Daily Progress Notes (The “SOAP” note)
advertisement
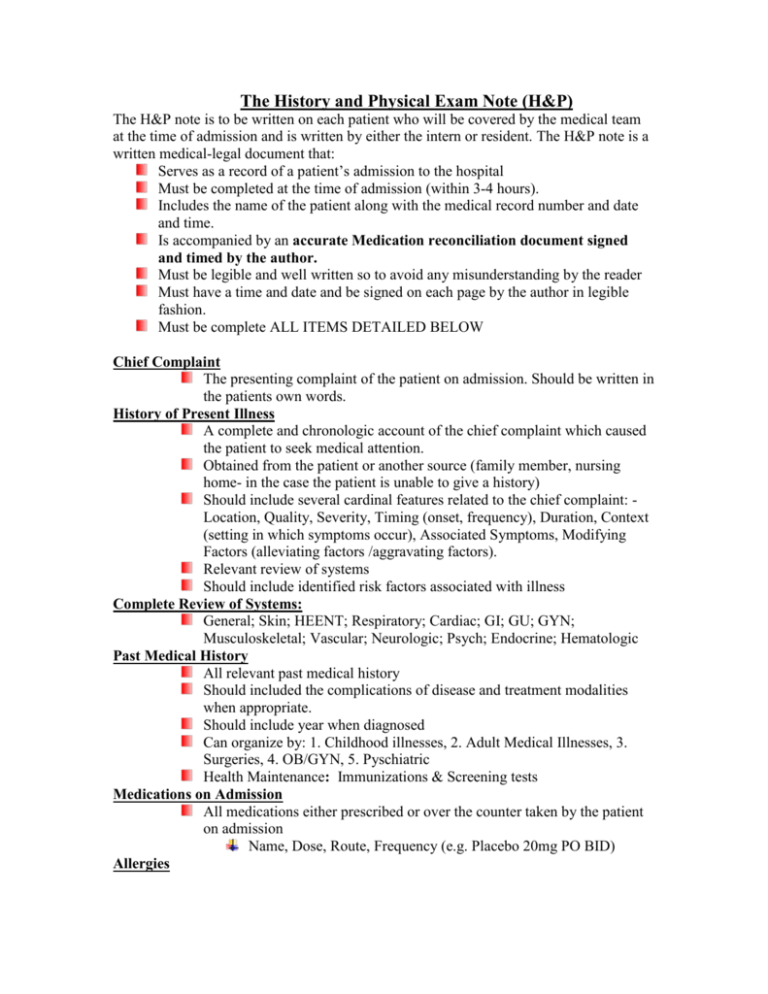
The History and Physical Exam Note (H&P) The H&P note is to be written on each patient who will be covered by the medical team at the time of admission and is written by either the intern or resident. The H&P note is a written medical-legal document that: Serves as a record of a patient’s admission to the hospital Must be completed at the time of admission (within 3-4 hours). Includes the name of the patient along with the medical record number and date and time. Is accompanied by an accurate Medication reconciliation document signed and timed by the author. Must be legible and well written so to avoid any misunderstanding by the reader Must have a time and date and be signed on each page by the author in legible fashion. Must be complete ALL ITEMS DETAILED BELOW Chief Complaint The presenting complaint of the patient on admission. Should be written in the patients own words. History of Present Illness A complete and chronologic account of the chief complaint which caused the patient to seek medical attention. Obtained from the patient or another source (family member, nursing home- in the case the patient is unable to give a history) Should include several cardinal features related to the chief complaint: Location, Quality, Severity, Timing (onset, frequency), Duration, Context (setting in which symptoms occur), Associated Symptoms, Modifying Factors (alleviating factors /aggravating factors). Relevant review of systems Should include identified risk factors associated with illness Complete Review of Systems: General; Skin; HEENT; Respiratory; Cardiac; GI; GU; GYN; Musculoskeletal; Vascular; Neurologic; Psych; Endocrine; Hematologic Past Medical History All relevant past medical history Should included the complications of disease and treatment modalities when appropriate. Should include year when diagnosed Can organize by: 1. Childhood illnesses, 2. Adult Medical Illnesses, 3. Surgeries, 4. OB/GYN, 5. Pyschiatric Health Maintenance: Immunizations & Screening tests Medications on Admission All medications either prescribed or over the counter taken by the patient on admission Name, Dose, Route, Frequency (e.g. Placebo 20mg PO BID) Allergies Allergies to medications (list of medications including specific reaction ellicited) Allergies to environmental agents Adverse drug reactions Social History Smoking and Drug History Marital Status Children Education Employment Housing/Living conditions Daily activities Important contact information Family History Medical history of all 1st degree relatives and relevant 2nd degree relatives. Code Status and Health Care Proxy Code status and name of Health care proxy. Physical Exam Vital Signs General Exam Physical exam of each body system Labortatory and Diagnostic Imaging All relevant labs and diagnostic imaging compared to prior results (it is important to compare with a “baseline” value.) Problem List From most important to least important Should be as detailed as possible. Assessment and Plan Each problem or group of problems should have a thorough assessment Differential diagnosis are discussed and evidence supporting the diagnosis (or arguing against them) should be outlined during the assessment of the problems. A detailed plan on each problem or set of problems should be generated Please see example below Each page of the H&P should be signed and dated. EXAMPLE A/P 1. Nausea / vomit / diarrhea: 50 y/o male with long standing complicated DM who presents with acute onset of fever, n/v/diarrhea and inability to take PO. Given his recent sick contact, normal WBC, and benign abdominal exam viral infection is highest on our differential diagnosis. However, in this long standing diabetic with known neuropathy possibility of other processes which include: occult cholecystitis, pancreatitis (high alcohol intake), and bacterial causes of diarrhea remain in our differential. Plan: IV hydration as outlined below Serial abdominal exams Add liver chemistries / amylase / lipase to labs done in ED Check stool for C.Dif, fecal leuks, O&P Check blood cultures / urine culture NPO for now – will reassess in AM KUB to r/o ileus/PSBO If any clinical decompensation will consider further imaging studies Hold antiHTN agents until no longer hypotensive 2. Acute on chronic renal failure: In this gentleman who has history of proteinuric CRF secondary to diabetes causes for his ARF include pre-renal, renal, and post renal causes. Highest in our differential dx. is pre-renal azotemia based on the clinical history, frank hypotension, tachycardia, metabolic alkalosis, concentrated urine and FENA <<1%. The possibility that this gentleman has developed ATN secondary to hypotension and NSAID use remains of concern. Other primary intrarenal causes seem unlikely. Pt has no history of urinary obstructive diseases making post renal causes unlikely. Plan: Check orthostatics now and in AM IV hydration: NS (with 40 meq KCL bolus x 1 liter over 2 hours. After bolus reassess BP / Orthostatics / cardiopulmonary exam and if remains hypotensive without signs of volume overload re-bolus. Once no longer hypotensive begin NS with 20 KCL at 100-200 cc per hour depending on urine output, vitals, and ongoing losses. Replete K Check MG Add Mg, PO4, Ca, Alb to labs done in ED Review urine sediment for evidence of ATN If U/O not increasing insert foley to r/o obstruction If CRT not improving by AM consider renal US D/C NSAIDS D/C Glucophage as contraindicated in renal failure Hold ACE until CRT at baseline Check urinary chloride to work-up metabolic alkalosis Repeat CBP in 4 hours – reassess K needs at that time Dose all meds for GFR 20-50cc/min Avoid nephrotoxic agents 3. Hyperglycemia: Uncontrolled DM secondary to inability to take oral hypoglycemic agents and acute illness. Plan: Hold Glucophage as described above IVF as described above Insulin SS for now – long acting insulin may be needed Accucheck QAC / QHS (or QID if NPO) Check GlycoHgB if not done in last 3 months Diabetic diet when taking PO 4. ETOH use: ETOH use is above healthy drinking guidelines Cage questionnaire when stable Review healthy drinking when stable Follow closely for DT’s over next 24-72 hours 5. Tobacco Abuse: Smoking cessation counseling to be given. 6. CAD: Stable. Obtain old EKG for comparison Resume B blocker when BP allows. Cont. ASA 7. Prophylaxis: Hep. SQ until able to be OOB TID