questions of the web
advertisement

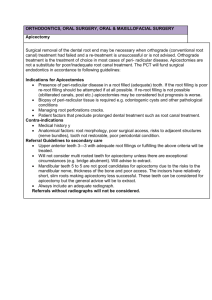
What are the elements of a SOAP note used for patient assessment? What should a patient be hospitalized for routine oral surgical procedures? What are the basic technical considerations in performing an incision? What factors influence the placement of incisions in the mouth? For making an incision in epithelial surface, how should the scalpel blade be oriented? What are the principles of flap design? What are the most frequent causes of the tearing of mucogingival flap? What are the means of promoting hemostasis? Describe and discuss the function of Allis forceps in oral surgery? What are the indications for tooth transplantation? Which teeth are most often transplanted? What is genioplasty? How are facial and palatal clefts classified? What is the role of the general dentist in managing oral cancer? What are the major oral side effects of radiation to the head and neck? What is the most common suture method? What are its advantages/ What are the advantages of continuous suture? What are the factors that determine the type of suture to be used? What forceps are typically used for the removal of mandibular teeth? What forceps are typically used for the removal of maxillary teeth? What are the components of extraction forceps? When should intraoral sutures be removed? What are the principles of suturing technique? What is the difference between monofilament and polyfilament sutures? What are the types of resorbable suture? Nonresorbable sutures? How are sutures sized? Name the indications for tooth extraction What are the major contrindcations for tooth extraction? What factors affect the difficulty associated with tooth extraction? What conditions may influence the difficulty of extraction? How are cases classified according to their difficulty? What are the major forces used for tooth extraction? What is the most common complication of tooth extraction? How can it be prevented? What are the major complications of tooth extraction? Should all impacted third molars be extracted? What are the indications for third molar extraction? What are the steps in postoperative management of an extraction site? What principles guide the use of elevators in tooth extraction? For multiple extractions, what is the appropriate order of tooth removal? Which tooth root is most likely to be displaced into an unfavorable anatomic site during extraction? Describe the prevention and treatment of postoperative bleeding? What is a dry socket? How can dry socket be prevented? How is dry socket treated? Describe pain control after extraction Which teeth are most commonly impacted? When infection erodes through the cortical plate, it does so in predictable manner. What factors determine the location of infection from a specific tooth? How is incision and drainage of soft tissue best performed? What is the treatment of choice for an odontogenic abscess? What are the principles of therapy for odontogenic infections as defined by Peterson? What are the significant complications of untreated odontogenic infection? What are the three clinical stages of odontogenic infection? What are the major origins of odontogenic infection? State the usual site of bone perforation, the relationship to muscle attachment, the determining muscle, and the site of localization for each tooth odontogenic infection? What is osteoradionecrosis? What are the indications for hospitalization of patients with infection? Despite the advent of numerous new antibiotics, penicillin remains the drug of choice for odontogenic infection. Why? What are alternative antibiotics for patients who are allergic to penicillin? What is the antibiotic of choice for odontogenic infection? What is cavernous sinus thrombosis? What is Ludwing's angina? What are the secondary fascial spaces? What are the primary mandibular fascial spaces? What are the primary maxillary fascial spaces? What are fascial space infections? What are the indications for antibiotic therapy in orofacial infection? What is the major side effect associated with erythromycin? What factors govern the selection of particular antibiotics? When should cultures be used for odontogenic infection? Why may antibiotics therapy fail? Why is penicillin V more desirable than penicillin G for the treatment of odontogenic infection? Does the initiation of antibiotic therapy obviate the need for surgical intervention in a patient with an infection? What are the most important questions to ask in evaluating a patient with acute trauma? Describe the following terms in relation to injuries involving the supporting structures of the dentition: concussion, subluxation, intrusion, extrusion, lateral luxation, avulsion. What should be included in the clinical evaluation of the traumatized dentition? How should an avulsed tooth be managed? What are the four best ways for a patient to preserve a recently avulsed tooth until he or she is seen by a dentist? What are the diagnostic methods of choice for evaluation of the pediatric patient with trauma? Discuss the primary assessment and management of the patient with trauma? What are the types and characteristics of the resorption phenomenon that may follow a traumatic injury: inflammatory external and internal resorption, replacement resorption. When resorption can be detected radiographically? Why should radiographs of the soft tissue be included in evaluation of a patient with dental trauma? When a lip laceration is encountered, what part of the lip is the most important landmark and the first area to be reapproximated? How should a small avulsion of the lip managed? How should a full-thickness, mucosa to skin laceration of the lip be closed/ which layers should be sutured? How should a facial laceration that extends into dermis or fat be closed/ What are the most likely signs and symptoms of a mandibular body or angle fracture/ Describe the management of type of dental fractures? What is a dentoalveolar fracture? How is it treated? What structures are at risk when a facial laceration occurs posterior to the anterior margin of the master muscle and inferior to the level of the zygomatic arch? Why is a layered closure important? How is a displaced fracture of the mandibular body or angle treated? What are the two caused of displacement of mandibular fracture? Are most fractures of the mandibular condyle treated by closed or open reduction? What radiographs are used to diagnose mandibular fractures? What are the likely signs and symptoms of a zygomatic fracture? Which radiographs are used to evaluate and diagnose zygomatic fractures/ Which bones articulate with zygoma? How may mandibular function be affected by a fracture of the zygoma or zygomatic arch? What are the symptoms and treatment for inadvertent injection of the facial nerve during administration of local anesthesia? Describe the best type of injections of local anesthesia for extractions of the upper and lower posterior teeth. Which nerves are anesthetized using the Gow-gate technique? How significant is the concentration of epinephrine in local anesthetic solution in affecting the hemostatic properties? What are the advantages of including epinephrine in local anesthetic solution? What is the role of PH in determining the effectiveness of a local anesthetic? What are the major classifications of local anesthetics used in dentistry? How does a hematoma form after the administration of a local anesthetic, How is it treated? What are the reasons for post injection pain following the administration of a local anesthetic? What causes blanching of the skin after the injection of local anesthesia? What is the toxic dose of most local anesthetics used in dentistry. What is the maximal volume of a 2% solution of local anesthetic that can be administered? What is the most common adverse reaction to local anesthesia, How is it treated? What are the principal components of postoperative orders? What is secondary hemorrhage? How is it treated? What is primary hemorrhage? How should it be treated? What are the causes of postoperative swelling after an oral surgical procedure? What is postoperative ecchymosis, How does it occur? How is it treated? What are the four ways that dead space can be eliminated? What is dead space means? Describe the stages of wound healing? What is the difference between healing by primary and secondary intention? What are the five phases of healing of extraction wound? What are dental implants? Describe the differences in the bone-implant interface between osseointegrated implants and blade implants. What type of implants is currently favored? What are the requirements for successful implant placement? The surgical placement of most osseiointegrated implants usually requires two steps. What are the, How long between them? Do any data suggest that osseointegration of implants may occur when implants are placed into an extraction site? What is the best way to ensure proper implant placement and orientation? During preparation of the implant recipient site, What is the maximum temperature that should develop at the drill-bone interface? Which radiographic studies are used for patient prior to implant placement? What is the prognosis of osseiointegrated implants placed in an edentulous mandible? What are some contraindications for the placement of implants? Describe some of the indications for the considerations of implants and treatment alternative. What anatomic features of the anterior maxilla must be evaluated prior to placement of an implant in the central incisor region? Which anatomic site is the most likely to yield failed implants? Are there definitive data to support the contention that implanted supported teeth should not be splinted to natural teeth? Is there any reason to avoid the use of fluoride in implant recipients? Do implants need periodic maintenance once they are placed? What is the most common sign that an implant is failing/ What is trigeminal neuralgia? Discuss the treatment of trigeminal neuralgia? What symptoms are associated with TMD? What are the two most common joint sounds associated with TMD, How do they different? What are the diagnostic criteria for myofacial pain syndrome? What patient group is at highest risk for MPD? What occlussal factors may contribute to MPD? What is the etiology of MPD? What is the most common disorder associated with the TMJ? What is the likelihood that a patient with TMJ symptoms will demonstrate identifiable pathology of the joint? What radiographic and imaging studies are of value in evaluating TMJ? What are parameters for normal mandibular motion? What should be included in the physical examination of the patient with TMJ symptoms? What are the components of evaluation of the patient with TMJ symptoms? What signs and symptoms are associated with MPD? What radiographic findings are associated with MPD? Describe the treatment approach to MPD? What are the indications for superficial heat in treatment of facial muscle and TMJ pain? What are the contraindications for using superficial heat to treat facial pain? What is the function of ultrasound in the therapy of myofacial pain? What is internal derangement of the TMJ? What are the main categories of internal derangement? What are the common symptoms of internal derangement? What imaging techniques are useful in the diagnosis of internal derangement? What is the treatment of internal derangemenet? What are the most common causes of ankylosis of the TMJ? Are tumors of the TMJ common? What is the effect of orthodontics therapy on the development of TMD? What about extraction therapy? What are degenerative diseases can affect the TMJ.