 Ph: (617) 632-2097 Fax: (617) 632-5899 roudier@jimmy.harvard.edu Ph: (310) 393-0411 x6107 Fax: (310) 451-6291 lhill@rand.org Protocol 001 Amendment #3, December 2005 Table of Contents 1. Introduction .............................................................................................................................. 1 2. Study Objectives ...................................................................................................................... 4 3. Study Population ................................................................................................................... ...5 4. Enrollment Procedures ............................................................................................................. 6 5. Study Design ............................................................................................................................ 9 6. Description of Data Sources ................................................................................................... 27 7. Data Transfer Protocols and Data Safeguarding Plans........................................................... 46 8. Risks and Benefits for Participants ......................................................................................... 50 9. Reference............................................................................................................................... 53 Appendix A: Method for Participant Identification and Contact (Site-Specific).............................. A-1 Appendix B: PDCR Sites and Geographic Area of Enrollment ..................................................... B-1 Appendix C: Disease Specific Eligibility Checklist........................................................................ C-1 Appendix D: Introductory Interview Scripts and Full Patient Survey ............................................. D-1 Appendix E: Brief Patient Survey................................................................................................. E-1 Appendix F: Surrogate Respondent Survey................................................................................. F-1 Appendix G: Follow-Up Interview Scripts and Surveys ................................................................ G-1 Appendix H: Translations of Patient Survey................................................................................. H-1 Appendix I: Physician Contact Letter .............................................................................................I-1 Appendix J: Patient and Surrogate Contact Letters and Brochure ................................................ J-1 Appendix K: Medical Release Consent Forms and Cover Letters................................................ K-1 Appendix L: Physician Contact Information Worksheets ...............................................................L-1 Appendix M: Provider Survey Protocol and Provider Surveys.....................................................M-1 Appendix N: Self-Administered Survey and Cover Letter............................................................. N-1 Appendix O: Medical Record Abstraction Instrument................................................................... O-1 List of Tables Table 5.1: Patient Survey Enrollment Goals by PDCR Site for Participants with Colorectal Cancer. .............. 12 Table 5.2: Patient Survey Enrollment Goals by PDCR Site for Participants with Lung Cancer. ...................... 14 Table 5.3: Summary of Oversampling Plans by PDCR Site. ............................................................................ 16 Table 5.4: Effective Sample Size (ESS) and Minimum Detectable Difference (MDD) of Representative Primary Analyses. ........................................................................................................................... 20 Table 5.5: Estimated Number of Physicians Involved in the Care of Subjects in PDCR Regions, by Specialty ......................................................................................................................................... 21 Table 5.6: Minimum Detectable Differences in Analyses Linking Data from Provider Survey to Patients’ Treatments and Outcomes ............................................................................................................. 25 Table 5.7: Provider Survey Sample Design ...................................................................................................... 26 Table 6.1: Domains in the Baseline Patient Survey, Full Primary Respondent Version. ................................. 29 Table 6.2: Priority Window for Interviewing ...................................................................................................... 31 Table 6.3 Follow-up Survey Algorithm .............................................................................................................. 33 Table 6.4: Domains in the Survivor Follow-up Survey. .................................................................................... 35 Table 6.5: Domains in the Decedent Follow-up Survey. .................................................................................. 36 i “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients 1. Protocol 001 Amendment #3, December 2005 Introduction 1.1 Overview The Cancer Care Outcomes Research and Surveillance (CanCORS) Consortium is a collaboration of seven teams of investigators from around the United States, and is funded by the National Cancer Institute (NCI) to evaluate the quality of cancer care in this country1. The goal of the CanCORS Consortium is to examine the care delivered to population-based cohorts of newly diagnosed patients with lung and colorectal cancer in multiple regions of the country and to assess outcomes associated with that care. As distinguished from randomized trials of specific treatments conducted among highly selected patients and providers, this study will use the best available observational data and statistical techniques to identify differences in the delivery of cancer treatment and to evaluate the reasons for these differences across a broad range of health-care providers and organizations. Where possible, the consortium will examine the degree to which those differences in care are associated with differences in outcomes. The study will be presented to potential participants under the name Share Thoughts on Care. The CanCORS Consortium consists of seven Primary Data Collection and Research (PDCR) sites and a Statistical Coordinating Center (SCC). All seven PDCR sites will enroll study participants using rapid case ascertainment (RCA) from cancer registries. Five of the PDCR sites will enroll study participants using RCA from cancer registries based on the geographic area in which the site is located. Two sites (DFCI/CRN and the VA) will enroll participants using RCA from cancer registries based on the provider organization participating in this study of which he/she is a member. In addition, DFCI/CRN and the VA will augment their case lists using clinically relevant health maintenance organization (HMO) or health system administrative data. Appendix B lists the geographic areas covered by the PDCR sites. Each PDCR site will identify patients with newly diagnosed lung cancer or colorectal cancer for combined population-based cohorts of approximately 5000 patients with each cancer type. Baseline patient-level data will be collected in a patient interview administered approximately four months after diagnosis; follow-up data will be collected in a second interview 11 - 13 months after diagnosis and in a review of medical records 15 months after diagnosis. The interviews and the medical record reviews will collect data about the care received during different stages of illness (including diagnosis, treatment, surveillance for recurrent disease, and palliation), as well as data on various clinical and patient-reported outcomes and information about patient preferences and behaviors. A health care provider survey will collect information about physician knowledge and attitudes about care and their practice characteristics. The SCC will assist the PDCR sites in the collection of standardized, core data across the individual research sites and will serve as the central repository for the pooled data. 1.2 Context The National Cancer Policy Board (NCPB) of the Institute of Medicine has described quality care as “providing patients with appropriate services in a technically competent manner with good communication, shared decision-making, and cultural sensitivity.”2 Based on past studies of cancer health services and expert opinion, however, the NCPB has concluded “for many Americans with cancer, there is a wide gulf between what could be construed as the ideal and the reality of their experience with cancer care.”2 Prior studies of cancer patients have demonstrated inadequate patient counseling regarding treatment options,3,4 under-use of evidence-based treatments such as surgery,5 radiation therapy,6-8 and adjuvant chemotherapy,9,10 and inadequate care at the end of life, including control of patients’ symptoms and use of hospice care.11,12 These lapses in care may have important implications for outcomes such as disease recurrence, survival, quality of life, or patient satisfaction. Moreover, prior research has demonstrated disparities in cancer care and 1 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 outcomes based on age,6,10,13-16 race,15-1718 insurance status,19,20 socioeconomic status,15,18,21 location of residence,22,23 the providers seen,15,24-26 and site of care (teaching status and volume of cases).22,27,28 Despite documentation of these differences for patients with various types of cancer, the underlying reasons for them, such as differences in patients’ preferences, access to care, patient-physician communication, provider knowledge, attitudes and preferences, provider bias, or other causes, are not well understood. Much of the prior research related to the quality of cancer care has studied care in selected or small populations of patients, has been conducted retrospectively, or has relied on data sources with limited clinical detail, such as Medicare claims data. Furthermore, although many studies have documented disparities in care, few have explored the reasons for these disparities. Finally, few data are available about process– outcome links for cancer treatments among patients who would not meet criteria for enrollment in many clinical trials, including elderly patients and those with substantial comorbidity. For these reasons, this project provides an important opportunity to generate scientifically rigorous insights that can improve the care and experiences of patients with lung and colorectal cancer, the two leading causes of cancer mortality in the U.S. The CanCORS Consortium provides a unique opportunity to examine care for lung and colorectal cancer patients in community settings in multiple regions of the United States, to identify variations in care, and to begin to understand the reasons for these variations. By collecting and analyzing data from a large number of patients in geographically diverse settings and care systems, we expect that the findings of this study will help clinicians and policy-makers improve cancer care and the experiences of cancer patients. 1.3 Specific Aims Analyses will explore the following two principal aims: To determine how the characteristics and beliefs of cancer patients and providers and the characteristics of systems of organizations delivering cancer care influence treatment and outcomes across the continuum of care from diagnosis to recovery or death. The study will evaluate the extent to which patients experience these positive elements of cancer care, with particular emphasis on the reasons for differences by (a) patients’ age, race, ethnicity, cultural and family support and socioeconomic status (SES); (b) types of providers delivering care; and (c) organizational aspects of care. To evaluate the effects of a select group of common and specific processes of care on clinical outcomes. Examples include: (a) evaluating the effectiveness of proven cancer therapies in types of patients who were underrepresented in those trials (e.g., elderly patients and those with significant co-morbidity); (b) evaluating the effectiveness of proven cancer therapies in routine community settings of care; and (c) exploratory assessments of the effectiveness of a limited number of new or established therapies that have not been definitively studied in randomized trials. The primary and secondary objectives are discussed in more detail in Section 2. 1.4 Overall Project Design Each PDCR site will identify cohorts of approximately 1000 patients with colorectal or lung cancer and will collect data about their care in the 15 months following diagnosis. Primary data will be collected from 3 sources: patient surveys, medical records, and surveys of health care providers. These data will be supplemented with cancer registry data and publicly available data sets. 2 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 1.4.1 Patient Survey Patients will be interviewed four months after diagnosis to collect information that can be obtained reliably only from the patient, or which corroboration from the patient is desirable. This includes patient baseline characteristics, health history and health behaviors, treatments received and discussions with providers about treatments, patients’ assessment of their care, outcomes (e.g., quality of life, functional status), and information that is used as a basis for collecting other information, such as the identities of physicians. The patient survey instrument has been designed to rely on previously validated instruments wherever possible to facilitate comparisons with other studies and to increase the validity of the data that we will collect. We have conducted a pilot test of 86 patients (as of March 13, 2003) with lung or colorectal cancer to estimate the time to complete the survey, assess item non-response, and identify questions that pose problems for respondents. The primary mode of interview will be a telephone survey. A brief version of the survey will be available for patients who cannot or do not wish to participate in the standard interview. Patients who are too ill to participate or who would rather have a close relative or other caregiver respond may elect a surrogate respondent. All versions of the patient survey will have validated Chinese and Spanish translations. Additional details about the domains of the patient survey along with findings from the pilot study can be found in Section 6.2. A follow-up survey will be conducted at 11- 13 months after diagnosis. 1.4.2 Medical Record Abstraction The medical record abstraction will be used to collect detailed information on stage and tumor characteristics, cancer treatments (surgery, chemotherapy, radiation therapy), complications of treatments, patients’ co-morbid illness, and the outcomes from therapy. Although some of this information will also be collected in the patient survey, we anticipate collecting details about the cancer and treatments that patients may not be able to report readily and accurately. Additional details about the medical record abstraction can be found in Section 6.4. 1.4.3 Health Care Provider Survey The provider survey will gather data about physicians and their practices that are not available from other sources, including provider beliefs about treatments, practice style, organization of practice, and provider demographics. Providers will not be asked about the care given to specific patients. Instead, physicians will be asked to respond to generic vignettes of clinical scenarios. Respondents will also be asked general questions about their knowledge and attitudes towards cancer treatment. The generic responses will be linked with patient-level data to assess the contribution of provider beliefs, attitudes, practice styles, and practice setting to processes and outcomes of cancer care. Additional details about the provider survey can be found in Section 6.5 and Appendix M. 1.4.4 Secondary Data We plan to supplement the patient survey, medical record abstraction, and provider survey data with cancer registry data and publicly available datasets, such as Medicare claims. These additional data will allow us to verify the completeness of data from other sources and will provide additional data, such as health care utilization. 3 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients 2. Protocol 001 Amendment #3, December 2005 Study Objectives 2.1 Primary Objectives The primary objectives will be to examine the influence of the characteristics and beliefs of cancer patients and providers, as well as the characteristics of systems of organizations delivering care, on the treatment and outcomes of cancer patients from diagnosis to recovery or death. The specific questions that have highest priority in these objectives are: 2.1.1 Why are there variations by patient race, ethnicity, and socioeconomic status in important processes or outcomes of care? While this study will examine all important aspects of care in lung and colorectal cancer, we will pay particular attention to the following processes of care: the use of adjuvant chemotherapy for stage III colon cancer and stage II and III rectal cancer, and the use of curative surgery for stage I and II lung cancer. 2.1.2 Why are elderly patients less likely to receive effective treatments, particularly curative surgery and adjuvant chemotherapy, for lung and colorectal cancer? We will pay particular attention to the effect of co-morbid conditions, as well as provider and patient beliefs about the effectiveness of care in this group. 2.1.3 What patient or provider characteristics are associated with variation in the use of chemotherapy for metastatic non-small cell lung cancer and metastatic colorectal cancer? 2.1.4 Are patient symptoms recognized and controlled effectively at different stages of illness, especially for symptoms such as pain, anxiety, and depression? Are patient characteristics such as age, gender, race/ethnicity, or socioeconomic status associated with differences in symptom control? 2.1.5 What patient or provider characteristics are associated with patients’ interpersonal experiences with cancer care, including patient perceptions of the coordination of care, provision of desired information, respect for patient preferences, and emotional support from health care providers? 2.2 Secondary Objectives The secondary objectives will be to evaluate the effects of a select group of common and specific processes of care on clinical outcomes. The specific questions with highest priority are: 2.2.1 How does the efficacy of the therapies listed below as measured in randomized trials compare with the effectiveness and toxicity of those therapies among patients who were underrepresented in those trials, particularly the elderly and patients with significant co-morbidity? Adjuvant therapy for stage III colon cancer Adjuvant therapy for stage II or III rectal cancer First-line chemotherapy for unresectable and metastatic colorectal or lung cancer 2.2.2 Why do patients with colorectal or lung cancer treated in high-volume hospitals have lower mortality rates than those experienced by patients treated in lower-volume hospitals? 2.2.3 Why is participation in clinical trials so low for lung and colorectal cancer? What determines whether patients are offered participation and whether they accept it? 4 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients 3. Protocol 001 Amendment #3, December 2005 Study Population 3.1 Introduction and Overview Share Thoughts on Care is a population-based study with cancer registry rapid case ascertainment (RCA) in all 7 participating PDCR sites. The target population in five of the sites consists of all patients diagnosed with colorectal or lung cancer during the enrollment period for the study who live in the geographical area in which the site is located. We refer to these sites as ‘geographically-based’ sites. The target population in the sixth and seventh sites (DFCI/CRN and the VA) consists of all patients diagnosed with colorectal or lung cancer during the enrollment period for the study who are members of each of the provider organizations participating in this study. In addition, DFCI/CRN and the VA will augment their case lists using clinically relevant HMO or health system administrative data. The DFCI/CRN and the VA will be referred to as ‘provider-organization-based’ sites. In some sites, the study team will attempt to enroll all patients from certain demographic subgroups (e.g., AfricanAmerican colorectal cancer patients in Alabama). In instances where the number of diagnosed cases in a demographic subgroup exceeds the number needed for enrollment, potential participants will be chosen randomly from the sequence of incident cases. Participants in the health care provider survey will all have participated in the diagnosis or care of the patient participants. The details of the sampling and enrollment plans are found in Sections 4 and 5. It is particularly important that the results from the study be as generalizable as possible and, consequently, that there be as few restrictions on eligibility for enrollment as is feasible. Appendix C contains an eligibility checklist reflecting the criteria in Section 3.2. 3.2 Inclusion Criteria for Patient Participants There are no exclusions based on patient race, gender, or ethnicity. 3.2.1 A participant must have a histologically or cytologically confirmed diagnosis of colorectal or lung cancer. The tumor must be one of the eligible subtypes listed in Appendix C. These subtypes include over 95% of all cancer of the lung and colon/rectum. 3.2.2 The cancer must be invasive (in-situ diagnoses are excluded). 3.2.3 The cancer must be a primary tumor of the lung, colon, or rectum (metastases to lung or colorectal sites from other primaries are excluded). 3.2.4 The cancer must be a first primary, that is, the patient must not have had a prior invasive cancer of the lung or colon/rectum. See exception in the following paragraph regarding simultaneous diagnoses. Simultaneous diagnoses are defined as two separate primary tumors, of the same or different sites, diagnosed within a two month period (based on SEER) definition. Persons having simultaneous diagnoses (within 2 months) at different sites are not eligible for CanCORS. However, persons having more than one primary tumor of the same site (that is, two lung primaries or two colon primaries) within 2 months are eligible for CanCORS. At least one of the diagnoses must occur with the eligible ascertainment period for CanCORS. 3.2.5 The cancer must be a new diagnosis; that is, patients, who have a recurrence of a lung or colorectal cancer diagnosed prior to the ascertainment period, are not eligible. 3.2.6 For the 5 geographically based PDCR sites, a study participant must be a resident of the PCDR-targeted geographic region at the time of diagnosis and initial contact. For the provider-organization-based DFCI/CRN and VA sites, a participant must either be enrolled in one of the CRN health plans or be a regular fee-for-service patient at the 5 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 time of diagnosis and initial contact or must be receiving medical services at one of the Veterans Affairs Medical Centers participating in the study. 3.2.7 The participant or the surrogate respondent must be able to complete the interview in English, Chinese (Mandarin or Cantonese), or Spanish. 3.2.8 A participant must be 21 years of age or older at the time of diagnosis. 3.2.9 An eligible surrogate respondent may complete the baseline interview for participants who do not wish to be interviewed or who are too ill to be interviewed or have died. A surrogate respondent for a participant who is alive at the time of the initial contact must meet the following criteria: 3.2.9.1 A surrogate respondent must be of majority age in the state in which the patient resides. 3.2.9.2 For patients alive at initial contact, the surrogate respondent must have been identified by the patient as being familiar with the participant’s care since diagnosis. 3.3 Exclusion Criteria for Patient Participants 3.3.1 Patients incarcerated in penal institutions are not eligible. 3.4 Inclusion Criteria for Health Care Provider Participants 3.4.1 Only physicians who have participated in the diagnosis or care of patient participants are eligible for participation. 3.4.2 Physicians must come from one of the following subspecialties: primary care physicians, gastroenterologists, pulmonologists, surgeons, medical oncologists, and radiation oncologists. 4. Enrollment Procedures 4.1 Overview This study will enroll patient participants with lung or colorectal cancer during the period from September 2003 through to approximately June 2005. Because not all sites began enrolling at the same time, all enrollment goals for cancer patients assume an 18-month enrollment period. Some sites may complete enrollment in less than 18 months. The study will also invite health care providers of these patients to participate in a survey. The detailed enrollment procedures for physicians participating in the survey are given in Section 6.5 and Appendix M. The enrollment process for participants diagnosed with lung or colorectal cancer consists generally of the steps outlined below. There may be local modifications to these steps in certain PDCR sites. Appendix A provides detailed enrollment procedures for this site. For DFCI/CRN and the VA, incident cases are identified either by a collaborating registry or using administrative and tumor registry records. Basic patient identifying and demographic information, including the patient name, contact information, race/ethnicity, date of birth, and cancer type are transmitted to the PDCR Principal Investigator or designee in the relevant geographic area. For PDCR sites that are not over-sampling based on race or ethnicity, the race/ethnicity need not be sent by the case ascertainment facility. The patient is screened for eligibility by the PDCR site staff. Appendix C contains a detailed checklist for eligibility screening based on the criteria in Section 3. The patient is either selected directly for participation (if a member of a demographic subgroup that was identified for complete enrollment from a PDCR site) or is randomly selected using a sampling probability designed to achieve overall enrollment goals in the patient’s demographic subgroup. 6 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 If the patient is selected for recruitment, study sites will notify the patient’s physician if required by the local Institutional Review Board (IRB) Registry or HMO entities. The procedures and requirements for this site are specified in Appendix A. Once local requirements for physician notification are met, the patient is sent a letter and brochure explaining the study, asking for his/her participation, and informing the patient that a member of the PDCR site study team will be calling to schedule an interview. The letter will contain a toll-free telephone number that the patient can call if s/he has questions or if s/he does not want any further contact from the study. Appendix J provides a sample patient contact letter. For six of the sites, the patient is called at the scheduled time and, with patient consent, the baseline patient survey is conducted. In the seventh (VA), patients with a medical appointment in the VA within 12 weeks of diagnosis will be approached by trained research assistants at the time of the appointment and will be provided with information and informed consent procedures in person. Once a patient is enrolled, his/her information will be transmitted to the PDCR site for telephone interview. If the patient does not have an appointment within that time period, the same procedures used by the other sites will be applied. The introductory scripts for the in-person recruitment and telephone interview will explain all aspects of study participation, including the follow-up survey, a forthcoming request for permission to abstract data from the patient’s medical records, and the anticipated use of Medicare claims data. If the patient is unable to complete the full version of the telephone survey, s/he will be given the option of participating in an abbreviated version of the telephone survey, or designating a surrogate respondent. Appendix D, the full patient survey, provides the interview scripts that will be used to present these options to the patient. At the end of the telephone survey, the interviewer will explain again the value and purpose of obtaining data from the participant’s medical records and Medicare claims. The interviewer will inform the participant that a consent form allowing the study team to obtain these data will be sent by U.S. mail the next day, unless already obtained prior to the interview. Some CRN sites may not require active consents for medical record review. For patients who are alive at the time of a conducted survey (primary or surrogate respondent), no data will be abstracted from medical records without the patient’s written consent (with the exception of some CRN and VA sites that have prearranged permission to abstract information from patient's medical records for research studies). For patients who have died before initial contact, consent for review of medical records will be determined in a way that is consistent with local regulations. To minimize the effects of time since diagnosis in patient responses, all baseline patient surveys should be administered between 12 and 18 weeks since diagnosis whenever possible. A survey of the PDCR geographically based sites has indicated that this is the earliest time that the majority of interviews could be scheduled after case ascertainment, physician notification, and patient contact. No participant should complete a survey earlier than 12 weeks from diagnosis or beyond 12 months post-diagnosis. Refer to Table 6.2 for the priority window for interviewing. For the purpose of case ascertainment and interview timing, date of diagnosis is the date of cancer diagnosis recorded by the cancer registry transmitting the patient contact information to the PDCR site. PDCR sites will attempt to enroll any patient ascertained by the site within 6 months from diagnosis even if the interview cannot be scheduled until a date later than 6 months after diagnosis. PDCR sites will sample randomly (with sampling probability 0.20, for a 20% random sample) from the set of cases ascertained more than 6 months following the date of diagnosis to learn about the reasons for delay and about the characteristics of these patients and their health care setting. 7 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 In addition to the core study data, each PDCR site will maintain a database of all patients ascertained, the patients selected for participation from the ascertained cases, and the reasons for not enrolling patients from the subset selected for enrollment. This database will be de-identified and transmitted to the SCC monthly for monitoring of the enrollment process. The number of attempts to contact patients for the baseline survey is at the discretion of the PDCR site. However, once patient contact has been made, if there is continued scheduling conflicts, a cut-off will occur after 5 actual contacts have been made with the patient to attempt to a schedule a time for the interview. If not previously appropriate, during the fifth actual contact with the patient, an attempt should be made to conduct a surrogate interview. 4.2 Summary of Participant Consenting Procedures The elements of patient consent are summarized here. All potential participants for whom physicians do not advise against participation will be mailed initial contact letters explaining the study (see Appendix J) and given a toll-free number to call to obtain more information. Patients at the VA PDCR site who have a clinic visit or admission scheduled within 12 weeks of diagnosis will be approached by trained research assistants at their visit. The research assistants will explain all aspects of participation and obtain written consent if the participant desires. At initial telephone contact, interviewers will explain all aspects of participation in the study at the beginning of the interview. Patients will give verbal consent to participation by indicating at that time if they wish to continue with the interview. All potential participants not excluded by physicians will be mailed a medical record review consent form unless they already signed one at the time of in-person recruitment at the VA site. For participants completing a telephone interview, or for instances in which a surrogate respondent has completed the interview, the medical record consent form will be mailed following the interview. (Some CRN sites may not require active consents for medical record review, but these sites will inform study participants during the interview that their survey responses will be combined with other health information contained in health plan files.) The medical record consent mailing will include a letter explaining the value of data in the medical records. It will also include a form for written consent of the use of Medicare claims data in the study. For patients not known to have died at the time of scheduled medical records review, no medical records will be reviewed without a signed medical record consent form. For patients who were deceased at initial contact for the baseline survey or who are known to have died by the time of scheduled medical record review, medical records will be reviewed in a manner consistent with the regulation of the facility or physician responsible for the record. The provider survey will include an assurance at the beginning of the survey that physician names or other directly identifying information will not be stored in the SCC database. The opening language of the survey will also explicitly state that completion of the survey will be regarded as consent to participate. 4.3 Participation Incentive Patients will be offered an incentive with a monetary value of $10 to $20 for participating in the study. The form of the incentive (cash, gift certificates, phone cards, etc) will vary from site to site. Sites will implement different strategies and use different forms of additional incentives to encourage nonresponders to participate. See Appendix A for more detailed information regarding this site. 8 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 Physicians participating in the health care provider survey will be offered an incentive of approximately $20 in value. 4.4 Definition of Enrolled Patient Participant Any participant who consents to the patient survey and who provides responses beyond the introductory script will be considered an enrolled participant. If an appropriately selected surrogate provides responses, the participant will also be considered enrolled. A patient who provides consent for medical record review but who does not consent to participate in any form of the survey will also be considered an enrolled case once a medical records consent form has been signed and returned to the PDCR site. During the enrollment period, the Statistical Coordinating Center and the CanCORS Participation Monitoring Committee will monitor enrollment rates and the types of data available for each enrolled case. If more than 5% of the participants in any PDCR site who agree to provide medical record data do not complete any version of the baseline survey, the Steering Committee and the Principal Investigator for that PDCR site will consider increasing the enrollment goals for that site. 4.5 Assisted Interviews If a patient is being interviewed and cannot remember the response to a question (e.g., when was your surgery), it is acceptable for the patient to ask a caregiver, and then provide the caregiver’s response. However, if a patient is cognitively able and willing to participate in a survey, but too weak to hold the phone for an interview, it is not acceptable for the caregiver to respond. In this case, attempts should be made to schedule a surrogate interview. 5. Study Design 5.1 Summary of Enrollment Goals In the patient survey, we intend to enroll a total of 5214 patients with colorectal cancer and 5617 patients with lung cancer as subjects for either the patient survey or the surrogate respondent survey. In some sites, we will oversample minority racial/ethnic groups. For medical record review, we expect to obtain patient consent and abstract records for 85% of the patients who participate in the patient survey (4432 patients with colorectal cancer, 4774 patients with lung cancer). We estimate that medical record data will be available for only a small fraction of patients for whom we do not have any survey data (primary or surrogate); we estimate that we will have survey data for approximately 98% of patients for whom we have medical record data. Thus we expect to have medical record data for a total of 4522 patients with colorectal cancer and 4871 patients with lung cancer. Total patient enrollment in the study, including all patients enrolled in the patient survey, the medical record review, or both, is therefore targeted to be 5304 patients with colorectal cancer and 5714 patients with lung cancer. In the health care provider survey, we expect to obtain completed surveys from 608 gastroenterologists, 839 pulmonologists, 3027 primary care physicians, 1891 general surgeons, 90 colorectal surgeons, 428 thoracic surgeons, 945 medical oncologists, and 450 radiation oncologists. The baseline patient survey is the initial and primary mode of contact for all participants; the enrollment goals for data from the other instruments follow from the sampling design for the baseline survey. The following subsections contain the detailed rationale for these sample size projections, beginning with the patient survey. Because the populations in this study have not been studied using rapid case ascertainment in several geographic areas simultaneously, all response rates are estimated. If the pre-study estimates are found to be substantially in error, the study Steering Committee will discuss possible revisions to the enrollment goals or enrollment period. The strategies for converting nonresponders into study participants, and 9 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 some of the details of sampling and enrollment schedules, are PDCR–specific. The strategy for this site is described in Appendix A. 5.2 Principles for the Enrollment Goals for the Patient Survey Two primary considerations motivate the sampling design: (1) to obtain samples that are representative of the study areas, and (2) to obtain sufficiently large samples representative of various racial/ethnic groups to make it possible to investigate the causes and correlates of disparities in care by race/ethnicity. (The term “race/ethnicity” is used here to refer to primary categories derived from the Office of Management and Budget categories used in federal programs, i.e., Hispanic, non-Hispanic white, non-Hispanic black, Asian-American, American Indian, and others. More detailed ethnic categories do not play a role in the sample design.) Thus, the study will oversample certain racial and/or ethnic subpopulations in sites where it is possible to substantially increase participants in those subgroups. For most sites, target enrollment is approximately 1000 survey participants for each disease (colorectal cancer or lung cancer) being studied at that site. Iowa will enroll patients with only lung cancer; UNC and the Temple VA (at this time) will enroll patients with only colorectal cancer. The Alabama site has a target enrollment of 700 cases for each cancer type, as originally proposed and budgeted. Specific goals by race/ethnicity at each site have been set to optimize power for race/ethnicity comparisons within the constraints set by anticipated accrual within the scheduled recruitment period and anticipated participation rates. For comparison of two groups (typically white and black, specifically at Alabama and North Carolina), this suggests approaching equal numbers for the two race groups. For the sites where there are four major race/ethnic groups (whites, blacks, Hispanics, Asian-Americans, specifically in Los Angeles and Northern California), a breakdown of 400 whites and 200 in each minority race/ethnicity provides a good compromise between efficient estimation of comparisons and efficient estimation of statistics that cut across the combined population, such as overall means or rates or contrasts of clinical groups that are not strongly related to race. However, the actual enrollment targets are also limited by the number of incident cases in the planned enrollment periods and by the rates at which these cases will be identified and will consent to participate in the study. 5.3 Enrollment and Participation Assumptions for the Patient Survey and Medical Record Review Tables 5.1 and 5.2 summarize the incidence and survey participation assumptions for each of the PDCR sites for colorectal and lung cancer. For each site, incidence and participation are estimated by race/ethnicity, but the breakdown of groups differs by site because of differences in groups that have substantial representation at the different sites. (“NH” represents nonHispanic, as in “white non-Hispanic”, etc.) Totals across races are shown for each site; also, a subtotal is given for the DFCI/CRN sites. Totals by race across sites appear at the bottom of the tables. The first numerical column projects the number of incident cases in 18 months. The exception is Los Angeles, for which all calculations are based on a 12-month enrollment period, because projected incidence is high enough to make it possible to recruit target sample sizes within that period. The second numerical column shows the percentage of incident cases that will be sampled for the 18-month period; these cases will be contacted and asked to participate in the study. These percentages reflect sampling rates during the accrual period; considerations affecting these rates are discussed below. For the Northern California site, it also reflects shortening of the accrual period to less than 18 months and limitations on identification of cases falling into race/ethnic strata. Details for this specific site appear in Appendix A. The third column is the product of the first two and shows the anticipated number of cases that will be sampled for contact. 10 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 The fourth numerical column is the projected participation rate. This represents the percentage of all sampled cases that are expected to participate in the patient survey, and reflects a loss of sample cases for all reasons, including ineligibility, lack of adequate contact information, and refusal. Anticipated participation rates are based on the local experience of sites in similar studies. Some non-uniformity in these projections is allowed because sites are dealing with local variation in the percent of the population speaking one of the translated languages of the survey (i.e., Spanish or Chinese), as well as attitudes toward survey participation, and the relationship between the patients and the relevant PDCR. Some sites have projected different participation rates for different race/ethnic groups, again reflecting a variation in language mix, local experience, and the socioeconomic mix associated with ethnicity in their areas. The fifth column in the tables is the product of the projected sample size and the projected participation rate, and represents the projected enrollment in the group at that site. Sampling and participation rates for subtotal and total lines are overall average rates calculated from total incidence, sample size, and enrollment reported on that line. As of Amendment 3 dated September 2005, the Portland VA site has been dropped and the following sites added – Atlanta, Indianapolis, Houston, and Seattle. The overall enrollment goals for the VA remain unchanged. 11 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 Table 5.1: Patient Survey Enrollment Goals by PDCR Site for Participants with Colorectal Cancer. Site Alabama No Carolina No California LosAngeles CRN: HFHS CRN: HPHC CRN: GHC CRN: Hawaii CRN KPNW CRN total Incident cases Sampling rate Sampled cases White+Other Black Site total 2160 640 2800 41% 100% 55% 888 640 1528 50% 40% 46% 444 256 700 162 White+other Black Site total 1478 432 1910 60% 100% 69% 883 432 1315 78% 72% 76% 689 311 1000 214 WhiteNH BlackNH Hispanic AsianNH Site total 2960 299 356 453 4068 43% 43% 71% 71% 48% 1265 128 252 320 1965 56% 54% 50% 30% 51% 709 69 126 96 1000 63 107 85 WhiteNH/Oth er BlackNH Hisp AsianNH Site total 2042 424 532 396 3395 54% 100% 100% 100% 73% 1111 424 532 395 2462 45% 37% 37% 37% 41% 500 157 197 146 1000 119 141 113 WhiteNH BlackNH Site total 118 110 228 100% 100% 100% 118 110 228 75% 70% 73% 89 77 166 41 WhiteNH BlackNH AsianNH Site total 121 6 5 132 100% 100% 100% 100% 121 6 5 132 75% 75% 75% 76% 91 5 4 100 5 4 WhiteNH BlackNH Hisp Asian NH Site total 351 11 1 16 379 100% 100% 100% 100% 100% 351 11 1 16 379 75% 75% 75% 75% 75% 263 8 1 12 284 8 1 11 WhiteNH BlackNH Asian Hawaiian Site total 41 2 72 33 148 100% 100% 100% 100% 100% 41 2 72 33 148 66% 60% 67% 50% 63% 27 1 48 17 93 1 17 10 WhiteNH Black NH Hisp Asian NH Other/Unkno wn Site total 298 7 2 6 100% 100% 100% 100% 298 7 2 6 65% 50% 40% 50% 194 4 1 3 7 320 100% 100% 7 320 50% 64% 4 206 (All races) 1207 100% 1207 70% 849 Race 12 Participation rate Respondents ESS vs. White 4 1 3 4 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 Table 5.1: Patient Survey Enrollment Goals by PDCR Site for Participants with Colorectal Cancer (cont’d). Site VA: NY Harbor VA: Baltimore VA: Durham VA: Nashville VA: Minneapolis VA: Chicago VA: Tucson VA: Portland VA: Biloxi VA: Temple VA Total ALL SITES Race Incident cases Sampling rate Sampled cases Participation rate Respondents ESS vs. White White+Other Black Site total 70 49 119 100% 100% 100% 70 49 119 70% 70% 70% 49 34 83 20 White+Other Black Site total 60 38 98 100% 100% 100% 60 38 98 70% 70% 70% 42 27 69 16 White+Other Black Site total 50 17 67 100% 100% 100% 50 17 67 70% 70% 70% 35 12 47 9 White+Other Black Site total 94 19 113 100% 100% 100% 94 19 113 70% 70% 70% 66 13 79 11 White+Other Black Site total 86 9 95 100% 100% 100% 86 9 95 70% 70% 69% 60 6 66 5 White+Other Black Site total 131 39 170 100% 100% 100% 131 39 170 70% 70% 70% 92 27 119 21 White+Other Black Site total 84 16 100 100% 100% 100% 84 16 100 70% 70% 70% 59 11 70 9 White+Other Black Site total 81 9 90 100% 100% 100% 81 9 90 70% 70% 70% 57 6 63 5 White+Other Black Site total 18 12 30 100% 100% 100% 18 12 30 70% 70% 70% 13 8 21 5 White+Other Black Site Total 41 27 68 100% 100% 100% 41 27 68 70% 70% 71% 29 19 48 11 White+Other Black VA Total 715 235 950 100% 100% 100% 715 235 950 70% 70% 70% 502 163 665 114 WhiteNH BlackNH Hisp AsianNH Other/UnKn/H awaiian 10284 2166 891 948 56% 92% 88% 86% 5792 1995 787 814 61% 53% 41% 38% 3508 1051 325 309 40 14330 100% 66% 40 9428 53% 55% 21 5214 13 731 250 233 14 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 Table 5.2: Patient Survey Enrollment Goals by PDCR Site for Participants with Lung Cancer. Site Alabama Iowa No California Los Angeles CRN: HFHS CRN: HPHC CRN: GHC CRN: Hawaii CRN KPNW CRN total Race Incident cases Sampling rate Sampled cases Participation rate Respondents ESS vs. White White+Other Black Site total 3690 810 4500 20% 100% 35% 752 810 1562 50% 40% 45% 376 324 700 174 White All other Site total 2442 59 2501 80% 100% 80% 1942 59 2001 50% 50% 50% 971 29 1000 28 WhiteNH BlackNH Hispanic AsianNH Site total 4403 587 421 637 6048 26% 26% 67% 68% 33% 1154 154 284 430 2021 56% 54% 50% 30% 49% 646 83 142 129 1000 74 116 108 WhiteNH BlackNH Hisp AsianNH Site total 2276 505 396 334 3511 50% 100% 100% 100% 68% 1136 506 395 333 2371 44% 41% 41% 41% 42% 500 205 160 135 1000 145 121 106 WhiteNH BlackNH Site total 292 200 492 100% 100% 100% 291 200 491 70% 65% 68% 204 130 334 79 WhiteNH BlackNH AsianNH Site total 145 16 4 165 100% 100% 100% 100% 145 16 4 165 75% 75% 75% 75% 109 12 3 124 11 3 WhiteNH BlackNH Hisp AsianNH Site total 351 3 14 14 382 100% 100% 100% 100% 100% 351 3 15 15 383 75% 75% 75% 75% 75% 263 2 11 11 287 2 11 11 WhiteNH BlackNH Asian Hawaiian Site total 72 2 71 38 183 100% 100% 100% 100% 100% 72 2 71 38 183 44% 50% 40% 38% 41% 32 1 28 14 75 1 15 10 WhiteNH BlackNH Hisp AsianNH Other/Unknown Site total 322 6 2 10 4 344 100% 100% 100% 100% 100% 100% 322 6 2 10 4 344 65% 50% 40% 50% 50% 64% 209 3 1 5 2 220 3 1 5 2 (All races) 1566 1566.4286 14 1040 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 Table 5.2: Patient Survey Enrollment Goals by PDCR Site for Participants with Lung Cancer (cont’d). Site VA: NY Harbor VA: Baltimore VA: Durham VA: Nashville VA: Minneapolis VA: Chicago VA: Tucson VA: Portland VA: Biloxi VA: Temple VA Total ALL SITES Race Incident cases Sampling rate Sampled cases Participation rate Respondents ESS vs. White White+Other Black Site total 72 50 122 100% 100% 100% 72 50 122 70% 70% 70% 50 35 85 21 White+Other Black Site total 62 38 100 100% 100% 100% 62 38 100 70% 70% 70% 43 27 70 17 White+Other Black Site total 110 37 147 100% 100% 100% 110 37 147 70% 70% 70% 77 26 103 19 White+Other Black Site total 124 26 150 100% 100% 100% 124 26 150 70% 70% 70% 87 18 105 15 White+Other Black Site total 112 11 123 100% 100% 100% 112 11 123 70% 70% 70% 78 8 86 7 White+Other Black Site total 108 33 141 100% 100% 100% 108 33 141 70% 70% 70% 76 23 99 18 White+Other Black Site total 210 40 250 100% 100% 100% 210 40 250 70% 70% 70% 147 28 175 24 White+Other Black Site total 109 11 120 100% 100% 100% 109 11 120 70% 70% 70% 76 8 84 7 White+Other Black Site total 60 40 100 100% 100% 100% 60 40 100 70% 70% 70% 42 28 70 17 White+Other Black Site Total — — — 100% 100% — — — 70% 70% — — — 0 White+Other Black VA Total 967 286 1253 100% 100% 100% 967 286 1253 70% 70% 70% 676 201 877 144 WhiteNH BlackNH Hisp AsianNH Other/UnKn/Haw aiian 14960 2330 833 1070 48% 85% 84% 81% 7132 1983 696 863 56% 48% 45% 36% 3986 961 314 311 101 19294 100% 56% 101 10774 45% 52% 45 5617 — 15 — 633 249 247 40 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 We anticipate that approximately 85% of those participating in the patient survey will give consent for medical record review. In addition, a small number (approximately 2% beyond the survey participants) will likely consent to medical record review but will be unwilling or unable to participate in the survey. Thus, projected numbers of enrolled cases (with patient survey, medical record review, or both) are as follows: Colorectal Cancer Lung Cancer 5214 4432 90 5304 5617 4774 97 5714 Survey participants Survey with medical record consent Medical record consent without survey Total enrollment 5.4 Patient Survey Sampling Plan This study will over-sample members of certain racial and/or ethnic subgroups at PDCR sites where that is feasible, within constraints imposed by incidence and participation assumptions. Table 5.3 qualitatively summarizes over-sampling plans by PDCR and race/ethnicity. Table 5.3: Summary of Oversampling Plans by PDCR Site. Site Oversampled Groups UAB African-Americans DFCI/CRN All cases sampled at 100% under current design and accrual projection Iowa African-Americans, Hispanics, Asian-Americans UCLA/RAND African-Americans, Hispanics, Asian-Americans UNC African-Americans HMS/NCCC Hispanics, Asian-Americans, Medicaid/uninsured from other race/ethnic groups VA All cases sampled at 100% under current design and enrollment projection The following considerations guided the projection of sampling rates: The sampling rates are determined to project total sample sizes of 1000 cases per site for each cancer, with some exceptions. The original UAB proposal called for enrolling 700 cases for each cancer, and that site is budgeted accordingly. The projected DFCI/CRN and VA enrollment rate will provide fewer than 1000 cases for colorectal cancer in 18 months, even with 100% sampling; the DFCI/CRN projected enrollment for lung cancer is slightly in excess of 1000. The identified “over-sampled groups” will be sampled at higher rates than whites in order to achieve desired sample sizes for comparisons. In most cases this implies sampling minority groups at 100%. In other cases, sampling rates for minority groups are less than 100% because target numbers of cases could be attained with sampling, but the sampling rate for minorities never falls below that for whites. Whites and minorities that are not targeted for over-sampling will be sampled at the same rate. Thus, for example, the small number of Asian American and Hispanic incident cases in North Carolina will be sampled at the same rate as whites, to facilitate site-wide estimates. For some sites a “white/other” category is defined to include such groups. At all sites at which there will be sampling, the sampling rates will be set initially to those displayed in Tables 5.1 and 5.2, which are based on statistics for incident cases from recent years. The rates may be adjusted during the study to reflect changes in racial distribution, unforeseen differences in participation rates by race, or either lower incidence rates or lower participation rates overall. For example, if a group’s number of incident cases falls short of projections, its sampling rate will be adjusted upwards. If a minority group is sampled at 100% but recruitment is slower 16 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 than anticipated, the sampling rate for groups sampled at less than a 100% will be adjusted upward to achieve the desired total sample size within the recruitment period. Initial determination of race for sampling purposes will occur during rapid case ascertainment (RCA) at most sites, using data routinely collected in RCA. Estimates from previous studies have shown that the RCA race data are accurate at most sites. Concordance between RCA and medical records was almost 99% in Alabama and over 96% in North Carolina; in both of these sites, almost all participants will be either white or African-American. In a Los Angeles study of breast cancer, most misclassification occurred through the classification of nonHispanic whites as Hispanic or vice versa; while this constituted a relatively small fraction of the white non-Hispanic population (<5%) it was substantial as a fraction of the smaller Hispanic group (around 20%). The sample for medical record abstraction is identical to that for the patient survey, since consent for abstraction is obtained as part of the survey process. We anticipate that approximately 85% of those who participate in the patient survey will give medical record consent. Thus, for analyses requiring medical record information (alone or in combination with the survey), the number of cases will be about 85% that for the survey alone. Patients or surrogates who are contacted but decline to participate in the survey will still be asked to consent to medical record abstraction. We expect only a small number of these, around 5% of all non-participants (or 2% of the nonrespondents, 1% of the entire sample), to consent to abstraction. Although these will make little contribution to primary analyses, there will be enough cases in this category (350 for colorectal cancer, 500 for lung cancer) to estimate some differences between participants in the survey and patients who decline participation. 5.5 Analysis Plans for Data from the Patient Survey and Medical Records No single method of analysis will be appropriate for the complex data that will be gathered in this project. In the simplest cases, standard methods for estimating the probability of a binary outcome (e.g., use of surgery in early stage lung cancer or use of adjuvant chemotherapy in colon cancer) or a population mean (e.g., a quality of life score) will be used for estimating population parameters with confidence intervals. Standard chi-square for contingency tables or t-tests can be used for comparing two or more groups with binary or continuous outcomes. The power calculations in Section 5.6 show anticipated standard errors for estimates of population characteristics and minimum detectable differences for comparing two groups for a variety of anticipated analyses. Many of the primary analyses will use regression models for estimating the association of one or more patient-level, physician-level, or health care system feature with an outcome of interest. For example, one of the analyses corresponding to primary objective 2.1.1 will model the binary response variable for the receipt of adjuvant chemotherapy following surgery for stage III colon cancer as a function of patient-level characteristics and attitudes or beliefs about the effectiveness of therapy. Other analyses will add surgeon or medical oncologist level variables to this analysis. Because the aim of this and similar analyses are explanatory and/or exploratory, a main goal of the statistical modeling for these analyses will be to find the model that best balances parsimony (as few independent variables as needed) and explanatory or predictive power. Consequently, it is not possible at the design stage to specify, even for this example, the exact form of the final regression model. There will be, however, some common issues encountered in the analyses and we will follow the general principles listed below whenever possible. The PDCR sites were not chosen randomly from regions of the United States, so study participants are not part of a stratified sample that can be recombined using standard sample survey methods to estimate national rates of processes of care. The best way to combine estimates from population quantities or effect sizes will be to estimate separate models from PDCR site-specific data, then combine estimates using 17 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 precision-weighted linear combinations. In some instances, we will estimate either stratified models, with PDCR sites as a stratification variable rather than as an explicit regressor, or, where justified, estimate models with PDCR site as an explicit regressor. For the sites using disproportionate sampling, case weights will be used to compute unbiased estimates of PDCR site-specific population parameters. The initial model of choice for binary outcomes will be logistic regression. In situations where there is a natural correlation caused either by clustering or a nesting of subjects within provider or health care facility, hierarchical models will be used. Graphical diagnostics for logistic regression will be used to detect cases (or clusters of cases) with high leverage or transformations of independent variables. The initial model of choice for continuous outcomes will be linear regression. In instances where the distribution or dimension of the dependent variable is not appropriate for standard linear regression, ordinary least squares will be replaced by generalized linear models or multivariate regression models. As with regression models for binary data, standard graphical diagnostics will be used to explore transformations of either the dependent or the independent variables and to detect cases with a large influence on the analysis, and hierarchical models will be used to account for clustering. We anticipate that the survey and medical record data will be subject to item-specific missingness. While no method is guaranteed to produce unbiased estimates in the presence of possible informative missingness, multiple imputations will be used for missing response items. In collaboration with the PDCR site investigators, the SCC statisticians will model the missing observations as a function of observable variables, and impute item-response missing data in the centrally archived data sets at the SCC. All data sets provided for analysis will contain the imputed data, along with the model for imputation and a recommended method of analysis. Exploratory regression analyses will, whenever possible, account for the possibility of the increased prediction error that results from over-fitting. Model selection procedures (e.g., stepwise regression methods) will attempt to reduce the effect of over-fitting through cross-validation, or the use of criteria that penalize models with large number of parameters, such as Mallow’s Cp. Because the data set is purely observational (i.e., there are no randomized assignments to therapies, providers, or health care facilities) causal inference about the effect of factors such as treatment received will be difficult. Patients self-select health care providers or health care plans, and may differ systematically across providers or plans and observed differences in outcome may be due to unmeasured patient-level variables that characterize the systematic differences among the patients. Two general approaches will be used to explore causal effects: (a) the use of the highdimensional information about patients in analyses that will posit no residual confounding, and (b) the use of instrumental variables. Each of the data sources will include variables that are likely candidates for instrumental variables. 5.6 Power Calculations for Analyses using Patient Survey and Medical Record Data The power calculations described in this section are based on primary analyses using data expected from the patient survey and medical record abstraction. (Power calculations using data from the provider survey are given in the next section.) We present power calculations for analyses that correspond to the first three primary research goals presented in Section 2.1. The calculations are defined by the populations being considered (either an entire disease cohort or a subpopulation defined by clinical or sociodemographic variables of interest) and by the nature of the estimates. The assumed 18 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 sample sizes for these calculations differ from those in Tables 5.1 and 5.2 by a factor of 85% representing the projected rate of consent to medical record review. For comparison groups defined by age or clinical characteristics such as stage, the distribution across groups is likely to be similar enough at all sites so that we can estimate power based on average proportions in the groups, such as the average percentage of colorectal cancer patients who are diagnosed in stage III. For comparisons of race groups, the proportions in different sites are too different to allow that approximation. For these comparisons, power calculations are based on an “effective sample size” (ESS) for comparison of a single race/ethnic group other than whites to whites. The ESS for a single site is defined by the formula nE =1/(1/nW + 1/nG), where nE =ESS, nW = sample size for whites, and nG = sample size for the comparison group. The ESS can be used in calculating the standard error (SE) of differences between groups; for example, SE=s/ n E for the difference of group means. Because our strategy for combined inferences across sites will be to combine site-specific analyses weighted according to their precision, the ESS for a combined analysis is the sum of the ESS for each site for the same analysis. ESS for each racial/ethnic comparison is shown in Tables 5.1 and 5.2 above, by site and in total. For one-sample (estimation) problems, including estimation of a single proportion and estimation of a regression coefficient, we present the standard error (SE) of the estimate. We frame most two-sample (testing) problems as comparisons of two proportions, since a twosample comparison of proportions is roughly equivalent to a logistic regression with a dichotomous categorical predictor variable. For two-sample problems, we present the minimum detectable difference (MDD), defined as the smallest true difference between groups for which there is power of 80% for a significant result in a two-sided 5% level test. Final analyses will be more complex, using multivariate regression methods to control for variables other than those mentioned in the power calculations below. This might either reduce or increase the power of the tests, depending on the correlations of the additional predictors with the primary variables of interest and the additional predictive power of the added predictors. Variations by race/ethnicity/SES in important processes of care: Three types of analyses are involved in addressing this research question: (1) to show the existence of racial/ethnic disparities in processes, (2) to identify an intervening process or characteristic that is significantly related to the focal process, and (3) to show that the intervening process or characteristic is also related to race/ethnicity. Calculations for chemotherapy in stage II/III rectal and stage III colon cancer are shown in Panel A of Table 5.4. We assume that 1/3 of colorectal cases are rectal cancer, the remainder colon cancer; stages II and III comprise 32% + 24% = 56% of rectal cancer cases and stage III comprises 24% of colon cancer cases. Thus 2/3 24% + 1/3 56% or 35% of all colorectal cancer cases are eligible for this analysis. We ignore variations in staging by race, which would have a minor effect on power calculations, and assume that about 70% of eligible patients receive chemotherapy. Minimum Detectable Differences (MDD) with 80% power are displayed in the table; thus, for example, a 9.4% black/white difference in chemotherapy rates would be detectable with 80% power. The MDD is presented on the next line for an intervening dichotomous variable with a roughly even split; this MDD is based on all eligible patients. Finally, MDD for racial/ethnic differences in the intervening variable appear on the next line. 19 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 Table 5.4: Effective Sample Size (ESS) and Minimum Detectable Difference (MDD) of Representative Primary Analyses. Colorectal cancer Lung cancer Panel A: Racial/ethnic differences in process of care ESS ESS MDD(%) MDD(%) Process differences vs. white Black NH 185 9.4% 105 12.5% Hispanic 63 16.1% 41 19.9% Asian NH 59 16.7% 41 20.0% Relation to intervening process N, MDD(p) for equal split 1551 6.5% 1098 7.7% Process differences vs. white (intervening) Black NH 185 10.3% 105 13.6% Hispanic 63 17.6% 41 21.8% Asian NH 59 18.2% 41 21.8% Panel B: Co-morbidity (CSS) as mediator of chemotherapy for younger/older patients N SE(CCS) SE (%chemo) Younger 884 0.027 1.2% Older 667 0.031 1.9% MDD 0.115 6.4% SE MDV Beta(Chemo on CCS) 1551 1.8% 5.1% Colorectal cancer Panel C: Receipt of chemotherapy for metastatic disease Number of cases MDD for 50-50 split MDD for 20-80 split 842 8.8% 11.1% Lung cancer 1671 6.3% 7.8% Similar calculations for curative surgery for stage I/II lung cancer patients appear in the adjacent columns, under the assumption that 23% of patients are so staged and about 70% receive curative surgery. Differences by age in receipt of effective care: Dividing the colorectal cancer population at 70 years of age, we project that about 43% of colorectal cancer patients are in the older group, and chemotherapy rates in younger and older groups are 85% and 50% respectively. An important intervening variable for age effects is co-morbidity, which might be quantified using the Charlson co-morbidity score (CCS); previous studies suggest that after categorizing this population as 0, 1, or 2 by that score, the proportions of patients in those categories are about 60%, 20%, and 20% respectively, so the SD of scores is about 0.8. Assuming conservatively the same SD within age class, the SE of the mean Charlson score in each group and MDD (at 80% power) between the groups is shown in the first part of panel B in Table 5.4. The corresponding values for percent receiving chemotherapy are also shown, assuming 85% receipt for the younger and 50% for the older group; the MDD for chemotherapy is 7.0%, less than the previously reported difference of approximately 35% 29. We next consider the regression of receipt of chemotherapy on Charlson scores. Based on the same distribution of scores, the SE of the regression coefficient (change in percentage of patients receiving chemotherapy for each point difference in Charlson) is 2.0%, and the minimum detectable value (MDV) with 80% power is 5.5%, about twice the coefficient for the relationship found in a preliminary study. 20 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 Chemotherapy for metastatic non-small cell lung cancer and colon cancer: A number of possible intervening factors have been proposed; we consider examples where the factor being studied is dichotomous with an equal split or with an 80%-20% split. We assume that 19% of cases are metastatic for colorectal cancer and 35% for lung cancer. MDD in chemotherapy rates for each split and cancer type are shown in Table 5.4, Panel C. 5.7 Power Calculations for Analyses of the Provider Survey 5.7.1 Estimates of the Number of Eligible Providers Table 5.5 shows the estimated number of physicians who will provide either cancer diagnosis or care information for lung or colorectal cancer in the seven PDCR sites. The estimates are drawn from the 2002 Area Resource Files (ARF) for the Northern California, LA, Alabama and North Carolina sites, from Iowa registry data for the Iowa site, and from estimates of physicians participating in cancer care at the provider-organization-based sites in the CRN and the VA. Based on registry data from HMS/NCCC we estimate that 60% of general surgeons in the community treat colorectal cancer patients. We also estimate that approximately 10% of thoracic surgeons perform only cardiac surgery. Finally, because the ARF did not report data for medical oncologists, we use projections on the number of incident cases at each site and the number of medical oncologists in the LA area to estimate the number of medical oncologists at sites where other data were unavailable (Northern California and North Carolina). The number of medical oncologists in Alabama was obtained from the Medical Association for the State of Alabama. Power calculations and sampling plans are based on these preliminary estimates. We will update sampling plans as needed as better data become available during the enrollment period. Table 5.5: Estimated Number of Physicians Involved in the Care of Subjects in PDCR Regions, by Specialty Number of Physicians PCP Gastroenterology Pulmonology Medical Oncology Radiation Oncology General Surgery Colorectal Surgery Thoracic Surgery Surgeons, unspecified 127e VA 432h 89h 93h 97h All sites 19172 1027 839 945 44 b 302 c 48b 253c 37h 102h 452 2059 — 40f 14 b 69 d 7b — 10h 29h 90 428 — — — — 84 CRN 976a 47a 36a 44a NCCC 5866b 282b 223b 315e LA 5922b 334b 302b 207e Iowa 1653f NC 1838b 141b 70f 49f UAB 2485b 134 b 115 b 106 g 19a — 128b 573c 138b 661c 38f 169f — — 26b 137d 33b 153d 84a — — a Number of physicians in 5 CRN sites Obtained from the ARF c 0.6* number of general surgeons reported in ARF d 0.9* number of thoracic surgeons reported in ARF e Projected based on number of incident cases and number of medical oncologists in LA based on data from prior study. f Obtained from Iowa registry data. g Obtained from Alabama Medical Association data. h Number of physicians in 11 VA sites b 21 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 5.7.2 Analysis Goals We plan to survey providers in three broad categories: physicians involved in the decisions to refer patients to cancer specialists; physicians involved in treatment decision-making and/or providers of cancer treatments; and physicians involved in the management cancer patients’ symptoms. The sample size calculations for the provider survey are based on seven high priority research hypotheses that relate to these three roles: Referral Hypotheses: Hypothesis 1: Patients with metastatic non-small cell lung cancer treated by physicians who believe chemotherapy is a highly effective treatment will be more likely to be referred to an oncologist compared to patients treated by physicians who do not believe chemotherapy is a highly effective treatment. Hypothesis 2: Elderly patients with colorectal cancer appropriate for curative chemotherapy (stage III colon; stage II/II rectal) treated by physicians with a high proportion of elderly cancer patients will be more likely to be referred to a medical oncologist compared to patients treated by physicians with a low proportion of elderly cancer patients. Treatment Hypotheses: Hypothesis 3: Patients with metastatic non-small cell lung cancer who discussed treatments with physicians who believe chemotherapy is a highly effective treatment will be more likely to receive chemotherapy compared to patients who discussed treatments with physicians who do not believe chemotherapy is a highly effective treatment or patients who did not discuss chemotherapy with any providers. Hypothesis 4: Elderly patients with colorectal cancer appropriate for curative chemotherapy who discussed chemotherapy with physicians with a propensity to prescribe chemotherapy to elderly patients will be more likely to undergo curative chemotherapy compared to patients who discussed chemotherapy with physicians with less propensity to prescribe chemotherapy to elderly patients or patients who did not discuss chemotherapy with any physicians. Symptom Management Hypotheses: Hypothesis 5: Patients who have their symptoms managed by physicians who have positive beliefs about end-of-life care will have less unmet need for symptom management compared to patients managed by physicians with less positive beliefs about end-of-life care. Hypothesis 6: Patients who have their symptoms managed by physicians who do not have positive beliefs about end-of-life care will report greater severity of symptoms compared to patients managed by physicians who do have positive beliefs about end-of-life care. Hypothesis 7: Patients with metastatic cancer who have their symptoms managed by physicians who do not have positive beliefs about end-of-life care will report greater decline in physical functioning (because their physicians did not recognize and treat their symptoms) compared to patients managed by physicians who do have positive beliefs about end-of-life care. 5.7.3 Power Estimates We have estimated power to test each of these hypotheses as a function of the rate at which we plan to sample providers according to their role in the care of participants and a range of plausible response rates to the provider survey. The sampling rate and the expected response rate are used to compute the expected number of completed provider surveys and thus the associated number of patients 22 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 with complete data that will be available in each analysis. For example, if we sample 100% of providers with whom patients report discussing chemotherapy and 80% of these providers complete the survey, data from 80% of the relevant patients will be available for analyses linking characteristics of the providers obtained from the provider survey to patient treatments and outcomes. These power estimates are slightly overstated, since they do not account for the effect of weighting analyses to reflect differential non-response rates to the provider survey. To estimate power to detect the effect of provider characteristics on the types of treatments received by patients and their outcomes, we assumed that primary analyses will use regression models fit to patient level data and that these models will account for the clustering of patient treatments and outcomes within providers (see Section 5.5 for more discussion of the planned analyses). For simplicity, we consider a simple twogroup comparison with an equal number of participants in each group. For example, for the first hypothesis we assume that half of the advanced stage non-small cell lung cancer patients will discuss treatments with physicians who believe chemotherapy is highly effective. We have adjusted the power calculations to account for the dependence among patient responses within providers assuming a moderate level of clustering of patient providers (intraclass correlation=10%). We have estimated the minimum detectable difference (Table 5.6), defined as the smallest true difference between groups for which there is 80% power for a significant result in a two-sided 5% level test for each hypothesis. For binary dependent variables, the detectable differences in Table 5.6 are expressed as the absolute differences in the percent of patients with a positive outcome between the two groups of interest. The assumed percent of patients with a positive outcome overall is also reported (column 6 of Table 5.6). For continuous response variables, the detectable differences are expressed as percentages of the standard deviation. The following additional assumptions were made for each hypothesis. Referral Hypotheses: Hypotheses 1: Approximately 1671 patients will have metastatic non-small cell lung cancer (35% of the 4774 enrolled lung cancer patients with medical record and survey data). To estimate the number of referral providers that will be associated with these patients, we assume that 50% of these patients will identify one of the approximately 838 pulmonologists as their referring provider, and the remaining patients will be treated by a unique physician of another specialty, mainly primary care physicians. Thus the sampling frame for this question will contain approximately 1671 physicians (approximately 1patient per physician). Hypotheses 2: Approximately 667 elderly colorectal patients will be appropriate candidates for curative chemotherapy (35% of 4432 enrolled colorectal patients with medical record and survey data will have stage II/III rectal or stage III colon cancer; 43% of these will be over 70 years of age). To estimate the number of referral providers that will be associated with these patients, we assume that each of these patients will identify a unique physician as their referring provider (85% will be general surgeons, 10% colorectal surgeons, and 5% primary care physicians). The sampling frame for this question will contain approximately 667 physicians (1 patient per physician). Treatment Hypotheses: Hypotheses 3: Approximately 1671 patients will have metastatic non-small cell lung cancer (35% of the 4774 enrolled lung cancer patients with medical record data). To estimate the number of physicians involved in discussions of chemotherapy with these patients, we assume that 80% of these patients will be 23 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 treated by one of the approximately 945 medical oncologists, and the remaining 334 patients will discuss chemotherapy with a unique physician (a mixture of pulmonologists and primary care physicians). The sampling frame for this question will contain approximately 1400 physicians (1.2 patients per physician). Hypotheses 4: Approximately 667 elderly colorectal patients will be appropriate candidates for curative chemotherapy (35% of 4432 enrolled colorectal patients with medical record data will have stage II/III rectal or stage III colon cancer; 43% of these will be over 70 years of age). To estimate the number of physicians involved in discussions of chemotherapy for these patients, we assume that 70% of these patients will discuss chemotherapy with one of the approximately 945 medical oncologists, and the remaining patients will discuss chemotherapy with a unique physician (a mixture of gastroenterologists and primary care physicians). The sampling frame for this question will contain approximately 667 physicians (1 patient per physician). Symptom Management Hypotheses: Hypotheses 5 and 6: Approximately 5797 patients will report at least one symptom (pain, fatigue, depression, cough, nausea/vomiting; 75% of enrolled lung cancer patients with medical record data and 50% of the enrolled colorectal cancer patients with medical record data). To estimate the number of physicians involved in managing these patients’ symptoms, we assume that 50% will be treated by one of the approximately 945 medical oncologists, and that the remaining patients will have their symptoms treated by a unique physician (PCP, or other). The sampling frame for this question will contain approximately 3850 physicians (1.5 patients per physician). Hypothesis 7: Approximately 2262 patients with either lung or colorectal cancer will have metastatic cancer and report at least one symptom (pain, fatigue, depression, cough, nausea/vomiting; 90% of patients with metastatic disease report at least one symptom). To estimate the number of physicians involved in treating these patients’ symptoms, we assume that 40% will be treated by one of the approximately 945 medical oncologists, and that the remaining patients will have their symptoms treated by a unique physician (PCP, or other). The sampling frame for this question will contain approximately 2262 physicians (1 patient per physician). Table 5.6 shows estimates of the minimum detectable difference for each hypothesis, expressed as the absolute differences in the percent of participants with a positive outcome between the two groups of interest. 24 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 Table 5.6: Minimum Detectable Differences in Analyses Linking Data from Provider Survey to Patients’ Treatments and Outcomes Expected Expected Baseline Minimal number of number of Sampling Response Rate of Detectable Hypothesis completed patients Rate (%) Rate (%) Dependent Difference physician available for Variable (%) (%) surveys analysis Referral Hypotheses 1 1 2 100% 2 80 1128 1128 80 6.7 50 705 705 80 8.4 80 534 534 70 11.1 50 334 334 70 14.1 Treatment Hypotheses 3 3 4 100% 4 80 971 1128 45 8.4 50 607 705 45 10.6 80 534 534 60 11.9 50 334 334 60 15.0 Symptom Management Hypotheses 5 80 2841 4190 20 3.5 5 50 1776 2619 20 4.5 80 2841 4190 5 1.9 50 1776 2619 5 2.4 7 80 1622 1622 7 50 1014 1014 6 6 100% Continuous measure 13.9 17.6 5.7.4 Summary of Health Care Provider Survey Enrollment Goals Sampling of physicians involved in treatment: We plan to sample 100% of physicians involved in discussions of chemotherapy, radiation, and surgery. Power estimates for hypotheses 3 and 4 suggest that we will have 80% power to detect at least a 15 percentage point difference in treatment rates as a function of provider characteristics. Thus we plan to survey approximately 945 medical oncologists, and 450 radiation oncologists, and 2493 surgeons. The number of patients who discuss treatments with primary care physicians and/or other medical sub-specialists likely varies widely by stage, cancer site, and PDCR site. Thus the number of nononcologists that will be identified by patients as being the primary physician with whom they discussed initial treatment decisions is hard to estimate. We will also sample 100% of these physicians. Sampling of referral physicians: We plan to sample 100% of physicians involved in decisions to refer colorectal patients to chemotherapy and radiation providers and 100% of physicians involved in the decisions to refer lung cancer patients to surgeons, chemotherapy and radiation providers. Power estimates for hypotheses 1 and 2 suggest that we will have 80% power to detect at least a 15 percentage point difference in referral rates as a function of provider characteristics. We expect to identify approximately 2189 PCPs, 839 pulmonologists, and 608 gastroenterologists as being involved in referral decisions in addition to the cancer specialists who will already be sampled because of their role in providing treatments. 25 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 Sampling of physicians involved in the management of patients’ symptoms: We plan to sample 100% of the physicians involved in the management of patients’ symptoms. Power estimates for a rare outcome such as experiencing quite a bit of pain or symptoms (hypothesis 6), suggest that we will be able to detect at least a 2.5 percentage point difference. We will also have sufficient power to detect a 5 percentage point difference (a quarter of the baseline rate) in a more frequent outcome such as unmet need for symptom control or experiencing moderate symptoms. Finally, this sampling plan provides sufficient power to detect effect sizes that are 20% of the standard deviation for a continuous outcome (such as physical functioning), even in a small subset of patients (hypothesis 8; patients with metastatic cancer reporting at least one symptom). Assuming approximately 10% of patients will identify a new physician (one not involved in either referral or treatment roles), we estimate that we will survey an additional 838 primary care providers to study the management of patients’ symptoms. Table 5.7: Provider Survey Sample Design Provider Expected Sampling DFCI/ HMS/ UCLA/ Iowa UAB UNC Role Provider Type Rate CRN NCCC RAND Medical Oncology 100% 44 315 207 49 106 127 Radiation Oncology 100% 19 128 138 36 44 48 Physicians General Surgery 100% -573 661 -302 253 involved in primary Colorectal Surgery 100% -26 33 -14 7 treatments Thoracic Surgery 100% -137 153 40 69 --Surgeons unspecified 100% 84 ----d Decision to Generalist 100% 354 340 340 340 238 -refer lung pts Pulmonology 100% 36 223 302 70 115 -to surgeona Decision to Generalistd 100% 36 43 43 -30 43 refer CRC pts to chemo Gastroenterology 100% 47 128 128 -89 128 providerb Symptom Generalistd 100% 161 170 170 85 119 85 Managementc Total # of Surveys 780 2081 2174 620 1127 690 a b c d All sites 97 945 37 450 102 1891 10 90 29 428 102 84 VA 351 1962 93 839 33 227 89 608 48 838 889 8360 Assumes that 40% of lung patients will identify a pulmonologist as the physician most involved in decisions to refer the patient to a surgeon, 40% of patients will identify a generalist in this role, and the remaining 20% will identify a cancer specialist (medical or radiation oncologist). We have also assumed that approximately 100% of providers most involved in decisions to refer lung cancer patients to chemotherapy and radiation providers will have already been identified as either one of the cancer specialists or as the provider responsible for referral for surgery and thus few additional providers will be surveyed solely because of their role in referring lung cancer patients to either chemotherapy or radiation providers. Assumes that 80% of CRC patients will identify another cancer specialist (primarily a surgeon) as the physician most involved in decisions to refer the patient to a chemotherapy provider and the remaining 20% of patients will identify a generalist (5%) or a gastroenterologists (15%) in this role. We have also assumed that approximately 100% of providers most involved in decisions to refer CRC cancer patients to radiation providers will have already been identified as either one of the cancer specialists or as the provider responsible for referral for chemotherapy and thus few additional providers will be surveyed solely because of their role in referring CRC cancer patients to radiation providers. We will not survey providers solely because of their involvement in the decision to refer CRC patients for surgery. Assumes that 10% of lung cancer and CRC patients will identify a new generalist (i.e., not one involved in previously specified roles) as the provider most likely to know about their symptoms. Includes generalists identified by the patient as being the physician filling appropriate role which may or may not be the physician that the patient identifies as his or her PCP. 26 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients 6. Protocol 001 Amendment #3, December 2005 Description of Data Sources 6.1 Overview This section contains general descriptions of all data sources and data collection instruments, including the domains of interest in the primary respondent patient survey, the general design of the medical record abstraction process, and the domains of interest in the health care provider survey. Section 6.6 briefly discusses some of the public use data sources that the study will use to augment study data. 6.2 Baseline Patient Survey 6.2.1 General Design The baseline patient survey will obtain information from participants regarding their cancer diagnosis and treatment, quality of life, experience of care, health habits, and other medical conditions, as well as demographic information, including insurance and income (see Appendix D). Most items for the survey are either verbatim or adapted from the following survey instruments: California Health Interview Survey, Los Angeles Women’s Health Care Study, the QualityMetric SF-12, version 2, the QualityMetric Vitality Scale, Medical Outcomes Study Social Support items, EORTC QLQ-30, EORTC-Colon, EORTC-Lung, CESD-8, Brief Pain Inventory, EQ5D, State of Michigan Survey, SUPPORT, and the National Health Interview Survey, and, therefore, have been used extensively in previous studies. In addition, the survey was pilot tested in 86 patients with newly diagnosed lung or colorectal cancer recruited across the study PDCR sites. Several instruments will be available for conducting the patient baseline survey. The primary mode of survey (and mode of choice for all participants) will be computerassisted telephone interviews (CATI). The CATI version of the survey will be programmed by the RAND Corporation Survey Research Group using Berkeley CASES 5.3j software. The following is the basic approach to interview data collection: 1. If the patient can be contacted by telephone, the study is explained and, if s/he agrees, the introductory consent scripts (Appendix D) are read, and the patient becomes a study participant. A one-hour telephone interview will be administered. If the participant requests it, the interview may be given at two separate times to ease any potential discomfort. If the patient refuses to participate, the interview will not proceed. 2. If the patient is not available for an interview but is willing to reschedule, the interviewer will arrange another time to call. This might occur if the patient is away, temporarily in a hospital or nursing home, or otherwise temporarily unavailable. The interviewer will attempt to reschedule the interview within two weeks, but interviews more than two weeks after the initial call will be acceptable. 3. If the patient cannot give a full interview, s/he is offered a brief version of the interview (also via CATI), which should take about 20 minutes to administer. 4. If the patient is reached but is unable to give the interview, s/he will be asked to identify a surrogate respondent, who will then be contacted for the interview. For patients who are alive, no surrogate interviews will be conducted without verbal or written consent from the patient and identification of the surrogate by the patient except as follows. An interviewer is allowed to qualify a surrogate of a living patient without first obtaining patient verbal or written consent if the adult answering the phone states the patient cannot come to the phone due to incapacity of coma, hearing problem/deafness, or difficulty understanding questions or difficulty speaking or otherwise communicating AND this potential 27 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 surrogate indicates they are currently involved in the patient's health care process and are confident they have sufficient knowledge to respond to survey questions. 5. If the patient is deceased at the time of initial contact with a potential surrogate respondent, condolences are offered and the interviewer will inquire whether the surrogate respondent would be willing to participate in the interview at that time. If bereavement or other matters preclude this, an interview will be scheduled at a later time. The surrogate survey instrument that will be used when the target patient is deceased is about 10 minutes longer than the surrogate instrument for patients who are alive, since it contains additional items on the end-of-life experience and the use of and satisfaction with terminal care. 6. In instances where potential study participants defer from participating, each PDCR site will follow a “non-response conversion” protocol that is tailored to the characteristics of each site to attempt to maximize participation rates among nonresponders. Appendix A contains the site-specific details for the nonresponse conversion strategy. Some site-specific non-response protocols may include the use of computer-assisted personal interviews (CAPI). This mode of interview should only be used in instances where CATI has been attempted and no interview (primary or surrogate) was conducted. 7. Self-administered surveys may be used in the following instances: a) If an interviewer is unable to speak with a patient after exhaustive efforts as defined by each site, coded in CATI as non-responder/non-contact, a self-administered survey can be mailed to the potential participant. b) If when an interviewer does speak to a patient the patient refused to give a full or brief telephone interview or to name a surrogate, the interviewer will have the option of offering to mail a self-administered survey to the patient. c) If the patient proactively asks about the possibility of a self-administered survey, the interviewer will have the option of offering to mail a self-administered survey to the patient. Table 6.1 provides an annotated list of the domains in the full baseline survey. The abbreviated baseline telephone survey contains a subset of items from the full telephone survey. The surrogate survey also contains a subset of the items of the full baseline patient survey, but in addition contains a small number of new items that pertain specifically to the surrogate’s experience of the patient’s cancer care (Section 6.2.5 provides a description of the Surrogate Survey). All versions of the survey will also be available in English, Spanish and Chinese (Mandarin and Cantonese) except for the self-administered version, which is only available in English. Based upon data from our pilot test, the full baseline telephone interview is anticipated to take an average of 60 minutes to complete. 6.2.2 Domains The following table lists the domains covered in the baseline patient survey, along with the specific content of each domain and its corresponding section within the survey. 28 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 Table 6.1: Domains in the Baseline Patient Survey, Full Primary Respondent Version. Domain Demographics Problem Recognition Initial Treatment– Surgery Initial Treatment– Radiation Therapy Initial Treatment– Chemotherapy Clinical Trials Identification of Surrogate Patient Assessment of Care Content Age Gender Ethnicity Languages spoken and English fluency Education Marital status Country of origin Year of immigration Confirm cancer diagnosis Identify the patient’s term for illness if not “cancer” Identify symptom that led to diagnosis Determine if the patient received or is scheduled to receive surgery, had a consult with a surgeon, and whether he/she received a recommendation for or against surgery Reasons for not having surgery Patient’s beliefs about the efficacy and side effects of surgery Patient’s role in decision-making about surgery Determine if the patient received or is scheduled to receive radiation, had a consult with a radiation oncologist, and whether he/she received a recommendation for or against radiation therapy Reasons for not having radiation therapy Patient’s beliefs about the efficacy and side effects of radiation therapy Patient’s role in decision-making about radiation therapy Determine if the patient received or is scheduled to receive chemotherapy, had a consult with a medical oncologist, and whether he/she received a recommendation for or against chemotherapy Reasons for not having chemotherapy treatment Patient’s beliefs about the efficacy and side effects of chemotherapy Patient’s role in decision-making about chemotherapy Determine if the patient participated in a clinical trial or, if participation was discussed, how the patient learned about trials If the patient participated in trial, determine the treatment modality Reasons for not participating in a clinical trial, if a trial was an option Patient’s role in decision-making about clinical trials Identify a primary surrogate respondent Identify a contact who would know about a change in address Identify a second surrogate respondent Obtain permission to contact Patient rating of care overall Perceived discrimination Access to specialists 29 Section 1 2 3 4 5 6 7 7 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Domain Quality of Life Supportive Care and Symptom Management Content Goals of Treatment and Prognosis Health History and Behaviors Insurance Coverage and Income Identification of Providers and Hospitals Protocol 001 Amendment #3, December 2005 General health status Cancer symptoms Brief pain inventory Depression Summary health status Health utility index Recalled physical functioning one year prior to diagnosis Social support For each symptom that the patient reports having during the prior four weeks, ascertain the following: Provider’s awareness of the symptom Patient’s desire for help with the symptom Whether the patient received help with the symptom Use of and unmet need for supportive care services, including hospice care Family’s role in decision-making Preferred decision-making role Perceived life expectancy Preferences for extending life vs. palliation Resuscitation preferences Co-morbid illness Prior cancer Prior radiation therapy Functional status Smoking history Alcohol history Complementary and alternative medicine use Vitamin use Height and weight Current insurance, changes and gaps in coverage, characteristics of coverage, including coverage for prescription drugs Tests or treatments forgone because of insurance problems Household income Wealth Identification of doctors and hospitals who provided care Contact information for providers and hospitals Section 8 9 10 11 12 13 6.2.3 Timing of Administration For most participants, the completion of the baseline survey will coincide with enrollment into the study. As discussed in Section 4, Enrollment Procedures, the baseline survey should be administered between 12 and 18 weeks from diagnosis, with a target date of 16 weeks from diagnosis. No participant should complete a survey earlier than 12 weeks from diagnosis. PDCR sites will attempt to enroll any patient ascertained by the site within 6 months from diagnosis even if the interview cannot be scheduled until a date later than 6 months after diagnosis. PDCR sites will sample randomly (with sampling probability 0.20, for a 20% random sample) from the set of cases ascertained more than 6 months following the date of diagnosis. These target dates for survey administration apply to all modes of administration for participants alive at the time of initial contact. No patient survey 30 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 (full or brief) will be conducted beyond 12 months post-diagnosis. Please refer to Table 6.2 for the priority window for interviewing. Table 6.2: Priority Window for Interviewing 1st Priority 12-18 weeks post-diagnosis 2nd Priority 18 weeks – 6 months post-diagnosis 3rd Priority 6-12 months post-diagnosis * * For cases identified 6-12 months post-diagnosis, PDCR sites will randomly sample 20% of these cases. 6.2.4 Abbreviated Versions of Baseline Survey There are two versions of an abbreviated telephone survey, designed for patients who are either too ill or otherwise unwilling to complete the full-length survey. The two versions are very similar, but one includes the items from the full-length survey needed to identify physicians and hospitals providing care to the patient. The other version, to be used by sites with electronic medical records systems that can identify treating physicians, has fewer questions about treating physicians, but includes additional items on patient beliefs and preferences regarding treatment options. Otherwise, the two versions are the same. The abbreviated telephone surveys both include the subset of items from the full survey that captures the most essential variables needed for later analyses. The abbreviated telephone surveys are designed to require an average of 20 minutes to complete. For example, in the Quality of Life domain, the SF-12 measure of health status was included, while most of the other items about functional status and disease-specific symptoms are excluded. Demographic items that may be available from cancer registry data or medical records are not included in the abbreviated survey. Items that might be either unusually difficult or time-consuming for seriously ill patients to respond to are also excluded. Copies of the abbreviated surveys are included in Appendix E. 6.2.5 Surrogate Respondent Patient Survey Although it is always preferable to interview the target respondent, there will be times when this is not possible due to illness or death. A well-informed surrogate can provide information that allows data from the patient in question to be included in the study sample. The goal in creating the surrogate respondent survey was to gather as much of the information contained in the patient survey as feasible. There are two surrogate respondent surveys in the study. The first is for surrogate administration when the patient is still alive but unable to complete an interview. The second is an afterdeath survey to be administered to the surrogate after a predetermined window of bereavement. Interviewer instructions and scripts have been adapted for surrogate administration and will be specific (by version) to reflect the status of the identified patient (i.e., alive but unable to be interviewed or deceased). 6.2.5.1 Domains of the Surrogate Respondent Survey Surrogate Respondent Survey When Patient is Alive: Most of the domains from the patient survey have been included in the surrogate survey, with appropriate deletions within domains, especially Problem Recognition (modified according to the abbreviated patient version), Quality of Life, and Health Beliefs. Surrogate Respondent Survey for a Deceased Patient: The following domains in this version were dropped or substantially reduced: Quality of 31 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 Life, Supportive Care and Symptom Management, and Goals of Treatment and Prognosis. A section on Quality of Care at the End of Life has been added. 6.2.5.2 Timing Between Death and Contact of a Surrogate Respondent If the patient is known to be deceased at the time of initial scheduled contact, the next-of-kin will be invited to participate in the study by way of a mailed letter with study information. The telephone interview will be attempted no earlier than one month after the death of the patient. At this time, appropriateness of this surrogate will be assessed using the interview script. If this surrogate is deemed to be appropriate but states that it is too soon to do the interview, then a call back will be scheduled. If this surrogate states that s/he is not the best person for this interview, then contact information on an alternate surrogate will be requested. If it is not known that the patient is deceased at the time of attempted initial telephone contact, interviewers will offer condolences and then assess the appropriateness of the individual answering the phone as a potential surrogate respondent using the interview script. If this surrogate states that s/he is not the best person for this interview, then contact information on an alternate surrogate will be requested. If the date of contact is at least one month following the death of the identified patient and this surrogate is deemed to be appropriate, an interview will be attempted. If s/he states that it is too soon to do the interview, a return call will be scheduled and study information will be sent in the mail. If the death was less than one month before the call, the interviewer will offer condolences, offer to call back at a better time (no sooner than one month after the death of the identified patient), and will send study information in the mail to the surrogate respondent. Surrogates of deceased patients can be interviewed as soon as possible, (even if that is before 12 weeks post patient diagnosis) after waiting one month beyond the date of the patient death. Surrogates of living patient should not be interviewed before 12 weeks post patient diagnosis. No surrogate interviews should take place beyond 12 months post-diagnosis of the patient. 6.2.5.3 Surrogate Selection For Patient Deceased at Initial Contact The most appropriate surrogate is one who was in close contact with the patient between diagnosis and death. In addition, a suitable surrogate is one who discussed or participated in medical decision-making and was aware or helped with financial matters. Surrogates of deceased patients should be interviewed if the surrogate knows of the patient’s cancer diagnosis or “problem” and should be asked for medical record consent. However, if the surrogate does not know of the patient’s cancer diagnosis or “problem”, the surrogate should not be asked to complete a survey, but should be asked to provide medical record consent. A surrogate respondent must be of majority age in the state in which the patient resides and in the judgment of the interviewer, must be without cognitive impairment. 6.3 Follow-up Patient Survey 6.3.1 General Design Follow-up surveys will be conducted for all participants who were alive at the time of the baseline survey. There will be no follow-up surrogate survey conducted in situations where the identified patient had died before initial contact for the baseline 32 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 survey, regardless of whether a surrogate respondent baseline survey had been completed. One of two types of follow-up survey will be administered, either: (1) a follow-up survey of cases who are alive at the time of the scheduled follow-up (survivor survey) or (2) a follow-up survey of surrogates for patients who have died since the time of the baseline survey. The purpose of the former is to collect details of treatment received after the baseline survey, cancer recurrence or progression, and changes in quality of life, functional status, symptoms, experiences of care, and changes in financial resources. The purpose of the decedent surrogate follow-up survey is to collect data on the quality of end-of-life care, especially symptom management and hospice care. The content of the survivor follow-up survey will vary depending on answers to a short screening questionnaire about disease status. Those who are doing well at follow-up based on response to the screening questions will be asked a subset of the domains from the baseline survey. Those who are doing poorly (i.e. patients with recurrent or refractory disease) will be asked a different subset of domains from the baseline survey. See Table 6.3 for the follow-up survey algorithm. The interview mode for the follow-up survey will be computer assisted telephone interviews (CATI) conducted by trained interviewers and developed with the same software as the baseline survey. There will be no surrogate respondent survey for patients alive at the time of the scheduled follow-up survey. The follow-up telephone interviews are anticipated to take an average of 15 to 20 minutes to complete. To reduce respondent burden, the CATI programming will prefill the follow-up surveys with information collected in the baseline survey. Table 6.3 Follow-up Survey Algorithm 6.3.2 Timing of Administration For most participants, the completion of the follow-up survey will occur 12 months after diagnosis (window, 11 to 13 months after diagnosis). The interval between baseline and follow-up survey will typically be 8 months. No participant should 33 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 complete a follow-up survey sooner than 3 months after the baseline survey or sooner than 11 months after diagnosis. 6.3.3 Patient/Surrogate Letters A letter will be mailed to patients one week before the target interview date. The letter will be on letterhead from the local PDCR site. A copy of the letter (which may require edits at each PDCR site in response to local IRBs) is included in Appendix J. The letterhead will also include the Share Thoughts on Care logo. Letters mailed to patients include a ‘return services requested’ for the post office so that if the letter requires forwarding to a new address, this address is returned to the site, the new information can be updated into the database and the letter re-mailed. Through ongoing cohort surveillance, sites will identify deceased patients and will substitute a surrogate letter for this initial mailing (Appendix J). An incentive will be provided for participating in the follow-up survey. The value and mode of incentive will vary by site. The site-specific incentive plan is included in Appendix A. 6.3.4 Mode of survey administration The mode of survey will be computer-assisted telephone interviews (CATI). The CATI version of the survey is being programmed by the RAND Corporation Survey Research Group using Berkeley CASES 5.3j software. To reduce respondent burden, the CATI programming will pre-fill the follow-up surveys with information collected in the baseline survey. The following is the basic approach to interview data collection: 1. If the patient can be contacted by telephone, the study is explained and, if s/he agrees, the introductory consent scripts (Appendix G) are read, and the Survivor Follow-up Survey will be administered. The telephone interview will be a half-hour in duration. If the participant requests it, the interview may be given at two separate times to ease any potential discomfort. If the patient refuses to participate, the interview will not proceed. If the patient is reached but is unable to give the interview, this will be recorded as a refusal and the interview will not proceed (there is no surrogate version of this survey). 2. If the patient is not available for an interview but is willing to reschedule, the interviewer will arrange another time to call. This might occur if the patient is away, temporarily in a hospital or nursing home, or otherwise temporarily unavailable. The interviewer will attempt to reschedule the interview within two weeks, but interviews more than two weeks after the initial call will be acceptable. 3. If the patient is known to be deceased prior to the time of scheduled contact, the surrogate identified in the baseline survey will be invited to participate in the study by way of a mailed letter with study information (Appendix J). At the time of telephone contact with the surrogate, the appropriateness of this surrogate will be assessed using the interview script. If this surrogate is deemed to be appropriate but states that it is too soon to do the interview, then a call back will be scheduled. If this surrogate states that s/he is not the best person for this interview, then contact information on an alternate surrogate will be requested. The Decedent Follow-up Survey will be the survey administered. Information about surrogate surveys is included in section 6.3.6 below. 4. If the patient is deceased at the time of contact with a potential surrogate, but this was not known prior to the telephone contact, condolences are offered and the interviewer will inquire whether the surrogate respondent would be willing to 34 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 participate in the interview at that time. If bereavement or other matters preclude this, an interview will be scheduled at a later time. The Decedent Follow-up Survey will be used. If this surrogate states that s/he is not the best person for this interview, then contact information on an alternate surrogate will be requested. The appropriateness of a willing surrogate will be assessed using the interview script. If the date of contact is at least one month following the death of the identified patient and this surrogate is deemed to be appropriate, an interview will be attempted. If s/he states that it is too soon to do the interview, a return call will be scheduled and study information will be sent in the mail. If the death was less than one month before the call, the interviewer will offer condolences, offer to call back at a better time (no sooner than one month after the death of the identified patient), and will send study information in the mail to the surrogate respondent. Further information about surrogate surveys is included in section 6.3.5 below. 6.3.5 Survivor Follow-up Surveys When the patient is alive at the time follow-up, the Survivor Follow-up Survey will be used. The following table lists the domains covered in this survey, along with the specific content of each domain and its corresponding section within the survey. Table 6.4: Domains in the Survivor Follow-up Survey. Domain Content Section Disease Status 1 Basic Information Surgery Radiation Therapy Chemotherapy Identify the patient’s term for illness if not “cancer” Whether cancer-free Marital status Type of residence Number in household Employment status Determine if the patient received surgery since the baseline Obtain names and addresses of new surgery providers. Patient’s beliefs about overall quality of care received for the new surgery. Determine if the patient received radiation since the baseline Obtain names and addresses of new radiation providers. Patient’s beliefs about overall quality of care received for the radiation therapy. Determine if the patient received chemotherapy since the baseline Obtain names and addresses of new chemotherapy providers. Patient’s beliefs about overall quality of care received for the chemotherapy. Determine if the patient participated in a clinical trial since the baseline 2 3 4 5 Participation in Clinical Trials Assessments of Cancer Care Patient rating of care overall 7 Quality of Life / Symptoms 8 General health status Cancer symptoms Brief pain inventory Depressive symptoms Side effects from medications Summary health status Social support 35 6 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 Domain Content Section Symptom management and supportive care For each symptom that the patient reports having during the prior four weeks, ascertain the following: Provider’s awareness of the symptom Patient’s desire for help with the symptom Whether the patient received help with the symptom Use of and unmet need for supportive care services, including hospice care Preferences for extending life vs. palliation 9 Co-morbid illness Current smoking Alcohol use Complementary and alternative medicine use Vitamin use Weight Changes in insurance since baseline Tests or treatments forgone because of insurance problems Perceived adequacy of household income 11 Identification of new doctors and hospitals who provided care Contact information for new providers and hospitals Contact information for proxies 13 Goals of treatment and prognosis Health History and Behaviors Health Insurance, Expenses, and Financial Resources Provider and Practice Review and Proxy Identification 10 12 6.3.6 Decedent Follow-up Surveys The most appropriate surrogate is one who was in close contact with the patient between diagnosis and death. In addition, a suitable surrogate is one who discussed or participated in medical decision-making and was aware or helped with financial matters. A surrogate respondent must be of majority age in the state in which the patient resides. Surrogate surveys will only be conducted for patients who have died since the baseline survey. In this case, the Decedent Follow-up Survey will be used. A main goal of this survey was to collect information about care received at the end of life. The following table lists the domains covered in this survey, along with the specific content of each domain and its corresponding section within the survey. Table 6.5: Domains in the Decedent Follow-up Survey. Domain Content Section Disease Status 1 Basic Information Surgery Identify the patient’s term for illness if not “cancer” Whether cancer-free Marital status Type of residence Number in household Employment status Determine if the patient received surgery since the baseline Obtain names and addresses of new surgery providers. Patient’s beliefs about overall quality of care received for the new surgery. 36 2 3 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 Domain Content Section Radiation Therapy Determine if the patient received radiation since the baseline Obtain names and addresses of new radiation providers. Patient’s beliefs about overall quality of care received for the radiation therapy. Determine if the patient received chemotherapy since the baseline Obtain names and addresses of new chemotherapy providers. Patient’s beliefs about overall quality of care received for the chemotherapy. Determine if the patient participated in a clinical trial since the baseline 4 Assessments of Cancer Care Patient rating of care overall 7 Symptom management and supportive care Use of and unmet need for supportive care services, including hospice care 8 Health History and Behaviors Co-morbid illness 9 Quality of Medical Care at the End of Life Palliative treatments received including hospice Surrogate’s beliefs about overall quality of care received Whether patient preferred treatments for extending life vs. palliation Changes in insurance since baseline Tests or treatments forgone because of insurance problems 10 Identification of new doctors and hospitals who provided care Contact information for new providers and hospitals 12 Chemotherapy Participation in Clinical Trials Health Insurance, Expenses, and Financial Resources Provider and Practice Review 5 6 11 6.4 Medical Record Abstraction 6.4.1 Timing of Medical Record Abstraction Study teams will collect data from medical records covering the peri-diagnosis and initial treatment phases for cancer. Whenever possible, the “window of time” will include the date at which the follow-up survey was administered. At a minimum, the medical record abstraction window for patient participants in each medical record will extend from 3 months prior to diagnosis to 15 months after diagnosis. In instances where the follow-up survey is administered later than 15 months after diagnosis, sites should make every effort to include the date of follow-up in the abstraction window. To attain economies of scale, especially with hospital-based records, the actual timing of chart abstraction may vary across PDCR sites. It is anticipated that sites will abstract information from batches of medical records accumulated at large treatment facilities and also from the offices of providers who care for only a few patients with cancer. For participants who have died earlier than 15 months from the date of diagnosis and for whom proper consent to review the medical record has been obtained, sites may abstract data from the records any time after the participant’s death. 6.4.2 Identification of Medical Records 37 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 For the geographically-based sites, pertinent medical records will be identified from patient or surrogate respondent surveys and cancer registry data. For the providerorganization-based sites, pertinent records will be identified from survey data and administrative records. When consent has been obtained for medical record review but no survey instrument has been completed, study teams will use registry or administrative data and available medical records, as well as information from the Physician Contact Information Worksheet to identify additional records for abstraction. Records documenting care during inpatient admissions and outpatient visits to hospitals, clinics, and hospital-affiliated or freestanding treatment facilities (e.g., radiotherapy or ambulatory surgery facilities) will be targeted for data abstraction. Study teams will not, however, abstract records from nursing homes, rehabilitation facilities, mental health providers, hospice or home health organizations. Records may be abstracted using either the original records stored at treatment facilities/physician offices or from photocopies mailed to PDCR offices. Data will be abstracted from ambulatory medical records for physicians and nurses who provide the following roles for patients: discuss or deliver surgery, chemotherapy, or radiation therapy treatments, provide primary or continuity care, provide symptom management, or provide a key role in decision-making regarding the possible use of treatments. This is likely to include providers from the following specialties: gastroenterologists or pulmonologists involved in the diagnosis of cancer for the patient; primary care physicians involved in coordinating the patient’s cancer care; and cancer specialists (surgeons, medical oncologists, and radiation therapists) routinely involved in cancer care in lung and colorectal cancer. Additionally, we will abstract hospital records associated with overnight and day visits to the hospital. An analysis of population-based cancer registry data linked with Medicare claims indicates that patients with these diseases encounter an average of 3.1 unique physicians from among the relevant specialty categories during the period of initial diagnosis and treatment, and visit an average of 1.2 unique inpatient facilities.30 6.4.3 Data Collection Procedures Medical record data will be abstracted using the MedQuest Clinical Data Collection and Design System, a software tool distributed and supported by the US Centers for Medicare and Medicaid Services (CMS). MedQuest is an open architecture system with predefined medical procedure codes and modules for data entry and exporting data. The methods for protecting the data gathered in MedQuest are described in Section 7.2. 6.4.4 Domains of Interest in Medical Record Abstraction 6.4.4.1 Diagnostic Tests 6.4.4.2 This section will document the use of radiologic, endoscopic or laboratory tests that might have demonstrated the presence and extent of cancer. Co-morbidity The ACE-27 instrument will be used to collect information on co-morbidity. This instrument was developed to obtain information on co-morbidities in 12 organ systems or topics (cardiovascular, respiratory, gastrointestinal, renal, endocrine, neurologic, psychiatric, rheumatologic, immunologic, malignancy, substance abuse, body weight) by level of severity. Other non ACE-27 items of interest include serum albumin levels, smoking history, cigarette pack years, and urinary continence. 6.4.4.3 Stage of Disease 38 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 The cancer stage will be collected using collaborative stage techniques and coding standards developed by the North American Association of Central Cancer Registries (NAACCR) and the American Joint Committee on Cancer (AJCC). This collaboration has developed a unified data set that combines and standardizes the information needed to assign stage in the AJCC (TNM), SEER (EOD) and Summary Stage (SS). Data elements include location, histopathologic type, grade, size, extent, lymph node development, and metastases. Algorithms will be used to assign stage. The medical record instrument will also collect stage of disease as assessed by the treating physician. This section will also include histology or cytology, primary tumor location, final margin status (if the patient had surgery to remove the cancer), and information on the location and extent of metastatic disease. 6.4.4.4 Surgical Processes The chart abstraction tool will enable data collection about the type of surgery performed to remove the cancer, a select group of intra-operative procedures that reflect the details of the surgery, e.g., ureter identified, peritoneum examined, and other surgeries the patient may have undergone during the abstraction window. We will also record whether the surgery was part of a clinical trial. 6.4.4.5 Chemotherapy Information on systemic chemotherapy, regional chemotherapy, and bisphosphonates will be collected. Each section will obtain information on the first and last doses of each drug including the drug name and start and stop dates, where it was given, route, and dose amount (for bisphosphates and systemic). The systemic chemotherapy section will also collect information on the regimen in which the first and last doses of each drug are given. The systemic chemotherapy section also includes information on intent (neoadjuvant, adjuvant, palliative), best response for all but adjuvant therapy, total dose, and whether the dose was tailored. In addition, we will obtain information on the use of growth factors and erythropoietin. We will also record whether in the chemotherapy was part of a clinical trial. 6.4.4.6 Radiation The radiation section obtains information on the body site irradiated, the start and stop dates, days the radiation was delivered, number of fractions, units of dose, whether the patient received a boost of radiation (with dates and dose), intent of radiation, best response for all but adjuvant and prophylactic therapy, interruptions in treatment, early termination and delay of treatment, dose reduction, and type of radiation used. We will also record whether the radiation was part of a clinical trial. 6.4.4.7 Visits 6.4.4.8 This section of the medical record abstraction instrument will include information on hospitalizations, medical encounters, referrals, decision-making, and symptoms. Clinical Trials: The medical record abstraction instrument will also allow abstractors to record data on whether or not a patient was enrolled in a clinical trial, the name of the trial, the type of trial and whether or not it was related to their cancer. 6.4.4.9 Medical Events 39 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 In this section, data will be collected on the first time a particular medical event occurs. Data on complications and outcomes will also be entered in this section. In addition to these topics, the medical record abstraction instrument will also collect data on triggering events, eligibility, sociodemographics, date of diagnosis, prior cancer history, recurrence, new malignancies and vital status. Information on PET scans (both cancer types), CEA tests and colonoscopies (colorectal only) collected throughout the abstraction window will also be entered. 6.5 Health Care Provider Survey Please refer to Appendix M for the Provider Survey protocol, which includes details regarding sampling, survey administration, and data entry and data transfer. 6.5.1 Target Population The target population of the provider survey is the physicians who have provided care to patient participants in Share Thoughts on Care. This population represents the physicians who are influential in the process and outcomes of care for colorectal and lung cancer patients within the catchment area of CanCORS. Specifically, this population will include medical oncologists, surgeons, radiation oncologists, pulmonologists, gastroenterologists, and primary care physicians. A sample of approximately 8360 CanCORS physicians will be surveyed. A sampling frame will be developed from responses to the patient survey. Responses from the patient survey will identify physicians who reportedly have been involved in diagnosing the patient’s cancer, performed surgery on the cancer, treated the patient with radiation, administered chemotherapy and managed patient’s symptoms. Specifically, we will identify: Referring Physicians (gastroenterologists pulmonologists, PCPs, surgeon or medical oncologists): We will identify physicians involved with the cancer diagnosis and decisions to refer patients to cancer specialists using several questions from the patient survey. These questions are aimed at identifying the providers who made referrals for patients who were referred and at identifying providers most important in making decisions about seeing cancer specialists for those who were not referred. If multiple providers are identified we will develop an algorithm to identify the most relevant provider so that the sampling frame for referral providers will be a single unique physician per patient. Physicians who discussed and/or provided surgical treatments will be identified using questions 3.4a (doctor who performed most recent surgery), 3.4c (surgeons performing earlier surgeries), 3.8a (surgeon scheduled to perform planned surgery), and 3.9 (surgeon seen by patients who did not and were not planning to receive surgery). If a patient does not identify a surgeon in any of these questions, we will assume that characteristics of the referring provider will be most relevant in the decision-making processes around surgical treatments. If multiple providers are identified, we will choose the physician who performed the surgery for patients who had surgery and the surgeon scheduled to perform surgery for those who plan to have surgery. Physicians who discussed and/or provided radiation therapy will be identified using question 4.7 (doctor treated or will be treating you with radiation) and question 4.9 (radiation doctor seen by patients who did not receive and are not planning to receive radiation). If a patient does not identify a radiation doctor in either of these 40 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 questions, we will assume that characteristics of the referring provider will be most relevant in the radiation therapy decision-making processes. Physicians who discussed and/or provided chemotherapy will be identified using question 5.6 (who is the physician who provided or is planning to provide chemotherapy) and question 5.8 (chemotherapy doctor seen by patients who did not receive and are not planning to receive chemotherapy). If a patient does not identify a chemotherapy doctor in either of these questions, we will assume that characteristics of the referring provider (or the PCP) will be most relevant in the chemotherapy decision-making processes. Physicians involved in the management of patient’s symptoms will be identified using question 9.2 (who is the one doctor who was most likely to know that you had a symptom). The physicians identified in the patient survey will have their practice location and contact information verified by comparing with a local listing of physicians for each PDCR site, such as a list from a state-licensing agency. Each physician will be assigned a unique identifier for the study. This number will be used to coordinate the data collection, and will assure that a physician will be surveyed only once, even if identified by multiple patients. 6.5.2 Domains of Interest Four domains will make up the provider survey: (1) physician beliefs about care, (2) physician practice style variables, (3) organization of practice factors, and (4) physician demographics and training. To measure beliefs about care, physicians will be given brief vignettes and asked how strongly they would recommend a particular treatment. Vignettes will describe decisions to use adjuvant chemotherapy, adjuvant radiotherapy, surgery, and first–line chemotherapy for specific cancers (e.g., adjuvant chemotherapy for stage III colon cancer). The provider survey also will collect information about physician practice styles, such as shared decision-making, communication with patients, therapeutic aggressiveness, communication with other practitioners, and referral patterns. These practice style variables describe how a physician interacts with patients and other practitioners, and can help explain cancer care choices. The third set of variables to be measured with the provider survey contains descriptors of the organization of practice in which a physician works. These variables will characterize the health system in which the physician provides care for patients and are predicted to explain variation in cancer treatments and outcomes. These variables include patient volume, practitioner mix, managed care techniques, and coordination mechanisms. 6.5.3 Mode of Contact and Incentives Surveys will be mailed to physicians with a cover letter describing the purpose of the study, as well as the confidential and voluntary nature of participation. The cover letter will provide the name and a toll-free phone number of a contact person from each PDCR site who can be contacted with any questions. Surveys will be distributed by mail and on the Internet. An incentive of approximately $20 may be offered to enhance participation. Two to three weeks after the initial mailing, we will send a second mailing to all nonresponders. Approximately three weeks after the second mailing, we will phone the office of nonresponding physicians. We will verify that the instrument has been received and remind them to complete and return it, and we will offer to mail or fax another instrument to them. All 41 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 contacts with the physicians or their office staff will be recorded in a contact database. 6.5.4 Enrollment Protocol As mentioned above, the provider survey will be in the form of a self-administered questionnaire. To minimize respondent burden, our goal is a survey instrument that will require no longer than 15 minutes to complete. 6.5.5 Data Linkage Each survey will be coded with a unique identifier to facilitate follow-up of nonresponders; however, physicians’ responses will not be linked to their names. We will also use these unique identifiers to link providers’ responses to data about patients in the study to examine how practice styles and beliefs of providers are related to patterns of care. Once the data are linked, the unique identifiers will be removed. At no time will we attempt to identify individual providers or their patients. 6.6 External Databases 6.6.1 Medicare Claims Data We plan to supplement the data from the patient survey, medical records and provider survey with Medicare claims data. Medicare is the primary health insurer for 97% of the U.S. population age 65 and older. We expect patients aged 65 and older to represent approximately 68% and 65% of our enrolled colorectal and lung cancer patients respectively. We plan to request data from the Center for Medicare and Medicaid Services (CMS, formerly the Health Care Financing Administration [HCFA]) resulting from claims for inpatient services, outpatient services, physician services, hospice care, and home health care. We will also obtain enrollment files that include information on Medicare eligibility, entitlements, HMO enrollment, and vital status. The Veterans Information and Research Education Center (VIREC) will provide linked Medicare claims data to the VA site. Data will be linked using the participant’s social security number, gender and date of birth. Therefore, the Social Security number of each patient needs to be collected. Each PDCR site will determine the best method to obtain social security numbers. Information necessary for the linkage will be sent to a third party contractor, AJ Durham, Cogitant Solutions, Minnetonka, MN, by each PDCR in a separate file that contains each participant’s social security number, gender, date of birth and CanCORS ID but no additional data. This identifying information will not be sent to the third party contractor until the request for Medicare data is being prepared. PDCR sites will develop HIPAA business agreements with the third party contractor. All SSN information sent to the contractor will be destroyed once the linkage has been finalized. The contractor will receive a SSN finder back from CMS that links a Medicare ID with each submitted SSN. The file will contain one record for each submitted SSN and will contain a Medicare ID, date of birth and gender information. CMS does not return any information on beneficiary names. The contractor will evaluate the accuracy of potential matches by comparing them with CanCORS information (date of birth, gender) using a method such as that described by Flemming and Fisher (1990). The contractor will prepare a site-specific report of match rates (acceptable vs. unacceptable and unmatched), which will be shared with the Medicare linkage subcommittee. Following discussion between the contractor and the subcommittee, it will be decided whether this process needs to be repeated for particular sites (or all sites). Once linkage has been finalized, the contractor will prepare a final CMS 42 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 finder that contains the Medicare IDs that belong to CanCORS participants. This finder will be sent to CMS and will be the basis for data requests. The contractor will send to the SCC a cross-walk file of CanCORS ID to Medicare ID. The contractor will not send the SCC any SSN information. The SCC will retain the cross walk in case further data requests are needed. However, the cross-walk containing Medicare IDs will be stored in a secure location separate from other CanCORS data to ensure Medicare ID is never linked to other CanCORS data. CMS will strip claims data of directly identifying information (beneficiaries name and address) before sending to the SCC. The SCC will replace Medicare ID with a CanCORS ID before the claims data are linked to the SCC database. Due to the possibility of inaccuracies in the coded dates of diagnosis, we will request data for services received one year prior to the date of diagnosis of the first enrolled patient as supplemental information regarding co-morbidities and use of services prior to the index cancer illness. We will also request sufficient data to ensure we measure services received up to 15 months post-diagnosis on the last enrolled patient to coincide with data abstracted from the medical records. Past experience in linking Medicare claims data for services provided to cancer patients through the SEER–Medicare program suggests that we will be able to link and obtain Medicare claims data for approximately 95% of our enrolled patients age 65 and older.31 Medicare claims data provide valuable information on co-morbidities, utilization patterns, and costs of care. There are however, several important limitations to using Medicare claims data to assess patterns of care. For example, HMOs do not normally submit data to CMS (although some CRN sites do), so Medicare claims data can provide reliable utilization and cost data only for traditional fee-for-service enrollees. In addition, claims data are collected for billing purposes and generally are less reliable measures of clinical processes than those obtained from medical record data. However, we foresee two major uses of the Medicare claims data. First, Medicare claims data will be used to provide supplemental information that may be missing due to limitations of our main data collection strategies. We will use the Medicare claims data obtained for the enrollees to supplement clinical and treatment utilization data obtained from the patient survey and medical record abstraction. For example, receipt of adjuvant chemotherapy may be missed during the medical record abstraction if we do not identify the appropriate physician providing chemotherapy and abstract the appropriate record. However, this information would be recorded in the Medicare claims data if the patient received his/her care under Medicare. Second, Medicare claims data will provide valuable information on the costs and utilization of services that we will not be able to assess fully as part of the main data collection strategy. For example, Medicare claims data for the enrollees age 65 and older will provide additional detail regarding the use of home health and hospice services that will be linked to the detailed patient and provider data collected in the surveys and medical records, allowing us to further investigate the use of these services in community-based samples of elderly patients with colorectal and lung cancer. In addition, we plan to use reimbursement levels on Medicare claims to obtain prices for the resources utilized in care. Total cost estimates will then be made by multiplying the resource utilization rates by their respective prices. In order to obtain data on broader patterns of care in our PDCR sites, we plan to make a separate request for Medicare data to CMS and create a database containing administrative data on the census of Medicare-eligible patients with colorectal or lung cancer in the geographic areas represented by our five 43 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 geographically-based sites and any provider-organization-based sites that have patients for whom bills are available from CMS. We will request enrollment data for this cohort, as well as claims data resulting from inpatient services, outpatient services, physician services, hospice care, and home health care received during the period of one year prior to diagnosis through 15 months post-diagnosis. We will request de-identified data from CMS on this cohort. Specifically, we will request that CMS provide encrypted patient, physician, and provider IDs to enable us to link claims longitudinally within patients and across physicians and providers. Patient and provider zip codes from these Medicare claims will be used to describe the practice “milieu” in each zip code in which CanCORS patients reside. This information will then be linked to individual patients by zip code and diagnosis year. Using Medicare claims we will measure: (1) the relative distance from patient residence to different provider types; (2) the availability and mix of providers and medical facilities in geographic areas surrounding the patient; (3) variation in treatment and referral patterns across geographic areas; and (4) the regional characteristics of the health care markets. We plan to use provider identification numbers to classify relevant providers by their propensity to treat patients or refer patients for further treatment. Once providers are classified, we will use their practice zip codes to develop a series of access-related measures for the universe of zip codes that contain patients. For example, we will measure the number of providers that supplied adjuvant treatments in defined areas around a zip code (e.g., within a 50-mile radius) in the year of diagnosis, and the distance a patient would have to travel to the nearest provider that supplies the treatment. In addition, we will classify primary care physicians and surgeons by their propensity to refer patients for adjuvant treatments. Using this information, we will calculate the percentage of high-referring physicians in defined areas around a patient’s residence, and then estimate the distance from a patient to the nearest highreferring provider and the nearest low-referring provider and compute a differential distance measure that has been shown in previous healthcare research to be related to treatment choice. 6.6.1.1 Data on Non-Responders Non-response has proven to be a significant problem for CanCORS. In order to assess the nature of non-response bias, we will analyze data obtained during the RCA process or available through sites ongoing relationships with registries on patients who did not respond or who declined participation in the larger CanCORS study. The types of information available from most sites (see Appendix A for site-specific details) include demographic data, characteristics of their tumors (including state), first course of treatment and vital status. These data will only be used to assess characteristics on the non-respondents and to develop non-response weights for enrolled participants. Data on non-respondents will not be included in consortium-wide data sets. In addition, we will request Medicare Claims data for non-respondents over the age of 65. These data will provide valuable information regarding potential differences between responders and non-responders in terms of comorbidity and use of health services prior to diagnosis and subsequent treatment for their cancer that will not be available in registry data. See Appendix A for site-specific details on data collection efforts for nonrespondents. 44 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 6.6.1.2 Data Safeguarding of Medicare Claims Data Prior to any linkage the SCC will complete a federal data use agreement. That agreement stipulates that no individual or individuals can be identified using Medicare data, that all results are presented in aggregate only with all cell sizes of 10 or more (either actual or implied), and that all results stemming from analysis of Medicare data receive approval from Medicare prior to publication. Medicare claims data obtained for enrolled patients and non-respondents will be treated with the same precautions aimed at preserving data security and privacy as the other sensitive data collected in this study. The SCC will make a central request for Medicare data across the consortium. The methods outlined in this section will be used to assure the security of data at the third party contractor, the coordinating center and the security of data transfer between the third party contractor, SCC and the sites. Medicare claims data will only be linked to other primary data collection efforts on enrolled patients who consent to this access and linkage. Consent for obtaining Medicare claims data will be included in the medical record consent form (see Appendix J). Some consortium-wide data sets will contain data obtained from enrolled patient’s Medicare claims data. Recipients will need to file a data use agreement with CMS prior to receiving any datasets with Medicare claims data. These data sets will contain encrypted patient and provider identifiers and we will take several additional steps to assure that these data sets do not contain any directly (e.g., social security number) or indirectly identifying data (e.g., exact date or birth or treatment, detailed geographic identifiers). Medicare claims data obtained on non-respondents will only be used to assess characteristics on the non-respondents and to develop non-response weights for enrolled participants. Data on non-respondents will not be included in consortium-wide data sets. Medicare claims data for the census cohorts will not contain any directly identifying patient or provider data. While these data may contain some indirectly identifying information, the SCC will follow the methods outlined above to assure that all indirectly identifying information is deleted from consortium-wide data sets. Recipients will need to file a data use agreement with CMS prior to receiving any datasets with Medicare claims data. Furthermore, we will follow the methods outlined in this section to assure the security of data at the coordinating center and the security of data transfer between the SCC and the sites. We will make no specific attempt to identify or link Medicare claims data on patients or providers who declined to participate in the study. Finally, for those studies that require information that could indirectly identify patients (e.g., access studies that use patient zip codes), no attempt will be made to specifically identify individual patients, and all results will be reported in a manner ensuring individual patient confidentiality. 6.6.2 Other external databases The healthcare system “structure” or “practice environment” that surrounds a patient/physician relationship often affects the treatment decisions that result from that relationship. To understand the impact of environmental and organizational 45 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 characteristics on the decision-making processes of individual cancer patients and their physicians, we plan to supplement the data from the patient survey, medical records, registry, and provider survey with data from several publicly available databases. We will select databases that will provide information about communication channels between physicians in an area; market characteristics, including degree of provider competition; heath insurance market characteristics; provider referral patterns in an area; area socioeconomic structures; and area cultural characteristics. Important sources of these variables may include the American Hospital Association Annual Survey; the Centers for Medicare and Medicaid Services Provider of Service Files; Hospital Cost Report Information Systems Files and Unique Physician Identification Number Directory; the American Medical Association Masterfile database, Census Databases; and the Area Resource File. 7. Data Transfer Protocols and Data Safeguarding Plans 7.1 Data Safeguarding and Transfer for the CATI surveys This section describes the steps that will be taken to maintain the security of the data as it is transmitted to the CATI and Statistical Coordinating Center. Site-specific plans for maintaining security of the RCA data during transmission from the case ascertainment facility and in storage of each PDCR are described in Appendix A. 7.1.1 Description of Potentially Sensitive Data At each PDCR site, potentially sensitive data will be collected from two sources: case ascertainment systems at each site and the patient survey instrument. This section describes the source and content of the sensitive data and the procedures that will be used to protect the data and the identity of the respondents through the research process. Specifically this section addresses the role of the CanCORS CATI Coordinating Center (CCC)/RAND Survey Research Group in the process of collecting data from PDCR sites and monitoring data collection activities at the sites. It also describes the secure data transfer procedures from the CATI Coordinating Center to the Statistical Coordinating Center. These procedures apply to both the baseline and follow-up surveys, for both primary and surrogate respondents, conducted using the CATI system. Although located at the RAND Corporation Offices in Santa Monica, CA, the CATI Coordinating Center is considered part of the Statistical Coordinating Center, and is supported by a subcontract from SCC. Under the direct supervision of senior statisticians from the SCC, the CCC will perform data quality control on the patient survey component of the study and provide consistent de-identified survey results to the SCC from all PDCR sites. The case ascertainment system will provide a wide range of respondent characteristics. To protect confidentiality, a subset of those characteristics necessary for the initial contact and continued follow-up of respondents throughout the course of the study will be stored separately from each site’s CATI system (CASES 5.3j). Specifically, the required subset of variables includes: patient name, telephone number, and address. The second source of potentially sensitive personal information will be collected as part of the patient survey and will form part of the analysis data set. These variables are: Patient Demographics: Date of Birth Gender Marital Status 46 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 Language Race/Ethnicity Level of Schooling Country of Origin Year of Arrival in US Income Level [categorical] Number of Persons in Household Number of Children under 18 Surrogate Respondent Information: Name(s) Address(es) Phone Number(s) Relation(s) to the Patient Health Care Insurance Coverage Information: Name of Primary Health Insurance Plan Dates of Health Services Delivery (date of surgery, etc.) Physician Information: Physician Name(s) Address(es) Phone Number(s) Site of Treatment Hospital/Clinic Name(s) Address(es) Data items collected during the interview process will be stored in the CASES system. The two sources of potentially sensitive data enter the CASES system in different ways. Data from the case ascertainment systems at each site will be displayed for interviewers during the interview using retrievals from a separate (external) database containing information that will not enter the study file. It is the external file that defines for the CASES system the identity of the persons to be called. The second set of potentially sensitive variables are elicited from respondents during the course of the interview and entered into the CASES system from the interviewer’s keyboard. Data in the CASES system, regardless of its mode of entry, populate the system in many different ways. The system maintains a “history” file that tracks all of the system events, throughout the course of the study. Changes to data made by interviewers, system errors, and changes in case status effected through system utilities are all recorded in the history file. During interviews, a trace file is normally written by the CASES system. The trace file tracks all keyboard events as correlated with system events (what was typed at the keyboard in response to a particular item, for instance). The trace file is an important tool for debugging questionnaire problems, evaluating interviewer performance, and reconstructing data for a case should the data become corrupted. In this way, potentially sensitive data collected from respondents will also be written to the trace files. For these reasons, patient name, telephone number and address will not populate the CATI system after the respondent has consented to the interview. Also, personal information will not enter the CASES study files for patients in the queue for contact, patients never sampled, or patients who refuse to participate. 7.1.2 Data Transfer Procedures PDCR sites will transmit to the CCC data collected by the CASES CATI system and audiotapes of randomly selected interviews. The information in the CASES system 47 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 at each site will be transferred to the CATI Coordinating Center monthly. The procedures for securing the data and transferring it to the CATI Coordinating Center will adhere to the following steps: Step 1: An archive file of the CASES study directory and its sub-directories will be created at each PDCR site. The archive file is a binary file readable only by using a utility provided by the CASES system. Step 2: The archive file will be encrypted at each site using a 128-bit algorithm with commercially available software (e.g. PGP). The project will employ an asymmetric public key methodology for encrypting the data. This method will allow the sites to use a public key for encrypting the archive file, while a different, private key is required for decrypting the file. Step 3: The encrypted file will be transmitted to the CATI Coordinating Center via secure FTP that provides a second layer of encryption during transmission. The FTP site will be open only during specified windows of time to further restrict unauthorized access. Step 4: CATI Coordinating Center staff will use a secure copy program to move the encrypted archive file from the FTP server to a second, internal server. The internal server is protected from access outside of RAND by a firewall maintained by RAND’s Internet service provider. Physical access to the internal server is restricted by password protection on the local network. The server itself is located in a locked room within the RAND Santa Monica facility. (RAND is a restricted access facility with 24-hour security). Step 5: The encrypted archive file will be decrypted on the internal server. The archive file will then be extracted into a CASES study directory on the internal server. The result is that the internal server will have an exact replica of the CASES study directories and data as they exist at each PDCR site. Step 6: Each succeeding month’s data will be archived and encrypted prior to the next month’s delivery. Two years following the close of data collection, the CATI Coordinating Center will destroy all files delivered from the PDCR sites. Each site will produce audiotapes of each interviewer’s work. Cases to be taped will be randomly selected and, at the end of the interview, the tape will be labeled with the site ID, the date, the ID of the interviewer, and a program–generated ID that is not the Share Thoughts on Care participant ID. Tapes will be batched and sent to RAND via Federal Express or registered mail quarterly. Once received at RAND, the tapes will be logged and reviewed as part of the quality control process. The tapes will be kept in locked file cabinets in a locked room with restricted access. Tapes will be destroyed 2 years after the close of data collection. From the CATI Coordinating Center (CCC) data will be transferred to the CanCORS Statistical Coordinating Center (SCC). Many of the same techniques for protecting the data will be employed in the CCC-to-SCC transfer. The essential difference is the data sent to the SCC will be de-identified flat files for use in analysis. The following describes the procedures for extracting the case variables and transferring them to the Statistical Coordinating Center: Step 1: Variables identified by the Statistical Coordinating Center as necessary for substantive analysis will be output from the CASES system. The resulting files will be flat ASCII files with an accompanying data map. Step 2: The Statistical Coordinating Center will create public and private keys using the same software used for encryption between the PDCR sites and the CATI Coordinating Center. The Statistical Coordinating Center will then send its public 48 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 key to the CATI Coordinating Center for their encryption. The analysis file will be encrypted using a 128-bit algorithm. Step 3: The encrypted file will be transmitted monthly to the Statistical Coordinating Center via a Secure Sockets Layer (SSL)-encrypted connection on the Statistical Coordinating Center Web site. Step 4: The SSL secured Statistical Coordinating Center Web site will authenticate the user twice, first at the home page, and again at the data upload page. Step 5: At the time of data upload the file is validated to make sure no malicious files are being uploaded instead of the expected data file. Step 6: The uploaded data file is moved into a private directory that is inaccessible through the Web page. Step 7: The file is decrypted using the SCC private key and validated for content. Access to the private directory is limited by UNIX file permissions. Only designated users will be able to upload the data files, and the data upload page is only made available at designated times. Access to the UNIX server holding the data is restricted to selected individuals, and all communication is conducted using the SSL protocol, which encrypts all network traffic between the users and the server. As noted above, the secure internal server at the CCC will house reconstructed CASES study directories identical to those at each PDCR site. This procedure will enable the CCC to: Replicate problems or errors encountered at the PDCR sites. Observe that the sample data are loaded correctly into the CATI system. Check that the structure of the underlying database and the ancillary data files are intact. Receive copies of the trace files (a keystroke record for every case opened by an interviewer) necessary for quality control monitoring and interviewer performance evaluation. Observe the system history for each case from the time it is loaded into the CATI system. This includes the history of call attempts, outcomes, system error messages and system events. These capacities are made possible through the transfer of the CASES archive files to the CCC. It is a consequence, not a goal, of this method that causes all CATI variables to be delivered to the CCC. The CCC has no particular interest in these variables beyond ensuring that they appear properly in the questionnaires at the PDCR sites. The procedures described present no more than minimal risk of harm to the study respondents. Access to the data is restricted and encrypted during data transmission between the PDCR sites and the CCC. Once at the CCC, only CCC staff will have access to the data. 7.2 Safeguarding and Transfer of Data Abstracted from Medical Records Data abstracted from medical records will be kept secure in all steps from the point of collection to storage at the SCC. All medical record abstractors using MedQuest on portable computers will be required to install BIOS passwords on the computer, protecting both the computer and the disk drive from unauthorized use. Data abstractors using portable computers will be required to transfer data to secure storage behind the PDCR firewall as soon as possible and to delete patient specific data files from the portable computer. All data gathered from electronic medical records will be stored on secure computers behind PDCR firewalls. 49 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 The transfer of medical record data to the SCC will follow the same procedures outlined in the data transfer protocol between the CATI Coordinating Center and the SCC, with the following differences: Each PDCR site will maintain a secure MedQuest database into which the data from the medical abstractions will be entered. The data dictionary for this database will be provided by the Statistical Coordinating Center. In step 1, the variables necessary for data analyses will be binary MedQuest database files. In step 2, the encryption keys will be shared between the Statistical Coordinating Center and the PDCR sites. All other steps remain identical. 7.3 Data Safeguarding of Medicare Claims Data Medicare claims data will only be obtained and linked to other primary data collection efforts on enrolled patients who consent to this access and linkage. Consent for obtaining Medicare claims data will be included in the medical record consent form (see Appendix J). Medicare claims data obtained for these patients will be treated with the same precautions aimed at preserving data security and privacy as the other sensitive data collected in this study. The SCC will make a central request for Medicare data on all consenting patients across the consortium. The methods outlined in this section will be used to assure the security of data at the coordinating center and the security of data transfer between the SCC and the sites. Some consortium-wide data sets will contain data obtained from patient’s Medicare claims data. These data sets will contain encrypted patient and provider identifiers and we will take several additional steps to assure that these data sets do not contain any directly (e.g., social security number) or indirectly identifying data (e.g., exact date or birth or treatment, detailed geographic identifiers). Medicare claims data for the census cohorts will not contain any directly identifying patient or provider data. While these data may contain some indirectly identifying information, the SCC will follow the methods outlined above to assure that all indirectly identifying information is deleted from consortium-wide data sets. Furthermore, we will follow the methods outlined in this section to assure the security of data at the coordinating center and the security of data transfer between the SCC and the sites. We will make no specific attempt to identify or link Medicare claims data on patients or providers who declined to participate in the study. Finally, for those studies that require information that could indirectly identify patients (e.g., access studies that use patient zip codes), no attempt will be made to specifically identify individual patients, and all results will be reported in a manner ensuring individual patient confidentiality. 8. Risks and Benefits for Participants There will be no direct benefits for study participants. However, it is hoped that the comprehensive data on patient and provider attitudes and processes of care gathered in this study will improve the future care and experiences of patients with lung and colorectal cancer, the two leading causes of cancer mortality in the United States. As stated in the introduction, this study provides a unique opportunity to examine care for lung and colorectal cancer patients in community settings in multiple regions of the United States, to identify variations in care, and to begin to understand the reasons for these variations. By collecting and analyzing data from a large number of patients in geographically diverse settings, we expect that the findings of this study will help clinicians and policy-makers improve cancer care and the experiences of cancer patients. 50 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 The main potential risks to patients in this study are a loss of confidentiality about their disease or treatment and possible psychological distress caused by discussing details of their disease and treatment with interviewers. 8.1 Strategies to Minimize Risk The details of the methods for minimizing the risk of a breach of confidentiality of patient and provider data are described in Section 7. The following steps will be taken to minimize psychological distress for patient participants: The introductory script for the telephone interview explains the nature of the survey and mentions the kind of questions that will be asked. Participants will have the opportunity to end the interview at that time. All interviewers will be trained personnel with experience in interviewing subjects about illness and its implications. Interviewers at each PDCR site will have the name and telephone number of the CanCORS PI for that site or of a trained clinician or social worker who can be contacted, if necessary. All domains of the questionnaire have been excerpted from previously published instruments that have been used with patients or from instruments that have been fieldtested and are in current use. Randomly selected interviews will be audiotaped and reviewed to insure that interviewers are carefully adhering to the CATI scripts and respectfully administering the interviews. It is possible that during the course of an interview, the interviewer may sense that a participant has become distressed. If this occurs, the interviewer will be sensitive to the emotional state of the interviewee and be supportive to him or her. The interviewer will check with the individual about their comfort level and willingness to continue. The interviewer will not press the participant to continue. If the participant chooses to stop the interview, the interviewer will thank the participant for their time and ask him/her if he/she would like the phone number of the CanCORS PI for that site or a trained clinician or social worker. If the participant becomes extremely upset, the interviewer will stop the interview and focus on the participant's emotional state. If the patient is sufficiently distressed, depressed, or emotionally disturbed, the interviewer will immediately contact the CanCORS PI for that site or a trained clinician or social worker, who will then call the participant. The scripts in Appendix D describe the language the interviewer will use in these instances. Since the survey may not be scored until months after the interview, interventions based on scale scores will not be feasible. Since there will also be delays in reviewing selected audiotapes of interviews (for quality control purposes), interventions based on the content of an audiotape will also not be feasible. Subjects will be clearly informed prior to the interview that their responses will not be shared with their providers. In addition, the CanCORS Statistical Coordinating Center has obtained a Certificate of Confidentiality (NCI-02-007) from the National Institutes of Health to protect the privacy of participants. As is stated in documentation sent with the certificate, CanCORS investigators “cannot be forced (for example, by court subpoena) to disclose information that may identify [a subject] in any federal, state, or local civil, criminal, administrative, legislative, or other proceedings.” This certificate cannot be used to block the release of data voluntarily requested by a study participant. The CanCORS Statistical Coordinating Center has also obtained a Memorandum of Understanding (AHRQ No. 03-438MO-03, NCI No. U01CA093344). This states that the Agency for Healthcare Research and Quality (AHRQ) will “provide expert advice and 51 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 consultation on patient outcomes and quality of care measures to CanCORS research projects through the NCI Program Director. Under this agreement, CanCORS will be subject to the confidentiality provisions of 924(c) of the U.S. Public Health Service Act.” This statute provides, in summary, that no identifying information obtained in the course of the AHRQsupported CanCORS projects may be used for any purpose other than for which it is provided to the CanCORS, and that such information may not be published or released unless the individual data subject(s) or person(s) or organization(s) providing the information has or have consented. Only authorized CanCORS and DHHS staff or agents will have access to the information collected. In addition, any unauthorized disclosure of the protected confidential information is punishable under the PHS Act (42 USC 299c-3(d)). 52 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients 9. Protocol 001 Amendment #3, December 2005 Reference 1 http://healthservices.cancer.gov/cancors 2 National Cancer Policy Board. Ensuring Quality Cancer Care. Washington, DC: National Academy Press; 1999. Hewitt M, Simone JV, eds. 3 Braddock CH III, Edwards KA, Hasenberg NM, Laidley TL, Levinson W. Informed decision making in outpatient practice: Time to get back to basics. JAMA 1999; 282(24):2313-20. 4 Keating NL, Weeks JC, Borbas C, Guadagnoli E. Treatment of early-stage breast cancer – Do surgeons inform patients about treatment alternatives? In press. 2002. 5 Bach PB, Cramer LD, Warren JL, Begg CB. Racial differences in the treatment of early-stage lung cancer. N Engl J Med 1999; 341(16):1198-205. 6 Ballard-Barbash R, Potosky AL, Harlan LC, Nayfield SG, Kessler LG. Factors associated with surgical and radiation therapy for early stage breast cancer in older women. J Natl Cancer Inst 1996; 88(11):716-26. 7 Nattinger AB, Hoffmann RG, Kneusel RT, Schapira MM. Relation between appropriateness of primary therapy for early-stage breast carcinoma and increased use of breast-conserving surgery. Lancet 2000; 356(9236):1148-53. 8 Schrag D, Gelfand SE, Bach PB, Guillem J, Minsky BD, Begg CB. Who gets adjuvant treatment for stage II and III rectal cancer? Insight from surveillance, epidemiology, and end results–Medicare. J Clin Oncol 2001; 19(17):3712-8. 9 Hillner BE, McDonald MK, Penberthy L, Desch CE, Smith TJ, Maddux P, et al. Measuring standards of care for early breast cancer in an insured population. J Clin Oncol 1997; 15(4):1401-8. 10 Schrag D, Cramer LD, Bach PB, Begg CB. Age and adjuvant chemotherapy use after surgery for stage III colon cancer. J Natl Cancer Inst 2001; 93(11):850-7. 11 Berry ZS, Lynn J. Hospice medicine. JAMA 1993; 270(2):221-3. 12 National Cancer Policy Board. Improving Palliative Care for Cancer. Washington, DC: National Academy Press; 2001. 13 Greenfield S, Blanco DM, Elashoff RM, Ganz PA. Patterns of care related to age of breast cancer patients. JAMA 1987; 257(20):2766-70. 14 Goodwin JS, Hunt WC, Samet JM. Determinants of cancer therapy in elderly patients. Cancer 1993; 72(2):594-601. 15 Hodgson DC, Fuchs CS, Ayanian JZ. Impact of patient and provider characteristics on the treatment and outcomes of colorectal cancer. J Natl Cancer Inst 2001; 93(7):501-15. 16 Potosky AL, Harlan LC, Kaplan RS, Johnson KA, Lynch CF. Age, sex, and racial differences in the use of standard adjuvant therapy for colorectal cancer. J Clin Oncol 2002; 20(5):1192-202. 17 Shavers VL, Brown ML. Racial and ethnic disparaties in the receipt of cancer treatment. J Natl Cancer Inst 2002; 94(5):334-57. 18 Earle CC, Venditti LN, Neumann PJ, Gelber RD, Weinstein MC, Potosky AL, et al. Who gets chemotherapy for metastatic lung cancer? Chest 2000; 117(5):1239-46. 19 Ayanian JZ, Kohler BA, Abe T, Epstein AM. The relation between health insurance coverage and clinical outcomes among women with breast cancer. N Engl J Med 1993; 329(5):326-31. 20 Riley GF, Potosky AL, Klabunde CN, Warren JL, Ballard-Barbash R. Stage at diagnosis and treatment patterns among older women with breast cancer: an HMO and fee-for-service comparison. JAMA 1999; 281(8):720-6. 53 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 21 Bradley CJ, Given CW, Roberts C. Race, socioeconomic status, and breast cancer treatment and survival. J Natl Cancer Inst 2002; 94(7):490-6. 22 Nattinger AB, Goodwin JS. Geographic and Hospital Variation in the Management of Older Women With Breast Cancer. Cancer Control 1994; 1(4):334-38. 23 Nattinger AB, Kneusel RT, Hoffmann RG, Gilligan MA. Relationship of distance from a radiotherapy facility and initial breast cancer treatment. J Natl Cancer Inst 2001; 93(17):1344-6. 24 Liberati A, Patterson WB, Biener L, McNeil BJ. Determinants of physicians' preferences for alternative treatments in women with early breast cancer. Tumori 1987; 73(6):601-9. 25 Tarbox BB, Rockwood JK, Abernathy CM. Are modified radical mastectomies done for T1 breast cancers because of surgeon's advice or patient's choice? Am J Surg 1992; 164(5):417-20; discussion 20-2. 26 Smitt MC, Heltzel M. Women's use of resources in decision-making for early-stage breast cancer: results of a community-based survey. Ann Surg Oncol 1997; 4(7):564-69. 27 Romano PS, Mark DH. Patient and hospital characteristics related to in-hospital mortality after lung cancer resection. Chest 1992; 101(5):1332-7. 28 Schrag D, Cramer LD, Bach PB, Cohen AM, Warren JL, Begg CB. Influence of hospital procedure volume on outcomes following surgery for colon cancer. JAMA 2000; 284(23):3028-35. 29 Ayanian JZ, Zaslavsky AM, Fuchs CS, Guadagnoli E, Creech CM, Cress RD, O'Connor LC, West DW, Allen ME, Wolf RE, Wright WE. Use of adjuvant chemotherapy and radiation therapy for colorectal cancer in a population-based cohort. J Clin Oncol 2003; Accepted for Publication. 30 Potosky, A. NCI, personal communication. 31 Potosky AL, Riley GF, Lubitz JD, Mentnech RM, Kessler LG. Potential for cancer related health services research using a linked Medicare-tumor registry database. Med Care. 1993; 31(8):732-748. 54 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 Appendix A: Method for Participant Identification and Contact (UNC) A-1 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 CANCORS: APPENDIX A UNVERSITY OF NORTH CAROLINA AT CHAPEL HILL P.I. – ROBERT SANDLER, MD, MPH Eligibility requirements We will enroll 1000 persons residing in a contiguous 33-county region of central North Carolina who are diagnosed with histologically or cytologically confirmed primary, invasive colorectal adenocarcinoma (ICD-10 C18, C19, C20) between May 1, 2003 and May 1, 2005. Eligible participants must be age 21 or over and may be of any ethnicity. Pregnant women are not excluded and women who become pregnant during the study will not be withdrawn. If cases are cognitively impaired, have language or hearing problems, or have died, we plan to conduct interviews with next of kin or an appropriate surrogate. Inducements for participation We will pay participants $15 to complete the baseline telephone interview and $20 for signing and returning consent forms. Methods of recruiting Cases will be identified through the Rapid Ascertainment System of the North Carolina Central Cancer Registry (CCR). This mechanism has been successfully used for six years in another study at our Center. Case reports from the CCR always include the name of the physician of record. The CCR requires us to notify this physician of our intent to contact the patient. If we do not receive an objection from the physician within three weeks, we will mail the patient a letter, a list of FAQ’s and a study brochure describing the study. Letters include a toll-free number for participants to call for questions or to decline participation. Approximately ten days after the introductory letter is sent, interviewers will phone potential participants to explain the study, answer questions, and seek participation. Once verbal permission is obtained, the interviewer will either complete the telephone interview at that time or make an appointment for a more convenient time. The target for the administration of the baseline telephone survey is 12 - 18 weeks from diagnosis. Interviews may be conducted up to 12 months after diagnosis. If the interviewer has not spoken to the potential participant after 10 call attempts, we will send a second letter and a study brochure by Federal Express. This letter will explain the study and also inform the participant of our wish to interview them before a specified date. Methods of obtaining informed consent After the participant has completed the interview, we will mail the incentive check, study consent, HIPAA authorization form, release/consent forms for medical record review and biological specimens as well as a cover letter and instructions for signing and returning the forms. Approximately two weeks after this is mailed, study staff will contact participants by phone to answer any questions concerning the materials. The consent forms will be color coded to facilitate discussion about each form over the phone. A postage paid envelope will be included for the return of the consent forms. A-2 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 If the participant agrees, arrangements will be made to collect a blood sample. The sample will be drawn either at the participant’s next clinic appointment or by a CanCORS staff member in the participant’s home. All costs for the blood draw will be borne by the research study. Methods of increasing participation rates If a participant does not wish to complete the one-hour telephone interview, we will offer the following options (in order of preference) on an as needed basis: Brief telephone interview (15-20 minutes) Surrogate telephone interview (with a family member identified by the participant) Self-administered survey Participation by medical records review only with no interview Data on non-participants: Non-response is proving to be a significant problem for CanCORS. Without an ability to assess the nature of non-response we will have difficulty placing the information we collect into proper context, thereby limiting the value of all data from the study. In order to assess the nature of non-response bias, we will provide the SCC data obtained during the RCA process on sampled patients who could not be reached or who declined participation in all or parts of the larger CanCORS study. Data on non-participants will only be used to assess characteristics of the non-respondents and to develop non-response weights for enrolled participants. Data elements available include demographic characteristics (age, race, gender), characteristics of their tumors (stage), and vital status. In addition, we will request Medicare Claims data for sampled participants age 65 and older who could not be reached or who declined participation in all or parts of the larger CanCORS study. Medicare claims data will allow us to better characterize non-participants in terms of comorbid illness and subsequent treatment and will therefore be invaluable in placing our study into the proper context and maximizing the value of data collected on enrolled patients. Medical claims data will only be used to assess characteristics on the non-respondents and to develop nonresponse weights for enrolled participants. Data will be linked using the participant’s social security number, gender and date of birth using the same methods described in section 6.6.1. A-3 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 Appendix B: PDCR Sites and Geographic Area of Enrollment B-1 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 Patients eligible to participate in the Share Thoughts on Care study will be recruited by the following sites according to their associated geographic regions of the United States. University of Alabama at Birmingham (UAB) The entire state of Alabama. Harvard Medical School/Northern California Cancer Center (HMS/NCCC) Including the following counties in northern California: Alameda Contra Costa Sacramento San Francisco San Joaquin San Mateo Santa Clara Solano University of Iowa (UI) The entire state of Iowa. UCLA/RAND Los Angeles County. University of North Carolina, Chapel Hill (UNC) Including the following counties in eastern and central North Carolina: Alamance Bertie Chatham Durham Edgecombe Greene Guilford Harnett Johnston Lee Lenoir Martin Montgomery Moore Nash Orange Pamlico Pitt Randolph Wake Wayne Wilson B-2 Beaufort Cabarrus Craven Davidson Forsyth Jones Mecklenburg Rowan Stanly Union Washington “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 Dana–Farber Cancer Institute/Cancer Research Network (DFCI/CRN) Patients recruited from this site will be identified through participation in the following HMOs: Group Health Cooperative – Seattle, WA Harvard Pilgrim Health Care – Boston, MA Henry Ford Health System – Detroit, MI Kaiser Permanente NorthWest – Portland, OR Kaiser Permanente Hawaii – Honolulu, HI Department of Veterans Affairs, Durham and Minneapolis VAMCs, and Duke University/University of Minnesota (VA) Patients recruited from this site will be identified through participation in the following Veterans Affairs Medical Centers: NY Harbor, NY ** Chicago, IL *** (Lakeside/Hines) Baltimore, MD Tucson, AZ Durham, NC Biloxi, MS Nashville, TN Temple, TX Minneapolis, MN Atlanta, GA Indianapolis, IN Houston, TX Seattle, WA ** The Harborside NY Harbor Healthcare System program has a combined registry between Manhattan and Brooklyn. ***The Chicago VA has a combined registry between Lakeside and Westside campuses. B-3 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 Appendix C: Disease Specific Eligibility Checklist C-1 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 Each site receives data on incident cases from their local RCA entity, typically a state operated tumor registry or, for CRN sites and the VA, a health-care entity based registry. RCA entities should be given a list of eligibility criteria to minimize reporting of ineligible cases. The following checklist can be used for this purpose: Eligibility Checklist Persons 21 years or older diagnosed with primary, invasive, non-recurrent tumors of the lung or colon/rectum are eligible as follows: Age at Diagnosis Residency Tumor site Tumor Stage Diagnosis Histology First Primary Recurrences Primary tumor 21 years or older Resident in geographic area of interest at time of diagnosis and initial contact (or patient in participating provider organization) Lung or colorectal Invasive cancers only (in-situ diagnoses excluded) Histologically or cytologically confirmed diagnoses only See Histology Codes below Only first primary diagnoses of lung or colorectal cancer are included (second primary tumors of the lung, colon, or rectum are excluded). Simultaneous diagnoses (within 2 months) at different sites are not eligible. However, patients with more than one primary tumor of the same site (that is, two lung primaries or two colon primaries within 2 months) are eligible. Newly diagnosed cancers only (recurrences of cancers diagnosed prior to the ascertainment period excluded) Must be primary tumor of the lung, colon, or rectum (metastases to lung/colon/rectum from another site excluded) Often, one or more of these criteria are not stated explicitly on the path report. The convention in applying these criteria should be that a case is eligible unless a positive statement in the data indicates otherwise. For example, if a path report does not state whether a tumor is a recurrence or not, it is assumed to be newly diagnosed, thus that case is considered eligible. Stated another way, all cases of lung or colorectal cancer in the relevant geographic area are eligible unless the data source indicates that it is not invasive, is not histologically or cytologically confirmed, is not one of the histologic subtypes, is a second primary or recurrence, or is metastatic to the site. Each site should review cases’ nominal eligibility after receiving RCA case reports in order to identify and exclude any ineligible cases that may have been reported in error by the local RCA entity. The extent of this review/confirmation will necessarily depend on the quality of the local RCA data and should be performed as determined locally by each site to minimize contacting an ineligible case. Thus, if a site determines that all the above criteria are highly reliably reported by their RCA source, then little if any review/confirmation is necessary. Histology Codes Each site receives diagnostic information from their local RCA source. Pathology reports and/or RCA data files may include ICD-coded histologic subtypes, while other path reports contain non-coded descriptive histology. Some path reports may contain other histologic coding besides ICD. This is due to variation in quality of path reports by hospital and variation in the extent of coding provided by RCA sources. The following lists the eligible ICD-coded histologic subtypes for this study (International Classification of Diseases for Oncology, 3rd Edition, U.S. Interim Version 2000, pages 69-81). Subtypes not on this list are rare and/or lead to substantively different treatment pathways and outcomes and thus are excluded to avoid subgroups that cannot be analyzed adequately in this study. The eligible codes C-2 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 listed include over 95% of all lung and colorectal cancers. As long as a case has at least one of the eligible histologic subtypes specified, they are eligible, even if they also have a histology subtype specified that is not on this list. To verify case eligibility with respect to histology, each site should use whatever specific information is included in the path report and/or RCA record to determine whether the histology is an eligible type. If the path report data includes ICD codes, use them. If the path report does not contain ICD codes, or contains other coding, the site will need to determine from the language in the path report whether the histology is one of the eligible types. One or more designated persons can perform this task at each site, with a provision for consult with a clinician or pathologist for adjudication of ambiguous reports. Given that this list was designed to capture 95% of all lung and colorectal cancers, cases may be presumed eligible unless the path data specifically indicates a subtype (by coding or by description) that is not one of the eligible types. Some path reports use non-specific coding when the pathologist cannot determine the subtype from the specimen. If a colorectal case is coded as: 8000/3 Neoplasm, malignant 8001/3 Tumor cells, malignant or a lung case is coded as: 8000/3 Neoplasm, malignant 8001/3 Tumor cells, malignant 8002/3 Malignant tumor, small cell type 8003/3 Malignant tumor, giant cell type 8004/3 Malignant tumor, spindle cell type 8005/3 Malignant tumor, clear cell type the case is eligible. However, for these general subtypes, follow-up with the RCA entity or hospital is required to see if a more specific coding is available from subsequent procedures. If so, and if it is not one of the eligible subtypes, the case should be re-coded as ineligible. ELIGIBLE HISTOLOGIC SUBTYPES: COLORECTAL COLORECTAL SITES: C18.0-C18.9 – COLON C19.9 – RECTOSIGMOID JUNCTION C20.9 – RECTUM Adenocarcinomas of the following subtypes are eligible: 8010/3 Carcinoma, NOS 8140/3 Adenocarcinoma 8210/3 Adenocarcinoma in an adenomatous polyp 8261/3 Adenocarcinoma in villous adenoma 8262/3 Villous adenocarcinoma 8263/3 Adenocarcinoma in tubulovillous adenoma 8480/3 Mucinous adenocarcinoma 8481/3 Mucin-producing adenocarcinoma 8490/3 Signet ring cell adenocarcinoma Non-specific diagnoses of the following subtypes are eligible: 8000/3 Neoplasm, malignant 8001/3 Tumor cells, malignant ELIGIBLE HISTOLOGIC SUBTYPES: LUNG C-3 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 LUNG SITES: C34.0 – C34.3, C34.8 – C34.9 – LUNG The following histologic subtypes are eligible: 8010/3 8011/3 8012/3 8013/3 8015/3 8020/3 8021/3 8022/3 8030/3 8031/3 8032/3 8033/3 8034/3 8035/3 8041/3 8042/3 8043/3 8044/3 8045/3 8046/3 8050/3 8051/3 8052/3 8070/3 8071/3 8072/3 8073/3 8074/3 8075/3 8076/3 8082/3 8083/3 8084/3 8090/3 8093/3 8094/3 8097/3 8120/3 8122/3 8123/3 8140/3 8141/3 8147/3 8200/3 8211/3 Carcinoma, NOS Epithelioma, malignant Large cell carcinoma, NOS Large cell neuroendocrine carcinoma Glassy cell carcinoma Carcinoma, undifferentiated, NOS Carcinoma, anaplastic, NOS Pleomorphic carcinoma Giant cell and spindle cell carcinoma Giant cell carcinoma Spindle cell carcinoma, NOS Pseudosarcomatous carcinoma Polygonal cell carcinoma Carcinoma with osteoclast-like giant cells Small cell carcinoma, NOS Oat cell carcinoma Small cell carcinoma, fusiform cell Small cell carcinoma, intermediate cell Combined small cell carcinoma Non-small cell carcinoma Papillary carcinoma, NOS Verrucous carcinoma, NOS Papillary squamous cell carcinoma Squamous cell carcinoma, NOS Squamous cell carcinoma, keratinizing, NOS Squamous cell carcinoma, large cell, nonkeratinizing, NOS Squamous cell carcinoma, small cell, nonkeratinizing Squamous cell carcinoma, spindle cell Squamous cell carcinoma, adenoid Squamous cell carcinoma microinvasive Lymphoepithelial carcinoma Basaloid squamous cell carcinoma Squamous cell carcinoma, clear cell type Basal cell carcinoma, NOS Basal cell carcinoma, fibroepithelial Basosquamous carcinoma Basal cell carcinoma, nodular Transitional cell carcinoma, NOS Transitional cell carcinoma, spindle cell Basaloid carcinoma Adenocarcinoma, NOS Schirrous adenocarcinoma Basal cell adenocarcinoma Adenoid cystic carcinoma Tubular adenocarcinoma C-4 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients 8250/3 8251/3 8252/3 8253/3 8254/3 8255/3 8260/3 8310/3 8314/3 8315/3 8320/3 8323/3 8333/3 8341/3 8342/3 8343/3 8430/3 8440/3 8441/3 8450/3 8452/3 8470/3 8471/3 8473/3 8480/3 8481/3 8490/3 8525/3 8530/3 8550/3 8551/3 8560/3 8562/3 8570/3 8571/3 8572/3 8573/3 Protocol 001 Amendment #3, December 2005 Bronchiolo-alveolar adenocarcinoma, NOS Alveolar adenocarcinoma Bronchiolo-alveolar carcinoma, non-mucinous Bronchiolo-alveolar carcinoma, mucinous Bronchiolo-alveolar carcinoma, mixed mucinous and non-mucinous Adenocarcinoma with mixed subtypes Papillary adenocarcinoma, NOS Clear cell adenocarcinoma, NOS Lipid-rich carcinoma Glycogen-rich carcinoma Granular cell carcinoma Mixed cell adenocarcinoma Fetal adenocarcinoma Papillary microcarcinoma Papillary carcinoma, oxyphilic cell Papillary carcinoma, encapsulated Mucoepidermoid carcinoma Cystadenocarcinoma, NOS Serrous cystadenocarcinoma, NOS Papillary cystadenocarcinoma, NOS Solid pseudopapillary carcinoma Mucinous cystadenocarcinoma, NOS Papillary mucinous cystadenocarcinoma Papillary mucinous cysadenoma, borderline malignancy Mucinous adenocarcinoma Mucin-producing adenocarcinoma Signet ring cell carcinoma Polymorphous low grade adenocarcinoma Inflammatory carcinoma Acinar cell carcinoma Acinar cell cystadenocarcinoma Adenosquamous carcinoma Epithelial-myoepithelial carcinoma Adenocarcinoma with squamous metaplasia Adenocarcinoma with cartilaginous and osseous metaplasia Adenocarcinoma with spindle cell metaplasia Adenocarcinoma with apocrine metaplasia Non-specific diagnoses of the following subtypes are eligible: 8000/3 Neoplasm, malignant 8001/3 Tumor cells, malignant 8002/3 Malignant tumor, small cell type 8003/3 Malignant tumor, giant cell type 8004/3 Malignant tumor, spindle cell type 8005/3 Malignant tumor, clear cell C-5 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 Appendix D: Introductory Interview Scripts and Full Patient Survey D-1 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 The following scripts have been approved by the CanCORS membership; however, changes may be made, if required by your IRB. Please note the text in red (underlined) cannot be modified. Interviewer Notes: After each phone contact, a disposition code will be generated. This will serve several purposes including making sure that appropriate call backs are generated, assessing patient and surrogate status, assessing quality, and describing the sample. If the person states that they have cancer, you should automatically switch to using the word cancer instead of “problem or disease” to make the participant feel more comfortable. PATIENT SCRIPTS WHEN A PERSON ANSWERS THE PHONE: “Hello, my name is ___________ and I am calling from (Name of Institution). May I please speak to (Name of Patient)?” SOMEONE BESIDES PATIENT ANSWERS THE PHONE, BUT PATIENT THEN COMES TO THE PHONE: “Hello, my name is ___________ and I am calling from (Name of Institution). I’m calling on behalf of the Share Thoughts on Care study, which is a study to learn more about the experiences of patients with newly diagnosed lung or colorectal problems. You have been identified as someone who may qualify for our study. Did you receive the information we recently mailed to you?” PATIENT ANSWERS THE PHONE: “I’m calling from the Share Thoughts on Care study, which is a study to learn more about the experiences of patients with newly diagnosed lung or colorectal problems. You have been identified as someone who may qualify for our study. Did you receive the information we recently mailed to you?” IF PATIENT INDICATES THAT THEY DID RECEIVE THE MAILING: “Do you have any questions?” (Answer any questions then ask about interview). “Is this a convenient time to do an interview?” IF NO: GO TO 1. (refusal conversion strategy) IF PATIENT INDICATES NOT A GOOD TIME, ASKS YOU TO CALL BACK, OR SIMILAR RESPONSE: GO TO 2. (call back procedure) IF PATIENT INDICATES WORRY ABOUT HAVING ENERGY OR TIME TO PARTICIPATE IN INTERVIEW – NOT EXACTLY REFUSING OR SAYING IT IS A BAD TIME: GO TO 3. IF YES: GO TO 4. (verbal consent) IF PATIENT INDICATES THAT THEY DID NOT RECEIVE THE MAILING: “I would be happy to mail you the information again if you like. Since I have you on the phone right now, may I take a few moments of your time to tell you about the study?” D-2 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 IF YES: “Share Thoughts on Care is designed to learn about treatment of diseases of the lung, colon and rectum. We hope to learn more about how people with newly diagnosed cases of lung or colorectal diseases are treated for their disease, what influences the treatments they choose, and their experiences with care. Your views and thoughts are very important, because they can help us gain valuable information about how to improve care now and in the future. Your doctor is aware that we are contacting you for this study. Share Thoughts on Care is sponsored by the National Institutes of Health and the Department of Veterans Affairs and is being conducted by researchers from twenty-five hospitals and institutions across the country. If you choose to participate in Share Thoughts on Care, you will be asked to take part in an interview. You will not be asked to take any medical tests, nor will you need to undergo any medical treatment. Share Thoughts on Care is interested in your opinions only. All of your answers and personal information will be kept confidential. The length of the interview depends on the treatments you have received and the amount of information you wish to share with us. The interview usually takes about an hour. (If concerned about the length, offer to administer it in sections). Would you be willing to participate in this study today?” (Move to appropriate number based on answer.) IF NO: GO TO 1. (refusal conversion strategy) IF PATIENT INDICATES NOT A GOOD TIME, ASKS YOU TO CALL BACK, OR SIMILAR RESPONSE: GO TO 2. (call back procedure) IF PATIENT INDICATES WORRY ABOUT HAVING ENERGY OR TIME TO PARTICIPATE IN INTERVIEW – NOT EXACTLY REFUSING OR SAYING IT IS A BAD TIME: GO TO 3. IF YES: GO TO 4. (verbal consent) IF PATIENT WANTS INFORMATION MAILED AGAIN: “Let me confirm your mailing address. The address we have is (Read Address). Is that correct?” IF YES: “Great. I’ll send the information to you and try to call back in about a week. Is there a day or time that works better for you? (Try to find out good time for callback) Thank you.” IF NO: “What is the correct mailing address? (Record Address.) Thank you. I’ll send the information to you and try to call back in about a week. Is there a day or time that works better for you? (Try to find out good time for callback) Have a nice day.” D-3 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients 1. Protocol 001 Amendment #3, December 2005 REFUSAL CONVERSION STRATEGY THE GOAL HERE IS TO GET THE COMPLETE SURVEY. THE BRIEF SURVEY SHOULD ONLY BE USED WHEN THE ALTERNATIVE IS COMPLETE REFUSAL 1a. “Lots of people aren’t very comfortable when they are called on the phone about studies. What kinds of concerns or worries do you have about being in this study?” (Avoid argumentative tone, use soothing, accepting understanding tone) 1ai. 1b. 1c. 1d. Respondent expresses one or more concerns, worry or questions Interviewer responds by answering questions/ provides reassurance using info sheet with common R concerns, questions and responses. Next steps depends on specific concerns but in general GO TO 1b 1aii. Respondent does not state specific worry or question. GO TO 1b Interviewer: “The National Institutes of Health asked well-respected researchers to conduct this study because they really want to understand the experiences of people like you. Each person is unique and so your information is really important to the study and I’d hate to see it left out. We could try getting started and then stop any time you want to and finish later. We would be happy to split up the interview over two or more calls at any time that is good for you.” 1bi. Respondent agrees. GO TO 4 (verbal consent) if the respondent agrees to start now, otherwise schedule callback. 1bii. Respondent declines. GO TO 1c (brief interview request) “I know that for many people it is just so hard to find time for a long interview. We have a very brief version that should only take 20 minutes to complete. I can do that now if you like.” 1ci. Respondent agrees. GO TO 4 (verbal consent) and then conduct BRIEF SURVEY if the respondent agrees to start now, otherwise schedule callback. 1cii. Respondent declines. GO TO 1d. Where appropriate (see interviewer guidelines), offer PROXY SURVEY. “Many people prefer to have family member or friend who knows a lot about their experiences do the interview instead. Is there someone who knows a lot about your recent colon/lung problem that we can talk to?” 1di. Respondent agrees. Get surrogate information and medical record consent (go to 1e) and then call surrogate to schedule interview. 1dii. Respondent declines or proxy not appropriate. If NOT CRN, GO TO 1e. (medical record only option). If CRN, offer CAPI “Would you be willing to meet with me to do the interview in person? I could meet you here at the research center, or at the clinic either before or after your next appointment, or I could come to where you are. Whatever is most convenient for you.” D-4 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 1diia. Respondent declines CAPI. GO TO 1e (Medical Record consent only). 1diib. Respondent accepts CAPI. “Thank you.” Schedule appt as written below. PATIENT PREFERS RESEARCH CENTER: GIVE DIRECTIONS AND SET UP A DATE AND TIME. PATIENT PREFERS CLINIC: ASK WHEN HIS/HER NEXT APPT IS AND IF THEY PREFER TO MEET FOR AN HOUR BEFORE THE APPT OR STAY FOR AN HOUR AFTER THE APPT. PATIENT PREFERS RESIDENCE: CONFIRM ADDRESS AND SET UP CONVENIENT TIME FOR INTERVIEW. 1e. ASK FOR MEDICAL RECORD CONSENT ONLY: “I understand that you are not interested in participating in the interview. With your permission, we would like to review your medical record so we can compare the medical care people receive in your community to other parts of the country. We would like your permission to request copies of your records from doctors you have seen or for services that may have been paid for by Medicare. Your participation is completely voluntary. We will keep these records private and confidential to the full extent of the law. We will only receive copies of the necessary parts of these medical and Medicare records. Would you be willing to let us review your records related to the treatment of your lung or colorectal problem?” 1ei. Respondent accepts. “Great, thank you. We will send you a medical and Medicare record release form, which will include instructions and a form to sign to give us permission to review your records. You should receive this in the next few days. If you have any questions you can call us at (TOLL FREE NUMBER). Thank you.” 1eii. Respondent declines. KEEP DOOR OPEN FOR FUTURE REFUSAL CONVERSION. “Thank you for your time with me today – I really appreciate it. Can we check back with you in the future to see how you are doing?” 1eiii Respondent says that surrogate will make decision. “Does named surrogate have legal authority to sign for you.” If yes, ask for medical record consent during surrogate interview. If no, offer to send release form and instructions for the respondent to look at with the help of the surrogate. D-5 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients 2. Protocol 001 Amendment #3, December 2005 CALL BACK PROCEDURE Make call-back appointment and (ideally): Send respondent postcard with call-back appointment, reiteration of the importance of study and value of their participation. SCRIPT FOR INITIAL CONTACT DURING CALLBACK WHEN A PERSON ANSWERS THE PHONE: “Hello, my name is ___________ and I am calling from (Name of Institution). May I please speak to (Name of Patient)?” SOMEONE BESIDES PATIENT ANSWERS THE PHONE, BUT PATIENT THEN COMES TO THE PHONE: “Hello, my name is ___________ and I am calling from (Name of Institution). I’m calling on behalf of the Share Thoughts on Care study. We spoke on (state date of last conversation) and you seemed interested in participating in our study to learn more about the experience of patients with newly diagnosed lung or colorectal problems. You had suggested I call back at this time. Is this a good time to start the interview? PATIENT ANSWERS THE PHONE: I’m calling on behalf of the Share Thoughts on Care study. We spoke on (state date of last conversation) and you seemed interested in participating in our study to learn more about the experience of patients with newly diagnosed lung or colorectal problems. You had suggested I call back at this time. Is this a good time to start the interview? Respondent agrees. Go to 4 (verbal consent). Respondent indicates not a good time, asks you to call back. “Your information is really important to the study. Is it possible to do a bit of it now and finish it up when you have more time?” Respondent accepts: Go to 4 (verbal consent) and proceed with interview and schedule call back time if needed. Respondent declines: GO TO appropriate number callback 2a. 1st and 2nd call back. IMPLEMENT REFUSAL PREVENTION: “Before we set up an appointment, do you have any concerns or questions about being part of the study?” 2b. 2ai. If yes, address any issues and provide reassurance using info sheet with common respondent concerns and questions. Then, “Do you have any other concerns or questions.” 2aii. If no, make callback appointment. 3rd and 4th call back. Interviewer offers brief survey. “I know that for many people it is just so hard to find time for an interview. We have a very brief version that should only take 20 minutes and won’t need a call back. I can do that now if you would like.” 2bi. Respondent accepts. GO TO 4 (verbal consent) and then BRIEF SURVEY D-6 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients 2bii. Protocol 001 Amendment #3, December 2005 Respondent declines. IMPLEMENT REFUSAL PREVENTION STRATEGY: “Before we set up a call-back appointment, do you have any concerns or questions about being part of this study?” If YES, address any issues and provide reassurance using info sheet with common respondent concerns and questions. Then, “Do you have any other concerns or questions.” If NO, make callback appointment. 2c. 5th call back. Interviewer offers brief survey: “I know that for many people it is just so hard to find time for an interview. We have a very brief version that should only take 20 minutes and won’t need a call back. I can do that now if you like.” 2ci. Respondent accepts. GO TO 4 (verbal consent) and then BRIEF SURVEY 2cii. Respondent declines. GO TO SURROGATE if appropriate (if not appropriate GO TO 2ciii): “We know it can be hard to find the time and energy to participate in these interviews. It is just so very important that everyone’s experiences are part of this study. We really want to be sure that you are not left out. Some people prefer to have family member or friend do the interview instead. Is there someone who knows a lot about your recent colon/lung problem that we can talk to? 2ciia. Respondent elects surrogate. Get medical record consent (2civ) and then call surrogate to schedule. 2ciib. Respondent declines. GO TO 2ciii 2ciii. If CRN, OFFER CAPI “Would you be willing to meet with me to do the interview in person? I could meet you here at the research center, or at the clinic either before or after your next appointment, or I could come to where you are. Whatever is most convenient for you.” If respondent declines or NOT CRN, GO TO 2civ (medical record consent). If respondent accepts, say “Thank you.” Schedule appt as written below. PATIENT PREFERS RESEARCH CENTER: GIVE DIRECTIONS AND SET UP A DATE AND TIME. PATIENT PREFERS CLINIC: ASK WHEN HIS/HER NEXT APPT IS AND IF THEY PREFER TO MEET FOR AN HOUR BEFORE THE APPT OR STAY FOR AN HOUR AFTER THE APPT. PATIENT PREFERS RESIDENCE: CONFIRM ADDRESS AND SET UP CONVENIENT TIME FOR INTERVIEW. D-7 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients 2civ. Protocol 001 Amendment #3, December 2005 ASK FOR MEDICAL RECORD CONSENT ONLY: “I understand that you are not interested in participating in the interview. With your permission, we would like to review your medical record so we can compare the medical care people receive in your community to other parts of the country. We would like your permission to request copies of your records from doctors you have seen or for services that may have been paid for by Medicare. Your participation is completely voluntary. We will keep these records private and confidential to the full extent of the law. We will only receive copies of the necessary parts of these medical and Medicare records. Would you be willing to let us review your records related to the treatment of your lung or colorectal problem? IF RESPONDENT ACCEPTS MEDICAL RECORD OPTION: “Great, thank you. We will send you a medical and Medicare record release form, which will include instructions and a form to sign to give us permission to review your records. You should receive this in the next few days. If you have any questions you can call us at (TOLL FREE NUMBER). Thank you.” IF RESPONDENT DECLINES: KEEP DOOR OPEN FOR FUTURE REFUSAL CONVERSION. “Thank you for your time with me to today – I really appreciate it. Can we check back with you in the future to see how you are doing?” IF RESPONDENTS SAYS THAT SURROGATE WILL MAKE DECISION. “Does named surrogate have legal authority to sign for you.” If yes, ask for medical record consent during surrogate interview. If no, offer to send release form and instructions for the respondent to look at with the help of the surrogate. D-8 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients 3. Protocol 001 Amendment #3, December 2005 RESPONDENT WORRIED ABOUT TIME OR ENERGY TO PARTICIPATE Interviewer: “Your information is really important to the study. We could try getting started and then stop any time you want to and finish later. We would be happy to split up the interview over two or more call and do the calls any time that is good for you. 3a. Respondent agrees. GO TO 4 (Verbal consent). Proceed with interview and schedule call back time if needed. 3b. Respondent is still very hesitant due to time or energy interview will take, is unwilling for these or similar response burden reasons, or is VERY close to refusal1 Offer brief survey: “I know that for many people it is just so hard to find time for an interview. We have a very brief version that should only take 20 minutes and won’t need a call back. Can we go ahead with that now?” 3bi. Respondent agrees. Go to 4 (verbal consent) and then BRIEF SURVEY. 3bii. Respondent is still hesitant. Make call-back appointment (goal is not to lose this respondent or push them into an outright refusal). 3biii. Respondent is refusing or on verge or refusing due to response burden: Offer surrogate. “We know it can be hard to find the time and energy to participate in these interviews. It is just so very important that everyone’s experiences are part of this study. We really want to be sure that you are not left out. Some people prefer to have family member or friend do the interview instead. Is there someone who knows a lot about what has been going on for you that we can contact?” Respondent accepts: Get surrogate information and medical record consent (3c) and then call surrogate to schedule interview. Respondent declines: (CRN ONLY GO TO CAPI) “Would you be willing to meet with me to do the interview in person? I could meet you here at the research center, or at the clinic either before or after your next appointment, or I could come to where you are. Whatever is most convenient for you.” If CRN respondent declines CAPI or not CRN, GO TO 3c (medical record consent). If respondent accepts, say “Thank you.” Schedule appt as written below. PATIENT PREFERS RESEARCH CENTER: GIVE DIRECTIONS AND SET UP A DATE AND TIME. PATIENT PREFERS CLINIC: ASK WHEN HIS/HER NEXT APPT IS AND IF THEY PREFER TO MEET FOR AN HOUR BEFORE THE APPT OR STAY FOR AN HOUR AFTER THE APPT. ______________________________ 1 These cases should be monitored; listen to audiotapes and provide supportive feedback and guidance. D-9 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 PATIENT PREFERS RESIDENCE: CONFIRM ADDRESS AND SET UP CONVENIENT TIME FOR INTERVIEW. 3c. ASK FOR MEDICAL RECORD CONSENT ONLY: “I understand that you are not interested in participating in the interview. With your permission, we would like to review your medical record so we can compare the medical care people receive in your community to other parts of the country. We would like your permission to request copies of your records from doctors you have seen or for services that may have been paid for by Medicare. Your participation is completely voluntary. We will keep these records private and confidential to the full extent of the law. We will only receive copies of the necessary parts of these medical and Medicare records. Would you be willing to let us review your records related to the treatment of your lung or colorectal problem? 3ci. Respondent accepts: “Great, thank you. We will send you a medical and Medicare record release form, which will include instructions and a form to sign to give us permission to review your records. You should receive this in the next few days. If you have any questions you can call us at (TOLL FREE NUMBER). Thank you.” 3cii. Respondent declines: KEEP DOOR OPEN FOR FUTURE REFUSAL CONVERSION. “Thank you for your time with me to today – I really appreciate it. Can we check back with you in the future to see how you are doing?” 3ciii. Respondent says that surrogate will make decision. “Does named surrogate have legal authority to sign for you.” If yes, ask for medical record consent during surrogate interview. If no, offer to send release form and instructions for the respondent to look at with the help of the surrogate. D-10 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients 4. Protocol 001 Amendment #3, December 2005 VERBAL CONSENT “I will first ask you the interview questions and then ask your permission to review your medical records and insurance claims information. After the interview today, we will be sending you (insert incentive) to thank you for participating in this study. We would also like to call you again in about a year to learn more about your medical care experiences. During the interview today, we will be asking about doctors you have seen. It is possible that one or more of your doctors may be surveyed as part of the Share Thoughts on Care study; however, none of your responses will be shared with your doctors, and none of the information we collect will identify you or your doctor. All the information we collect will be kept totally confidential. Before we begin, there are a couple of important things I need to go over with you that were included in the information that we sent to you. Your participation in this interview is voluntary. If you decide not to participate, it will not affect you or your care in any way. This is a research interview so none of your responses will be used for treatment purposes. The risks of participation are minimal. Rarely, some persons may become upset when discussing their lung or colorectal problem. If that happens, you may skip that question or stop the interview. There are no personal benefits to participating in this study. Some people will get a sense of satisfaction from being able to think about and share their health care experiences. There will be no costs related to participation in the study. Your answers and personal information will be kept completely confidential to the full extent of the law. All study files will be kept in locked file cabinets. All electronic data for this study will be kept on secure computers that cannot be used by anyone except the study teams. When files are moved electronically from our research site to our central coordinating center, secure transmission methods will be used to protect the information. The information from this study will not be presented or published in any way that would allow the identification of any participant. Your answers will be combined with the answers of other people for statistical analysis. The investigators have obtained a Certificate of Confidentiality from the Department of Health and Human Services (DHHS). This Certificate means that the investigators cannot be forced to tell people who are not connected with this study about your participation without your written consent. You or a member of your family, however, may voluntarily release information about yourself or your involvement in this research. This telephone interview will last about one hour. You are free to stop this interview at any time. You are also free to decide to at any time to withdraw from this study, either during this interview, or before the follow-up survey, or before we obtain your medical records. Parts of the interview may be monitored by my supervisor for quality control purposes. Do you have any questions about the study?” (IF PARTICIPANT HAS QUESTIONS THAT YOU CANNOT ANSWER, MAKE A NOTE AND TELL THE PARTICIPANT THAT YOU WILL CALL THEM BACK.) “Do you agree to take part in the study and answer the interview questions?” IF NO: Go to 1. above. IF YES: “By answering the interview questions, you are consenting to the use of your answers in our research study. Thank you for your willingness to talk with me today about your experiences after your diagnosis. As we go along with the interview, please remember D-11 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 There are no right or wrong answers. Please try to answer questions as honestly and as accurately as you can. Take your time and If you are not sure what a question means or what kind of answer is wanted be sure to ask me If there is a question that you don’t want to answer, just tell me and I will skip it. May we begin?” Note: In some states, explicit permission to audiotape an interview must be given. If that applies, the following script should be used. IF YES & SUPERVISOR WANTS INTERVIEW TO BE RECORDED: “For quality control purposes, I would like to have your permission to tape record this interview. The tape will not be labeled with your name. Your tape may be randomly selected for review. If you do not wish to have this interview recorded, we still want to proceed with the interview. May I record?” IF YES: “Thank you.” (Turn on Tape Recorder) IF NO: “That is perfectly fine. This interview will not be recorded. Let’s begin.” (Do not turn on tape recorder) IF THE PATIENT STATES THEY HAVE A CANCER OTHER THAN LUNG OR COLORECTAL OR DENIES HAVING A LUNG OR COLORECTAL PROBLEM (questions 2.2, 2.4): “This study is only for patients with newly diagnosed lung or colorectal problems. Since you do not have either, I would like to stop the interview at this time. Thank you very much for your time and patience.” D-12 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 SCRIPT FOR MEDICAL RECORD REQUEST TO BE USED AFTER AN INTERVIEW WITH TARGET PATIENT IS COMPLETED: “We would also like to review your medical record so we can compare the medical care people receive in your community to other parts of the country. We would like your permission to request copies of your records from doctors you have seen or for services that may have been paid for by Medicare. Your participation is completely voluntary. We will keep these records private and confidential to the full extent of the law. We will only receive copies of the necessary parts of these medical and Medicare records. Would you be willing to let us review your records related to the treatment of your lung or colorectal problem? IF PATIENT AGREES TO MEDICAL RECORD OPTION: “Great, thank you. We will send you a medical and Medicare record release form, which will include instructions and a form to sign to give us permission to review your medical records. You should receive this in the next few days. If you have any questions you can call us at (TOLL FREE NUMBER). Thank you.” IF PATIENT DISAGREES: “Thank you for your participation in our study.” IF THE PATIENT IS UNSURE ABOUT PARTICIPATING: “Your participation in this interview is completely voluntary, and all of your responses will be confidential. Your participation in this study will not affect your health plan benefits or your relationship with your doctor. This is a research interview, so none of your responses will be used for treatment. There are no right or wrong answers. If there are any questions you do not want to answer, just say so. You are free to stop this interview at any time. You are also free to decide to at any time to withdraw from this study, either during this interview, or before the follow-up survey, or before we obtain your medical records. If you get too tired to continue, we can stop and schedule another time to finish. Do you agree to take part in the study and answer the interview questions?” IF YES: Go to consent above (4). IF NO: Go to refusal conversion strategy above (1). AFTER (X-To be determined before study begins) NUMBER OF ANSWERING MACHINE ATTEMPTS, AND GET MACHINE AGAIN: “Hello, my name is ___________, and I am calling from (Institution). I would like to speak to (Patient Name) about a health study called “Share Thoughts on Care”. Your participation is important. We recently mailed an informational packet to you describing this study. Could you please call our 24-hour message number at 800-XXX-XXXX or my direct number in (City) at XXX-XXX-XXXX? Please leave your name, phone number and a good day and time for us to reach you. Thank you.” IF PATIENT IS UNABLE TO UNDERSTAND OR SPEAK ENGLISH CLEARLY: “It seems as if we might have difficulty understanding each other. Do you speak another language?” IF “NO” OR NAMES A LANGUAGE OTHER THAN SPANISH OR CHINESE: “Thank you for your time. I am sorry to have bothered you.” D-13 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 IF SPANISH OR CHINESE: “Thank you. Have a nice INTERVIEWS/MAILINGS) day.” (PROCEED WITH STEPS FOR TRANSLATED PATIENT IS NOT HOME: “When would be a good time for me to call again?” WRONG NUMBER: “Is this (READ PHONE NUMBER BACK)? I’m sorry to have bothered you.” (PROCEED WITH STEPS FOR FINDING NEW NUMBER) PATIENT IS UNABLE TO COME TO THE TELEPHONE RIGHT NOW: “Is there a time when (Patient Name) would be available to talk with me?” (IF THERE IS A FAMILY GATEKEEPER WHO ASKS QUESTIONS, DO NOT REVEAL ANY INFORMATION REGARDING THE PATIENT’S MEDICAL CONDITION. YOU MAY TELL THEM THAT YOU ARE CALLING ABOUT A HEALTH STUDY CALLED SHARE THOUGHTS ON CARE AND THAT YOU RECENTLY SENT THE PATIENT INFORMATION ABOUT THE STUDY AND THAT YOU ARE CALLING TO SEE IF THE PATIENT IS WILLING TO PARTICIPATE IN THE STUDY.) PATIENT IS UNABLE TO COME TO THE PHONE BECAUSE OF ILLNESS OR COMMUNICATION DIFFICULTIES (other than language communication difficulties): “We recently sent a letter to (Name of Patient) about a study called Share Thoughts on Care. (Name of Patient) was identified as someone who qualifies for our study. We are calling today to see (if/when) (Name of Patient) might be able to participate in a telephone interview.” INTERVIEWER: INQUIRE AS TO WHEN THE TARGET PATIENT MAY BE ABLE TO BE INTERVIEWED. IF POSSIBLE, RESCHEDULE WITHIN 2 -4 WEEKS. IF THEY SEEM UNSURE ABOUT WHEN THE PATIENT MIGHT BE FEELING WELL ENOUGH, SUGGEST THAT YOU COULD CHECK BACK IN A FEW WEEKS AND SEE HOW HE/SHE IS DOING. (IDEALLY, WE WANT AS MANY PATIENT INTERVIEWS AS POSSIBLE). IF THIS PERSON DOES NOT EXPECT THE PATIENT TO BE ABLE TO PARTICIPATE IN THAT TIME FRAME, EXPLAIN THAT WE ALSO HAVE A SURVEY THAT MAY BE ANSWERED BY SOMEONE CLOSE TO THE PATIENT IF THE PATIENT GIVES US PERMISSION, AND ASK IF IT WOULD BE POSSIBLE TO GET THE PATIENT’S CONSENT TO DO A SURROGATE SURVEY. IF THE PATIENT IS ALIVE AND IS NOT ABLE TO CONSENT FOR A SURROGATE SURVEY, DO NOT ENROLL THE SURROGATE. FOR EXAMPLE, “If a patient is unable to participate, we are asking that someone who is familiar with the medical care that (he/she) has received complete a telephone interview for them. Would it be possible for (Name of Patient) to come to the phone now to give us permission to interview someone else on (his/her) behalf?” D-14 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 IF YES: “Thank you.” WHEN PATIENT COMES TO THE PHONE SAY “Hello, my name is ___________ and I am calling from (Name of Institution). I'm calling on behalf of the Share Thoughts on Care study, which is a study to learn more about the experiences of patients with newly diagnosed with lung or colorectal problems. You have been identified as someone who may qualify for our study. (Person who answered the phone) told me that this is not a good time for you to complete a telephone interview, but that you might be willing to give permission for me to interview someone else on your behalf about your recent medical care. Who knows the most about your medical care and how you have been doing since your diagnosis?" (GET SURROGATE CONTACT INFORMATION & SCHEDULE INTERVIEW WITH SURROGATE IF NOT DONE IMMEDIATELY. MAIL INFORMATION IF NECESSARY. IF AFTER HEARING ABOUT THE STUDY, THE PATIENT WISHES TO PARTICIPATE THEMSELVES, GO TO 4). THANK THEM AND THEN ASK FOR MEDICAL RECORD CONSENT “We would also like to review your medical record so we can compare the medical care people receive in your community to other parts of the country. We would like your permission to request copies of your records from doctors you have seen or for services that may have been paid for by Medicare. Your participation is completely voluntary. We will keep these records private and confidential to the full extent of the law. We will only receive copies of the necessary parts of these medical and Medicare records. Would you be willing to let us review your records related to the treatment of your lung or colorectal problem?” IF PATIENT AGREES TO MEDICAL RECORD OPTION: “Great, thank you. We will send you a medical and Medicare record release form, which will include instructions and a form to sign to give us permission to review your records. You should receive this in the next few days. If you have any questions you can call us at (TOLL FREE NUMBER). Thank you.” IF PATIENT DISAGREES: “Thank you for listening. Take care.” IF PATIENT SAYS THAT SURROGATE WILL MAKE DECISION. “Does named surrogate have legal authority to sign for you.” If yes, ask for medical record consent during surrogate interview. If no, offer to send release form and instructions for the respondent to look at with the help of the surrogate. IF NO: “Would it be okay if I called back in a week or two to see if (Name of Patient) is feeling better then?” IF INDICATES A CALL BACK PREFERENCE, THANK THEM AND RESCHEDULE CONTACT. IF STATES THAT THEY DO NOT WANT YOU TO CALL BACK, “I understand your feelings and I do not want to cause undue burden or inconvenience for you and your family. D-15 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 Thank you for your time.” IF THEY SEEM RECEPTIVE TO THE STUDY ASK FOR PERMISSION TO SEND MEDICAL RECORD CONSENT TO THE PATIENT: “We would also like to review (Name of Patient’s) medical record so we can compare the medical care people receive in your community to other parts of the country. We would like (Name of Patient’s) permission to request copies of (his/her) records from doctors (he/she) has seen and any records of services paid for by Medicare. (His/her) participation is completely voluntary. We will keep these records private and confidential to the full extent of the law. We will only receive copies of the necessary parts of these medical and Medicare records.” “Is (Name of Patient) able to sign a form releasing (his/her) medical records?” IF NOT: “Do you have legal authority to sign on (his/her) behalf?” IF NOT: “Whom should I contact to get permission for this?” (INTERVIEWER SHOULD TAKE APPROPRIATE STEPS TO ENSURE MEDICAL RECORD CONSENT IS TO APPROPRIATE PERSON). PATIENT IS IN NURSING HOME: “We recently sent a letter to (Name of Patient) about a study called “Share Thoughts on Care”. (Name of Patient) was identified as someone who qualifies for our study. Would it be possible for me to call (Name of Patient) at the nursing facility?” IF YES: “Could you tell me the address and phone number where (he/she) can be reached?” (RECORD ADDRESS AND ENTER INTO CATI. SEND STUDY INFORMATION AND RESCHEDULE CONTACT WITH TARGET PATIENT.) IF NO: “If a patient is unable to participate, we are asking that someone who is familiar with the medical care that (he/she) has received complete a telephone interview for them. Is (Name of Patient) well enough to give us permission to let someone else answer the questions for (him/her)?” IF NO: “Thank you for your time.” IF YES: “What is the best way for me to get (his/her) permission?” (PROCEED WITH STEPS TO GET PATIENT’S PERMISSION FOR SURROGATE INTERVIEW AND/OR MEDICAL RECORD RELEASE.) PATIENT IN NURSING HOME BUT PERSON EXPECTS PATIENT WILL BE HOME WITHIN A WEEK OR TWO. INTERVIEWER: ASK IF THE PATIENT IS ABLE TO COMPLETE A TELEPHONE INTERVIEW WHILE IN THE NURSING HOME. IF YES, CATI WILL BRING UP CONTACT INFORMATION QUESTIONS AND PROMPT TO SEND A NEW LETTER TO THE NURSING HOME. IF NOT, SCHEDULE A CALL BACK IN A FEW WEEKS TO SEE IF THE PATIENT HAS RETURNED HOME. PATIENT IS NEAR DEATH: INTERVIEWER: WE DO NOT WANT TO TRY TO RECRUIT IF THE PERSON WHO ANSWERS THE TELEPHONE STATES THAT THE PATIENT IS NEAR DEATH. IN THIS SITUATION, TELL THEM THAT YOU ARE SORRY TO HEAR THAT THE PATIENT IS NOT DOING WELL AND THANK D-16 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 THEM FOR THEIR TIME. INTERVIEWER SHOULD PASS THIS INFORMATION ALONG TO THE STUDY RECRUITMENT TEAM TO KEEP IN CLOSE CONTACT WITH THE PATIENT’S PHYSICAN TO ASSESS THE PATIENT’S VITAL STATUS. IF APPROPRIATE, THIS CASE SHOULD BE SWITCHED OVER TO AN AFTER DEATH SURROGATE CASE. PATIENT IS DECEASED: INTERVIEWER: IN THIS SCENARIO, THE GOAL IS TO IDENTIFY AN APPROPRIATE SURROGATE, ASSESS THE BEREAVEMENT WINDOW (MUST BE AT LEAST ONE MONTH SINCE DEATH), AND SCHEDULE AN INTERVIEW USING THE AFTER DEATH SURROGATE SURVEY. “Please accept our deepest sympathy over the loss of (Name of patient). We recently sent a letter to (Name of patient) about a study that we are conducting to learn more about the experiences of patients diagnosed with lung or colorectal problems. (Name of patient) was identified by (his/her) doctor as someone who qualified for our study.” “May I ask when (PATIENT) died?” (DOCUMENT DATE OF DEATH) “Who am I speaking with?” IF NEEDED, “Can you tell me how you are related to (Name of patient)?” “Because it is important to gather information on everyone who is eligible, we are also interviewing next of kin for those patients who are recently deceased. We are asking that someone who was familiar with how the patient was doing since the diagnosis with lung or colorectal problems to complete a telephone interview on their behalf. Are you the person who knows the most about the medical care and how (Name of patient or relationship) was doing during (his/her) illness?” IF NO: “Is there someone else that we should speak with?” GET CONTACT INFORMATION ON AN ALTERNATE SURROGATE. OFFER TO SEND STUDY MATERIALS IN THE MAIL TO THIS POTENTIAL PARTICIPANT. CONFIRM CONTACT INFORMATION FOR THIS MAILING. IF YES: “May I tell you more about this study? Is this a good time for us to talk?” IF THE SURROGATE STATES THAT IT IS TOO SOON TO TALK, ASK IF YOU CAN SEND STUDY INFORMATION IN THE MAIL AND SCHEDULE A TIME TO TALK. IF APPROPRIATE, BEGIN CONSENT PROCESS WITH AFTER-DEATH INSTRUMENT: “I would first like to ask you the interview questions and then ask your permission to review (Name of Patient’s) medical records and insurance claims information. After the interview today, we will be sending you (insert incentive) to thank you for participating in this study. During the interview today, we will be asking about doctors (Name of Patient) may have seen. It is possible that one or more of (his/her) doctors may be surveyed as part of the Share Thoughts on Care study; however, none of your responses will be shared with any of (Name of Patient’s) doctors, and none of the information we collect will identify (him/her) or (his/her) doctor. All the information we collect will be kept totally confidential. Before we begin, there are a couple of important things I need to go over with you that were included in the information that we sent. Your participation in this interview is voluntary. If you decide not to participate, it will not affect you in any way. This is a research interview so none of your responses will be used D-17 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 for treatment purposes. The risks of participation are minimal. There may be psychological or emotional stress in that discussion of (Name of Patient’s) lung or colorectal problems may cause feelings of sorrow or grief. There may be no personal benefit to participating in this study. There will be no costs related to participation in the study. Your answers and any personal information collected will be kept completely confidential to the full extent of the law. All study files will be kept in locked file cabinets. All electronic data for this study will be kept on secure computers that cannot be used by anyone except the study teams. When files are moved electronically from our research site to our central coordinating center, secure transmission methods will be used to protect the information. The information from this study will not be presented or published in any way that would allow the identification of any participant. Your answers will be combined with the answers of other people for statistical analysis. The investigators have obtained a Certificate of Confidentiality from the Department of Health and Human Services (DHHS). This Certificate means that the investigators cannot be forced to tell people who are not connected with this study about your participation without your written consent. This telephone interview will last about one hour. You are free to stop this interview at any time. Parts of the interview may be monitored by my supervisor for quality control purposes. Do you have any questions about the study?” (ANSWER ANY QUESTIONS. IF SURROGATE HAS QUESTIONS THAT YOU CANNOT ANSWER, MAKE A NOTE AND TELL THEM THAT YOU WILL CALL THEM BACK.) “By answering the interview questions, you are consenting to the use of your answers in our research study. Thank you for your willingness to talk with me today about (Name of Patient’s) experiences. As we go along with the interview, please remember There are no right or wrong answers. Please try to answer questions as honestly and as accurately as you can. Take your time and If you are not sure what a question means or what kind of answer is wanted be sure to ask me If there is a question that you don’t want to answer, just tell me and I will skip it. May we begin?” CONTINUE WITH INTERVIEW IF SURROGATE STATES THE PATIENT HAD A CANCER OTHER THAN LUNG OR COLORECTAL OR DENIES PATIENT HAD A LUNG OR COLORECTAL PROBLEM (questions 2.3, 2.4): “This study is only for patients with newly diagnosed lung or colorectal problems. Since (Name of Patient) did not have either, I would like to stop the interview at this time. Thank you very much for your time and patience.” SCRIPT FOR MEDICAL RECORD REQUEST TO BE USED AFTER AN AFTER-DEATH SURROGATE INTERVIEW IS COMPLETED: D-18 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 “Thank you for answering all of those questions. We would also like to review (Name of Patient’s) medical record so we can compare the medical care people receive in your community to other parts of the country. We will keep these records private and confidential to the full extent of the law. We will only receive copies of the necessary parts of these medical and Medicare records.” Do you have legal authority to sign on (his/her) behalf? IF NOT: Whom should I contact to get permission for this? (INTERVIEWER SHOULD TAKE APPROPRIATE STEPS TO ENSURE MEDICAL RECORD CONSENT IS TO APPROPRIATE PERSON) IF YES: Would you be willing to let us review (Name of Patient’s) records related to the treatment of (his/her) lung or colorectal problem?” IF SURROGATE AGREES TO MEDICAL RECORD OPTION: “Great, thank you. We will send you a medical and Medicare record release form, which will include instructions and a form to sign to give us permission to review (Name of Patient’s) records. You should receive this in the next few days. If you have any questions you can call us at (TOLL FREE NUMBER). Thank you.” IF SURROGATE DISAGREES: “Thank you for your participation in our study.” D-19 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 SURROGATE SCRIPT The following scripts have been approved by the CanCORS membership; however, changes may be made, if required by your IRB. Please note the text in red cannot be modified. THE FOLLOWING SCRIPT SHOULD BE USED WHEN YOU CALL TO SPECIFICALLY TALK TO THE SURROGATE WHO HAS ALREADY BEEN IDENTIFIED BY THE PATIENT (PATIENT HAS GIVEN CONSENT FOR THIS SURROGATE INTERVIEW). “Hello, my name is ________________, and I am calling from (Name of Institution). May I please speak with (Surrogate Name)?” WHEN SURROGATE IS ON THE PHONE: “I’m calling on behalf of a study called Share Thought on Care. (Name of Patient) was identified by (his/her) doctor as someone who qualifies for our study, which is a study to learn more about the experiences of patients with newly diagnosed lung or colorectal diseases. (Name of Patient) has told us that (he/she) is unable to be interviewed for this study but would like you to participate on (his/her) behalf because you can speak about (his/her) recent medical experiences. The interview will take about one hour. Is this a good time for us to talk?” IF NOT A GOOD TIME: RESCHEDULE WITHIN ONE WEEK. OFFER TO SEND ANOTHER STUDY INFORMATION PACKET IN THE MAIL. CONFIRM CONTACT INFORMATION (e.g., Is there another telephone number where you can be reached?) IF NO, DO NOT WANT TO PARTICIPATE: “Can you tell me why you do not want to take part in this study?” IF SURROGATE SAYS THAT HE/SHE MAY NOT BE THE BEST PERSON TO ANSWER THESE QUESTIONS FOR THE PATIENT, A) THANK THE PARTICIPANT AND GO ON TO THE NEXT SURROGATE LISTED IF THERE IS ONE OR B) IF NO OTHER SURROGATE IS LISTED, TELL SURROGATE THAT HE/SHE IS THE ONLY PERSON IDENTIFIED BY THE PATIENT AND WE ARE NOT ABLE TO CONTACT ANYONE ELSE WITHOUT THE PATIENT’S PERMISSION. C) IF THE SURROGATE WANTS TO CHECK WITH THE PATIENT BEFORE CONSENTING, THEN SCHEDULE AN APPOINTMENT FOR THE INTERVIEW. IF SURROGATE STATES THAT HE/SHE IS JUST NOT INTERESTED PARTICIPATING THEN TERMINATE THE INTERVIEW (Thank you for your time). IF YES: Thank you. Your participation in this study is very important. (BEGIN CONSENT PROCESS & INTERVIEW) D-20 IN “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 IF PATIENT ALREADY MADE DECISION ABOUT MEDICAL RECORDS RELEASE “I will ask you the interview questions and the after the interview today, we will be sending you (insert incentive) to thank you for participating in this study.” IF PATIENT SAID THAT SURROGATE WOULD MAKE DECISION ABOUT MEDICAL RECORD “I would first like to ask you the interview questions and then ask permission to review (Name of Patient’s) medical records and insurance claims information. After the interview today, we will be sending you (insert incentive) to thank you for participating in this study. REMAINDER OF CONSENT PROCESS (EVERYBODY) “During the interview today, we will be asking about doctors (Name of Patient) may have. It is possible that one or more of (his/her) doctors may be surveyed as part of the Share Thoughts on Care study; however, none of your responses will be shared with any of (Name of Patient’s) doctors, and none of the information we collect will identify (him/her) or (his/her) doctor. All the information we collect will be kept totally confidential. Before we begin, there are a couple of important things I need to go over with you that were included in the information that we sent to (Name of Patient). Your participation in this interview is voluntary. If you decide not to participate, it will not affect you or (Name of Patient) in any way. This is a research interview so none of your responses will be used for treatment purposes. The risks of participation are minimal. There may be psychological or emotional stress in that discussion of (Name of Patient’s) lung or colorectal problems may cause feelings of sorrow or grief. There may be no personal benefit to participating in this study. There will be no costs related to participation in the study. Your answers and any personal information collected will be kept completely confidential to the full extent of the law. All study files will be kept in locked file cabinets. All electronic data for this study will be kept on secure computers that cannot be used by anyone except the study teams. When files are moved electronically from our research site to our central coordinating center, secure transmission methods will be used to protect the information. The information from this study will not be presented or published in any way that would allow the identification of any participant. Your answers will be combined with the answers of other people for statistical analysis. The investigators have obtained a Certificate of Confidentiality from the Department of Health and Human Services (DHHS). This Certificate means that the investigators cannot be forced to tell people who are not connected with this study about your participation without your written consent. This telephone interview will last about one hour. You are free to stop this interview at any time. Parts of the interview may be monitored by my supervisor for quality control purposes. Do you have any questions about the study?” (ANSWER ANY QUESTIONS. IF SURROGATE HAS QUESTIONS THAT YOU CANNOT ANSWER, MAKE A NOTE AND TELL THE PARTICIPANT THAT YOU WILL CALL THEM BACK.) D-21 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 “By answering the interview questions, you are consenting to the use of your answers in our research study. Thank you for your willingness to talk with me today about (Name of Patient’s) experiences. As we go along with the interview, please remember There are no right or wrong answers. Please try to answer questions as honestly and as accurately as you can. Take your time and If you are not sure what a question means or what kind of answer is wanted be sure to ask me If there is a question that you don’t want to answer, just tell me and I will skip it. Note: In some states, explicit permission to audiotape an interview must be given. If that applies, the following script should be used. IF YES & SUPERVISOR WANTS INTERVIEW TO BE RECORDED: “For quality control purposes, I would like to have your permission to tape record this interview. The tape will not be labeled with your name. Your tape may be randomly selected for review. If you do not wish to have this interview recorded, we still want to proceed with the interview. May I record?” IF YES: “Thank you.” (Turn on Tape Recorder) IF NO: “That is perfectly fine. This interview will not be recorded. Let’s begin.” (Do not turn on tape recorder) May we begin?” CONTINUE WITH INTERVIEW. IF SURROGATE STATES THE PATIENT HAS A CANCER OTHER THAN LUNG OR COLORECTAL OR DENIES PATIENT HAS A LUNG OR COLORECTAL PROBLEM (questions 2.3, 2.4): “This study is only for patients with newly diagnosed lung or colorectal problems. Since (name of patient) does not have either, I would like to stop the interview at this time. Thank you very much for your time and patience.” IF PATIENT SAID THAT SURROGATE WOULD MAKE DECISION ABOUT MEDICAL RECORD RELEASE “Thank you for answering all those questions. “We would also like to review (Name of Patient’s) medical record so we can compare the medical care people receive in your community to other parts of the country. We would like permission to request copies of (Name of Patient’s) records from doctors (he/she) has seen and any records of services paid for by Medicare. Participation in this way is completely voluntary. We will keep these records private and confidential to the full extent of the law. (Name of Patient) asked that you make the decision about signing a form releasing (his/her) records? Do you have legal authority to sign on (his/her) behalf? IF NOT: Whom should I contact to get permission for this? (INTERVIEWER SHOULD D-22 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 TAKE APPROPRIATE STEPS TO ENSURE MEDICAL RECORD CONSENT IS TO APPROPRIATE PERSON) IF YES: Would you be willing to let us review (Name of Patient’s) records related to the treatment of your lung or colorectal problem?” IF YES: “Great, thank you. We will send you a medical and Medicare record release form, which will include instructions and a form to sign to give us permission to review his/her records. You should receive this in the next few days. If you have any questions you can call us at (TOLL FREE NUMBER). Thank you.” IF NO: “Okay. Thank you for your participation in our study.” IF PATIENT PREVIOUSLY AGREED TO RELEASE MEDICAL RECORDS “(Name of Patient) gave us permission to review his/her medical records and insurance claims. We have sent him/her a medical records release form that needs to be signed. If you or (name of patient) have any questions you can call us at (TOLL FREE NUMBER). Thank you.” D-23 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 SCRIPT FOR DISTRESSED PATIENTS OR SURROGATES IF, AT ANY TIME THE INTERVIEWER FEELS THAT THE TONE OF THE CONVERSATION IS TENSE, IT MAY BE USEFUL TO SAY ANY OF THE FOLLOWING: “I get the sense that these questions are bringing up feelings that are upsetting you.” “I know that it's hard to talk about these things but it is very helpful for us to learn what kind of experiences people have.” “Would you like to take a break and have me call you back in a few minutes or another day?” “I can hear that this is a difficult topic for you. Thanks for sharing your experiences.” “I know these times can be hard.” IF PATIENT SAYS THEY ARE UPSET, INDICATE TO THE PATIENT THAT YOU EMPATHIZE WITH THEM. ASK THE PATIENT IF HE/SHE WISHES TO CONTINUE WITH THE SURVEY. DO NOT PRESS THE PARTICIPANT TO CONTINUE. “It’s certainly natural to feel this way. This must be a very difficult time for you and your family. We want to do what is best for you. If you don’t feel comfortable continuing the interview we can stop right now.” IF THE PARTICIPANT WISHES TO STOP THE INTERVIEW, THANK THEM FOR THEIR TIME AND ASK IF HE/SHE WOULD LIKE THE PHONE NUMBER OF THE PI OR A TRAINED CLINICIAN OR SOCIAL WORKER OR CRISIS HOTLINE. TO FOLLOW UP AFTER USING ONE OF THE ABOVE COMMENTS, IT WOULD BE APPROPRIATE AT THE COMPLETION OF THE SURVEY FOR THE INTERVIEWER TO SAY: “During our interview I sensed that you might be having a difficult time. Have you discussed this with your doctor?” a. IF HE/SHE SAYS YES THEN RESPOND, “I’m glad to hear that.” b. IF HE/SHE SAYS YES, BUT…(AS IF THEY FEEL THEY NEED MORE HELP) OR IF THEY SAY NO, THEN RESPOND “Would you like the phone number of someone who can help you find someone to talk about your feelings with?” INTERVIEWER: IF YOUR SITE HAS SPECIFIC NAMES AND/OR PHONE NUMBERS TO GIVE TO PATIENTS YOU MAY OFFER THOSE TO PATIENTS (e.g. physician, social worker, cancer counselor, etc.). IF NOT, YOU CAN SUGGEST THEY ASK THEIR NURSE OR DOCTOR FOR THE NAME OF A SOCIAL WORKER OR CLERGY MEMBER. YOU MAY ALSO WISH TO GIVE OUT THE NUMBER OF THE LOCAL AMERICAN CANCER SOCIETY (THEY HAVE INFORMATION ABOUT LOCAL SUPPORT GROUPS). IF A PARTICIPANT BECOMES EXTREMEMLY UPSET, STOP THE INTERVIEW AND FOCUS ON THE PARTICIPANT’S EMOTIONAL STATE. IF THE PATIENT IS SUFFICIENTLY DISTRESSED, DEPRESSED, OR EMOTIONALLY DISTURBED, OR IF DURING THE COURSE OF THE TELEPHONE SURVEY CONTACT, THE INTERVIEWER ENCOUNTERS A LIFE-THREATENING D-24 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 SITUATION THEN HE/SHE WILL USE THE FOLLOWING PROTOCOL TO RESPOND TO THE SITUATION AND TO ALERT THE APPROPRIATE PERSONNEL. A LIFE-THREATENING SITUATION IS DEFINED AS THE OCCURRENCE OF ANY OF THE FOLLOWING SITUATIONS: He or she is “thinking of suicide.” He or she feels “like I want to kill myself.” He or she wants to “kill himself/herself” or “hurt himself/herself.” He or she “wishes I were dead.” He or she “wishes my life were over.” He or she uses the words “I feel I can’t go on” or “I can’t go on.” He or she expresses thoughts about harming himself/herself. THIS PROTOCOL SHOULD BE FOLLOWED WHETHER OR NOT THE LIFE-THREATENING SITUATION IS TRIGGERED BY SOMETHING DISCUSSED IN THE SURVEY INTERVIEW. IF THE RESPONDENT APPEARS TO BE IN IMMEDIATE DANGER AS DEFINED BY USING THE WORDS NOTED ABOVE, THE INTERVIEWER SHOULD STAY CALM IN TALKING WITH THE CANCER PATIENT AND USE THE FOLLOWING SCRIPT: “You seem to be having a difficult time. Would you like me to have one of our study physicians give you a call? Our study physician is a doctor who is familiar with the kinds of feelings you are having.” INTERVIEWER: PLEASE FOLLOW YOUR SITE-SPECIFIC PROTOCOLS FOR DEALING WITH DISTRESSED PATIENTS. D-25 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Appendix E: Brief Patient Survey E-1 Protocol 001 Amendment #3, December 2005 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 Appendix F: Surrogate Respondent Surveys F-1 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 Appendix G: Follow-Up Interview Scripts and Surveys G-1 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 Interviewer Notes: After each phone contact, a disposition code will be generated. This will serve several purposes including making sure that appropriate call backs are generated, assessing patient and surrogate status, assessing quality, and describing the sample. If the person states that they have cancer, you should automatically switch to using the word cancer instead of “problem or disease” to make the participant feel more comfortable. The following scripts have been approved by the CanCORS membership; however, changes may be made, if required by your IRB. Please note the text in red cannot be modified. PATIENT OR INTENDED SURROGATE SCRIPTS WHEN A PERSON ANSWERS THE PHONE: “Hello, my name is ___________ and I am calling from The University of Iowa. May I please speak to (Name of Patient/Surrogate)?” SOMEONE BESIDES PATIENT OR INTENDED SURROGATE ANSWERS THE PHONE, BUT PATIENT OR INTENDED SURROGATE THEN COMES TO THE PHONE: “Hello, my name is ___________ and I am calling from _____________[PDCR site name]. I’m calling on behalf of the Share Thoughts on Care study. Several months ago [PATIENT NAME/you] participated in an interview for our study and now it is time for the follow up interview. Did you receive the information we recently mailed to you?” PATIENT OR INTENDED SURROGATE ANSWERS THE PHONE: I’m calling on behalf of the Share Thoughts on Care study. Several months ago [PATIENT NAME/you] participated in an interview for our study and now it is time for the follow up interview. Did you receive the information we recently mailed to you?” IF PATIENT OR INTENDED SURROGATE INDICATES THAT THEY DID RECEIVE THE MAILING: “Do you have any questions?” (Answer any questions then ask about interview). “Is this a convenient time to do an interview?” IF NO: GO TO 1. (refusal conversion strategy) IF PATIENT OR INTENDED SURROGATEINDICATES NOT A GOOD TIME, ASKS YOU TO CALL BACK, OR SIMILAR RESPONSE: GO TO 2. (call back procedure) IF PATIENT OR INTENDED SURROGATE IS HESITANT TO PARTICIPATE IN INTERVIEW – NOT EXACTLY REFUSING OR SAYING IT IS A BAD TIME: GO TO 3. IF YES: GO TO 5 (Interview Introduction). G-2 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 IF PATIENT OR INTENDED SURROGATE INDICATES THAT THEY DID NOT RECEIVE THE MAILING: “I would be happy to mail you the information again if you like. Since I have you on the phone right now, may I take a few moments of your time to tell you about the follow up interview?” IF YES: “Several months ago [PATIENT NAME/you] participated in an interview for our study called Share Thoughts on Care. The purpose of the study is to learn how people are treated for their cancer, what factors influence their choice of treatment, and about their experiences with cancer. The National Cancer Institute is funding this research study. When we spoke with [PATIENT NAME/you] last we said we would call again in a few months to follow up on any changes that may have taken place. It is now time for us to call. The interview usually takes about 30 minutes. [IF PATIENT IS DECEASED: Because it is important to gather information on everyone in the study, we are also contacting next of kin for those patients who are recently deceased. We are asking that someone who was close to the patient – someone who was familiar with how the patient was doing since their diagnosis with ________ cancer – complete a telephone interview.] Would you be willing to participate in this interview today?” (Move to appropriate number based on answer.) IF NO: GO TO 1. (refusal conversion strategy) IF PATIENT INDICATES NOT A GOOD TIME, ASKS YOU TO CALL BACK, OR SIMILAR RESPONSE: GO TO 2. (call back procedure) IF PATIENT INDICATES WORRY ABOUT HAVING ENERGY OR TIME TO PARTICIPATE IN INTERVIEW – NOT EXACTLY REFUSING OR SAYING IT IS A BAD TIME: GO TO 3. IF YES: GO TO 4. (verbal consent) IF PATIENT OR INTENDED SURROGATE WANTS INFORMATION MAILED AGAIN: “Let me confirm your mailing address. The address we have is (Read participant address). Is that correct?” IF YES: “Great. I’ll send the information to you and try to call back in about a week. Is there a day or time that works better for you? (Try to find out good time for callback) Thank you.” IF NO: G-3 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 “What is the correct mailing address? (Record Address.) Thank you. I’ll send the information to you and try to call back in about a week. Is there a day or time that works better for you? (Try to find out good time for callback) Have a nice day.” 1. REFUSAL CONVERSION STRATEGY 1a. “Lots of people aren’t very comfortable when they are called on the phone about studies. What kinds of concerns or worries do you have about being in this study?” (Avoid argumentative tone, use soothing, accepting understanding tone) 1ai. Respondent expresses one or more concerns, worry or questions Interviewer responds by answering questions/ provides reassurance using info sheet with common R concerns, questions and responses. Next steps depends on specific concerns but in general GO TO 1b 1aii. 1b. Interviewer: “The National Institutes of Health asked well-respected researchers to conduct this study because they really want to understand the experiences of people like you. Each person is unique and so your information is really important to the study and I’d hate to see it left out. We could try getting started and then stop any time you want to and finish later. We would be happy to split up the interview over two or more calls at any time that is good for you.” 1bi. Respondent agrees. If the respondent agrees to start now, but has not received the letter, GO TO 4 (verbal consent) if the respondent agrees to start now and has received the letter or GO TO 5 (interview introduction) otherwise schedule callback. 1bii. 2. Respondent does not state specific worry or question. GO TO 1b Respondent declines. KEEP DOOR OPEN FOR FUTURE REFUSAL CONVERSION. “Thank you for your time with me today – I really appreciate it. Can we check back with you in the future to see how you are doing?” CALL BACK PROCEDURE Make call-back appointment and (ideally): Send respondent postcard with call-back appointment, reiteration of the importance of study and value of their participation. SCRIPT FOR INITIAL CONTACT DURING CALLBACK WHEN A PERSON ANSWERS THE PHONE: “Hello, my name is ___________ and I am calling from The University of Iowa. May I please speak to (Name of Patient/Surrogate)?” SOMEONE BESIDES PATIENT OR INTENDED SURROGATE ANSWERS THE PHONE, BUT PATIENT OR INTENDED SURROGATE THEN COMES TO THE PHONE: G-4 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 “Hello, my name is ___________ and I am calling from ________________________ [PDCR site name]. I’m calling on behalf of the Share Thoughts on Care study in which (Name of Patient / you) have previously participated. We spoke on (state date of last conversation) and you seemed interested in participating in a follow-up interview. You suggested I call back at this time. Is this a good time to start the interview? PATIENT OR INTENDED SURROGATE ANSWERS THE PHONE: I’m calling on behalf of the Share Thoughts on Care study in which (Name of Patient / you) have previously participated. We spoke on (state date of last conversation) and you seemed interested in participating in a follow-up interview. You suggested I call back at this time. Is this a good time to start the interview? Respondent agrees. Go to 4 (verbal consent). Respondent indicates not a good time, asks you to call back. “Your information is really important to the study. Is it possible to do a bit of it now and finish it up when you have more time?” Respondent accepts: Go to 4 (verbal consent) and proceed with interview and schedule call back time if needed. Respondent declines: IMPLEMENT REFUSAL PREVENTION: “Before we set up an appointment, do you have any concerns or questions about being part of the study?” 3. 2ai. If yes, address any issues and provide reassurance using info sheet with common respondent concerns and questions. Then, “Do you have any other concerns or questions.” 2aii. If no, make callback appointment. RESPONDENT WORRIED ABOUT TIME OR ENERGY TO PARTICIPATE Interviewer: “Your information is really important to the study. We could try getting started and then stop any time you want to and finish later. We would be happy to split up the interview over two or more call and do the calls any time that is good for you. 3a. Respondent agrees. GO TO 4 (Verbal consent). Proceed with interview and schedule call back time if needed. 3b. Respondent is still hesitant. “All of your responses would be confidential. Your participation in this study will not affect your health plan benefits or your relationship with your doctor. This is a research interview, so none of your responses will be used for treatment. There are no right or wrong answers. If there are any questions you do not want to answer, you can just say so. You are free to stop this interview at any time. If you get too tired to continue, we can stop and schedule another time to finish. G-5 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 Do you agree to take part in the study and answer the interview questions?” IF YES: Go to 4. (verbal consent) IF NO: Make call-back appointment (goal is not to lose this respondent or push them into an outright refusal). 3c. Respondent declines: KEEP DOOR OPEN FOR FUTURE REFUSAL CONVERSION. “Thank you for your time with me to today – I really appreciate it. Can we check back with you in the future to see how you are doing?” 4. VERBAL CONSENT: “ I will first ask you the interview questions. After the interview today, we will be sending you (insert incentive) to thank you for participating in this study. Before we begin, there are a couple of important things I need to go over with you that were included in the information that we sent to you. Taking part in the interview is completely voluntary. You may choose not to take part at all. If you decide to participate in the interview, you may stop at any time. If you decide not to participate, you won’t be penalized or lose any benefits for which you otherwise qualify. Your answers will be kept strictly confidential and will not be shared with [PATIENT NAME’s] doctor or other health care providers. Records of participation in this research project will be kept confidential to the full extent permitted by law. The investigators have obtained a Certificate of Confidentiality from the Department of Health and Human Services. This Certificate means that the investigators cannot be forced (for example by court subpoena) to tell people who are not connected with this study about your participation without your written consent. However, you may voluntarily release information about yourself or your involvement in this research.” 5.Interview Introduction “Parts of the interview may be monitored by my supervisor for quality control purposes. Do you have any questions about the study?” (IF PARTICIPANT HAS QUESTIONS THAT YOU CANNOT ANSWER, MAKE A NOTE AND TELL THE PARTICIPANT THAT YOU WILL CALL THEM BACK.) “Do you agree to take part in the study and answer the interview questions?” IF NO: Go to 1 above. IF YES: “By answering the following questions, you are consenting to the use of your answers in our research study. Thank you for your willingness to talk with me today about your experiences after your diagnosis. As we go along with the interview, please remember There are no right or wrong answers. Please try to answer questions as honestly and as accurately as you can. Take your time and G-6 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 If you are not sure what a question means or what kind of answer is wanted be sure to ask me If there is a question that you don’t want to answer, just tell me and I will skip it. Note: In some states, explicit permission to audiotape an interview must be given. If that applies, the following script should be used. IF YES & SUPERVISOR WANTS INTERVIEW TO BE RECORDED: “For quality control purposes, I would like to have your permission to tape record this interview. The tape will not be labeled with your name. Your tape may be randomly selected for review. If you do not wish to have this interview recorded, we still want to proceed with the interview. May I record?” IF YES: “Thank you.” (Turn on Tape Recorder) IF NO: “That is perfectly fine. This interview will not be recorded. Let’s begin.” (Do not turn on tape recorder) AFTER (X-To be determined before study begins) NUMBER OF ANSWERING MACHINE ATTEMPTS, AND GET MACHINE AGAIN: “Hello, my name is ___________, and I am calling from (Institution). I would like to speak to (Patient Name) about the “Share Thoughts on Care” study. Your participation is important. We recently mailed an informational packet to you. Could you please call our 24-hour message number at 800-XXX-XXXX or my direct number in (City) at XXX-XXX-XXXX? Please leave your name, phone number and a good day and time for us to reach you. Thank you.” IF PATIENT IS UNABLE TO UNDERSTAND OR SPEAK ENGLISH CLEARLY: “It seems as if we might have difficulty understanding each other. language?” Do you speak another IF “NO” OR A NAMES A LANGUAGE OTHER THAN SPANISH OR CHINESE: “Thank you for your time. I am sorry to have bothered you.” IF SPANISH OR CHINESE: “Thank you. Have a nice INTERVIEWS/MAILINGS) day.” (PROCEED WITH STEPS FOR TRANSLATED PATIENT OR INTENDED SURROGATE IS NOT HOME: “When would be a good time for me to call again?” WRONG NUMBER: “Is this (READ PHONE NUMBER BACK)? I’m sorry to have bothered you.” (PROCEED WITH STEPS FOR FINDING NEW NUMBER) G-7 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 PATIENT OR INTENDED SURROGATE IS UNABLE TO COME TO THE TELEPHONE RIGHT NOW: “Is there a time when (Patient /Surrogate Name) would be available to talk with me?” (IF THERE IS A FAMILY GATEKEEPER WHO ASKS QUESTIONS, DO NOT REVEAL ANY INFORMATION REGARDING THE PATIENT’S MEDICAL CONDITION. YOU MAY TELL THEM THAT YOU ARE CALLING ABOUT A HEALTH STUDY CALLED SHARE THOUGHTS ON CARE AND THAT YOU RECENTLY SENT THE PATIENT INFORMATION ABOUT THE STUDY AND THAT YOU ARE CALLING TO SEE IF THE PATIENT IS WILLING TO PARTICIPATE IN THE SECOND INTERVIEW FOR THE STUDY.) PATIENT OR INTENDED SURROGATE IS UNABLE TO COME TO THE PHONE BECAUSE OF ILLNESS OR COMMUNICATION DIFFICULTIES (other than language communication difficulties): “We recently sent a letter to (Name of Patient/Surrogate) about a study called Share Thoughts on Care. (Name of Patient/Surrogate) participated in our study several months ago. We are calling today to see (if/when) (Name of Patient) might be able to participate in the second telephone interview for this study.” INTERVIEWER: INQUIRE AS TO WHEN THE TARGET PATIENT/SURROGATE MAY BE ABLE TO BE INTERVIEWED. IF POSSIBLE, RESCHEDULE WITHIN 2 -4 WEEKS. IF THEY SEEM UNSURE ABOUT WHEN THE PATIENT MIGHT BE FEELING WELL ENOUGH, SUGGEST THAT YOU COULD CHECK BACK IN A FEW WEEKS AND SEE HOW HE/SHE IS DOING. PATIENT IS IN NURSING HOME: “We recently sent a letter to (Name of Patient) about a study called “Share Thoughts on Care”. (Name of Patient) has previously participated in our study. Would it be possible for me to call (Name of Patient) at the nursing facility?” IF YES: “Could you tell me the address and phone number where (he/she) can be reached?” (RECORD ADDRESS AND ENTER INTO CATI. SEND STUDY INFORMATION AND RESCHEDULE CONTACT WITH TARGET PATIENT.) IF NO: “Thank you for your time.” PATIENT IN NURSING HOME BUT PERSON EXPECTS PATIENT WILL BE HOME WITHIN A WEEK OR TWO. INTERVIEWER: ASK IF THE PATIENT IS ABLE TO COMPLETE A TELEPHONE INTERVIEW WHILE IN THE NURSING HOME. IF YES, CATI WILL BRING UP CONTACT INFORMATION QUESTIONS AND PROMPT TO SEND A NEW LETTER TO THE NURSING HOME. IF NOT, SCHEDULE A CALL BACK IN A FEW WEEKS TO SEE IF THE PATIENT HAS RETURNED HOME. PATIENT IS NEAR DEATH: G-8 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 INTERVIEWER: WE DO NOT WANT TO TRY TO INTERVIEW IF THE PERSON WHO ANSWERS THE TELEPHONE STATES THAT THE PATIENT IS NEAR DEATH. IN THIS SITUATION, TELL THEM THAT YOU ARE SORRY TO HEAR THAT THE PATIENT IS NOT DOING WELL AND THANK THEM FOR THEIR TIME. INTERVIEWER SHOULD PASS THIS INFORMATION ALONG TO THE STUDY RECRUITMENT TEAM TO KEEP IN CLOSE CONTACT WITH THE PATIENT’S PHYSICAN TO ASSESS THE PATIENT’S VITAL STATUS. IF APPROPRIATE, THIS CASE SHOULD BE SWITCHED OVER TO A DECEDENT FOLLOWUP SURVEY CASE. PATIENT IS DECEASED: INTERVIEWER: IN THIS SCENARIO, THE GOAL IS TO IDENTIFY AN APPROPRIATE SURROGATE, ASSESS THE BEREAVEMENT WINDOW (MUST BE AT LEAST ONE MONTH SINCE DEATH), AND SCHEDULE AN INTERVIEW USING THE DECEDENT FOLLOW-UP SURVEY INSTRUMENT “Please accept our deepest sympathy over the loss of (Name of patient). We recently sent a letter to (Name of patient) about a study that we are conducting to learn more about the experiences of patients after they have been diagnosed with lung or colorectal problems. (Name of patient) previously participated in an interview for this study.” “May I ask when (PATIENT) died?” (DOCUMENT DATE OF DEATH) “Who am I speaking with?” IF NEEDED, “Can you tell me how you are related to (Name of patient)?” “Because it is important to gather information on everyone who is eligible, we are also interviewing next of kin for those patients who are recently deceased. We are asking that someone who was familiar with how the patient was doing since the diagnosis with lung or colorectal problems to complete a telephone interview on their behalf. Are you the person who knows the most about the medical care and knows the most about how (Name of patient or relationship) was doing during (his/her) illness?” IF NO: “Is there someone else that we should speak with?” GET CONTACT INFORMATION ON AN ALTERNATE SURROGATE. OFFER TO SEND STUDY MATERIALS IN THE MAIL TO THIS POTENTIAL PARTICIPANT. CONFIRM CONTACT INFORMATION FOR THIS MAILING. IF YES: “May I tell you more about this study? Is this a good time for us to talk?” IF THE SURROGATE STATES THAT IT IS TOO SOON TO TALK, ASK IF YOU CAN SEND STUDY INFORMATION IN THE MAIL AND SCHEDULE A TIME TO TALK. IF APPROPRIATE, BEGIN CONSENT PROCESS WITH DECEDENT FOLLOW-UP SURVEY INSTRUMENT: “I would first like to ask you the interview questions. After the interview today, we will be sending you (insert incentive) to thank you for participating in this study. Before we begin, there are a couple of important things I need to go over with you that were included in the information that we sent. G-9 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 The National Cancer Institute is funding this research study. Your participation in this interview is voluntary. If you decide not to participate, it will not affect you in any way. This is a research interview so none of your responses will be used for treatment purposes. Your answers will be kept strictly confidential and will not be shared with [PATIENT NAME’s] doctor or other health care providers. Records of participation in this research project will be kept confidential to the full extent permitted by law. The investigators have obtained a Certificate of Confidentiality from the Department of Health and Human Services. This Certificate means that the investigators cannot be forced (for example by court subpoena) to tell people who are not connected with this study about your participation without your written consent. However, you may voluntarily release information about yourself or your involvement in this research. This telephone interview will last about 30 minutes. You are free to stop this interview at any time. Parts of the interview may be monitored by my supervisor for quality control purposes. Do you have any questions about who is doing the study or anything else about to the study?” (ANSWER ANY QUESTIONS. IF SURROGATE HAS QUESTIONS THAT YOU CANNOT ANSWER, MAKE A NOTE AND TELL THEM THAT YOU WILL CALL THEM BACK.) “By answering the following questions, you are consenting to the use of your answers in our research study. Thank you for your willingness to talk with me today about (Name of Patient’s) experiences. As we go along with the interview, please remember There are no right or wrong answers. Please try to answer questions as honestly and as accurately as you can. Take your time and If you are not sure what a question means or what kind of answer is wanted be sure to ask me If there is a question that you don’t want to answer, just tell me and I will skip it. May we begin?” CONTINUE WITH INTERVIEW IF SURROGATE SAYS THAT HE/SHE MAY NOT BE THE BEST PERSON TO ANSWER THESE QUESTIONS FOR THE PATIENT, A) THANK THE PARTICIPANT AND GO ON TO THE NEXT SURROGATE LISTED IF THERE IS ONE OR B) IF NO OTHER SURROGATE IS LISTED, TELL SURROGATE THAT HE/SHE IS THE ONLY PERSON IDENTIFIED BY THE PATIENT AND ASK WHETHER THERE IS SOMEONE ELSE WHO MAY KNOW ABOUT THE CARE THE PATIENT RECEIVED IF SURROGATE STATES THAT HE/SHE IS JUST NOT INTERESTED IN PARTICIPATING THEN TERMINATE THE INTERVIEW (Thank you for your time). G-10 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 Appendix H: Translations of Patient Survey UNC administers only English version of surveys. H-1 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Appendix I: Physician Contact Letter I-1 Protocol 001 Amendment #3, December 2005 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 CANCER CARE OUTCOMES RESEARCH STUDY Date Name Address Address City, State Zip Dear Dr. ____________: We are conducting an NIH-funded study of colorectal cancer in a 33-county area of North Carolina. The purpose of this research study is to learn how access to health care, differences in prescribed treatments and differences in patients’ lifestyles may be related to disparities in clinical outcomes for people diagnosed with colorectal cancer. Let me emphasize that this is NOT a treatment study. Participants in this study complete a telephone interview, donate a small sample of blood and sign releases for their medical records and tumor blocks. We will pay them $35 for their time. One of your patients (see attached page) might be eligible for the study. We are notifying you that we will contact your patient about this research study unless you have any objections. If we do not hear from you within three weeks we will contact this patient. Your patient was identified through the North Carolina Central Cancer Registry (NCCCR) as someone who was recently diagnosed with colorectal cancer. The NCCCR mailed a brochure to this person with information about the role of the Central Cancer Registry, including a notification that the patient may be contacted by researchers who are working to improve the health of citizens of North Carolina. If you have objections to our contacting this patient, please return this form in the enclosed envelope, or fax it to 1-919-966-7592. If we do not hear from you within three weeks, we will contact the participant. A patient can decline to participate at any time. Many patients with colon cancer welcome the chance to participate in a study that might help others. If you have any questions about the Cancer Care Outcomes Research Study, please contact me at our toll free number: 1-800-840-9754. Thank you for your support of this important research. Sincerely, Robert Sandler, MD, MPH Professor of Medicine and Epidemiology Principal Investigator I-2 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 CANCER CARE OUTCOMES RESEARCH STUDY PHYSICIAN NOTIFICATION FORM DATE OF NOTIFICATION: PHYSICIAN: Patient Name: Address: DOB: SSN: We plan to contact the above named person about the Cancer Care Outcomes Research Study. If you have no objections to our contacting this person, you do not need to return this form. We will contact the above named person if we do not hear from you within three weeks of the date printed at the top of this form. I have no objection to your contacting this person about this study. I do have objections about your contacting this person. I am not the physician for this patient. Physician Name & Phone # _______________________________ I do not know who the physician is. ________________________________________ Physician Signature PLEASE FAX TO: (919) 966-7592 ______________ Date Ref#: _________ OR USE ENCLOSED ENVELOPE AND MAIL TO: Cancer Care Outcomes Research Study CB# 7555, 4104 Bioinformatics Bldg. UNC Chapel Hill, NC 27599-7555 FOR QUESTIONS CALL: (800) 840-9754 I-3 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 Appendix J: Patient and Surrogate Contact Letters and Brochures J- 1 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 Introductory Letter (Participant) Date Name Address Address City, State Zip Dear Name, We are writing to invite you to take part in a research study. The purpose of this study is to learn more about people’s experiences with medical care when they have colorectal cancer. We believe that the results of this study could identify ways to improve the lives of patients with cancer. The study is funded by the National Institutes of Health. Researchers from the University of North Carolina at Chapel Hill and five other universities are conducting the study. We got your name from the North Carolina Central Cancer Registry. All hospitals are required by law to report new cancer cases to the State Cancer Registry. The Registry works with researchers in North Carolina on important studies. We let your doctor know that we planned to contact you. If you decide to take part in the study, there are several things we will ask you to do. You do not have to complete all of the parts if you do not want to. It would be most helpful, however, if you agreed to all parts of the study so we will have the best chance of answering some important questions. 1. Telephone interview: The interviewer will ask you questions about how you were diagnosed with cancer and what kind of treatments you have received. It will take about one hour to answer all the questions. If there are any questions you do not want to answer, you may skip them. This interview can be scheduled at a time that is convenient for you, including evenings and weekends. 2. Medical Records: We will ask you to sign a release form so we can collect information from your medical record. If you have Medicare, we will ask your permission to collect information about the claims your doctor has submitted on your behalf. 3. Tumor Tissue: After every person’s surgery, the hospital saves part of the tumor that was removed. We will ask you to sign a release form so we can borrow this tumor from the hospital. After our researchers are finished with it, we will return it to the hospital. 4. Blood Sample: We will make arrangements for your doctor to take a small sample of your blood and mail it to our laboratory. This can be done at your convenience, probably during your next doctor’s visit. If there is a charge for the blood draw, we will pay for it. There is no cost to you. In fact, we will pay you $35 for your help - $15 following the interview and $20 once the release forms have been returned. Your participation is completely voluntary. Whether or not you participate in this study will not influence your current medical care. All of the information that you give us will be kept confidential. None of your answers will be given to your doctor or to anyone else without your permission. The scientific reports from the study will not identify you. J- 2 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 A member of our study staff will be calling you within two weeks to tell you more about the study, answer questions, and set up a convenient time for an interview. We very much hope that you will say “yes”. Please call us at our toll-free number if you have any questions about this research study, if your address or telephone number has changed, or if you do not wish to participate. The toll free number is 1-888-819-4393. We very much hope that you will decide to take part in this important research study. You can play an important role in cancer research by giving just a little of your time. Thank you for your consideration. Sincerely, Robert S. Sandler, M.D., M.P.H. Professor of Medicine and Epidemiology J- 3 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 Introductory Letter (Proxy - Participant Deceased) Date Name Address Address City, State Zip Dear Name, We are writing to invite you to take part in a research study. The purpose of this study is to learn more about colorectal cancer. The study is funded by the National Institutes of Health. Researchers from the University of North Carolina at Chapel Hill and five other universities are conducting the study. We work with the North Carolina Central Cancer Registry to identify people who might be interested in helping with the study. They let us know that participant’s name recently had colorectal cancer. Please accept our sympathy for your loss. When you are ready, we would like to learn more about the care that your relationship received after he/she had colorectal cancer. We are hoping to learn about people’s experiences with cancer so we can help future generations that might also experience it. If you decide to take part in the study, we will ask you to complete a telephone interview. The interviewer will ask you questions about how participant’s name was diagnosed with cancer and what kind of treatments he/she received. It will take about one hour to answer all the questions. If there are any questions you do not want to answer, you may skip them. This interview can be scheduled at a time that is convenient for you, including evenings and weekends. We will ask you to sign release forms that will allow us to collect information from participant’s name’s medical record and allow us to borrow the tumor tissue removed during surgery from the hospital. After our researchers are finished with the tissue, we will return it to the hospital. There is no cost to you. In fact, we will pay you $35 for your help - $15 following the interview and $20 when the release forms are returned. Your participation is completely voluntary. All of the information that you give us will be kept confidential. None of your answers will be given to participant’s name’s doctor or to anyone else without your permission. The scientific reports from the study will not identify you. Please call us toll-free at 1-888-819-4393 if you have any questions about this research study, if you would like to schedule an interview, or if you do not wish to participate. If we do not hear from you within two weeks, a member of our staff will call you to tell you more about the study and answer your questions. We very much hope that you will decide to take part in this important research study. You can play an important role in cancer research by giving just a little of your time. Sincerely, Robert S. Sandler, M.D., M.P.H. Professor of Medicine and Epidemiology J- 4 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 Introductory Letter (Proxy – Participant Living) Date Name Address Address City, State Zip Dear Name, We are writing to invite you to take part in a research study. The purpose of this study is to learn more about people’s experiences with colorectal cancer. We believe that the results of this study could identify ways to improve the lives of patients with cancer. The study is funded by the National Institutes of Health. Researchers from the University of North Carolina at Chapel Hill and five other universities are conducting the study. We spoke to participant’s name who gave us your name as someone who might help with this research study. He/She felt unable to participate in the study and thought you might take part on his/her behalf. We got participant’s name’s name from the North Carolina Central Cancer Registry. All hospitals are required by law to report new cancer cases to the State Cancer Registry. The Registry works with researchers in North Carolina on important studies. About 1000 people with colorectal cancer will be contacted about this study. Some people take part in the study themselves and some people identify family members or friends to take part for them. Participant’s name gave us permission to contact you and ask if you would take part in the study for them. There is no cost to you. In fact, we will pay you $15 for your help. If you decide to take part in the study, we will ask you to complete a telephone interview. The interviewer will ask you questions about how participant’s name was diagnosed with cancer and what kind of treatments he/she received. It will take about one hour to answer all the questions. If there are any questions you do not want to answer, you may skip them. This interview can be scheduled at a time that is convenient for you, including evenings and weekends. Your participation is completely voluntary. All of the information that you give us will be kept confidential. None of your answers will be given to participant’s name’s doctor or to anyone else without your permission. The scientific reports from the study will not identify you. Please call us toll-free at 1-888-819-4393 if you have any questions about this research study, if you would like to schedule an interview, or if you do not wish to participate. If we do not hear from you within two weeks, a member of our staff will call you to tell you more about the study and answer your questions. We very much hope that you will decide to take part in this important research study. You can play an important role in cancer research by giving just a little of your time. Sincerely, Robert S. Sandler, M.D., M.P.H. Professor of Medicine and Epidemiology J- 5 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 Follow-up, No Contact Letter Date Name Address Address City, State Zip Dear Name, We recently sent you a letter about the “Share Thoughts on Care” Study that is being conducted at the University of North Carolina at Chapel Hill. Please read the enclosed brochure to learn more about the study. We have been trying to contact you to find out if you are interested in taking part in a telephone interview. Unfortunately, we have been unable to reach you. It would be very helpful if you let us know the best way to get in touch with you. Please call us toll-free at (888) 819-4393 or use the postage paid envelope to return the form below. Even if you are not sure if you would like to take part in the study, it is important that we hear from you soon. We would be glad to answer any questions you might have. If you decide to take part in the study, we will pay you $35. Thank you for your cooperation. Sincerely, Robert S. Sandler, M.D., M.P.H. Professor of Medicine and Epidemiology PLEASE COMPLETE AND RETURN IN POSTAGE-PAID ENVELOPE We have not been able to contact you. Please call our toll-free number (888) 819-4393 or return this part of the letter to let us know your correct phone number. «Partic_FullName» My phone number is ______________________________________ The best time to reach me is: ____________________________________________________________ Comments: __________________________________________________________________________ «StudyID» J- 6 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 Letter to Undecided Participants Date Name Address Address City, State Zip Dear Name, Thank you for speaking with the staff from the “Share Thoughts on Care” Study. We wanted to make you aware of the many ways you can be a part of this research project: It is your choice how you participate. We will pay you up to $35 if you take part in the study - $15 for completing the interview and $20 for the return of release forms.. If you’re interested, you may choose one or more of the options listed below: □ You may take part in a telephone interview that will last about one hour. □ You may take part in a brief telephone interview that will last about 20 minutes. □ You may select someone who is familiar with your medical care to complete the telephone interview on your behalf. □ You may sign forms allowing us to collect information from your medical records and get a sample of your tumor. □ You may donate a blood sample. If it is convenient for you, this can be done the next time you go to your doctor. If your doctor charges for this service, we will pay the bill. The study will continue for several months, so if you would like to take part please call us at 1-888-819-4393 (toll free) to let us know. Again, thank you for your time and patience. With your help, we hope that our research will benefit others through an improved understanding of the best ways to provide treatment to people with colorectal cancer. Sincerely, Robert S. Sandler, M.D., M.P.H. Professor of Medicine and Epidemiology Follow-up Survey Introductory Letter - Participant Date J- 7 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 Follow-up Survey Introductory Letter – Participant Name Address Address Address Dear Mr./Mrs./Ms.: Several months ago you participated in an interview for our study, Share Thoughts on Care. The purpose of this study is to learn how people are treated for their cancer, what things influence their choice of treatment, and about their experiences with cancer. The study is sponsored by the National Cancer Institute and is being conducted by scientists and researchers in seven areas around the United States. When we spoke with you last, we told you we would call you again to follow up on any changes that may have taken place. It is now time for us to call. A study staff member will call you in a few days to conduct the interview on the telephone. Taking part in the interview is completely voluntary. You may choose not to take part at all. If you decide to participate in the interview, you may stop at any time. If you decide not to participate, you won’t be penalized or lose any benefits for which you otherwise qualify. If you choose to participate in the interview, it will take about 30 minutes and, if you prefer, can be completed in more than one session. The interview will be given over the phone by one of our trained research interviewers. There will be no costs involved if you participate; in fact, if you participate in the telephone interview we will pay you $10 for your time. Your answers will be kept strictly confidential and will not be shared with your doctor or other health care providers. Records of participation in this research project will be kept strictly confidential, and, to ensure this, the investigators have obtained a Certificate of Confidentiality from the Department of Health and Human Services. This Certificate means that the investigators cannot be forced to tell people who are not connected with this study about your participation without your written consent. You or a member of your family, however, may voluntarily release information about yourself or your involvement in this research. Please call us at our toll-free number if you have any questions about this research study, if your address or telephone number has changed, or if you do not wish to participate. The toll free number is 1-888-819-4393. If you have questions about the rights of research subjects, you may contact the UNC Office of Human Research Ethics at 919-966-1344. We thank you for your participation in this study. Sincerely, Robert Sandler, M.D., M.P.H. Professor of Medicine and Epidemiology J- 8 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 Follow-up Survey Introductory Letter – Participant/Baseline Proxy Interview Date Name Address Address Address Dear Mr./Mrs./Ms.: Several months ago (SURROGATE NAME) participated in an interview on your behalf for our study called Share Thoughts on Care. The purpose of this study is to learn how people are treated for their cancer, what things influence their choice of treatment, and about their experiences with cancer. The study is sponsored by the National Cancer Institute and is being conducted by scientists and researchers in seven areas around the United States. When we spoke with you and with (SURROGATE NAME) last we said we would call again in a few months to follow up on any changes that may have taken place. It is now time for us to call. A study staff member will call you in a few days to conduct the interview with you on the telephone. Taking part in the interview is completely voluntary. You may choose not to take part at all. If you decide to participate in the interview, you may stop at any time. If you decide not to participate, you won’t be penalized or lose any benefits for which you otherwise qualify. If you choose to participate in the interview, it will take about 30 minutes and, if you prefer, can be completed in more than one session. The interview will be given over the phone by one of our trained research interviewers. There will be no costs involved if you participate; in fact, if you participate in the telephone interview we will pay you $10 for your time. Your answers will be kept strictly confidential and will not be shared with your doctor or other health care providers. Records of participation in this research project will be kept strictly confidential, and, to ensure this, the investigators have obtained a Certificate of Confidentiality from the Department of Health and Human Services. This Certificate means that the investigators cannot be forced to tell people who are not connected with this study about your participation without your written consent. You or a member of your family, however, may voluntarily release information about yourself or your involvement in this research. Please call us at our toll-free number if you have any questions about this research study, if your address or telephone number has changed, or if you do not wish to participate. The toll free number is 1-888-819-4393. If you have questions about the rights of research subjects, you may contact the UNC Office of Human Research Ethics at 919-966-1344. We thank you for your participation in this study. Sincerely, Robert Sandler, M.D., M.P.H. Professor of Medicine and Epidemiology J- 9 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 Follow-up Survey Introductory Letter - Decedent Date Name Address Address Address Dear Mr./Mrs./Ms.: Several months ago [PATIENT NAME] participated in an interview for our study called Share Thoughts on Care. The purpose of this study is to learn how people are treated for their cancer, what things influence their choice of treatment, and about their experiences with cancer. The study is sponsored by the National Cancer Institute and is being conducted by scientists and researchers in seven areas around the United States. When we spoke with [PATIENT NAME] last, we said we would call again in a few months to follow up on any changes that may have taken place. It is now time for us to call. Because it is important to gather information on everyone in the study, we are also contacting next of kin for those patients who are recently deceased. We are asking that someone who was close to the patient – someone who was familiar with how the patient was doing since being diagnosed with colon cancer – complete a telephone interview. [PATIENT NAME] gave us permission to speak with you if we were unable to reach [HIM/HER] in the future. A study staff member will call you in a few days to conduct the interview on the telephone. Taking part in the interview is completely voluntary. You may choose not to take part at all. If you decide to participate in the interview, you may stop at any time. If you choose to participate in the interview, it will take about 30 minutes and, if you prefer, can be completed in more than one session. The interview will be given over the phone by one of our trained research interviewers. There will be no costs involved if you participate; in fact, if you participate in the telephone interview we will pay you $10 for your time. Your answers will be kept strictly confidential and will not be shared with [PATIENT NAME]’s doctor or other health care providers. Records of participation in this research project will be kept strictly confidential, and, to ensure this, the investigators have obtained a Certificate of Confidentiality from the Department of Health and Human Services. This Certificate means that the investigators cannot be forced to tell people who are not connected with this study about your participation without your written consent. However, you may voluntarily release information about yourself or your involvement in this research. Please call us at our toll-free number if you have any questions about this research study, if your address or telephone number has changed, or if you do not wish to participate. The toll free number is 1-888-819-4393. If you have questions about the rights of research subjects, you may contact the UNC Office of Human Research Ethics at 919-966-1344. We thank you for your participation in this study. Sincerely, Robert Sandler, M.D., M.P.H. Professor of Medicine and Epidemiology J-10 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 Follow-up Survey Thank You Letter - Participant Date Name Address Address City, State Zip Dear Name, Please accept our sincere thanks for participating in the Share Thoughts on Care study. As promised, we are enclosing a check for $10 to express our appreciation for the time you took to participate in our follow-up survey. With your help, we hope that our research will benefit others through an improved understanding of the best ways to provide treatment to people with colorectal cancer. Sincerely, Robert S. Sandler, M.D., M.P.H. Professor of Medicine and Epidemiology J-11 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 Follow-up Survey Thank You Letter - Decedent Date Name Address Address City, State Zip Dear Name, Please accept our sincere thanks for participating in the Share Thoughts on Care study. As promised, we are enclosing a check for $10 to express our appreciation for the time you took to participate in our follow-up survey on behalf of [NAME]. With your help, we hope that our research will benefit others through an improved understanding of the best ways to provide treatment to people with colorectal cancer. Sincerely, Robert S. Sandler, M.D., M.P.H. Professor of Medicine and Epidemiology J-12 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 Letter to Participant Requesting Missing Consent Forms Date Name Address 1 Address 2 Dear Name, Thank you again for your participation in the Share Thoughts on Care Study. We hope you are doing well. We received some of your signed consent forms in the mail, but, according to our records, we are missing the following: □ Two consent forms describing the study, how we will use the information you shared with us, and how to withdraw from the study if you choose to do so (pink) □ Consent for Storing Blood, Tissue, or Body Fluid and a brochure explaining storage and use of specimens (blue) □ Authorization for the release of medical records and specimens (yellow). Please check to make sure that all information is correct and that we have included all hospitals and clinics where you had tests, surgery or were treated for your cancer. I have enclosed copies of the missing form(s). Please read, sign and return the colored form(s) in the postage-paid envelope. The white copy (copies) is (are) for your records. Please call us toll-free at 1-888-819-4393 if you have any questions. Thanks again! Sincerely, Name J-13 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Text for Patient Brochure and General Brochure [Actual brochures are included as well.] J-14 Protocol 001 Amendment #3, December 2005 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 PATIENT BROCHURE TEXT What Is Share Thoughts on Care? Share Thoughts on Care is a research study for people who have been recently diagnosed with lung or colorectal disease, including cancer. The goal of Share Thoughts on Care is to learn about the treatment choices patients make, and to find out how satisfied they are with their care. The National Cancer Institute is sponsoring Share Thoughts on Care, which includes researchers from fourteen hospitals, managed care organizations, and research organizations across the country. Eleven VA Medical Centers are also participating in the project; the Department of Veterans Affairs sponsors the VA sites. Who May Participate in Share Thoughts on Care? Share Thoughts on Care is for people who have lung or colorectal diseases, including cancer. These diseases affect large numbers of people in the United States, and your views and experiences can help improve how these diseases are treated. Your thoughts are important! Why is the Study Being Conducted? The study sponsors, research teams, and participating healthcare providers care deeply about the experiences of people with lung or colorectal diseases, including cancer. The information participating patients share with us will be made available in summary form to healthcare providers, policy and decision makers, and insurers, as well as other people diagnosed with these diseases so that care may be improved in the future. What Does Participation Involve? If you choose to participate in Share Thoughts on Care, you will take part in a personal interview about your health and treatment and how they have affected your quality of life. This interview will take place over the phone with a specially trained Share Thoughts on Care research interviewer. J-15 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 During the interview you will be asked about: the symptoms of your disease, if any your experiences with care providers your health history and care received You will also be asked to provide permission for the research team to review the medical records related to your care. You will not be asked to take any medical tests or undergo any medical treatments or procedures. Share Thoughts on Care is interested in your opinions only. About a year after the interview, we will contact you again to follow up on any changes that may have occurred. What If I Decide to Participate? Taking part in Share Thoughts on Care is your choice. Any information you share in your interview will be kept confidential. It will not be shared with your doctors or other healthcare providers, and your answers will not affect your health care in any way. If you decide not to take part in the study, or if you take part in the study now and decide to stop participating later on, it will not affect your care or your relationships with your doctors. How Do I Learn More? A Share Thoughts on Care staff member will call you at home to talk with you about the study and ask if you’d like to participate. In the meantime, if you would like to learn more, please call the Share Thoughts on Care staff at the toll-free number below. Place sticker with PDCRs 1-800 number here NCI logo and VA logo appear here J-16 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 General Provider Brochure Text What is the purpose of this brochure? This brochure is intended to provide background information to the health care provider of patients who may be eligible for this study. Providers identified by tumor registries or medical records as the attending health care provider at the time of cancer diagnosis may be notified of the research group’s intent to solicit patient participation in the study. Some providers who treat these patients will be surveyed about the volume of cancer patients in their practices and about their opinions on therapies for lung, colon, and rectal cancers. Health care providers will not be asked about specific patients. What is Share Thoughts on Care? Share Thoughts on Care is a national study for people who have been recently diagnosed with cancer of the lung, colon, or rectum. The goal of Share Thoughts on Care is to learn what factors affect lung and colorectal patients’ treatment choices and outcomes. Patients’ views and experiences can help shape how these diseases are treated. This study will look at medical practices that might prove of value but have never been subjected to clinical trials. Through patient interviews, reviews of medical records, and surveys across a wide range of health care providers and organizations, Share Thoughts on Care will gain valuable information on how to improve care in the future. Who may take part in Share Thoughts on Care? Using tumor registries or medical records, study staff will select a sample of newly diagnosed patients with invasive primary tumors of the lung, colon or rectum. Persons with a prior history of lung or colorectal cancer are not eligible. Trained interviewers will be available for patients whose primary language is English and at some centers for patients whose primary language is Spanish or Chinese. A friend or family member may complete the interview for a participant who is too ill to be interviewed or is deceased. How are participants enrolled in this study? People who are selected will be invited by letter and phone to be interviewed. Participation is voluntary. Deciding whether to take part in the study will have no effect on a patient’s care, relationship with his or her doctor, or health plan benefits. Although most participants will be fully aware of their cancer diagnosis, the recruitment letters and surveys for this study are also designed to be used with patients who may not be aware of their cancer diagnosis, either because of memory loss or requests by legal guardians to withhold this information. What kinds of questions will be asked in the interview? Trained interviewers will ask patients about the treatments they received and how decisions about their care were made. There also will be some basic questions about their health status and how their care affected their cancer and their quality of life. In addition, interviewers will ask for some demographic information, such as age and ethnic background. Of course, participants may choose not to answer any question. The interview is expected to take about one hour and fifteen minutes. Are there any potential risks to participants? The risks and benefits for study participants have been carefully reviewed and approved by the Institutional Review Boards at each of the participating research sites and the central coordinating center. This observational study involves only interviews and medical record reviews to collect information about participants. It does not include any treatment or intervention. Although risks to participants include loss of privacy and breach of confidentiality, the study has been carefully designed to protect their privacy. J-17 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 How will Share Thoughts on Care protect the confidentiality of study participants? The National Institutes of Health has granted this project a Certificate of Confidentiality. This certificate protects participating researchers from being forced to disclose any information that may identify any participants in any federal, state, legislative, or other proceedings. What is the schedule for the Share Thoughts on Care study? Enrollment for this study began in the Summer of 2003. Researchers will enroll approximately 5,000 patients with lung cancer and 5,000 patients with colorectal cancer across the U.S. Study staff will gather information about patients’ cancer treatment between 2003 and 2005. The research team expects to publish its findings in 2005 and 2006. Who is sponsoring Share Thoughts on Care? The study is funded by the National Cancer Institute of the National Institutes of Health. The Department of Veterans Affairs funds the VA sites. Who is conducting Share Thoughts on Care? The study is being conducted by the CanCORS (Cancer Care Outcomes Research and Surveillance) Consortium, involving researchers from the following hospitals and institutions: University of North Carolina at Chapel Hill University of Alabama at Birmingham University of Iowa A collaboration between RAND and UCLA A collaboration of Harvard Medical School with the Northern California Cancer Center and Kaiser Permanente Northern California A collaboration between the Dana-Farber Cancer Institute and the Cancer Research Network, a network of health maintenance organizations, including Group Health Cooperative, Harvard Pilgrim Health Care, Henry Ford Health System, Kaiser Permanente Hawaii, and Kaiser Permanente Northwest Department of Veterans Affairs. This includes the following VA Medical Centers: Baltimore, MD; Biloxi, MS; Durham, NC; Hines and Lakeside, IL; Minneapolis, MN; Nashville, TN; New York Harbor, NY; Portland, OR; Temple TX; Tucson, AZ. Share Thoughts on Care also has a central coordinating center at the Dana-Farber Cancer Institute in Boston, Massachusetts. Where can I get more information? For more information, please contact the principal investigator for the project at: (affix local site contact info. sticker) If your patients have questions about the study please direct them to the Share Thoughts on Care recruitment staff at: (affix local site 800# sticker) Also, please visit the Share Thoughts on Care Web page at: http://cancercontrol.cancer.gov/ARP/research/cancors.asp © Copyright 2003, Share Thoughts on Care J-18 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 Appendix K: Medical Release Consent Forms and Cover Letters K-1 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 Consent Letter - Participant Date Name Address Address City, State Zip Dear Name, Please accept our sincere thanks for participating in the Share Thoughts on Care study. As promised, we are enclosing a check for $15 to express our appreciation for the time you took to participate in our survey. In addition to the information you shared during the interview, it would be very helpful if we could collect information from your medical records and get a sample of your blood and tumor. To do this we need your written permission. The following forms are enclosed: □ Two consent forms describing the study, how we will use the information you shared with us, and how to withdraw from the study if you choose to do so (pink) □ Consent for Storing Blood, Tissue, or Body Fluid and a brochure explaining storage and use of specimens (blue) □ Authorization for the release of medical records and specimens (yellow). Please check to make sure that all information is correct and that we have included all hospitals and clinics where you had tests, surgery or were treated for your cancer. There are white copies of each of the enclosed forms for you to keep for your records. Please read, sign and return the colored forms to us in the postage-paid envelope. We understand that these forms can be very confusing. The University of North Carolina requires that everyone who takes part in research studies sign forms like these to make sure your privacy is protected. If you have any questions, please call our office toll-free at 1-888-819-4393. Once we receive the forms, we will send you a second check for $20. Although the interviews will continue through the year 2004, we will be glad to send you a copy of the findings when they are available. Please contact us at 1-888-819-4393 (toll-free) if you would like to receive copies of the results. Again, thank you for your time and patience. With your help, we hope that our research will benefit others through an improved understanding of the best ways to provide treatment to people with colorectal cancer. Sincerely, Robert S. Sandler, M.D., M.P.H. Professor of Medicine and Epidemiology K-2 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 Consent Letter – Proxy for Deceased Participant Date Name Address Address City, State Zip Dear Name, Please accept our sincere thanks for participating in the Share Thoughts on Care study. As promised, we are enclosing a check for $15 to express our appreciation for the time you took to participate in our survey. Please accept our sympathy for your loss. In addition to the information you shared during the interview, it would be very helpful if we could collect information from «Patient»’s medical records and get a sample of «HisHer» tumor. To do this we need your written permission. The following forms are enclosed: □ Two consent forms describing the study, how we will use the information you shared with us, and how to withdraw from the study if you choose to do so (pink) □ Consent for Storing Blood, Tissue, or Body Fluid and a brochure explaining storage and use of specimens (blue) □ Authorization for the release of medical records and specimens (yellow): Please check to make sure that all information is correct and that we have included all hospitals and clinics where «Patient» had tests, surgery or was treated for cancer. There are white copies of each of the enclosed forms for you to keep for your records. Please read, sign and return the colored forms to us in the postage-paid envelope. We understand that these forms can be confusing. The University of North Carolina requires that everyone who takes part in research studies sign forms like these to make sure your privacy is protected. If you have any questions, please call our office toll-free at 1-888-819-4393. Once we receive the forms, we will send you a second check for $20. Although the interviews will continue through the year 2004, we will be glad to send you a copy of the findings when they are available. Please contact us at 1-888-819-4393 (toll-free) if you would like to receive copies of the results. Again, thank you for your time and patience. With your help, we hope that our research will benefit others through an improved understanding of the best ways to provide treatment to people with colorectal cancer. Sincerely, Robert S. Sandler, M.D., M.P.H. Professor of Medicine and Epidemiology K-3 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 Consent Letter – Proxy for Living Participant Date Name Address Address City, State Zip Dear Name, Please accept our sincere thanks for participating in the Share Thoughts on Care study. As promised, we are enclosing a check for $15 to express our appreciation for the time you took to participate in the study. In addition to the information you shared during the interview, it would be very helpful if we could collect information from «Patient»’s medical records and get a sample of «HisHer» blood and tumor. To do this we need «HisHer» written permission. We are hoping you can help us get this. The following forms are enclosed: □ Two consent forms for «Patient» to sign describing the study, how we will use the information you shared with us, and how to withdraw from the study if you or «Patient» choose to do so (pink) □ Two consent forms for you to sign (pink) □ Consent for Storing Blood, Tissue, or Body Fluid and a brochure explaining storage and use of specimens (blue) □ Authorization for the release of medical records and specimens (yellow): Please check to make sure that all information is correct and that we have included all hospitals and clinics where «Patient» had tests, surgery or was treated for cancer. There are white copies of each of the enclosed forms for you to keep for your records. Please read, sign and return the colored forms to us in the postage-paid envelope. We understand that these forms can be confusing. The University of North Carolina requires that everyone who takes part in research studies sign forms like these to make sure your privacy is protected. If you have any questions, please call our office toll-free at 1-888-819-4393. Once we receive the forms, we will send you a check for $20. Although the interviews will continue through the year 2004, we will be glad to send you a copy of the findings when they are available. Please contact us at 1-888-819-4393 (toll-free) if you would like to receive copies of the results. Again, thank you for your time and patience. With your help, we hope that our research will benefit others through an improved understanding of the best ways to provide treatment to people with colorectal cancer. Sincerely, Robert S. Sandler, M.D., M.P.H. Professor of Medicine and Epidemiology K-4 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 Consent Letter – Medical Records Only Date Name Address Address City, State Zip Dear Name, Thank you for speaking with the staff from the “Share Thoughts on Care” Study. It would be very helpful to our research efforts if we could collect information from your medical records and get a sample of your blood and tumor. To do these things we need to have your written permission. The following forms are enclosed: □ Two consent forms describing the study, how we will use the information you shared with us, and how to withdraw from the study if you choose to do so (pink) □ Consent for Storing Blood, Tissue, or Body Fluid and a brochure explaining storage and use of specimens (blue) □ Authorization for the release of medical records and specimens (yellow). Please complete a separate form for each hospital and clinic where you had tests, surgery or were treated for your cancer. There are white copies of each of the enclosed forms for you to keep for your records. Please read, sign and return the colored forms to us in the postage-paid envelope. We understand that these forms can be very confusing. The University of North Carolina requires that everyone who takes part in research studies sign forms like these to make sure your privacy is protected. If you have any questions, please call our office toll-free at 1-888-819-4393. An important part of the study is to collect a blood sample from everyone. The researchers will look at parts of your blood to learn more about why some people get cancer and what treatments might help different types of people. One of our staff members will call you to make arrangements to have your blood drawn. If it is convenient for you, this can be done the next time you go to your doctor. If your doctor charges for this service, we will pay the bill. After the blood is collected, it will be mailed to our lab at UNC. After the consent forms and the blood sample are received, we will send you a check for $20 as a thank you for taking part in the study. Although the study will continue through the year 2004, we will be glad to send you a copy of the findings when they are available. Please contact us if you would like to receive copies of the results. Again, thank you for your time and patience. With your help, we hope that our research will benefit others through an improved understanding of the best ways to provide treatment to people with colorectal cancer. Sincerely, Robert S. Sandler, M.D., M.P.H. Professor of Medicine and Epidemiology K-5 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 Follow-up Survey Thank You Letter and Consent Request - Participant Date Name Address Address City, State Zip Dear Name, Please accept our sincere thanks for participating in the Share Thoughts on Care study. As promised, we are enclosing a check for $10 to express our appreciation for the time you took to participate in our follow-up survey. In addition, our records indicate that we have not received one or more of your consent forms. We have enclosed the outstanding consent forms, along with a postage-paid envelope for returning them. The following forms are enclosed: Two consent forms describing the study, how we will use the information you shared with us, and how to withdraw from the study if you choose to do so (pink) Consent for Storing Blood, Tissue, or Body Fluid and a brochure explaining storage and use of specimens (blue) Authorization for the release of medical records and specimens (yellow): Please check to make sure that all information is correct and that we have included all hospitals and clinics where you had tests, surgery or was treated for cancer. There are white copies of each of the enclosed forms for you to keep for your records. Please read, sign and return the colored forms to us in the postage-paid envelope. We understand that these forms can be very confusing. The University of North Carolina requires that everyone who takes part in research studies sign forms like these to make sure your privacy is protected. If you have any questions, please call our office toll-free at 1-888-819-4393. Once we receive the forms, we will send you a second check for $20. Again, thank you for your time and patience. With your help, we hope that our research will benefit others through an improved understanding of the best ways to provide treatment to people with colorectal cancer. Sincerely, Robert S. Sandler, M.D., M.P.H. Professor of Medicine and Epidemiology K-6 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 Follow-up Survey Thank You Letter and Consent Request - Decedent Date Name Address Address City, State Zip Dear Name, Please accept our sincere thanks for participating in the Share Thoughts on Care study. As promised, we are enclosing a check for $10 to express our appreciation for the time you took to participate in our follow-up survey on behalf of [NAME]. In addition to the information you shared during the interview, it would be very helpful if we could collect information from [NAME]’S medical records and get a sample of his/her tumor. To do this we need your written permission. The following forms are enclosed: Two consent forms describing the study, how we will use the information you shared with us, and how to withdraw from the study if you choose to do so (pink) Consent for Storing Blood, Tissue, or Body Fluid and a brochure explaining storage and use of specimens (blue) Authorization for the release of medical records and specimens (yellow): Please check to make sure that all information is correct and that we have included all hospitals and clinics where [NAME] had tests, surgery or was treated for cancer. There are white copies of each of the enclosed forms for you to keep for your records. Please read, sign and return the colored forms to us in the postage-paid envelope. We understand that these forms can be confusing. The University of North Carolina requires that everyone who takes part in research studies sign forms like these to make sure your privacy is protected. If you have any questions, please call our office toll-free at 1-888-819-4393. Once we receive the forms, we will send you a second check for $20. Again, thank you for your time and patience. With your help, we hope that our research will benefit others through an improved understanding of the best ways to provide treatment to people with colorectal cancer. Sincerely, Robert S. Sandler, M.D., M.P.H. Professor of Medicine and Epidemiology K-7 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 Letter to Participant Requesting Missing Consent Forms Date Name Address 1 Address 2 Dear Name, Thank you again for your participation in the Share Thoughts on Care Study. We hope you are doing well. We received some of your signed consent forms in the mail, but, according to our records, we are missing the following: Two consent forms describing the study, how we will use the information you shared with us, and how to withdraw from the study if you choose to do so (pink) Consent for Storing Blood, Tissue, or Body Fluid and a brochure explaining storage and use of specimens (blue) Authorization for the release of medical records and specimens (yellow). Please check to make sure that all information is correct and that we have included all hospitals and clinics where you had tests, surgery or were treated for your cancer. I have enclosed copies of the missing form(s). Please read, sign and return the colored form(s) in the postagepaid envelope. The white copy (copies) is (are) for your records. Please call us toll-free at 1-888-819-4393 if you have any questions. Thanks again! Sincerely, Name K-8 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 University of North Carolina-Chapel Hill Consent to Participate in a Research Study _________________________________________________________________________________ Medical IRB Study #: 01-MED-390-ORC Consent Form Version Date: March 30, 2004 Title of Study: NC Colorectal Cancer Care Outcomes Research Study Sponsor: National Cancer Institute Principal Investigator: Robert S. Sandler, M.D., M.P.H. UNC-CH Department: Department of Medicine Phone number: 919-966-0090 _________________________________________________________________________________ You are being asked to take part in a research study. The investigator listed above is in charge of the study; other professional persons may help him or act for him. The name of this study is “Share Thoughts on Care”. What are some general things you should know about research studies? Research studies are designed to gain scientific knowledge that may help other people in the future. You may or may not receive any direct benefit from participating. There may also be risks associated with participating in research studies. Your participation is voluntary. You may refuse to participate, or may withdraw your consent to participate in any study at any time, and for any reason, without jeopardizing your future care at this institution or your relationship with your doctor. If you are a patient with an illness, you do not have to participate in research in order to receive treatment. Details about this particular study are discussed below. It is important that you understand this information so that you can decide in a free and informed manner whether you want to participate. You will be given a copy of this consent form. You are urged to ask the investigators named above, or staff members who may assist them, any questions you have about this study at any time. What is the purpose of this study? The purpose of this research study is to learn more about cancer care for people with colorectal cancer. We believe that the results of this study could identify ways to improve the life span and functioning of patients with cancer. We wish to learn how access to health care, differences in prescribed treatments, and differences in patients’ lifestyles may be related to disparities in clinical outcomes for people diagnosed with colorectal cancer. How many subjects will participate in this study? Approximately 1000 people who live in North Carolina and have colorectal cancer will take part in this study. All of the participants were identified through the N.C. Central Cancer Registry. In addition, approximately 9000 more people from around the United States will participate in the study at other research centers. How long will your participation last? Your participation in this study will last for about two years. What will happen if you take part in the study? There is no treatment involved in this study, and participating in the study will not affect your treatment in any way. If you decide to participate, you will be asked to complete an interview over the telephone with a trained interviewer. The interview will last about one hour and should be done about four months after you were first diagnosed with colorectal cancer. The interviewer will ask you about your medical history, how you were diagnosed with cancer, and what kind of treatment you have received. You may skip any questions you do not wish to answer. Your interview might be audiotaped for quality control purposes. If your interview is taped, the interviewer will obtain your permission before the interview begins. If you choose to do so, you may refuse to have your interview audiotaped. K-9 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 We will also ask for your permission to obtain a copy of your medical records (including Medicare claims, if relevant). We will request information related to your diagnosis and treatment of colorectal cancer as well as information about other diseases or conditions you might have. We will also ask your permission to obtain a sample of your tumor tissue from the hospital where you had surgery. After the researchers in our laboratory use a portion of this tissue, we will return it to the hospital. We will also ask you to donate a small sample of blood. This will be drawn at your doctor’s office or another convenient location. If there is any charge for this blood draw, you will not have to pay for it. Our study will cover all costs associated with the blood draw and shipment. Some people in this study will be asked to complete a short in-home survey. If you are chosen to take part in this piece of the study, an interviewer will come to your home for about 20 minutes to ask you questions about how well you understand certain words that have to do with health. About a year after the first telephone interview we will follow up with you to find out how you are doing. At that time, you will be asked to complete a brief telephone interview and to sign updated consent forms granting permission for us to request your medical records. You may be contacted at other times during the course of the four-year study. Are there any reasons you should not participate? You should not participate in this study if you do not wish to be interviewed over the telephone or if you do not wish to donate a blood sample. What are the possible risks or discomforts? There is a minimal risk of discomfort answering questions about your lifestyle or medical history. There is a minimal risk of loss of confidentiality although we will take every precaution to make sure this does not happen. Your name will not be placed on the questionnaires. When you have your blood drawn, you might experience some minor soreness or discoloration on your arm. What are the possible benefits? You will not receive any direct benefit from participating in the study. However, by taking part in this study, you may benefit from the knowledge that you have helped researchers learn more about ways to improve the prognosis and functioning of persons who are diagnosed with colorectal cancer in the future. What if we learn about new risks during the study? If we learn about any new risks related to your participation in the study, we will inform you immediately. Given the minimal risks in this study, this is unlikely. You may also stop participating in the study at any time. How will your privacy be protected? No subjects will be identified in any report or publication about this study. Although every effort will be made to keep research records private, there may be times when federal or state law requires the disclosure of such records, including personal information. This is very unlikely, but if disclosure is ever required, UNC-CH will take all steps allowable by law to protect the privacy of personal information. Records with identifying information are kept in locked cabinets separate from any questionnaire data you provide. Only staff who need this information for their day-to-day work duties will have access to it. Electronic records are encrypted and maintained on secure servers with password protection. Will you be paid for participating? Participants in this study receive $35: $15 following the telephone interview and $20 after the consent forms have been signed and returned. You will receive payment within two months of the date the telephone questionnaire is completed and the consents returned. If you decide in the future that you no longer want to participate, you will not be asked to return the money. Will it cost you anything to participate? The National Cancer Institute will pay for the costs of this research. This means that the sponsor is compensating the research team for conducting the study. The researchers do not, however, hold a direct financial interest in the sponsor. Who is sponsoring this study? K-10 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 This research is sponsored by the National Cancer Institute. This means the sponsor is paying the research team to conduct this study. The researchers do not, however, hold a direct financial interest in the sponsor or the outcome of the study. What if you want to stop before your part in the study is complete? You can withdraw from this study at any time without penalty by notifying the principal investigator of the study. The investigators also have the right to stop your participation at any time. This could be because the entire study has been stopped. What if you have questions about this study? You have the right to ask, and have answered, any questions you may have about this research. If you have further questions, you should call Dr. Robert Sandler at 919-966-0090 or Shelby Dunivant, Project Manager, at 1-888-819-4393 (toll-free). What if you have questions about your rights as a subject? This research has been reviewed and approved by the Committee on the Protection of the Rights of Human Subjects (Medical IRB) at the University of North Carolina at Chapel Hill. If you have any questions or concerns regarding your rights as a research subject, you may contact the Chairman of the Committee at (919) 966-1344. Subject’s Agreement: I have read the information provided above. I voluntarily agree to participate in this study. _____________________________ Signature of Research Subject ___________ Date ___________________________ Printed Name of Research Subject _____________________________ Signature of Person Obtaining Consent ___________ Date ___________________________ Printed Name of Person Obtaining Consent K-11 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 University of North Carolina-Chapel Hill Consent to Participate in a Research Study Participant (Surrogate Interviewed) Medical IRB Study #: 01-MED-390-ORC Consent Form Version Date: March 30, 2004 Title of Study: NC Colorectal Cancer Care Outcomes Research Study Sponsor: National Cancer Institute Principal Investigator: Robert S. Sandler, M.D., M.P.H. UNC-CH Department: Department of Medicine Phone number: 919-966-0090 ______________________________________________________________________________ You are being asked to take part in a research study. The investigator listed above is in charge of the study; other professional persons may help them or act for him. The name of this study is “Share Thoughts on Care”. What are some general things you should know about research studies? Research studies are designed to gain scientific knowledge that may help other people in the future. You may or may not receive any direct benefit from participating. There may also be risks associated with participating in research studies. Your participation is voluntary. You may refuse to participate, or may withdraw your consent to participate in any study at any time, and for any reason, without jeopardizing your future care at this institution or your relationship with your doctor. If you are a patient with an illness, you do not have to participate in research in order to receive treatment. Details about this particular study are discussed below. It is important that you understand this information so that you can decide in a free and informed manner whether you want to participate. You will be given a copy of this consent form. You are urged to ask the investigators named above, or staff members who may assist them, any questions you have about this study at any time. What is the purpose of this study? The purpose of this research study is to learn more about cancer care for people with colorectal cancer. We believe that the results of this study could identify ways to improve the life span and functioning of patients with cancer. We wish to learn how access to health care, differences in prescribed treatments, and differences in patients’ lifestyles may be related to disparities in clinical outcomes for people diagnosed with colorectal cancer. How many subjects will participate in this study? Approximately 1000 people who live in North Carolina and have colorectal cancer will take part in this study. All of the participants were identified through the N.C. Central Cancer Registry. In addition, approximately 9000 more people from around the United States will participate in the study at other research centers. How long will your participation last? Your participation in this study will last for about two years. What will happen if you take part in the study? K-12 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 There is no treatment involved in this study, and participating in the study will not affect your treatment in any way. If you decide to participate, you will be asked to identify a relative or friend who will complete a telephone interview on your behalf. It would be very helpful to the success of the research study if you allowed us to talk with one of your relatives or friends but you may still be a part of the study if you do not wish to do this. We will also ask for your permission to obtain a copy of your medical records (including Medicare claims, if relevant). We will request information related to your diagnosis and treatment of colorectal cancer as well as information about other diseases or conditions you might have. We will also ask your permission to obtain a sample of your tumor tissue from the hospital where you had surgery. After the researchers in our laboratory use a portion of this tissue, we will return it to the hospital. We will also ask you to donate a small sample of blood. This will be drawn at your doctor’s office or another convenient location. If there is any charge for this blood draw, you will not have to pay for it. Our study will cover all costs associated with the blood draw and shipment. About a year after the first telephone interview we might follow up with you to find out how you are doing. You may be contacted at other times during the course of the four-year study. Are there any reasons you should not participate? You should not participate in this study if do not wish to donate a blood sample or sign forms allowing access to your medical records and tumor blocks. What are the possible risks or discomforts? There is a minimal risk of loss of confidentiality although we will take every precaution to make sure this does not happen. When you have your blood drawn, you might experience some minor soreness or discoloration on your arm. What are the possible benefits? You will not receive any direct benefit from participating in the study. However, by taking part in this study, you may benefit from the knowledge that you have helped researchers learn more about ways to improve the prognosis and functioning of persons who are diagnosed with colorectal cancer in the future. What if we learn about new risks during the study? If we learn about any new risks related to your participation in the study, we will inform you immediately. Given the minimal risks in this study, this is unlikely. You may also stop participating in the study at any time. How will your privacy be protected? No subjects will be identified in any report or publication about this study. Although every effort will be made to keep research records private, there may be times when federal or state law requires the disclosure of such records, including personal information. This is very unlikely, but if disclosure is ever required, UNC-CH will take all steps allowable by law to protect the privacy of personal information. Records with identifying information are kept in locked cabinets separate from any questionnaire data you provide. Only staff who need this information for their day-to-day work duties will have access to it. Electronic records are encrypted and maintained on secure servers with password protection. Will you be paid for participating? K-13 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 Participants in this study receive $35: $15 for completing the telephone interview and $20 for signing and returning the consent forms. You will receive payment within two months of the date you enroll in the study and donate a blood sample. If you decide in the future that you no longer want to participate, you will not be asked to return the money. Will it cost you anything to participate? The National Cancer Institute will pay for the costs of this research. This means that the sponsor is compensating the research team for conducting the study. The researchers do not, however, hold a direct financial interest in the sponsor. What if you want to stop before your part in the study is complete? You can withdraw from this study at any time without penalty by notifying the principal investigator of the study. The investigators also have the right to stop your participation at any time. This could be because the entire study has been stopped. What if you have questions about this study? You have the right to ask, and have answered, any questions you may have about this research. If you have further questions, you should call Dr. Robert Sandler at 919-966-0090 or Shelby Dunivant, Project Manager, at 1-888-819-4393 (toll-free). What if you have questions about your rights as a subject? This research has been reviewed and approved by the Committee on the Protection of the Rights of Human Subjects (Medical IRB) at the University of North Carolina at Chapel Hill. If you have any questions or concerns regarding your rights as a research subject, you may contact the Chairman of the Committee at (919) 966-1344. Subject’s Agreement: I have read the information provided above. I voluntarily agree to participate in this study. _____________________________ Research Subject ___________ Date ___________________________ Signature of Printed Name of Research Subject _____________________________ ___________ ___________________________ Signature of Person Obtaining Consent Date Printed Name of Person Obtaining Consent K-14 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 University of North Carolina-Chapel Hill Consent to Participate in a Research Study Surrogate ______________________________________________________________________________ Medical IRB Study #: 01-MED-390-ORC Consent Form Version Date: March 30, 2004 Title of Study: NC Colorectal Cancer Care Outcomes Research Study Sponsor: National Cancer Institute Principal Investigator: Robert S. Sandler, M.D., M.P.H. UNC-CH Department: Department of Medicine Phone number: 919-966-0090 ______________________________________________________________________________ You are being asked to take part in a research study. The investigator listed above is in charge of the study; other professional persons may help him or act for him. The name of this study is “Share Thoughts on Care”. What are some general things you should know about research studies? Research studies are designed to gain scientific knowledge that may help other people in the future. You may or may not receive any direct benefit from participating. There may also be risks associated with participating in research studies. Your participation is voluntary. You may refuse to participate, or may withdraw your consent to participate in any study at any time, and for any reason. Details about this particular study are discussed below. It is important that you understand this information so that you can decide in a free and informed manner whether you want to participate. You will be given a copy of this consent form. You are urged to ask the investigators named above, or staff members who may assist them, any questions you have about this study at any time. What is the purpose of this study? The purpose of this research study is to learn more about cancer care for people with colorectal cancer. We believe that the results of this study could identify ways to improve the life span and functioning of patients with cancer. We wish to learn how access to health care, differences in prescribed treatments, and differences in patients’ lifestyles may be related to disparities in clinical outcomes for people diagnosed with colorectal cancer. How many subjects will participate in this study? Approximately 1000 people who live in North Carolina and have colorectal cancer will take part in this study. For the people who are unable to provide the information themselves, we are asking their family members or friends to provide the information for them. All of the patients were identified through the N.C. Central Cancer Registry. In addition, approximately 9000 more people from around the United States will participate in the study at other research centers. How long will your participation last? Your participation in this study will last for about two years. K-15 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 What will happen if you take part in the study? If you decide to participate, you will be asked to complete an interview over the telephone with a trained interviewer. The interview will last about one hour. The interviewer will ask you about your relative or friend’s medical history, how he/she was diagnosed with cancer, and what kind of treatment he/she may have received. You may skip any questions you do not wish to answer. Your interview might be audiotaped for quality control purposes. If your interview is taped, the interviewer will obtain your permission before the interview begins. If you choose to do so, you may refuse to have your interview audiotaped. We will also ask for permission to obtain a copy of your relative or friend’s medical records (including Medicare claims, if relevant). We will request information related to his/her diagnosis and treatment of colorectal cancer as well as information about other diseases or conditions. We will also ask permission to obtain a sample of your relative or friend’s tumor tissue from the hospital where he/she had surgery. After the researchers in our laboratory use a portion of this tissue, we will return it to the hospital. About a year after the first telephone interview we might follow up with you to find out how you are doing. At that time, you will be asked to complete a brief telephone interview and to sign updated consent forms granting permission for us to request your relative or friend’s medical records. You may be contacted at other times during the course of the four-year study. Are there any reasons you should not participate? You should not participate in this study if you do not wish to be interviewed over the telephone. What are the possible risks or discomforts? There is a minimal risk of discomfort answering questions about your relative or friend’s lifestyle or medical history. There is a minimal risk of loss of confidentiality, although we will take every precaution to make sure this does not happen. Your name and your friend or relative’s name will not be placed on the questionnaires. What are the possible benefits? You will not receive any direct benefit from participating in the study. However, by taking part in this study, you may benefit from the knowledge that you have helped researchers learn more about ways to improve the prognosis and functioning of persons who are diagnosed with colorectal cancer in the future. What if we learn about new risks during the study? If we learn about any new risks related to your participation in the study, we will inform you immediately. Given the minimal risks in this study, this is unlikely. You may also stop participating in the study at any time. How will your privacy be protected? No subjects will be identified in any report or publication about this study. Although every effort will be made to keep research records private, there may be times when federal or state law requires the disclosure of such records, including personal information. This is very unlikely, but if disclosure is ever required, UNC-CH will take all steps allowable by law to protect the privacy of personal information. Records with identifying information are kept in locked cabinets separate from any questionnaire data you provide. Only staff who need this information for their day-to-day work duties will have access to it. Electronic records are encrypted and maintained on secure servers with password protection. Will you be paid for participating? Participants in this study receive $35: $15 following the telephone interview and $20 after the consent forms have been signed and returned. You will receive payment within two months of the date the telephone K-16 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 questionnaire is completed and the consents returned. If you decide in the future that you no longer want to participate, you will not be asked to return the money. Will it cost you anything to participate? The National Cancer Institute will pay for the costs of this research. This means that the sponsor is compensating the research team for conducting the study. The researchers do not, however, hold a direct financial interest in the sponsor. Who is sponsoring this study? This research is sponsored by the National Cancer Institute. This means the sponsor is paying the research team to conduct this study. The researchers do not, however, hold a direct financial interest in the sponsor or the outcome of the study. What if you want to stop before your part in the study is complete? You can withdraw from this study at any time without penalty by notifying the principal investigator of the study. The investigators also have the right to stop your participation at any time. This could be because the entire study has been stopped. What if you have questions about this study? You have the right to ask, and have answered, any questions you may have about this research. If you have further questions, you should call Dr. Robert Sandler at 919-966-0090 or Shelby Dunivant, Project Manager, at 1-888-819-4393 (toll-free). What if you have questions about your rights as a subject? This research has been reviewed and approved by the Committee on the Protection of the Rights of Human Subjects (Medical IRB) at the University of North Carolina at Chapel Hill. If you have any questions or concerns regarding your rights as a research subject, you may contact the Chairman of the Committee at (919) 966-1344. Subject’s Agreement: I have read the information provided above. I voluntarily agree to participate in this study. _____________________________ Signature of Research Subject _____________________________ Signature of Person Obtaining Consent ___________ Date ___________________________ Printed Name ___________ Date ___________________________ Printed Name K-17 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 ADDENDUM TO CONSENT FORM FOR PARTICIPATING IN A RESEARCH STUDY HIPAA Authorization for use of Protected Health Information University of North Carolina at Chapel Hill __________________________________________________________________________ Title of Study: NC Colorectal Cancer Care Outcomes Research Study Medical IRB Study #: 01-MED-390-ORC Sponsor: National Cancer Institute Form Version Date: October 25, 2004 Principal Investigator: Robert Sandler, MD, MPH UNC-CH Department: Department of Medicine Mailing Address: 4111 Bioinformatics Building, CB 7555, Chapel Hill, NC 27599 __________________________________________________________________________ What is the purpose of this form? You have been asked to take part in a research study. The consent form for this study describes your participation, and that information still applies. This extra form is required by the federal “Health Insurance Portability and Accountability Act” (HIPAA). The purpose is to get your permission to use health information about you that is created by or used in connection with the research. If you are signing on behalf of someone other than yourself, this permission applies to that person’s health records. What if I don’t want my personal health information to be used in this research study? You may refuse to give this permission. A decision not to sign this form will not change your ability to get health care outside of this research study. However, you may not be able to participate in this research study unless you sign this permission form. You should discuss this, and any other questions, with the researchers. Who will be allowed to use my personal health information for this research? And why? The researcher named above and his assistants will be allowed to see and to use your health information for this research study. We may use it to check on your progress during the study, or analyze it along with information from all other subjects. Sometimes research information is shared with collaborators at other institutions. The researchers on this study work with a data processing center called RAND Corporation that will help with the collection and analysis of the data. What personal health information am I allowing to be used for this research study? The information we might use includes: your name, address, telephone number, date of birth, social security number, the information you provide during the interview, and the information we learn from analyzing your specimens. If you give us permission, we will also obtain your pathology reports and tumor tissue blocks that were used to diagnose your colorectal cancer. In addition, if you give us permission to look at your medical record, we will gather information about the tests done to diagnose your cancer and details about the treatments you have received. We will also collect information about other diseases or conditions you had at the time you were diagnosed with colorectal cancer. The research team for this study includes staff from the North Carolina Medical Review who will complete the medical record abstracts. Where will investigators go to find my personal health information? We may ask to see your personal information in records at hospitals where you have received care in the past, including but not limited to facilities in the UNC Health Care System. Based on what we know at this time, the places we will seek access to your records include all of the doctor’s offices, hospitals or clinics where you had appointments, procedures, or treatments for your colorectal cancer. K-18 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 What are the privacy protections for my health information used in this research study? The federal privacy regulations (HIPAA) apply to personal health information in the records of health care providers and other groups that share such information. There are some differences in how these regulations apply to research, as opposed to regular health care. One difference is that you may not be able to look at your own records that relate to this research study, at least until the study is over. The HIPAA privacy protections may no longer apply, once your personal health information has been shared with others who may be involved in this research. How long does this permission allow my personal health information to be used? If you decide to be in this research study, your permission to access and use your health information in this study will not expire, unless you revoke or cancel it. Otherwise, we will use your information as long as it is needed for the study. What if I change my mind after I give this permission? You have the right to cancel this permission to use your personal health information for research. In this case, we will not get any more of your health information for use in this research. However, canceling this authorization will not reverse uses of your personal health information that have already happened, or uses that have already been promised and cannot reasonably be reversed. If you want to cancel this permission, you must put this in writing and deliver to the Principal Investigator at the mailing address listed at the top of this form. You should clearly state that you want to cancel this permission to use your personal health information in this particular research study (attaching a copy of this form would be very helpful). SUBJECT’S AUTHORIZATION I have read the information provided above. By signing this form, I am giving permission for my personal health information to be used in research as described above. I will be given a copy of this authorization form after I have signed it. _________________________ __________________________ _______________ Printed Name of Research Subject (or authorized representative) Signature Date __________________________ __________________________ _______________ Printed Name of Person Signature Date Obtaining Authorization K-19 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 North Carolina Colorectal Cancer Care Outcomes Research Study HIPAA Authorization for Release of Protected Health Information for Patient Name: Date of Birth: I authorize my health care providers to release medical records about my colorectal cancer and any coexisting conditions to: Robert S. Sandler, M.D. and the Medical Review of North Carolina UNC Department of Medicine CB #7555, 4111 Bioinformatics Building University of North Carolina at Chapel Hill Chapel Hill, NC 27599-7080 Information to be released includes but not limited to: diagnostic and screening tests, surgery, radiation therapy, chemotherapy, reconstructive surgery, cancer staging, follow-up care, medications, reports for x-rays, scans or MRIs, laboratory tests, pathology reports, tumor tissue and slides, and health insurance information. If appropriate, I also grant permission to release information about my Medicare claims. Health Care Providers <<Provider 1 with Address>> <<Provider 2 with Address>> <<Provider 3 with Address>> Etc. I understand that this information will be used for the Cancer Care Outcomes Research Study. My participation in this study will be ongoing for three years. I authorize release of my records for three years after the date this form was signed. ___________________________________________ Signature of the patient or authorized representative ____________ Date ___________________________________________ Relationship of authorized representative to patient Study ID _________________ K-20 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 UNC-CH SCHOOL OF MEDICINE / UNC HOSPITALS INFORMATION ABOUT STORAGE AND USE OF SPECIMENS WITH IDENTIFYING INFORMATION This brochure provides information that may help you decide whether to allow some of your blood, tissue and/or body fluid (specimens) which will be collected as part of this research study to be stored and used for future medical research. WHAT WILL HAPPEN TO THE SPECIMEN? The specimens will be processed for storage, catalogued and placed in a secured facility at the UNC-CH School of Medicine, UNC Hospitals, or another site. All identifying information, including your name and medical record number, will be removed from the specimens. The specimens will be given a unique identifier (code). The researcher in this study and his/her associates will have access to the specimens and the code which links the specimens to you. WILL RESEARCH RECORDS AND PERSONAL INFORMATION BE KEPT PRIVATE? Although every effort will be made to keep research records private, there may be times when federal or state law requires the disclosure of those records, including personal information about you. When disclosure is required, the UNC School of Medicine and/or UNC Hospitals will take all steps allowable by law to protect the privacy of your personal information. IS THERE ANY COST FOR STORAGE OF THE SPECIMENS? There is no cost to you or your insurance company for the storage and use of the specimens. WHO OWNS THE SPECIMENS? By signing the consent form, you will donate the specimens for medical research purposes. Your donation does not entitle you to compensation from any commercial use of the products that may be derived from the specimens. HOW WILL THE SPECIMENS BE USED IN THE FUTURE? The research studies in which the specimens may be used have not yet been determined. The studies may involve genetic research. Genetic research is about finding the specific location of genes, learning how genes work, and developing treatments and cures for diseases which are genetically based. Before any research involving the specimens is conducted, a committee at the UNC School of Medicine called The Committee on the Protection of the Rights of Human Subjects will review and approve the research proposal. The Committee includes scientists and non-scientists, including community representatives. The purpose of the Committee is to assure that the interests of individuals participating in research studies are well protected. WILL RESEARCHERS SEEK CONSENT TO DO FUTURE STUDIES INVOLVING THE SPECIMENS? In some cases, the Committee may require that you be contacted and asked for your consent to participate in the specific research study in which the specimens will be used. You have the right not to participate in any research study for which your consent is sought. Refusal to participate will not jeopardize your medical care or result in loss of benefits to which you are entitled. WILL YOU RECEIVE STUDY RESULTS OF RESEARCH INVOLVING YOUR SPECIMENS? K-21 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 There may be times when the Committee will require that you be notified about the results of a research study in which your specimens were used. You have the right to be told of the results and their meaning, or to decide not to be told of those results, or to have the information sent directly to your personal physician. HOW WILL RESEARCHERS FIND YOU IN THE FUTURE? If you decide to allow the specimens to be stored and used in future medical research studies, you will be asked to provide your social security number. Your social security number will be used by the researchers and their associates in this study when it is necessary to contact you to seek your consent to participate in a specific research study or to notify you about the results of that study. If you allow your specimens to be stored with identifying information, you will be asked to choose, at the time you sign the consent form, a course of action that will be taken in the event that the researchers are unable to locate you in the future, even with your social security number. The options include allowing continued storage and use of your specimens with the identifying code remaining, continued storage and use of the specimens after removing the identifying code, and disposing of the specimens according to standard medical procedures. WILL THE SPECIMENS BE SHARED WITH OTHER INSTITUTIONS? The specimens may be shared with researchers from other institutions. Research studies may be conducted at several locations at the same time. No identifying personal information about you will be provided to researchers from other institutions who will use the specimens. HOW LONG WILL THE SPECIMENS BE STORED? The specimens will be stored indefinitely. Specimens may also be disposed of at any time at the discretion of the investigators, using standard medical procedures. If in the future you should decide that you no longer wish for the specimens to be stored, you may contact the researcher and/or his/her associates on the study in which you are participating. You may also contact The Committee on the Protection of the Rights of Human Subjects at (919) 966-1344 and request that the specimens be disposed of. K-22 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 University of North Carolina-Chapel Hill Consent For Storing Blood, Tissue or Body Fluid With Identifying Information _________________________________________________________________________________ Medical IRB Study #: 01-MED-390-ORC Consent Form Version Date: December 16, 2002 Title of Study: NC Colorectal Cancer Care Outcomes Research Study Principal Investigator: Robert S. Sandler, MD, MPH UNC-CH Department: Medicine Phone Number: 919-966-0090 Sponsor: National Institutes of Health You are asked to give permission for some of your blood, tissue or body fluid (collectively referred to as “specimens”) which will be collected in this research study to be stored for future medical research studies. The specimens will be stored at the UNC School of Medicine, UNC Hospitals, or another site. All identifying information including your name and medical record number will be removed from the specimens and replaced with a code. Dr. Sandler and his associates will have access to the specimens and the code which links the specimen to you. There is no cost to you or your insurance company for the storage and use of the specimens. Although every effort will be made to keep research records private, there may be times when federal or state law requires the disclosure of those records, including personal information about you. When disclosure is required, the UNC School of Medicine and/or UNC Hospitals will take all steps allowable by law to protect the privacy of your personal information. By signing this form, you will donate the specimens for medical research purposes. Your donation does not entitle you to compensation from any commercial use of the products that may be derived from the specimen. The research studies in which the specimens may be used have not yet been determined, but they may involve genetic research. Before any research involving the specimens is conducted, a committee at the UNC School of Medicine called The Committee on the Protection of the Rights of Human Subjects will review and approve the research proposal. In some cases, the Committee may require that you be contacted and asked for your consent to participate in the specific research study in which the specimens will be used. You have the right not to participate in any research study for which your consent is sought. Refusal to participate will not jeopardize your medical care or result in loss of benefits to which you are entitled. In other cases, the Committee may require that you be notified about the results of a research study in which the specimens were used. You have the right to be told the results and their meaning, or to decide not to be told of those results, or to have the information sent directly to your personal physician. You are asked to provide your social security number and agree that it may be used by Dr. Sandler and his associates if it necessary to contact you to ask your consent to participate in a specific research study or to notify you about the results of the study. The specimens may be shared with other institutions and research studies may be conducted at several locations at the same time. Non-identifying personal information about you will be provided to investigators from other institutions. K-23 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3, December 2005 If in the future you should decide that you no longer wish for the specimens to be stored, you may contact Dr. Sandler and/or his associates at The University of North Carolina at Chapel Hill at (919) 966-0090 or The Committee on the Protection of the Rights of Human Subjects at (919) 966-1344 and request that the specimens be disposed of according to standard medical research procedures. If you do not make such a request, the specimens will be stored indefinitely. They may be disposed of at any time at the discretion of the investigators. Before signing this consent form, please read the brochure entitled Information About Storage and Use of Specimens With Identifying Information that is designed to answer your questions. Please check which course of action is to be followed in case, even with your social security number, the investigators cannot find you after reasonable time and effort: _____I agree to allow the specimens to continue to be stored with identifying information, for as-yetundesignated purposes that may include genetic research. _____I request that the identifying code be removed from the specimens; after that is done, the specimens may continue to be stored and used for as-yet-undesignated purposes that may include genetic research. _____I request that the identifying code be removed from the specimens; after that is done the specimens may continue to be stored and used for as-yet-undesignated purposes NOT INCLUDING genetic research. _____I request that the specimens be disposed of. I consent to the donation and storage of the specimens, as described above. _______________________________________ Name of Subject _______________ Date _______________________________________ Social Security Number K-24 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3 December 2005 Appendix L: Physician Contact Information Worksheet [UNC DOES NOT SEND THESE FORMS TO STUDY PARTICIPANTS.] L- 1 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3 December 2005 In order to get the most accurate physician contact information possible, one of the enclosed physician contact information worksheet may be included in the post-interview mailing to study participants. The worksheet labeled PHYSICIAN CONTACT INFORMATION WORKSHEET—Interview Participants will be mailed to all participants who complete the brief telephone survey, or to surrogate respondents who complete a survey in lieu of the patient. The worksheet may be mailed to patients who complete a full survey if incomplete or inaccurate physician data was obtained during the interview. For patients who have given some information about physicians during their interview, that information will be printed on the worksheet. Only the relevant categories of physicians will be listed on the worksheets mailed to participants. The worksheet labeled PHYSICIAN CONTACT INFORMATION WORKSHEET—Interview NonParticipants is a worksheet for those patients from whom no information has been obtained. This blank worksheet gives the patient an opportunity to fill in all their physician information. L- 2 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3 December 2005 PHYSICIAN CONTACT INFORMATION WORKSHEET—Interview Participants PHYSICIAN LISTING Physicians From Whom We Plan To Obtain Your Medical Records In order to understand the treatment you received for your [FILL colon/ lung] problem, the research team must review your medical record. These medical records may be kept in several locations because your physicians have different office locations. Understanding who the physicians are and what their role in your [FILL colon/ lung] care was will help us locate the medical records that we need to review for this study. To review a copy of your confidential medical records from your physicians’ offices, we provide your physicians with a Medical Records Consent form that shows you approve of the research team confidentially reviewing your medical records as part of the research. Some physicians may ask for a signed medical records consent form with their name appearing on the form. In that case, we will send another form for you to sign with that physician’s name. Please list any additional physicians who do not appear on the attached blue physician list and who diagnosed or treated your [FILL colon/ lung] problem so we can contact your physicians about your medical records. Once you have completed the blue physician list, please return it along with the completed pink Medical Records Consent form in the pre-paid, self-addressed envelope provided. INSTRUCTIONS FOR PROVIDING MEDICAL RECORDS CONSENT 1) We ask you to review and correct the names, phone numbers and addresses of the physicians we have listed for you on the blue Physician List Form. Please write with a pen to correct any errors you see and to fill in any missing information that you can. 2) Next, please write the name of any other physicians who are not already listed on the blue Physician List Form and who you have seen for the diagnosis or treatment of your [FILL colon/ lung] problem. Please write the name, area code and phone number of these physicians, as well as the addresses or the places where your physicians treated you. 3) Complete the pink medical records consent form required for the research team to review your medical records. Thank you for your participation. L- 3 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Physician Role Physician Name Telephone Protocol 001 Amendment #3 December 2005 Facility Name Surgeon who performed your operation Medical oncologist who provided chemotherapy Radiation oncologist who delivered radiation therapy Physician most likely to know of symptoms or need for help (even if no or inadequate help provided) Hospital where stayed Surgeon consultant who did not operate Medical oncologist consultant who did not provide chemotherapy Radiation oncologist consultant who did not provide radiation therapy Physician responsible for referrals Physician most involved with decision-making Primary Care Physician Physician most likely to coordinate care during next six months L- 4 Street Address City ZIP “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Protocol 001 Amendment #3 December 2005 PHYSICIAN CONTACT INFORMATION WORKSHEET—Interview Non-Participants PHYSICIAN LISTING Physicians From Whom We Plan To Obtain Your Medical Records In order to understand the treatment you received for your [FILL colon/ lung] problem, the research team must review your medical record. These medical records may be kept in several locations because your physicians have different office locations. Understanding who your physicians are and their roles in your [FILL colon/ lung] care, will help us locate the medical records that we need to review for this study. To review a copy of your confidential medical records from your physicians’ offices, we will, with your permission, provide your physicians with a Medical Records Consent form that shows you approve of the research team confidentially reviewing your medical records as part of the research. Some physicians may ask for a signed medical records consent form with their name appearing on the form. In that case, we will send another form for you to sign with that physician’s name. Please list all of the physicians who diagnosed or treated your [FILL colon/ lung] problem so we can contact your physicians about your medical records. Once you have completed the attached blue physician list, please return it along with the completed pink Medical Records Consent form in the pre-paid, self-addressed envelope provided. INSTRUCTIONS FOR PROVIDING MEDICAL RECORDS CONSENT 1) Please clearly write the name of all the physicians you have seen for the diagnosis and / or treatment of your [FILL colon/ lung] problem on the blue Physician List Form. Please write the names, area codes and phone numbers of these physicians, as well as the addresses or the places where your Physicians treated you. 2) Complete the pink medical records consent form required for the research team to review your medical records. Thank you for your participation. L- 5 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Physician Name Telephone Protocol 001 Amendment #3, December 2005 Facility Name Street Address L- 6 City ZIP “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Amendment #3, December 2005 Appendix M: Provider Survey Protocol and Provider Survey M-1 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Amendment #3, December 2005 Cancer Care Outcomes Research and Surveillance Consortium (CanCORS) Protocol for Identifying Doctors and Survey Administration of the Provider Survey Primary Data Collection and Research (PDCR) Sites: University of Alabama at Birmingham UCLA/RAND Dana-Farber Cancer Institute/CRN Harvard Medical School/ Northern California Cancer Center University of Iowa University of North Carolina at Chapel Hill Veterans Affairs Health Services Research/Duke and University of Minnesota (VA) Provider Survey Implementation Committee Members Nancy Keating Anita Ambs Susan Baum Steven Clauser Bill Doucette Shelby Dunivant Bob Fletcher Mark Hornbrook Katherine Kahn Carrie Klabunde Mary Beth Landrum Selwyn Rogers Dana Sock Diana Tisnado M-2 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Amendment #3, December 2005 1.0 Summary This document outlines the procedures for fielding the provider survey that will serve as one of the data sources for the Share Thoughts on Care study, conducted by the Cancer Care Outcomes Research and Surveillance Consortium (CanCORS). The full Share Thoughts on Care study will entail obtaining data from patient surveys, patient medical records, surveys of physicians treating patients in the sample, and external data bases, such as the AMA Master File and Medicare/Medicaid claims data. This protocol describes the plans for sampling and survey administration only for the provider survey, and will not cover data collection from other sources, although the sampling will involve use of data collected in the patient survey. This document briefly outlines the design of the provider survey (Section 2), plans for identifying doctors to be surveyed (Section 3), plans for survey administration (Section 4), and mechanisms for data entry and transfer to the Statistical Coordinating Center (Section 5). The draft survey instruments are provided in the Appendix, as are copies of the cover letter to be included in the initial contact with providers in the sample, letters of support, and a sample data tracking sheet. 2.0 Design of the Provider Survey 2.1. Information to be collected The provider survey is designed to collect information that can only be obtained reliably from the provider. The survey consists of four primary domains: (1) physician beliefs about treatments, (2) physician practice style variables, (3) physician practice characteristics and financial arrangements, and (4) physician demographics. The survey also includes a question about physicians’ overall career satisfaction. To measure beliefs about treatments, physicians will be given brief vignettes and asked how strongly they would recommend particular treatments. Vignettes will describe decisions to use adjuvant chemotherapy and adjuvant radiotherapy for colorectal cancer, surgery for early-stage lung cancer, and chemotherapy for metastatic colorectal and lung cancer). To obtain information about physician practice styles, providers will be asked to what extent they typically manage certain elements of care for patients with lung or colorectal cancer themselves versus co-manage with or refer to other doctors. Elements of care include establishing goals for treatment and prognosis, assessing patient preferences for treatment, determining the first treatment modality, and evaluating and treating symptoms. The survey will also ask about factors limiting referrals and participation in multidisciplinary meetings. Finally, the survey will include questions about providers’ discussion of DNR status, end-of-life options, and use of hospice. These practice style variables describe how a physician interacts with patients and other practitioners, and can help explain cancer care choices. To measure physicians’ practice characteristics, the survey will include questions about practice type, size, and ownership; availability of various components of medical records; and the proportion of patients enrolled in managed care plans. To measure financial arrangements, the survey will inquire about base clinical income, bonuses and withholds, and factors that influence income. To measure physician demographics, the survey will collect information about each physician’s age, gender, year of graduation from medical school, specialty and training, board certification, race and ethnicity, fluency in languages other than English, involvement in teaching residents and students. M-3 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Amendment #3, December 2005 2.2. Instrument development To the extent possible, questions were derived from previously developed instruments. In some cases we have adapted these instruments to the particular characteristics of our population or because of the need to shorten the overall survey. In other cases, new questions were developed. A series of “at a glance” documents have been developed to identify the sources of questions in the surveys. The survey instruments underwent 2 rounds of cognitive testing by survey development staff at WESTAT, each followed by revisions to the instrument. The first round of cognitive testing took place in spring 2003 and included physicians that were recruited from the Washington, D.C. metropolitan area. Twelve physicians participated in interviews and provided feedback about specific questions. This was followed by revisions to the survey instrument. For the second round of cognitive testing, which took place during the summer of 2003, physicians were recruited from around the country, particularly from settings that were likely to be more representative of the PDCR areas. Sixteen physicians were mailed a survey and asked to complete the instrument and record the time taken. They then were interviewed by WESTAT. Following this round of testing, major revisions were made to the instrument to improve clarity and decrease the length of the survey. Questions were dropped if they were difficult to answer, were not likely to provide data with variation, or were of lower priority relative to the CanCORS synthesis document and analytic work plans. 2.3 Physicians to be surveyed The target population of the provider survey is physicians who have cared for patient participants in CanCORS. This population represents the physicians who are influential in the process and outcomes of care for colorectal and lung cancer patients within the catchment area of CanCORS. This population will primarily include medical oncologists, surgeons, radiation oncologists, pulmonologists, gasteroenterologists, and primary care physicians. Approximately 7881 CanCORS physicians will be surveyed (Table 1). The physicians to be surveyed will be identified from responses from the CanCORS patient survey (see section 3.1). Responses from the patient survey will identify physicians who have been involved in caring for the cancer patient, either as a surgeon, a chemotherapy provider, a radiation therapy provider, or as a provider important in referrals and/or caring for the patient’s symptoms. M-4 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Amendment #3, December 2005 Table 1. Expected number of physicians sampled per site Expected Sampling DFCI/ HMS/ UCLA/ Provider Role Iowa UAB Provider Type Rate CRN NCCC RAND 100% 44 315 207 49 106 Medical Oncology 100% 19 128 138 38 44 Physicians Radiation Oncology 100% -573 661 -302 involved in General Surgery primary 100% -26 33 -14 Colorectal Surgery treatments Thoracic Surgery 100% -137 153 40 69 -100% 84 ---Surgeons unspecified Decision to Generalistd 100% 354 340 340 340 238 refer lung pts to Pulmonology 100% 36 223 302 70 115 surgeona Decision to Generalistd 100% 36 43 43 -30 refer CRC pts to chemo Gastroenterology 100% 47 128 128 -89 providerb Symptom Generalistd 100% 161 170 170 85 119 Managementc 780 2081 2174 622 1127 Total # of Surveys 127 48 253 7 --- 84 42 ---102 All sites 932 457 1789 80 399 186 -- -- 1612 -- -- 746 43 33 227 128 78 597 85 67 856 690 406 7881 UNC VA a Assumes that 40% of lung patients will identify a pulmonologist as the physician most involved in decisions to refer the patient to a surgeon, 40% of patients will identify a generalist in this role, and the remaining 20% will identify a cancer specialist (medical or radiation oncologist). We have also assumed that approximately 100% of providers most involved in decisions to refer lung cancer patients to chemotherapy and radiation providers will have already be identified as either one of the cancer specialist or as the provider responsible for referral for surgery and thus few additional providers will be surveyed solely because of their role in referring lung cancer patients to either chemotherapy or radiation providers. b Assumes that 80% of CRC patients will identify another cancer specialist (primarily a surgeon) as the physician most involved in decisions to refer the patient to a chemotherapy provider and the remaining 20% of patients will identify a generalist (5%) or a gastroenterologists (15%) in this role. We have also assumed that approximately 100% of providers most involved in decisions to refer CRC cancer patients to radiation providers will have already be identified as either one of the cancer specialist or as the provider responsible for referral for chemotherapy and thus few additional providers will be surveyed solely because of their role in referring CRC cancer patients to radiation providers. We will not survey providers solely because of their involvement in the decision to refer CRC patients for surgery. c Assumes that 10% of lung cancer and CRC patients will identify a new generalist (ie not one involved in previously specified roles) as the provider most likely to know about their symptoms. d Includes generalists identified by the patient as being the physician filling appropriate role which may or may not by the physician that the patient identifies as his or her PCP. 3.0 Protocol for Identifying Doctors to be Surveyed 3.1 Identification of Key Providers The SCC will work with the provider survey group to implement an algorithm for identifying providers based on patients’ responses to the patient survey. The question numbers listed in this algorithm refer to specific questions in the patient baseline survey. Algorithm for identifying doctors at all sites (see below for details specific to the VA & CRN sites) 1) Physicians involved in discussions of treatment decisions and provision of treatments (mostly cancer specialists). Sample rate 100%. a) Physicians who discussed and/or provided surgical treatments i) If patient had surgery (question 3.1 = 1), then sample doc who performed surgery 3.4a [Note: current plan to sample first surgeon. Other surgeons under 3.4c] ii) If patients did not have surgery (question 3.1 ne 1) but is scheduled to have surgery (question 3.6 = 1 [are you scheduled to have surgery]), then sample doc 3.8a M-5 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Amendment #3, December 2005 iii) If patient did not have surgery (question 3.1 ne 1) and is not scheduled to have surgery (question 3.6 ne 1) but saw a surgeon (question 3.9 = 1 [did you ever see a surgeon, answered by those with no surgery]), then sample 3.10 iv) If patient did not have surgery (question 3.1 ne 1) and is not scheduled to have surgery (question 3.6 ne 1) and did not see a surgeon (question 3.9 ne 1), then sample doc 13.4 b) Physicians who discussed and/or provided chemotherapy i) If patient is receiving or has had chemo (question 5.1 = 1) or is scheduled to have chemo (question 5.4 = 1) then sample doc who is/will be treating (question 5.6) ii) If patient did not have chemo (question 5.1 ne 1) and is not scheduled to have chemo (question 5.4 ne 1) but has seen a chemotherapy doctor (question 5.7 = 1) then sample doc 5.8 iii) If patient did not have chemo (question 5.1 ne 1) and is not scheduled to have chemo (question 5.4 ne 1) and has not seen a chemotherapy doctor (question 5.7 ne 1) then sample doc 13.4 c) Physicians who discussed and/or provided radiation therapy i) If patient has had XRT (question 4.1 = 1) or is scheduled to have XRT (question 4.5 = 1) then sample doc who is/will be treating (question 4.7) ii) If patient did not have XRT (question 4.1 ne 1) and is not scheduled to have XRT (question 4.5 ne 1) but patient saw a radiation doctor (question 4.8 = 1) then sample radiation doctor (question 4.9) iii) If patient did not have XRT (question 4.1 ne 1), is not scheduled to have XRT (question 4.5 ne 1), and did not see a radiation doctor (question 4.8 ne 1) then sample doc 13.4 2) Physicians involved in decisions to refer lung patients to a surgeon. Sample rate 100%. [Note: Some of these providers will have been identified already.] a) If patient had surgery (question 3.1 = 1 [did you have surgery] then sample referring doc in 3.4b b) If patient did not have surgery (question 3.1 ne 1) but is scheduled to have surgery (question 3.6 = 1 [are you scheduled to have surgery]), then sample doc 3.8b c) If patient did not have surgery (question 3.1 ne 1) and is not scheduled to have surgery (question 3.6 ne 1) but saw a surgeon (question 3.9 = 1 [did you ever see a surgeon, answered by those with no surgery]), then sample 3.10a d) If patient did not have surgery (question 3.1 ne 1), is not scheduled to have surgery (question 3.6 ne 1) and did not see a surgeon (question 3.9 ne 1), then sample doc 13.4. 3) Physicians involved in decisions to refer colorectal patients to a surgeon. Sample rate 0%. No providers will be identified for this role. 4) Physicians involved in decisions to refer lung and colorectal patients to a chemotherapy provider. Sample rate 100%. [Note: Many of these providers will have been identified already.] a) If patient is receiving or has had chemo (question 5.1 = 1) or is scheduled to have chemo (question 5.4 = 1) then sample doc who referred to the chemotherapy provider (question 5.6a) b) If patient did not have chemo (question 5.1 ne 1) and is not scheduled to have chemo (question 5.4 ne 1) but has seen a chemotherapy doctor (question 5.7 = 1) then sample doc 5.8a c) If patient did not have chemo (question 5.1 ne 1) and is not scheduled to have chemo (question 5.4 ne 1), and has not seen a chemotherapy doctor (question 5.7 ne 1) then sample doc 13.4. M-6 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Amendment #3, December 2005 5) Providers involved in decisions to refer lung and colorectal patients to a radiation provider. Sample rate 100%. [Note: we expect almost all of these providers to already be identified in one of the above roles.] a) If patient has had XRT (question 4.1 = 1) or is scheduled to have XRT (question 4.5 = 1) then sample doc who referred to treating doc (question 4.7a) b) If patient did not have XRT (question 4.1 ne 1) and is not scheduled to have XRT (question 4.5 ne 1) but patient saw a radiation doctor (question 4.8 = 1) then sample radiation doctor (question 4.9a) c) If patient did not have XRT (question 4.1 ne 1), is not scheduled to have XRT (question 4.5 ne 1), and did not see a radiation doctor (question 4.8 ne 1) then sample doc 13.4. 6) Providers identified as the physician most likely to know that patient had a symptom. Sample 100%. [Note: we expect that most of these providers will have been already identified above.] a) Sample doc from question 9.2. 7) The medical record group is developing plans to identify KEY providers that were not named by patients but identified during medical record review. If a KEY provider is identified at the time of the medical record review for the same roles as above who has not already been surveyed, they will be surveyed at this later date, assuming that funds are available. Variation in above sampling algorithm for VA and CRN sites Because the VA and CRN sites have real-time access to electronic medical records, they may use these data to supplement data from the patient survey. For each doctor identified in the algorithm above, the sites will examine electronic medical records to verify that the doctor identified is the doctor who provided the care. Thus, their protocols will contain the following minor modifications: 1) If a patient names Dr. X, Dr. X will be surveyed. However, if the medical record clearly suggests that Dr. Y provided the relevant care, then Dr. Y will also be surveyed (in most cases, Dr. Y will have already been sampled based on another patient). 2) If the patient identifies Dr. X and Dr. X is a non-VA or non-CRN provider, and the record suggests that the patient received care outside of the VA, then Dr. X, the non-VA or nonCRN provider will be surveyed. Both sites will work hard to identify non-VA/non-CRN providers, including reviewing medical records and asking patients explicitly about out of VA/network care. 3) If Dr. X is implausible (i.e., patient says Dr. X did surgery, but Dr. X is a VA internist and Dr. Y is the surgeon of record), then Dr. Y will be surveyed. 4) If the patient can’t recall the doctor’s name, the medical record will be used to identify the doctor most likely to have filled the relevant role. Because of the large emphasis on physician training at the VA sites, patients at the VA site may be more likely to be cared for by trainees than at other sites. If a patient names a physician who is a trainee, the VA site will attempt to survey that physician. However, if (based on experience during the run-in phase of the study) the trainees cannot be located, then they will survey the trainee’s supervisor (who is responsible for signing all of the notes and is the official doctor of record and should be working closely with the trainee). [Note: The survey is designed as a physician survey. Some sites, particularly the VA, employ independently-practicing PAs and NPs. We expect that there will be few PAs and NPs identified, and they are likely to be working as primary care providers and not as providers of surgery, chemotherapy, or radiation therapy. When implementing the doctor identification algorithm, we will M-7 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Amendment #3, December 2005 specifically examine how often NPs or PAs are sampled. If it turns out that this is relatively frequent, the group will consider making some relatively minor changes the survey instrument to create an additional version of the instrument that would then be tested with a small sample of NPs or PAs.] 3.2 Algorithm to determine which version of the survey each identified doctor receives For each individual patient, the following algorithm will be used to determine which survey to send to each physician. 1) If doc 3.4a, 3.8a, or 3.10 sampled, they get surgeon survey 2) If doc 5.6 or doc 5.8 sampled, they get chemotherapy provider survey 3) If doc 4.7 or doc 4.9 sampled, they get radiation oncologist survey 4) If doc 3.4b, 3.8b, 3.10a, 5.6a, 5.8a, 4.7a, 4.9a, 13.4 or 9.2 sampled a) First check to make sure that this same doctor hasn’t already been identified by the patient (or by another patient) as doc 3.4a, 3.8a, 3.10, 5.6, 5.8, 4.7, or 4.9. If they have, send them the appropriate survey using #1-3 above. b) If the doc has not already been named in one of these other roles, and the patient is a colorectal cancer patient, send them the non-cancer specialist—GI survey. c) If the doc has not already been named in one of these other roles, and the patient is a lung cancer patient, send them the non-cancer specialist—lung survey. 5) If the doc has been named by another patient who has already been identified, decisions about which instrument they receive will depend on the timing and whether they have already been sent a survey. If they have not already been sent a survey, they will be sent the survey for the role that appears first in the following list: surgeon; chemotherapy provider; radiation therapy provider; non-cancer specialist (either lung or colorectal depending on which type of patients they have seen. If equal numbers of both, one will randomly be selected). If they have already been sent a survey, they will not be surveyed again. Once the providers for each patient have been identified, the average number of providers per patient with each condition will be calculated. Preliminary analyses will also assess how often the same provider is sampled for different patients and how well the algorithm works to identify the providers and determine the appropriate survey to be administered. In the course of the run-in, some docs were identified for whom the algorithm specified a version of the survey that was not necessarily the most appropriate. For example, a general internist received Version A; a medical oncologist received Version C. The group decided that we would ask each site to collect specialty information on the docs when verifying contact information. They will use specialty information to revise the version of the survey to be administered in certain situations, using the following algorithm. Algorithm: If primary specialty is general surgery or other surgical subspecialty (e.g., thoracic surgery)—physician should get version A If primary or secondary specialty is medical oncology, oncology, or hematology/oncology and primary specialty is not surgery or radiation oncology—physician should get version B If primary specialty is radiation oncology—physician should get version C. If primary or secondary specialties are not surgery or surgical subspecialty, physician should not get Version A. This algorithm will be revised as needed based on actual physicians at the sites. M-8 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Amendment #3, December 2005 3.3 Verifying Contact Information Each site’s CATI instrument will be pre-populated with lists of providers, identifying the provider name, address, city, phone number in separate fields. After the CATI is completed, before finalizing the survey data, the sites have the opportunity to update provider information from other files (state databases, AMA Masterfile, etc). The SCC is also working on a mechanism for the sites to correct the CATI information if they get better information at a later date. Sites will use the pre-populated datasets to get the most updated and current information on providers. When patient names a doc who is not in the pre-populated database, site will collect phone number. Site will call and verify doctor’s name and spelling, address, and specialty, adding this information to the pre-populated database. [Please see Appendix D for a draft script.] Sites will also reconcile any docs who may be the same at this time (i.e., Dr. Tom Jones and Dr. T. Jones). Sites can edit provider fields of CATI after survey complete. If a doctor identified has 2 addresses, site will flag (either using an ID or a new flag) to be sure that those docs can be identified. SCC will work out procedures for updating pre-populated databases and making sure SCC gets most current version of provider data. The SCC will apply the doctor identification algorithm to identify doctors from CATI by role. All sampling rates are 100% or 0% depending on role. The SCC will create lists that include: Provider name to establish the uniqueness of the provider. Name should include last and first, middle if possible. Provider address including suite number. Provider specialty type [Note: this should be in site’s pre-populated database. If not site could add this using other data sources (see below). This variable will be most helpful in trying to identify unique providers]. The SCC will look for identical duplicates in these lists. They will then send list of sampled providers to sites, along with a notation for which version of the survey that they should get. The sites will look for other likely duplicates including doctors with similar names (i.e., Dr. S. Jones and Dr. Sam Jones at same clinic) and doctors with the same name but different addresses (Dr. John Smith on Main Street and Dr. John Smith on Prospect Street. To verify provider contact information and/or obtain additional information, each PDCR site will rely on various databases. There are likely site-specific variations, but several useful strategies include: WebMD: www.webmd.com (free access) AMA databases that can be purchased. (The UCLA/RAND experience is that Web MD is more current.) ASCO (for medical oncology) and ASTRO (for radiation oncology) have hard copy or on-line directories that are available to members. The UCLA/RAND experience is that even most current hard copy documents are outdated; online password protected member-only files are most helpful. Despite these “look-ups”, some information will remain missing. To optimize respondents receiving the survey documents, sites will contact providers’ offices by phone to verify and update mailing, fax, phone information if the provider has been selected into the provider survey sample. M-9 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Amendment #3, December 2005 Additionally, it is likely that many offices will need to be contacted anyway so that the provider address information can be confirmed with respect to medical record accession. Prior to each wave of survey administration, each PDCR site will collect the following information about each provider: Name: last, first, middle Title Gender Patients associated with this provider Assumed specialty type and source of data for assumed specialty type Street address (number and street) City, State, Zip code Area code and phone number Fax number (specifically requesting the fax where medical record consent forms and surveys could be mailed). [Note: some offices have policies about surveys, and may not want to give out a fax number for the purpose of receiving a survey.] Email address where the URL link to the electronic version of the survey or a PDF version of the survey could be mailed. [Note: It may be possible or even preferable to obtain this information from alternate sources, such as ASCO, the American College of Surgeons, and other medical societies.] In cases where alternate databases are used to identify providers that are not already in the sites’ pre-populated databases, certain variables, such as age, gender, year of graduation from medical school, specialty, board certification, foreign medical status may be important to document. Such information will be useful in the event of survey non-response to compare respondents with nonrespondents. [Note: most of this information is already in the PDCR pre-populated databases. For example, the Iowa physician database contains: age, gender, year of med school graduation, specialty, board certification, foreign med school grad, among other variables.] Physicians who moved out of state. The goal to still try to track down these docs, esp. if they are key providers who care for more than one patient, because it would be very important to get their responses. We will continue to track this in the “limited sample” implementation to see how difficult it is to get contact info. In some ways these are not too different from those whose addresses we are unable to obtain. Addendum (8/2/05): Sites have identified a small number of doctors who have retired and have not been successful getting forwarding contact information or any surveys returned. The group has decided that this small group will not be eligible. However, docs who have moved will still be considered eligible. If no forwarding information is available, we will document the fact that no contact information is available, which will be useful in calculating response rates among those for whom we did and did not have contact information. Mental Health Providers. To be consistent with other decisions made in CanCORS, if a provider who was named is found to be a mental-health provider, they will not be surveyed. 3.4. Testing of doctor identification algorithm and verification of contact information In early spring, the SCC will test the doctor identification algorithm on CATI responses for 50 patients at each PDCR site. This test will be used primarily for de-bugging the algorithm. In addition, we will ask each PDCR site to verify contact information on these providers by calling the offices (some sites may have done this in real time when the patients were surveyed; they will not be asked to do this step again). M-10 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Amendment #3, December 2005 In late spring, just before the initial run-in survey administration (in May), the SCC will run the doctor identification algorithm on CATI responses for all patients surveyed thus far. This step will be used to revise estimates of the physician sample sizes for each site. 4.0 Survey Administration 4.1 Cover letter and letters of endorsement The cover letter will be co-signed by Dr. Andrew VonEschenbach, the director of the National Cancer Institute, and Dr. Harmon Eyre, medical director of the American Cancer Society. A copy of the cover letter is included in Appendix 1. These letters will not be photocopies. The letterhead will also include the Share Thoughts on Care logo. The cover letter and survey will be mailed with letters of endorsement that are matched for the expected recipient of each survey. For example, surveys mailed to surgeons will include a letter of endorsement from the American College of Surgeons, surveys mailed to chemotherapy providers will include a letter of endorsement from the American Society of Clinical Oncologists, surveys mailed to radiation oncology providers will include a letter of endorsement from the American Society of Therapeutic Radiology and Oncology, and surveys mailed to non-cancer specialists will include letters of endorsement from the American Gastroenterological Association as well as the American College of Physicians and the American Academy of Family Physicians. 4.2. Incentives For each survey, the initial mailing will include an incentive in the form of a $20 check. Some physicians may be contacted initially by email. In this case, the body of the email will include a brief message that mentions the survey, describes the attachments (cover letter, endorsement letter, printable copy of the survey), includes the URL to take the survey on-line, and notes that they will be receiving by U. S. Mail within the week a $20 check and a paper copy of the instrument. 4.3 Surveys administration procedures 4.3.1 Initial mailing The surveys that are mailed will be sent by priority mail to maximize the possibility that the physician will personally open them. A stamped, self-addressed envelope will be included in the packet in which to return the survey. A fax number will also be provided should the physician prefer to fax the survey back. When initial contact will occur via email, a direct link to the URL for the website, and information about the unique identifier and password to log in, will be included. In such case, the email message will include a brief message and the cover letter, endorsements, and survey instrument will be included as PDF attachments. A draft of the body of the email text is included in Appendix 3. 4.3.2 Unique identifiers Each survey will be coded with a unique identifier to be used to link providers with patients, for tracking of surveys, and to serve as a mechanism for identification of a particular case. For example, ID numbers can be used for quick identification of different factors associated with the case or administration. M-11 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Amendment #3, December 2005 4.3.3 Follow-up mailings and phone calls Three weeks after the initial mailing, a second mailing will be sent with a cover letter by first class mail to all nonresponders. Approximately two weeks after the second mailing, a phone call will be placed to the office of nonresponding physicians. A research assistant will verify that the instrument has been received, remind them to complete and return it, and offer to mail or fax another instrument to them. Sites will also use email when email addresses are available to remind physicians to complete the survey and will provide the link to the electronic version and offer to send another paper version. All contacts with the physicians or their office staff will be recorded in a contact database; up to 10 attempts will be made to reach the provider. If the provider is reached and refuses to do the survey, he/she will not be contacted further. The survey includes a question inquiring whether the provider would like to receive results of the study. If he/she responds affirmatively, a thank you letter and brief summary will be mailed after the data have been analyzed at the conclusion of the project. Sites will enter response status into a tracking database using status codes provided by the SCC. 4.4 Modes of survey administration The survey will be offered in 2 modes: a paper and pencil mode and a web-based mode. Medical offices will be called to verify the addresses of physicians to whom the survey will be administered. Office staff will be asked if the physician would prefer to receive the survey by e-mail. For those who are willing, initial contact will occur via email. The body of the email will include a brief message that mentions the survey, describes the attachments, includes a direct link to the URL for the website, and provides the unique identifier and password to log in. The email message will include as a PDF attachment the cover letter, endorsement letter, and survey instrument, should the provider prefer to answer the survey on paper and return it by US mail. The body of the email message will also note that the physician will receive a mailing within the week that includes a $20 check and a paper copy of the instrument. For those who do not provide an email address, the initial mailing will include a paper and pencil survey, but will also refer individuals to a URL where they can complete the survey via the web (after logging in with a unique identifier and password). The web survey will be hosted by the CanCORS SCC using the Cogix ViewsFlash web survey application. The application will allow physicians to complete part of the survey and log in again later to complete the rest. 4.5. Survey run-in, structured pause, full implementation phase with rolling survey design To test the mailing and follow up procedures, survey administration will begin in May of 2004 with a sample of 30 surveys. This initial wave of survey administration will then be followed by a structured pause (during July and August 2004) during which time the UNC CanCORS staff and the SCC will review the mailing and follow up procedures and make adjustments to the protocol as necessary. In mid-September, the first large wave of surveys will be administered. When ready for full implementation, a “limited sample” of docs will be identified from the first 50-100 patients. This can: allow for sites to work out larger scale logistics with smaller sample of patients than originally planned (which was to do surveys on docs of all patients identified to date) allow for some sites to use this to test additional contact strategies, incentives. Examples include: increase in incentive, mailing of the Ayanian et al JCO paper with packet M-12 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Amendment #3, December 2005 This wave will be followed by additional waves until the survey administration is completed. Sites may choose to mail small batches approximately weekly or larger batches at less frequent intervals, depending on the site’s workflow preferences. It is expected that the last wave of surveys will be mailed approximately 2 months after the completion of the patient surveys. 5.0 Data Entry and Transmission and Centralized Study Operations 5.1 Data Entry For web-based survey responses, data will go directly into the SCC database. For paper survey responses, data will be entered into a web version of the instrument specifically designed for data entry by PDCR site staff. Specifically identified PDCR data entry staff will be given unique logins and passwords to the web survey site to perform the data entry. Data will be double entered. More details about the data flow and data transfer procedures can be found in the document: “CanCORS Provider Survey Technical Design.” Data entry: specific rules for problem responses. 1. If the response for a text field is illegible, please enter “ILLEGIBLE” 2. If the response to a question requiring a number is a range (i.e., 60-90) please enter the average (i.e., 75) 3. When entering years, be sure to enter all 4 digits (i.e., 1975 not 75) 4. If someone enters <x or >x for a number (i.e., # patients cared for), enter x-1 for <x and x+1 for >x. 5. If ≥x or ≤ x, please enter x. 6. If fractions or decimals are added, please round up from .5 and greater; round down when < .5. 5.2 Data Quality Control Principal Investigators at each of the participating PDCR sites will be responsible for supervising the survey administration. All questionnaire responses will be entered into the database via the web-based program developed by the SCC at the PDCR. This database system is password protected and will have limited access. The SAS system will be used for initial tabulations of the questionnaire data and for analysis of times to complete the questionnaire, of completion rates overall and by strata, and for an exploratory analysis of item responses. These analyses will be conducted by CanCORS SAS programmers and statisticians at the SCC. Results of analyses will be posted for review on the secure CanCORS members web site with limited access to the provider survey implementation team members. 5.3 Data Confidentiality The following steps will be taken to maintain confidentiality: Surveys will be marked with a unique identifier to be used for tracking purposes and for linking physician survey responses with data collected from patients, who will also be identified only by a unique identifier Provider contact information and corresponding ID codes will be kept in a locked file cabinet in each of the PDCR sites. Any computerized information on provider contacts should be stored in restricted access, password protected files. The completed paper versions of the surveys will be stored in locked file drawers at PDCR sites. M-13 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Amendment #3, December 2005 All electronic data transfers regarding the survey and its administration (including the administration of the web survey itself) will be conducted through an encrypted secure channel (SSL) between the providers, the PDCR sites and the SCC. In particular, the web survey will be conducted using an SSL connection between the survey respondent's web browser and the SCC via the Cogix ViewsFlash application. No third party entity will host or maintain any part of the web survey. No protocols for any data exchange will occur without authentication using a combination of user name and password. After the successful completion of a web survey, the respondent's access to the SCC survey web site will be terminated and the respondent will no longer have access to the survey web site. The SCC provider survey web site will have a URL distinct and separate from the main CanCORS members web site. The SCC has obtained a Certificate of Confidentiality (NCI-02-007) from the National Institutes of Health to protect the privacy of participants. As is stated in the certificate, CanCORS investigators ”cannot be forced (for example, by court subpoena) to disclose information that may identify [a subject] in any federal, state, or local civil, criminal, administrative, legislative or other proceedings.” The certificate cannot be used to block the release of data voluntarily requested by a study participant. 6.0 Timeline See timeline in Appendix M5. M-14 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Amendment #3, December 2005 Appendix M1: Cover Letter and Follow-up Letter M-15 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Amendment #3, December 2005 Cover Letter Date name address address address Dear Dr. _______, We are writing to request your participation in the Share Thoughts on Care study, a national research study of the health care and outcomes for more than 10,000 cancer patients around the U.S. This study is jointly endorsed by the National Cancer Institute, the Department of Veterans Affairs, and the American Cancer Society. It is being conducted by a group of investigators at institutions across the U.S. (the Cancer Care Outcomes Research and Surveillance [CanCORS] Consortium) whose goal is to assess the health outcomes of patients with lung and colorectal cancer. Patients participating in the study have identified health care providers involved with their cancer care. We are surveying these providers to obtain their perspectives about management of cancer patients. We hope you will help us in this effort to better understand cancer care in the U.S. by completing the enclosed survey and returning it in the postage-paid envelope. Your participation in this study will directly influence its outcome and is, therefore, very important. The survey should take 10 to 15 minutes to complete. Your participation is entirely voluntary and, although we hope you will answer all of the questions, you may skip over any that you prefer not to answer. Your survey is labeled with a unique number that we will use to facilitate an additional mailing and telephone call to physicians who do not respond to this initial mailing, but your responses will not be linked to your name and will remain completely confidential. This number will also be used to link your responses with data collected from patients, who will also be identified only by a unique identifier. We will not ask you questions about care provided to any specific patients. No individual patients or providers will be identified in any of the analyses or reports from this study. If you prefer to complete the survey via the Internet, please go to www.cancors.org/provider/survey and enter your user id ______ and password ______. If you choose not to complete the survey, please return the blank survey in the envelope provided so that we can remove your name from our list. Thank you for participating in this important project. We have enclosed a check for $20 as a gesture of appreciation for your time. If you have any questions, please call Shelby Dunivant, Project Director, at 919843-9006 or toll-free at 1-888-819-4393. The human subjects committees at all participating institutions have approved the study. You can learn more about the CanCORS Consortium and the Share Thoughts on Care study at http://healthservices.cancer.gov/cancors/. Sincerely, Robert Sandler, M.D., M.P.H. Chief, Division of Gastroenterology & Hepatology University of North Carolina Andrew von Eschenbach, M.D. Director National Cancer Institute M-16 Harmon Eyre, M.D. Chief Medical Officer American Cancer Society “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Amendment #3, December 2005 Follow-up Letter Date name address address address Dear Dr. _______, Recently we wrote you to request your participation in the Share Thoughts on Care study, a national research study intended to contribute to our understanding of the health care and outcomes of patients with lung and colorectal cancer. This study is jointly endorsed by the National Cancer Institute, the Department of Veterans Affairs, and the American Cancer Society, and will enroll more that 10,000 cancer patients nationally. The patients participating in the study have identified physicians involved with their cancer care. We are surveying these physicians to obtain their perspectives on management of cancer patients. If you have already completed and returned the survey, we thank you, and you may disregard this letter. If you have not, we hope you will take approximately 10 to 15 minutes to complete the survey and return it in the enclosed postage-paid envelope. Your participation in this study is VERY IMPORTANT. Your response will ensure that we get a complete and accurate picture of all physicians’ opinions and practices. Your participation is entirely voluntary and, although we hope you will answer all of the questions, you may skip over any that you prefer not to answer. Your survey is labeled with a unique number that we will use only to follow-up with physicians who do not respond to this initial mailing. Your responses will never be linked to your name and will remain completely confidential. This number will also be used to link your responses with data collected from patients, who will also be identified only by a unique identifier. We will not ask you questions about any specific patients. No individual patients or physicians will be identified in any of the analyses or reports from this study. If you prefer to complete the survey via the Internet, please go to https://www.cancors.org/provider/survey and enter your User ID ______ and Password ______. If you choose not to complete the survey, please return the blank survey in the envelope provided so that we can remove your name from our list and spare you any more mailings. Thank you for participating in this important project. If you have any questions, please call Shelby Dunivant, Project Director, at 919-843-9006 or toll-free at 1-888-819-4393. The human subjects committees at all participating institutions have approved the study. You can learn more about the CanCORS Consortium and the Share Thoughts on Care study at http://healthservices.cancer.gov/cancors/. Sincerely, Robert Sandler, M.D., M.P.H. Chief, Division of Gastroenterology & Hepatology University of North Carolina Andrew von Eschenbach, M.D. Director National Cancer Institute M-17 Harmon Eyre, M.D. Chief Medical Officer American Cancer Society “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Appendix M2: Letters of Endorsement M-18 Amendment #3, December 2005 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Amendment #3, December 2005 Appendix M3: Text for body of email to be sent when e-mail is first means of contact M-19 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Amendment #3, December 2005 Email Text Dear Dr. _____, We are writing to request your participation in the Share Thoughts on Care study, a national research study of the health care and outcomes for more than 10,000 cancer patients around the U.S. Patients participating in the study have identified health care providers involved with their cancer care. We are surveying these providers to obtain their perspectives about management of cancer patients. Attached, please find a letter describing the study, a letter of endorsement from ____, and a copy of a survey instrument that can be printed, completed, and returned to the address on the last page. If you prefer to complete the survey over the Internet, please go to www.surveyurl.com and enter your username ______ and password ______. Within the next week, you will receive a check for $20 in the mail, as well as a paper version of the survey that you can complete if you prefer. We want to thank you in advance for your help with this important project. If you have questions, please contact Shelby Dunivant, Project Director, at 919-843-9006 or tollfree at 1-888-819-4393 or by email at dunivant@med.unc.edu. Sincerely, Robert Sandler, MD, MPH Professor of Medicine and Epidemiology University of North Carolina M-20 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Appendix M4: Sample tracking sheets M-21 Amendment #3, December 2005 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Amendment #3, December 2005 Sample Tracking Sheet 1 PROVIDER SURVEY PILOT WEEKLY REPORT SITE #_______ (each site currently has a # assigned to it for the CATI) Date ________ TOTAL TO DATE: Type of Survey Goal # sent med onc _____ _____ _____ _____ rad onc _____ _____ _____ _____ surg _____ _____ _____ _____ lung _____ _____ _____ _____ colorectal _____ _____ _____ _____ TOTAL _____ _____ _____ #completed via mail #completed via web M-22 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Amendment #3, December 2005 Sample Tracking Sheet 2 PROVIDER SURVEY PILOT CASE REPORT This page of the form only to be completed for each case after it is closed due to such things as the survey being completed and returned OR getting a request for no further contact, etc. 1. SITE #_______(each site currently has a # assigned to it for the CATI) 2. CASE #______ 3. SURVEY TYPE: ___ med onc ___ rad onc ___ surg ___ lung ___ colorectal 4. MAILINGS Date sent how sent (1st class, etc.) 1st mailing ___________ _________________ 2nd mailing ___________ _________________ If mailing returned due to incorrect contact info: Date of receipt _____________ 5. SITE-INITIATED FOLLOW-UP CALLS Call Date/time Length Made by Spoke with 1 ____/____ _____ __________ _________ 2 ____/____ _____ __________ _________ 3 ____/____ _____ __________ _________ 4 ____/____ _____ __________ _________ Outcome __________________________________ __________________________________ __________________________________ __________________________________ Office/physician requested survey to be mailed again: Office/physician requested survey to be faxed: ____ yes (date req’d_______) ____ yes (date req’d_______) ____ no ____ no Call length–approximate Made by—e.g. interviewer, med. student Spoke with—e.g. physician, office asst. Outcomes of calls—e.g. no answer, left message voice mail, left message secretary, office asst. to remind MD, request for no more contact & reason, refusal & reason 6. PHYSICIAN-INITIATED CALLS Date: ____ Spoke with: ____________ Reason for call: __________________________________ 7. FAXES Date of 1st fax: __________ Date of 2nd fax: __________ 8. EMAILS Date of 1st email: __________ Date of 2nd email: __________ Purpose: __________________________________ Purpose: __________________________________ Purpose – e.g. send copy of survey, respond to question, reminder 9. RETURNS Receipt date of returned survey: __________ Survey complete: ____ yes ____ no 10. INCENTIVES Date incentive sent: ______________ M-23 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Appendix M5: Timeline M-24 Amendment #3, December 2005 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Appendix M6. Survey Instruments Version A – Surgeon Version B – Radiologist Version C – Medical Oncologist Version D – CRC Specialist M-25 Amendment #3, December 2005 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Amendment #3, December 2005 Appendix N: Self-Administered Survey Protocol, Cover Letters and Questionnaire (Revised July 2005) N-1 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Amendment #3, December 2005 Self-Administered Survey Protocol The University of North Carolina at Chapel Hill July 27, 2005 Objectives To give participants who preferred a written survey to a telephone survey an opportunity to participate in the study To give participants who could not be reached by telephone before baseline interviews ended an opportunity to participate in the study To identify differences that may exist in responses given by telephone and on paper Survey Population Self-administered surveys will be mailed to patients whose diagnosis date occurred during the last six months of ascertainment (July 31, 2004 through January 31, 2005) in the following instances: a) If an interviewer was unable to speak with a patient after exhaustive efforts, and the patient was coded in CATI as non-responder/non-contact, a self-administered survey will be mailed to the potential participant. b) If an interviewer spoke to a patient and the patient refused to give a full or brief telephone interview or to name a surrogate, but agreed to complete a self-administered survey, a self-administered survey will be mailed to the potential participant. c) If a patient proactively asked about the possibility of a self-administered survey, a selfadministered survey will be mailed to the potential participant. Survey Procedures Eligible patients will be sent a packet including: a) A cover letter b) A self-administered questionnaire labeled only with a unique identification number c) A postage-paid addressed envelope to return the questionnaire d) A $15.00 incentive There will be no follow-up for non-responders. Data Transfer Procedures Returned questionnaires will be checked for any identifying information the respondent might have written in the margins. This information will be concealed with a permanent marker. A copy of the survey will then be made and filed in a locked cabinet at UNC that is accessible only to study personnel. The original survey will be sent by FedEx to the Statistical Coordinating Center in Boston for data entry and cleaning. The Statistical Coordinating Center will not have access to any patient identifying information. N-2 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Amendment #3, December 2005 Self-Administered Survey Letter to Contacted Participant July 27, 2005 Date Name Address City, State, Zip Dear Mr./Ms./Mrs. ____________________ Recently we spoke with you about taking part in a study called Share Thoughts on Care, a study designed to learn about the treatment of certain diseases of the colon. We hope to learn more about how people are treated for their disease, what influences the treatments they choose, and their experiences with care. Because your views and thoughts are important to this study, we are writing to ask you to fill out the enclosed survey. The survey usually takes about 20-30 minutes to complete. Your participation is voluntary and you may leave blank any questions you do not wish to answer. Your answers are confidential. Your answers will be grouped with those of other participants, and you will not be identified in any report or publication about this study. After we receive the survey, we will send forms for you to sign giving us permission to review your medical records about your colon problem. When you are finished with the survey, please return it in the enclosed postage-paid envelope. We have enclosed a check for $15.00 for your time and effort. If you have questions, you may call us toll-free at 1-888-819-4393. You may also contact the UNC Biomedical Institutional Review Board, which approved this study, at 1-919-966-1344 or at biomed_irb@unc.edu. We hope that you will take a few minutes to complete this survey. Thank you for your consideration. Sincerely, Robert S. Sandler, M.D., M.P.H. Professor of Medicine and Epidemiology Enclosures: Share Thoughts on Care Brochure Share Thoughts on Care Survey Postage-paid envelope Check for $15.00 N-3 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Amendment #3, December 2005 Self-Administered Survey Letter to Non-Contact July 27, 2005 Date Name Address City, State, Zip Dear Mr./Ms./Mrs. ____________________ We are writing to you about taking part in a study called Share Thoughts on Care, a study designed to learn about the treatment of certain diseases of the colon. We hope to learn more about how people are treated for their disease, what influences the treatments they choose, and their experiences with care. We were unable to reach you by telephone, but because your views and thoughts are important to this study, we are writing to ask you to fill out the enclosed survey. The survey usually takes about 20-30 minutes to complete. Your participation is voluntary and you may leave blank any questions you do not wish to answer. Your answers are confidential. Your answers will be grouped with those of other participants, and you will not be identified in any report or publication about this study. After we receive the survey, we will send forms for you to sign giving us permission to review your medical records about your colon problem. When you are finished with the survey, please return it in the enclosed postage-paid envelope. We have enclosed a check for $15.00 for your time and effort. If you have questions, you may call us toll-free at 1-888-819-4393. You may also contact the UNC Biomedical Institutional Review Board, which approved this study, at 1-919-966-1344 or at biomed_irb@unc.edu. We hope that you will take a few minutes to complete this survey. Thank you for your consideration. Sincerely, Robert S. Sandler, M.D., M.P.H. Professor of Medicine and Epidemiology Enclosures: Share Thoughts on Care Brochure Share Thoughts on Care Survey Postage-paid envelope Check for $15.00 N-4 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Amendment #3, December 2005 Self-Administered Survey Participant Consent Letter September 21, 2005 Date Name Address Address City, State Zip Dear Name, Please accept our sincere thanks for participating in the Share Thoughts on Care study. In addition to the information you shared in the survey, it would be very helpful if we could collect information from your medical records and get a sample of your blood and tumor. To do this we need your written permission. The following forms are enclosed: □ Two consent forms describing the study, how we will use the information you shared with us, and how to withdraw from the study if you choose to do so (pink) □ Consent for Storing Blood, Tissue, or Body Fluid and a brochure explaining storage and use of specimens (blue) □ Authorization for the release of medical records and specimens (yellow). Please check to make sure that all information is correct and that we have included all hospitals and clinics where you had tests, surgery or were treated for your cancer. There are white copies of each of the enclosed forms for you to keep for your records. Please read, sign and return the colored forms to us in the postage-paid envelope. We understand that these forms can be very confusing. The University of North Carolina requires that everyone who takes part in research studies sign forms like these to make sure your privacy is protected. If you have any questions, please call our office toll-free at 1-888-819-4393. Once we receive the forms, we will send you a second check for $20. Although the interviews will continue into the year 2006, we will be glad to send you a copy of the findings when they are available. Please contact us at 1-888-819-4393 (toll-free) if you would like to receive copies of the results. Again, thank you for your time and patience. With your help, we hope that our research will benefit others through an improved understanding of the best ways to provide treatment to people with colorectal cancer. Sincerely, Robert S. Sandler, M.D., M.P.H. Professor of Medicine and Epidemiology N-5 “Share Thoughts on Care”: A Population-based Study of Care and Outcomes in Lung and Colorectal Cancer Patients Amendment #3, December 2005 Appendix O: Medical Record Abstraction Instrument O-1