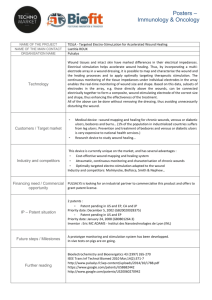
Table No: 1 - WebmedCentral.com
advertisement

CHAPTER 1 Introduction 1 Plant has a pivotal role in medicine through out all recorded history, in virtually all human cultures. Indeed, plants are foundation upon which effective medicine has been built. Often discoveries about plant medicines have catalyzed the progress of basic medical research. There has been a resurgence of interest in plants as sources of medicines in the recent decades. 80% of the world population relies on medicinal plants for their primary health care. Such herbal medicines that are easily available, cheaper, time tested and considered safer than most of modern synthetic drugs. Over 50% of the best selling pharmaceuticals in use today were derived from natural products. By providing scientific information on medicinal plants, which influence its productivity, enhance its therapeutic efficiency and competitiveness in the field of medicine and pharmacy. Over the past decade, herbal medicine has become an item of global importance both medicinal and economical. Although usage of these herbal medicines has increased, their quality, safety and efficiency are serious concerns in industrialized and developing countries. Thus accurate scientific assessment has become a prerequisite for acceptance of herbal health claims. Pothos scandens Linn. (Family: Araceae) have a great medicinal value for its wound and burn healing properties. The plant is seen many parts of South India especially in wild areas. Traditionally the plant is used by Ayurvedic physicians of Cheruvathur, Kerala mainly for its burn healing properties. For natural product discovery the conventional approach of extraction, identification and characterization of compounds, test for desired biological activity and finally formulating in a suitable dosage forms. Ayurveda based drug discovery uses “Reverse Pharmacology” in which drug candidates are first identified based on large-scale use in population, and then validated in clinical trials. Experts say this approach can cut time from 12 to 15 years for drug discovery and are economical. India is the largest producer of medicinal herbs and is called the botanical garden of world. There is about approximately 45,000 plant species in India, with concentrated hot spots in the region of eastern Himalayas, Western Ghats and Andaman and Nicobar Islands. The officially documented plants with medicinal potential are about 3000 but traditional practitioners use more than 6,0001. 2 CHAPTER 1.1 Importance of Phytochemical Screening 3 Plants and trees had always been a rich source of lead compounds (e.g. Morphine, Cocaine, Digitalis, Quinine, Tubocurarine, Nicotine, Muscarnine, and many others). Many lead compounds are useful drugs in themselves (e.g. Morphine and Quinine), while others have been basis for synthetic drugs (e.g. local anaesthetics developed from Cocaine). Plants remain a promising source of new drugs which have recently been isolated from plants include anticancer agent from Taxol from the yew tree, and the antimalarial agent from the artemisinin from a Chinese plant. Plants provide a bank of rich, complex and highly varied structures, which are unlikely to be synthesized in laboratories. Furthermore, evolution has already carried out a screening process whereby plants are more likely to survive if they contain potent compounds, which deter animals or insects from eating them. These potent compounds are secondary metabolites with quite complex structures, in which most of them are biologically active compounds. It is sobering that very few plants were been fully studied and the vast majorities have not been studied at all. It is often worthwhile studying the medical folklore of ancient civilizations depended greatly on local flora and fauna for their survival. Therefore, study of medical folklore can give clues as to which plants might be worth studying in more detail. In general, natural products are particularly good at providing radically new chemical structure which no chemist would dream of synthesizing. As a preliminary of phytochemical screening, specific test for secondary metabolites were performed for alkaloids, glycosides, flavanoids, proteins & amino acids, gum & mucilage, carbohydrates. 4 CHAPTER 1.2 Gels as topical application 5 Gels as topical application2,3,4 Gels are semisolid system in which a liquid phase is constrained within a three dimensional polymeric matrix [natural or synthetic gums] in which a high degree of physical or sometimes chemical cross linking has been introduced some of these systems are as clear as water in appearance, aesthetically pleasing as in gelatin deserts and other turbid. Their clarity ranges from clear to a whitish translucence2. Gels are divided into inorganic [two-phase system] and organic [single phase] gels on the basis of nature of the colloidal phase. In a two phase system, the gel mass consists of a network of small discrete particles [e.g. Aluminum hydroxide gel]. If the particle size of the dispersed phase is relatively large, the gel mass sometimes is referred to as magma [e.g. Bentonite Magma]. Single phase gels consist of organic macromolecules distributed uniformly throughout a liquid in such a manner that no apparent boundaries exist between the dispersed macromolecules [e.g. Carbopol] or from natural gums [e.g. Tragacanth]. Although these gels are commonly aqueous, alcohol and oils may be used as the continuous phase. Likewise the nature of the solvent determines whether the gel is a Hydrogel [i.e. water based] e.g. Bentonite or an Organogel [with a nonaqueous solvent] e.g. Plastibase. Solid gels with low solvent concentration are known as Xerogels. They are often produced by evaporation of the solvent, leaving the gel framework behind. The can be referred to the gel sate by introduction of an agent, which on imbibitions, swells the gel matrix. Examples of Xerogels, include Tragacanth ribbons, acacia tears, dry cellulose and polystyrene Gels can be prepared from a number of pharmaceutical agents such as Tragacanth, [2-5%], Sodium alginate [2-10%], Gelatin [2-15%], Methyl cellulose [2-4%], Sodium carboxy methyl cellulose [2-5%], Carbopol [0.35%] or Polyvinyl alchohol [10-20%]. Other gelling agents include Methyl hydroxyethyl cellulose, Hydroxymethyl cellulose, Poly oxy ethylene, Polyoxypropylene [poloxamers] and metallic stearates. 6 Preservatives are to be incorporated into the gels especially for those prepared from natural sources Preservative should be incorporated into the gels especially for those prepared from natural sources. Appropriate preservatives depending upon the use and the gelling agent include the Parabens [0.2%], Benzoic acid [0.2%] and Chlorocresol [0.1%] The gels, particularly the single-phase gels, are being used more frequently in pharmacy and cosmetics because of several properties such as 1. Semisolid state 2. High degree of clarity 3. Ease of application 4. Ease of removal and use. The gels often provide a faster release of drug substances, independent of water solubility of the drug as compared to creams and ointments. GEL CHARACTERISTICS Ideally, gelling agents for pharmaceutical and cosmetic use should be inert, safe and non-reactive to other formulation components. The gelling agent should a provide responsible solid like nature during storage that can be broken easily when subjected to the shear forces generated by squeezing a tube or during topical application. The gel should exhibit little viscosity change under the temperature variations of normal use and storage. The gel characteristics should match the intended use. A topical gel should not be tacky. FORMULATION CONSIDERATIONS In the formulation of gel, the efficacy is often dependent on the composition of the vehicle. The ability of a drug in gel formulation to penetrate the skin and exert its effect depends on to consecutive physical events. The drug must first diffuse out of the vehicle to the skin surface and then, it must penetrate the natural barrier to enter into the site of action. Many so called ‘vehicle effects’ reported in the literature are the consequences of this to diffusion processes. Depending on which process is slower, either event could determine the overall effectiveness of the topical 7 gel dosage form. These two processes are intimately related and are dependent upon physicochemical properties of the drug, vehicle and barrier. FORMATION OF GEL All polymer solutions are possible prone to setting to gels because the solute consists of long and flexible chains of molecular thickness that become entangled & attract each other by secondary valency forces. When the three dimensional polymerization of multifunctional monomers reaches a given conversion, gelation occurs at a sharp gel point. Cross-linking of dissolved polymer molecule also causes their solutions to gel, both type of reaction produce permanent gels held together by primary valence forces. A gel often contract on standing and some of the interstitial liquid is squeezed out. This phenomenon called syneresis is due to crystallization or to the formation of additional contact points between polymer segments on aging. In the case of irreversible gels formed by 3-dimensional polymerization, continuing cross-linking or poly condensation reaction tighten the polymer network and shrink the solid phase. Even though varieties of structures are associated with a gel networks, most of the pharmaceutical gels are random coil networks. Random coil gelation mechanisms are rooted inter polymer – polymer and polymer – solvent interaction. With a given polymer, the gel net work increases in strength with increase in polymer concentration. These results in a reduction of inter particle distance, which subsequently leads to chain entanglement and further development of cross-links. Continual addition of polymer strengthens the gel network and results in increased viscoelasticity. Although the gel network is formed through polymeric interactions, the nature of the polymer-solvent affinity, actually determines the integrity of the gel. Classical gel theory is distinguished between three categories of solvents: 1. Free solvents that are very mobile. 2. Solvent bound as a salvation layer usually through hydrogen bonding. 3. Solvent entrapped with in the network structure. 8 The ratio of three solvent types in a given gel, are dependent on the polymer concentration and the solvent affinity for the polymer .solvent affinity governs the extension of this random coil. The greater the solvent affinity the more the coil expands and entangles with adjacent coils to form crosslinks. In a good solvent the polymer chains are interpenetrated by solvent molecules and the solvation layer is enhanced, which facilitates random expansion and network formation. In a poor solvent, the polymer chains contract, to minimize the solvent contact, thereby reducing the effective number of cross links and weakens the gel network structure. Gelation theory can be readily applied when formulating gel products and some of the desirable attributes of the gel formulations are in the following order. For optimum consumer appeal, the gel should have good optical clarity and sparkling appearance. To preserve product integrity, the gel should maintain its viscosity at all temperatures that may be countered during shipment and storage. 9 CHAPTER 1.3 Skin Characteristics 10 Structure of Skin5 11 Anatomy and Organization of Human Skin5 The skin constitutes one of the largest interfaces between the body and the environment. One the other hand, the function of human skin is to protect our body against physical, chemical, microbes, loss of water and other endogenous substances; on the other hand it is involved in thermoregulation of the body and serves as an excretory organ. This bifunctional nature of the skin depends on its highly differentiated structure of the skin. Understanding the skin absorption process, such as safety aspects of chemicals, other xenobiotics and cosmetic formulations and utilizing the opportunity to deliver drug substances to the skin further to systemic circulation it is essential to study the structure of skin. Functions Skin performs the following functions: 1. Protection: an anatomical barrier from pathogens and damage between the internal and external environment in bodily defense; Langerhans cells in the skin are part of the adaptive immune system. 2. Sensation: contains a variety of nerve endings that react to heat and cold, touch, pressure, vibration, and tissue injury; see somatosensory system and haptics. 3. Heat regulation: the skin contains a blood supply far greater than its requirements which allows precise control of energy loss by radiation, convection and conduction. Dilated blood vessels increase perfusion and heat loss while constricted vessels greatly reduce cutaneous blood flow and conserve heat. Erector pili muscles are significant in animals. 4. Control of evaporation: the skin provides a relatively dry and impermeable barrier to fluid loss. Loss of this function contributes to the massive fluid loss in burns. 5. Aesthetics and communication: others see our skin and can assess our mood, physical state and attractiveness. 6. Storage and synthesis: acts as a storage center for lipids and water, as well as a means of synthesis of vitamin D by action of UV on certain parts of the skin. 12 7. Excretion: sweat contains urea, however its concentration is 1/130th that of urine, hence excretion by sweating is at most a secondary function to temperature regulation. 8. Absorption: Oxygen, nitrogen and carbon dioxide can diffuse into the epidermis in small amounts, some animals using their skin for their sole respiration organ. In addition, medicine can be administered through the skin, by ointments or by means of adhesive patch, such as the nicotine patch or iontophoresis. The skin is an important site of transport in many other organisms. 9. Water resistance: The skin acts as a water resistant barrier so essential nutrients aren't washed out of the body. Components of normal human skin Human skin consists of a stratified, cellular epidermis and an underlying dermis of connective tissue. The dermal-epidermal junction is undulating in section; ridges of the epidermis known as rete ridges, project into the dermis. The junction provides mechanical support for the epidermis and acts as a partial barrier against exchange of cells and large molecules below the dermis is a fatty layer, the panniculus adiposus, usually designate as‘subcutaneous’. This is separated from the rest of the body by a vestigial layer of striated muscle, the panniculus carnosus. There are two main kinds of human skin. Glabrous skin (Non-hairy skin), found on the palms and soles, is grooved on its surface by continuously alternating ridges and sulci, in individually unique configurations known as dermatoglyphics. It is characterized by a thick epidermis divided into several well marked layers including a compact stratum corneum, by the presence of encapsulated sense organs within the dermis, and by a lack of hair follicles and sebaceous glands. Hair bearing skin on the other hand, has both hair follicles and sebaceous glands but lacks encapsulated sense organs. There is also wide variation between different body sites. For example, the scalp, with its large hair follicles may be contrasted with the forehead, which has only small vellus-producing follicles with albeit associated with large sebaceous glands. The axilla is notable because it has apocrine glands in addition to the eccrine sweat glands, which are found throughout the body. 13 Anatomical Structure of Human Skin The multitude of different functions of human skin can be achieved by unique anatomical structure of different skin layers. These are as follows: Epidermis Dermis Subcutaneous tissue Skin appendages EPIDERMIS The epidermis is composed of stratified squamous epithelium and contains four different types of cells. They are: 1. Keratinocytes 2. Melanocytes 3. Langerhans cells 4. Granstein cells The keratinocytes of the epidermis are organized into the following layers from superficial to deepest region. Because of practical reasons the human epidermis can be divided into: Stratum corneum(horny layer) Stratum lucidum Stratum granulosum (granular layer) Stratum spinosum (prickly cell layer) Stratum germinativum (basal layer and dermoepidermal junction). The multilayer envelope of epidermis varies in thickness, depending on the cell size and number of layers, ranging from about 0.8mm on the palms and the soles, down to 0.06mm. Cells provide epithelial tissue differ from those of all other organs. The cells that ascend from the proliferative layer of basal cells, they do change in an ordered fashion from metabolically active dividing cells to dense, dead, keratinized protein. 14 LAYERS OF EPIDERMIS5 15 Stratum corneum (horny layer) This is the main barrier function being located in the outermost skin. It consists of separated, nonviable, cornified, almost non permeable corneocytes embedded into a continuous lipid bilayer made up of various classes of lipids, for example: ceramides, cholesterol, cholesterol esters, free fatty acids and triglycerides. Stratum corneum is crucial for controlling the percutaneous absorption of dermally applied substances and regulating fluid homeostasis. The selective permeability of its elegant structure provides a central theme in many aspects of design of cosmetics. The thickness of stratum corneum is usually 10-25 micrometer with exceptions in the soles and palms, and it swells several folds when hydrated. All components of stratum corneum originate from the basal layer of epidermis, the stratum germinativum. Stratum lucidum (prickly cell layer) These are present only at the palm of the hand and soles of the foot. The cells are non nuclear. It has an anatomically distinct, poorly staining hyaline zone forms a thin layer. Stratum granulosum (granular layer) The stratum granulosum (or granular layer) is a layer of the epidermis found between the stratum corneum (and possibly stratum lucidum) and stratum spinosum. In this layer, keratinocytes are now called granular cells, and contain keratohyalin and lamellar granules. Stratum spinosum The stratum spinosum (or spinous layer) is a layer of the epidermis found between the stratum granulosum and stratum basale. This layer is also referred to as the "spinous" or "prickle-cell" layer. Keratinization begins in the stratum spinosum. Cells that move into the spinosum layer (also called prickle cell layer) change from being columnar to polygonal. In this layer the cells start to synthesize keratin. 16 Stratum germinativum The Stratum germinativum (or basal layer, stratum basale) is the deepest layer of the epidermis, a continuous layer of cells often described as one cell thick, though it may be two to three cells thick in glabrous skin and hyperproliferative epidermis. The basal cells of this layer can be considered the "stem cells" of the epidermis, undifferentiated, proliferating, and creating daughter cells that migrate upward, beginning the process of differentiation. DERMIS The dermis is a layer of skin between the epidermis and subcutaneous tissues, and is composed of two layers, the papillary and reticular dermis. Structural components of the dermis are collagen, elastic fibers, and extrafibrillar matrix (previously called ground substance). It is about 0.2 to 0.3cm thick. The elasticity of the skin is due to the network or gel structure of the cells. The upper papillary layer, contain a thin arrangement of collagen fibers. The lower reticular layer is made up of thick collagen fibers arranged parallel. SUBCUTANEOUS TISSUE The subcutaneous tissue is a layer of fat that lies between the dermis of the skin and underlying fascia. Subcutaneous fat insulates the body, absorbs trauma, and is a reserve energy source. This tissue may be further divided into two components, the actual fatty layer, or panniculus adiposus, and a deeper vestigial layer of muscle, the panniculus carnosus. The subcutaneous layer contains fat and connective tissue that houses larger blood vessels and nerves. This layer is important is the regulation of temperature of the skin itself and the body. The size of this layer varies throughout the body and from person to person. SKIN APPENDAGES Skin appendages are appendages that are associated with the skin and serve a particular function. In humans some of the more common skin appendages are hairs (sensation, heat loss, filter for breathing, protection), arrector pilli (smooth muscles that pull hairs straight), sebaceous glands 17 (secrete sebum onto hair follicle to oil the hair), sweat glands (can be sweat secreted with strong odour (apocrine) or with a faint odour (eccrine)) and nails (protection). FACTORS IN SKIN PENETRATION Factor that influence skin penetration are the physicochemical properties of drug and vehicle, pH and concentration. Different physiological variables involve the condition of the skin i.e. whether intact or injured, the skin age, the area of the skin treated thickness of the skin barrier phase, the species variation and the skin moisture content. The principle physicochemical factor in skin penetration is the hydration state of stratum corneum, which affect the rate of passage of all substances that penetrate the skin. The solubility of a drug determines the concentration presented to the absorption site and the water/lipid partition coefficient influences the rate of transport. An inverse relation ship appears to exist between absorption rate and molecular weight. 18 CHAPTER 1.4 Wound Healing 19 Introduction5,6 Wound healing is a natural restorative response to tissue injury. Healing is the interaction of a complex cascade of cellular events that generates resurfacing, reconstitution, and restoration of the tensile strength of injured skin. Healing is a systematic process, traditionally explained in terms of 3 classic phases: inflammation, proliferation, and maturation. A clot forms and inflammatory cells debride injured tissue during the inflammatory phase. Epithelialization, fibroplasia, and angiogenesis occur during the proliferative phase. Meanwhile, granulation tissue forms and the wound begin to contract. Finally, during the maturation phase, collagen forms tight cross-links to other collagen and with protein molecules, increasing the tensile strength of the scar. For the sake of discussion and understanding, the process of wound healing may be considered a series of separate events. In actuality, the entire process is much more complicated, as cellular events that lead to scar formation occur in tandem. Many aspects of wound healing have yet to be elucidated. Surgeons should have an understanding of the process of wound healing to help produce scars that are cosmetically pleasing and do not impair function. TYPES OF WOUND HEALING Wounds may be broadly classified into categories: Closed wounds Open wounds Open wounds Open wounds can be classified according to the object that caused the wound. The types of open wound are: Incisions or incised wounds, caused by a clean, sharp-edged object such as a knife, a razor or a glass splinter. Lacerations, irregular tear-like wounds caused by some blunt trauma. The term laceration is commonly misused in reference to incisions. 20 Abrasions (grazes), superficial wounds in which the topmost layer of the skin (the epidermis) is scraped off. Abrasions are often caused by a sliding fall onto a rough surface. Puncture wounds, caused by an object puncturing the skin, such as a nail or needle. Penetration wounds, caused by an object such as a knife entering the body. Gunshot wounds, caused by a bullet or similar projectile driving into or through the body. There may be two wounds, one at the site of entry and one at the site of exit, such is generally known as a throughand-through. Closed wounds Closed wounds have fewer categories, but are just as dangerous as open wounds. The types of closed wounds are: Contusions, more commonly known as bruises, caused by blunt force trauma that damage tissue under the skin. Hematomas, also called blood tumors, caused by damage to a blood vessel that in turn causes blood to collect under the skin. Crushing injuries, caused by a great or extreme amount of force applied over a long period of time. INFLAMMATORY PHASE The early events of wound healing are characterized by the inflammatory phase, a vascular and cellular response to injury. An incision made through a full thickness of skin causes a disruption of the microvasculature and immediate hemorrhage. Following incision of the skin, a 5 to 10 minute period of vasoconstriction ensues, mediated by epinephrine, norepinephrine, prostaglandins, serotonin, and thromboxane. Vasoconstriction causes temporary blanching of the wound and functions to reduce hemorrhage immediately following tissue injury, aid in platelet aggregation, and keep healing factors within the wound. Endothelial cells retract to expose the sub endothelial collagen surfaces; platelets attach to these surfaces. Adhesion to exposed collagen surfaces and to other platelets occurs through adhesive glycoproteins: fibrinogen, fibronectin, thrombospondin, and von Willebrand factor. The 21 aggregation of platelets results in the formation of the primary platelet plug. Aggregation and attachment to exposed collagen surfaces activates the platelets. Activation enables platelets to degranulate and release chemotactic and growth factors, such as platelet-derived growth factor (PDGF), proteases, and vasoactive agents (eg, serotonin, histamine). The coagulation cascade occurs via 2 different pathways. The intrinsic pathway begins with the activation of factor XII (Hageman factor) when blood is exposed to extravascular surfaces. The extrinsic coagulation pathway occurs through the activation of tissue factor found in extravascular cells in the presence of factors VII and VIIa. Both pathways proceed to the activation of thrombin, which converts fibrinogen to fibrin. The fibrin product is essential to wound healing and is the primary component of the wound matrix into which inflammatory cells, platelets, and plasma proteins migrate. Removal of the fibrin matrix impedes wound healing. In addition to activation of fibrin, thrombin facilitates migration of inflammatory cells to the site of injury by increasing vascular permeability. By this mechanism, factors and cells necessary for healing flow from the intravascular space and into the extravascular space. The result of platelet aggregation and the coagulation cascade is clot formation. Clot formation is limited in duration and to the site of injury. Clot formation dissipates as its stimuli dissipate. Plasminogen is converted to plasmin, a potent enzyme that aids in cell lysis. Clot formation is limited to the site of injury because uninjured nearby endothelial cells produce prostacyclin, an inhibitor of platelet aggregation. In uninjured adjacent areas, antithrombin III binds thrombin, and protein C binds factors of the coagulation cascade, namely, factors V and VII. The vasoconstriction period is followed by a more persistent period of vasodilation mediated by histamine, prostaglandins, kinins, and leukotrienes. Vasodilation is responsible for the erythema, edema, and heat observed after tissue injury. Vasodilation is an important means by which the wound can be exposed to increased blood flow, accompanied by the necessary inflammatory cells and factors that fight infection and debride the wound of devitalized tissue. Alterations in pH (secondary to tissue and bacterial degradation), swelling, and tissue hypoxemia at the injury site contribute to the sensation of wound pain. 22 Following injury, the products of the earliest cellular events activate intricately related inflammatory pathways that modify subsequent events in the wound-healing process. For example, Hageman factor activates the kinin pathway, which produces bradykinin. Bradykinin stimulates vasodilation and increased vascular permeability. Histamine released from platelets and circulating mast cells increases vascular permeability and indirectly stimulates vasodilation through the production of prostaglandins E1 and E2. Prostaglandins cause vasodilation through the activation of the adenylate cyclase pathway via the production of cyclic adenosine monophosphate. Prostaglandins also accumulate at the area of injury through the activation of phospholipases located on injured cell membranes. Phospholipases stimulate the release of arachidonic acid, ultimately leading to the production of prostaglandins, leukotrienes, and other factors. Hageman factor also activates the classic complement pathway during the inflammatory phase. Inactive proteins of the complement system (ie, C1C9) are activated by means of a cascade of reactions. These proteins stimulate important inflammatory events such as chemotaxis, degranulation of mast cells, and cytolysis. C5a and C567 are chemotactic agents for neutrophil migration. C3a, C4a, and C5a cause degranulation of mast cells, which leads to release of histamine and increased vascular permeability. The membrane attack complex, C567, is responsible for cytolysis. The cellular aspect of the inflammatory phase occurs within hours of injury. Neutrophils are the predominant cell type for the first 48 hours after injury but do not appear essential to the wound-healing process. Neutrophils cleanse the wound site of bacteria and necrotic matter and release inflammatory mediators and bactericidal oxygen-free radicals. The absence of Neutrophils does not prevent healing. Macrophages are essential to wound healing and perhaps are the most important cells in the early phase of wound healing. Macrophages phagocytose debris and bacteria. Macrophages also secrete collagenases and elastases, which break down injured tissue and release cytokines. In addition, macrophages release PDGF, an important cytokine that stimulates the chemotaxis and proliferation of fibroblasts and smooth muscle cells. Finally, macrophages secrete substances that attract endothelial cells to the wound and stimulate their proliferation to promote angiogenesis. Macrophage-derived growth factors play a pivotal role in new tissue formation, as evidenced by the fact that new tissue formation in macrophage-depleted animal wounds demonstrates defective repair. In 23 studies in which experimental wounds are rendered monocytopenic, subsequent stages of fibroplasia and granulation tissue formation are impaired and the overall rate of wound healing is delayed. T lymphocytes migrate into the wound during the inflammatory phase, approximately 72 hours following injury. T lymphocytes are attracted to the wound by the cellular release of interleukin 1, which also contributes to the regulation of collagenase. Lymphocytes secrete lymphokines such as heparin-binding epidermal growth factor and basic fibroblast growth factor. Lymphocytes also play a role in cellular immunity and antibody production. PROLIFERATIVE PHASE Formation of granulation tissue is a central event during the proliferative phase. Inflammatory cells, fibroblasts, and neovasculature in a matrix of fibronectin, collagen, glycosaminoglycans, and proteoglycans comprise the granulation tissue. Granulation tissue formation occurs 3-5 days following injury and overlaps with the preceding inflammatory phase. Epithelialization Epithelialization is the formation of epithelium over a denuded surface. Epithelialization of an incisional wound involves the migration of cells at the wound edges over a distance of less than 1 mm, from one side of the incision to the other. Incisional wounds are epithelialized within 24-48 hours after injury. This epithelial layer provides a seal between the underlying wound and the environment. The process begins within hours of tissue injury. Epidermal cells at the wound edges undergo structural changes, allowing them to detach from their connections to other epidermal cells and to their basement membrane. Intracellular actin microfilaments are formed, allowing the epidermal cells to creep across the wound surface. As the cells migrate, they dissect the wound and separate the overlying eschar from the underlying viable tissue. In superficial wounds (e.g. wounds due to laser resurfacing, dermabrasion, chemical peel treatments) adnexal structures (e.g. sebaceous glands, hair follicles) contribute to reepithelialization. Epidermal cells secrete collagenases that break down collagen and plasminogen activator, which stimulates the production of plasmin. Plasmin promotes clot dissolution along the path of epithelial cell migration. The 24 extracellular wound matrix over which epithelial cells migrate has received increased emphasis in wound-healing research. Migrating epithelial cells interact with a provisional matrix of fibrin cross-linked to fibronectin and collagen. The matrix components may be a source of cell signals to facilitate epithelial cell proliferation and migration. In particular, fibronectin seems to promote keratinocyte adhesion to guide these cells across the wound base. Wounds in a moist environment demonstrate a faster and more direct course of epithelialization. Occlusive and semiocclusive dressings applied in the first 48 hours after injury may maintain tissue humidity and optimize epithelialization. When epithelialization is complete, the epidermal cell assumes its original form, and new desmosomal linkages to other epidermal cells and hemidesmosomal linkages to the basement membrane are restored. Fibroplasia The fibroblast is a critical component of granulation tissue. Fibroblasts are responsible for the production of collagen, elastin, fibronectin, glycosaminoglycans, and proteases Fibroblasts grow in the wound as the number of inflammation cells decrease. The demand for inflammation disappears as the chemotactic factors that call inflammatory cells to the wound are no longer produced and as those already present in the wound are inactivated. Fibroplasia begins 3-5 days after injury and may last as long as 14 days. Skin fibroblasts and mesenchymal cells differentiate to perform migratory and contractile capabilities. Fibroblasts migrate and proliferate in response to fibronectin, platelet-derived growth factor (PDGF), fibroblast growth factor, transforming growth factor, and C5a. Fibronectin serves as an anchor for the myofibroblast as it migrates within the wound. The synthesis and deposition of collagen is a critical event in the proliferative phase and to wound healing in general. Collagen consists of 3 polypeptide chains, each twisted into a left-handed helix. Three chains of collagen aggregate by covalent bonds and twist into a right-handed superhelix, forming the basic collagen unit. A striking structural feature of collagen is that every third amino acid is glycine. This repeating structural feature is an absolute requirement for triple-helix formation. Collagen is rich in hydroxylysine and hydroxyproline moieties, which enable it to form 25 strong cross-links. The hydroxylation of proline and lysine residues depends on the presence of oxygen, vitamin C, ferrous iron, and -ketoglutarate. A deficiency of oxygen and vitamin C, in particular, result in underhydroxylated collagen that is less capable of forming strong cross-links and, therefore, is more vulnerable to breakdown. Collagen is secreted to the extracellular space in the form of procollagen. This form is then cleaved of its terminal segments and called tropocollagen. Tropocollagen can aggregate with other tropocollagen molecules to form collagen filaments. Filaments consist of tropocollagen molecules arrayed in a staggered fashion, joined by intermolecular crosslinks. Filaments aggregate to form fibrils. Collagen fibrils, in turn, aggregate to form collagen fibers. Filament, fibril, and fiber formation occur within a matrix gel of glycosaminoglycans, hyaluronic acid, chondroitin sulfate, dermatan sulfate, and heparin sulfate produced by fibroblasts. Intermolecular cross-links within the collagen fiber stabilize it, making it resistant to destruction. Age, tension, pressure, and stress affect the rate of collagen synthesis. Collagen synthesis begins approximately 3 days after injury and may continue at a rapid rate for approximately 2-4 weeks. Collagen synthesis is controlled by the presence of collagenases and other factors that destroy collagen as new collagen is made. Approximately 80% of the collagen in normal skin is type I collagen; the remaining is mostly type III. In contrast, type III collagen is the primary component of early granulation tissue and is abundant in embryonic tissue. Collagen fibers are deposited in a framework of fibronectin. An essential interaction seems to exist between fibronectin and collagen; experimental wounds depleted of fibronectin demonstrate decreased collagen accumulation. Elastin is also present in the wound in smaller amounts. Elastin is a structural protein with random coils that allow for stretch and recoil properties of the skin. Angiogenesis A rich blood supply is vital to sustain newly formed tissue and is appreciated in the erythema of a newly formed scar. These blood vessels disappear as they become unnecessary, as does the erythema of the scar. The 26 macrophage is essential to the stimulation of angiogenesis and produces macrophage-derived angiogenic factor in response to low tissue oxygenation. This factor functions as a chemoattractant for endothelial cells. Basic fibroblast growth factor secreted by the macrophage and vascular endothelial growth factor secreted by the epidermal cell are also important to angiogenesis. Fibronectin is chemotactic for endothelial cells. Capillaries bud from existing capillaries in response to these growth factors. Endothelial cells coalesce and bind fibrin, which adds support to the vessel wall. Angiogenesis results in greater blood flow to the wound and, consequently, increased perfusion of healing factors. Angiogenesis ceases as the demand for new blood vessels ceases. New blood vessels that become unnecessary disappear by apoptosis. New blood vessel formation is a complex process that relies on several angiogenic factors such as vascular endothelial growth factor, angiogenin, and angiotropin. Contraction Wound contraction begins almost concurrently with collagen synthesis. Contraction, defined as the centripetal movement of wound edges that facilitates closure of a wound defect, is maximal 5-15 days after injury. Contraction results in a decrease in wound size, appreciated from end to end along an incision; a 2-cm incision may measure 1.8 cm after contraction. The maximal rate of contraction is 0.75 mm/d and depends on the degree of tissue laxity and shape of the wound. Loose tissues contract more than tissues with poor laxity, and square wounds tend to contract more than circular wounds. Wound contraction depends on the myofibroblast located at the periphery of the wound, its connection to components of the extracellular matrix, and myofibroblast proliferation. Radiation and drugs, which inhibit cell division, have been noted to delay wound contraction. Contraction does not seem to depend on collagen synthesis. Although the role of the peripheral nervous system in wound healing is not well delineated, recent studies have suggested that sympathetic innervation may affect wound contraction and epithelialization through unknown mechanisms. 27 Contraction must be distinguished from contracture, a pathologic process of excessive contraction that limits motion of the underlying tissues and is typically caused by the application of excessive stress to the wound. MATURATION PHASE Collagen Collagen remodeling during the maturation phase depends on continued collagen synthesis in the presence of collagen destruction. Collagenases and matrix metalloproteinases in the wound assist removal of excess collagen while synthesis of new collagen persists. Tissue inhibitors of metalloproteinases limit these collagenolytic enzymes, so that a balance exists between formation of new collagen and removal of old collagen. During remodeling, collagen becomes increasingly organized. Fibronectin gradually disappears, and hyaluronic acid and glycosaminoglycans are replaced by proteoglycans. Type III collagen is replaced by type I collagen. Water is resorbed from the scar. These events allow collagen fibers to lie closer together, facilitating collagen cross-linking and ultimately decreasing scar thickness. Intramolecular and intermolecular collagen cross-links result in increased wound bursting strength. Remodeling begins approximately 21 days after injury, when the net collagen content of the wound is stable. Remodeling may continue indefinitely. The tensile strength of a wound is a measurement of its load capacity per unit area. The bursting strength of a wound is the force required to break a wound regardless of its dimension. Bursting strength varies with skin thickness. Peak tensile strength of a wound occurs approximately 60 days after injury. A healed wound only reaches approximately 80% of the tensile strength of unwounded skin. Cytokines Cytokines have emerged as important mediators of wound healing events. By definition, a cytokine is a protein mediator, released from various cell sources, which binds to cell surface receptors to stimulate a cell response. Cytokines can reach their target cell by endocrine, paracrine, 28 autocrine, or intracrine routes. Some important cytokines are described as follows: Epidermal growth factor was the first cytokine described and is a potent mitogen for epithelial cells, endothelial cells, and fibroblasts. Epidermal growth factor stimulates fibronectin synthesis, angiogenesis, fibroplasia, and collagenase activity. Fibroblast growth factor is a mitogen for mesenchymal cells and an important stimulus for angiogenesis. Fibroblast growth factor is a mitogen for endothelial cells, fibroblasts, keratinocytes, and myoblasts. This factor also stimulates wound contraction and epithelialization and production of collagen, fibronectin, and proteoglycans. PDGF is released from the alpha granules of platelets and is responsible for the stimulation of neutrophils and macrophages and for the production of transforming growth factor. PDGF is a mitogen and chemotactic agent for fibroblasts and smooth muscle cells and stimulates angiogenesis, collagen synthesis, and collagenase. Vascular endothelial growth factor is similar to PDGF but does not bind the same receptors. Vascular endothelial growth factor is mitogenic for endothelial cells and plays an important role in angiogenesis. Transforming growth factor- is released from the alpha granules of platelets and has been shown to regulate its own production in an autocrine manner. This factor is an important stimulant for fibroblast proliferation and the production of proteoglycans, collagen, and fibrin. The factor also promotes accumulation of the extracellular matrix and fibrosis. Transforming growth factor- has been demonstrated to reduce scarring and to reverse the inhibition of wound healing by glucocorticoids. Tumor necrosis factor is produced by macrophages and stimulates angiogenesis and the synthesis of collagen and collagenase. Tumor necrosis factor is a mitogen for fibroblasts. 29 Overview of involved growth factors Following are the main growth factors involved in wound healing: Growth factor Abbreviation Main origins Effects Epidermal EGF growth factor Activated macrophages Salivary glands Keratinocytes Transforming TGF-α growth factor-α Activated macrophages T-lymphocytes Keratinocytes Hepatocyte HGF growth factor Mesenchymal cells Vascular endothelial VEGF growth factor Platelet PDGF derived growth factor Mesenchymal cells Platelets Macrophages Endothelial cells 30 Keratinocyte and fibroblast mitogen Keratinocyte migration Granulation tissue formation Hepatocyte and epithelial cell proliferation Expression of antimicrobial peptides Epithelial and endothelial cell proliferation Hepatocyte motility Vascular permeability Endothelial cell proliferation Granulocyte, macrophage, fibroblast and Smooth muscle cells Keratinocytes Fibroblast growth factor FGF-1, -2 1 and 2 Macrophages Mast cells T-lymphocytes Endothelial cells Fibroblasts Transforming TGF-β growth factorβ Platelets 31 smooth muscle cell chemotaxis Granulocyte, macrophage and fibroblast activation Fibroblast, endothelial cell and smooth muscle cell proliferation Matrix metalloproteinas e, fibronectin and hyaluronan production Angiogenesis Wound remodeling Integrin expression regulation Fibroblast chemotaxis Fibroblast and keratinocyte proliferation Keratinocyte migration Angiogenesis Wound contraction matrix deposition Granulocyte, macrophage, lymphocyte, T-lymphocytes Macrophages Endothelial cells Keratinocytes Smooth muscle cells Fibroblasts Keratinocyte KGF growth factor Fibroblasts 32 fibroblast and smooth muscle cell chemotaxis Angiogenesis Fibroplasia Matrix metalloproteinas e production inhibition Keratinocyte proliferation Keratinocyte migration, proliferation and differentiation CHAPTER 1.5 Biological Methods for the Study Of Wound Healing7 33 Biological Methods for the Study of Wound Healing7 Animal models and in-vitro assays have become indispensable tools for researchers in nearly every scientific discipline. In product development there is a need for translational research to obtain data that can lead to sound clinical trials and ultimately, improved wound care. This process is usually performed in a stepwise fashion starting with in-vitro testing, preclinical, and then clinical evaluations (Figure 1). In-vitro studies help determine which concentrations may be effective in-vivo and determine whether certain products are effective on various cell types (e.g. fibroblasts and keratinocytes). The next step is to examine the effect of the product’s use in an animal model(s). This facilitates investigation of the product in the presence of wound fluid, blood, immune cells, proteases, etc., which can have an effect on the activity of the active agent. Many in-vivo animal studies initially investigate the safety and/or irritancy of the product. It is important to be sure that these agents do 34 not have a toxic effect on tissues. Efficacy animal trials are conducted after the safety studies are completed. This eventually allows the product to be evaluated in human trials. Although definitive studies conducted on human subjects are needed, such studies present several practical, ethical, and moral concerns. For example, in order to examine wounds histologically throughout the entire healing process one must biopsy a human subject at multiple time points, which is impractical. Furthermore, ethical considerations prevent the intentional infection of a wound on a human or the use of an untreated control subject. Some of the practical difficulties lie in obtaining enough subjects with similar or identical situations to conduct well controlled studies. Another complication to factor in with human trials is compliance (e.g. subject’s level of cooperation, ability to understand and follow instructions). The above difficulties have led researchers to develop multiple in-vitro and in-vivo models that attempt to mimic or reproduce human conditions. [1] In-vitro technique In-vitro assays are great for examining the effect of agents on particular cell types. They are relatively inexpensive, fast, and convenient for the researcher. In addition to providing useful results in a short time, they possess an obvious humane appeal since they usually do not involve the use of animals or humans. In-vitro assays are useful in wound healing research for determining the possible effectiveness of various treatments, particularly antimicrobial and healing enhancing agents. Another noteworthy attribute of in-vitro testing is the ability to screen multiple agents or samples simultaneously. Assays can aid in the early detection of antimicrobial resistance among pathogens and determination of minimal inhibitory concentrations (MIC), and allow for highly specific control over the experimental conditions. However, it is difficult to simulate a “real world” application. Although some variables such as pH, salinity, and temperature are easily controlled, in-vitro assays are incapable of completely reproducing biological conditions (e.g. immune responses, healing) and diseases, such as diabetes. In order to approximate in-vivo experiments, in-vitro assays have been developed that incorporate some variety of cell or tissue system. Wound closure studies have been conducted on single cell monolayer systems. 35 The principle in vitro technique for studying the skin penetration evolves the use of variety of diffusion cells in which animal or human skin is fastened to a holder and the passage of compounds from epidermal surface to a fluid bath is measured. Many chemical agents can be used which penetrate in sufficient concentration to be determined by different physical and chemical analysis. More recently model systems have been used which do not use membranes. Solvent such as alcohol –water have been used as models chosen to have negligible solubility in phase representing the skin, but in which drug is fairly soluble. A receptor phase like chloroform and isopropyl myristate can also be used to receive the penetrant. Important factors influencing release in to receptor phase are solubility in the vehicle and partition coefficient of the drug between vehicle and the receptor phase. Optimum release is obtained from vehicle containing the minimum concentration of solvent required for complete solubilization of the drug. [2] In-vivo technique Small mammal wound healing models. Rodent and small mammal models of wound healing have emerged as the model of choice for many researchers. This type of study is beneficial to wound research for multiple reasons. Small animals are inexpensive, easily obtainable, and require less space, food, and water. Additionally, they often have multiple offspring, which develop quickly allowing experiments to proceed through multiple generations. Small animals usually have accelerated modes of healing compared to humans, thus experiment duration lasts for days, as opposed to weeks or months in human experiments. Some small mammals can easily be altered genetically and provide a wound model capable of approximating defective human conditions such as diabetes, immunological deficiencies, and obesity. Another advantage of small mammal models is their ability to serve in experiments where death is an endpoint, as is some cases of bacterial or viral infection. Small animals provide a multitude of model choices for various human wound conditions. Some models have been developed to investigate the mechanistic particulars of certain aspects of healing. 36 The major in-vivo methods are histological techniques, use of tracers, analysis of body fluids and tissues and elicitation of biological response. Tissue changes in skin following the application of various substances to the cuetaneous surface can yield information about specific tissues affected, so that not only absorption is revealed but also the route of penetration. For studying the wound in the laboratory, mainly two types of wounds are produced experimentally. These are excised or open wounds and incised or sutured wounds. The assessment of healing is made by studying the regenerating tissue by different parameters. Following types of wounds are made in laboratory animals for studying the effect of various drugs. 1) Excised wound or Open Wound These types of wounds are prepared either on rats or guinea pigs. Back of each animal is shaved and prepared after washing with spirit for operation. An area of about 2.0 sq cm is marked out by an Indian market ink with the help of stencil. The marked area is excised with sharp knife and scissors under ether anesthesia. After making wound the animals are divided in two groups. One control group and the other test group and are kept in isolated cages. Topical application of ointments or lotions are made on is founds daily. On desired postoperative days this founded animals are sacrifice and the contraction measured. Biochemical estimation of granulation tissue and histological examination’s are done. 2) Incised Or Sutured Skin Wounds After preparing the animals for operation under aseptic conditions, a longitudinal cutaneous incision measuring about 3-5c.m was made at the back or abdomen according to the type of animals selected. Wounds are closed by interrupted cotton threads stitches, which are placed approximately at equal distance. The tensile strengths, biochemical and histological study of the wound are carried out. 37 3) Musculoperitoneal Wounds To prepare this wound, animals are prepared in the same fashion as described earlier but their abdomen is opened completely incision measuring between 2-5c.m according to the size of the animals are made. The wound is caused in one layer by interrupted linen stitches. Tensile strength and busting abdomen, by chemical and histological studies are done on this wounds tissue, after sacrifice the animals on desired post operative days. 4) Burn wounds The burn is produced under aseptic condition on hair removed areas of back of rats/guinea pigs with special device cosseting of a square sheet of an iron piece measuring 4.8sq.cm with wooden handle. It is heated to a red hot over flying and is placed in contact with the back of the anaesthetized rat up to ten seconds, with out any pressure. Medication is applied these animals are sacrificed on desired days and the regenerated tissues are removed for biochemical and the histological studies etc. their wounds are also measured for the contraction. 5) Dead Space Wound Method Subcutaneous implantation of sterilize cotton pellets (10 mg each) and a plastic road (25-30mm) in the axial are anti groin respectively is done under ether anesthesia in male albino rabbits. The 10th day old granulomas are carefully dissected and cleared of the tissues. 38 METHOD OF ASSESSMENT8 1. MACROSCOPIC EXAMINATION OF THE WOUNDS:Gross examination of wound gives some information regarding the healing. One can easily distinguish the normally healing wounds with that of a wound with delayed healing by a careful gross examination provided the different is marked in both the wounds. Gross examination sometimes may not give much information; hence quantitative methods can be used in such cases. For this purpose measurement the size of the wounds gives sufficient information. This can be done using a planimeter or using a graph paper 2. MICROSCOPIC METHOD This method involves histological examination of tissue. 3. ELECTRON MICROSCOPIC METHOD This technique is used for the study of details about the cellular morphology and other alteration at cellular levels during healing and regeneration. 39 CHAPTER 1.6 Plant Profile9 40 Pothos scandens (Araceae) 41 BOTANICAL INFORMATION9 Botanical Name : Pothos scandens Division : Magnoliophyta Class : Liliopsida Subclass : Monocots Order : Alismatales Family : Araceae Subfamily : Pothoideae Tribe : Potheae Vernacular Names Malayalam Tamil Kannada : Annaparuva, Paruvakodi : Anaparuga : Adkebiluballi Botanical Description: Pothos scandens is the botanical name of the plant. It is a climbing shrub having adventitious aerial roots. The internodes of the plant are 1.32.5 cms and its leaves are very variable. The leaves are obovate, elliptic or lanceolate and coriaceous, having a bright green colour. The apex of the plant is acute, acuminate or apiculate, with cuneate or rounded base. The petioles of Pothos scandens are semiamplexicaul and broadly winged. They have a length of 2.5-7.5 cms and a width of 0.6-1.7 cm at the base. The green Spathe is 0.4-0.7 cm long, ovate and erect, with cuspidate apex. The stipe of the plant is deflexed, to 0.6 cm long and the spadix is yellow, with an approximate length of 0.5 cm. The spadix is globose, ovoid or shortly oblong. The fruits or berries of the plant are oblong and 1.3-1.7 cm long and they are scarlet when ripe. 42 Geographical Source: AFRICA Western Indian Ocean: Comoros; Madagascar; Seychelles ASIA-TEMPERATE China: China - Yunnan ASIA-TROPICAL Indian Subcontinent: Bangladesh; India - Assam, Bihar, Goa, Karnataka, Kerala, Maharashtra, Meghalaya, Orissa, Tamil Nadu, Tripura, West Bengal, Andaman and Nicobar. Indo-China: Cambodia; Laos; Myanmar; Thailand; Vietnam Indonesia - Java, Kalimantan, Lesser Sunda Islands, Moluccas, Sumatra; Ethnobotanical Uses Pothos scandens has quite a few medicinal properties and usages. The bruised root of the plant is reportedly applied to promote healing of abscesses, after being fried in oil. The Indian people use an infusion of the leaves of this plant as a bath for curing convulsions and epilepsy. Apart from that, the stem is also reportedly used to treat asthma, after being cut up with camphor and smoked like tobacco. Traditionally the plant is used by Ayurvedic physicians of Cheruvathur, Kerala mainly for its burn healing properties. Other uses include in treatment of vermifuge and small pox. 43 CHAPTER 1.7 Polymer Data10 44 Carbopol 940 Polymer10 Technical Data General INCI (International Nomenclature for Cosmetic Ingredients) Name: Carbomer Appearance: Fluffy, white dry powder Odour: Slightly Acetic Safety: 25-year history demonstrating non irritating and non sensitizing Elegance: Luxurious feel Efficiency: Forms gel at very low concentration Viscosity: 40,000-60,000 cps of a 0.5% aqueous dispersion Moisture Content: Maximum 2.0% Microorganism Resistance: No support for bacteria fungus and mould growth Physical Properties: The three dimensional nature of these polymers confers some unique characteristics, such as biological inertness, not found in similar linear polymers. The Carbopol resins are hydrophilic substances that are not soluble in water. Rather, these polymers swell when dispersed in water forming a colloidal, mucilage-like dispersion. Carbopol polymers are bearing very good water sorption property. They swell in water up to 1000 times their original volume and 10 times their original diameter to form a gel when exposed to a pH environment above 4.0 to 6.0. Because the pKa of these polymers is 6.0 to 0.5, the carboxylate moiety on the polymer backbone ionizes, resulting in repulsion between the native charges, which adds to the swelling of the polymer. The 45 glass transition temperature of Carbopol polymers is 105°C (221°F) in powder form. However, glass transition temperature decreases significantly as the polymer comes into contact of water. The polymer chains start gyrating and radius of gyration becomes increasingly larger. Macroscopically, this phenomenon manifests itself as swelling. Chemical properties Carbopol pentaerythritol. 940 polymer is acrylic acid cross linked with General Structure of Carbopol Polymers in figure No: 1 Fig. No. 1 Shelf life Carbopol polymers are stable for years when protected from moisture. In powder form there is no reason for polymer to degrade. Storage Keep in a tightly closed container Features and Benefits of Carbopol 940 Polymer Short flow properties High viscosity High suspending ability High clarity 46 Recommended Applications Hair styling gels Hydroalcoholic gels Moisturizing gels Bath gels Hand, body and face lotions Creams Selecting the Right Carbopol Polymer Requirement Recommended Carbopol Polymer Clear gels > 3000 cP Suspensions or emulsions at > 3000 cP 940 934, 940 Suspensions or emulsions at < 3000 cP 941 Higher shear resistance Better ion resistance Better thermal stability 934, 940 941 934, 940 47 CHAPTER 2 Review of Literature11 48 Review of Literature 11 S. Ignacimuthu et al studied the traditional knowledge of Kani tribals in Kouthalai of Tirunelveli hills, Tamil Nadu, India. An ethnobotanical survey was carried out among the ethnic groups (Kani/Kanikaran) in Southern Western Ghats of India. Traditional uses of 54 plant species belonging to 26 families are described under this study including Pothos scandens. In this communication, the information got from the tribal was compared with the already existing literature on ethnobotany of India. The documented ethnomedicinal plants were mostly used to cure skin diseases, poison bites, wounds and rheumatism. The medicinal plants used by kanis are arranged alphabetically followed by family name, local name, major chemical constituents, parts used, mode of preparation and medicinal uses. Christine A. Williams et al studied the Anthocyanin pigments and leaf flavonoids in the Family: Araceae. The study revealed that Anthocyanins, variously identified in inflorescence, fruit, leaf or petiole of 59 representative species of the Araceae, are of a simple type. Mohsin Raza et al studied the anticonvulsant activities of 334 medicinal plants used for the treatment of epilepsy and convulsive disorders in the indigenous system of medicine including Pothos scandens. Geoffrey C. Kite et al studied the Polyhydroxyalkaloids in the Aroid Tribes Nephthytideae and Aglaonemateae. They conducted a survey of polyhydroxyalkaloids in species of 52 genera of Araceae revealed the presence of 2,5-dihydroxymethyl-3,4-dihydroxypyrrolidine (DMDP) and αhomonojirimycin (HNJ). S.A. Salgare et al studied the effect of Ambient Air (from Chembur) on the Chlorophyll Content of Cultivated Plants. The ambient air from Chambur inhibited the chlorophyll content of plants collected from polluted zones. The plants were collected from three different zones i.e. Collector’s colony, Chembur Colony and Colaba (treated as control). Collections were made in the winter season. The plants for this study are Malvaviscus arboreus, Graptophyllun bertense. Ixora cocclnea, Nerlum odorum, Pothos scandens, Quisqualis Indic, Tanbernae Montana coronarl. Chlorophyll was estimated using Arnon’s method. Maximum inhibition in the chlorophyll content was found with plants collected from Collector’s colony. 49 Grewal,-J-S12 investigated the biochemical factors responsible for susceptibility or resistance of various plants against the scarlet mite, Brevipalpus phoenicis: I. amino acids analysis. Results are presented of amino acid analysis by thin layer chromatography for 11 out of 31 plant species screened for resistance or susceptibility to infestation by Brevipalpus phoenicis. Species stated to be resistant (Pothos scandens, Bauhinia variegata, Eucalyptus globulus and maize) contained tryptophan, tyrosine and hydroxyproline. Plant species lacking dihydroxyphenylalanine (Vicia feba [faba beans], Dalbergia sissoo and Cestrum nocturnum) did not support the development of B. phoenicis Dhanavel,-D13 et al conducted Cytotaxonomical studies in South Indian Araceae. Studies were carried out in 27 species belonging to 15 genera of Araceae from Tamil Nadu, India. First record of chromosome numbers were made in 10 species, namely Alocasia macrorrhiza var. dark pink (2n=28), Pothos scandens (2n=32), Anthurium cubense (2n=30), A. polyrrhizum [A. polyrrhizon] (2n=16), Caladium bicolor var. local (2n=24), C. bicolor var. white stick with red spot (2n=40), Philodendron cymbispathum (2n=36), P. mello-baretoanum [P. mello-barretoanum = P. bipinnatifidum] (2n=30), Spathiphyllum wallisii (2n=18) and Dieffenbachia amoena (2n=54). The somatic chromosome number (2n) ranged from 16 to 54. The primary basic chromosome number may be 8 and other basic numbers should have originated by the addition of one or few basic chromosome numbers. The karyotype analyses show that each genus and species of a particular genus has a particular combination of different types of chromosomes. Therefore, karyotype alteration of chromosome play an important role in speciation, along with aneuploidy, euploidy and higher polyploidy. Hence, the present study of interrelationship among them will be more useful for future breeding programmes.. 50 CHAPTER 3 Objectives 51 OBJECTIVES The major objective is to develop this traditional medicinal plant into scientifically validated drug which is safe and therapeutically active. For the evaluation, the plant is subjected to: Phytochemical screening Formulating the extract into conventional dosage form. Biological evaluation 52 CHAPTER 4 Plan of Work 53 PLAN OF WORK PHARMACOGNOSTICAL STUDIES The Phytochemical investigations of a plant involve the following: Authentication of the plant Determination of Physicochemical Parameters Extraction of the plant Isolation and Characterization PHARMACEUTICAL STUDIES 1. Formulation with Carbopol 940 2. Evaluation of Carbopol 940 Estimations of drug Content Physical Observation Extrudability pH determination PHARMACOLOGICAL STUDIES Primary Skin Irritation Test Wound Healing Studies 54 Chapter 5 Pharmacognostical Studies 55 COLLECTION AND AUTHENTIFICATION OF THE PLANT The plant Pothos scandens Linn. (Family: Araceae) was selected for proposed study and was collected from Perinthalmanna, Malapuram District Kerala state, India. The collected plant was authenticated by Dr. Jiji Joseph, Assistant Professor of plant breeding, College of Horticulture, Kerala Agricultural University, Vellanikara, Thrissur. PRELIMINARY TREATMENT The foreign, earthy matter and residual materials were removed carefully from the leaves and stem parts and then subjected for washing and stored. The fresh leaves are cut and are subjected for extraction. PREPARATION OF AQUEOUS AND ALCOHOLIC EXTRACT 150gms of freshly cut leaves was placed in inside a thimble made from thick filter paper, which is loaded into the main chamber of the Soxhlet extractor. The Soxhlet extractor is placed onto a flask containing the extraction solvent i.e.; using 250ml distilled water and ethanol (90%) respectively for 80oC & 90oC for 6hrs. DETERMINATION OF PHYSICOCHEMICAL PARAMETERS14 The determination of water-soluble or ethanol-soluble extractive is used as a means of evaluating drugs the constituents of which are not readily estimated by other means. It indicates the nature of constituents present. The selected plant leaves are subjected for the following extractive values. ALCOHOL EXTRACTIVE VALUES About 5gm of powdered fresh leaves was macerated with 100ml of 90% ethanol in a stoppered conical flask for 24hrs with occasional stirring during first 6hrs and the first 5ml is discarded. Then 25ml of the filtrate was 56 evaporated on a tarred evaporating dish, and the residue was dried at 105 oC until a constant weight is obtained. WATER EXTRACTIVE VALUES About 5gm of powdered fresh leaves was macerated with 100ml of distilled water in a stoppered conical flask for 24hrs with occasional stirring during first 6hrs and the first 5ml is discarded. Then 25ml of the filtrate was evaporated on a tarred evaporating dish, and the residue was dried at 105 oC until a constant weight is obtained. PHYTOCHEMICAL SCREENING OF Pothos scandens The plant is subjected to preliminary phytochemical screening for the detection of various plant constituents present. The term qualitative analysis refers to the establishing and proving the identity of a substance. Systematic investigation of the plant material for its phytochemical behavior involves the following stages: 1. Procurement of raw material 2. Qualitative Phytochemical analysis 57 QUALITATIVE PHYTOCHEMICAL ANALYSIS15,16,17,18,19 The 90% ethanolic and aqueous extract of fresh leaves of Pothos scandens were subjected to the following chemical test separately for identification of various constituents. 1. Detection of Alkaloids a. Mayer’s Test: To 1ml of the extract added to 2ml of Mayer’s reagent, a dull white precipitate is obtained. Indicates presence of alkaloid b. Dragendroff’s Reagent: To 1ml of the extract added to 1ml Dragendroff’s reagent, an orange red precipitate is obtained. Indicates presence of alkaloid c. Hager’s Test: To 1ml of the extract added to 3ml of Mayer’s reagent, a yellow precipitate is obtained. Indicates presence of alkaloid d. Wagner’s Test: To 1ml of the extract added to 2ml of Wagner’s reagent, a reddish brown precipitate is obtained. Indicates presence of alkaloid 2. Detection of Carbohydrates a. Molish Test: To 1ml of the extract added to 1ml of alpha naphthol solution and concentrated sulphuric acid through sides of test tubes. Purple or Reddish violet colour at the junction of two liquid indicates presence of carbohydrate. b. Iodine Test: To 1ml of the extract added to 3 drops of iodine. Blue colour indicates presence of starch. c. Fehling’s Test: To 1ml of the extract added equal quantities of Fehling’s solution A and Fehling’s solution, upon heating 58 formation of brick red precipitate. Indicates presence of carbohydrate. d. Benedict’s test: To 1ml of the extract added Benedict’s solution, upon heating for 2min, formation of red precipitate. Indicates presence of carbohydrate. 3. Detection of Glycosides a. Borntragers Test: A few ml of dilute sulphuric acid was added to 1ml of the extract. Boiled, filtered, cooled and extract the filtrate with chloroform. The chloroform layer was treated with 1ml of ammonia. The formation of red colour in the ammoniacal layer indicates presence of anthraquinone glycoside. b. Modified Borntragers Test: To a few ml of dilute hydrochloric acid was added to 1ml of the extract and add few drops ferric chloride solution. Boiled, filtered, cooled and extract the filtrate with benzene. The chloroform layer was treated with 1ml of ammonia. The formation of red colour in the ammoniacal layer indicates presence of anthraquinone glycoside. c. Legal Test: The extract was dissolved in pyridine and sodium nitroprusside solution to make it alkaline. The formation of pink to red colour shows the presence glycoside. d. Baljet Test: To 1ml of the test extract was added to 1ml sodium picrate solution. The formation of yellow to orange colour indicates presence of glycoside. 4. Test for Saponin Glycosides a. Foam Test: the extract were diluted with distilled water upto 20 times and shaken in a graduated cylinder for 15min. formation of 1cm foam indicates presence of saponins. 59 b. Haemolysis test: a blood smear was prepared and 1drop of extract was added. Formation of hemolytic zone after 5min indicates presence of saponins. 5. Test for Steroids a. Libermann sterol test: To a solution of glycosides or steroidal aglycones in glacial acetic acid, one drop of concentrated sulphuric acid was added. A play of colours was observed starting from rose, red, violet, blue to green. b. Libermann Buthard Test: The extract was dissolved in 2ml of chloroform in adry test tube. 10 drops of acetic anhydride and 2drops of concentrated suphuric acid is added on U.V chamber shows fluorescence c. Salkowaski Test: The extract was dissolved in chloroform and equal volumes of sulphuric acid are added. The formation of bluish red to cherry red colour in the chloroform layer and green florescence in acid layer. Indicates presence of steroids. 6. Detection of Amino acids and Proteins a. Biuret Test: 1ml of extract was added to 1ml of 40% sodium Hydroxide solution and two drops of 1% copper sulphate solution. Formation of violet colour indicates presence of protein. b. Xanthoproteic Test: 1ml of extract was added to 1ml of concentrated nitric acid. Awhite precipitate is formed; it is then boiled and cooled. Then 20% sodium hydroxide or ammonia is added. Orange colour indicates presence of aromatic aminoacid. c. Ninhydrin Test: 2drops of freshly prepared 0.2% ninhydrin reagent was added to the extract solution and heat. Development of blue colour reveals proteins and peptides. 60 7. Detection of Tannins and Phenolics a. Ferric chloride Test: 1ml of extract was added to 1ml of ferric chloride .formation of a dark blue or greenish black colour. Indicates presence of tannins b. Potassium Dichromate Test: The extract was added to potassium dichromatic solution, formation of a precipitate shows presence of tannins and phenolics. c. Lead Acetate Test: to the extract added 1ml of lead acetate solution. Formation of white precipitate indicates presence of tannins. 8. Detection of Flavones and Flavonones a. Aqueous NaOH: To the test solution add few drops of sodium hydroxide solution, gives an intense yellow colour which turns to colourless on addition of dilute acid. Indicates presence of flavanoid. b. Shinoda Test: To the extract add few magnesium turnings and concentrated hydrochloric acid and boiled. Red colour was produced. Indicates presence of flavanoid. 9. Detection of Fixed oils a. Spot test: A small quantity of extract was pressed between two filter papers. Oil stains indicates presence of fixed oils. b. Saponification test: To 1ml of the extract was added to a few drops of 0.5N alcoholic potassium hydroxide along with a drop of phenolphthalein. The mixture was heated on a water bath for 2hrs.The formation of soap or partial neutralization indicates the presence of fixed oils. 61 Chapter 6 Pharmaceutical Studies 62 FORMULATION TRIALS OF Pothos scandens ALCOHOLIC EXTRACT WITH CARBOPOL 940 Working Formula INGREDIENDS A1 %w/w A2 A3 A4 4 0.5 45 0.1 q.s 100 4 1 45 0.1 q.s 100 4 2 45 0.1 q.s 100 Pothos scandens alcohol extract Carbopol 940 Polyethylene glycol 400 Methyl paraben Triethanolamine Distilled water q.s upto 4 1.5 45 0.1 q.s 100 Procedure To a beaker accurately weigh Carbopol 940 which is dispersed in 35ml of distilled water with constant stirring using a mechanical stirrer for 30 min at 600-800rpm. To another beaker, add 4ml of the alcoholic extract in 45gm of PEG 400 and 0.1% methyl paraben in a mechanical stirrer for 30min. Mix the two solutions by constant stirring with adjustment of pH to neutral using triethanolamine until a clear consistent gel is obtained. (It is seen that neutralized aqueous gels of Carbopol show maximum viscosity at pH at 6-9) 63 EVALUATION OF GELS Pothos Scandens Linn ALCOHOLIC EXTRACT WITH CARBOPOL 940 PHYSICAL OBSERVATIONS: The gel formulations were observed for their visual appearance and transparency and homogeneity. EXTRUDABILITY The formulations were filled in collapsible tubes after the gels were set in the container. The Extrudability of formulation is checked. PH MEASUREMENTS PH measurements of the gel were carried out using a digital P H meter by dipping the glass electrode completely in to the gel system to cover the electrode. 64 Chapter 7 Pharmacological Studies 65 PRIMARY SKIN IRRITATION TEST20 Primary irritation test was done on rats by placing a piece of cotton wool soaked in a saturated solution of ethanolic extract of Pothos scandens on a shaved portion of dorsal skin and securing it firmly in place with adhesive plaster. This was allowed to remain in close contact with the skin for 24 hours, after which the site of application was examined for irritation with 0.8% formalin as control. WOUND HEALING STUDIES21,22,23 Healthy male albino rats was selected (150-250), from Kerala Agriculture University, Mannuthy, Thrissur were used. The animals are kept in cage for 20 days well fed. The back of the animal was shaved and washed with spirit. A circular area of 1cm diameter was marked with a marker on either side of bump region. The animals were anaesthetized with a combination of ketamine and xylazine. The back of the animal was shaved and washed with spirit. A circular area of 1cm diameter was marked with a marker on either side of bump region. A trichotomy of the back of the rats was performed, sufficient for 2 perforations are made (test and control). The pieces of tissue were subsequently excised with aid of scissors, scalpel and a forceps. The wounds on the left side were filled with gel extract (test wounds) and on the right side (control wounds) were filled with alcohol. After these procedures, the animals receive no other treatment until they are fully recovered. The application was received daily for the next 24 hours post operative days. The wound contractions were measured as percentage reduction in wound area for the 4th, 8th, 10th, and 12th days. The progressive decrease in the wound area was monitored periodically by tracing the wound margin on a tracing paper and area is accessed by placing a graph paper over a tracing paper. 66 Chapter 8 Result and discussion 67 PHARMACOGNOSTICAL STUDIES 1. PHYSICOCHEMICAL PARAMETER Physicochemical parameter like extractive values were determined for the selected plant material the result are shown in table No: 1 Table No: 1 Data showing different extractive value for the leaves of Pothos scandens Linn Extractive value (%w/v) Alcohol Water Soluble Soluble S.No Plant material 1 Fresh leaves scandens of Pothos 19.32% 19.22% 2. Preliminary Phytochemical Evaluation The 90% ethanolic extract and aqueous extract of the fresh leaves of Pothos scandens was subjected to preliminary phytochemical evaluation. The results are shown in table No: 2 68 Table No: 2 S.N 1 a. b. c. d. 2 a. b. c. d. 3. a. b. c. d. 4. a. b. 5. a. b. c. 6.. a. b. c. 7.. a. b. c. 8. a. b. 9. a. b. TESTS 90% ethanolic extract ALKALOIDS Dragendroff’s Test +ve Wagners test +ve Hagers test +ve Mayer’s Test +ve CARBOHYDRATES Molish test -ve Iodine test -ve Fehling’s test -ve Benedict’s test -ve GLYCOSIDES Borntrager’s test -ve Modified Borntrager’s test -ve Legal’s test -ve Baljet test -ve SAPONIN GLYCOSIDES Foam Test -ve Haemolysis test -ve STEROIDS Libermann sterol test -ve Libermann-Butchard test -ve Salkowsky test -ve AMINO ACIDS & PROTEINS Biuret test +ve Xanthoproteic test +ve Ninhydrin test -ve TANNINS & PHENOLICS K2Cr 2O7 test -ve FeCl 3 -ve Lead acetate -ve FLAVONES & FLAVONONES Aqueous NaOH +ve Shinoda Test +ve FIXED OILS Spot Test -ve Saponification Test -ve 69 Aqueous extract +ve -ve +ve +ve +ve -ve +ve +ve -ve -ve -ve -ve -ve -ve -ve -ve -ve +ve +ve -ve -ve -ve -ve +ve +ve -ve -ve It has been found that the 90% alcoholic extract contain alkaloids, proteins and flavanoids. Aqueous extract contain alkaloids, carbohydrates, proteins and flavanoids. PHARMACEUTICAL STUDIES FORMULATION TRIAL The given polymer concentration of 0.5, 1.0, 1.5 and 2.0%, the gel consistency in 0.5% was less when compared to higher polymer concentration. EVALUATION OF GELS Pothos scandens ALCOHOLIC EXTRACT WITH CARBOPOL 940 PHYSICAL OBSEVATION TABLE 3 Appearance PH Measurement EXTRUDABILITY A1 A2 A3 A4 A1 A2 A3 A4 A1 A2 A3 A4 Transparent with less gel consistency Transparent, ,Non greasy gel Slightly Translucent gel Translucent gel 7.0 7.2 6.9 7.1 ++ +++ +++ +++ ++ Good +++ Excellent 70 PHARMACOLOGICAL STUDIES PRIMARY SKIN IRRITATION TEST There was no sign of any kind of reaction, thus the ethanolic extract of Pothos scandens was found to be safe. WOUND HEALING STUDIES Excision wound healing studies showing percentage reduction in wound size in rats (% closure) TABLE-4 TEST DAYS RAT RBT RCT RDT RET RFT AVG 20% 22.42% 17.11% 19.92% 20.46% 18.46% 19.73% 4TH 43.16% 56.93% 30.80% 32.48% 31.96% 28.43% 37.29% 8TH 10TH 12TH 75.53% 87.18% 53.23% 59.49% 53.26% 57.85% 67.42% 83.62% 90.2% 75.29% 80.29% 82.13% 88.76% 83.38% TABLE-5 CONTROL DAYS RAC RBC RCC RDC REC RFC AVG 10.23% 9.76% 11.14% 12.28% 10.87% 13.73% 11.34% 4TH 17.87% 16.23% 19.23% 20.71% 16.58% 17.55% 18.03% 8TH 10TH 12TH 29.23% 27.12% 26.78% 27.25% 27.44% 25.43% 27.21% 34.47% 32.21% 35.46% 33.33% 34.86% 84.67% 34.17% RA , RB , RC , RD , RE - Designation for each rats C - Control T - Test 71 Graph 1 Average Percentage contraction of wounds in rats after treating with Carbopol 940 Avg % contraction of wounds 90 80 70 60 50 40 30 20 10 0 Test Control 4th day 8th day 10th day 12th day On the first day after the excision of skin wounds made at area of approximately 274mm.sq and its macroscopical studies were performed as percentage decrease in wound size. On the forth day, the average percentage decrease in wound size in test was found to be 19.73% and that of the control 11.34% On the eight day, the average percentage decrease in wound size in test was found to be 37.29% and that of the control 18.03% On the tenth day, the average percentage decrease in wound size in test was found to be 64.42% and that of the control 27.21% On the twelth day, the average percentage decrease in wound size in test was found to be 83.38% and that of the control 37.17% It was found that complete wound healing for the Test Formulation took place on 14th day and for the control has taken additional six days for the complete wound healing. So the given formulation of ethanolic extract of the plant Pothos scandens was affective in wound healing. 72 Chapter 9 Conclusion 73 Conclusion The plant Pothos scandens was selected for the study, whose extract was very useful in the treatment of wounds. Literature survey revealed that this plant is used traditionally for various ailments, especially for its wound healing property. Extensive scientific studies were not performed on this plant. Its wound healing property was not under taken for any scientific study. Hence the present work is performed. Form the present study entitled “FORMULATION & PHARMACOLOGICAL EVALUATION OF HERBAL GEL OF Pothos scandens” the following conclusions could be drawn. Physicochemical parameters both alcohol-soluble and water-soluble extractive values were determined and the results were tabulated in Table No.1 Preliminary phytochemical studies of 90% ethanolic extract were found to contain alkaloids, protein and flavanoid. Aqueous extract contain carbohydrate, protein, flavanoid and the results were tabulated in Table No. 2 Different gel formulations of the ethanolic extract were prepared using Carbopol 940 in varying proportions of 0.5, 1.0, 1.5 and 2.0%. On physical evaluation the gel consistency of Formulation A1 was less when compared to Formulation A2, A3, and A4. Formulation A3 and A4 were found to be translucent. But formulation A2 was found to be transparent, non greasy and stable. The PH of the formulation ranges from 6.8 to 7.6 and had an excellent Extrudability and the results were tabulated in Table No. 3. Hence Formulation A2 was selected for further study. Primary Skin Irritation test were performed for Formulation A2 and there was no signs of irritation. As no relevant data was available regarding the dose of topical application of the formulation, wound healing studies were carried out. Wound healing took place on 14th day in case of Test formulation and control has taken additional six days for complete wound healing. The results were shown in Table 4 and Table 5.Average % contraction of wounds in Rats were plotted against no: of days and was shown in Graph 1.Therefore, the given formulation of ethanolic extract of the plant Pothos scandens was affective in wound healing. 74 Chapter 10 Suggestions for future work 75 SUGGESIONS FOR FUTURE WORK In recent years the plant is not subjected to many research works as we know by the literature review. Different similar species were the subject of studies in many countries but the studies in Pothos scandens species were less. This may be due to the less availability of the plant, since it is on the verge of extinction. So lots of research works can be suggested in bringing this plant to limelight and its importance. Suggestions are made in the order of importance for work in pharmaceutical study in a stepwise manner. PHARMACOGNOSY Microscopical characteristics PHARMACEUTICAL ANALYSIS The real molecules responsible for the activity are not yet been identified and separated. In modern medical science the identity of the active molecule is essential for the further works. The future works in pharmaceutical analysis may include: TLC characterization that consists of: Preparation of plates Separation of components Selection of mobile phase Nature of substances to be separated Nature of the stationary phase Chromatographic mode 76 HPLC Characterization Schematic representation of HPLC The HPLC finger print Column Chromatographic Isolation FT-IR Analysis NMR PHARMACOLOGICAL STUDIES Anti-microbial activity Anti-inflammatory Anticonvulsant activity Anti-asthmatic Activity Other activity can be evaluated PHARMACEUTICAL STUDIES Studies on different formulation for its topical applications Oral dosage forms 77 Chapter 11 References 78 References 1. C.K.Kokate, A.P.Purohit, S.B. Gokhale, Pharmacognosy Page no: 105-108 2. Banker and Rhodes, Modern Pharmaceutics, 2nd edition, Marcel Deckker Inc, 1990, P.302 3. Lieberman H.A, Rieger M.M and Banker G.S., Pharmaceutical Dosage Forms –Disperse systems, Vol-2, Marcel Deckker Inc, 1989, Page No: 495-505 4. Collett and Aulton, Pharmaceutical Practice, ELBS,1993, Page No:127 5. http://en.wikipedia.org/wiki/Ski 6. Robbins Basic Pathology, 7th edition, Page No: 3-2 7. Bernard Testa, Gerd Folkers, Richard guy A Pharmacokinetic Optimization in drug Research. Page No: 18-19. 8. Udupa.K.N, Advances in Research in Indian Medicine, B.H.U. Publishers, Banaras, 1970, Page No: 270-303 9. www.Globemed.com 10.www.Noveon.com 11. www.sciencedirect.com 12. Grewal,-J-S, International-Journal-of-Environmental-Studies. 1993; 43(4), PageNo: 293- 295 13. Dhanavel,-D; Subramanian,-D Plant-Archives. 2004; 4(1): 81-88 14. T.B Harbuorne, Physiochemical methods. A Guide to Modern Techniques of Plant Analysis, 3rd Edition, Page no: 207-213 79 15. Trease and Evans, Pharmacognosy by W.C .Evans, 15th edition, Page No: 137-149. 16. S.S Handa and V.K Kapoor Text book of Pharmacognosy, 2nd Edition, Page no: 306-308 17. Mohammed Ali, Text book of Pharmacognosy, 2nd Edition, Page No: 58-59 18. Shah and Qadry’s Pharmacognosy, 12th Edition,Page No: 7-8 19. Vinod .D. Rangari Pharmacognosy & Phytochemistry. Part-1, 1st Edition, Page no: 99-100 20. Chien Y.N, Novel Drug Delivery Systems, Fundamentals, Developmental Concepts and Biomedical Applications, Marcell Deckker,N.Y ,Page No: 508-512. 21. P. Michael Conn, Sourcebook of Models for Biomedical Research, Page No: 63-65 22. Ghosh, Fundamentals of Experimental Pharmacology. 3rd Edition by Page No: 35-38 23. Carsten Ehrhard,Kwang-Jin Kim, Biotechnology: Pharmaceutical Aspects, Drug Absorption studies, In Situ, In Vitro and In Silico Models, Page No. 3-23. 80