Online Figures Figure S1. Visualisation of atherosclerotic plaques
advertisement

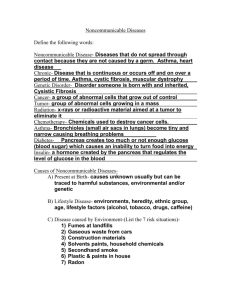
Online Figures 1 Figure S1. Visualisation of atherosclerotic plaques and aortic endothelial function. (A) An aorta from an old ApoE-/- mouse is shown intact and longitudinally sectioned (i), with plaques indicated by oil red O staining (red, arrows indicate same point in both images). The aortic arch showed very dense staining. For comparison, an aorta from a young ApoE-/- mouse (ii) and old WT mouse (iii) are shown. (B) Cumulative concentration response curves to ACh (top panel) and SLIGRL (bottom panel) in aortas from young WT and ApoE-/- mice in the absence (Control) and presence of 100 µM L-NAME (n=4-8). *P<0.05 compared with the control response of the same strain and age; †P<0.05 compared to WT. Figure S2. Cumulative concentration response curves to isoprenaline in mesenteric arteries from young WT and ApoE-/- mice (n=3). 2 Online Methods Solutions and Drugs Composition of the MOPS buffer (mM): NaCl 145.0, KCl 4.7, CaCl2·2H2O 2.0, MgSO4·7H2O 1.17, MOPS 2.0, NaH2PO4·H2O 1.20, glucose 5.0, pyruvate 2.0, EDTA 0.02 NaOH 2.75, and adjusted to pH 7.40 ± 0.02. All chemicals were purchased from Sigma (Poole, UK) with the exception of SLIGRL (Auspep, Australia); apamin and IbTx (Latoxan, Valence, France); Mac-3 antibody (BD Pharmingen, Europe); chicken anti-rat antibody IgG (H+L) and Oregon Green 488 BAPTA-1 (Invitrogen, UK). All stock solutions were prepared in distilled water with the exception of oil red O, dissolved in 60% aqueous triethyl phosphate; TRAM-34, dissolved in DMSO; and IbTx, dissolved in MOPS buffer. Prior to use in experiments all drugs were diluted in physiological buffer, and kept chilled (∼4°C). All inhibitors were added to the superfusion solution and the artery exposed for a minimum of 20 min prior to obtaining responses. Oil red O staining Mouse aortas or mesenteric beds were cleaned of connective tissue and fixed in 4% PFA for 24 hours at room temperature. After washing, tissues were rinsed with 60% aqueous triethyl phosphate, and 0.5% oil red O was applied intraluminally for 10 min. The vessels were then rinsed intraluminally with 60% aqueous triethyl phosphate followed by distilled water. Aortic segments were cut open longitudinally and pinned out on a sylgard base in phosphate buffer saline (PBS) intimal side up. The plaque size was measured offline following image capture with a Powershot A650 IS camera (Canon, UK) mounted on a Discovery V12 stereomicroscope (Zeiss, Germany). Arteries were also transferred onto 3 coverslips for imaging using the laser-scanning confocal microscope (FV500, Olympus Japan) with 40x/0.9NA objective (Olympus). Oil red O staining was visible following excitation at 633 nm, and simultaneous brightfield images were used to confirm the presence of plaques. Mac-3 immunohistochemistry Mac-3 (BD Pharmingen, 550292, purified rat anti-mouse, M3/84) staining was performed in mouse aorta and pressurized triple cannulated mouse mesenteric arteries. Aortas were fixed with 4% formaldehyde, permeablized using 0.1% Tween 20 for 10 min and rinsed in PBS solution. Following overnight incubation at 4°C in DAKO blocking solution (DAKO, X0909) with 3% BSA, the Mac-3 Ab (dilution 1:100) was added to DAKO blocking solution with 9% BSA, and the aorta was incubated in this solution for 2 hours at room temperature, followed by the 2º Ab (dilution 1:100, Invitrogen, A21470, Alexa Fluor® 488 chicken anti-rat IgG) for 45 min at room temperature. Propidium iodide was added to the bath to stain the nuclei and the aortas were cut in half and inserted between coverlips. From the same animals, and after functional experiments, the mesenteric arteries with bifurcations were fixed with 4% paraformaldehyde for 7 mins. The bath was then washed with PBS before the addition of blocking buffer (1% BSA and 0.1% Tween 20) to the bath and the lumen for 60 min at 37ºC. The lumen was perfused and bath contents replaced with Mac-3 Ab (dilution 1:100), and incubated overnight at 4ºC. The bath solution was then replaced with PBS and the lumen was perfused with 2º Ab (dilution 1:100 as above), which was incubated for 30 min at room temperature. The artery was washed in PBS containing propidium iodide to stain the nuclei. The arteries were visualized with a laser scanning confocal microscope (FV500, Olympus, Japan, excitation 488 nm for 2º Ab, and 633 nm for nuclei) and with a 40x/0.9NA objective (Olympus). 4 Artery isolation and cannulation The abdominal and thoracic aorta below the arch was cut into four 2 mm long segments and each was mounted in a 4-channel wire myograph using 40 µm wire (Danish MyoTech). Each artery was tensioned using the normalization programme as previously described 25, resulting in a resting tension near 5 mN. Second-order branches of the superior mesenteric artery were dissected, isolated, and cannulated as previously described (diameter 120 to 250 µm).8, 26, 27 Once pressurized, the absence of small side-branches was ascertained by a lack of diameter change following occlusion of all perfusion inflows. The MOPS-buffer solution was heated to 36.5 ± 0.2°C in all experiments, and arteries were pressurized by a gravity-fed inflow and outflow system. The assembly was secured to a block that was moved along a vertical track and held in position at the required height above the artery to maintain pressure. Arteries were pressurized to 60 mmHg, and for dilation experiments, were sub maximally contracted with phenylephrine (2–4 µM) to generate a consistent level of tone between treatments and preparations. Endothelial cell viability was assessed as > 90% relaxation to 3 µM SLIGRL. When arteries were imaged with video microscopy, outer diameter was measured online using vessel edge-detection software (DiamTrak, Neild, V3.5); whereas in those imaged using confocal microscopy. Smooth muscle cell membrane potential recordings in pressurized arteries An artery was cannulated and pressurized and placed in a custom-built chamber to minimize superfusion solution turbulence and backflow (volume 1 mL, width 6 mm, length 30 mm). Membrane potential was recorded via a pre-amplifier (Neurolog system, Digitimer Ltd., U.K.) linked to a MacLab data acquisition system (AD Instruments Model 4e, at 200 Hz). In one set of experiments, smooth muscle cell membrane potential was measured before 5 and during addition of 10 and 30 µM SLIGRL to the superfusion reservoir. In experiments examining the upstream spread of hyperpolarization, a glass micropipette (tip ~ 5 µm) filled with 1 mM SLIGRL was positioned using a micromanipulator independent of the microscope, either near the recording microelectrode (0 mm) or 1.0 mm downstream from the electrode. The pipette was advanced carefully until it just touched the adventitia, then stepped back to a position <20 μm from the artery. The direction of superfusion solution flow was checked using microspheres and shown to occur from upstream to downstream. The SLIGRL was pressure-pulse ejected for 30, 50, or 100 ms onto arteries without pre-constriction. In all experiments the superfusion flow was continuously on, and set to between 1 and 2 mL/min. Endothelial cell Ca2+ in pressurized arteries In separate experiments, mesenteric artery segments were mounted in a small chamber seated in a heated stage as described above. Images were captured with a laser scanning confocal microscope (FV1000-MPE, Olympus, Japan, excitation 488 nm) and recorded with Fluoview Software (FV10-ASW version 2.01, Olympus, Japan). After an equilibration period, the pressurized artery was luminally-perfused with filtered (0.2 µm pore) MOPS-buffered solution containing a cell-permanent acetoxymethyl ester form of Oregon Green 488 1,2-bis(2-aminophenoxy) ethane-N,N,N’,N’-tetraacetate (Oregon Green 488 BAPTA-1 AM, 2 µM) and 0.025 % Pluronic F-127 for 60 min to load endothelial cells. Due to the rapid loss of dye from endothelial cells, the dye remained in the lumen of the artery to maintain cellular levels throughout experiments. Endothelial cell fluorescence intensity was visualised towards the bottom of the artery, and if smooth muscle cell fluorescence was evident, the focal plane was moved towards the vessel midplane to ensure endothelial cell fluorescence was clearly discernible from smooth muscle cells. In a 512 x 148 pixel clip box, at least 10 cells were visible (40x/1.15 NA water immersion objective, 6 Olympus) and were recorded at a frequency of 3 Hz. Changes in endothelial cell [Ca2+]i were investigated in response to bath addition of SLIGRL (1 and 10 µM). In some experiments, 10µM Alexa Fluor 633 hydrazide was used to clearly and simultaneously visualize the internal elastic lamina (IEL) and other elastin structures. This allowed subtle changes in artery movement to be detected, which was useful for assessing small artefacts associated with changes in endothelial cell focal plane when the confocal pinhole was small (~100 µm). Conducted dilation to luminally perfused agonists In this series of experiments, three cannulation pipettes were used as previously described (Winter & Dora, 2007). Three ends of a branched isolated artery were cannulated and continuously superfused at 2 ml/min with MOPS solution. The upstream end of the artery (Feed artery) and one side of the bifurcation (Branch 2) were attached to gravity-fed pressurizing syringe reservoirs. The upstream and downstream perfusion pressures through the Feed artery were adjusted to generate luminal flow (7–9 cmH2O gradient, 10–30 μl/min flow) whilst maintaining a constant average transmural pressure, in order to avoid upstream flow of infused agonists. Phenylephrine was added to the superfusion solution, and each agonist used to study conducted dilation in the Feed artery was infused into one of the sidebranches (Branch 1) for at least 2 min at 20 μl/min using a BeeHive® syringe pump system (Bioanalytical systems, USA). In all experiments the movement of perfusion solution was monitored by including 0.1 μM carboxyfluorescein in the agonist solution. Under no conditions did flow itself stimulate dilation in mouse mesenteric arteries. Arteries were visualized using a laser scanning confocal microscope (FV500-SU, Olympus, Japan, excitation 488 nm) to enable simultaneous fluorescence and brightfield imaging, with a 4x/0.13 NA objective (UplanFl, Olympus, Japan), and images were recorded with Fluoview software (Olympus, USA) at 1 Hz. There was a short delay in observing responses to luminal 7 perfusion of agonists due to voiding the tubing and pipette dead-space volume. For all measurements of conducted dilation, artery outer diameter was measured offline using motion analysis software (MetaMorph, Universal Imaging, USA). This enabled simultaneous analysis of multiple, calibrated distances along the artery wall, and direct comparisons of local dilation to conducted dilation for a single application of agonist. Fluorescence intensity was also measured offline simultaneously at multiple positions in the lumen of arteries, which was temporally matched to diameter measurements. Feed artery diameter was only measured if no upstream flow of fluorescent indicator was detected, as previously shown (Winter & Dora, 2007). Since the extent of conducted dilation would be influenced by the magnitude of the local response, a maximal concentration of SLIGRL (30 µM) was used, and values at all sites along the vessel taken at the time at which 80% of maximum dilation was observed at the 0.0 mm site in the Feed artery. When dilation to ACh did not reach 80% of maximum diameter at the 0.0 mm site, the peak response at 0.0 mm was used together with the simultaneous responses at the other sites along the vessel. 8