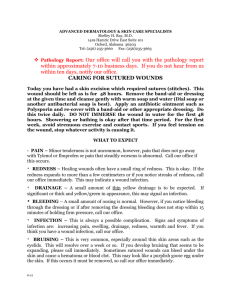
Wound Care Policy 2012-2014
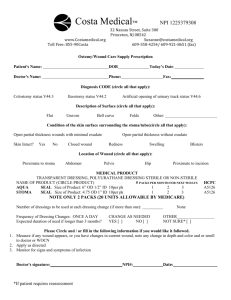
advertisement

2012 - 2014 BARNSLEY WOUND CARE POLICY FOR THE PREVENTION AND MANAGEMENT OF PRESSURE DAMAGE & TREATMENT & MANAGEMENT OF ALL WOUNDS CONTROLLED DOCUMENT 1 LEAD: LYNNE HEPWORTH DATE: Sept 2012 TISSUE VIABILITY NURSE SPECIALIST SWYPFT REVIEW DATE: Sept 2014 INTRODUCTION - Why Have A District Policy? PART I - Prevention of Pressure Damage 1.1 Multi-Disciplinary Approach 1.1.1 1.1.2 1.1.3 1.1.4 1.1.5 1.1.6 1.1.7 Role of the Nurse Role of the Hospital Doctor Role of the General Practitioner Role of the Physiotherapist Role of the Occupational Therapist Role of the Pharmacist Role to the Dietician 1.2 Education and Training 1.3 Mattress Replacement 1.4 Linen for Patient Use 1.5 Equipment 1.6 Assessment of the Patient’s Risk 1.7 Risk Assessment Tools in use in Barnsley 1.7.1 Norton Score 1.7.2 Waterlow Risk Assessment 1.7.3 Modified Andersen Score 1.8 2 Action for “At Risk” Patients PART 2 - Management of Pressure Damage 2.1 Wound Assessment and Management 2.1.1 2.1.2 2.1.3 2.1.4 2.1.5 2.1.6 2.1.7 2.1.8 2.2 Patient Assessment General Assessment of the Patient Assessment and Routine Investigations Wound Assessment Dressing Assessment Fluid filled blisters Completing incident reports (Datrix) Wound Assessment Flow Chart Treatment Protocols and Formulary 2.2.1 Using the Formulary 2.2.2 Wound Management Formulary Protocols 1 & 2 Protocols 3 & 4 Protocols 5 & 6 Protocols 7 & 8 Protocol 9 2.3 Factors affecting Healing 2.3.1 Systemic Infection 2.3.2 Diabetes 2.3.3 Carcinoma 2.3.4 Anaemia 2.3.5 Poor Nutritional State 2.3.6 Reduce Immunity 2.3.7 Poor Circulation 2.3.8 Wound Contaminated by Impacted Material 2.3.9 Position of the Wound 2.3.10 Local Infection of Wound 2.4 3 Medical and Surgical Measures 2.5 Transporting Patients 2.5.1 2.5.2 2.5.3 2.5.4 2.5.5 2.5.6 2.5.7 Internal Transportation of Patients Mode of Transport Minimising Delays External Transportation of Patients Patients requiring Stretcher Overlays Action by Ambulance Crew Handover – Continuity of Care 2.6 Medical & Surgical Measures 2.7 Transporting Patients 2.7.1 2.7.2 2.7.3 2.7.4 2.7.5 2.7.6 2.7.7 Internal transportation of patients Mode of transport Minimising delays External transport of patients Patients requiring stretcher overlays Action by ambulance crew Handing over continuity of care 2.8 Discharge and Transfer 2.9 Monitoring Information 2.9.1 Prevalence Monitoring Information 2.9.2 Incidence Monitoring Information 2.9.3 Prevalence and Incident Monitoring Returns 4 PART 3 - Policies For Specialist Areas 3.1 Ambulance Services 3.1.1 3.1.2 3.1.3 3.1.4 3.1.5 3.2 Accident and Emergency Department 3.2.1 3.2.2 3.2.3 3.2.4 3.2.5 3.2.6 3.2.7 3.2.8 3.2.9 5 Education and Training Equipment Assessment of the Patient’s Risk Transferring Patients General Prevention Measures Assessment Equipment Trolley Patients Incontinence Specific Nursing Action Transfer/Liaison with Other Departments Wards Transfer to Other Hospitals / Nursing Homes Staff Training / Induction 3.3 Operating Theatres 3.4 X-ray and Departments 3.5 Patients with Spinal Injuries PART 4 - Leg Ulcer Guidelines 4.1 Treatment for Venous Leg Ulcers 4.1.1 4.1.2 4.1.3 4.1.4 4.1.5 4.1.6 4.2 Medical History Limb Assessment Doppler Pain Control After Care Leg Ulcer Assessment Form Compression Therapy 4.2.1 4.2.2 4.2.3 4.2.4 4-Layer Bandage System Reduced Compression Bandage Types Compression Hosiery 4.3 Leg Ulcer Referral Route 4.4 Differential Diagnosis 4.5 General Advice Leaflet 4.6 Advice for Healed Leg Ulcers PART 5 – Skin Tears 5.1 Definition 5.2 Risk Factors 5.3 Common Precipitating Causes 5.4 Dressings APPENDICES Appendix 1 30° Tilt – A Pressure Relieving Position Appendix 2 Basic Care Guide for Patients Undergoing Long Ambulance Journeys Appendix 3 Pain Control Charts Appendix 4 Guide to Equipment Selection Flow Charts Appendix 5 Nutrition and Pressure Damage Appendix 6 Wound Assessment Chart 6 INTRODUCTION 7 INTRODUCTION WHY HAVE A DISTRICT POLICY? The purpose of this manual is to set out, in one document, a policy for the prevention and prevention of pressure damage and management of all wounds that is based on evidence based practice and draws together the expertise and best practice from the health services and care homes within Barnsley. One of the first steps in the implementation of the policy was the formation of a Wound Care Advisory Group. This continuing group consists of representation from primary and secondary care providing health services within Barnsley and the private sector. The Wound Care Advisory Group is responsible for ensuring that a co-ordinated and systematic approach exists across the district to wound care and for developing, monitoring and evaluating the policy. Group members will act as a resource person for their Trust, speciality or sphere of work. They are responsible for ensuring that all the information is disseminated throughout their organisation. It will be necessary for each unit that delivers patient care, to form a multi-disciplinary subgroup or other appropriate mechanism that will take responsibility for the following areas: Ensuring the necessary structures are in place to implement the policy Developing local procedures, training packages and standards, within the framework of the District Policy Implementation of the policy Monitoring and evaluating local performance against the standards set Evaluating the proposals of the advisory group for implementation within their unit Providing, to their unit, a network of information, education, support and advice The effective development and implementation of the Wound Care Policy is a catalyst for change, raising standards, developing practice and optimising patient care. Throughout this manual and the policies within them, the term unit refers to a Trust, Care Home, Ambulance Service or other deliverer of health care services. PART I PREVENTION OF PRESSURE DAMAGE 1.1. Multi-Disciplinary Approach 1.1.1 1.1.2 1.1.3 1.1.4 1.1.5 1.1.6 1.1.7 Role of the Nurse Role of the Hospital Doctor Role of the General Practitioner Role of the Physiotherapist Role of the Occupational Therapist Role of the Pharmacist Role of the Dietician 1.2. Education and Training 1.3. Mattress Replacement 1.4. Linen for Patient Use 1.5. Equipment 1.6. Assessment of the Patient’s Risk 1.7. Risk Assessment Tools in use in Barnsley 1.7.1 1.7.2 1.7.3 1.8. Norton Score Waterlow Risk Assessment Modified Andersen Score Action for “At Risk” Patients PREVENTION OF PRESSURE DAMAGE 1.1 Multi-Disciplinary Approach The prevention and management of pressure damage requires a multi-disciplinary and holistic approach to patient care. Though in the past, pressure ulcers have been seen as the domain (and responsibility when they develop) of the nursing profession, today it is increasingly acknowledged that the many factors involved in the development of a pressure ulcer cannot be addressed by good nursing care alone. The contribution of all disciplines is mentioned frequently throughout this policy. A multi-disciplinary approach to pressure damage requires three things if it is going to work: Firstly, multi-disciplinary team members need to acknowledge that pressure ulcers cannot be prevented or treated by nursing care alone; it is a shared problem with a shared solution. This is a perception that is becoming increasingly uncommon as demonstrated by the sections that follow later, each written by the relevant health care professional about their role. Secondly, nurses traditionally involved to the exclusion of all others, need to recognise the valuable contributions to be made by their non-nursing colleagues by bringing appropriate patients to their attention. And thirdly, a co-ordinator is required, who can ensure continuity of care and can monitor the effect of the prevention and/or treatment plan. 1.1.1 Role of the Nurse The nurse has a focal role in co-ordinating the care required to prevent and/or treat pressure damage. Aspects of this care are covered in detail throughout this Policy, from the initial assessment of risk to discharge, and it is not intended to list them all again here. It is, however, worthwhile to emphasise here, the importance of the nurse’s role as co-ordinator, particularly for patients in the community – own home or nursing/residential home – who do not have the same access to non-nursing care, as do patients in hospital. 10 1.1.2 Role of the Hospital Doctor The role of a doctor in prevention of pressure ulcers is mainly two fold: Identification of all the “at risk” groups of patients, for example people with neurological disease, e.g. CVA, cord-injury, motor neurone disease, very ill patients, patients with symptomatic disease and with poor mobility, incontinent patients. These should have anti-pressure protection started immediately (high risk foam mattress and 30 degree tilt). To identify and treat underlying medical problems vigorously that affect the wound healing process: - Prescribing appropriate treatments e.g. Vitamin supplements, Vasodilators, Recommended wound treatments (per policy document) - Maintain good nutritional status, fluid balance - Pain relief to enhance early mobility and to prevent depression - Consideration should be given to the catheterisation of incontinent patients - Early referral for surgical opinion for deep sores which are not healing rapidly avoiding months of slow medical treatment - Participate in a planned hospital discharge for those in “at risk” groups to ensure continuity of care in the community 1.1.3 Role of the General Practitioner As soon as a patient is identified as having pressure damage or at risk of developing pressure damage, the patient’s general practitioner should be promptly informed. Where pressure damage already exists the GP will need to know: The size and quantity of dressings to be prescribed If any wound swabs have been taken and what organisms, if any, have been grown and subsequent sensitivities If no wound swabs have been taken, but there are clinical signs of wound infection, an antibiotic may still be prescribed blindly in line with existing guidelines The degree of discomfort experienced by the patient to enable the GP to prescribe appropriate analgesia 11 Where the wound does not respond to treatment and persists longer than 3 months or is recurrent, the nurse or GP may wish to consider arranging a referral to a tissue viability nurse or hospital consultant. General practitioners can play a primary role in the prevention of pressure damage by educating “at risk” patients and their carers in prevention strategies during home visits and routine surgery consultations. This can be of particular value for those patients or carers that, through choice, do not have day-to-day assistance from other health care professionals. General practitioners also, like the hospital doctor, play a key role in the management of underlying conditions that increase the risk of pressure damage or delay healing e.g. cerebral vascular accidents, diabetes, obesity etc. 1.1.4 Role of the Physiotherapist The most important preventive measure offered by the physiotherapists is that of educating carers in positioning of the patient, to avoid exposure of the tissues to excessive concentrations of pressure. One method of achieving this is the 30° tilt. (See appendix 1) In addition to good positioning, it is vital when maintaining skin integrity to use safe transfers when moving a patient; to encourage mobility – stimulating efficient systemic function and to promote continence through exercise, education and electrotherapy, if necessary. 1.1.5 Role of the Occupational Therapist Occupational therapists can, by assessment, offer methods and equipment for the prevention and management of pressure sores. Intervention is particularly valuable for those who are wheelchair dependent, or spend a large proportion of their time sitting. The areas in which such people are particularly at risk are in the seating equipment, bed and bath and during transfers. Correct wheelchairs, cushioning and special seating can be provided by liaison with the Disablement Services Centre. Occupational therapists work as part of a multi-disciplinary team, and in liaison with nursing staff, can assess for the provision of the correct mattresses and, because a percentage of pressure sores are caused by shearing, Easi-glide sheets can make it safer to move people in bed. Hoists with the correct slings, or transfer boards for the more able, can be provided, after assessment. 12 Bathrooms are a particular hazard and the provision of the correct equipment for getting into and out of the bath, and cushioning in the bath is important. During home assessments it is necessary to identify any risks within the home. If people are at risk from pressure damage, advice on suitable clothing is also necessary. 1.1.6 Role of the Pharmacist The pharmacist’s role in a multi-disciplinary wound management team is to provide information about the physical properties of dressings, their usage and cost. As dressings and wound management products have become more sophisticated, they have also become more wound specific. No single dressing is suitable for the management of all wound types and few are ideally suited for the treatment of a single wound during all the stages of the healing cycle. The pharmacist can advise on the most appropriate product for use in any given situation and can help in the development of wound management policies. The pharmacist can also help in the assessment of new products as and when they become available. The aims of good care and management of a wound should include individualised therapy for each patient and for each wound. The patient should be treated holistically and any co-existing condition that could affect wound healing treated. The pharmacist can give advice on medication that may affect wound healing, and also give advice on pain relief for painful wounds. The pharmacist can also liaise with community colleagues to ensure continuity of treatment when patients are discharged from hospital, especially when products are not available on FP10 prescriptions. 1.1.7 Role of the Dietician Dieticians play a role in both the prevention and management of pressure damage. The dietician will assess the patient’s current and previous nutritional intake and make appropriate recommendations. This may require the prescription of nutritional supplements. In assessing the diet, external factors such as a physical and mental state, dentition and social circumstances need to be taken in to account. The multi-disciplinary team can help in determining these factors. 13 It is important that an appropriate follow-up system is available to community patients. The dietician can provide ongoing training to all staff in how to assess a patient’s nutritional state using a Body Mass Index score (BMI) and the role of dietary supplements. 1.2 Education and Training It is the responsibility of each practitioner to ensure that their knowledge and practice is up-to-date, reflecting the outcome of current research and known best practice. Each unit will ensure that there are education and training programmes, including refresher training, available for relevant staff that cover the following, as appropriate to their area and sphere of work: Moving and handling and positioning (to meet the requirements of current Health and Safety legislation) Assessment of the patient and their risk of developing pressure damage Prevention of pressure damage Management of pressure damage It is each individual’s responsibility to ensure that they use the correct techniques and selects the appropriate equipment when moving and handling and positioning a patient, to minimise harm to the patient, themselves and their colleagues. The appropriate moving and handling equipmant will be readily available and staff should know where to obtain these aids and be trained in their safe operation. 1.3 Mattress Replacement Each unit has a continuing, effective replacement programme for mattresses, mattress covers and trolley overlays that is co-ordinated by a designated individual. Each unit will follow the manufacturer’s recommendations for care and maintenance of the mattress/cover/overlay. Manufacturers of the standard NHS contract 150mm mattress, recommend that it have a life span of 5 years. Each unit using these mattresses will have, therefore, a mattress replacement programme over a 5-year period. This programme then becoming a perpetual programme every 5 years. 14 Units utilising types of mattress/cover/overlay other than standard NHS contract 150mm mattress, will have a replacement programme specific to the manufacturer’s recommendations of life expectancy of the mattress. Each unit will follow the manufacturer’s recommendations of care of the mattress/cover/overlay whist in use that may include: Date stamping of the mattress/cover/overlay on receipt and use Turning/rotation of the mattress whist in use (following manufacturers guidance) Routine inspection of the mattress/overlay (including internal inspection of the inner foam, inbetween patients) Mattress covers not to be cleansed with phenol-based solutions Any cracked/torn/worn mattress covers to be replaced All new beds should be supplied with a new mattress. Each unit will be aware of the methods for evaluating the effectiveness, comfort and appearance of the mattress (see mattress turning program files): Testing of mattress foam for indentation – Hand Compression Assessment Recovery of the foam indentation after a 24 hours rest period Contamination of the foam with body fluids, condensations – Water Penetration Test Units utilising other mattresses/overlays will follow the manufacturer’s recommendations for assessment of effectiveness, comfort and appearance. 1.4 Linen for Patient Use All linen – sheets, pillow slips, stretcher and trolley overlays, etc should be free from creases, darns, patches and roughened areas within the area in contact with the patient. Linen that is unsatisfactory should be returned to the laundry for relaundering or disposal where appropriate. 15 1.5 Equipment Each unit will have a system for storing and managing the distribution of pressure relieving equipment, ensuring equipment is used appropriately. Pressure relieving equipment and aids should be of proven effectiveness. The Department of Health Medical Devices Directorate evaluates pressure-relieving equipment and produces reports available free to the NHS. Trials of new equipment must be ratified by the Medical Devices Group. Written criteria will be available to enable the patient’s key worker to select the most appropriate pressure relieving aid. The appropriateness of the pressure relieving aid will be re-assessed following changes in the patient’s condition, level of risk or grade of existing pressure damage. Where indicated, the pressure relieving aid will be promptly changed for one providing a higher or lower degree of relief from pressure as appropriate. 1.6 Assessment of the Patient’s Risk The multi-disciplinary team should undertake assessment of the patient’s risk of developing new or further pressure damage as soon as practical. Part II, section 2.1 shows some of the factors to be considered when assessing risk. Any risk assessment tool used, should be seen as an aid to deciding the level of risk and to provide guidance when selecting the most appropriate pressure relieving equipment. The tool should not be viewed as an acceptable alternative to a proper multi-disciplinary assessment. Each ward/home or unit will identify a risk assessment tool that is appropriate for his or her patients. Patients will have their risk of developing pressure damage assessed within one hour of admission/transfer/first contact. For patients in the community, the community nurse will assess their risk of developing pressure damage on the first visit. Each patient will be re-assessed for their risk of developing pressure damage following a change in their condition. The result of such assessments will be documented in the patient’s personal records. The result of the most recent assessment will be communicated to other health care professionals when responsibility for the patient’s care is transferred from one individual/team to another. 16 1.7 Risk Assessment Tools in Barnsley 1.7.1 Norton Score Score Mental State Activity Mobility Incontinence 4 General Condition Good Alert Ambulant Full Not 3 Fair Apathetic Poor Confused Slightly limited Very limited Occasional 2 Walks with help Chair-bound Usually/urine 1 Very bad Stuporous Bed-fast Immobile Doubly At risk = score of 14 or less 1.7.2 Waterlow Risk Assessment BUILD – WEIGHT FOR HEIGHT Average Above average Obese Below average 0 1 2 3 SKIN TYPE VISUAL RISK AREAS Healthy Tissue paper Dry Oedematous Clammy/pyrexia Discoloured Broken/split 0 1 1 1 1 2 3 SEX/AGE Male Female 14-49 50-64 65-75 75-80 81+ 1 2 1 2 3 4 5 SPECIAL RISKS TISSUE MALNUTRITION Terminal Cachexic 8 Cardiac failure 5 Peripheral vascular disease 5 Anaemia 2 Smoking 1 NEUROLOGICAL DEFICIT Diabetes 4 CVA 6 MS 6 Paraplegia 6 Motor/sensory 6 MAJOR SURGERY Orthopaedic – 5 Below waist/ spinal cord On table > 2 hours MEDICATION Steroids Cytotoxics High dose antiinflammatory 5 Ring scores in table, add total. Several scores per category can be used. Score: 10+ = at risk 15+ = high risk 20+ = very high risk 17 4 1.7.3 Modified Andersen Score Absolute (Score 2) Relative (Score 1) Not conscious Limb mobility restricted Orthopaedic trauma/surgery (major) Incontinent Requires fluid/rehydration Nutritionally deficient/emaciated Tetraplegia/paralysis Coloured red over bony area Hasn’t to/can’t/won’t move 70 years old or more Total Score = Score of 2 or more = “At Risk” 1.8 Action for “At Risk” Patients Patients will have an individual documented plan of care of their identified risk factors and this will be implemented within a maximum of 2 hours from admission. The management of “at risk” patients should involve all members of the multidisciplinary team as appropriate. (See Section 1.1) The care plan will be communicated to all other health care workers contributing to the patient’s care. Evaluation of care will be continuous, however, the patient’s care will be evaluated and reviewed following any change in their condition or treatment. The patient’s plan of care will be communicated to other health care professionals when responsibility for the patient’s care is transferred from one individual/team to another. 18 PART 2 MANAGEMENT OF PRESSURE DAMAGE 2.1 Wound Assessment and Management 2.1.1 2.1.2 2.1.3 2.1.4 2.1.5 2.1.6 2.1.7 2.1.8 2.2 Patient Assessment General Assessment of the Patient Assessment and Routine Investigations Wound Assessment Dressing Assessment Fluid filled blisters Completing Datrix Reports Wound Assessment Flow Chart Treatment Protocols and Formulary (Barnsley Business Unit Only) 2.2.1 Using the Formulary 2.2.2 Wound Management Formulary Protocols 1 and 2 Protocols 3 and 4 Protocols 5 and 6 Protocols 7 and 8 Protocol 9 2.3 Pain and Wound Management 2.4 Guidelines to Selection of Equipment 2.4.1 2.4.2 2.4.3 2.4.4 2.4.5 2.4.6 2.4.7 2.4.8 DHSS Standard Issue Mattress Vaperm, Soft Foam, Key 2 Care, Pentaflex Cairwave Therapy very high risk mattressess Sheepskins Chair Cushions and Devises User Guide – Pressure Reducing Equipment – Seating Systems User Guide – Pressure Reducing Equipment – Lying Systems User Guide – Pressure Reducing Equipment – Specialist Beds 2.5 Factors affecting Healing 2.5.1 Systemic Infection 2.5.2 Diabetes 2.5.3 Carcinoma 2.5.4 Anaemia 2.5.5 Poor Nutritional State 2.5.6 Reduce Immunity 2.5.7 Poor Circulation 2.5.8 Wound Contaminated by Impacted Material 2.5.9 Position of the Wound 2.5.10 Local Infection of Wound 2.6 Medical and Surgical Measures 2.7 Transporting Patients 2.7.1 2.7.2 2.7.3 2.7.4 2.7.5 2.7.6 2.7.7 Internal Transportation of Patients Mode of Transport Minimising Delays External Transportation of Patients Patients requiring Stretcher Overlays Action by Ambulance Crew Handover – Continuity of Care 2.8 Discharge and Transfer 2.9 Monitoring Information 2.9.1 Prevalence Monitoring Information 2.9.2 Incidence Monitoring Information 2.9.3 Prevalence and Incident Monitoring Returns 20 MANAGEMENT OF PRESSURE DAMAGE 2.1 Wound Assessment and Management 2.1.1 Patient Assessment A holistic approach to the management of patients with pressure damage is vital and requires input from the multi-disciplinary team. On the following pages is a list of factors to consider when undertaking a comprehensive assessment of the patient followed by guidance on routine investigations. 2.1.2 General Assessment of the Patient FACTORS TO DOCUMENT Age IMPORTANCE Age related changes affect the elasticity and healing properties in the skin. Nutritional status may be affected in relation to income. People over the age of 70 have the highest prevalence of mixed arterial and venous disease. Skin Inspection An inspection of the skin/vulnerable areas should be done within 1 hour of admission in patient areas and on first contact in other areas (Local Policy) Specific Illness: All of these diseases may delay healing or Diabetes, cardiac failure, cause particularly severe wounds. rheumatoid arthritis and other collagen diseases and cancer 21 Known Allergy The prevention essential. of allergic reactions is Nutritional Status Obesity and malnourishment can delay wound healing. Lack of protein, vitamin C and zinc reduces collagen synthesis. Lack of iron reduces the oxygen carrying capacity of the blood cells. Degree of Mobility Pain and stiffness will reduce mobility and exercise. This will contribute to poor blood circulation and muscle wasting. Sleep Patterns Sleeping more comfortably in a chair or having a history of hanging a leg over the side of the bed may indicated the presence of arterial disease. Smoking Habits Smoking is an important factor in the development of peripheral vascular disease. Daily Living Activities Poor hygiene and/or the inability to wash can exacerbate wounds and delay healing. Incontinence may cause skin excoriation. There is a need to be aware of the limitations placed on individuals where particular dressings or sutures are used. The mental health status and ability to understand wound causes and treatment need to be considered as well as the home environment. Medicines Some drugs delay healing and/or affect surrounding skin, such as prolonged treatment with steroids, antibiotics and chemotherapy. History of the Wound The date of onset of the wound, previous treatment and family history may provide useful clues to planning effective treatment. 2.1.3 Assessment and Routine Investigations INVESTIGATIONS IMPORTANCE Urinalysis To exclude the possibility of diabetes or a case of incontinence or urinary tract infection. Blood Pressure To detect hypertension that may influence circulation and oxygen reaching the tissue. Peripheral Pulses Reduction or absence of these pulses may indicate the presence of ischaemia. Wound swabs in the presence of To identify pathogenic organisms, which obvious pain, oedema and would delay the healing process. cellulitis associated with infection. Blood Tests: Immune status. Detection of anaemia, Erythrocyte Sedimentation Rate diabetes, vitamin deficiency, low white cell (ESR), rheumatoid factor, count and electrolyte imbalance. syphilis. Haemaglobin 22 Other Factors: Temperature, type of tissue involvement, pH of wounds, fibrosis of wound margin, foreign bodies, haematoma, malignant disease and mechanical stress on tissue. Temperature of wounds less that 37oc will heal more slowly. An acid environment improved wound healing. Fibrosing rings around a wound margin will cause bridging. Continued trauma to a wound will prevent tissue repair. 2.1.4 Wound Assessment Grading of pressure damage for documentation and monitoring will be according to the four-point Clinitron Grading System, as shown below. Clinitron Grading System for Pressure Damage All pressure sores should be graded. Do not use unclassified, ungradeable or unstageable. If you are unsure regarding pressure sores grade 3 or 4, the pressure sore should be graded 3. An RCA completed with documentation to support your decision and note the possibility that the pressure sore could deteriorate. 23 Grade 1 Non-blanching, persistent erythema Damage to the micro-circulation Reversible Grade 2 Partial thickness skin loss involving epidermis and/or dermis Superficial and presents clinically as an abrasion, blister or shallow crater Grade 3 Full thickness skin loss Damaged to sub-cutaneous tissue Eschar or slough may be present Look for undermining Grade 4 Full thickness wound with extensive damage to muscle, bone or supporting structures High risk of sepsis Life threatening The site(s) of all pressure damage will be documented using the Wound Assessment Chart (See Appendix 6). The size and shape of all areas of pressure damage will be recorded. Where pressure damage is particularly irregular, consideration should be given to measuring and sketching the area in the patient’s record. Also consider taking a photograph using a measure/tape on the skin to show size of wound (with signed consent) All visible areas should be re-assessed at each change of the patient’s position, areas occluded by dressings will be reassessed at each dressing change. Any improvement or deterioration of the site(s) of pressure damage will be documented. On Discharge/transfer the site(s), grade and size of pressure damage will be notified to the person taking over the responsibility for the patient’s care. Wherever possible a photocopy of the Wound Assessment Chart and RCA (Root Cause Analysis) form if applicable, should be sent out with the discharge letter. 24 2.1.5 Dressing Assessment The flow chart on the following page should be used as guidance to determine the appropriate treatment protocol for the type of pressure ulcer in consultation with the patient’s doctor. The treatment protocols, in Part II, Section 2.2, describe the range of products most suitable for a particular pressure ulcer/wound. The selected product should be altered to meet the changing nature of the pressure ulcer/wound, but it should be give a minimum of 5 to 7 days to take effect unless there is an adverse reaction. Dressings should be changed in accordance with the manufacturer’s instructions and the protocol for the type of wound, and to meet the requirements of the individual patient. The number of dressings inserted into the wound should be documented in the care plan. When dressing a deep wound, ensure all dressings are removable, tie together or use and alternative longer product. On discharge/transfer to another team’s care, the dressings currently used and when last changed should be documented in the discharge/transfer letter and 2 dressing changes should be sent home with the patient if discharged from a hospital site. 2.1.6 Fluid Filled Blisters Fluid filled blisters of lower legs Associated with cellulitis Protect the blister with jelonet, if they are distended, aspirate the fluid using a fine needle and syringe to prevent the tissue tearing, then protect with jelonet. 2.1.7 Incident Reports If a patient develops pressure damage of grade ΙΙ or above, then a clinical incident report (Datrix) should be made. This will highlight the plan of intervention to prevent further pressure damage and ensure appropriate support surfaces are provided. If a patient is transferred to your care with existing pressure damage Grade ΙΙ or above, then a clinical incident report (Datrix) should be made. Identifying numbers of ulcer sites, grades etc. and where the patient has come from. SEE FLOW CHART FOR REPORTING PRESSURE DAMAGE (Appendix 8) 25 2.1.8 Root Cause Analysis (R.C.A) If a patient has a Grade ΙΙΙ or above pressure ulcer, then a root cause analysis form should be completed with action plan attached (see Appendix 7). A copy of this should be attached to the Datrix report. When the patient is transferred or discharged from your care, send a copy of the RCA with discharge papers. SEE FLOW CHART REPORTING PRESSURE DAMAGE (Appendix 8) 26 2.1.7. Wound Assessment Flow Chart Skin Intact Superficial Wound Wound not improving Open Wound Flat Moist Infected Clean Necrotic Flat Dry No treatment required Implement prevention plan as necessary 27 Shallow Deep Shallow Deep Shallow Deep Protocol Protocol Protocol Protocol Protocol Protocol Protocol 9 2 3 4 5 6 7 8 Seek specialist advice Protocol Protocol 1 SECTION 2.2 TREATMENTS PROTOCOLS AND FORMULARY APPLIES TO BARNSLEY BUSINESS UNIT ONLY 2.2 Treatment Protocols and Formulary The treatment protocols and formulary on this section describe the range of products most suitable for a particular pressure ulcer/wound. The flow chart should be used as a guide to determine the appropriate treatment protocol. 2.2.1 Using the Formulary Selecting Products All dressings and treatments within the formulary have been reviewed and approved for the treatment of wounds by the Wound Care Advisory Group. Advice on this can be obtained from the tissue viability nurse. Where a product cannot be obtained outside the hospital, advice should be sought from the tissue viability nurse on an appropriate alternative that will be available on prescription. Additions to the Formulary No products can be added to this formulary without the approval of Wound Care Advisory Group. Staff wishing to have a product included should contact their areas representative to the Wound Care Advisory Group, the District Tissue Viability Nurse or a Pharmaceutical Advisor. 2.2.2 Wound Management Formulary - - 29 Protocols 1 and 2 Protocols 3 and 4 Protocols 5 and 6 Protocols 7 and 8 Protocol 9 TREATMENT PROTOCOLS AND FORMULARY Wound Management Formulary Protocols 1 & 2 Lilac Protocols 3 & 4 Yellow Protocols 5 & 6 Blue Protocols 7 & 8 Pink Protocol 9 Green 30 WOUND MANAGEMENT FORMULARY Non or Low Adherent Dressing a. Suitable for dry wounds or lightly exuding wounds - Melolin (Smith & Nephew) - Telfa (Tyco) b. Knitted Viscose Primary Dressing - N-A Ultra (Systagenix)) - N-A Dressing (Systagenix)) c. Silicone Wound Contact Dressing d. Knitted polyester contact dressing Impregnated with triglycerides - Mepitel (Molnlycke) - Silflex (Advancis - Adaptic Touch (Systagenix) - Utrgotul (Urgo) e. Foam dressing with low adherence suitable for skin tears etc. - Atrauman (Hartmann) - Transorbent (Aspen) Semi-Permeable Films Suitable for relatively shallow wounds - Clearfilm (Richardson HC) e.g. dermabrasion or partial thickness - Hydrofilm (Hartmann) burn or secondary dressing to e.g. Kaltostat or Intrasite Gel Island Dressings Suitable for relatively shallow wounds e.g. dermabrasion or partial thickness burn or secondary dressing to e.g. Kaltostat or Intrasite Gel - Clearpore (Richardson HC) - Opsite Post-op (Smith & Nephew) - Cosmopore-E (Hartmann) - Softpore (Richardson Healthcare) Hydrogels Suitable for desloughing and for light to medium exuding wounds, but not if anaerobic infection is present - Activeheal hydrogel (Medlogic) - Actiform Cool (Activa) - Intrasite Conformable (Smith & Nephew) Hydrocolloids a. Semi Permeable Suitable for desloughing and for light to medium exuding wounds, but not if anaerobic infection is present b. 31 Fibrous - Comfeel Ulcer (Coloplast) Granuflex (Convatec) Duoderm Extra Thin (Convatec) Comfeel Transparent (Coloplast) Comfeel Paste (Coloplast) - Aquacel (Convatec) - Versiva XC (Convatec) Alginate Dressings a. Suitable for exuding wounds only - Sorbsan (Aspen) b. Alginate dressings with absorbent backing - Sorbsan Plus (Aspen) Polyurethane Foam Dressings a. Adhesive margin Suitable for exuding wounds - Activheal Foam (Medlogic) - Allevyn (Smith & Nephew) - Tegaderm foam Adhesive (3M Healthcare) b. Non-adhesive Suitable for exuding wounds Flat Wound - Activheal Foam (Medlogic) - Allevyn (Smith & Nephew) Wound with Cavity - Allevyn Cavity Wound Dressing (S&N) c. Silicone Adhesive Suitable for fragile skin - Allevyn Gentle border (Smith & Nephew) - Mepilex border (Molnlycke) Odour Absorbing Dressing - Actisorb Silver 220 (Systagenix) - Carboflex (Convatec) - Sorbsan Plus Carbon (Aspen) Paste Bandages Suitable for treating skin conditions associated with leg ulcers e.g. eczema, inflammation - Icthopaste (Smith & Nephew) Viscopaste (Smith & Nephew) Coltapaste (Smith & Nephew) Zipzoc (Smith & Nephew) Paraffin Tulle (Non-Medicated) Dressing Suitable for clean, superficial wounds e.g. dermabrasion or partial thickness - Jelonet – normal loaded product (S&N) burns, skin tears 32 Desloghers Used to deslough wounds Antibacterials - a. For infected or colonised wounds - Activheal hydrogel (Medlogic) Actiform Cool (Activa) Granuflex (Convatec) Comfeel (Coloplast) Aquacel (Convatec) Sorbsan (Aspen) Acticoat Range (S&N) Flaminal (Crawford) Urgotul SSD (Urgo) Silver Sulphadiazine 1% cream (S&N) Activon (Advancis) Actilite (Advancis) Algivon (Advancis) Aquacel AG (Convatec) Sivercel Non Adherent (Systagenix) Cutimed Sorbact (BSN) ASkina Calgitrol Ag (B Braun) b. For malodorous fungating wounds - Metrotop Metronidazole gel - Anabact Antiseptics a. Cleansers b. Dressings - 10% Povidone Iodine Solution - Octenalin (MRSA only) - Inadine (Systagenix) - Cadexomer Iodine/Iodoflex/Iodosorb (Smith & Nephew) Wound Irrigation - Sterile Sodium Chloride 0.9% Solution - Tap Water Protease Modulating - Promogram (Systagenix) - Promogram Prisma (Systagenix) - Aquacel (Convatec) Highly Absorbent - Eclypse (Advancis) - Kerramax (Ark) - Drymax (Aspen) Silicone Dressings - 33 Mepitel (Molnlycke) Silflex (Advancis) Urgotul (Urgo) Adaptic Touch (Systagenix) Allevyn Gentle border Mepilex border Protocols 1&2 PROTOCOLS 1 AND 2 SUPERFICIAL WOUNDS FLAT DRY WOUNDS FLAT MOIST WOUNDS Telfa (first choice) Atrauman Melolin Jelonet N-A Dressing Silflex (first choice) Softpore Mepitel (second choice) Clearpore Comfeel Transparent Opsite post-op Duoderm Range CosmoporE Urgotul Hydrofilm Clear film Adaptic touch 35 PROTOCOL 1 - FLAT DRY WOUNDS Flat dry wounds require a simple dressing, such as a low adherent dressing. NB: These dressings are low adherent rather than non-adherent. Low adherent dressings are the modern alternative to traditional dressings such as cotton wool, gauze, lint and gamgee. NB: Secondary dressings may be needed e.g. bandages or adhesive tape. MELOLIN Consists of a film of polyethylene , onto which is bonded an absorbent layer, consisting of a mixture of cotton, viscose and polyacrylonitrile fibres, backed with a layer of an apertured non-woven cellulose fabric. The plastic film is present to prevent the dressing adhering to the wound surface and is perforated to allow the passage of exudate from the wound into the body of the pad. Indications Melolin may be used on its own to dress dry sutured wounds, superficial cuts and abrasions, and other lightly exuding lesions. It may also be used as a primary wound contact layer for more heavily exuding wounds, if backed by a secondary absorbent dressing. Contra-Indications In common with other perforated film dressings, Melolin should be used with caution in the treatment of leg ulcers that produce copious quantities of very viscous exudate. Under these circumstances, the exudate may become trapped under the dressing, leading to maceration and inflammation of the surrounding skin. Application Melolin has a relatively low absorbent capacity and is, therefore, intended for use on lightly exuding wounds. In these situations, a single dressing may be secured in position by surgical tape. On more heavily exuding wounds, Melolin may be used as a wound contact layer, beneath a secondary absorbent pad, held in position with tape or bandage. Removal The frequency with which the dressing should be changed depends entirely upon the nature and condition of the wound. 36 TELFA Telfa consists of an absorbent perforated plastic film faced dressing, open at two ends surrounding an absorbent core. The perforated plastic film is present to prevent the dressing adhering to the wound surface and is perforated to allow the exudate to pass through it into the absorbent pad. Indications Telfa may be used on its own to dress dry sutured wounds, superficial cuts and abrasions and other lightly exuding lesions. It can be held in place with tape or bandages. For more heavily exuding wounds, it may be used as the wound contact dressing with a secondary absorbent dressing. Contra-Indications In common with other perforated film dressings, Telfa should be used with caution in the treatment of leg ulcers that produce copious quantities of very viscous exudate. Under these circumstances, the exudate may become trapped under the dressing, leading to maceration and inflammation of the surrounding skin. Application Telfa has a low absorbent capacity and is therefore, intended for use on lightly exuding wounds. Unless used as a wound contact layer with a secondary dressing. Removal If the dressing is adhered to the wound, irrigate with tap water or saline to ease the dressing from the tissue without disturbing granulation of new epithelialisation. N-A DRESSING N-A Dressing comprises of a warp knitted fabric manufactured from a viscose monofilament. Indications Low adhesive wound contact on ulcerative or granulating wounds. Ideal to use with Vacuum Assisted Closure treatment. 37 SOFTPORE and COSMOPORE Softpore and Cosmopore are island dressings, with an adhesive border. This island pad has a low adherent wound contact layer and is perforated to allow exudate to pass in to the absorbent padding. Indications To be used on dry to low exuding wounds and to cover sutures lines, cuts, grazes and small ulcers. Contra-Indications Not to be used on frail skin, where the adhesive can be harsh and cause tearing of the tissues. Application Softpore and Mepore have a low absorbent capacity and should be used on lightly exuding wounds. Removal To remove, carefully ease one corner from the skin and ease gently by supporting the skin as you remove the adhesive border. If the absorbent pad is stuck to the wound, irrigate with normal sterile saline, to prevent any tissue damage PROTOCOL 2 - FLAT MOIST WOUNDS Flat moist superficial wounds require dressings, which will promote moist wound healing and epithelisation. Semi-permeable film Clearfilm Hydrofilm Permeable to gases and moisture vapour – impermeable to water and microorganisms – consists of a thin polyurethane layer, coated with a vinyl adhesive. These dressings are only suitable for shallow pressure sores/wounds, producing a small amount of exudate. NB: Exudate may be aspirated using a syringe and needle, employing aseptic techniques – a small patch of film dressing must be placed over the puncture to prevent leakage or contamination occurring. 38 CLEARFILM Clean the wound and surrounding skin with sterile sodium chloride 0.9% solution or tap water and allow the skin to dry completely. As with all adhesive products, the skin must be dry and free of detergent residue to assist good adhesion. Application - Peel open the pack and remove the sterile dressing. Remove and discard the centre cut-out piece, exposing the window. Peel the paper backing from the dressing to expose the adhesive surface. View the site through the transparent dressing window and centre the dressing over the wound. Press in place, smooth from the centre towards the edges. - Remove the paper ‘frame’ as you smooth down the dressing edge. Removal Observe the site without removing the dressing. The dressing may remain in place for as long as it is needed for up to 7 days, provided it remains intact. Frequent removal is unnecessary and may cause irritation. Gently grasp the edge of the dressing and slowly pull the dressing from the skin in the direction of hair growth, by stretching the dressing to break the adhesive. Observe the site without removing the dressing. The dressing may remain in place for as long as it is needed for up to 7 days, provided it remains intact. Frequent removal is unnecessary and may cause irritation. Gently grasp the edge of the dressing and slowly pull the dressing from the skin in the direction of hair growth, by stretching the dressing to break the adhesive. HYDROFILM Clean the wound and surrounding skin with sterile sodium chloride 0.9% solution or tap water. Dry /or allow skin to dry completely. As with all adhesive products the skin must be free of grease/cream/detergent residue to allow good adherence. Application Peel open the sterile pack. The backing papers are numbered (1,2,3 & 4). Remove number 1, take hold of the clean edge of exposed dressing, then remove backing paper 2. Place the adhesive side of the dressing over she wound, smooth down to ensure adhesion. Remove paper 3 then paper 4. Finally smooth down the dressing. 39 Peel open the sterile pack. The backing papers are numbered (1,2,3 & 4). Remove number 1, take hold of the clean edge of exposed dressing, then remove backing paper 2. Place the adhesive side of the dressing over she wound, smooth down to ensure adhesion. Remove paper 3 then paper 4. Finally smooth down the dressing. Removal The dressing can stay in place for up to 7 days. To remove the dressing see instructions for removal of Tegaderm dressing (stretching technique). NB: Do not apply film dressings under tension. Skin shearing or blistering may result if excessive tension is present. OPSITE POST OP / CLEARPORE Opsite post op and Clearpore are vapour permeable adhesive film dressings with an island absorbent pad. The island pad is a low adherent dressing. Indications To be used on dry to low exuding wounds and to cover suture lines, cuts, grazes and small ulcers. Contra-indications Not to be used on patients with a known sensitivity to films. Application Expose the central section of the dressing by lifting the two covering sheets on the adhesive side of the dressing, gentle press on the film border to enable adhesion to the per-wound skin. Slowly remove each side of the backing paper smoothing down the dressing to ensure adhesion. Removal To remove, place flat hand over the dressing, lift one corner of the film, gently stretch the film laterally moving the flat hand across the dressing whilst stretch short sections until all the dressing is loose. This method will break the adhesive, thereby reducing pain at dressing change. 40 PARAFFIN GAUZE – JELONET Jelonet is a paraffin gauze dressing with not less than 175g of paraffin per m2 of cloth. Indications Use as a primary wound contact layer in the treatment of burns, ulcers, skin grafts (both donor and receptor sites) and a variety of traumatic injuries. The material is also used as a transfer medium for skin during grafting. Contra-Indications Although there are no absolute contra-indications to the use of paraffin gauze, if the dressing is placed upon a heavily exuding wound, its semi-occlusive nature may cause tissue maceration, by preventing free movement of exudate away from the surface of the wound. Application Apply directly to the surface of the wound and cover with an absorbent pad, held in place with tape or bandage, as appropriate. Removal The frequency of dressing change will depend entirely upon the nature of the wound. NB: If paraffin gauze is left in position for prolonged periods of time it can become adherent and cause damage upon removal. 41 MEPITEL, SILFLEX & ADAPTIC TOUCH Mepitel, Silflex AND Adaptic touch are soft silicone wound contact dressings, which do not adhere to the moist wound surface, but gently to the dry surrounding skin. This significantly reduces pain and trauma during dressing change. Indications They are indicated for painful or macerated wounds, weak or sensitive skin, leg and foot ulcers, abrasions, skin tears, pressure ulcers, traumatic wounds, burns, blisters, fixation of skin grafts and dermatological conditions such as epidermolysis bullosa. They also reduce the need for frequent primary dressing changes in moderate to heavily exuding wounds. As the wound can be irrigated through the Mepitel/Silflex/Adaptic touch and the outer dressing only can be changed. Contra-Indications In the treatment of heavily bleeding wounds, Mepitel/Silflex/Adaptic touch should be covered with a sterile saline moistened pad until bleeding has stopped. When Mepitel/Silflex/Adaptic touch is used on blisters, or for the fixation of skin grafts, the dressing should not be changed before the fifth day post application. If the wound is infected, consult a healthcare professional for the appropriate medical treatment. Application Clean the wound carefully, if needed, and dry the surrounding skin. Choose a size of dressing that will overlap dry surrounding skin by at least 1cm. Mepitel/Silflex/Adaptic touch can be cut to size, if needed, before removing the protective films. If more than one piece of Mepitel/Silflex/Adaptic touch is required, overlap the dressings by at least 1cm. If an overlap is necessary over the wound surface, ensure that the pores of the dressing are not blocked. While holding the larger protective film, remove the smaller one. adherence to gloved hands, moisten gloves in sterile saline. To avoid Apply Mepitel/Silflex/Adaptive touch over the wound. Smooth dressing in place on to the surrounding skin, ensuring a good seal. Remove the remaining protective film. Where clinically indicated, treatments such as topical steroids, topical antimicrobials or Hydrogels can be applied over the top of, or under, Mepitel/Silflex/Adaptic touch. 42 Apply an inexpensive secondary absorbent dressing pad (e.g. Mesorb or Eclypse) on top of Mepitel/Silflex/Adaptic touch. In contoured or jointed areas, ensure sufficient padding is applied to keep the Mepitel/Silflex/Adaptic touch held flat against the surface of the wound. Fix in place with a suitable fixation device. Mepitel/Silflex/Adaptic touch can be used under compression bandages. Removal Mepitel/Silflex/Adaptic touch can be left in place up to 14 days, depending on the clinical condition of the wound. The secondary absorbent dressing pad (e.g. Xupad/Eclypse/Kerramax/Drymax) can be changed as required. Exudate should pass freely through the dressing and the pores should not be blocked. If the pores do become blocked, gently irrigate with sterile saline, ensuring that any excess saline is removed carefully with clean absorbent material. Alternatively, a new dressing should be applied. Mepitel/Silflex/Adaptic touch are single use dressings and should not be re-used. If the condition of the wound deteriorates unexpectedly, discontinue use and consult a healthcare professional for the appropriate medical treatment. COMFEEL PLUS TRANSPARENT Comfeel Plus Transparent is a thin transparent hydrocolloid dressing made of sodium carboxymethylcellulose, artificial elastomer, tackifier and plasticiser with a top layer made from semi-permeable polyurethane film. Indication Comfeel Plus Transparent is indicated for superficial, acute wounds, e.g. superficial burns, superficial partial thickness burns, donor sites, minor traumatic wounds, post-operative wounds, minor chronic ulcers i.e. pressure sores and leg ulcers in the final stages of healing. Contra-Indications Comfeel Plus Transparent provides an optimal moist-wound healing environment locally. 43 Wounds which are solely or mainly caused by an arterial insufficiency or complicated diabetic wounds (primarily lower leg and foot) should be inspected by a physician or nurse regularly. Wounds with signs of clinical infection, fever and local symptoms, such as pain, erythema (redness) or pus should have a bacterial swab examination. The use of Comfeel Plus Transparent may be continued at the discretion of a physician, together with the appropriate medical treatment. NB: Not to be used on patients with systemic infections such as tuberculosis, syphilis or leprosy until the infection is under medical control. Not for use on deep partial thickness or full thickness burns. Not for use on patients allergic to one or more of the components declared. Application To apply Comfeel Plus Transparent dressing, use the handles to ensure aseptic application. Remove the protective paper. Place the adhesive side to the wound, ensuring the dressing extends over the edges of the wound by at least 1.5cms, to ensure good adhesion. Remove the handles. Removal Comfeel Plus Transparent dressing should remain in place for the longest possible period time, but no more than 7 days. When the Comfeel Plus Transparent dressing absorbs wound exudates, a whitish gel is formed in the wound bed. When the gel reaches the upper film surface of the dressing, the appearance becomes ‘marbled’ or transparent. When transparency has been reached the dressing should be changed. In the case of leakage, the dressing should be changed immediately. To remove Comfeel Plus Transparent dressing, press down on the skin, lift 2 corners of the dressing and stretch the dressing to break the adhesive, this will aid the ease of removal and reduce any pain caused by the removal of the dressing. 44 DUODERM EXTRA THIN Duoderm Extra Thin is a sterile hydrocolloid dressing, consisting of an inner layer of hydrocolloids (gelatine, pectin, sodium carboxymethylcellulose) contained within an adhesive polymer matrix and an outer layer of polyurethane film. The outer film is impermeable to exudate and micro-organisms. The hydrocolloid component of the dressing interacts with wound exudate to produce a soft mass, which enables removal with little or no damage to newly formed tissue. Indications The dressing is indicated in the management of lightly exuding acute wounds, such as minor burns, abrasions and lacerations, post-operative wounds and lightly exuding chronic wounds. Contra-Indications In the presence of anaerobic infection, occlusive therapy is not recommended. Inappropriate use, or too frequent dressing changes may result in skin irritation or stripping. Application Carefully irrigate and clean the wound with sterile sodium chloride 0.9% solution. Dry the surrounding skin, making sure that any ointments, creams or other oily substances are removed. Choose a dressing to allow a minimum of 2cm overlap onto intact skin. Remove from backing paper and apply dressing using a rolling motion and gently, but firmly, smooth and mould the dressing into place, concentrating on wound margins. Removal Frequency of dressing changes will depend on the state of the wound. Duoderm Extra Thin should be changed just before the softened area reaches the edge of the dressing, or when leakage occurs. The dressing should not be left in place for longer than 7 days. To remove the dressing, press down on the skin, lift the edge of the dressing all round the wound margin then carefully remove. Sterile saline will aid removal of gel from wound bed. Irrigate the wound with sterile sodium chloride 0.9% solution; remove any gel on the wound bed and dry surrounding skin. 45 ATRAUMAN Atrauman ais a non-medicated impregnated dressing for atraumatic wound treatment. The support fabric is made of hydrophobic polyester tulle, impregnated with a non-medicated ointment based on triglycerides (neutral fats). The water repellent polyester filaments and the smooth surface structure of the tulle counteract adhesion to the wound by preventing new tissue from penetrating the dressing. The non adherent properties are enhanced by the ointment base. It has no occlusive effects and does not cause maceration of the surrounding skin. Exudate can drain freely into an absorbent secondary dressing. By keeping the edges of the wound soft and supple it is thought that it may enhance epithelialisation. Indications For the treatment of wounds, especially for exuding wounds. May be useful for patients with sensitive skin. May be applied in combination with a topical medication of choice. Contra-indications None known. Application Remove from sterile peel pack and cut to size if necessary. After removal of one of the cover papers, place this side of the dressing to wound and remove second cover. Will require a secondary dressing to absorb exudate. Removal Can be removed painlessly without causing any new damage. The ointment base may be absorbed when left in place for an extended period in this case wound adhesion which may occur, this can be eliminated by placing a secondary Atrauman dressing over the first one. 46 URGOTUL Non-adherent soft polymer wound contact dressing. Indications For treatment of moist wounds where adherence would be an issue. Ideal for fragile skin conditions e.g. Skin tears, blistering skin etc. Contra-indications Known allergy to the product. Application Remove the dressing from its sterile pack (aseptic technique). Moistened glove finger tips to prevent the dressing sticking to item – remove one backing sheet, place the dressing onto the wound overlapping good skin by at least 1 cm. Remove the second backing sheet – Place secondary dressing over the top to hold dressing in place. Removal Can be left in place for up to 7 days. Can be removed by gently easing the dressing from the wound, saline or warm tap water can be used for any stubborn areas where adherence occurs. 47 Protocols 3&4 PROTOCOLS 3 AND 4 INFECTED WOUNDS NB: Where infection is diagnosed, systemic antibiotics should be prescribed after checking wound swab result. SHALLOW INFECTED WOUND DEEP INFECTED WOUNDS Inadine Povidone iodine 10% solution Actisorb Silver 220 Cadexomer iodine – Iodoflex/Iodosorb Urgotul SSD Aquacel Ag Cadexomer iodine – Iodoflex/Iodosorb Activon Tube (paste) Silvercel non-adherent Actisorb silver 220 Aquacel Ag Silvercel Activon Tulle / Tube Algivon Actilite Cutimed Sorbact Algivon Silver Sulphadiazine 1% cream (Flamazine) Cutimed Sorbact Askina Calgitrol Ag Flaminal Hydro / Forte Metronidazole gel Excillon AMD (drain sponge) HEAVILY EXUDING Aquacel Ag Allevyn Ag Silvercel non-adherent Algivon 49 HEAVILY EXUDING Aquacel Ag Silvercel Algivon MALODOROUS WOUNDS (Due to anaerobic infection) 1. Metronidazole Gel 2. Actisorb Silver 220 3. Sorbsan Plus Carbon 4. Carboflex NB: Clinical infected wounds will not heal, however, it is usually not necessary to sterilise wounds. 50 PROTOCOL 3 – INFECTED WOUNDS NB: Where infection is diagnosed, systemic antibiotics should be prescribed, NEVER topical. POVIDONE IODINE DRESSING (Inadine) Inadine consists of a knitted viscose fabric, impregnated with a polyethylene glycol (PEG) base, containing 10% povidone-iodine, equivalent to 1% available iodine. In the presence of wound fluid, the povidone-iodine, a potent bactericidal agent with a broad spectrum of activity, is readily released from the PEG base. The dressing, which is designed as a low adherent wound contact material, is yellowbrown in colour and superficially resembles paraffin gauze. Unlike paraffin or lanolin, the base used in the production of Inadine is water-soluble and easily removed from the skin or wound surface. Indications Inadine is indicated for the prophylaxis and treatment of infection in minor burns, superficial skin-loss injuries and as a dressing for adjunctive therapy in the treatment of infected ulcerative wounds. Contra-Indications Inadine should not be used on patients who are sensitive to iodine or povidoneiodine. Warnings and Precautions Inadine is for topical uses only and not more than four dressings should be applied at any one time. The product should be used with caution in pregnant or lactating mothers, because of the possible effects of elevated serum iodine levels on the foetus or neonate. Povidone-iodine may be absorbed through the unbroken skin of the neonate and young child. Monitoring serum iodine levels and thyroid function tests are advisable in these patients. Application Inadine is applied directly to the surface of the wound and covered with a sterile secondary dressing held in position with tape or bandage, as appropriate. 51 Removal Adherence to the surface of the wound is unlikely with Inadine, but if it does become a problem, the dressing may be removed following irrigation with sterile sodium chloride 0.9% solution or tap water. The frequency of dressing changes depends primarily upon the condition of the wound. If large quantities of exudate are produced, daily changes will probably be required, but if the wound is relatively dry the interval between changes may be extended. For most applications, however, it is unlikely that the dressing will retain significant levels of antibacterial activity if left in position longer than two days. POVIDONE IODINE SOLUTION Povidone iodine solution has the broadest spectrum of actions of any antiseptic commonly available. The antibacterial effect is reduced by contact with pus and exudate. Active iodine is brown; on inactivation iodine is converted to colourless iodides. NB: Povidone iodine must be applied at intervals sufficiently short for brown coloration to persist. METRONIDAZOLE GEL / TABLETS Metronidazole tablets can be given systemically to remove odour (200mg – 400mg tds). Topical gel indicated for de-odourisation of fungating, malodorous wounds / tumours. Metronidazole is active against the anaerobic bacteria associated with the pungent odour. Use once or twice daily, as necessary. Metronidazole is now available for use as a topical application in a commercially available gel, Metrotop 0.8%. CADEXOMER IODINE (Iodoflex/Iodosorb) Iodoflex/Iodosorb is an antibacterial agent, which cleans the wound, reduces pain and speeds up the healing process. Indications Iodoflex/Iodosorb is indicated for the topical treatment of leg ulcers. When applied to the wound Iodoflex/Iodosorb cleans and reduces bacteria at the wound surface. In long-term (chronic) ulcers, it speeds up the healing process and reduces pain. 52 Contra-Indications Iodoflex/Iodosorb should not be used on patients who are sensitive to iodine. Pre-cautions Patient with thyroid problems should have their thyroid profile monitored whilst on iodine preparations as their medication dose may need adjusting. Application Clean the wound and the surrounding area with either a gentle stream of sterile water or saline, or using a sterile wet swab, if necessary. For Iodoflex Paste - remove the carrier gauze on both sides of the paste, mould the paste to the shape of the wound and apply to the wound surface/cavity. For Iodosorb Ointment - apply Iodosorb ointment to a dry sterile dressing, ensuring sufficient to cover all parts of the wound to a depth of 3mm. Position the prepared dressing onto the wound. Lightly smooth a gloved finger over the dressing to spread the ointment underneath to the shape of the ulcer and to a minimum depth of 3mm. Apply compression bandaging, where appropriate Discard any remaining Iodoflex/Iodosorb Removal Iodoflex/Iodosorb should be change three times a week or when it has become saturated and lost its colour. If necessary, soak the dressing for a few minutes and then remove. Remove the remaining Iodoflex/Iodosorb with a gentle stream of sterile water or saline, using a sterile wet swab if necessary. Tap water should be used when treating leg ulcers. Use warm water in a socially clean bowl, emollient can be used as a soap substitute, to give the foot and leg a thorough clean. Gently blot any excess fluid, leaving the wound surface slightly moist, before reapplying Iodoflex/Iodosorb. 53 Warnings and Precautions A single course of treatment should not exceed 3 months. The product should be used with caution in pregnant or lactating mothers because of possible effects of elevated serum iodine levels on the foetus or neonate. Does the patient have Thyroid disease? Is the patient is taking any other medicines, which include lithium and certain sulphonamide drugs, which are anti-diabetic or anti-infective. M.R.S.A. (Methicillin Resistant Staphylococcus Aureus) IN WOUNDS M.R.S.A. can colonise wounds without causing an infection. therefore, not always necessary. Treatment is, When treatment is deemed in the best interest of the patient, de-colonisation of the wound may be required. The following solutions/preparations are recommended for wound cleansing in M.R.S.A. colonised wounds Povidone Iodine 10% Solution Clean the wound daily for 7 days with Povidone Iodine 10% solution. Ensure that no contra-indications are presents for treatment e.g. pregnancy, thyroid disease etc. OCTENILIN Irrigate the wound thoroughly with Octenilin wound cleanser. Rinse thoroughly with sterile water or sterile sodium chloride 0.9% solution. Dress the wound according to the agreed procedure. NB: 54 Keep out of eyes – Rinse thoroughly with tap water and consult the doctor if splash into the eyes. Silver Sulphadiazine 1% Cream (Flamazine) Clean the wound thoroughly with sterile sodium chloride 0.9% solution. Apply the cream to the affected area daily with a sterile gloved hand and/or spatula. NB: As Silver Sulphadiazine Cream can cause maceration of normal skin on prolonged contact; care should be taken to prevent spread onto non-affected areas. An absorbent pad, Jelonet or gauze dressing should be applied on top of the layer of Silver Sulphadiazine Cream. Contra-Indications / Warnings Silver Sulphadiazine should not be used in pregnancy or in neonates or in infants during the first few month of life. Silver Sulphadiazine Cream is contra-indicated in patients with a known sensitivity to Silver Sulphadiazine or other components of the preparation, such as cetyl alcohol or propylene glycol. Once opened the tube must be discarded after 7 days and new tube used. AQUACEL AG Aquacel Ag – silver impregnated antimicrobial absorbent dressing is a soft, sterile, non-woven ribbon dressing composed of Hydrofiber and ionic silver. The silver in the dressing kills a broad spectrum of wound bacteria and aids in creating an antimicrobial environment. The dressing absorbs high amounts of wound fluid and bacteria and creates a soft cohesive gel that intimately conforms to the wound surface, maintains a moist environment and aids in the removal of non-viable tissue from the wound (autolytic debridement). A moist wound environment and control of wound bacteria supports the body’s healing process and helps the risk of wound infection. Indications Aquacel Ag may be use for the management of: Wounds where there is an infection or an increased risk of infection Wounds that are prone to bleeding, such as wound that have been mechanical or surgically debrided Surgical wounds 55 Traumatic wounds Oncology wounds with exudates, such as fungoides – cutaneous tumours, fungating carcinoma Contra-Indications Aquacel Ag should not be used on individuals who are sensitive to, or who have had an allergic reaction to silver or sodium carboxymethylcellulose. Aquacel Ag is not compatible with oil-based products such as petroleum. Application Aquacel Ag is sterile and should be handled appropriately. Prior to application the wound may be debrided, if necessary, and then cleansed with an effective cleansing agent, to be determined by the healthcare professional. Aquacel Ag ribbon should be introduced into the wound cavity, leave at least 2.5cm outside the wound for easy retrieval. For dry wounds – introduce the Aquacel Ag into the wound and wet with sterile saline. Cover the dressing with a moisture retentive dressing to avoid drying out of the dressing. Removal Aquacel Ag should be changed when the dressing becomes saturated with exudates or when good clinical practice dictates that the dressing should be changed. Gently remove the secondary dressing according to the instructions of that product. Remove the Aquacel Ag and discard in clinic waste. Irrigation of the wound with normal saline may be necessary to remove the residual gel. Re-dress the wound site with a new Aquacel Ag and cover with a secondary dressing. 56 ACTIVON RANGE (HONEY) Activon is a medical grade Manuka honey, which can be used as a topical treatment for infected wounds. It can also be used for the treatment of malodorous wounds. The anti-bacterial effects of the Manuka honey are also assisted by the presence of hydrogen peroxide in a very low concentration (an oxidising agent released by the action of the enzyme peroxidase, which is added by bees to the nectar they collect). ACTIVON TULLE Activon Tulle is low adherent gauze dressing loaded with Manuka honey, held in place by an appropriate secondary dressing. The honey is donated to the wound and will debride sloughy tissue, whist dealing with bacteria in the wound, thus de-odourising the exudate ACTIVON TUBE Activon Tube is a single use tube of Manuka honey; this can be used in combination with the Activon Tulle to give an increased loading of honey to the wound, or with other secondary dressings. Indications Activon may be use for the management of infected wounds, malodorous wounds, fungating malodours tumours, sloughy wounds and colonised wounds Activon is safe for use with diabetic patients. Removal of dressing Carefully remove the Tulle from the wound and irrigate remaining honey from the wound, using sterile saline, or in the case of leg ulcers, wash the foot and leg in a bowl of warm tap water. Contra-Indications Not to be used where honey allergies exist. Precautions: Honey can be painful for some patients because of the osmotic effect it has on the wound. 57 ACTILITE Actilite is a non-adherent knitted viscose dressing impregnated with a combination of pure medical grade Manuka honey with Manuka oil. It is an effective antibacterial for preventing or reducing bacterial colonisation in a wound whilst maintaining a moist healing environment. Indications The manufacturers state Actilite can be used on all wound types e.g. cuts and abrasions, pressure ulcers, leg ulcers, surgical wounds, bums, graft sites. Contra-indications Do not use if the patient is allergic to bee venom, bee products or essential oils, e.g. tea tree oil or any materials used in the dressing. Application Place Actilite directly onto wound bed, either side down. To cover larger wounds place additional dressing side by side or for smaller wounds, cut to size (the viscose material does not fray). Cover with an appropriate secondary dressing depending on levels of exudate e.g. a film dressing or absorbent pad. Actilite may be left in place for up to 7 days. To maintain the level of efficacy, change the dressing when the colour fades significantly. Removal Occasionally it may be necessary to facilitate the removal of Actilite by irrigating the wound bed with saline (0.9%) solution. ALGIVON Algivon is an absorbent, sterile, non-adherent wound contact dressing comprising of calcium alginate mechanically bonded fibres, impregnated with medical grade Manuka honey. When wet the fibres swell and form a sodium calcium gel when in contact with wound exudate. The Manuka honey used in the dressing is produced to the highest standards for medical use, having a minimum ant-bacterial efficiency equivalent to 12% phenol. Indications All acute and chronic infected wounds. sloughy wounds, leg ulcers, pressure ulcers, fungating lessions, abrasions, malodourous wounds. 58 Contra-Indications Arterial bleeds or hevily bleeding wounds. Patients with a known sensitivity to calcium alginate or bee venom. Some patients may experience a drawing sensation, this can be painful. Application Algivon is placed either side down onto the wound surface or can be placed side by side to cover large wound areas or cut to size ensuring the dressing does not touch the periwound as this may cause breakdown of good tissue. Depending on levels of exudate an appropriate secondary dressing should be selected. Wounds with low exudate use film or bandage, wounds with high levels of exudate should be covered with a more absorbent secondary dressing. Frequency of changes depends on levels of exudate, but Algivon can be left in place for up to 7 days if exudate allows. Removal of Dressing Algivon will need changing as the honey is highly diluted by exudate of which the calcium fibres have substantially gelled. In some cases it may be necessary to irrigate the wound bed with saline solution (0.9%) before removal. SILVERCEL / SILVERCEL NON-ADHERENT Silvercel is a hydro-alginate antimicrobial dressing with silver in a sterile woven pad, composed of high alginate, carboxymethylcellulose (CMC) and silver coated fibres. The unique composition of the dressing manages exudate in moderate to heavily exuding wounds. The silver fibres kill a broad spectrum of microorganisms associated with the bacterial colonisation and infection of wounds. The non-adherent version has a perforated film coating on both sides of the dressing. Indications Silvercel is intended for use in the management of moderate to heavily exuding partial and full thickness chronic wounds, including pressure ulcers, venous ulcers, diabetic ulcers, donor sites, traumatic ulcers and surgical wounds. Contra-Indications Silvercel should not be used on surgical implantations or on patients with known sensitivities to silver. Precautions Silvercel dressing is not intended to stop bleeding, nor for use on dry wounds, as the dressing relies on exudate to enable the release of the silver. 59 Application Cut or fold the dressing to fit the wound, loosely pack in to deep cavities, ensuring the dressing does not overlap the wound margins. Cover and secure the Silvercel with a non-occlusive secondary dressing. Removal The frequency of the dressing change will depend on the patient’s condition and the level of exudate. The dressing should be changed when the secondary dressing has reached its absorbency capacity or up to 7 days. Gently remove the secondary dressing as per manufacturers instruction. If the wound appears dry, saturate the Sivercel dressing with normal saline 0.9% prior to removal, or tap water if dealing with leg ulcers. Gently remove the dressing from the wound bed. Irrigate the wound with normal saline 0.9%, or tap water, prior to applying the new dressing. URGOTUL S.S.D Urgotul S.S.D is a hydrocolloid dressing which is non-adhesive, non-occlusive and does not adhere to the wound bed. The dressing consists of a polyester mesh, impregnated with hydrocolloid particles (carboxymethylcellulose) Vaseline and silver sulphadiazine. The presence of silver sulphadiazine, which is an antibacterial agent, confers on the Urgotul S.S.D dressing the ability to act on the organisms, which are most frequently responsible for infecting wounds. Silver sulphadiazine has a broad spectrum of antimicrobial activity covering the Gram +ve and Gram –ve bacteria and certain moulds and yeasts. It is particularly effective against staphylococcus aureus and pseudomonas aeruginosa. It is pliable and comfortable for the patient. Directions for Use Clean the wound as per policy. If an antiseptic cleanser is used first, rinse the wound thoroughly with normal saline. Remove the protective wings from the dressing. Apply Urgotul S.S.D directly onto the wound. Urgotul S.S.D will adhere to surgical gloves, consequently it is recommended that the gloves be moistened with normal saline 0.9% to aid with ease of handling. Cover with a secondary dressing. 60 NB: The silver sulphadiazine is active for up to 2 days, so dressing changes should be planned with this guidance. Side effects The silver sulphadiazine can give rise to erythemas, contact eczemas and in rare cases photosensitivity and leucopenias. The passage of Sulphadiazine into the systemic blood stream exposes the patient to a risk of systemic sulphonamide complications e.g. haematological. renal, intestinal and skin complaints. Contra-Indications Do not use if the patient has any known sensitivity to sulphonamides and other ingredients. Not to be used in patients with renal impairment, pregnant or breast feeding women, newborn and premature babies. Removal Gently remove the secondary dressing, following the manufacturers instructions. Urgotul S.S.D dressing can be peeled away from the wound gently, which will not cause trauma or pain. CUTIMED SORBACT An antimicrobial product – bacteria binding gauze, Green in colour. By the principles of hydrophobic interaction, bacterial and fungi become physically and irreversible bound to the dressing. The dressing is coated with a fatty acid derivative (DACC) which gives the dressing its water repellent properties (Hydrophobic) Removing the dressing removes the bound bacteria which cannot multiply or escape once bound to the dressing fibres. Indications All types of colonised or infected wounds. 61 Contra-indications Dry wounds. Application Swabs – Open out the swab, can overlap onto good skin. The dressing can be cut if needed. Removal If dressing has adhered use saline or tap water to ease removal. MALODOUROUS WOUNDS SORBSAN PLUS CARBON Sorbsan Plus Carbon is a highly absorbent alginate dressing with a layer of activated carbon to trap and absorb wound odour. See Protocols 7 & 8 – Sorbsan range. Indications Sorbsan Plus Carbon is intended for use in the management of flat shallow wounds, wounds with moderate to high exudates, infected wounds, fungating wounds and malodorous wet wounds. ACTIVATED CHARCOAL DRESSINGS Used to help in the management of discharging, purulent and contaminated wounds by bacterial infection and offensive odour. The dressings are intended to be applied directly to the wound surface and covered with appropriate secondary dressings. ACTISORB SILVER 220 Incorporates a woven cloth consisting of 95-98% carbon. The charcoal cloth is enclosed in a sleeve of spun-bonded non-woven nylon fabric, which is sealed along all found edges to facilitate handling and reduce particle and fibre loss. Activated charcoal has the property of absorbing odour and noxious materials, such as toxins and degradation products from the wound. 62 The charcoal cloth contains silver residue, chemically and physically bound onto carbon. These impart antimicrobial properties to the fabric, in addition to the absorptive characteristics described above. Application Actisorb Silver 220 is intended for use as a primary wound dressing. In use, the product is applied directly to the surface of the wound and covered with a secondary dressing held in place with tape or bandage, as appropriate. The secondary dressing chosen will depend upon the nature of the wound, but in general, a simple absorbent pad will be sufficient. NB: There may be circumstances where it is not considered appropriate to place Actisorb Silver 220 directly onto the surface of a malodorous wound. In these instances, the dressing may be placed between the selected wound contact material and secondary dressing. On wounds, which tend to dry out, care is needed if Actisorb Silver 220 is used as a primary dressing because adherence may be a problem. Frequency of dressing Change Depends entirely upon the nature and condition of the wound. NB: Actisorb Silver 220 should be used in the intact state and not cut to shape prior to application to the wound. CARBOFLEX Carboflex is a sterile non-adhesive dressing with an absorbent wound contact layer (containing alginate and hydrocolloid), an active charcoal central pad and a smooth water resistant top layer. Indications Carboflex is indicated for the management of malodours acute and chronic wounds. It may be used as a primary dressing for shallow wounds or with deeper wounds as a secondary dressing over wound fillers. Carboflex may be used on infected malodorous wounds under medical supervision, together with appropriate antibiotic therapy and frequent monitoring of the wound. 63 Contra-Indications Do not use on individuals with a known sensitivity to the dressing or its components. Application These dressings are sterile and should be handled appropriately. If required, the wound should be debrided and necrotic tissue removed. Cleanse the wound site, rinse well and dry the surrounding skin. NB: Do not cut the dressing. Choose a dressing, sized so that it is larger than the wound area to ensure that the dressing overlaps the wound edge by at least 3.2cm. For shallow wounds the dressing may be placed directly onto the wound as a primary dressing, and for cavity wounds, Carboflex can be laid over a wound filler/gel as a secondary dressing. Place the fibrous (non-shiny) surface on to the wound or cavity filler. Secure Carboflex in place over the wound with tape of other appropriate material. The absorbent wound contact layer will take up exudate and form a soft gel. Change the dressing when clinically indicated or if there is exudate strike-through to the top layer or if the odour is no longer being absorbed. With non-infected malodorous wounds, the dressing may be left undisturbed for up to 3 days. If the wound is infected, then the dressing should be changed more frequently. Removal Carefully lift away from the wound by grasping one corner of the dressing. FLAMINAL (FORTE / HYDRO) Flaminal Hydrogel – For light or moderately exuding Flaminal is an enzymatic alginogel for use in infected wounds. There are two types: Flaminal Hydro – Indicated for low to moderately exuding wounds Flaminal Forte – Indicated for moderate to high exuding wounds Flaminal debrides and desloughs, it contains natural occurring enzymes glucose oxidase and lactoperoxidase for antimicrobial activity with damaging healing cells. It contains alginate to balance moisture levels and protect wound edges. It is safe to use on all types of wounds at any stage of the healing process. 64 It provides a biodegradable, soft and soothing wound interface whilst reducing pain and trauma. It kills bacterial without damaging key healing cells. Flaminal can be re-capped and re-used for the same patient providing and aseptic technique is followed Application - Follow aspesis throughout the procedure Flaminal can be applied directly to a secondary dressing of applied to a piece of sterile gauze and introduced to the wound bed. Syringe method – Flaminal can be precision applied using a syringe. Remove the plunges from a sterile syringe, squeeze the desired amount of Flaminal into the barrel of the syringe, replace the plunger then apply the Flaminal to the wound. Ideal for narrowed wounds. Removal Flaminal is biodegradable, irrigate the wound with saline / tap waer to remove the excess gel. EXCILON AMD (drain sponge) A primary dressing embedded with PHMB 0.2% (polytexamethylene biguanide), a bacterial killing polymer. PHMB attacks bacteria on and within the dressing fabric, helping keep infection out of the wound and limiting cross contamination. Indications The Excilon AMD drain sponge is a pack of 2 pre-cut gauze swabs embedded with PHMB ideal for around tracheostomy sites, chest drain sites, external fixation sites, suprapubic sites. P.E.G / feeding tubes, IV lines / central lines, post surgery drains, pin-sites / external orthopaedic castings etc. Two sizes available 5 x 5cm and 10 x 10 cms. Dressing changes cost pennies 15p for pack of 5 x 5cm (Sept 2012 NHS Supplies). Application Secondary dressings are not necessary, can be held in place by simple tape. Each pack has 2 sponge/swabs. Provides total coverage and conceals the exit Site. Place one sponge around the site then place the other on top, in the opposite direction to ensure total coverage – can be taped in place. 65 ASKINA CALGITROL Ag A highly absorbent non-adherent dressing with a wound contact of silver alginate matrix which has a strong antimicrobial protective action, which has a slow extended release of silver ions, whilst providing a moist environment. In contact with wound exudate, the alginate matrix forms a soft gel allowing the immediate liberation of silver ions. The release of silver is maintained for up to 7 days. Indications Infected wounds, moderate to highly exuding wounds of partial and full thickness. Pressure ulcers, venous leg ulcers, second degree burns and donor sites. Active against a broad spectrum of microorganisms including M.R.S.A. Application Thoroughly clean the wound with saline, tap water or Octenalin. Select an appropriate size dressing that will completely cover the wound surface, ensluring2 – 3 cms margin beyond the wound. Apply the dressing with the silver matrix (dark grey surface) touching the wound. Secure in place with an appropriate fixation dressing. Removal Remove fixation and /or secondary dressings, gently remove the Askina Calgitrol Ag. Thoroughly cleanse the wound to remove any residue left from the Askina Calgitrol Ag (dark staining may occur). Contra Indications Not to be used on patients with known silver allergies, or allergies to any other component of the dressing. 66 Protocols 5&6 PROTOCOLS 5 AND 6 BLACK NECROTIC SHALLOW WOUNDS YELLOW BROWN SLOUGHY SHALLOW WOUNDS Granuflex Intrasite Conformable Activheal hydrogel and Clearfilm /Hydrofilm Granuflex Activheal hydrogel and Clearfilm / Hydrofilm Comfeel Paste Comfeel Plus Comfeel Plus Actiform Cool (Backing film on) Actiform Cool (Backing film on) YELLOW BROWN SLOUGHY SHALLOW MOIST WOUNDS Granuflex YELLOW / BROWN SLOUGHY SHALLOW WOUNDS (WET) Aquacel Actiform Cool (Backing film off) Sorbsan flat Intrasite conformable Sorbsan plus Activheal hydrogel Comfeel Plus Aquacel Sorbsan flat BLACK NECROTIC DEEP WOUNDS 68 YELLOW BROWN SLOUGHY DEEP WOUNDS Activheal gel and Aquacel Aquacel Comfeel Paste Comfeel Paste / Granugel Sorbsan flat / packing Sorbsan packing DEBRIDEMENT AND DESLOUGHING SLOUGHY/NECROTIC WOUNDS NB: These wounds will not heal until the slough is removed. Depending on the type and condition of the wound, the slough may be composed of necrotic tissue or a mixture of fibrin and pus, which contains bacteria, leukocytes and significant quantities of DNA protein. Inflammatory mediators may also be present, which can cause inflammation of the skin surrounding the wound. The presence of slough and devitalised tissue will predispose a wound to infection, by acting as a bacteriological culture medium and inhibiting the action of leukocytes in controlling invading organisms. It follows, therefore, that effective wound cleansing is essential if infection is to be avoided and healing is to take place at the optimum rate. Surgical debridement / Versajet therapy are by far the most rapid method, but this may not always be appropriate and alternative techniques are required. COMFEEL PLUS Comfeel Plus hydrocolloid has a range of dressings: Comfeel Plus Ulcer Dressing Comfeel Plus Contour Dressing Comfeel Plus Sacral Dressing Comfeel Plus is made of calcium alginate sodium carboxymethylcellulose, artificial elastomer, tackifier and plasticiser and a top layer made from semi-permeable polyurethane film. Indications Comfeel Plus Ulcer Dressing is indicated for the treatment of leg ulcers and pressure sores, also for superficial burns, superficial partial thickness burns, donor sites and skin abrasions. Comfeel Plus Contour Dressing is indicated for use in treatment of wounds in difficult to dress sites. Comfeel Plus Sacral Dressing is indicated for low to medium exudating sacral wounds. 69 Application Comfeel Plus Ulcer Dressing Use the ‘handles’ to ensure aseptic application. Remove the protective paper. Place the adhesive side to the wound. Ensure that the dressing extends over the edges of the wound by at least 1.5cm to ensure good adhesion. Remove the handle. Comfeel Plus Contour Dressing Remove the protective paper from the centre of the dressing and place the dressing on the wound. Remove the protective paper from the wings without stretching the thin hydrocolloid and gently press, one at a time, to ensure the dressing adheres to the skin. The frame of the dressing acts as a suitable border ensuring good adhesion, providing that the wound edges do not extend beyond the central island. Removal To remove the dressing, press down on the skin. Lift the edge of the dressing all round the wound margin until the edges are free from the skin surface, then remove carefully from the wound, by stretching the dressing to break the adhesive. COMFEEL PASTE Comfeel Paste is composed of sodium carboxymethylcellulose, guar gum, cetostearyl alcohol, white soft paraffin and artificial elastomer. Indications Comfeel Paste is primarily indicated for the management of pressure sores and leg ulcers. It can also be use for filling other cavity wounds to provide added absorption and may be used to enhance debridement to moderate necrosis. Contra-Indications Not to be used on patient allergic to one of more of the components declared. Not to be used on patients with systemic infections such as tuberculosis, syphilis or leprosy until the infection is under medical control. 70 Application Fill the cavity to approximately one third of the wound depth. Then cover with a Comfeel Plus dressing. Removal Irrigate the wound with sterile sodium chloride 0.9% solution to remove any gel left on the wound bed. GRANUFLEX Granuflex consists of a thin polyurethane sheet bonded on to a semi-permeable polyurethane film, which is impermeable to exudate and micro-organisms. The surface of the dressing, to be placed in contact with the wound, is coated with a cross linked adhesive mass containing a dispersion of gelatine, pectin and carboxymethylcellulose together with other polymers and adhesives. Indications Granuflex may be used in the treatment of leg ulcers, pressure sores, minor burns, donor sites (after haemostasis has been achieved) and many types of granulating wounds. If applied to small wounds containing dry slough or necrosis, the dressing prevents the loss of water vapour from the surface of the skin, and this effectively rehydrates the dead tissue, which is then removed by autolysis. Contra-Indications Granuflex should not be used on patients who have a known sensitivity to Granuflex or its components. Strict vegetarians may not wish to use the dressing, because of the gelatine content. Colonisation of chronic wounds is common and is not a contra-indication to the use of Granuflex. Where systemic or local infection develops during the use of the dressing, appropriate adjunctive therapy should be initiated. The use of Granuflex may be continued, but the progress of the wound should be monitored carefully and all treatment should be under medical supervision. NB: The use of Granuflex in the presence of anaerobic infection is not recommended. 71 Application An appropriately sized dressing is removed from its paper backing and lightly pressed into position over the wound. In order to ensure good adhesion to the surrounding skin, a minimum overlap of 2-3cm from the margin of the wound should be allowed. The dressing should be applied with a rolling motion – the dressing must not be stretched. The dressing should be smoothed gently but firmly into place with particular attention being paid to the wound margins. NB: Do not hurry this procedure as initial adhesion improves as the dressing warms up. Removal The frequency of dressing change will be governed by the state of the wound. If large volumes of exudate are produced, daily changes may be required, but on some wounds the dressing may be left in place for 4-5 days before it is changed. It is generally recognised, however, that the dressing is not left in place for longer than 7 days. To remove the dressing, press down on the skin. Lift the edge of the dressing all round the wound margin until the edges are free from the skin surface, and then remove carefully from the wound. Irrigate the wound with sterile sodium chloride 0.9% solution to remove any gel on the wound bed, and then dry the surrounding skin. 72 GRANUGEL Granugel is a sterile gel composed of hydrocolloids (pectin, sodium carboxymethylcellulose) in a clear, viscous vehicle. Granugel has the capacity to donate water, as may be required to hydrate a dry wound, or to absorb fluid as would be required in a lightly exuding wound. Indications Granugel is indicted for the management of dry, necrotic, sloughy and granulating wounds, either superficial or cavity wounds. Contra-Indications Do not use if the patient has a known sensitivity to the gel or other ingredients. When a wound is clinically infected, Granugel may be used together with an appropriate antibiotic therapy and the progress of the wound monitored carefully under medical supervision. Do not use in the presence of anaerobic infection. Application Apply Granugel directly into the wound. Do not fill the wound beyond the level of the surrounding skin. Cover with an appropriate secondary dressing e.g. Granuflex. Granugel should be changed when the cover dressing leaks or for routine dressing changes. On necrotic and sloughy wounds, Granugel should be changed every 3 days. For clean granulating wounds, Granugel can be left on for up to 7 days, depending on the level of exudate. If necessary, the gel can be irrigated with sterile saline. NB: Product – Drug interaction with Povidone Iodine preparations, due to the starch content of the dressing. or iodine AQUACEL Aquacel Hydrofibre Wound Dressing is a soft, sterile non-woven pad of ribbon dressing, composed of hydrocolloid fibres (sodium carboxymethylcellulose). This conformable and highly absorbent dressing interacts with wound exudate and forms a soft gel, which maintains a moist environment for optimal wound healing, debridement and easy removal, with little or no damage to healing tissue. Aquacel has been re-catogorised as a protease modulating dressing. Aquacel locks away harmful proteases that are responsible for delaying wound healing. 73 The dressing may be left in place for up to 7 days. However, when used on heavily exuding wounds or for other clinical reasons, the dressing may have to be changed more frequently. Indications Aquacel is indicated for the management of exuding wounds. These include chronic wounds such as pressure sores and leg ulcers and acute wounds such as abrasions, lacerations, incisions, donor sites and first and second degree burns. This dressing is further intended for use in the management of surgical or traumatic wounds that have been left to heal by secondary intent. For local management of wounds that are prone to bleeding, such as wounds that have been mechanically or surgically debrided, donor sites and traumatic wounds. Aquacel facilitates the control of minor bleeding. Contra-Indications Aquacel should not be used on patients with a known sensitivity to this dressing or its components. Application Aquacel is sterile and should be handled appropriately. Prior to application, the wound may be debrided, if necessary, and then cleansed with an effective cleaning agent, to be determined by the health care professional. Apply Aquacel to the wound site and cover with a moisture retentive secondary dressing. Removal Aquacel should be changed when the dressing becomes saturated with exudate, or when a good clinical practice dictates that the dressing should be changed. This dressing can remain in place for up to 7 days. Gently remove the secondary dressing, according to the package insert of that product. Remove the Aquacel and discard in clinical waste. 74 Occasionally, irrigation of the wound, with normal sterile, is necessary to remove the residual gel without disrupting the delicate granulation tissue. Redress the wound site with a new Aquacel dressing and cover with a secondary dressing as previously described. ACTIFORM COOL Actiform Cool is a hydrogel sheet wound dressing. The dressing is blue in colour with a protective wing to the wound contact side, and a top liner to be left in place, for drier wounds. Indications Actiform Cool is indicted for use on leg ulcers, burns, scalds and radiation therapy. It can be used as a method of relieving pain in the wound bed and under compression for moderate to highly exuding wounds. Contra-Indications Actiform Cool should not be used as a covering for deep, narrow cavities or sinuses. Haemostasis must be achieved before applying the dressing. Application Lightly Exuding Wounds Remove the sterile dressing from the package. First remove one of the overlaid white plastic liners. Position and smooth into place, whist removing the second folded white plastic liner. Take care not to remove the clear top-liner from the back of the dressing, as this is required to position the dressing and maintain hydration. Leave the film top-liner in place and secure with a suitable cover dressing or bandage. Moderate to Heavily Exuding Wounds Remove the sterile dressing from the package and if necessary, cut the dressing to fit the wound. 75 Remove one of the overlaid white plastic liners. Position and smooth into place, whist removing the second folded white plastic liner. Once in place, the top-liner should be removed to allow exudate to pass though into a secondary absorbent dressing or pad and bandage. Removal Actiform Cool should be changed as often as the condition of the wound dictates. The time between dressing changes could be up to 7 days, but in the initial stages, frequent monitoring is recommended. The dressing should be changed at the first sign of strike-through of fluid. Remove the dressing by lifting gently from one corner and peeling back the dressing. If necessary, removal may be facilitated by soaking the dressing with water or normal saline 0.9% to rehydrate any part of the dressing that is dry. As exudate is absorbed into the dressing, a soft gel is formed and the dressing will appear cloudy, swollen and the colour of the exudate. This is normal. ACTIVHEAL HYDROGEL Activheal Hydrogel is an amorphous hydrogel in 15grm tubes. Under an occlusive dressing the aqueous gel protects the wound and aids autolytic debinderment of necrotic tissue therefore facilitating wound healing. Indication for use Hydrogel is designed to maintain a moist wound healing on wounds such as pressure ulcers, leg ulcers, skin graft donor sites and diabetic foot ulcers. Contra – indications Activheal Hydrogel should not be used on third degree burns or surgical implantations. 76 Directions for use Remove the cap from the tube; turn the tube over and allow the plastic collar to drop off. Replace the cap and screw fully to the bottom to pierce the cap. Apply gel to the wound to a depth of 5mm. Do not apply the gel to the healthy skin. Cover the wound with an occlusive dressing i.e. Felm/Hydrogel. This is a single use product discard any left over gel. Removal Change the dressing every two – three days. Clean the wound with normal saline to remove necrotic debris or excess gel. Storage Store at room temperature. Avoid freezing or excessive heat. INTRASITE CONFORMABLE A soft non-woven dressing with a light load of intrasite gel. Indications Hydrogel dressings are most commonly to donate liquid to dry sloughy wounds and facilitates autolytic debridement of necrotic tissue. Ideal on areas of the body where it would be difficult to place hydrogel. Secondary dressings would be required. Removal Remove the secondary dressings, then carefully remove the intrasite conformable dressing, if stuck apply saline to soak the dressing. Contra-indications Not to be used on patients where known allergy / reaction to the hydrogel. 77 SORBSAN Sorbsan is a highly conformable sterile non-woven primary dressing made of calcium alginate BP and is available as flat dressing, packing and ribbon. Sorbsan Plus is hydrophilic, so wound exudate is drawn into the dressing along with contaminating bacteria. Indications There are no known contra-indications to the use of Sorbsan. However, the dressing will be of little value if applied to wounds, which are very dry or completely covered with hard, black necrotic tissue. Lightly exuding wounds are normally considered less appropriate for treatment. The simultaneous use of topical agents, such as antiseptics and antibiotics with alginates may be inappropriate as some of these agents alone may induce reactions. Therefore, their use with Sorbsan may reduce or negate its beneficial effects. Application Sorbsan Plus has a blue backing, which indicated the outside of the dressing. First Sorbsan Application Cleanse the wound with sterile chloride 0.9% solution. (If the site has a completely dry necrotic cover then remove this by an acceptable debriding technique.) Dry the skin around the wound. Select the appropriate size dressing (see presentation table) that will completely cover the wound surface. NB: Apply Sorbsan dressing directly to the wound surface, leaving a margin of at least 2mm around the wound. Cut the dressing to fit the wound. Cover with secondary dressing pad. Secure with surgical tape or bandage as appropriate. 78 Subsequent Dressing Changes Remove the tape or bandage. Lift the dressing and irrigate away any gelled alginate with sterile sodium chloride 0.9% solution, removing the dressing in one piece. Dry the skin around the wound. Select the appropriate size Sorbsan dressing (see presentation table, overleaf) that will completely cover the wound surface. NB: Apply Sorbsan dressing directly to the wound surface, leaving a margin of at least 2mm around the wound. Cut the dressing to fit the wound. Cover with secondary dressing. Secure with surgical tape or bandage as appropriate. Frequency of Dressing Change Dressing changes should normally occur when the area of alginate covering the wound is completely gelled. Therefore, the interval between dressing changes will depend entirely upon the state of the wound. On heavily exuding and sloughy wounds, daily changes may be required at the beginning of treatment, but this may be reduced to twice a week as the healing progresses. Wound Progress The wound may initially appear to increase in size in the early stages of alginate treatment. This is normal, as sloughy tissue is removed from the edges of the wound. This is necessary to promote the healing process. NB: 79 When the wound reaches little or nor exudate levels, it may be more suitable to consider other suitable wound care products. PRESENTATION TABLE TYPE OF DRESSING 80 INDICATIONS FOR USE Flat Dressing Shallow wet wounds and ulcers Packing Large deep open wet wounds Ribbon Small deep open wet wounds Large wet wounds Sinuses Wet wounds in awkward locations e.g. toes and breasts Sorbsan Plus Large shallow, very wet wounds and ulcers Protocols 7&8 PROTOCOLS 7 AND 8 SHALLOW CLEAN WOUNDS HEAVILY EXUDATING MEDIUM EXUDATING Activheal Foam Range Activheal Foam Range Allevyn Allevyn , Allevyn Gentle (1st choice silicone border) Tegaderm Foam Adhesive Mepilex border (2nd choice silicone border) Tegaderm Foam Adhesive Sorbsan Plus Aquacel Xupad – (1st choice) Sorbsan Range Eclypse – (2nd choice) Versiva XC Superabsorbers Kerramax – (1st choice) Drymax – (2nd choice) Aquacel Alione Advadraw The aim is to stimulate epidermal regeneration as quickly as possible. DEEP CLEAN WOUNDS HEAVILY EXUDATING Allevyn Cavity Wound Dressing Sorbsan Packing/Rope Sorbsan Aquacel Aquacel Activheal Foam – island (Adhesive) 82 MEDIUM EXUDATING Activheal foam is a sterile wound dressing consisting of a pink polyurethane membrane coated with pressure sensitive adhesive with a centrally located hydrophilic absorbent polyurethane island. The dressing is self-adhesive, soft and highly absorbent, comfortable and creates the ideal environment for moist wound healing. Application The dressing is applied to the skin with the central part of the dressing in contact with the wound. The dressing has a self-adhesive border; therefore no other secondary dressings are required. Apply the dressing with the pink side up. Activheal Foam – (non-adhesive) The same as the foam island but without the polyurethane membrane and adhesive border. Application The dressing is applied to the skin with the central part of the dressing in contact with the wound. A secondary product is needed to hold the foam in place i.e. bandages, tapes etc. Indication for use Activheal foam dressings may be used on wounds where there is moderate to high exudate. ALLEVYN FOAM Allevyn consists of a layer of soft, hydrophilic polyurethane foam, 4mm thick, bonded onto a polyurethane film. The film, which is permeable to moisture vapour, provides a barrier to the passage of water or wound exudate, and also prevents the passage of micro-organisms into or out of the dressing. The surface of the dressing to be place in contact with the wound is covered with an apertured three-dimensional plastic net, which is claimed to reduce adherence to granulating tissue. The dressing has a high absorbency strike through is prevented by the semipermeable backing. 83 By virtue of these characteristics, the dressing provides a micro-environment at the surface of the wound, which is conducive to moist wound healing, and within limits, independent of the rate of exudate formation. Presentation of the Dressings: Non-adhesive version Adhesive version Shaped dressing – i.e. sacral, heel, etc Sillicone adhesive Indications Allevyn may be applied to a variety of heavily exudating wounds and may be used as a secondary dressing. The silicone adhesive version should be used on patients with fragile skin. Contra-Indications No absolute contra-indication to the use of Allevyn have been reported, but the dressing will be of limited use if applied to a wound covered by a dry scab of black necrotic tissue. This should first be removed surgically or by some other means. The Allevyn heel dressing should not be used as a pressurerelieving device. Application A size of Allevyn should be chosen that would overlap the edges of the wound by 2-3 cm. This is placed with the white side next to the skin. The non-adhesive dressing may be secured with tape or a piece of dressing retention sheet, e.g. Mefix or held in position with a suitable bandage, as appropriate. If necessary, Allevyn may be cut to shape with a pair of sterile scissors. The Allevyn Adhesive should be applied by peeling back the proactive wings and applying the dressing centrally over the wound. Smooth down the edges of the border, to ensure good adhesion. 84 Frequency of Dressing Changes The frequency at which the dressing should be changed depends upon the nature of the wound. On a clean, non-infected wound, it is possible to leave Allevyn in position for up to 4 days, although this will depend upon the amount of exudate produced. Removal The Allevyn Adhesive has a low-tac adhesive, which is dissolved in contact with exudate. To remove the dressing, peel the adhesive border away from the skin, by stretching the dressing to break the adhesive. Irrigate the stuck foam with saline to release it from the skin. AQUACEL Aquacel Hydrofibre Wound Dressing is a soft, sterile non-woven pad of ribbon dressing, composed of hydrocolloid fibres interacts with wound exudate and forms a soft gel, which maintains a moist environment for optimal wound healing, debridement and easy removal, with little or no damage to the healing tissue. Also Aquacel has been re-categorised as a protease modulating dressings, Aquacel locks away the harmful proteases that are responsible for delaying wound healing. The dressing may be left in place up to 7 days. However, when used on heavily exuding wounds, or for other clinical reasons, the dressing may have to be changed more frequently. Indication Aquacel is indicated for the management of exuding wounds. These include chronic wounds, such as pressure sores and leg ulcers and acute wounds such as abrasions, lacerations, incisions, donor sites and first and second degree burns. This dressing is further intended for the use in the management of surgical or traumatic wounds that have been left to heal by secondary intent. For the management of wounds, which are prone to bleeding, such as wounds that have been mechanically or surgically debrided, donor sites and traumatic wounds. Aquacel facilitates the control of minor bleeding. Contra-Indications Aquacel should not be used on patients with a known sensitivity or allergy to any of its components. 85 Application Aquacel is sterile and should be handled appropriately. Prior to application, the wound may be debrided, if necessary and then cleansed with an effective cleansing agent, to be determined by the health care professional. Apply Aquacel to the wound site and cover with a moisture retentive appropriate secondary dressing. Removal Aquacel should be changed when the dressing becomes saturated with exudate, or when good clinical practice dictates that the dressing should be changed. This dressing can remain in place for up to 7 days. Gently remove the secondary dressing, according to the package insert of that product. Remove the Aquacel and discard in clinical waste. Occasionally irrigation of the wound with normal saline or tap water is necessary, to remove the residual gel without disrupting the delicate granulation tissue. Redress the wound site with a new Aquacel dressing and cover with a secondary dressing as previously described. ALLEVYN CAVITY WOUND DRESSING Allevyn Cavity Wound Dressing is a highly comfortable, absorbent dressing consisting of a soft, polymeric outer membrane with a three-dimensional honeycomb like structure containing a mass of hydrophilic polyurethane foam chips. The outer membrane, which provides an effective low adherent wound contact layer is perforated to allow exudate to be drawn into the interior of the dressing where it is absorbed and retained by the polyurethane foam chips. The dressings are available in a range of shapes and sizes for the management of cavity wounds. Indications Allevyn Cavity Wound Dressing is indicated for the extended management of full thickness cavity wounds healing be secondary intention, or for the temporary treatment of wounds prior to delayed primary closure. Contra-Indications There are no absolute contra-indications to the use of Allevyn Cavity Wound Dressing, but the dressing is not appropriate for the management of very dry or relatively superficial wounds. 86 Application An appropriate size dressing should be gently inserted into the wound and held in place with tape, a semi-permeable film dressing or a bandage, as appropriate. If necessary, depending upon the condition and location of the wound, an absorbent secondary dressing may be applied. Removal The interval between dressing changes will depend mainly on the condition of the wound and the amount of exudate produced. Heavily exudating or sloughy wounds may require that the dressing is changed daily, but in clean lightly exudating wounds the dressing may be left undisturbed for 2-3 days or sometimes even longer. If the wound is infected however, frequent changes are advisable. NB: Allevyn Cavity Wound Dressing must not be cut open. TEGADERM FOAM ADHESIVE A polyurethane foam dressing with a film adhesive border. The dressing is highly absorbent and the film backing / border allows moisture vapour transfer. INDICATIONS Tegaderm foam adhesive dressing can be used as a primary or secondary dressing On moderate to highly exudating wounds. APPLICATION Select a dressing large enough to ensure the foam overlaps the wound by 2 – 3 cms. Remove the backing paper and place the dressing onto the wound, smooth down the film border. Remove the individual ‘spider like’ backing papers from the centre of the dressing to the outside, smoothing down the film to the contours of the body. REMOVAL Gently lift one edge of the film border, place a hand on to the dressing, pull the film laterally to break the adhesive, thereby reducing the pain at dressing changes that some adhesive dressings can cause. Lift the hand supporting the dressing, move over and repeat the lateral stretching of the film until the dressing can be lifted off the wound. CONTRA INDICATIONS Not to be used on patients with known sensitivity to film dressings 87 SORBSAN Sorbsan is a highly conformable sterile non-woven primary dressing made of calcium alginate BP and is available as flat dressing, packing and ribbon. Sorbsan Plus is hydrophilic, so wound exudate is drawn into the dressing along with contaminating bacteria. Indications There are no known contra-indications to the use of Sorbsan. However, the dressing will be of little value if applied to wounds, which are very dry or completely covered with hard, black necrotic tissue. Lightly exuding wounds are normally considered less appropriate for treatment. The simultaneous use of topical agents, such as antiseptics and antibiotics with alginates may be inappropriate as some of these agents alone may induce reactions. Therefore, their use with Sorbsan may reduce or negate its beneficial effects. Application Sorbsan Plus has a blue backing, which indicated the outside of the dressing. First Sorbsan Application Cleanse the wound with sterile chloride 0.9% solution. (If the site has a completely dry necrotic cover then remove this by an acceptable debriding technique.) Dry the skin around the wound. Select the appropriate size dressing (see presentation table) that will completely cover the wound surface. NB: Apply Sorbsan dressing directly to the wound surface, leaving a margin of at least 2mm around the wound. Cut the dressing to fit the wound Cover with secondary dressing pad. Secure with surgical tape or bandage as appropriate. 88 Subsequent Dressing Changes Remove the tape or bandage. Lift the dressing and irrigate away any gelled alginate with sterile sodium chloride 0.9% solution, removing the dressing in one piece. Dry the skin around the wound. Select the appropriate size Sorbsan dressing (see presentation table, overleaf) that will completely cover the wound surface. NB: Apply Sorbsan dressing directly to the wound surface, leaving a margin of at least 2mm around the wound. Cut the dressing to fit the wound. Cover with secondary dressing. Secure with surgical tape or bandage as appropriate. Frequency of Dressing Change Dressing changes should normally occur when the area of alginate covering the wound is completely gelled. Therefore, the interval between dressing changes will depend entirely upon the state of the wound. On heavily exuding and sloughy wounds, daily changes may be required at the beginning of treatment, but this may be reduced to twice a week as the healing progresses. Wound Progress The wound may initially appear to increase in size in the early stages of alginate treatment. This is normal, as sloughy tissue is removed from the edges of the wound. This is necessary to promote the healing process. NB: 89 When the wound reaches little or nor exudate levels, it may be more suitable to consider other suitable wound care products. PRESENTATION TABLE TYPE OF DRESSING INDICATIONS FOR USE Flat Dressing Shallow wet wounds and ulcers Packing Large deep open wet wounds Ribbon Small deep open wet wounds Large wet wounds Sinuses Wet wounds in awkward locations e.g. toes and breasts Sorbsan Plus Large shallow, very wet wounds and ulcers ECLYPSE Eclypse is an absorbent cellulose-dressing pad, with a fluid repellent backing. Indications Eclypse can be used as a primary or secondary dressing for medium to heavily exuding wounds. XUPAD Xupad is an absorbent dressing pa. Indications for use Can be used on all types of wet wounds as primary or secondary dressing. Can be secured in place by using surgical tape or bandages. 90 KERRAMAX / DRYMAX A super absorbent polyacrylate primary or secondary dressing. locks in fluid swelling to more than 10 times its thickness. INDICATIONS All types of wet / moderate to highly exudating wounds. Can be used under compression bandages. Locks fluid in the dressing. Locks away bacteria. APPLICATION Either side of dressing can be placed on the wound. VERSIVA XC Versiva XC is a non-adhesive gelling foam dressing. It is a sterile wound dressing consisting of: a top polyurethane foam/film layer, an absorptive non-woven fibrous layer and a thin, non adhesive wound contact layer. The outer foam/film layer protects the wound from external contaminants and manages the moisture vapour transmission of the exudate absorbed by the dressing. The non-woven fibrous layer absorbs and retains exudate by forming a cohesive gel. The dressing absorbs wound fluid and creates a moist environment to aid autolytic debridement without damaging new tissue. Indications Versiva X may be used on a wide variety of wound types as a primary or secondary dressing. It may be used alone or in combination with other wound care products. Contraindications It should not be used on individuals who are sensitive to or have had an allergic reaction to any of the components. Application Choose a dressing size and shape to ensure that the central absorbent pad is larger than the wound area. Line up the centre of the dressing with the centre of the wound. It may be cut to size for convenience. Maximum recommended wear time is up to 7 days. 91 Removal Press down gently on the skin and lift one corner of the dressing. Continue until all edges are free. Carefully lift away the dressing and discard according to local protocol. ADVADRAW A rapid capillary action dressing. A three layer dressing designed to rapidly absorb exudates and intestinal fluids and optimize conditions for healing at the wound interface. Rapid capillary action dressings have a central wicking layer that quickly distributes absorbed fluid throughout the dressing and creates sustained movement of fluid away from the wound bed. It is made from a triple layer of polyester and viscose fibres with a perforated wound contact polymer film on either side to prevent adhesion of the newly formed tissue to the dressing. The non-adherent film readily allows passage of fluid but prevents granulation tissue adhering to the dressing. Indications Wet wounds, sloughy wounds, deep or shallow wounds, wounds with a deep cavity or sinus where previously topical negative pressure therapy has been problematic for the patient. Application Advadraw is available in a range of rectangular sizes as well as a spiral. It can be cut to size or a narrow ribbon to fit into larger sinus / channelled wound. The dressing can be left in place for up to 7 days. Advadraw can be used under compression bandages. It can be held in place by a film, surgical tape or a secondary dressing. CONTRA-INDICATIONS Advadraw must not be used on wounds that are actively bleeding 92 MEPILEX BORDER An absorbent soft silicone dressing with polyurethane foam with an adhesive border. The dressing has 5 layers: 1. Safetac technology wound contact layer to minimise pain and trauma. 2. The absorption layer attracts moisture / exudate rapidly and prevents it returning to the wound. 3. The spreading layer distributes exudate evenly to maximise the full surface area of the retention layer above. 4. The highly absorbent retention layer stores exudate and ‘locks’ it safely from the wound and surrounding skin. 5. Shower-proof barrier and viral barrier backing film, with high permeability to allow effective vapour transmission Indications For use on patients with fragile skin on all types of wounds. Application Pull back the backing papers to expose the central region of the dressing, place over the wound, gently remove each backing paper, smoothing down the dressing at the same time. The dressing can be lifted and adjusted to ensure a good fit around shapes of the body the silicone adhesive will remain effective. Removal Lift one corner of the dressing, gently pull back the dressing from the wound. The safe-tac technology ensures that no epidermal cells are removed, therefore there is no skin stripping at removal of a dressing. 93 ALIONE Alione is a hydrocapilliary dressing, which is highly absorbent, which provides an optimal moist wound-healing environment. It is an all-in-one dressing. The wound contact layer is a non-adherent material; the inner layer is a highly absorbent material that works similar to the principles of a disposable nappy, locking the moisture in the hydrocapilliary fibres. The outer layer is a semi-permeable water resistant, bacteria proof film, which allows moisture vapour transfer. It comes in two presentations: Alione Adhesive (with a hydrocolloid adhesive) Alione Non-adhesive Indications For use on pressure ulcers, leg ulcers, leaking surgical wounds and very wet wounds. Contra-Indications Not to be used on dry wounds. Application Alione Adhesive Use the handles on the films of the dressing to ensure aseptic application, remove the larger paper covering and apply the dressing over the wound. Then remove the remaining plastic film ensuring the dressing is smoothed down to achieve good adhesion. Alione Non-adhesive Apply directly over the wound and secure in place with bandages Removal Alione Adhesive To remove the dressing, lift a corner of the adhesive border. Place the flat of one hand over the dressing; with the other hand stretch the hydrocolloid border to break the adhesive, work around the border until the entire adhesive is loose. Gently remove the dressing. If any part of the dressing is stuck to the wound, irrigate it with normal sterile saline 0.9%. Alione Non-adhesive Remove by gently lifting the dressing from the wound. If any part of the dressing is stuck to the wound, irrigate with normal saline 0.9% or tap water. 94 Protocol 9 95 PLEASE NOTE Products on Protocol 9 Are to be prescribed by a Doctor or Extended Prescriber ONLY 96 PROTOCOLS 9 Dressing and Therapies Under Specialist Advice Only THERAPY Maggot Therapy (Larvae) Topical Negative Pressure Therapy (VAC, Venturi, PICO) Flowtron Therapy Versajet Therapy DRESSINGS Acticoat Acticoat Absorbent Promogran / Prisma 97 SPECIALIST THERAPIES MAGGOT THERAPY (Larvae) Maggots can be used as a bio-surgical debridement method of preparing the wound bed, by removing sloughy tissue and exposing clean healthy tissue. Available on prescription – Contact TV Team. TOPICAL NEGATIVE PRESSURE (TNP) Topical Negative Pressure therapy creates a sealed environment to remove bacteria a exudate from wounds. This promotes a wound bed which will granulate much quicker than with conventional dressings. The three systems available in Barnsley are: debris, Vacuum Assisted Closure (V.A.C) therapy - using foam and a track pad. VAC therapy units deliver controlled negative pressure to the wound and monitor accurate therapy delivery to ensure fast and effective wound healing. The VAC system has Sensa T.R.A.C. technology which enables the monitoring of the negative pressure at the wound site and adjusts accordingly. There are several models of VAC units: VAC ATS – A large non-portable unit ideal for bedfast/immobile patients. Has a short battery back up of 2 – 4 hours which enables transfer of patients to other area. Canister capacity 500 or 1000 mls. VAC Freedom – A small portable unit, battery powered which requires a daily Recharge of the batteries (ideally overnight), leaving the freedom of full mobility whilst carrying the pump in a shoulder bag and having the ability to leave home without compromising the therapy. Canister capacity 300mls. ACTIVAC – The update to the battery powered Freedom unit. A small portable unit with a 14 hour battery life. Having all the benefits of the Freedom pump. Canister capacity 300mls. INFOVAC – the update to the VAC ATS pump. A non portable unit ideal for bedfast immobile patients. Canister capacity 500mls. Application of VAC therapy Follow the procedure in the Royal Marsden clinical procedure manual. 98 Pressures of a VAC therapies are measured in millimetres of mercury (mmHg) in 25 mmHg units. Black foam (granufoam) normal pressure should be 125 mmHg. White foam (versafoam) normal pressure should be 150 mmHg. Contact the Tissue Viability team for guidance on application and prescribing pressures and where necessary reduce the pressure by 25mmHg to prevent complications of bleeding VAC therapy should be used with caution on patients on anticoagulant therapy (Warfarin) VENTURI TNP therapy - using moist gauze and a drain (channel or Flat) There are tow types of Venturi pumps in use in Barnsley. Both are portable and battery powered. Venturi Advanti The larger of the two pumps – with a 600ml capacity canister. The unit is battery powered and requires charging at least 4 hours in 24 hours (ideally over night), leaving the patient fully mobile and able to leave the home during the day. Venturi Compact A small version of the Avanti which is a third of the size bsattery powered with a 300ml capacity canister. The Venturi has a gauze and drain method of delivering the negative pressure to the wound. There are two drain choices: Flat Drain - cut to fit inside the wound Indications: - Shallow or deep wounds - Minimal to heavy exudate - The wound should always be lined with gauze before placing the drain inside - Rationale – tissue will granulate into the drain holes causing pain and bleeding on removal. 99 Channel Drain - can be coiled inside the wound or cut to fit inside the wound Indications: - Shallow or deep wounds - Minimal to heavy exudates - Wounds with tunnelling or undermined areas - Sinus wounds - Requires a layer of moistened gauze between the drain and the wound bed unless managing a sinus or tunnelled area when it can be placed directly down the sinus/tunnel tract - Rationale – Tissue will granulate into the drain holes causing pain and bleeding on removal. Application of Venturi dressings Follow the procedure in the Royal Marsden clinical procedure manual. Pressure for both the Venturi systems are measured in millimetres of mercury 80 mmHg being the standard automatic setting. Pressure can adjust up or down in 5 mmHg unit. Contact the Tissue Viability team for guidance on application or pressure setting. Consumables for the above systems are available on prescription and via the supplies department. When NOT to use Topical Negative Pressure therapy pump Should not be used on patient with actively bleeding wound. Should not be used on wounds with untreated oestemylitis Should not be used on cancerous wounds IF IN ANY DOUBT PLEASE CONTACT THE TISSUE VIABILITY TEAM Consumables for TNP systems are all available on prescription with an exception of the VAC ATS canisters which can be obtained via supplies. 100 PICO – A single use TNP system. Pico consists of a small discrete pump, powered by two ‘AA’ lithium batteries. The pump is coupled to an advanced foam’ dressing which negates the need for a canister. The dressing consists of: * A silicone adhesive wound contact which helps establish and effective seal yet is gentle to the peri-wound * An airlock layer that distributes the negative pressure across the dressing * A superabsorbent layer which holds the wound exudate away from the skin. * A high rate moisture vapour transmission (MVTR) film which allows a one way transpiration of the collected exudate vapour and makes the canister redundant. Pico is supplied in a single pack. It contains one pump and two dressings. The pump life is 7 days. The dressing can be changed once during the 7 days treatment if needed. Additional fixation strips are also supplied allowing the wound to be inspected if required during the 7 days. There are several dressing sizes available. The pressure is set at 80mmHg. Indications Trauma wounds that have been sutured, skin graft sites and post surgical wounds. Application Clean the peri-wound skin to ensure it is free of creams/ointments etc. Each Pico system has a set of application instructions (laminated). Follow the manufacturers guidance. A wound with a slight depth more that 0.5cm can be filled with a AMD gauze (moistened) Kerlix - as used in Talley systems. Pico may be used over the top of a non-adherent layer if required (Silflex/Mepitel/Adaptic touch), for example skin grafts. NB: Keep the laminated Quick Reference guide in the patients home as there are instructions regarding the pump status, alarms and errors (trouble shooting). Removal / Dressing Change To change the dressing within the 7 day period, press the orange button on the pump to stop the Pico therapy. Disconnect the dressing from the pump. Apply the 2 nd dressing to the wound, connect it to the pump. Press the orange button to reinitiate the therapy. 101 The pump will automatically stop functioning after 7 days of use. All the lights will turn off at this point. The dressing should be gently removed and disconnected from the pump, then discarded in clinical waste. Another system may be applied if appropriate. The batteries should be removed from the pump and disposed of as per local policy (battery recycling). The empty pump should be disposed of as clinical waste. 102 FLOWTRON THERAPY Flowtron therapy can be used in the treatment of venous leg ulcers. Flowtron therapy is the use of intermittent pneumatic compression (IPC) to reduce swelling and aid venous return. The first line treatment for venous leg ulcers is by sustained compression, using bandages. Flowtron therapy using the sequential garments has been shown to improve the healing rates in venous leg ulcers. Flowtron Therapy consists of a pump with a variable pressure setting and garments of varying size and lengths for the leg. The therapy is used for 30-60 minutes twice a day, over the top of the bandages. One leg or both legs can be treated at the same time. The patient can use this independently at home, in the community. The garment, which may be knee or thigh high, is attached to the pump and works by gently inflating and deflating, stimulating venous return. VERSAJET – Hydrosurgery System The Versajet II system enables the practitioner to precisely select, excise and evacuate non-viable tissue bacteria and contaminants from wound burns and soft tissue injuries using a jet of saline under controlled pressure. It consists of the Versajet II unit, a hand piece delivering normal saline under high pressure and a collection canister unit. The hand piece is slowly moved over the soft tissue surface, it creates a smooth wound bed while maximising good tissue preservation. The tissue preservation technique reduces time in the wound healing rates by preparing the wound bed for healing. Outcomes Reduces bacterial burden Preserves viable tissue Removes slough, necrosis and debris Minimises peripheral damage Benefits Reduced number of debridements Reduced healing time (compare to conventional methods) Minimises cross infection Reduces treatment costs Versajet II therapy is available in Barnsley via the Tissue Viabilty team and within the diabetes podiatry service. 103 ACTICOAT – This dressing should only be used on wounds that have a confirmed infection following wound swab. TWO WEEK ONLY Acticoat is an absorbent wound dressing that helps to maintain a moist environment at the wound bed. It is an antimicrobial barrier dressing that contains nanocrystalline silver. It contains three layers; an absorbent rayon/polyester inner core sandwiched between outer layers of nanocrystalline silver-coated, low adherent polyethylene net. The low adherent wound contact layer helps minimise trauma at dressing changes. The nanocrystalline silver provides an effective anti-microbial barrier to microbial contamination protecting the wound from invasive pathogen and microorganisms. The nanocrystalline silver is effective against micro-organisms in the wound, helping reduce the risk of cross infection. There are two presentations of Acticoat: Acticoat – effective for 3 days Acticoat 7 – effective for 7 days Indications For use on infected partial and full thickness wounds, pressure ulcers, venous ulcers, diabetic ulcers, burns, donor and recipient graft sites and infected wounds. Contra-Indications Not to be used on patients with a known sensitivity to silver. Not to be used on patients undergoing MRI (Magnetic Resonance Imaging) examinations. 104 Precautions Do not use if the dressing colour is not uniform. For external use only – DO NOT PUT INTO CAVITIES. Not compatible with oil based products i.e. petroleum – DO NOT USE 50/50 OINTMENT. Avoid contact with electrodes or conductive gels during electronic measurements e.g. EEG and ECG. Application Remove the dressing from the packaging using an aseptic technique. Moisten the dressing with water (tap or sterile). DO NOT USE SALINE. Squeeze out any excess water or leave the dressing on the sterile field for approximately 2 minutes. Cut the dressing to the desired shape, using sterile scissors. Apply the dressing to the wound with the blue surface as wound contact. Secure in place with appropriate secondary dressing that will maintain a moist wound-healing environment. Change the dressing depending on the amount of exudate present and the condition of the wound. Frequency of Dressing Changes Acticoat - Every 3 days or sooner if exudate levels dictate Acticoat 7 - Every 7 days Removal Remove the secondary dressing. Should the dressing be dry or adhered to the wound, moisten or soak the dressing with sterile saline 0.9% or tap water, to assist removal and avoid disrupting the healing process. NB: Acticoat may cause transient discolouration of the sounding skin. ACTICOAT ABSORBENT -This dressing should only be used on wounds that have a confirmed infection following wound swab. 105 Acticoat absorbent consists of an absorbent alginate coated in nanocrystalline silver. The dressing is dark grey in appearance. The nanocrystalline silver provides an effective antimicrobial barrier to microbial contamination protecting the wound from invasive pathogenic micro-organisms. In the presence of exudate, the alginate turns to a gel and will help to maintain a moist wound-healing environment. Indication For use on infected full and partial thickness wounds, pressure ulcers, venous ulcers, diabetic ulcers, burns, donor and recipient sites, cavity wounds and infected wet wounds. Contra-Indication Not to be used on patients with known sensitivity to silver. Not to be used on patients with known sensitivity to alginate dressings. Not to be used on patients undergoing MRI (Magnetic Resonance Imaging) examinations. DO NOT USED ON DRY OR LOW EXUDATING WOUNDS. Precautions Do not use if the dressing colour is not uniform. Not to be used in wounds, which are heavily bleeding. Acticoat Absorbent is not compatible with oil-based products such as petroleum (Do not use 50/50 ointment). Avoid contact with electrode or conductive gels, during electronic measurements, e.g. EEG or ECG. Application Remove the Acticoat Absorbent from the packaging using an aseptic technique. Choose a dressing that is slightly larger than the wound. The dressing should have intimate contact with the wound, ensuring the entire surface is covered. Do no overlap onto good skin. The dressing does not need to be moistened prior to application, (only use on exuding wounds). Cut the dressing to shape with sterile scissors or fold into the wound. 106 Secure with an appropriate secondary dressing. Change the dressing as exudate levels dictate. The dressing may be left in place for up to 7 days. Removal Remove the secondary dressing and gently ease off the Acticoat Absorbent. If any areas of the dressing are stuck to the wound, soak thoroughly with sterile saline 0.9% or tap water, to allow the dressing to be removed easily without disrupting the healing wound. NB: Acticoat Absorbent surrounding skin. may cause transient discolouration of the PROMOGRAN / PRISMA Promogran is a dressing, which has a protease modulating matrix. NB: Protease is an enzyme, which breaks down proteins, therefore preventing wound healing if present in a wound. The Promogran is a fibre dressing, which is a hexagon shape (6 sided), and it comes in 2 sizes: 28 cm2 = Approximately 5.3 cm x 5.3 cm 123 cm2 = Approximately 11.1 cm x 11.1 cm Promogran reduces the amount of the enzyme protease in the wound, so that the healing process can progress. Indications The wound bed should be free of necrotic (black) and thick sloughy tissue (yellow). Promogran can be used on pressure ulcers, leg ulcers (both venous and arterial), traumatic wounds, diabetic ulcers, non-healing skin graft donor sites and nonhealing surgical wounds. Infection should be treated before using Promogran, with appropriate antibiotics and anti-microbial dressings. 107 Application Apply Promogran directly onto the wound bed, covering the whole of the wound. Do not overlap onto the surrounding skin. (If the wound is dry, before applying, moisten the dressing with saline.) Sufficient Promogran should be applied to the wound, so that a small amount is still present at the dressing change. (Depending on the size of the wound and the levels of exudate.) Promogran can be layered onto the wound under compression, for dressings that are changed less frequently. Promogran is a bio-degradable gel when in contact with moisture, that will naturally dissolve into the wound. Cover the Promogran with an anti-microbial dressing, such as Actisorb Silver 220 (Activate Charcoal Dressing with Silver) for patients who are susceptible to infection. Or if using Prisma a secondary SIMPLE DRESSING SHOULD BE USED. Secure in place with an appropriate secondary dressing. 108 2.3 Pain and Wound Management Pain relief is often considered to be of secondary importance, with emphasis being placed upon wound healing rates, and the ease of dressings. Although a certain amount of pain or discomfort will almost always occur whenever the skin is damaged or traumatised, it is the responsibility of the nurse to ensure that this is not made worse by subsequent treatments. Pain associated with wound management can be subdivided into 2 categories: first, the pain, which is experienced while the dressing is in place (or immediately following its application); second, the more acute pain, which results when an adherent dressing is removed. Much of the pain experienced with partial thickness wounds is probably caused by stimulation of nerve endings by localised dehydration of the area. The use of semipermeable films and hydrocolloid and hydrogel dressings, that retain moisture, can help ease this situation. Probably the most severe pain is experienced at the time of the dressing. Gauze swabs (both woven and non-woven) and traditional non-adherent dressings, such as paraffin gauze, often cause pain and trauma on removal, due to the granulating tissue growing through the fibres of the dressings. Some wound cleansing solutions containing hypochlorites and acids also cause pain and discomfort. NB: 2.4 Appendix 3 provides examples of pain control charts. Guidelines to Selection of Equipment 2.4.1 DHSS Standard Issue Mattress (No longer purchased in Barnsley health services) The standard mattress does not provide sufficient support for vulnerable patients. The foam within this mattress wears very quickly. All such mattresses need to be replaced every 5 years. 2.4.2 Vaperm, Soft Form, Pentaflex These are examples of thicker and more expensive foam mattresses, but they have a longer lifespan then the DHSS standard issue and provide some pressure reduction. Spenco, Permalux, Bodypillow, Propad etc These mattresses are classed as mattress toppers or overlays and are placed on top of the normal mattress. They provide comfort rather than protection and are washable. The average lifespan of a Spenco is 2 years. NB: See the User Guide on the following pages for examples of use. 2.4.3 Alternating Mattress Therapy This mattress can either be hired or purchased. By completely removing pressure from all parts of the body, during its 7.5 minute cycle, the mattress often reduces the need for frequent repositioning of the patient. This will free valuable nursing time for other nursing care, whilst reducing pain and discomfort for the patient and allowing undisturbed sleep. Alternating therapy increases the supply of oxygen to the wound site, resulting in significant improvements in the healing of pressure sores. However the patient should be repositioning every 2–4 hours using 30 degree tilt and the use of off-loading devises for the heels whilst on the alternating mattress. NB: See the User Guide on the following pages for examples of use. 2.4.4 Overlay Alternating Mattresses These beds should be placed on top of a standard hospital or divan mattress and not directly on the bed base. - Very few overlay alternating mattresses are left in Barnsley. A decision was made to only purchase full mattresses 6 years ago. NB: See the User Guide on the following pages for examples of use. 2.4.5 Sheepskins Sheepskins do not relieve pressure but can be very effective when used in conjunction with other support systems, as they keep the skin dry and reduce friction. The patient states they offers some comfort as some alternating mattresses can feel very hard. 2.4.6 Chair Cushions and Devices Any patient confined to a wheelchair should have a chair cushion. Alternating cushions are available for high risk patients – these should not be placed in a wheelchair as mains supply is needed. NB: 110 See the User Guide on the following pages for examples of use. 2.4.7 User Guide Pressure Reduction Equipment – Seating Systems COMFORT LOW RISK MEDIUM RISK HIGH RISK VERY HIGH RISK Care Lite II Dunlopillo Nester Cushion Proactive II Proactive II Transoft Seat Cushion Transflo Seat Cushion Supatec Multi-Tec Eclipse Alternating Cushion Eclipse Full Lumbar Alternating Cushion Vaperm Cushion Alpha Trancell Multi-Tec Flotech Plus AirWorks CareChair Propad Fibre Cushion Propad Flotech Eclipse Alternating Cushion STM 3 STM 4 Permaflow Cushion Permaflow Cushion STM2 Repose Contur (recliner chair/inflateable device) Spenco 111 2.4.8 User Guide Pressure Reduction Equipment – Lying Systems COMFORT MEDIUM RISK HIGH RISK VERY HIGH RISK Vaperm Mattress Superdown Overlay Pentaflex Overture – Overlay Viaclin – Overlay Aircare – Overlay Extracare Plus Bi-Wave Convertible II Cairwave / Airwave Unidown Overlay Softform Mattress Propad Overlay Alpha Excell – Overlay AlphaTrancell Autologic Sidhill Trio Softform Mattress Propad Overlay Permaflow Overlay Memaflex Overlay Memaflex Mattress Eclypse Phase III Quattro Prime Permaflow Overlay Transform Mattress Medicus First Step Mattress Topper Transair PPS 2000 Spenco Overlay Premier Mattress Therapulse Pulsation Bed System Sheepskins Sidhill Plus 2 Carelite II LOW RISK Transform Mattress 112 2.4.9 User Guide Pressure Reduction Equipment – Specialist Beds COMPANY KCI KCI KCI LYNETTE TYPE OF MATTRESS PEDICARE Paediatric Critical Care System (Cot) MONARCH Low Air Loss Therapy (Bed) MAGNUM Low Air Loss Therapy (Bed) LATERA MOST SUITABLE USE An air support surface providing pulsation therapy and controlled air suspension therapy for paediatric patients. Built-in digital scale for weighing patients. Built-in heater. Suitable for patients 18-25 stone in weight. Provides complete pressure relief. Built-in digital scale, for weighing patients. Built-in heater. Suitable for patients up to 57 stone in weight, can sit/stand the patient unaided. Built-in digital scale for weighing patients. Built-in heater. Lateral rotation bed to aid 30 degree tilt. Suitable for patients up to 29 stones 113 COMPANY TYPE OF MATTRESS MOST SUITABLE USE EGERTON PARAGON 8000 Cardiac Bed Able to provide the traditional cardiac posture, where the patient’s legs fall naturally to the dependant position as the back is raised. EGERTON PARAGON 5000 Air Fluidised Bed Paragon 5000W – Wider, to accommodate the larger patient. EGERTON PARAGON 9000 Turning Bed Paragon 5000L – for use when mobilising the patient or in the domiciliary situation. Provides extensive range of movements to facilitate the repositioning of all patients, irrespective of how immobile, heavy, seriously ill or severely injured. The lists of equipment are not exhaustive, merely a selection of the various types of mattresses available. The choice of mattress should be determined by the individual patient’s requirements and to the hirer’s preference. This guide offers basic information only. The flow charts, see appendix 4, provide a quick guide to selecting the most appropriate equipment. Any other companies supplying these products will be more than happy to visit and arrange demonstrations for you. 114 2.5 Factors Affecting Healing 2.5.1 Systemic Infection A severe systemic infection can lead to breakdown of healthy tissue. Control of systemic infection is essential to obtain wound healing. 2.5.2 Diabetes Diabetic patients not only have the primary metabolic abnormalities, but an increased susceptibility to infection. Often associated with decreased vascular efficiency. 2.5.3 Carcinoma The poor healing ability of patients suffering from a malignancy is well recognised. Cytotoxic therapy and irradiation affect the process of cell division. 2.5.4 Anaemia Reduction in haemoglobin concentration decreased the capacity of the blood to transport and deliver oxygen to the tissues. 2.5.5 Poor Nutritional State Deficiency in essential vitamins, protein, calcium, vitamins C and A contributes to slowing down the rate of healing. 2.5.6 Reduced Immunity The wound healing process is slowed considerably when the patient’s immune system is compromised by the use of steroids and cytotoxic drugs. 2.5.7 Poor Circulation A good blood supply to the tissue is essential to the healing process. 2.5.8 Wound Contaminated by Impacted Material Impacted material or foreign bodies present in the wound may affect healing, by causing infection, irritation or becoming covered by granulating tissue. The presence of dead tissue can cause secondary wound breakdown. 2.5.9 Position of the Wound Wounds situated in difficult sites can be a problem to keep clean and free from interference wounds in folds of skin i.e. the apron of the abdomen are suseptable to fungal infections. 2.5.10 Local Infection of Wound Acute local infection is visually evident with the wound being swollen, hot and inflamed. Surrounding cellulitis may occur. If the infection is not treated bacteraemia septicaemia and death can follow. 2.6 Medical and Surgical Measures Pressure ulcers, their prevention and management, have historically been seen as a nursing problem but as Section 1.1 shows, the multi-disciplinary team demonstrates, every member of the health care team has a contribution to make. For certain patients the involvement of the relevant responsible doctor is vital if a ulcer is to be avoided or for healing to take place and examples of these are given also in Part 2 Section 2.1 - General assessment of the patient, routine investigations etc. This is particularly important consideration for patients who may not routinely be seen by a doctor, for example patients in the community or in a nursing home. Below are some further examples of where medical treatment beyond prescribing is necessary. 2.7 Medical intervention in cases of locally infected ulcers, use of appropriate antibiotic therapy etc can assist in the healing process. Surgical debridement of necrotic tissue at an early stage can greatly hasten the healing process. Many ulcers can be rapidly and effectively be treated by plastic surgery if referred early enough. Unfortunately this referral is usually left too late, the pressure ulcer deteriorates, patients are cachexic and septicaemic and beyond help. This is unsatisfactory, and any patient with serious pressure damage i.e. Grade 3 or above, should be referred to a plastic surgeon at an early stage. Transporting Patients 2.7.1 Internal Transportation of Patients Where patients with or at risk of pressure damage are required to attend other departments for tests, investigations etc this should be organised to address the following: 2.7.2 Mode of Transport A trolley may be more suitable for a patient with a pressure ulcer on their sacrum or buttocks even though they might otherwise be considered fit to be moved in a wheelchair. Where trolley overlays are available, these should be used for vulnerable patients. Wheelchairs without both footplates must not be used to transport patients. Where a wheelchair cushion is available, this should be used. Where patients are being moved from bed to trolley, attention should be given to preventing shearing forces on the patients skin. Slide sheets and transfer boards should be used. 116 2.7.3 Minimising Delays Departments will have systems to fast-track patients with or at risk of developing pressure damage. When arranging tests in other departments, the patient’s status should be notified to the department concerned. When a patient is escorted by a member of the nursing team they should ensure that the patient receives appropriate pressure relieving care during the time spent away from the ward. Where the care of the patient is temporarily transferred to another department, the nurse responsible for the patient should inform the department of the care provided. 2.7.4 External Transportation of Patients When arranging ambulance transport for patients, the ambulance service will be notified where the patient has, or is at risk of developing, pressure damage. The ambulance service will be asked to supply a stretcher ambulance for all patients with a pressure ulcer on their sacrum or buttocks or at high risk of developing pressure damage. If a patient is being taken to a hospital for tests, the relevant department should be notified if the patient is at risk, to endeavour to minimise delays. Where a stretcher overlay is used to transport the patient, this should be used on any trolley at the hospital, where the patient is attending for tests, and returned with the patient on the return journey. Prior to transporting patients, the patient should be nursed wherever possible in a position that they will not be travelling in, i.e. a patient who will travel laying on their back, should be nursed on their side for two hours prior to the journey. On the return to the ward/home, the patient should have their position altered again after the journey. The nurse escorting the patient will have continuing responsibility for ensuring that any pressure area care required during the time away from the ward/home is delivered. Where a patient will not have a nurse escort, the nurse handing over care to the ambulance service will detail the care required during the journey. 2.7.5 Patients Requiring Stretcher Overlays When booking the ambulance for a patient with, or at risk of developing, pressure damage, it is necessary to identify on the booking form the following information: Patient at risk of or with pressure damage Stretcher required, with or without overlay This information can be recorded on the special instructions section on the form. 117 2.7.6 Action by Ambulance Crew Upon receipt of the call, where a stretcher overlay is required, the ambulance crew will collect the overlay from the nearest available point. Propad overlays will be stored at: Barnsley Ambulance Station Hoyland Ambulance Station BHNFT Ambulance Liaison Station - I overlay available - 1 overlay available - 2 overlays available 2.7.7 Handover – Continuity of Care The ambulance crew will be briefed by the nurse/carer of the patient’s special needs during the journey. 2.8 Discharge and Transfer When discharging a patient with, or at risk of, pressure damage the same principle apply as with any discharge and transfer. Preparation and planning should begin as early as possible in order that continuity of care can be achieved. Information that should be notified in advance of the discharge/transfer within the written document should include: 1. 2. 3. 4. Patient’s risk assessment score Grade of ulcer – Clinitron Grading System Site(s) of ulcer Present dressings and date last changed If a patient requires nursing on a pressure relieving bed, the receiving area will require sufficient notice of the discharge/transfer in order that they may arrange to provide similar support. Also send photocopies of the Wound Assessment Chart, Tissue Viability Advice sheet (if in use) and an Root Cause Analysis (if applicable). 2.9 Monitoring Information in Nursing Care Homes The purpose of monitoring information is to ascertain the number of residents in Barnsley nursing homeswith pressure damage and its origins, to identify problem areas, implement prevention programmes – including staff training, and evaluate the overall effectiveness of existing prevention programmes. It is not a tool to be used punitively. 2.9.1 Prevalence Monitoring Information The purpose on monitoring prevalence is to find out, at a point in time, the overall number of patients with pressure damage currently being cared for by the hospital, community services or the nursing or residential home. It will distinguish between those admitted with pressure damage and those who developed damage since admission. 118 Caution should be used in interpreting the latter information; a patient admitted as an emergency having being found lying on the floor of their home, may arrive at Accident and Emergency with intact skin. The damage to their skin however, will have already begun. Data will be collected twice yearly 2.9.2 Pressure Ulcer Reporting Process All pressure damage grade II and above will be recording on an incident report via Datix including patient admitted to your care with existing pressure damage and patients who develop pressure damage whilst in your care. (follow flow chart on next page). 2.9.3 R.C.A. (Root Cause Analysis) All pressure ulcers grade III and above should have a R.C.A with action plan completed including patients admitted with existing grade III or above and patients who develop grade III or above whilst in your care (see following forms). The incident report with an attached RCA should be sent via the Datix system to the patient safety department. 119 PRESSURE ULCER REPORTING PROCESS Patient admitted with pressure ulcer Complete Incident Report via Datix To include: Grade, where ulcer originated from (if known i.e BHNFT, Care Home), site(s) of wound, number of pressure ulcers. Also complete Incidence Report via Datix If patient develops pressure ulcer whilst in your care: Date pressure ulcer identified & date of admission to your care Responsible person to complete the investigation report on Datix for Grades II and above (Ward/Unit Manager- District Nurse) Community Patients: With an RCA in place who are admitted to BHNFT – Fax or Email a copy to Ian Boldy - Safeguarding Adults Fax No: 01226 435396 Email: ian.boldy@nhs.net Residential patients: Full Root Cause Analysis (RCA) for Grade III and above (Sister/District Nurse) Attach a copy of RCA To Datrix Report Patient Safety sends e-mail to Lead Nurse or Matron for your area & Lead TVN and send copy to: Leave a copy to be attached to care home’s hospital admission pro forma to take in case of emergency admission In-patients: On discharge from the ward, photocopy the RCA and send to discharge destination i.e. Nursing Home, Residential Home, District nurse team etc. Patient Safety Department Email to Lead Tissue Viability Nurse Tissue viability Nurse Investigates Patient Safety Department at Kendray Hospital Process new attachment Patient Safety Department: Provide monthly report for Matron/District Nurse Lead & Tissue Viability Nurse 120 2.94 Incidence & Prevalence Monitoring in Nursing Home Monthly statistics are collected from nursing homes and returned to the Community Tissue Viablity Service. Root cause analysis forms will be completed for all pressure ulcers grade 3 and above by a member of the tissue viability team. Reporting forms for incidence and prevalence monitoring within Barnsley nursing homes are on next pages. 121 Community Tissue Viability Service Barnsley Business Unit SWYPT Mount Vernon Hospital Mount Vernon Road Barnsley S70 4DP Tel: 01226 433215 Fax: 01226 433359 DATE Manager/s Barnsley Nursing / Care Homes Dear Manager RE: MONTHLY INCIDENCE & PREVALENCE MONITORING FIGURES Please find enclosed copy of the pressure ulcer Incidence & Prevalence forms (sheet 1 & sheet 2). Could you please familiarise yourself with the new forms and ensure they are completed accurately. Residents with more than one pressure ulcer need all wounds documenting and grading on the form. It will be the responsibility of each Care Home to complete both forms on the 20th of each month and post them to Carmen Kilner, Tissue Viability Secretary (return address labels enclosed). Your PROMPT RETURN by the 25th is essential. Failure to return this information could trigger a low level concern being raised with the commissioners. Yours sincerely Lynne Hepworth Lead Tissue Viability Specialist Nurse 122 NURSING / CARE HOMES INCIDENCE & PREVALENCE MONITORING - Sheet 1 PRESSURE DAMAGE MONTH COMPLETED: ……………………………………………………………. COMPLETED BY: ………………………………………………………………….. CARE HOME: ………………………………… Tel No: …………………………. A Number of nursing residents in the care home B Number of nursing residents AT RISK (i.e. Norton Score 14 or below or Waterlow 10 or above) C Number of nursing residents at risk WITHOUT Pressure Damage D Number of nursing residents at risk WITH Pressure Damage Check FORMULA - Add C + D should = B E Number of nursing residents who developed Pressure Damage whilst in YOUR NURSING CARE Please complete an incidence form for grade ΙΙ and above and submit the form to your care home manager Please complete sheet 1 & 2 on the 20th of each month and post both sheets to the Tissue Viability Office by the 25th of each month. Many thanks Lynne Hepworth Lead Tissue Viability Nurse Specialist Tel: 01226 4332 123 INCIDENCE & PREVALENCE MONITORING PRESSURE DAMAGE – TISSUE VIABILITY INFORMATION - Sheet 2 Please complete and enter all patients with any pressure damage or pressure care intervention. All pressure ulcers need documenting as some patients may have more than one pressure ulcer. Form completed by: …………………………… NHS Number Residents Initials D.O.B SEX M/F Care Home: …………….………………….. Pressure ulcer present on admission to care home Date pressure ulcer occurred Site of pressure ulcer Grade of pressure ulcer Month end: ……………… Reposition chart in place Y/N Frequency of re-positioning Name of mattress in use Y/N Please keep a photocopy of this form for your record 124 PART 3 POLICIES FOR SPECIALIST AREAS Ambulance Services Education and Training Equipment Assessment of the Patient’s Risk Transferring Patients General Prevention Measures Accident and Emergency Department Assessment Equipment Trolley Patients Incontinence Specific Nursing Action Transfer/Liaison with other Departments Wards Transfer to other Hospitals/Nursing Homes Staff Training/Introduction Operating Theatres X-ray and Departments Patients with Spinal Injuries POLICIES FOR SPECIALIST AREAS 3.1 Ambulance Service 3.1.1 Education and Training There will be a staff education and training programme, which covers the following areas: Lifting, moving and positioning of patients to prevent damaged to their skin Assessment of the patient and their risk of developing pressure damage Prevention of pressure damage through identification of contributing factors and action, where possible, to minimise or remove these contributing factors 3.1.2 Equipment Pressure relieving equipment and aids should be of proven effectiveness. The Department of Health Medical Devices Directorate evaluates pressure relieving equipment and produces reports available free to the NHS. Pressure relieving equipment and aids will be cleaned, maintained and replaced in accordance with the manufacturer’s instructions. 3.1.3 Assessment of the Patient’s Risk Patients’ whose first contact with the health services is with the ambulance service e.g. as a result on a 999 call, will have their risk of developing pressure damage assessed using the Modified Andersen Pressure Risk Screening system. The ambulance staff will document the Modified Andersen score and will communicate this to the receiving hospital staff, along with any other contributory factors, e.g. the situation and position that the patient was found in. 3.1.4 Transferring Patients Patients being transferred from one health care unit to another, either permanently or for investigations, should have their risk of pressure damage noted to the ambulance services at the time of booking the ambulance. When arranging ambulances for at risk patients, the ambulance service will endeavour to minimise delays in transporting these patients. Where stretcher overlays are available, these should be used for vulnerable patients. 127 Where a nurse is escorting a patient, the responsibility for ensuring appropriate care for the patient to prevent further or new pressure damage will rest with the nurse. The ambulance service will cooperate with the nurse to provide that care and will ensure that when moving or positioning the patient, due regard is given to preventing skin damage. Where a patient is to be transferred without a nurse escort, particularly where the journey time is in excess of 2 hours, it is the responsibility of the nurse handing over care to the ambulance service to detail the care required by the patient during the journey. This will include positioning, easing of pressure areas and how frequently this will be required. (See Section 2.7 – Transporting patients with pressure damage) 3.1.5 General Prevention Measures For all patients being transferred by ambulance, certain simple measures can be taken in order to minimise new or further pressure damage: Remove wet clothing, where possible Ensure the patient is not lying on creased linen or clothing. Re-position clothing to ensure that zips etc do not lie beneath the patient. Items in trouser pockets, such as keys, should be removed. Ambulance stretcher covers that have ironed-in creases, darns or patches should be rejected and returned to the laundry for re-laundering or disposal, as appropriate. Use pressure relieving aids where available. When lifting or moving, always ensure that the patient is lifted clear of the surface beneath them to prevent shearing forces on their skin. For patients undergoing long journeys, without a nurse escort, the protocol is a basic guide to care (See Appendix 2). The ambulance crew should, however, always obtain advice from the nurse handing over care. 128 3.2 Accident and Emergency Department 3.2.1 Assessment All trolley patients must be assessed for their risk of developing pressure damage using the Anderson Score. Certain patients will always be classed at high risk and must be attended to immediately. These patients are those who are: Unconscious Paralysed Grossly dehydrated, or Suffering from major trauma/surgery The assessment must be made on the Anderson scoring sheet and a report made of the nursing action taken. Where the patient is identified as being at risk or where existing pressure damage is found, a pressure damage prevention programme must commence immediately. 3.2.2 Equipment Ensure the patient is placed on a trolley with a pressure relieving mattress. Ensure that a minimum of three pillows, are available to aid positioning. Stretcher covers/padding should be free from creases, soiling or wrinkles. Trolley Mattresses that are damaged must be reported and action taken immediately. Damaged equipment or linen must not be used. 3.2.3 Trolley Patients Remove outer clothing to prevent damaged from lying on zips, buttons etc. Gowns must be made of soft material. NB: Gowns should not be fastened or tucked beneath patients lying on trolleys. 3.2.4 Incontinence All patients who are soiled must be attended to immediately. Patients confined to a bed/trolley should be offered bedpans or urinals as necessary. 129 3.2.5 Specific Nursing Action Trolley patients should have their pressure areas checked for signs of reddening at regular intervals. Any changes should be recorded, including action taken. Patients confined to a wheelchair due to their injury should be stood or lifted at least every 30 minutes to relieve pressure. 3.2.6 Transfer/Liaison with other Departments The presence of pressure damage or risk will be noted on the X-ray card and the radiographer informed of the risk. Patients at high risk of pressure damage should remain in the A&E Department until the radiographer is ready for them. This will allow nursing staff to continue pressure area care. 3.2.7 Wards The ward will be notified by telephone of the presence of pressure damage/risk and the relevant score. A copy of the ‘at risk’ score and action taken will be sent to the ward. 3.2.8 Transfer to other Hospitals/Nursing Homes When booking ambulance transport the presence/risk of pressure damage with the relevant ‘at risk’ score will be made known. A Propad stretcher overlay will be requested. The ambulance crew will also be notified of the pressure damage/risk. The receiving unit will be advised by telephone of the presence of pressure damage/risk. A copy of the nurse transfer form will be sent to the receiving unit or ward. 3.2.9 Staff Training/Induction All new staff to the department will be asked to read of this policy and the system explained to them by a registered nurse. Staff will be expected to up-date their knowledge and attend lectures, seminars etc when the opportunity arises. All staff will be aware of Barnsley Hospital NHS Foundation Trust’s Moving and Handling procedure. 130 3.3 Operating Theatres The patient’s safety and comfort whilst in theatre is the shared responsibility of nursing staff, operating department assistants, surgeons and anaesthetists. Aims of the policy: To prevent pressure damage occurring whilst the patient is in theatre To manage the care of pressure damaged already present 131 The following guidelines will apply throughout the patient’s stay in theatre: CRITERIA GUIDELINES ACTION Waterlow Score 10+ Medium to low risk patient Thick mattress Heel supports Oasis pressure pad Waterlow Score 15+ High risk patient Thick mattress Heel supports Oasis pressure pad Other risk factors Eczema, ulcers, dry fragile Thick mattress skin or long-term steroid Heel supports therapy Oasis pressure pad Position on theatre table other than supine Lateral Thick mattress Heel supports Oasis pressure pad Lithotomy/ Lloyd Davies Thick mattress Padding around ankles and feet or jelly stirrups Oasis pressure pad Prone/knee chest Thick mattress Heel supports Pillows to support chest Induced hypotension Patients at risk due decreased vascularity extremities to Thick mattress to Heel supports Oasis pressure pad Pressure sores present Named nurse on ward to Check adequate write sites of sores on protection before, theatre check sheet during and after operation Thick mattress Heel supports Oasis pressure pad 132 3.4 X-ray and Departments The patient’s safety and comfort whilst in the X-ray Department is the responsibility of the radiologists, radiographers and assistant radiographers, nurses and portering staff. It is the responsibility of the ward or department that is sending the patients for an x-ray to identify patients already with pressure damage or those who are at high risk of developing pressure damage, this will be done by marking the x-ray card with a red dot in the top right hand corner. For all patients, friction should be avoided when transferring patients from the trolley, bed or chair to the x-ray table. Patients should be lifted onto the table or a patient slide used as appropriate. X-ray staff should ensure that patients are not left on the x-ray table for long periods without pressure damage protection. Patients with damage or at risk should be given priority by portering staff to ensure a speedy return to the ward. 3.5 Patients with Spinal Injuries The care required by patients with spinal injuries, who are being transferred to a specialised unit is as follows: When requesting an ambulance, request a stretcher overlay and scoop stretcher. Immediately it is known that the patient is to be transferred, he/she should be nursed on their side for a period of 2 hours or until the ambulance arrives. Once the patient is on the ambulance stretcher, the traction cord should be tied to the stretcher handle and removed on the scoop leaving the patient resting on the stretcher overlay for the duration of the journey. 133 PART 4 LEG ULCER GUIDELINES 4.1 Treatment for Venous Leg Ulcers 4.1.1 4.1.2 4.1.3 4.1.4 4.1.5 4.2 Leg Ulcer Assessment 4.2.1 4.2.2 4.2.3 4.2.4 4.2.5 4.2.6 4.3 Leg Ulcer Assessment, Including Doppler Compression Bandaging Patient Education Diet Exercise Medical History Limb Assessment Doppler Pain Control After Care Leg Ulcer Assessment Form Compression Therapy 4.3.1 4.3.2 4.3.3 4.3.4 4-Layer Bandage System Reduced Compression Bandage Types Compression Hosiery 4.4 Leg Ulcer Referral Route 4.5 Differential Diagnosis 4.6 General Advice Leaflet 4.7 Advice for Healing Leg Ulcers 4.1 Treatment for Venous Leg Ulcers To reduce/reverse venous hypotension by supporting the superficial venous system and increase the flow of blood back up through the deep veins. 4.1.1 Leg Ulcer Assessment, Including Doppler All wounds on the lower leg that remain non-healing, no later than 6 weeks should have an initial full assessment, if not showing signs of healing after 12 weeks, repeat. 4.1.2 Compression Bandaging If no cellulitis in the skin, 4-layer is the first choice for achieving graduated compression. Important to measure the leg to get correct size of bandages, and to assist shaping the leg using wool bandages to achieve a graduated shape. 4.1.3 Patient Education Give the patient verbal and written information. 4.1.4 Diet Advise a healthy, well balanced diet that includes proteins, vitamins and minerals e.g. meat, fish, fresh fruit and vegetables and milk. If the patient is overweight advise to try and lose some weight, involve dietician via GP if necessary. 4.1.5 Exercise Advise against standing for long periods, walking is good exercise. When resting advise to try and elevate legs, preferably heart level or above. Advise not to cross legs when sitting and not to wear tight fitting shoes or socks. Advise exercising the ankle and rotating the foot to aid the calf muscle pump action. 4.2 Leg Ulcer Assessment (To Be Carried Out On All Lower Leg Wounds Of 6-Weeks Duration Or More) 4.2.1 Medical History Medication, diet, family traits (if parents had ulcers), lifestyle, any underlying disease or allergies. 135 Underling conditions such as malnourishment, anaemia, thyroid problems, obesity, diabetes, rheumatoid arthritis, hypertension, varicose veins should be treated if possible; if not ulcers will not heal or will be very slow to heal. Other conditions that should be identified are coronary heart disease, stroke, claudication and TIA as these help to identify the type of ulcer i.e. venous, arterial or mixed. 4.2.2 Limb Assessment Is the leg warm/cold, hairless, shiny? Is oedema present (if yes, when and type)? Is there staining, eczema, induration or ankle flair? Is the leg painful, if so, when day/night, resting active? 4.2.3 Doppler Should confirm interpretation of other information. If APBI <0.8 compression consult TV team. Refer to GP for vascular assessment. Treat the wound without compression, until another opinion is obtained. Listen to the arterial sounds during the assessment, Triphasic, Biphasic or Monophasic. Triphasic sounds are healthiest, Monophasic indicate some arterial disease. 4.2.4 Pain Control Very important, pain can restrict movement. Pain control is essential for compliance. In some cases (e.g. severe arterial disease) the patient may require regular analgesics for pain relief. Also consider other comfort actions, such as footstool, bed cradle. 4.2.5 After Care When the wound is healed, it is important to prevent recurrence. Verbal and written information, on care of legs should be given. Compression hosiery should be worn. Prescriptions should be issued for 2 pairs every 6 months. Annual Doppler test to check ABPI. Advice on the use of emollients and skin care to prevent tissue breakdown. 136 TISSUE VIABILITY SERVICE - LEG ULCER ASSESSMENT side 1 Patient No: NHS No. Date: Surname : Title: Forenames: D.o.b: Sex: M / F Medication: Allergies: Urinalysis: Current Treatment: MEDICAL HISTORY HEALTH PROMOTION (tick, cross or circle) MI Weight Management Advice: CVA Height: Weight: TIA Claudication Mobility: walks freely / walks with aids / exercise Previous Arterial Surgery Substance misuse: Diabetes Alcohol units per week: Arthritis Leg Oedema Pulmonary Embolism Personal Hygiene: Continence Issues: Communication Issues: Previous DVT Pain score: Thrombophlebitis Where do you sleep? Bed / Chair Lower Leg Fractures Day …… Night ……. Resting ….. Do you Smoke? Yes / Previously / Never How Many per day? Previous VV Surgery Comments: VV’s present Lipodermatosclerosis Number of pregnancies DOPPLER ASSESSMENT Blood Pressure: Right Leg Left Leg Please record results using the following codes: T - Triphasic B - Biphasic M - Monophasic RIGHT Result Ankle (cms) Gaiter (cms) Calf (cms) Brachial Pulse Ankle movement Full Restricted Fixed Ankle Brachial Pressure: ABPI Index: T LEFT B M Result T B M Dorsal Pedis Pulse: DPP Posterior Tibial Pulse: PTP NORMAL RANGE ABPI = 0.8 TO 1.3 137 POSITION OF ULCER (Indicate by Numbers) side 2 Ulcer Number 1 2 3 4 5 6 Ulcer Site Duration of present ulcer (months) Size of Ulcer Appearance: Sloughy Granulating Epithelialising Depth: Superficial Deep Skin: Normal Eczema Dry Eczema Wet Maceration Cellulitis Summary of Causes - please circle Venous Arterial Arthritic Vasculitic Diabetic Obesity Trauma Malignancy Frailty Poor Mobility Other .................................................. RECOMMENDED TREATMENT…………………………………………………………………. ADDITIONAL INFORMATION …………………………………………………………… 138 4.3 Compression Therapy Compression can be applied to a leg ulcer when there is no history of arterial disease. Be aware of conditions that can indicate arterial disease, e.g. CVI, heart disease, severe heart failure, claudication, MI, rheumatoid arthritis, diabetes, Raynaud’s disease, sickle cell anaemia. Do not apply compression if cellulitis is present. If applying compression for the first time, written and verbal instructions should be given so that the patient will know how to remove the bandage if the toes should become numb or discoloured and how to contact the nurse if needed. There should be a followup visit from the nurse within 24 hours to check for any problems. Record wound progress every 4 weeks on Wound Assessment Chart. If not showing signs of improvement, check for systemic infection, i.e. pain, heat, inflammation, swelling then treat, if necessary. If not showing signs of infection, with the GP’s permission, take blood samples for FBC, U&E, TFT, RBS, check for compliance and continue to compress. Also check if patient is sleeping in bed at night. If no improvement at 12 weeks, refer to the TV Nurse for further investigation. 4.3.1 4-Layer Bandage (long stretch) Contact layer - Non-adherent dressing Layer 1 - Orthopaedic wool to protect the limb, spiral toe to knee. Bony prominence padded and leg shaped with the wool to provide shape to give graduated compression. Use a tape measure to ensure the calf circumference is 10cms greater than the ankle circumference. 2-3 rolls of wool may be needed (or even more). Layer 2 – Crepe, or light support equivalent bandage over the wool layer toe to knee with 50% overlap spiral. Layer 3 – Class 3a bandage toe to knee, 50% overlap, 50% stretch in a figure of eight. Layer 4 – Cohesive layer, toe to knee, 50% overlap spiral. NB: Never apply compression before assessment. suspected, refer as appropriate. If arterial disease is 4.3.2 Reduced Compression If patients are referred out of hospital on reduced compression therapy, ensure clear instructions are given regarding bandaging techniques (i.e. 3 Layer top spiral or figure 8). 139 4.3.3 Bandage Types Retention Bandages Keeps dressings close to the wound without inhibiting movement or restricting blood flow. They are available in widths of 5cm, 7.5cm, 10cm and 15cm. Some of those commonly used are Slinky, Kband, Acti-wrap, and Easyfix. Light Support Used to support mild sprains and joints. There is no evidence to support the effectiveness, however, they do provide light support without exerting undue pressure. Available in widths of 5cm, 7.5cm, 10cm and 15cm. Bandages in this range are Crepe, Soffcrepe, Setocrepe, Hospicrepe, Klite, Profore 2 and Clinilite. Type 3A Compression Used to give light compression for varicose ulcers, used for reduction of oedema. Available in 10cm and 15cm. Bandages in this range are Elset, KPlus, and Profore 3. Type 3B Compression Used to provide support in sports injuries or as a secondary securing bandage e.g. over zinc bandages in the treatment of venous ulcers. Can cause skin reactions if next to the skin, if too tight, it can create a tourniquet effect. Not to be used with arterial ulcers. Available in widths of 2.5cm, 5cm, 7.5cm, 10cm and 15cm. Coban, Cohfast, Co-plus, Ko-flex, Profore 4. Type 3C Compression High compression used in venous insufficiency, venous leg ulcers and gross oedema in an averaged sized person. Require skill to achieve graduated compression. Not to be used if arterial insufficiency suspected. If applied wrongly, it can cause severe, sometimes irreversible damage to the limb. Only available in 10cm widths. Setopress, Tensopress, Surepress, Profore+, K-type C. Type 3D Compression Extra high compression, must never be used routinely, it can only be used in extreme cases, under specialised supervision. Mostly with the largest and most oedematous limbs. Available in 7.5cm and 10cm. Blue Line Webbing, Red Line Webbing. Short Stretch Sustained Compression Bandage Short stretch bandaging is used to provide sustained compression therapy in the treatment of venous leg ulcers. More commonly used in Europe than in Britain at the moment. It works by maintaining a position as the calf muscle expands and because the bandage does not give way, force is directed back to the leg where it can act more effectively on the deep vein. It must never be used on patients who have marked arterial problems. 140 Advantages Easy to apply with little training – bandage is applied at full stretch. Low resisting pressure therefore tolerated better for patients who find difficulty coping with compression bandages. Shoes usually fit over the bandage. The patient can often apply the bandage themselves when shown how. Not as hot to wear as the 4-Layer bandage. No rubber in the bandages. Safer in ulcers of mixed aetiology as there is little residual compression when the leg is at rest, provides low resting pressures. Disadvantages Can slip down, particularly after the first 24 hours, when oedema is reduced by the compression. Usually requires the patient to be ambulant to achieve the massage effect of the bandage. Short Stretch Bandage - available on prescription Actiban Actico Comprilan Rosidal K Silkolan High compression cotton bandage High compression cohesive bandage High compression cotton bandage High compression cotton bandage High compression cotton bandage Two layer bandage systems Giving 40mmHg at the ankle Easy to apply Cool for the patient Shoes usually fit over the bandages Systems Available: Coban 2 K-Two System Proguide Two-layer Bandage Systems Systems available for reduced compression. Coban 2 little (for ABPI as low as 0.5) K-Two (Reduced) 141 Multi-Layer Compression Bandaging Profore System (Smith & Nephew) NB: Tricotex contact layer Profore 1 Profore 2 Profore 3 Profore 4 Softban natural Soffcrepe 25cm – 30cm Litepress Coplus Kit Sizes available 18cm – 25cm above 30cm (The bandages will vary in each kit) Profore System should be ordered by ankle circumference. System Four (Molnlycke) Setoprime primary dressing 4#1 Softexe 4#2 Setocrepe 4#3 Elset 4#4 Coban Only in 18cm - 25cm ankle circumference Ultra Four (Robinson) NB: Setoprime Ultra Four #1 Ultra Four #2 Ultra Four #3 Ultra Four #4 contact layer Sohfast Reduced compression K-Lite up to 18cm K Plus 18cm – 25cm Cohfast Ultra Four should be ordered by ankle circumference. K-Four (Urgo) Paratex contact layer Layer #1 K-Soft Layer #2 K-Lite Layer #3 K-plus Layer #4 Ko-flex Only in 18cm – 25cm / 26 – 32 cm ankle circumference Proguide System (Smith & Nephew) NB: Foam wound contact layer Layer #1 Proguide 1 Layer #2 Proguide 2 Kit Sizes available 18cm – 22cm 22cm – 28cm 28cm – 32cm Ankle circumference Proguide System should be ordered by ankle circumference. K-Two System (Urgo) K – Tech K - Press 142 Coban 2 (3M) Multilayered bandage system (One Size) 4.3.4 Compression Hosiery TYPE DESCRIPTION USE Class Light support 1 Compression at ankle 14-17 mm/hg Available below knee or thigh length Made to measure Available on FP10 Superficial or early varicosities Class Medium support 2 Ankle pressure 18-24 mm/hg Available below knee or thigh length Made to measure (closed heel/open toe) Varicosities of medium severity, prophylaxis and treatment of ulcers and mild oedema Class Strong support 3 Ankle pressure 25 – 35 mm/hg Available below knee or thigh length Made to measure Available on FP10 Gross varicosities, post thrombotic venous insufficiency, gross oedema, ulcer treatment and prophylaxis. Two Layer Hosiery for Treating Ulceration (instead of multi-layer bandages) NAME Activa Leg Ulcer Kit Jobst Ulcercare (with MANUFACTURER Activa AMOUNT OF COMPRESSION AT THE ANKLE 40 mmHg BSN 40 mmHg Convatec 35 mmHg zip) Surepress Light Compression Hosiery (10 mmHg liner stockings) For patients who have difficulty applying class Ι or ΙΙ stockings or who need less compression. Activa Liner Stockings Giving 10 mmHg at the ankle in sizes – Small, Medium, Large, X Large and XX Large. Two of these stockings can be worn together on one leg where patients have difficulty applying Class ΙΙ hosiery, giving 20mmHg at the ankle 143 4.4 Leg Ulcer Referral Route Clinical assessment indicates varicose disease. Doppler index 0.8 or above. Treat as venous for 12 weeks. Assessment and clinical investigations should be undertaken by a healthcare professional, trained in leg ulcer management. Clinical assessment indicates diabetic ulcer NB: ABPI may by unreliable in this group of patients. Review Leg Ulcer Clinical assessment suggests arterial disease, Doppler index below 0.8. Routine vascular referral. No compression. Below 0.6 requires urgent referral If not already been screened, then refer to diabetes centre for foot screening. No compression to be used until peripheral vascular status has been confirmed. If definite signs of improvement continue and review monthly Ulcer healed – re Doppler and arrange compression hosiery and aftercare Annual re-assessment and Doppler No improvement Full re-assessment and Doppler to identify reason for nonhealing. Refer to beginning or TV Nurse NB: Check list for re-assessment If ulcer is not showing definite measurable progress towards healing consider: 1. Bandage – is sufficient graduated compression being achieved? 2. Is leg being appropriately elevated? 3. Dressing – is it appropriate? 4. Has general health/mobility altered? 5. Has ulcer developed arterial component? 6. Consider dermatology referral for non-responding ulcers/non-responding eczema cellulitis. 7. May need to consider specialist referral in cases of rheumatoid disease. 144 4.5 Differential Diagnosis VENOUS ARTERIAL Site Usually gaiter area Anywhere on lower leg Shape Usually shallow, flat margins, irregular shape Often deep punched out edges Pain Some, often relieved by rest Oedema Generalised Greater at night. Relieved by lowering leg Claudication on exercise Localised Varicosities Sometimes Never Surrounding skin Venous eczema, Lipodermatosclerosis, atrophy blanche, ankle flare, staining Shiny, hairless, pale cold blue feet, dependent rubor Pulses Present Absent or diminished ABPI Greater than 0.8 Less than 0.8 Mixed Mixed ulcers can be defined as being of both venous and arterial aetiology. A mixed ulcer involves venous and arterial insufficiency. GENERAL ADVICE LEAFLET LOOKING AFTER VENOUS ULCERS DO 1. Walk or exercise if possible as this improves the blood flow around the body. Gentle ankle exercises when sitting help to improve blood supply to legs and feet eg: i) Rotate ankles in circular motion clockwise and anticlockwise ii) Pump your calf muscle by pointing toes and then bringing foot back to a right angle with your leg. 2. Rest during the day for a couple of hours – raise legs so that ankles are level or above your heart to help blood return to the heart and to help reduce any swelling 3. Eat a healthy balanced diet – this will help healing 4. If overweight, try to lose weight, ask your nurse or G.P. for advice. 5. If you smoke, try to reduce the number per day or stop smoking 6. Look after your skin, apply creams if prescribed 7. Examine your legs and feet regularly, look for changes in colour or any new sores 8. Wear comfortable shoes 9. Avoid extremes in temperature i.e. hot baths, hot water bottles or extra cold things 10. Keep bandages on. They are meant to feel firm but comfortable. If worried about them, contact your district nurse for advice 11. When you are healed, you will probably be prescribed and fitted with support socks as prevention is better than cure. BARNSLEY PCT (N DON’T 1. 2. 3. 4. 5. Do not wear tight shoes or socks Do not cross your legs Do not stand for long periods of time Do not ignore sores or any changes to legs/feet Do not remove dressings, contact your nurse if worried CONTACT NUMBERS: Tissue Viability Nurse: …………………………………………… Your District Nurse/Practice Nurse: …………………………….. 146 PATIENT ADVICE LEAFLET “prevention is better than cure” COMPRESSION STOCKINGS/SOCKS 1. It is very important that you take special care of your legs and wear the stockings that have been prescribed for you. These will keep the circulation working well in your legs and hopefully prevent your legs from swelling. If not, you are at risk of skin breakdown or the start of an ulcer. 2. The stockings should be comfortable but have to fit firmly and need to every day. be worn 3. If you take them off for bed, you need to put them back on first thing in morning before your legs have time to swell. the 4. Your stockings should fit smoothly along your leg and have no wrinkles creases. Never turn them over at the top or 5. Renew your stockings every 3 – 6 months depending on the manufacturer’s instructions, sooner if they no longer fit firmly and comfortably, or if they become laddered. 6. Wash your stockings gently as directed by the manufacturer. Avoid detergents or fabric softeners which may irritate your skin. Do not use direct heat or tumble dry, do not iron them. HOW TO PUT ON STOCKINGS /SOCKS 1. 2 3. 4. 5. Turn stocking inside out up to heel Pull foot of stocking over your foot Gradually ease stocking up over heal and ankle Ease rest of stocking up the leg. Avoid pulling hard at the top Check toe and ankle piece is in place SKIN CARE ADVICE Looking after the skin on your legs helps prevent infection and breakdown. Use an emollient cream to moisturise your legs as shown in clinic. Many of these creams can also be used instead of soap to wash your legs – check with your nurse if you are not sure. Apply any cream in the direction that hair grows, this prevents build up of cream at the root of the hair. Avoid injury – knocks, scratches, insect bites etc. Do not sit too close to the fire. Contact your nurse or doctor if there is any damage or irritation or if the skin begins to break down again. 147 EXERCISE Walking (if possible) improves the blood flow around the body. Gentle exercises when sitting help improve the blood supply to the legs and feet eg: i) ii) rotate ankles in circular motion clockwise and anticlockwise pump your calf muscle by pointing your toes and then bringing foot back to a right angle with your leg. REMEMBER EVEN SMALL MOVEMENTS ARE BETTER THAN NONE ELEVATION Both legs should be elevated regularly. They need to be at least level with your heart to have a good effect. Lie down on your settee or bed with your legs raised on a pillow. Do not wear tight garters, socks or shoes which could restrict the blood flow Do not stand still for long periods of time or sit with legs crossed as this will interfere with the blood flow to and from your legs. DIET Eat a healthy balanced diet. Ask your nurse if you need advice. Drinking plenty of fluids, especially water each day will help to prevent skin becoming dry. Contact your nurse or doctor: 1. If you notice any signs of a new ulcer developing or if you notice pain, when walking or cramp type symptoms. 2. To arrange a repeat doppler test in 12 months time (telephone - 01226 433215) CONTACT NUMBERS: Your District Nurse: …………………….. Your Practice Nurse: …………………… Tissue Viability Office: 01226 433215 148 PART 5 SKIN TEARS 5.1 Definition 5.2 Risk Factors 5.3 Common Precipitating Causes 5.4 Dressings 149 5.1 Definitions A skin tear is a traumatic wound that occurs principally on the extremities of older adults as a result of friction alone or shearing and friction, which separates both the epidermis and the dermis (partial thickness wound) or which separates both the epidermis and the dermis from underlying structures (full thickness wound). 5.2 5.3 5.4 Risk Factors Advances age Dependence for activities of daily living, including bathing, dressing and Transferring Impaired mobility and confined to bed, chair or wheelchair History of previous skin tears Compromised nutritional status Sensory and cognitive deficits Visible changes in skin including serule purpura, dryness, pitting, oedema and fragility Drugs such as corticosteroids and anticoagulants Agitated behaviour in the elderly Cardiac, pulmonary and vascular disorders Common Precipitating Causes Knock or bump into bed rail, other furniture or equipment Transfers from beds or charts Falls Use of restraint Removal of tape or adhesive dressings and taking blood Staff jewellery, watches, fingernails (see uniform policy) Dressings Skin closure strips are not always successful due to swelling, especially on elderly skin. Avoid where possible on the elderly 150 Appropriate dressing will vary depending on classification, exudate amount, skin fragility and individual patient factors. Cleanse to remove residual clot or debris Replace and secure skin flap where present Cover with appropriate dressing 151 APPENDICES Appendix 1 300 Tilt – A Pressure Relieving Position Appendix 2 Basic Care Guide for Patients undergoing Long Ambulance Journeys Appendix 3 Pain Control Charts Appendix 4 Guide to Equipment Selection Flow Charts Appendix 5 Nutrition and Pressure Damage Appendix 6 Wound Assessment Chart Appendix 7 Pressure Ulcer grade III and IV Root Cause Analysis (RCA) 152 Appendix 1 - 300 Tilt – A Pressure Relieving Position The most important measure for preventing pressure damage is to avoid pressure of the tissue to excessive concentrations of pressure. A simple and cheap method of achieving this is done by using three extra pillows in the bed to maintain a 300 tilt of the patient’s body in relation to the surface of the bed. This position is particularly useful for patients being nursed in the community as it can be taught to carers. The need for “turning” is reduced to a tilting from one side to the other, totally avoiding weight transmission through the bony prominences, using the soft gluteal mass instead. Turning a patient over no longer requires the carer to take the patient’s weight, as the patient is eased from one side to the other rather than being lifted and turned. The period between changes of position can be extended for up to 8 hours * allowing a full night’s sleep for both patient and carer, although a 4 hour * period is more normally used, where no special mattress is available. (This method was developed in 1981 in a YDU in Lincoln and has since been advocated by Ken Preston – a Nurse Specialist in Pressure Area Prevention.) *Careful, ongoing assessment of the patient is required to ensure that they can be safely left in one position for extended periods without damage to the skin. An illustration of the 300 tilt is on the next page. 153 Appendix 1 - The 300 Tilt - A Pressure Relieving Position To be scanned The pillows can be positioned on either side of the patient and, if positioned correctly, the patient can be safely left up to four hours*. The pillows should be positioned so that the patient is lying 300 from flat and weight is taken through the fleshier areas, such as the buttocks, but not the bony areas like the hips of sacrum. *Careful, ongoing assessment of the patient is required to ensure that they can be safely left in one position for extended periods without damage to the skin. 154 Appendix 2 - Basic Care for Patients Undergoing Long Ambulance Journeys Where a patient is to be transferred without a nurse escort and the anticipated journey time is in excess of two hours: Obtain specific advice from the nurse handing-over, as to the patient’s individual needs concerning positioning and re-positioning during the journey. It is important that this advice is strictly adhered to, and in particular the recommended time intervals for re-positioning the patient should not be exceeded. Remove any wet clothing, where possible. Ensure the patient is not lying on creased linen and/or clothing. Re-position clothing to ensure that zips etc do not lie beneath the patient. Items in trouser pockets, such as keys, should be removed. Ambulance stretcher covers (green sheets), that have ironed-in creased, darns or patches, should not be used. Use pressure relieving aids where available. When lifting or moving the patients, ensure that the patient is always lifted clear of the surface beneath them in order to prevent shearing forces on the skin. 155 Appendix 3 - Guidelines For Using The Pain Control Chart Patient’s Name:_____________________________ Unit No: ______________ Allergies, if any Type of Pain Patient’s description of the pain, and nurse’s assessment of pain, plus site and grading. Indicate site(s) of pain on the body chart, using letter ‘A – E’. Grade degree of pain, for each site, using number ‘0 – 5’ (see grading scale) e.g. site ‘A’ graded ‘3’, site ‘B’ graded ‘1’. Example: Date Time 12.7.06 09.03 5 4 3 A 2 1 B 0 Action Taken Alternative measures, e.g. change of position, relieved by food/drink, or elimination. Diversion therapy, physiotherapy, counselling etc. Review requirements of analgesia given. Additional drugs required, e.g. sedatives, hypnotics, relaxants etc. Analgesia Given Name of drug, route and dose. Evaluation of Drugs Given Patient’s own evaluation of drug effect and nurse’s assessment of effect. Review of site and grading. Comments/Evaluation of Actions Taken See ‘Action Taken’ NB: When possible it is envisaged that the chart will accompany the patient on admission and discharge to afford continuity of care. 156 Date & Time Type of Pain: Description of site(s): Evaluation of Drug(s) Given Action Taken Comments / Evaluation of Action Taken Analgesia (if given) Route / Dose Signature 157 Appendix 3 - Pain Control Chart Grading Scale Date Time 5 4 3 2 1 0 Date Time 5 As much pain as I could possibly bear A very bad pain 5 Quite a lot of pain 3 A little pain 2 No pain at all 1 Sleeping 0 4 3 2 4 1 0 158 ACUTE PAIN SERVICE OF ________________HOSPITAL Appendix 3 Postoperative pain assessment and observation chart Name: Unit No: Address: DoB: Consultant: Ward: Patients on PCA or Epidural infusions must have observations completed 2 hourly 1. Respiratory rate: While the patient is at rest count the respiratory rate for one minute. 2. Sedation score: Look at the patient and decide which of the following apply: Awake 1 Dosing intermittently 2 Mostly sleeping 3 Enter score as O in graph Only awakens when aroused 4 (1-4 below) 3. Pain assessment score: Ask the patient “Which of the following words describes the pain you are experiencing at the moment?” No pain 1 Mild pain 2 Moderate pain 3 Enter score at X in graph Severe pain 4 (1-4 below) Time 40 39 38 37 36 35 170 160 150 140 130 120 110 100 90 80 70 60 50 40 240 220 180 170 160 150 140 130 120 110 100 90 80 70 60 50 40 Resp Resp IF PAIN SCORE IS 3 OR 4 REVIEW CURRENT REGIME 4 3 2 1 Nausea Yes/No 4 3 2 1 Nausea Yes/No 159 Appendix 3 PCAS RECORD FORM Date: Name: DoB: AM/PM Perioperative Opiates Procedure: Pre-Op: Surgeon: Per-Op: Anaesthetist: Recovery: WT: Local Block: WD: Unit No: Details of PCA Infusion Morphine ………………………… mg in 30ml syringe Conc………………………………. mg/ml Loading dose given……………… mg at ……………. hrs Lockout duration…………………. (normally 5 mins) 4hr maximum dose……………… mg Background infusion……………. mg/hr Date Time Resp Rate Conc Level Signed……………………………. Pain 0-3 IV Site Total Received to Date Nausea & Vomiting Seen by Anaesthetist Reason for discontinuation…………………………………………………………….. Amount of drug wasted………………………… Nurse’s signature …………….. 160 Appendix 3 - Nursing Observations Nursing observations are to be recorded: ¼ hourly in recovery 1 hourly for 4 hours on Ward 4 hourly until discontinued Respiratory Rate: If <12 – call anaesthetist If <8 – switch off pump and call anaesthetist NB: Anaesthetist on call for obstetrics is also on call for PCA Conscious Level: 0 = Unrousable – CALL ANAESTHETIST 1 = Asleep but rousable 2 = Awake but drowsy 3 = Awake and alert Pain: 0 = No pain at rest or moving 1 = No pain at rest, slight pain on movement 2 = Some rest pain, moderate pain on moving 3 = Continuous pain, severe pain on moving IV Site: Ok / Inflamed (I) / Tissued (T) Total Tries and Number Good: Read from PCAS by pressing history button Nausea and Vomiting Enter N, V or O (neither) PLEASE RETURN FLOPPY FORM TO ANAESTHETIC DEPARTMENT FOR AUDIT THANK YOU 161 Appendix 4 - Guidance For The Use of Pressure Reducing Equipment For patients with pressure damage Grade 1 –2 Adopt prevention plan Reduce risk factors - Foam mattress and cushions - Mattress toppers - Turning regime NB: Alternating system may be required Adopt a Prevention Plan to Reduce Risk Factors Grade 2-3 Adopt prevention plan - Alternating mattress i.e. Alpha Xcell Alphatranscell Overture Viaclin Aircare Extracare Plus - Cushion Foam and gel Turning regime Frequent position changes Correct handling technique Nutritional assessment Pain control Consider drug therapy Continence – skin care Pressure reducing aids Grade 3-4 NB: Adopt prevention plan - Alternating mattress i.e. Bi-Wave Cairwave Autologic Eclypse Phase III - Cushion i.e. STM 3/4 Roho Proactive 2 Turning regime Eclypse Cushion Alternating Cushion Heel and elbow pressure ulcers may only require accessories such as heel off loading devices and elbow supports. Pillows or Repose Foot Protectors can be used to raise the affected limb from the bed to remove the pressure. 162 Appendix 4 - Guidance For The Use of Pressure Relieving Equipment Low Risk Waterlow 10 – 14 Norton 15 – 12 Medium Risk Waterlow 15 – 19 Norton 11 – 8 High Risk Waterlow 20+ Norton below 8 Adopt a prevention plan to reduce risk factors Frequent position changes Correct handling technique Nutritional assessment Pain control Consider drug therapy Continence – skin care Pressure reducing aids Pressure reducing aids (No pressure damage present) Lying Surfaces Foam mattress i.e. Vaperm Key 2 Care SoftForm Pentaflex Mattress toppers i.e. Propad Spenco NB: Accessories Dermal pads Elbow pads Heel off loaders Leg troughs Repose Foot Protectors Totally immobile patients who cannot be moved may require an alternating system as the best preventative choice. 163 Appendix 5 - Nutrition and Pressure Damage It is important at any age the dietary intake of any individual fulfils the nutritional needs of that person. A regular and varied diet is more likely to fulfil nutritional requirements. Factors, which influence and may diminish nutritional intake include chronic physical and/or mental illness or disability, poor dentition, reduction in the sense of taste and smell, poverty and poor social conditions. Ageing is associated with many of these factors as well as natural changes occurring in the physiology of the skin, the vascular system and the body’s metabolism. Nutrients affecting the development and healing of pressure damage include protein to maintain and regenerated body tissues, as well as carbohydrates and fats to provide energy, protect body mass and maintain cell membranes. Vitamin C, which is depleted in the body during illness or infection, plays a dominant role in wound healing, being necessary for collagen synthesis. Vitamin A and Thiamine (B1) also plays a role in collagen synthesis. Vitamin K helps indirectly by preventing internal bleeding problems. Deficiency in zinc inhibits wound healing, while iron deficiency anaemia leads to reduced appetite and poor wound healing. Nutrition and Prevention of Pressure Damage All patients/clients should be provided with a nutritionally adequate diet. All patients/clients should be screen to identify those as risk. This screening should be reviewed regularly, using the nutritional screening tool to assess the Body Mass Index (BMI). The dietician will assess those patients/clients referred requiring nutritional intervention. Health promotion, to encourage sound nutrition, should be carried out. Those patients/clients who do have pressure damage should receive a diet, which will improve their medical condition. GRADE 0–1 Food and fluid intake should be observed referring patient/client to a dietician if intake is inadequate. 2 and above Following referral, an individual nutrition plan should be advised and communicated to those concerned. The plan should give special consideration to: Energy - to cover needs Protein - 1.2-2 g/kg body weight Vitamin C – Supplementation as necessary Zinc – to correct deficiency Iron – to correct deficiency Nutritional needs can be fulfilled in different ways: 164 Normal diet Changed to high protein/high calorie diet where someone has the ability and appetite to consume it. Fruit juice should be encouraged daily. Normal/soft diet Where a patient/client’s appetite and ability to eat is limited. and supplement Complete liquid When a patient/client can only take fluids via the oral or enteral route – an individual regime being drawn up by the dietician. Supplements available on prescription Indications for prescribing: Disease related malnutrition Intractable malabsorption Pre-operative preparation of patients who are under-nourished Treatment for those with proven inflammatory bowel disease Dysphagia Continuous ambulatory peritoneal dialysis Short bowel syndrome Bowel fistula Haemodialysis Following total gastrectomy 165 Prescribable supplements Fresubin A balanced 1 kcal/ml liquid in carton, various flavours. Stocked by pharmacy. 3.8g protein, 13.8g carbohydrates per 100ml Ensure Plus 1.5 kcal/ml liquid in 200ml cartons, various flavours. should be used as recommended by a dietician. pharmacy. 6.25g protein, 20.4g carbohydrate per 100ml. Fortimel High protein supplement, 1 kcal/ml in 200ml carton. For use only as recommended by a dietician. Stocked by Catering Department. 10g protein, 10.3 g carbohydrate per 100ml. Enlive Plus 1.5 kcal/ml. Various flavours. Should be used as recommended by dietician. Gluten, lactose and fat free. 4.8g protein, 32.7g carbohydrate per 100ml. Fortisip 300 kcal/ml. Various flavours. Should be used as recommended by dietician. 6g protein, 18.4 carbohydrate per 100ml. Fortijuice 300 kcal/ml in 200ml. Various flavours. Should be used as recommended by dietician. Gluten, lactose and fat free. 4g protein, 33.5g carbohydrate per 100ml. Ensure Plus Stocked by 166 Appendix 6 - Wound Assessment Chart Wound Assessment Chart NAME: _______________________UNIT NO: _______________ DOB: ___________ TYPE OF WOUND: __________________________LOCATION: __________________ DATE OF ONSET: _______________________________________________________ DATE OF ASSESSMENT: _________________________________________________ SIGNATURE OF NURSE: _________________________________________________ DATE WOUND MEASUREMENTS LENGTH: BREADTH: DEPTH: WOUND DESCRIPTIO DIAGRAM Shade area to identify sloughy necrosis granulation – percentage etc. DATE DATE DESCRIPTION OF WOUND BED PRESSURE ULCER (ONLY) GRADING I, II, III, IV (if pressure ulcer) EXUDATE AMOUNT YES/NO Type eg serous fluid, blood, pus, colour eg infected ODOUR NONE / SOME / OFFENSIVE SURROUNDING SKIN CONDITION: COLOUR: OEDEMA: eg pitting, leaking, red excoriated etc. PAIN TREATMENT 0 = NONE INFECTION SWAB SENT TREATMENT YES/SUSPECTED/NO NO/YES/DATE: PRESCRIBED DRESSING TYPE: SIZE: PROTOCOL SELECTED 1 – 9 (from wound Care Policy) DRESSING CHANGES FREQUENCY: PROPOSED REVIEW DATE DATE: ASSESSING NURSE SIGNATURE: 5 = SEVERE 167 Appendix 7 (1) PRESSURE ULCER (GRADE III + IV) ROOT CAUSE ANALYSIS TOOL Name completing this form ………………………… Date of completion ………………………. Name: Unit No: D.O.B GP: Patient’s Address: Date of Admission to your service / care home: Pressure Damage Visible on Admission: Risk Assessment Date: Safe Guarding issues: Yes low level concerns Risk Tool Used: Risk Score: Weight/BMI: Waterlow / Norton Medical History / Diagnosis: Medication: Wound Assessment Chart in place Last date wound was assessed and documented: Continence Details: Continence products used: Nutritional Status: Nutritional products used: Skin Condition: Skin products used: 168 Appendix 7 (2) Name: Unit No: DOB: Mobility: Turning / Movement Regime: Date Commenced: Equipment Used: Date Commenced: Type: Static Cushion Alternating Cushion Static Mattress Alternating Mattress Heel/Elbow Protectors Other Patient’s Journey / Chronology of Events (last 4 weeks): PRESSURE ULCER/S: Date Detected: Site Grade: Treatment Used: Completed By: IR1 Serial No: (if applicable) 169 Appendix 7 (3) ACTION PLAN FOLLOWING PRESSURE ULCER ROOT CAUSE ANLAYSIS (RCA) PATENTS NAME: RECOMMENDATIONS / SOLUTIONS UNIT NO: ACTIONS LEAD PERSON DATE: TIMESCALE DATE COMPLETED