How to Manage a Dizzy Patient 1st October 2014 Programme Day 1
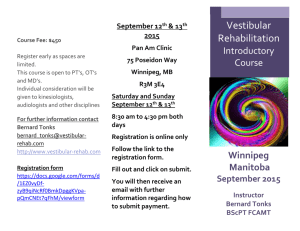
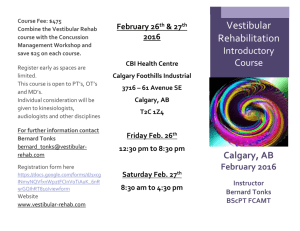
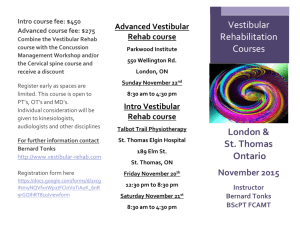
advertisement

How to Manage a Dizzy Patient 1st October 2014 Programme Day 1 9.00 - 9.30: Registration 9.30 -10.30: How do we stop feeling dizzy: Adaptation and compensation in the vestibular disordered patient. Professor Deepak Prasher Sudden unilateral loss of vestibular function sets off a series of symptoms which may include involuntary eye movements, postural instability, nausea and vomiting. Over time these symptoms spontaneously resolve and the person is able to resume most of their daily activities. This occurs as there is adaptation of the reflexes that are mediated by vestibular input; namely vestibule-ocular reflex (VOR), vestibulospinal reflex (VSR), vestibulocollic (VCR) and the cervico-ocular (COR) reflexes. It is the plasticity of the central nervous system which allows the brain to compensate for the loss of peripheral input and re-balance through adaptive control such that loss of input is no longer a detriment to postural stability. These will be discussed in the context of how patients stop feeling dizzy and some that do not compensate and what happens when decompensation occurs. 10.30-11.00 Psychogenic Aspects of Dizziness Dr. Richard Gans It is estimated that as many as 25% of patients with personality or psychiatric disorders will report symptoms of dizziness, vertigo, imbalance or spatial disorientation. The otolaryngology literature has also noted an increased prevalence of emotional, anxiety and panic associated co-morbidities with the “dizzy patient” population in clinical settings. These patients are often challenging for the busy clinician trying to identify and differentiate an organic from non-organic origin. This presentation will provide an overview of common personality disorders and the range of manifestations including: Migraine Anxiety Related Dizziness (MARD) Space and Motion Discomfort (SMD), Phobic Postural Vertigo, and Motor Conversion Disorders. Vestibular Rehabilitation Therapy (VRT) and Cognitive Behavioral Therapy (CBT) will be presented as useful management strategies. The presentation will be highlighted with videos of actual patients undergoing examination and treatment. Learning Objectives: At the conclusion of the presentation, participants will be able to … 1. Name three personality disorders commonly seen with psychogenic dizziness patients. 2. Differentiate history and symptoms of physiological versus psychogenic symptoms. 3. Discuss the role of VRT and CBT in the management of psychogenic dizziness. 11.00-11.15 Coffee Break 11.15-12.45 The mechanism of BPPV and treatment of BPPV Dr. Richard Gans Barany published the first report of BPPV in 1921, followed 50 years later, of course, by Dix and Hallpike (1951). Semont published one of the first papers on treating BPPV specifically with a physical maneuver in 1988. Since then, numerous investigators have reported varying levels of success with a variety of treatment protocols. Canalith Repositioning Maneuvers (CRM) is now universally recognized as the gold standard of treatment for BPPV. Despite this global acceptance, there is often a disconnect between the clinical and evidence-based science of BPPV treatment and what is actually practiced. This workshop will provide attendees with a historical and evidence-based review of the literature concerning its pathophysiology, variants, i.e. canalithiasis vs. cupulolithiasis, canal involvement, treatment methodologies and need for post-treatment restrictions, recurrence rates and other co-morbidities. The presentation will be followed by a “hand-on” laboratory session to facilitate the demonstration and practice of the preferred treatment maneuvers facilitating patient safety and comfort. Learning Objectives: At the conclusion of the presentation, participants will be able to … 1. Explain the conditions and co-morbidities, which facilitate macula degeneration and otoconia displacement including absorption issues. 2. Describe the preferred methods of modified positioning maneuvers to test specific semicircular canals. 3. Name and discuss the three primary complications of CRM. 4. Demonstrate Canalith Repositioning Maneuvers to treat all variants and canals. 12.45-13.45 Lunch Break 13.45-15.00 BPPV assessment and management practical Dr. Richard Gans The techniques for BPPV assessment and management will be demonstrated practically. 15.00- 15.30 Coffee Break 15.30- 16.30 Continuation of Practical 18.00: Evening Dinner: A chance to network with other members of the seminar as well as the lecturers Day 2 9.00-10.00 How to use adaptation, substitution and habituation techniques in unilateral vestibular dysfunction, bilateral vestibular dysfunction, visual vertigo, and multifactor etiological cases. Dr. Nicola Topass Each patient is an individual, but broadly speak you are able to characterise them into categories based on their history, functional complaints and vestibular diagnostic test results. Vestibular rehabilitation patients can broadly be characterised into many treatment groups, but the four most common that will be discussed include: unilateral vestibular dysfunction (stable versus unstable), bilateral vestibular hypofunction, visual vertigo, and multifactor etiological cases. This section will look at which techniques are appropriate for which categories of patients. 10.00- 10.45 How to create an individualized treatment plan Dr. Nicola Topass This section will look at how to individualize a treatment plan to the needs of your patient. It would look at how to customize exercises within the technique category of adaptation, substitutions and habituation. It will address techniques such as pacing and self monitoring to ensure that the therapy program, exercises and level is set appropriately. It also teaches simplistic counselling techniques which are the corner stone of any successful vestibular rehabilitation program. Delegates are made aware of the differences of personal adjustment counselling versus informational counselling and how these techniques can be employed by an audiologist. 10.45-11.00 Coffee Break 11.00- 11.45 How to optimise your therapy, beyond the use of physical exercises: use of bibliotherapy, goal setting, and motivation counselling in individualised therapy Dr. Nicola Topass For any vestibular rehabilitation program to be successful it is important that the patient be motivated. A non-motivated patient will never improve no matter how much time or expertise is employed by the clinician. As such it is important to assess the motivation of the patient, be it via a simple conversation or by formally completing a motivation questionnaire such as the Multidimensional Health Locus of Control (MHLC) Scale. You are also shown how to incorporate the LINE, BOX and Circle motivational counselling tools into your therapeutic practise. Once a patient is motivated then goals setting can be discussed. It is important for the patient to have realistic goals or they set themselves up for failure, this is another corner stone concept for successful treatment. It is important that the clinician is able to listen to the patient and formulate appropriate goals with them. Studies have shown that patients only remember a small amount of what is actually said in any clinical interaction, and that is based on them having normal hearing. Thus our patients with balance and often hearing problems would remember even less. Thus it is important that all information is documented appropriately and that patients are directed to ‘safe’ internet sites for further reading to further understand their condition. 11.45-12.30 Support groups for successful treatment of vestibular patients Ms. Natasha Harrington-Benton Director, Ménière’s Society Synopsis “When I was diagnosed with Ménière's I felt completely abandoned. Nobody told me of your Society and I felt lost…after searching the internet I have found you, and just to know that someone understands and I am not alone has made a world of difference.” The Meniere’s Society is the only UK registered charity dedicated solely to supporting people with dizziness and imbalance from vestibular disorders. The Society offers support at all stages of a person’s condition. For those who are newly diagnosed and want help locating a health professional who specialises in vestibular disorders, through to those in the later stages of the condition or if their symptoms have returned after a period of remission. Peer support, whether one-to-one, in a group, by telephone or online, plays an important part in the management of vestibular disorders and is often a valuable tool. The Ménière’s Society can give support and information and put people in contact with others facing the same problems. Knowing they are not alone and others share their concerns can be an enormous help to them in the management of their symptoms. Ménière’s Society The Ménière’s Society is a UK registered charity dedicated to supporting people with dizziness and balance problems caused by vestibular disorders. The Society provides information to patients and those who care for them, health professionals and the general public. Members are from all over the UK, with a small number overseas. With over 25 years experience providing information to those affected by vestibular disorders, the Ménière’s Society helps people source specialists in their local area, publishes a quarterly magazine, Spin, and factsheets on a variety of subjects (e.g. driving, surgery and vestibular rehabilitation), as well as providing a telephone information line during working hours. For health professionals, the Society offers information and support for their patients, we are able to supply booklets on vestibular rehabilitation and provide a list of ENT and vestibular rehabilitation specialists; useful if referring a patient for further testing and treatment. The Society maintains an active relationship with interested clinicians and researchers and, where funds allow, funds vital research into vestibular disorders. 12.30-13.30 Lunch Break 13.30-15.00: How to use bedside tests to identify treatment goals and also use them to identify progress with therapy plans. Putting key elements of a vestibular rehabilitation plan into practice with practical hands on session. Dr. Nicola Topass Bedside tests can be used as objective measures to assess uncompensated vestibular lesions. Post-head shake nystagmus is able to identify if there is tonic asymmetry at the level of the vestibular nuclei, hence depicting a centrally uncompensated lesion. The Fukuda stepping test evaluates the vestibular spinal reflex and thus gives insight into how the vestibular system is affect postural stability. Dynamic visual acuity is a measure of the VOR, and gives insight into how vision with head movement may be affected due to the vestibular deficit. The Motion Sensitivity Quotient can be employed to quantify the degree of motion sensitivity the patient is experiencing, but this can take a long time to employ in a busy clinic. Thus a version of the MSQ is used in clinic, which is base on the psychological ‘pacing technique’. All of these measures would initially identify the uncompensated lesion and how it affects various reflex systems which are dependent on vestibular input. They would also change as the patient compensates, hence improves as a measure of vestibular rehabilitation. The Fukuda would give insight for the need for stability exercises; the DVA would identify the need for Herman VOR exercises, and the modified symptoms scale would identify the need for habituation exercises such as the Cawthorne-Cooksey exercises. These tests will be demonstrated in a practical session. It will be shown how to use these tests to identify, implement and modify an exercise program. 15.00-15.30 Coffee Break 15.30- 17.00 Continuation of practical session Day 3 9.30-10.00 How to assess the value of therapy: use of outcome measures Ms. Danielle Howard and Ms. Joanne Rhodes-Brown The only way to ensure that the service you are providing your patients is beneficial is to measure that benefit. If you don’t measure it, it does not exist. There are two types of assessing benefit, namely by subjective assessment and by objective assessment. Subjective assessment can take place in the form of questionnaire assessment. There are several different outcome measurements available for vestibular rehabilitation from the more general SF 36 Health questionnaire to the more disease specific such as the Dizziness Handicap Inventory, Vertigo Symptom Scale and the Vestibular Rehabilitation Benefit Questionnaire. This section will focus on the VRBQ as it is a questionnaire that provides psychometrics. It is thus able to identify how much of a change pre-post therapy would be considered as a significant change due to the intervention offered. Objective assessment can be in the form of assessing postural sway. An example of an objective measure of postural sway is the EquiTest system by Neurocom. It enables the clinician to assess the increase in postural stability, decreased sway and increased limits of stability as the patient improves with the vestibular rehabilitation program. 10.00- 10.30 VR case studies form a Physiotherapy Perspective Ms. Michelle Dawson Michelle is going to present a variety of case studies of patients who have undergone vestibular rehabilitation with a physiotherapy bias. Michelle is part of the vestibular rehabilitation MDT and was kindly invited to attend last year’s excellent study day and would highly recommend this informative study day. 10.30-10.45 The Vestibular Rehabilitation process from the patient’s point of TBC 10.45- 11.15 Coffee 11.15-12.00 Case Studies 12.00 -13.00 Lunch 13.00-13.45 How to manage the anxious and depressed patient and employ pacing and communication strategies. The use of psychological techniques in treating VR patients. Sarah Whitaker (Clinical Psychologist) Anxiety and depression are closely linked with many chronic conditions, it is thus no surprise that patient with vestibular disorders often have anxiety and depression. Stress, anxiety and depression are closely linked and can enhance dizzy symptoms and thus intern enhance the stress, anxiety and depression. It is a vicious cycle that can perpetuate itself and end in the patient being withdrawn from society. If the patient is in this anxiety state their ability to centrally compensation to their vestibular disorder is vastly diminished and they do not progress with their program. It is thus important that these patients be identified early and appropriate intervention is offered. This section will discuss how to identify these patients and the therapy programs that are currently offered for patient who have been identified. 13.45-14.00 Coffee Break 14.00- 17.00 Innovations in Cognitive Behavioural Therapy in Vestibular Rehabilitation Sarah Whitaker (Clinical Psychologist) This session aims to cover 1) Working pragmatically with the biology and psychology of anxiety, low mood and Vestibular Rehabilitation disorders. Identifying how avoidance plays a role in increasing symptoms and how approaching symptoms can be a more workable way forwards. 2) Working to help people change their relationship with their thoughts. Identify and helpfully work with thoughts that get in the way of engagement with rehabilitation and life 3) Spotting patterns in body and behaviour that feed vicious cycles of avoidance and increase symptoms 4) Doing what matters and helping people to learn to take the symptoms with them and live alongside them Outcomes for 3 day training: Upon completion of the course, participants should be able to: Moving away from aiming to cure symptoms to developing skills to help people live with symptoms that won't go away Helpfully be able to work with thoughts that get in the way Understand how to develop a values based activity management schedule for therapy Understand how to develop an ‘activity management schedule’ for therapy. Understand how motivational interviewing and how this relates to ‘Change Talk’ Name three personality disorders commonly seen with psychogenic dizziness patients. Differentiate history and symptoms of physiological versus psychogenic symptoms. Understand the concepts behind vestibular reflex pathway adaptation and central compensation Identify the canal and side involved with BPPV and treat the patient appropriately Know how to classify a patient into treatment categories and how to identify exercises types based on categories Understand how to use bibliotherapy, goal assessment, and motivation in your vestibular rehabilitation program Understand the patient’s journey through the vestibular rehabilitation process Understand the importance of outcome measures and how they influence your therapy program Understand how to employ ‘psychological pacing’ to your treatment programs Understand how patient’s different ‘communication styles’ can affect their treatment outcomes